Accreditation Council for Graduate Medical Education The Next

- Slides: 13
Accreditation Council for Graduate Medical Education The “Next Accreditation System” and the Context of the Health Care System Society of Neurological Surgeons Meeting May 20, 2012, Atlanta, GA Ingrid Philibert, Ph. D, MBA, Senior Vice President, Department of Field Activities
The “Big Picture”: GME and the rising expectations for public accountability • IL 372, PATH Audits, Quality of Care – Determine whether payment differential for Teaching Hospitals is justified • House of Representatives codifies “New Physician Competencies” (Section 1505) • Positioning health care for accountable care organization model under Section 3022 of the Affordable Care Act (ACA) • Med. PAC recommendations to make a portion of GME funding “contingent” on programs’ attainment of quality/accountability goals • Public/media interest in resident hours, perception of long hours as factor in reduced patient safety • Backdrop of an ongoing debate over the size and function of government, the role and effectiveness of accreditation and regulation
What is common or underlying these calls? • They recognize the ACGME as: • Either as the agent of change/improvement, • Or as the blocker of change/improvement • They expect more from the ACGME than accreditors have traditionally provided • They call for rapid change and improvement • The ACGME to drive change, do it in the context of promoting innovation • The expect ACGME to be accountable for the outcomes of “medical education” (not just GME)

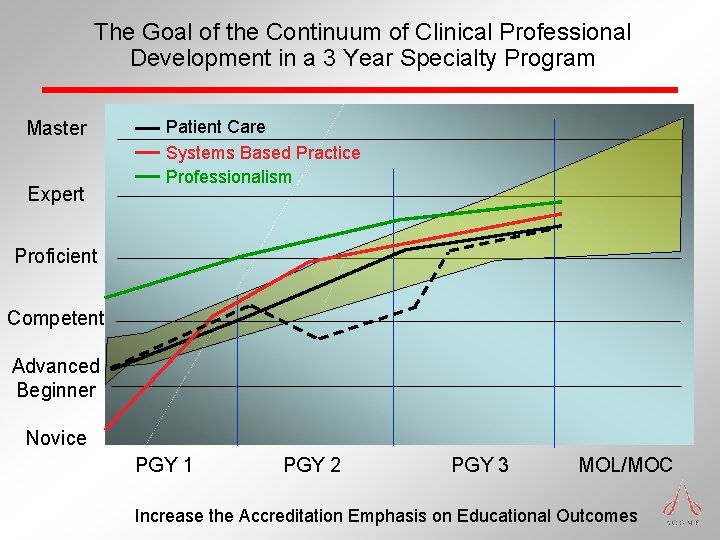
The Six Competencies, and the Continuum of Clinical Medical Education – Dreyfus (modified) Conceptual Model 1 • Medical Knowledge • Novice • Patient Care and Procedural Skills 2 • Advanced Beginner • Interpersonal and Communication Skills • Proficient • Professionalism • Master • Practice Based Learning and Improvement • Systems Based Practice • Competent • Expert • Undergraduate • Graduate • Continuing as presented by Leach, D. , modified by Nasca, T. J. American Board of Internal Medicine Summer Retreat, August, 1999. 2 Patient Care Competency modified 9/2010 by ACGME and ABMS 1
Brief History of the Competencies and Milestones 1997 -2005 • Late 1990’s – ACGME/ABMS Competencies developed • ACGME requires: • Competency framework for curriculum • Phased incorporation of competency evaluation • Culminates in “competency based accreditation” • The “field” left to develop “tools” for the “toolbox” • ABMS organizes individual certification in Competency framework • Initial Certification • Maintenance of Certification • Tools developed that may be relevant in GME phase
Brief History of Competencies/Milestones 2005 -Present November 2005, the ACGME Executive Committee endorsed four strategic priorities designed to enable emergence of the new accreditation model: Competency evaluation development stalls – • The field struggled with the high level competencies • ACGME begins Milestones and “Next Accreditation System” development in 2008 • Questions re: the quality of preparation of graduates (in key dimensions) for the “future” health care delivery system
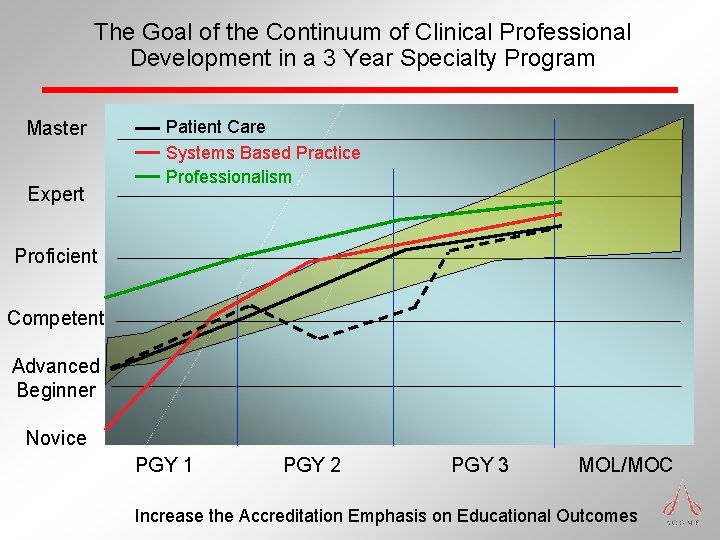
The Goal of the Continuum of Clinical Professional Development in a 3 Year Specialty Program Master Expert Patient Care Systems Based Practice Professionalism Proficient Competent Advanced Beginner Novice PGY 1 PGY 2 PGY 3 MOL/MOC Increase the Accreditation Emphasis on Educational Outcomes
The Milestones • Observable developmental steps moving from Novice to Expert/Master • Organized under the rubric of the six domains of clinical competency • Describe a trajectory of progress from neophyte towards independent practice • Articulate shared understanding of expectations • Subset of all dimensions of clinical competency • Required of all residents in that discipline • Set goals of excellence • Provide a framework and language for discussions across the continuum
ACGME Goal for Milestones – Move toward “Outcomes Based Accreditation” • Specialty-specific national normative data on resident progress • Begins with existing tools and observations of the faculty • Clinical Competency Committee triangulates progress of each resident • ABMS Board tracks the individual’s development • ACGME Review Committee tracks unidentified individuals’ trajectories • Allows • Less prescriptive program requirements, lengthened site visit cycles, less frequent standards revision • Free good programs to innovate; Assist poor programs in improving • Provide public accountability for outcomes (with ABMS) • Opportunity for communication and improvement across the continuum of medical education
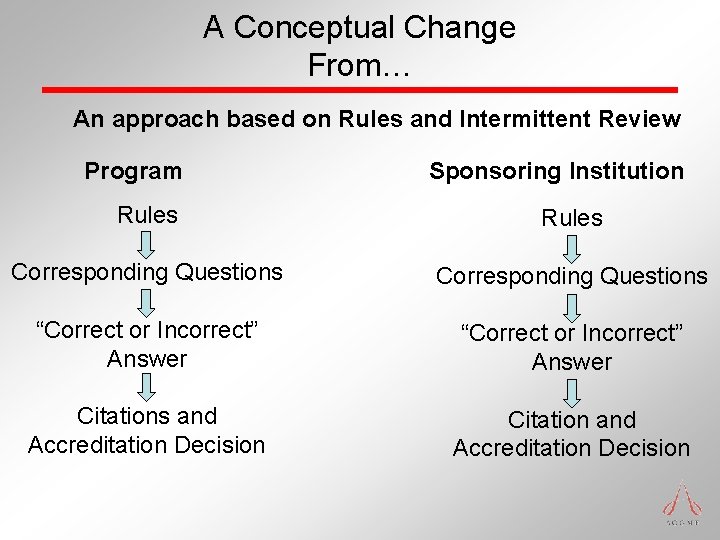
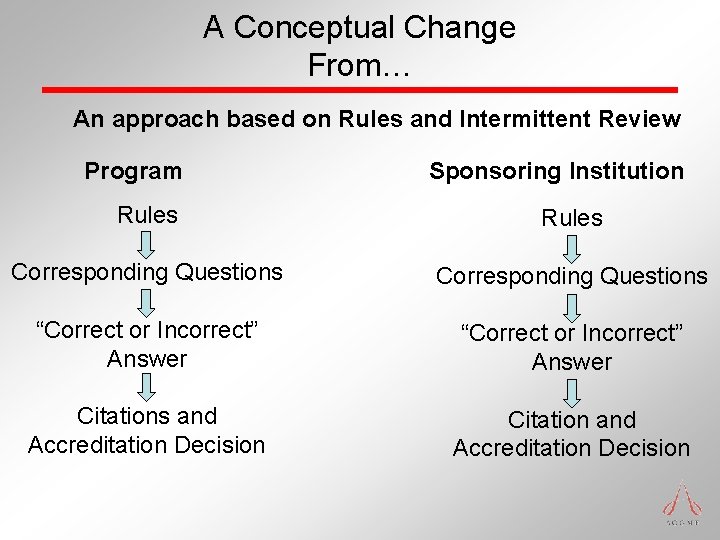
A Conceptual Change From… An approach based on Rules and Intermittent Review Program Sponsoring Institution Rules Corresponding Questions “Correct or Incorrect” Answer Citations and Accreditation Decision Citation and Accreditation Decision
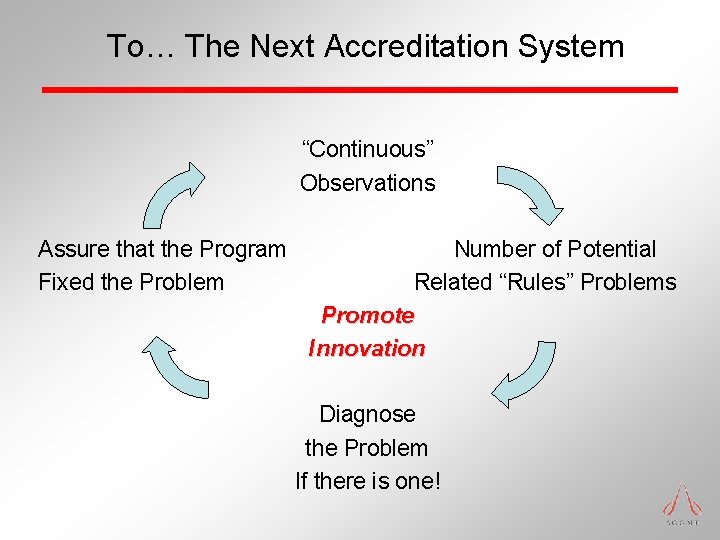
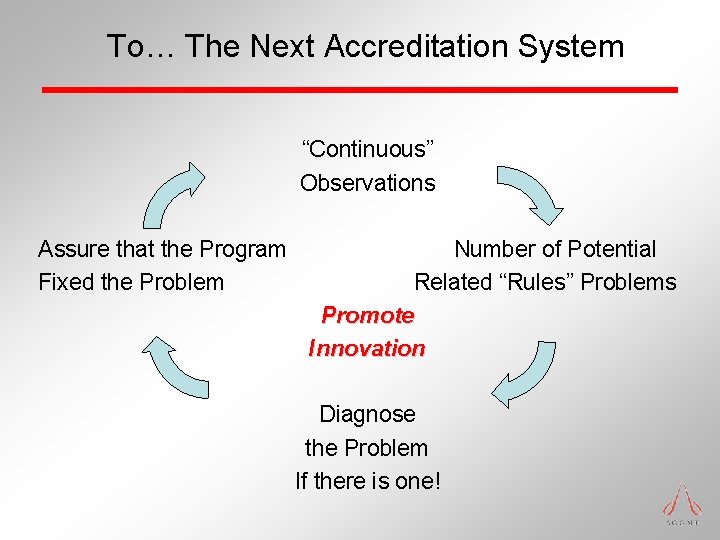
To… The Next Accreditation System “Continuous” Observations Assure that the Program Fixed the Problem Number of Potential Related “Rules” Problems Promote Innovation Diagnose the Problem If there is one!
Potential Reasons for the Public Interest in GME • Practicing physicians are not made in medical school • Residents care for real patients during learning process • Knowledge/Skills/Attitudes learned in residency influence the future care rendered by these physicians • > $9 billion per year paid to US Teaching Hospitals • GME Required for: • Licensure • Board Certification • Institutional payment for GME • US reputation for quality, technology, innovation • GME as the focal point for change leading to positive action
Questions and Answers