Acinetobacter n n n n Oxidase negative Nitrate
Acinetobacter
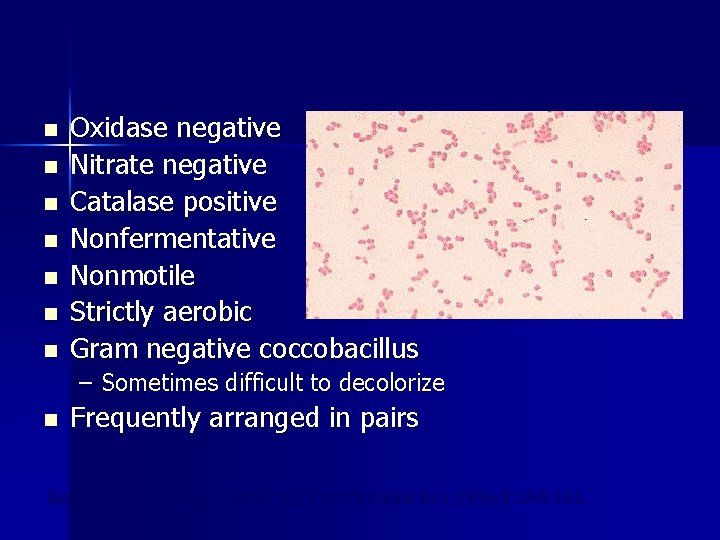
n n n n Oxidase negative Nitrate negative Catalase positive Nonfermentative Nonmotile Strictly aerobic Gram negative coccobacillus – Sometimes difficult to decolorize n Frequently arranged in pairs Bergogne-Bérézin E, Towner KJ. Clin Microbiol Rev 1996; 9: 148 -165.
Acinetobacter background Non-motile gram negative coccobacillus n Often mistaken for staph on bad gram stain n A colonizer of skin & mucosa in the tropics, but not temperate climates n Increased cases in summer perhaps biofilm bloom in tapwater n
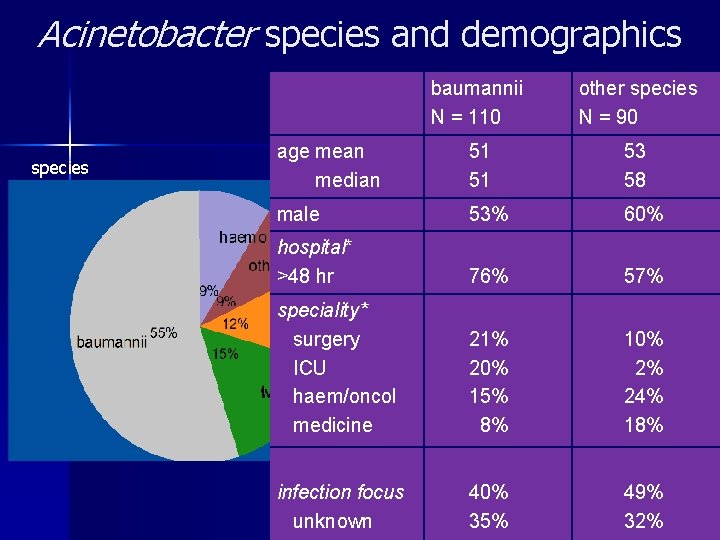
Acinetobacter species and demographics species baumannii N = 110 other species N = 90 age mean median 51 51 53 58 male 53% 60% hospital* >48 hr 76% 57% speciality* surgery ICU haem/oncol medicine 21% 20% 15% 8% 10% 2% 24% 18% infection focus unknown 40% 35% 49% 32%
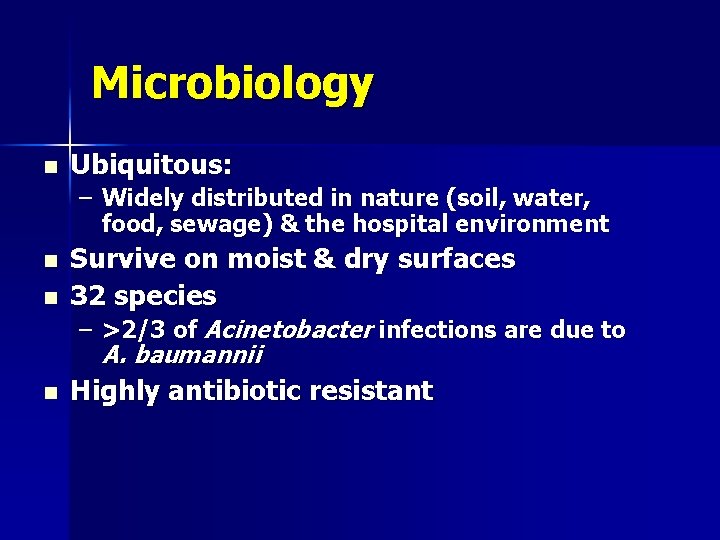
Microbiology n Ubiquitous: – Widely distributed in nature (soil, water, food, sewage) & the hospital environment n n Survive on moist & dry surfaces 32 species – >2/3 of Acinetobacter infections are due to A. baumannii n Highly antibiotic resistant
Major infections due to Acinetobacter Ventilator-associated pneumonia n Urinary tract n Bloodstream infection n Skin/wound infections n Endocarditis n Peritonitis n
Acinetobacter Ventilator. Associated Pneumonia n Acinetobacter accounts for 5 -25% of all cases of VAP n Risk factors: – Advanced age – Surgery – Use of antimicrobial agents – Invasive devices – Prolonged ICU stay
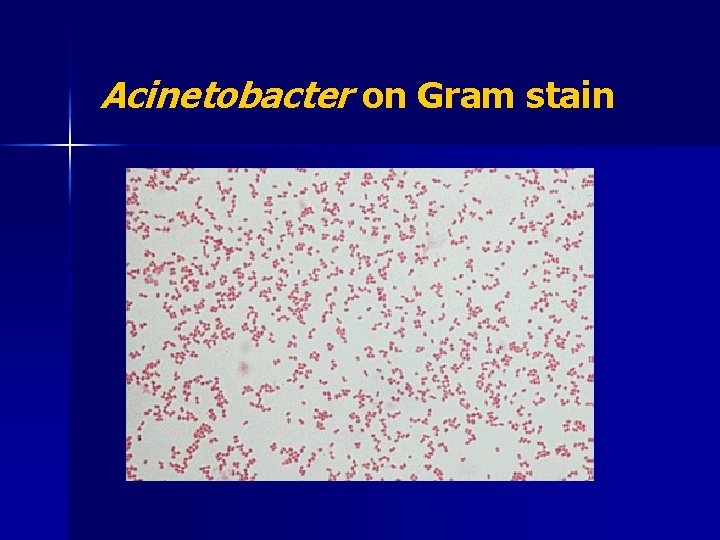
Acinetobacter on Gram stain
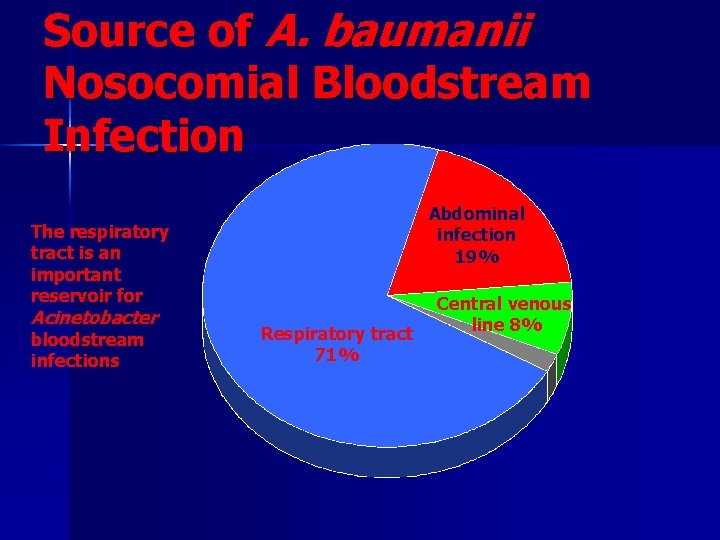
Source of A. baumanii Nosocomial Bloodstream Infection Abdominal infection 19% The respiratory tract is an important reservoir for Acinetobacter bloodstream infections Respiratory tract 71% Central venous line 8%
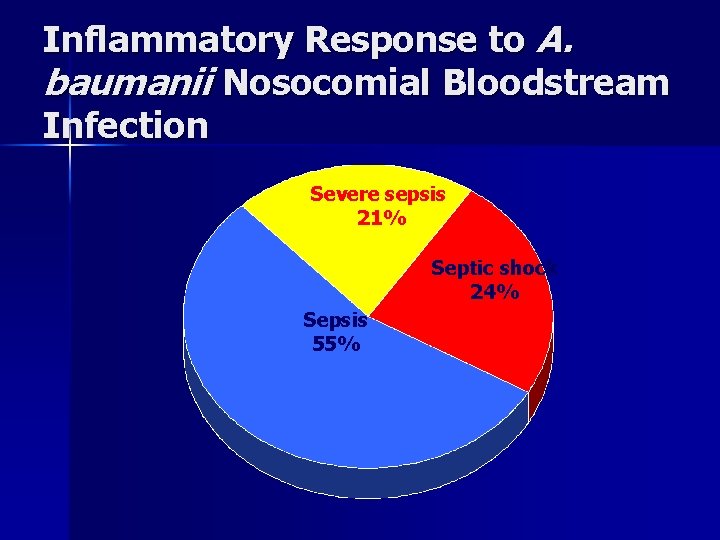
Inflammatory Response to A. baumanii Nosocomial Bloodstream Infection Severe sepsis 21% Septic shock 24% Sepsis 55%
Opportunities for cross transmission are multiple
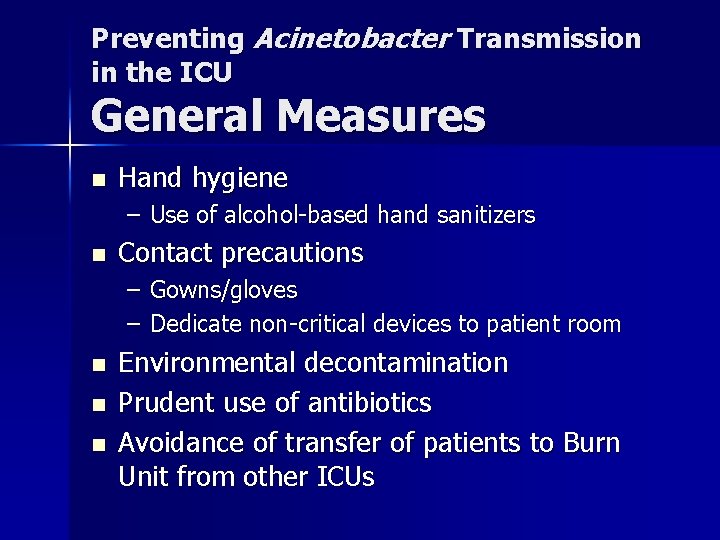
Preventing Acinetobacter Transmission in the ICU General Measures n Hand hygiene – Use of alcohol-based hand sanitizers n Contact precautions – Gowns/gloves – Dedicate non-critical devices to patient room n n n Environmental decontamination Prudent use of antibiotics Avoidance of transfer of patients to Burn Unit from other ICUs
Preventing Acinetobacter Transmission in the ICU Outbreak Interventions n n n n Hand cultures Surveillance cultures Environmental cultures following terminal disinfection to document cleaning efficacy Cohorting Ask laboratory to save all isolates for molecular typing Healthcare worker education If transmission continues despite above interventions, closure of unit to new admissions
Summary n n n Although commonly found on the skin of healthy humans, Acinetobacter plays the role of an opportunistic pathogen in the critically ill patient High level of antibiotic resistance makes it well suited as a pathogen in areas with high use of antibiotics (e. g. , ICU setting) Control requires good hand hygiene, barrier precautions & environmental decontamination – Alcohol-based products containing chlorhexidine should be considered the hand hygiene agents of choice

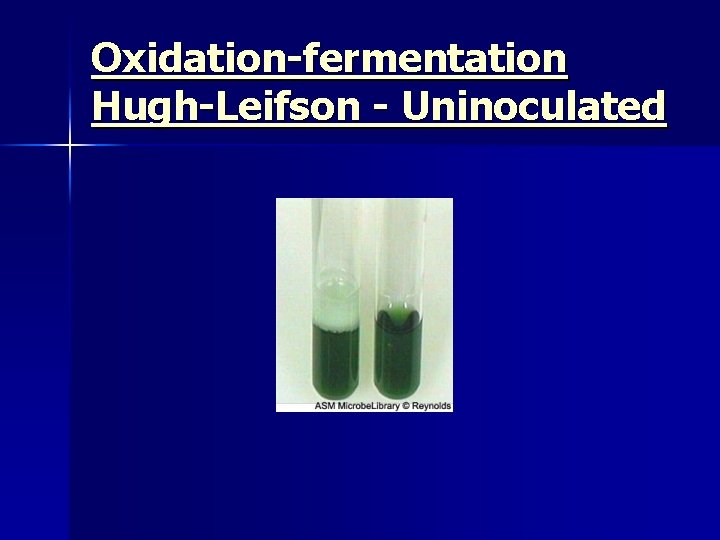
Oxidation-fermentation Hugh-Leifson - Uninoculated
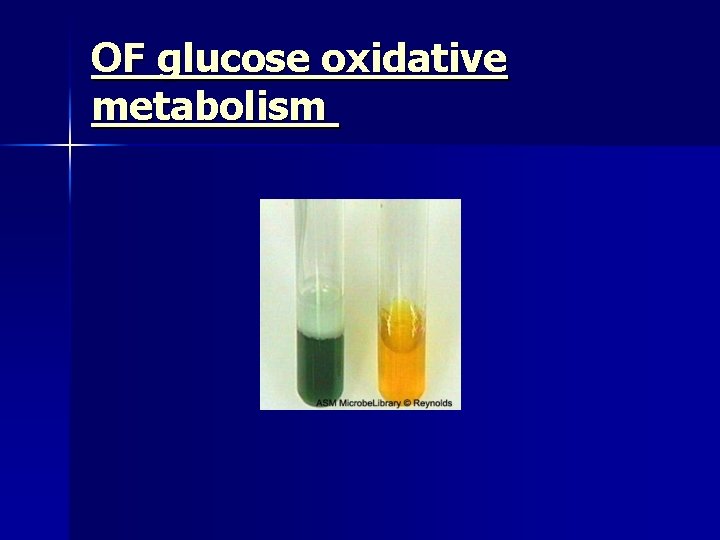
OF glucose oxidative metabolism
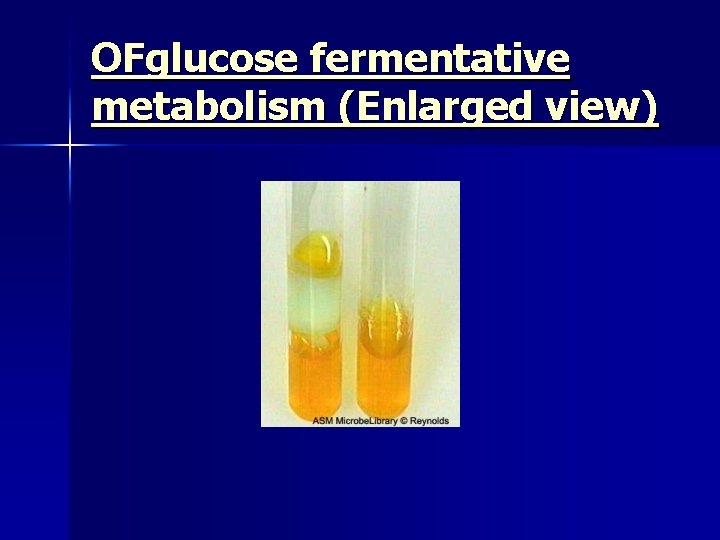
OFglucose fermentative metabolism (Enlarged view)
Identification characteristics of Acinetobacter baumanni (Unknown)
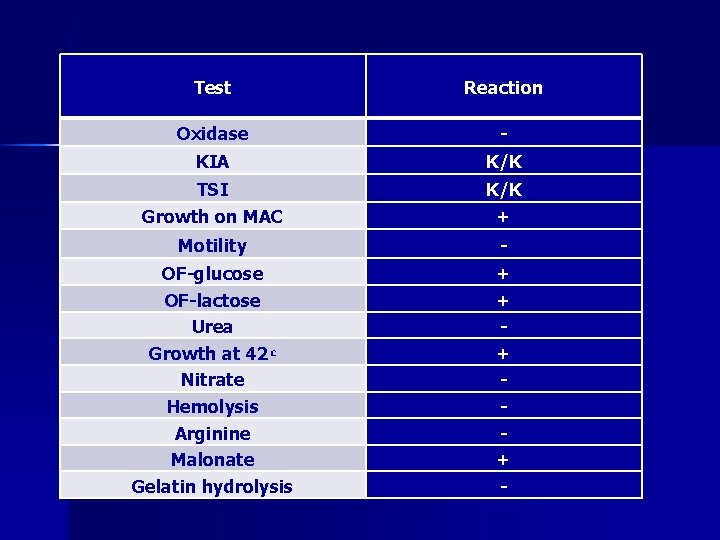
Test Reaction Oxidase - KIA K/K TSI K/K Growth on MAC + Motility - OF-glucose OF-lactose Urea Growth at 42 C Nitrate Hemolysis Arginine Malonate Gelatin hydrolysis + + -
- Slides: 20