ACLS MEDICATIONS AND THEIR USE Garrett Thompson Pharm




- Slides: 37
ACLS MEDICATIONS AND THEIR USE Garrett Thompson, Pharm. D. Wake Forest University Baptist Medical Center 11/25/2020 1
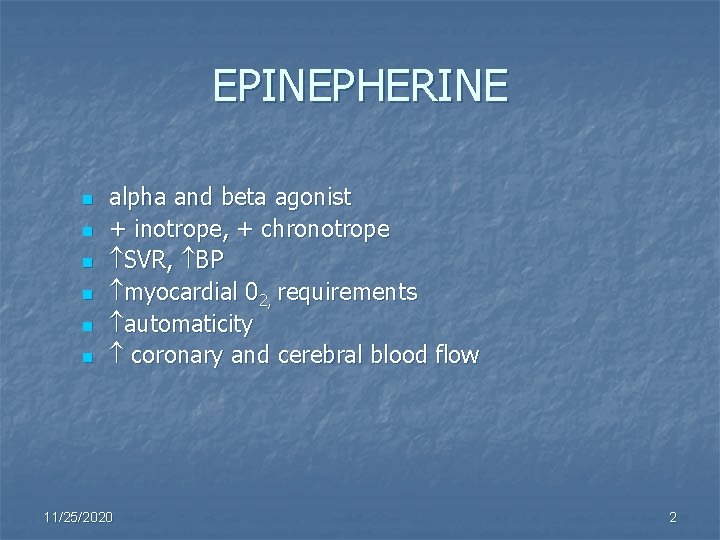
EPINEPHERINE n n n alpha and beta agonist + inotrope, + chronotrope SVR, BP myocardial 02, requirements automaticity coronary and cerebral blood flow 11/25/2020 2
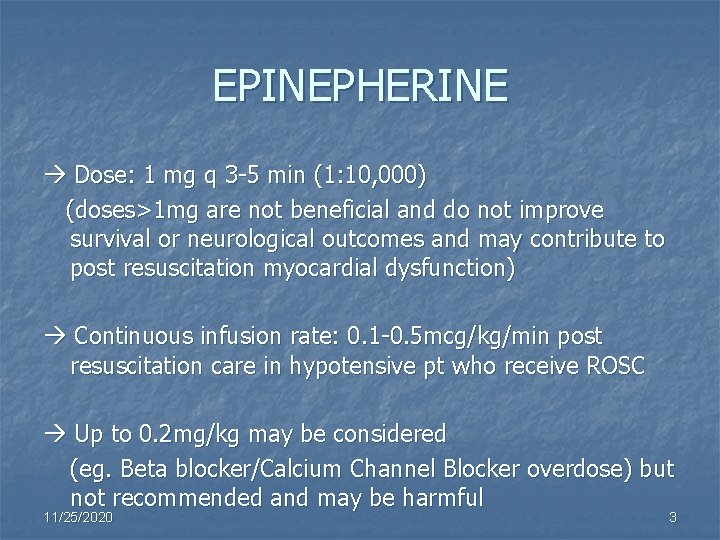
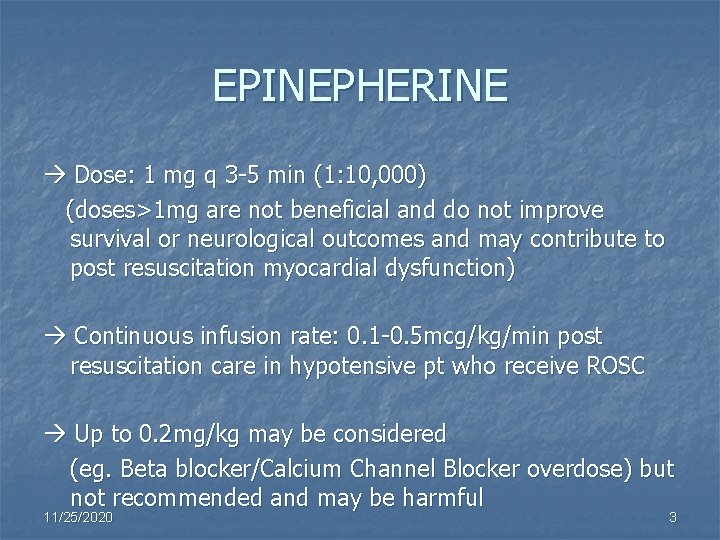
EPINEPHERINE Dose: 1 mg q 3 -5 min (1: 10, 000) (doses>1 mg are not beneficial and do not improve survival or neurological outcomes and may contribute to post resuscitation myocardial dysfunction) Continuous infusion rate: 0. 1 -0. 5 mcg/kg/min post resuscitation care in hypotensive pt who receive ROSC Up to 0. 2 mg/kg may be considered (eg. Beta blocker/Calcium Channel Blocker overdose) but not recommended and may be harmful 11/25/2020 3
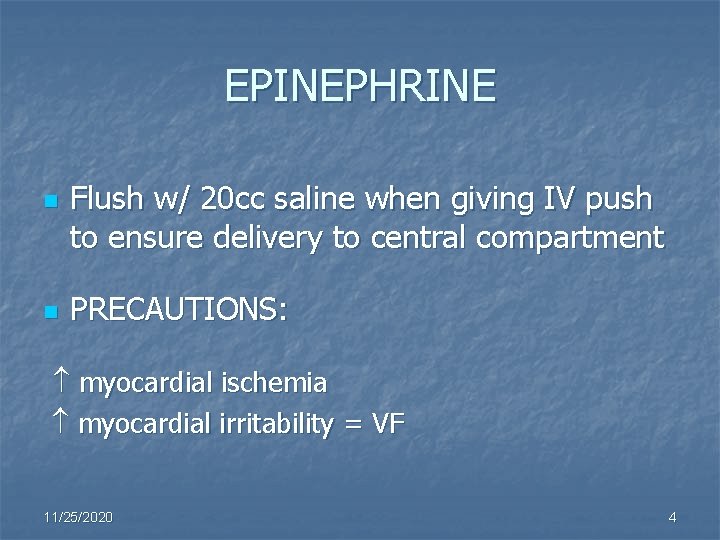
EPINEPHRINE n n Flush w/ 20 cc saline when giving IV push to ensure delivery to central compartment PRECAUTIONS: myocardial ischemia myocardial irritability = VF 11/25/2020 4
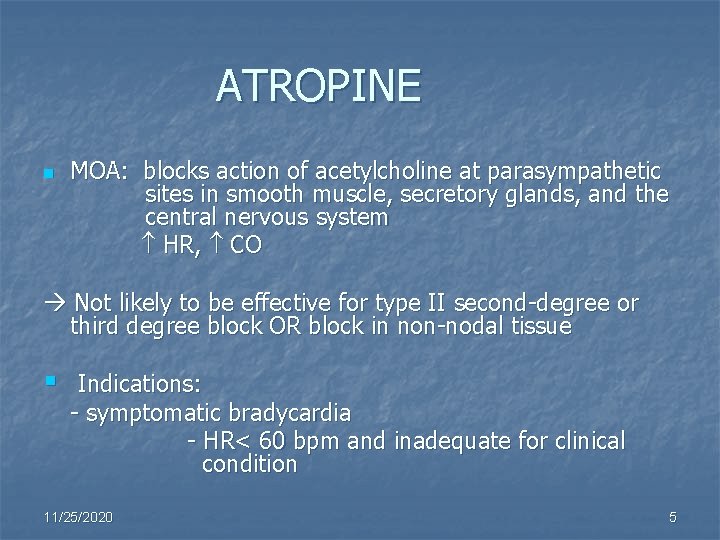
ATROPINE n MOA: blocks action of acetylcholine at parasympathetic sites in smooth muscle, secretory glands, and the central nervous system HR, CO Not likely to be effective for type II second-degree or third degree block OR block in non-nodal tissue § Indications: - symptomatic bradycardia - HR< 60 bpm and inadequate for clinical condition 11/25/2020 5
ATROPINE n Treatment considerations are based on adequate perfusion OR n S/S of poor perfusion caused by the bradycardia (Pacing, Atropine 0. 5 mg, Epi, Dopamine) 11/25/2020 6
ATROPINE n § DOSE: 0. 5 mg q 3 -5 min for symptomatic bradycardia Max. = 3 mg (usually 2 -3 mg is a full vagolytic dose in most patients) Side Effects: HR, coma, flushed hot skin, ataxia, blurred vision, myocardial ischemia 11/25/2020 7
MAGNESIUM SULFATE n n § MOA: physiological calcium channel blocker Indications: Torsades de pointes Hypomagnesemic states that may lead to arrhythmias Cardiac Arrest Dose: VT, Torsades = 1 – 2 grams § mix in 10 ml D 5 W IV/IO over 5 – 20 min. Torsades w/ pulse or AMI w/ hypomagnesemia - 1 – 2 grams in 50 – 100 ml D 5 W over 5 – 60 min IV/IO then 0. 5 gm – 1 gm / hr § Side Effects: flushing, sweating, mild HR/BP 11/25/2020 8
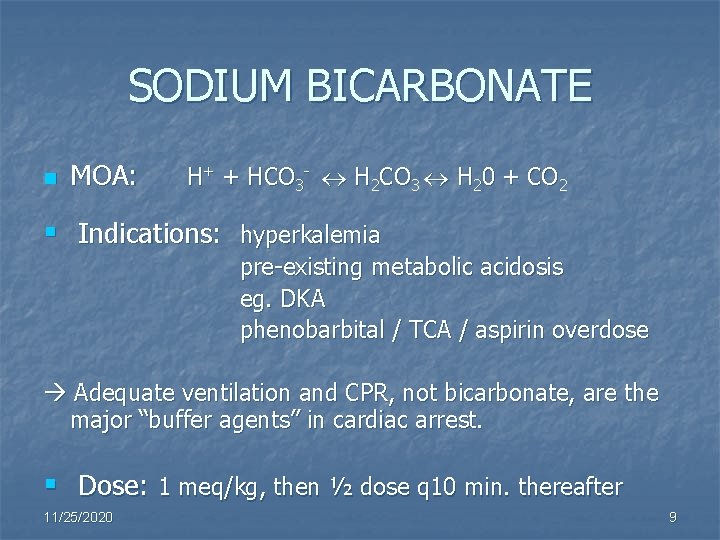
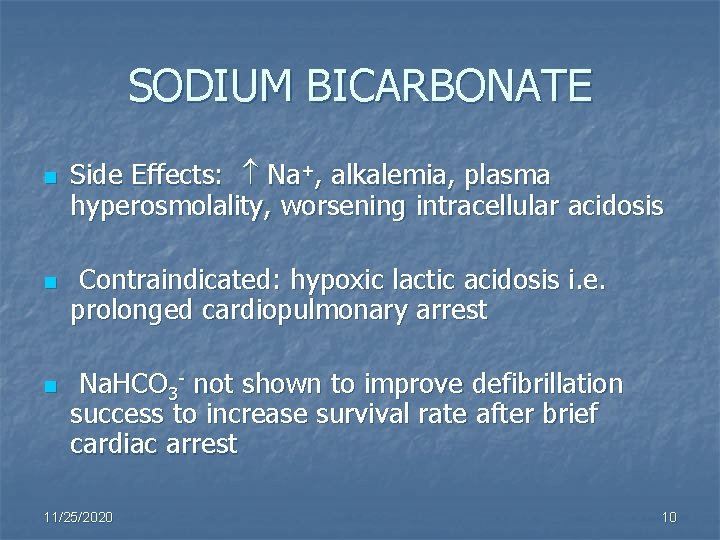
SODIUM BICARBONATE n MOA: H+ + HCO 3 - H 2 CO 3 H 20 + CO 2 § Indications: hyperkalemia pre-existing metabolic acidosis eg. DKA phenobarbital / TCA / aspirin overdose Adequate ventilation and CPR, not bicarbonate, are the major “buffer agents” in cardiac arrest. § Dose: 1 meq/kg, then ½ dose q 10 min. thereafter 11/25/2020 9
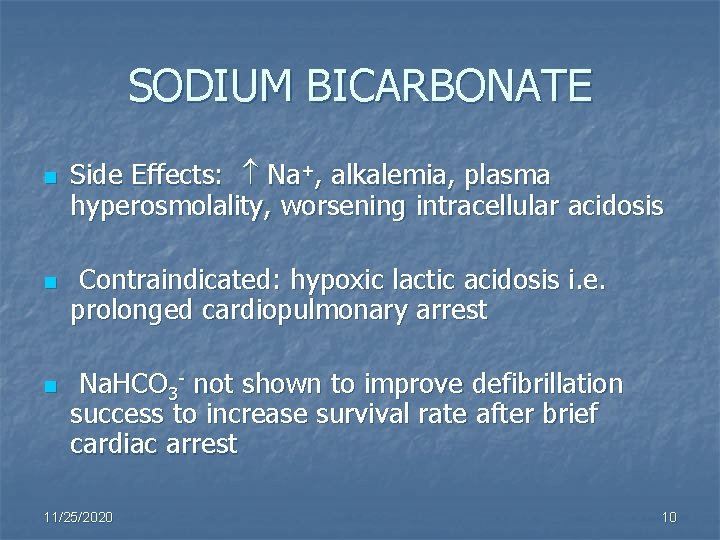
SODIUM BICARBONATE n n n Side Effects: Na+, alkalemia, plasma hyperosmolality, worsening intracellular acidosis Contraindicated: hypoxic lactic acidosis i. e. prolonged cardiopulmonary arrest Na. HCO 3 - not shown to improve defibrillation success to increase survival rate after brief cardiac arrest 11/25/2020 10
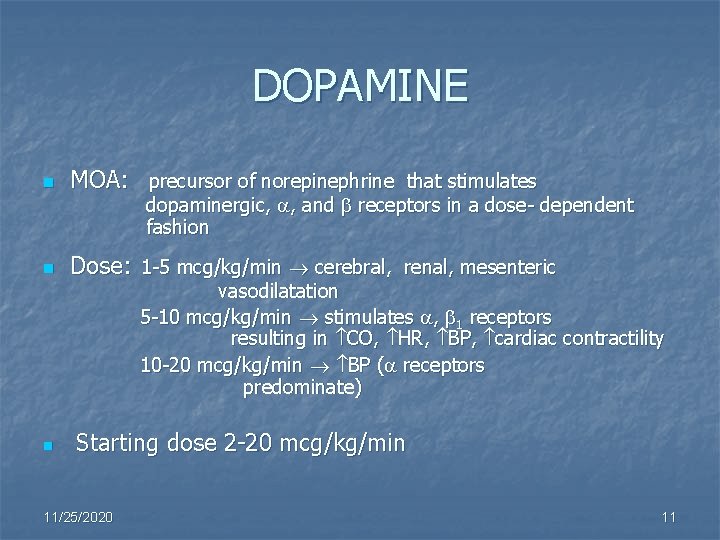
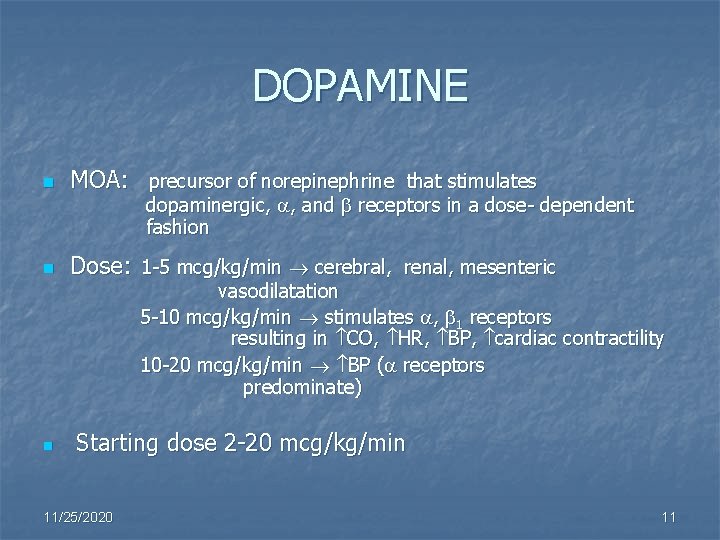
DOPAMINE n MOA: precursor of norepinephrine that stimulates n Dose: 1 -5 mcg/kg/min cerebral, renal, mesenteric n dopaminergic, , and receptors in a dose- dependent fashion vasodilatation 5 -10 mcg/kg/min stimulates , 1 receptors resulting in CO, HR, BP, cardiac contractility 10 -20 mcg/kg/min BP ( receptors predominate) Starting dose 2 -20 mcg/kg/min 11/25/2020 11

DOPAMINE n Indications: severe symptomatic bradycardia (after atropine), hemodynamically significant hypotension in absence of hypovolemia After : pacing, atropine, - start dopamine or epinephrine drip (2 -10 ug/min) n Side Effects: HR, induce /exacerbate arrhythmias, exacerbate pulmonary congestion and compromise CO, tissue sloughing if extravasation occurs ****Do not administer w/ sodium bicarbonate**** 11/25/2020 12
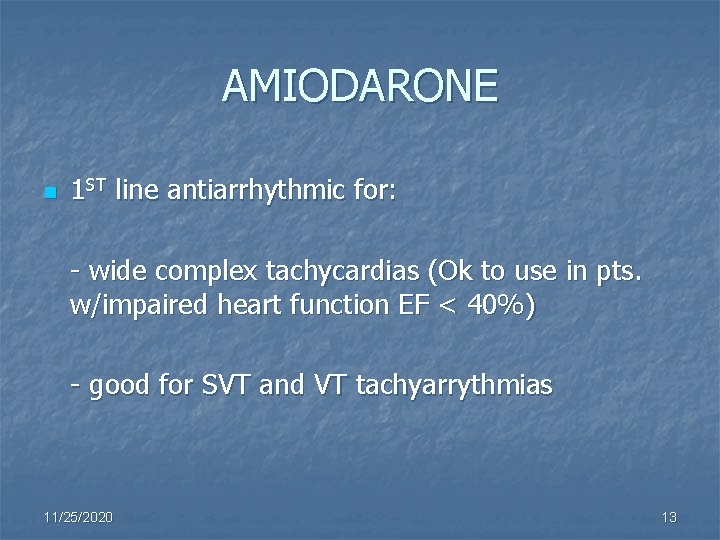
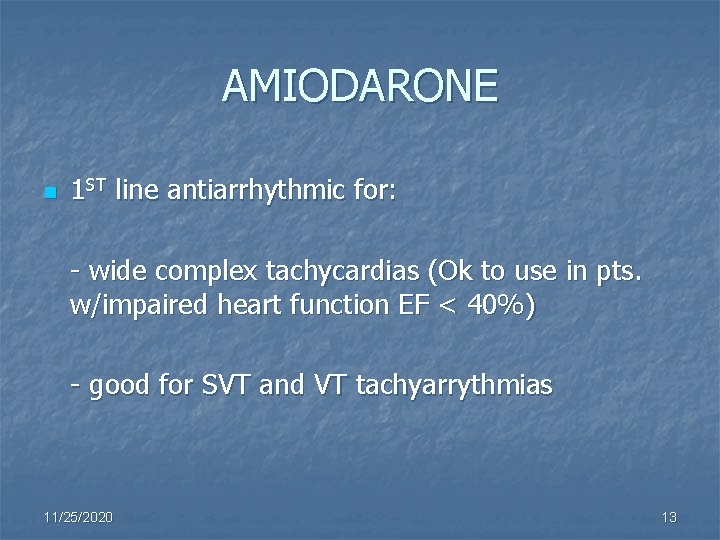
AMIODARONE n 1 ST line antiarrhythmic for: - wide complex tachycardias (Ok to use in pts. w/impaired heart function EF < 40%) - good for SVT and VT tachyarrythmias 11/25/2020 13
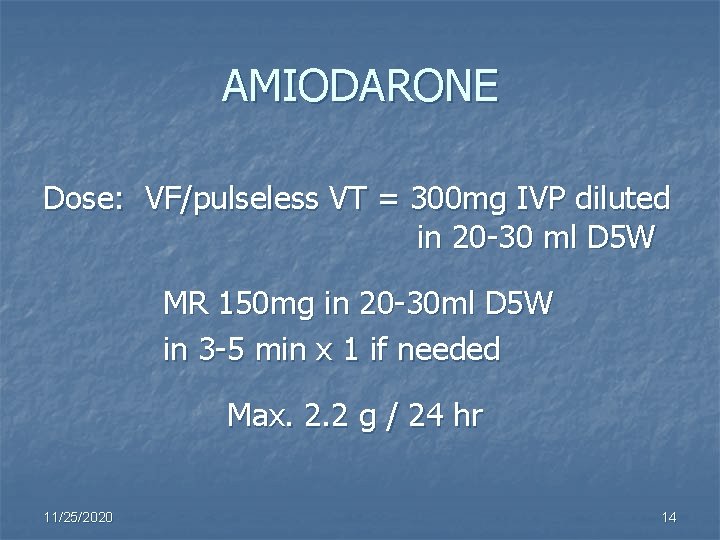
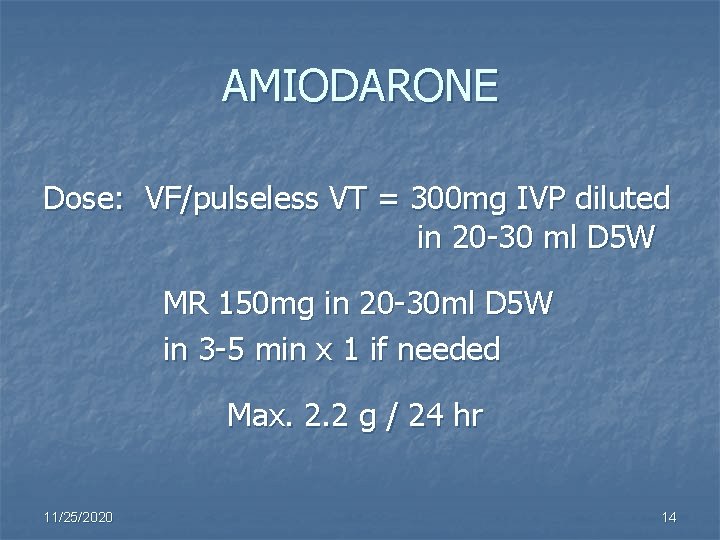
AMIODARONE Dose: VF/pulseless VT = 300 mg IVP diluted in 20 -30 ml D 5 W MR 150 mg in 20 -30 ml D 5 W in 3 -5 min x 1 if needed Max. 2. 2 g / 24 hr 11/25/2020 14
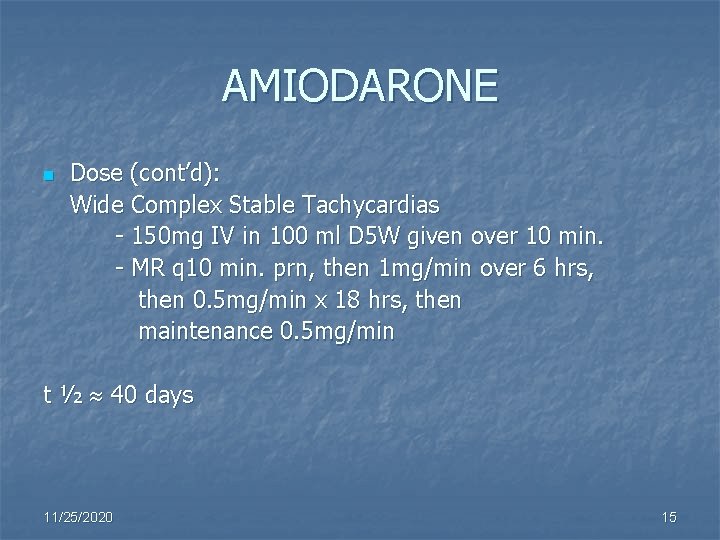
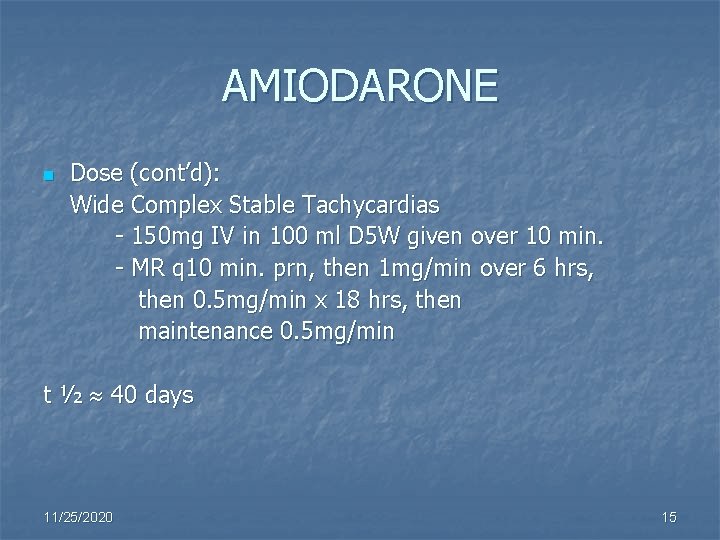
AMIODARONE n Dose (cont’d): Wide Complex Stable Tachycardias - 150 mg IV in 100 ml D 5 W given over 10 min. - MR q 10 min. prn, then 1 mg/min over 6 hrs, then 0. 5 mg/min x 18 hrs, then maintenance 0. 5 mg/min t ½ 40 days 11/25/2020 15
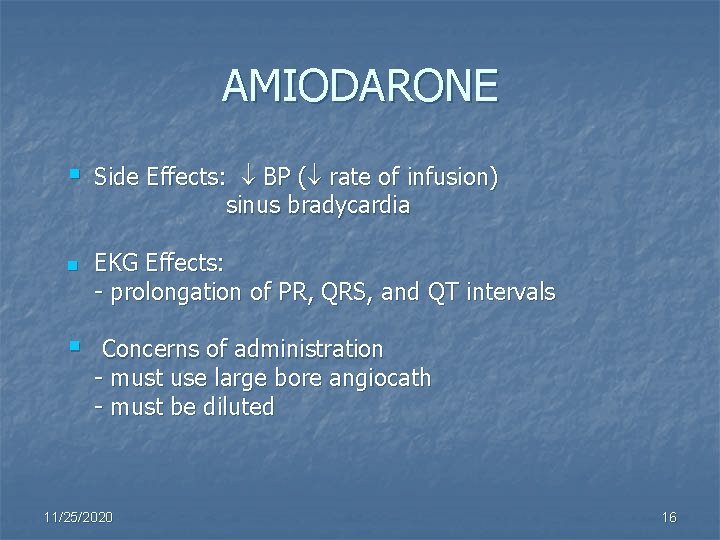
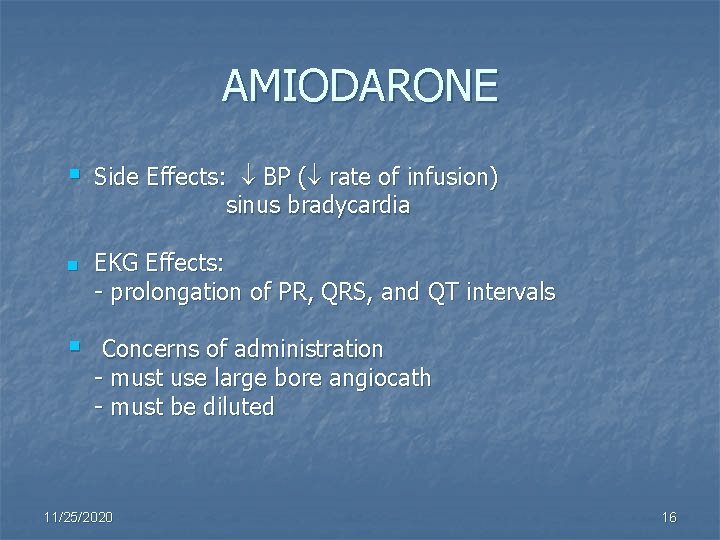
AMIODARONE § n § Side Effects: BP ( rate of infusion) sinus bradycardia EKG Effects: - prolongation of PR, QRS, and QT intervals Concerns of administration - must use large bore angiocath - must be diluted 11/25/2020 16
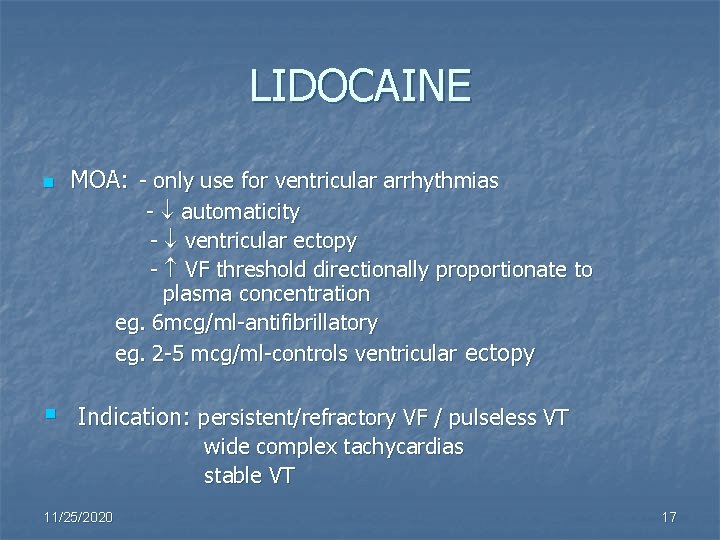
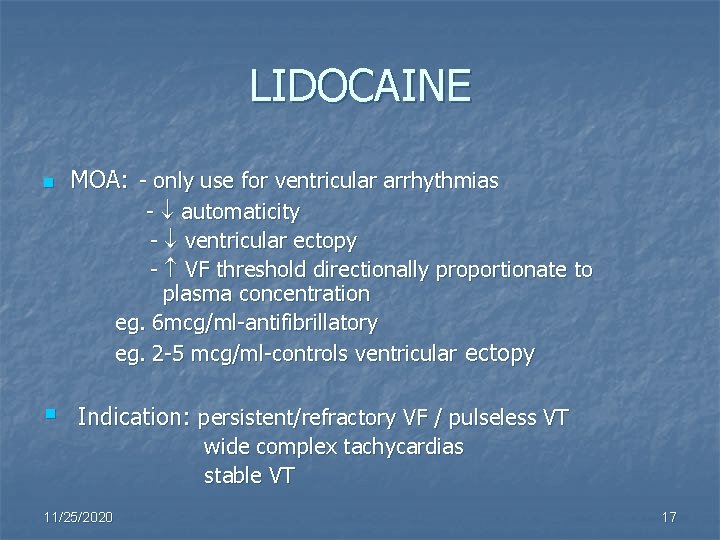
LIDOCAINE n MOA: - only use for ventricular arrhythmias - automaticity - ventricular ectopy - VF threshold directionally proportionate to plasma concentration eg. 6 mcg/ml-antifibrillatory eg. 2 -5 mcg/ml-controls ventricular ectopy § Indication: persistent/refractory VF / pulseless VT 11/25/2020 wide complex tachycardias stable VT 17
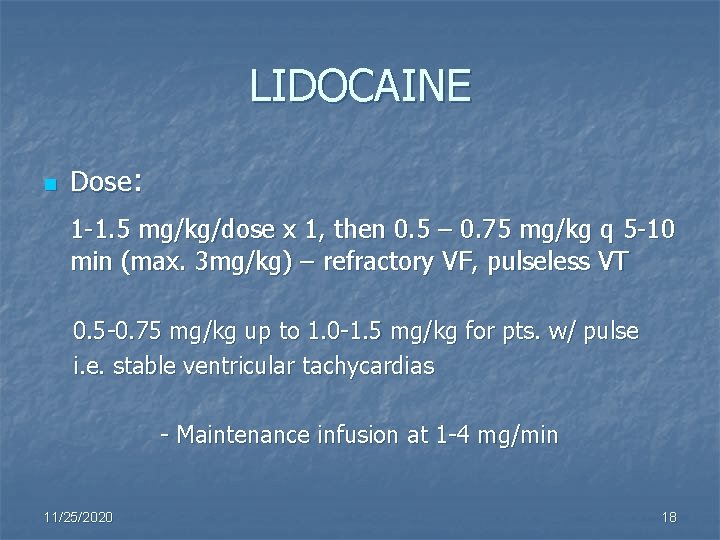
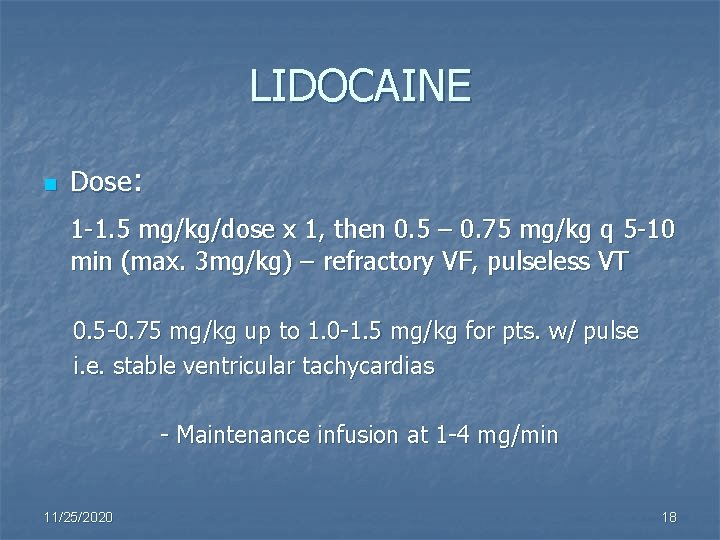
LIDOCAINE n Dose: 1 -1. 5 mg/kg/dose x 1, then 0. 5 – 0. 75 mg/kg q 5 -10 min (max. 3 mg/kg) – refractory VF, pulseless VT 0. 5 -0. 75 mg/kg up to 1. 0 -1. 5 mg/kg for pts. w/ pulse i. e. stable ventricular tachycardias - Maintenance infusion at 1 -4 mg/min 11/25/2020 18
LIDOCAINE Side Effects: muscle twitching focal / grand mal seizures 11/25/2020 19
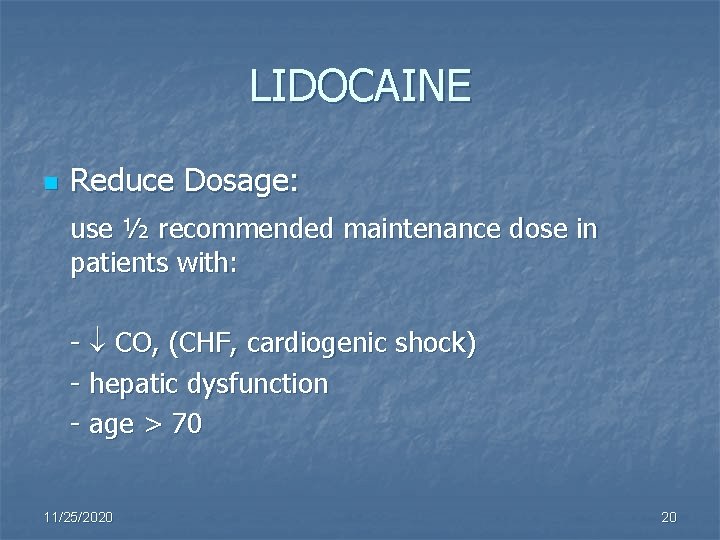
LIDOCAINE n Reduce Dosage: use ½ recommended maintenance dose in patients with: - CO, (CHF, cardiogenic shock) - hepatic dysfunction - age > 70 11/25/2020 20
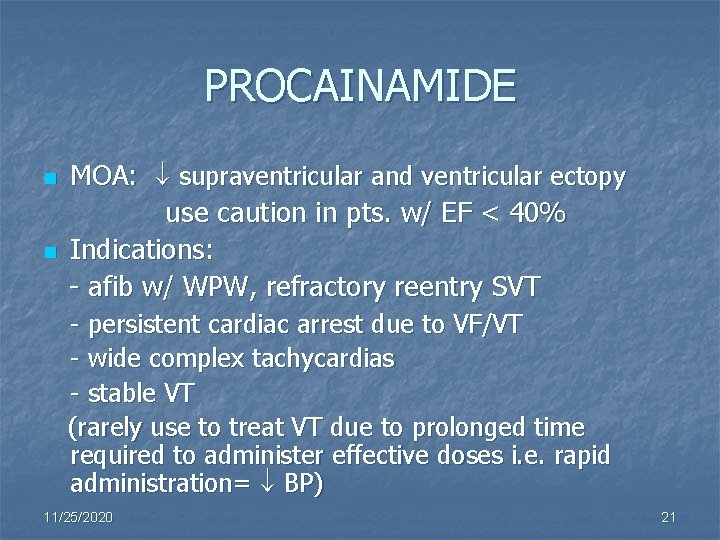
PROCAINAMIDE n n MOA: supraventricular and ventricular ectopy use caution in pts. w/ EF < 40% Indications: - afib w/ WPW, refractory reentry SVT - persistent cardiac arrest due to VF/VT - wide complex tachycardias - stable VT (rarely use to treat VT due to prolonged time required to administer effective doses i. e. rapid administration= BP) 11/25/2020 21
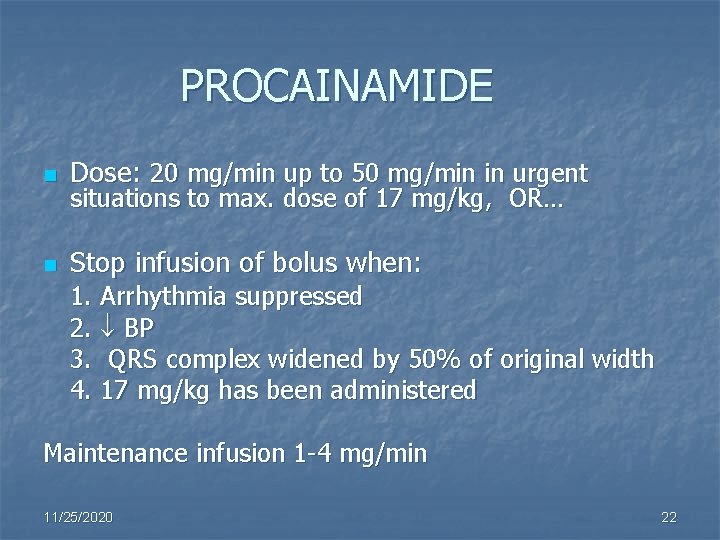
PROCAINAMIDE n Dose: 20 mg/min up to 50 mg/min in urgent n Stop infusion of bolus when: situations to max. dose of 17 mg/kg, OR… 1. Arrhythmia suppressed 2. BP 3. QRS complex widened by 50% of original width 4. 17 mg/kg has been administered Maintenance infusion 1 -4 mg/min 11/25/2020 22
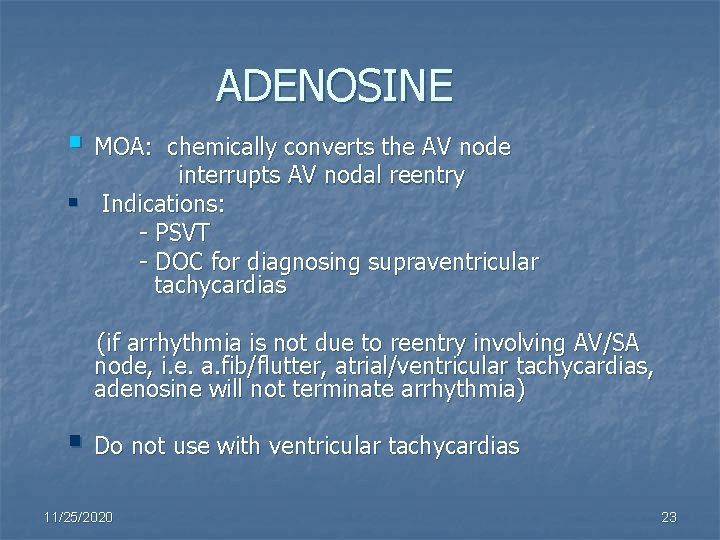
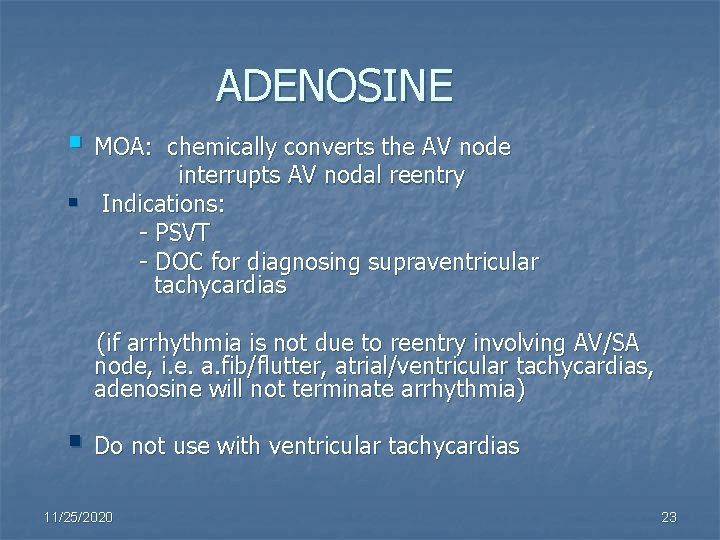
ADENOSINE § MOA: chemically converts the AV node interrupts AV nodal reentry § Indications: - PSVT - DOC for diagnosing supraventricular tachycardias (if arrhythmia is not due to reentry involving AV/SA node, i. e. a. fib/flutter, atrial/ventricular tachycardias, adenosine will not terminate arrhythmia) § Do not use with ventricular tachycardias 11/25/2020 23
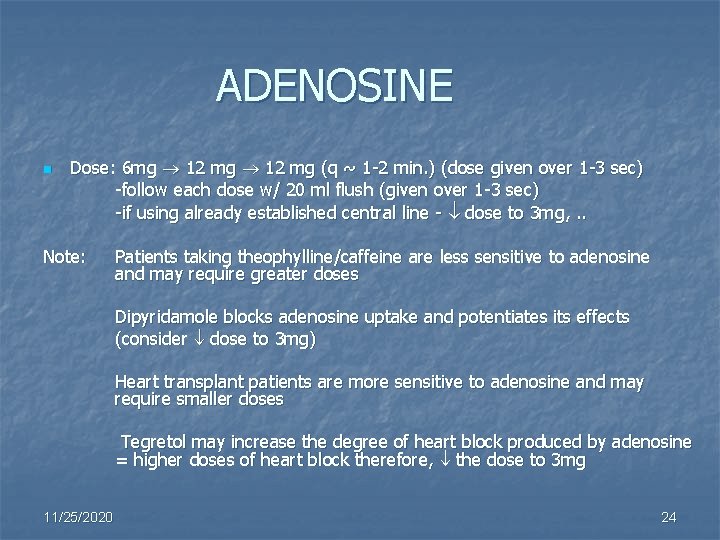
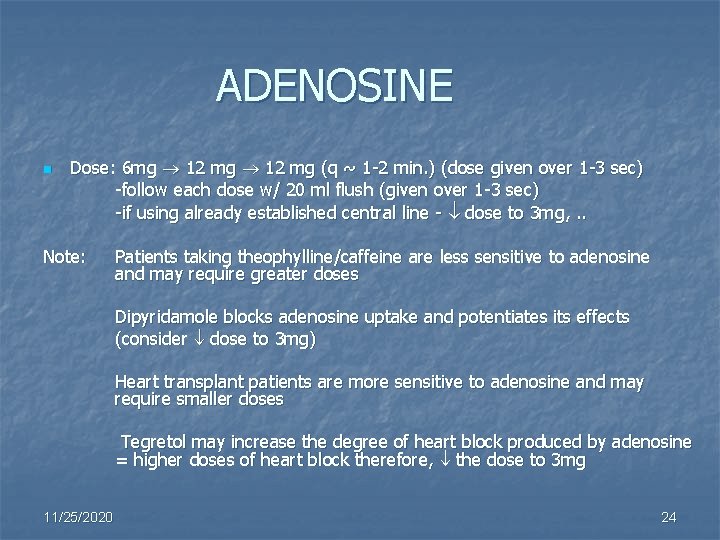
ADENOSINE n Dose: 6 mg 12 mg (q ~ 1 -2 min. ) (dose given over 1 -3 sec) -follow each dose w/ 20 ml flush (given over 1 -3 sec) -if using already established central line - dose to 3 mg, . . Note: Patients taking theophylline/caffeine are less sensitive to adenosine and may require greater doses Dipyridamole blocks adenosine uptake and potentiates its effects (consider dose to 3 mg) Heart transplant patients are more sensitive to adenosine and may require smaller doses Tegretol may increase the degree of heart block produced by adenosine = higher doses of heart block therefore, the dose to 3 mg 11/25/2020 24
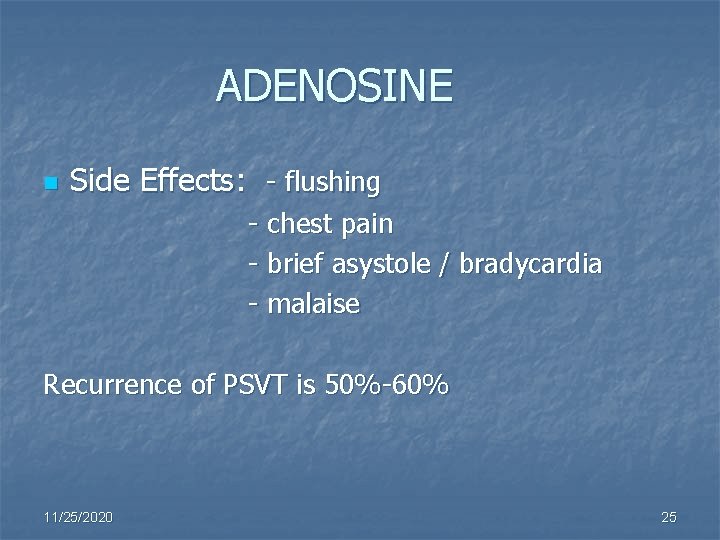
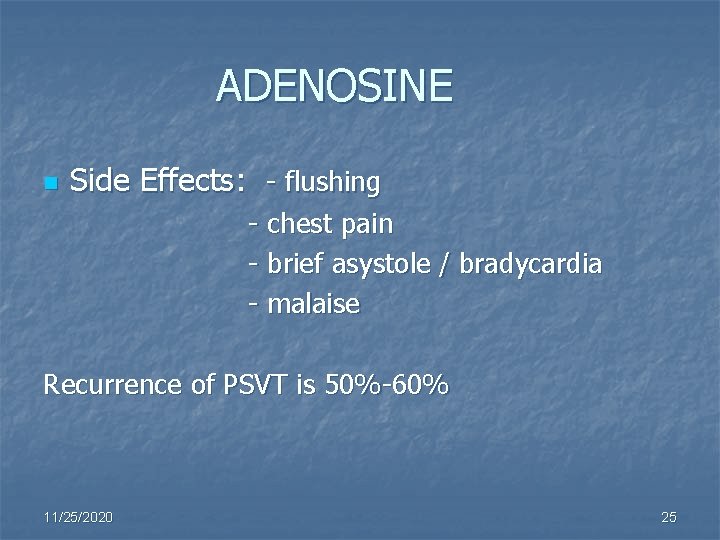
ADENOSINE n Side Effects: - flushing - chest pain - brief asystole / bradycardia - malaise Recurrence of PSVT is 50%-60% 11/25/2020 25
Drug Administration Medications should be delivered DURING CPR ASAP after rhythm checks 11/25/2020 26
Oxygen and Aspirin n Oxygen – 1 - 6 L/min §Aspirin – 160 mg – 325 mg - Aspirin (non-enteric coated) should be administered to ALL patients suspected of acute coronary syndromes, unless contraindicated 11/25/2020 27

Nitroglycerin n Nitroglycerin – MOA: - initial antianginal for suspected ischemic pain - preload at lower doses - afterload at higher doses - dilates large coronary arteries - coronary collateral blood flow to ischemic myocardium - antagonizes vasospasms 11/25/2020 28

Nitroglycerin (cont’d) Dose: SL 0. 4 mg tab q 5 min x 3 IV Bolus 12. 5 -25 mcg if no SL given, then 10 -20 mcg/min titrated to effect (range 50 -200 mcg/min) 11/25/2020 29
Morphine n Morphine - myocardial O 2 requirements - venous capacitance - treatment of pain - SVR - chest pain w/ ACS unresponsive to nitrates Side Effects: respiratory depression BP 11/25/2020 30
Antiplatelet Agents: Glycoprotein IIB/IIIa agents n Blocks glycoprotein IIb/IIIa receptors on platelets n Blocked receptors cannot attach to fibrinogen n Fibrinogen cannot aggregate platelets to platelets n Indications: Acute Coronary Syndrome -STEMI or non. STEMI /UA undergoing PCI -NONSTEMI/Unstable angina managed medically n Examples: abciximab (Reo. Pro), eptifibitide (Integrilin), tirofiban (Aggrastat) 11/25/2020 31
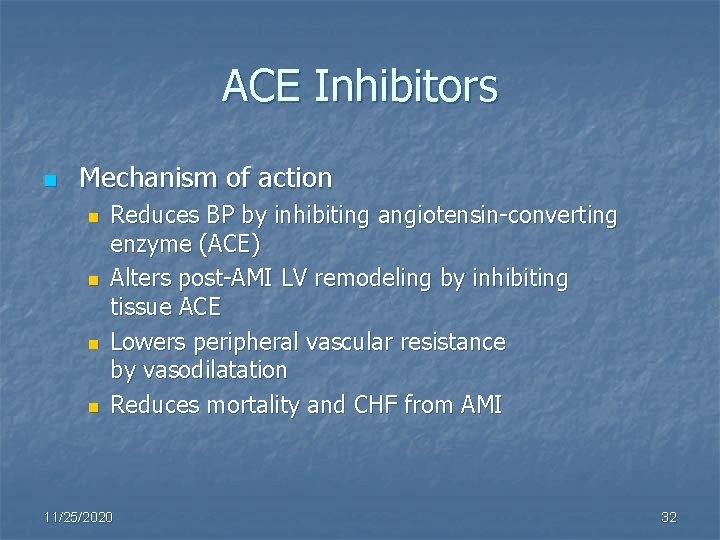
ACE Inhibitors n Mechanism of action n n Reduces BP by inhibiting angiotensin-converting enzyme (ACE) Alters post-AMI LV remodeling by inhibiting tissue ACE Lowers peripheral vascular resistance by vasodilatation Reduces mortality and CHF from AMI 11/25/2020 32
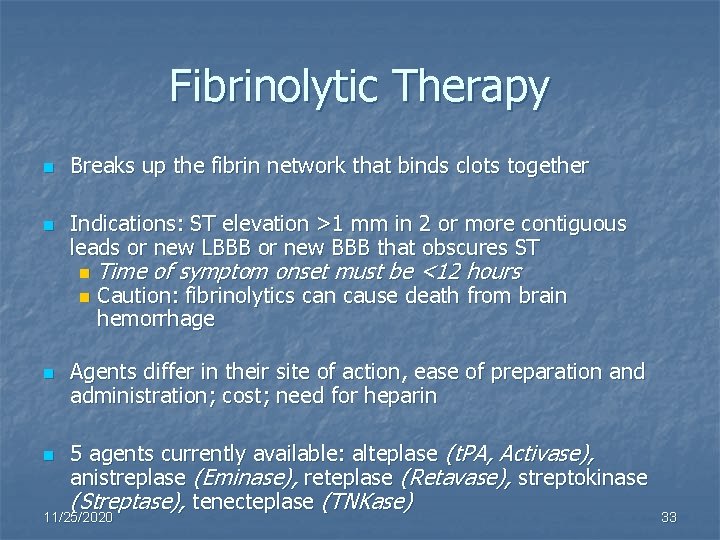
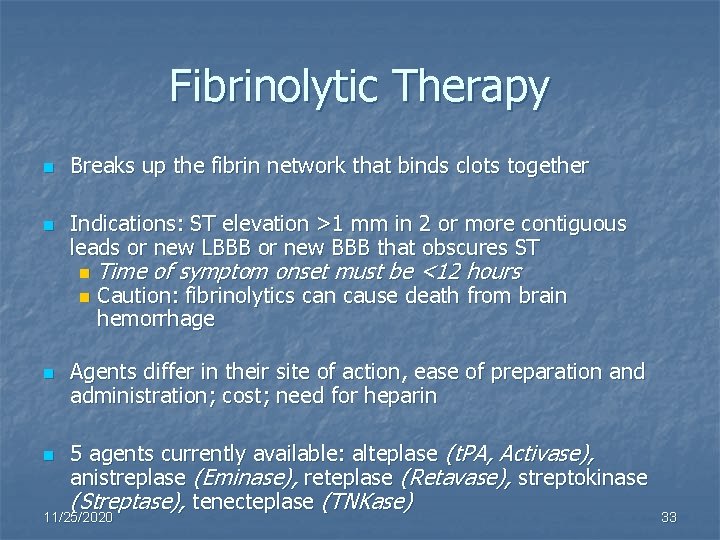
Fibrinolytic Therapy n n Breaks up the fibrin network that binds clots together Indications: ST elevation >1 mm in 2 or more contiguous leads or new LBBB or new BBB that obscures ST n n Time of symptom onset must be <12 hours Caution: fibrinolytics can cause death from brain hemorrhage Agents differ in their site of action, ease of preparation and administration; cost; need for heparin 5 agents currently available: alteplase (t. PA, Activase), anistreplase (Eminase), reteplase (Retavase), streptokinase (Streptase), tenecteplase (TNKase) 11/25/2020 33

Heparin n Mechanism of action n n Indirect thrombin inhibitor (with AT III) Indications n n n PTCA or CABG With fibrin-specific lytics High risk for systemic emboli n 11/25/2020 Conditions with high risk for systemic emboli, such as large anterior MI, atrial fibrillation, or LV thrombus 34
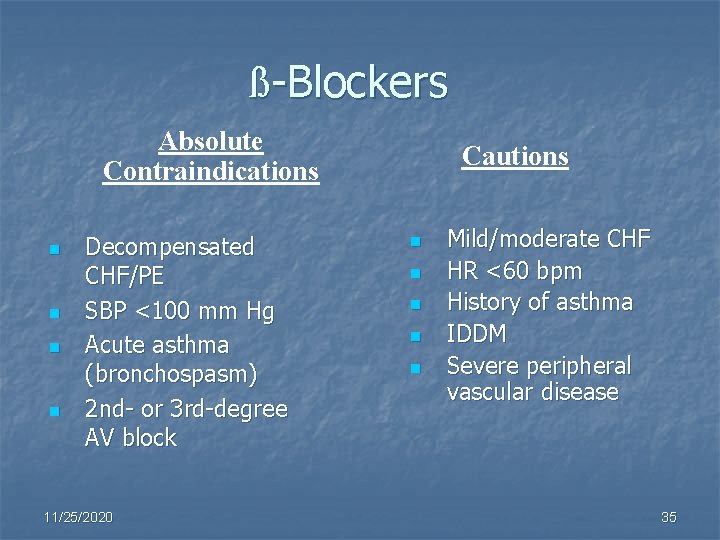
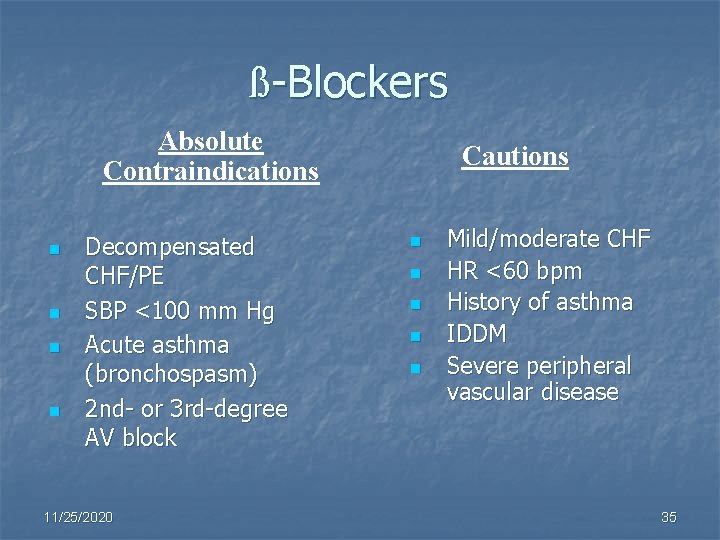
ß-Blockers Absolute Contraindications n n Decompensated CHF/PE SBP <100 mm Hg Acute asthma (bronchospasm) 2 nd- or 3 rd-degree AV block 11/25/2020 Cautions n n n Mild/moderate CHF HR <60 bpm History of asthma IDDM Severe peripheral vascular disease 35
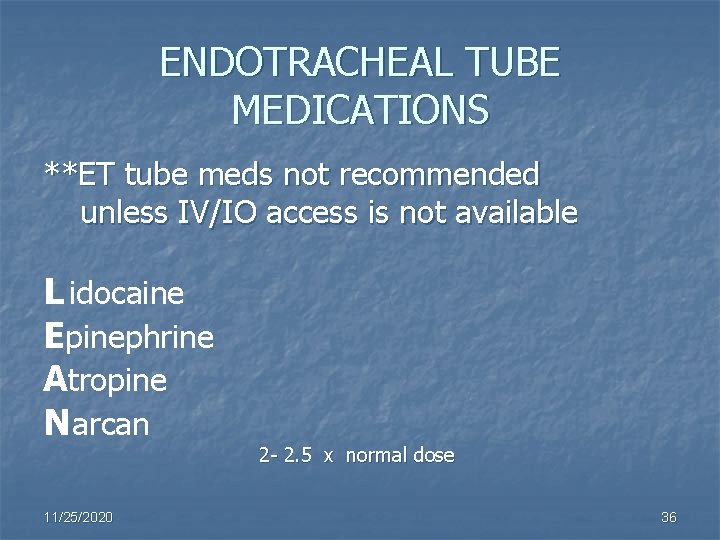
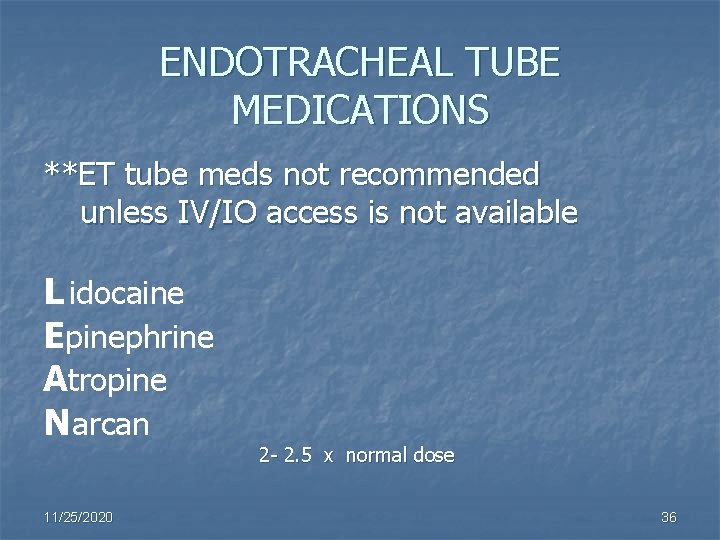
ENDOTRACHEAL TUBE MEDICATIONS **ET tube meds not recommended unless IV/IO access is not available L idocaine Epinephrine Atropine N arcan 11/25/2020 2 - 2. 5 x normal dose 36
CRITICAL POINTS n Know dosages, indications, contraindications, and side effects of drugs n Know concentrations of drugs n Know what drugs look like at your organization 11/25/2020 37
 Desarrollo cognitivo en la edad adulta
Desarrollo cognitivo en la edad adulta Chapter 11 medications and drugs
Chapter 11 medications and drugs Common pediatric medications
Common pediatric medications Tuohy needle sizes
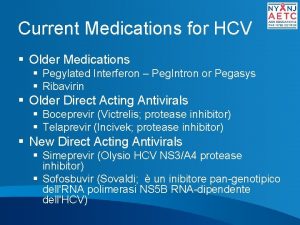
Tuohy needle sizes Hepatitis c medications
Hepatitis c medications List of high-alert medications jci
List of high-alert medications jci Mock code medications
Mock code medications 5 rights of medication
5 rights of medication Which types of drugs are distributed by the envelope method
Which types of drugs are distributed by the envelope method Chapter 30 administering medications
Chapter 30 administering medications Medications
Medications Debbie norrie
Debbie norrie Reconciliation medical definition
Reconciliation medical definition High risk medications
High risk medications Chapter 30 administering medications
Chapter 30 administering medications Peripheral nervous system medications
Peripheral nervous system medications What is the transport system of the body
What is the transport system of the body Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Outfield pharm
Outfield pharm Pharm d means
Pharm d means Pharm 406
Pharm 406 Bc bio-pharm
Bc bio-pharm Pharmlink
Pharmlink Pharm gkb
Pharm gkb Secur pharm
Secur pharm Purdue retail pharmacy
Purdue retail pharmacy Forensic pharmacist
Forensic pharmacist Pharm
Pharm Klucel exf
Klucel exf Friciton
Friciton Pharm id
Pharm id Ambio pharm
Ambio pharm H's and t's acls
H's and t's acls 4h 4t
4h 4t Jjg visual vocabulary
Jjg visual vocabulary Garrett model of speech production
Garrett model of speech production Speech errors examples
Speech errors examples Garrett's model of speech production
Garrett's model of speech production