According to Ogden 2004 health psychology represents one











- Slides: 48
According to Ogden (2004), health psychology represents one of several challenges that were made during the twentieth to the biomedical model. This maintains that: Ø disease either come from outside the body and invade it, causing internal physical changes, or originate as internal involuntary physical changes; such diseases imbalances, can bacteria, be caused viruses by chemical or genetic

Ø Individuals aren’t responsible for their illnesses, which arise from biological changes beyond their control; people who are ill are victims. Ø treatment should consist of vaccination, surgery, chemotherapy or radiotherapy, all of which aim to change the physical state of the body. Ø responsibility for treatment rests with the medical profession.
Ø health and illness are qualitatively different-you are either healthy or ill, and there’s no continuum between the two. Ø mind and body function independently of each other; the abstract mind relates to feelings and thoughts, and is incapable of influencing physical matter. Ø illness may have psychological consequences, but not psychological causes.
In opposition to these ideas, health psychology maintains that human beings should be seen as complex systems. Illness is often caused by a combination of biological (e. g. viruses, psychological (e. g. behaviors and beliefs) and social (e. g. employment) factors. The biomedical model, by ignoring the role of psychological and sociocultural factors, is unable to explain: vhow pre-operative psychological preparation (including anxiety reduction) can affect wound healing and recovery rate.
v the relationship between patients’ perception of symptoms and symptom control. vwhy patients sometimes don’t comply with treatment. vhow the attitudes towards their illness can affect its course and prognosis in patients with chronic illnesses (such as HIV/AIDS, cancer, obesity and coronary heart disease) and
v the enormous diversity in patients’ experience/ tolerance of pain. In all these cases, the relationship between the patient and the nurse (or doctor, physiotherapist, etc. ) also plays a crucial role.
What is Health Psychology? Maes and Van Elderen (1998) define health psychology as: ‘… a sub-discipline of psychology which addresses the relationship between psychological processes and behavior on the one hand health and illness on the other hand… however…. health psychologists are more interested in ‘normal’ every-life behaviour and ‘normal’ psychological processes in relation to health and illness than bahaviour… in psycho-pathology or abnormal
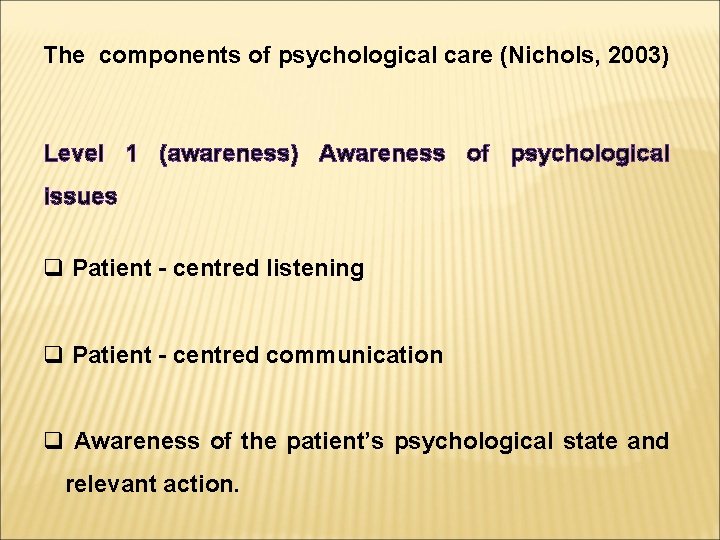
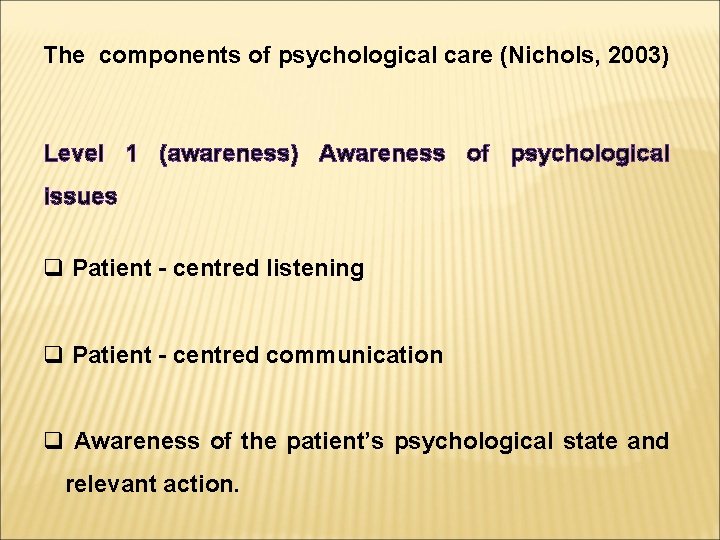
The components of psychological care (Nichols, 2003) Level 1 (awareness) Awareness of psychological issues q Patient - centred listening q Patient - centred communication q Awareness of the patient’s psychological state and relevant action.
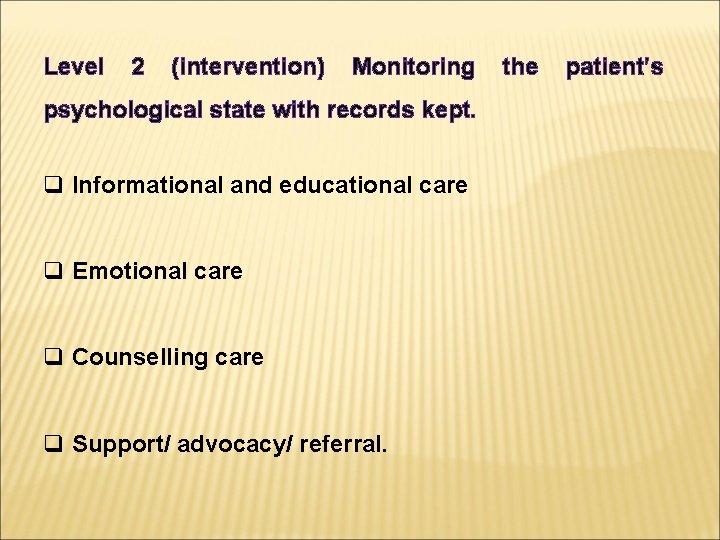
Level 2 (intervention) Monitoring psychological state with records kept. q Informational and educational care q Emotional care q Counselling care q Support/ advocacy/ referral. the patient’s
Level 3 (therapy) Psychological therapy. Gross R. (2007) Psychology for Nurses and allied health professionals, Hodder Arnold, London.
Egan (1977) cited in by Gross 2007 suggests that the provision of understanding, support and encouragement enables another person to feel secure enough to disclose important emotional concerns. This would involve an individual being listened to, being allowed to speak without interruption, and receiving feedback that shows they have been understood. way’ (Minardi and Riley, 1988 cited in Gross 2007).

It requires recognition of the person’s beliefs, values, needs and wishes without judging that person: ‘It would appear, therefore, that the provision of psychological safety centers around the ability to communicate to an individual that their beliefs, values, needs and wishes are recognized and understood in an open and non-judgmental.
Psychological safety can be enhanced by what Bernard (1987) calls ‘ therapeutic conversation’. Five components of therapeutic conversation (based on Burnard, 1987). v Emphasis on the here-and-now: Many people find the present painful to live in, while the past, however in accurate our recollection, feels more comfortable.
But it’s more therapeutic if the nurse stays with the patient’s moment-to-moment phenomenology and notes his/her changing verbal and non-verbal cues as they occur. This requires concentration, close awareness of subtle changes and the ability to ‘ stay awake’ and remain focused on the patient.
v. Focus on feelings: The nurse uses reflection and empathy-building to convey that s/he understands what the patient is feeling. This helps the patient to confront the feelings as they occur, rather than having a theoretical debate about why the patient is feeling this way. This focus on feelings requires training in basic counseling techniques.
v Empathic understanding: This involves attempting to enter the other person’s frame of reference or way of looking at the worldthat is, to see things from their perspective, rather than our own. By understanding the patient’s belief and value system, we can better appreciate why they are experiencing this set of feelings at this time. This too requires training.
v A non-prescriptive approach: To be prescriptive is to make suggestions or offer opinions about what the patient should do. It’s usually more appropriate in a health care setting to help the patient to make his/her own decisions and draw his/her own conclusions.

v The patient should remain the central focus: While in ordinary social conversation there’s a toand-fro between the two speakers, in therapeutic conversation the patient is ‘telling the story’ while the nurse is essentially listening. This is another skill that can be developedthrough experiencing what it’s like to be heard.
The participants were interviewed about their understanding of the phenomenon of care and caring. Transcriptions from the taped interviews were read to develop a ‘feeling’ for them and to make sense of them. Statements were then categorised according to their perceived meanings and arranged into five main themes, as follows: 1. Encouraging autonomy. This relates to patient empowerment, wanting to allay patients’ fears and anxieties by giving greater control over their care.

2. Giving of oneself: ‘Caring, it can be argued, is the essence of giving of oneself’ (Bassett, 2002). Nurses give to patients in terms of time, energy and effort. They spend time learning skills and gaining knowledge, both as students and throughout their nursing careers. But to simply provide mechanical care may not be enough in their eyes-providing care without genuineness isn’t adequate.
3. Taking risks: This theme comprises the subcategories ‘taking risks’, getting a buzz’ and ‘challenge’. Taking risks in nursing isn’t about putting patients at risk, but refers to testing the boundaries of accepted care, moving from the defined boundaries, and developing new and innovative ways of caring for patients. Sometimes it may be necessary to disobey a doctor’s orders if this is in the patient’s best interests or to take a stand against colleagues’ interpretations of normal nursing procedures or protocols.

For students this means ‘standing up’ for patients when they feel the care was less than the patient deserved. 4. Supporting care: Certain supporting factors are essential to ensure that care can be delivered effectively. These are managerial, organisational and psychological support systems.
5. Emotional labour: This theme was unique to the student participants and seemed to reflect the fact that learning to nurse can constitute an emotional assault. It describes the often difficult things that nurses are expected to do in their daily work, causing them to experience sadness and emotional trauma. If unresolved or buried, these responses may lead nurses to leave nursing or not develop the caring attributes necessary for quality nursing care.

For many people, patients and relatives alike, hospitals and other health care settings can be unpleasant, frightening, even bewildering places. Those environments within a hospital that are designed to help those with the most life-threatening conditions are also likely to evoke the most extreme negative reactions – in both patients and staff. These ‘extreme’ environments include coronary care units (CCUs), cancer wards/ units, intensive care units (ICUs) and Accident and Emergency (A & E) departments.

PRE-SURGICAL ANXIETY Hospital admission is a stressor that produces severe anxiety in some form or another in 10 -80 per cent of patients. Although medication is often used to manage pre-operative anxiety, many nurses believe that reassurance and listening to patients’ concerns are more beneficial. However, research suggests that nurses generally play a minor part in patients’ psychological care, and the nurse-patient relationship on most surgical wards is task-related, short and to the point, with therapeutic discussion almost non-existent (Toogood, 1999)
Severe anxiety can affect a patient’s ability to assimilate and retain information, while moderate anxiety can produce increased adrenaline and cortisol levels, inhibiting wound healing (Pediani, 1992; Toogood, 1999). It can also cause electrolyte imbalance and harm the body’s immune response, leading to increased risk of wound infections.

It’s widely acknowledged that understanding helps reduce anxiety. If a situation cannot be interpreted, it cannot be dealt with and the individual experiences helplessness and anxiety (Lazarus and Averill, 1978). However, just giving information, though beneficial, isn’t enough. Even assuming the patient is able to understand the information sent before admission, it can actually increase stress (Salmon, 1993, in Toogood, 1999).

What’s needed is a careful assessment of a patient’s needs and appropriate care. Nurses must bear in mind that patient’s levels of intelligence and understanding vary, and that one answer may not suit the needs of any two patients (Toogood, 1999). Boore (1978, in Pediani, 1992) compared a group of ‘informed’ patients with an ‘uninformed’ group, both groups receiving the same amount of ‘nurse time’ prior to surgery.
The former had lower levels of steroids in their urine, suggesting that information allows patients to interpret and understand their surroundings and helps them to anticipate the events usually occurring in the postoperative period. This minimises feelings of helplessness and so lowers anxiety. Other studies have found that good psychological preparation can lead to earlier discharge from hospital, less need for analgesia, lower incidence of urinary retention and lower pulse rate and blood pressure (Pediani, 1992).
What these studies suggest is that ‘good wound care is not just a matter of physical administration of dressings; it involves the need to prepare the patient psychologically’ (Pediani, 1992). Panda et al. (1996, in Toogood, 1999) suggest that patients value information from doctors most. But, in reality, nurses offer an emotional support service and are often required to fill in the gaps left by doctors, interpreting medical information that patients don’t understand, so providing them with clear, detailed and logical explanations.

Is interpreting medical information an aspect of advocacy? Although Maisie would have been given a pre-operative examination, she no doubt needed reassurance about her operation and her stay in hospital.
INTENSIVE CARE UNIT (ICUs) According to Calne (1994), some adult patients in ICU undergo a process of dehumanisation. Dehumanisation and self-identity v The term is sometimes used to refer to situations where an individual loses his/ her human identity and becomes (or is perceived as) machine-or animal-like.
v It can include the restriction or denial of attributes that contribute to an individual’s self-identity and personality, leading to a loss of ‘humanness’. v According to Goffman (1971), there are two fundamental ways of expression self-identity: (a) ‘narrow’ communication (direct communication through talking or body language); and (b) ‘broad’ communication – a wide range of actions and activities, including how an individual gives an impression of self-identity through physical appearance or dress, which may signal social status or
Typically, dehumanised patients have developed multiple organ failure and have been in ICU for a long time. They are always intubated and unable to communicate verbally, are mostly unresponsive and require complex technical monitoring. According to Calne (1994), the key factors that affect critically ill patients’ freedom of self-expression are: v reduced ability to communicate v the distracting nature of the technical equipment v altered physical appearance v lack of personal belongings.
Critically ill patients often experience restricted selfidentity because they’re unable to communicate verbally or non-verbally. They are dependent on the nurse’s ability to interpret the fragmentary clues (such as change in the sound of the ventilator or in displayed patterns on their chart), which reveal their real fears and desires (Ashworth, 1990, in Calne, 1994). Similarly, a sudden rise in heart rate, or a previously settled patient becoming agitated, would lead most nurses to infer that the patient is in pain, uncomfortable or frightened.

At the same time, technical equipment can be a source of distraction, diverting attention away from the patient (Ashworth, 1990, in Calne, 1994). Changes in a critically ill patient’s physical appearance can occur as a result of drug therapies, surgical interventions and altered physiology. These changes may include surgical wounds, extensive oedema, jaundice, anaemia, exaggerated skin loss, bruising from clotting disorders, and loss of body mass. Their physical appearance may be so radically altered that even relatives don’t immediately recognise the patient.
Calne (1994) cites several studies showing that ICU nurses may actually distance themselves, both psychologically and physically, from critically ill patients. They may protect themselves from emotional involvement with patients who are ‘unlikely to survive’. Patient’s physical appearance can be a source of stress for ICU staff and non-task-related/ non-invasive interaction is often limited.
This is a situation where the patient would depend heavily on the nurse to be an advocate. It’s also an example of difficult emotional labour, where health professionals must sort out their own feelings in order to help patients and relatives.
According to Glide (1994), patients in ICUs experience both sensory overload and sensory deprivation. Noise levels are excessive and there’s evidence that long-term exposure to high noise levels leads to increased tension and anxiety. The most significant form of sensory deprivation patients experience appears to be lack of human touch. Although ICU patients are often exposed to physical touch, this is mostly associated with technical intervention (task-related/ invasive interaction) rather than personal, comforting physical contact.
Clearly, relatives can help to provide touch but nurses can also help to reduce the sensory deprivation by allowing patients to wear glasses, hearing aids or dentures if at all possible. These also sustain the patients’ dignity, and ability to communicate. Significantly, it was when Sally took Maisie’s hand that she allowed her feelings to show. Her husbands death had changed her social circumstances too; no doubt she missed his caring presence.
Rather than being seen as a passive response to biomedical factors, chronic illnesses (such as HIV/ AIDS, cancer, coronary heart disease/ CHD and obesity) are better undertood in terms of a complex interaction between physiological and psychological processes (Ogden, 2004). Health psychology has studied HIV, for example, in terms of attitudes towards HIV, changing these attitudes and examining predictors of behaviour.
According to Hedge (1995): … the uncertainty attached to the course of disease (HIV) and its poor prognosis frequently cause intense emotional reactions, even in those who are clinically well and asymptomatic. Good care addresses an individual’s quality of life as well as its length: it aims to help people live with HIV infection rather than simply wait to die from it …
As the number of people infected with HIV continues to rise, it’s essential for all health carers to have some knowledge of the psychological implications of the disease. and social
Although people with HIV infection and AIDS develop mental health threatening problems illnesses, common they to may other life- experience psychological disorders that are specifically related to: Ø uncertainty surrounding disease progression and outcomes, the distressing nature of the symptoms themselves, and the knowledge that HIV is potentially fatal; related disorders include acute stress reactions, adjustment disorders, functional psychoses (such as depression and schizophreniform disorders.
Ø the direct effects of the virus (Firn and Norman, 1995); these include a dementia-type illness characterised by progressive cognitive and/ or motor impairment, which may be accompanied by behavioural disturbances. Some of these reactions are related to the stigma associated with the disease, and anti-gay (and anti-drug user) prejudice and discrimination. This means that many people following a positive test result have to deal not only with the medical implications of the diagnosis but also with the potentially negative reactions of partners, friends, family and other social contacts.
This is likely to exacerbate any existing mental health problems. Also, the continued spread of HIV and improved treatment prophylaxis, which ensures that people with HIV live longer, mean that the incidence of HIV-related mental health problems is likely to increase (Firn and Norman, 1995). People with it are often perceived as having engaged in activities that may be proscribed by society and, by implication, as belonging to a stigmatised group (such as gay men and drug users).
These beliefs are often expressed in the language of blame – and even nurses who’ve chosen to work in specialist wards caring for AIDS patients can have difficulties in viewing them completely non- judgementally. Stigma adds a social dimension to this disease and highlights all aspects of the biopsychosocial approach to health and illness. However, even a seemingly simple wound dressing like Maisie’s turned out to be a lesson in looking for all three components of the model.