Access Basics Femoral Artery and Vein Andr C
Access Basics Femoral Artery and Vein André C. Lapeyre, III, M. D. Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Preferred appoach Poor radial pulses Contralateral or bilateral IMA grafts Markedly dilated or distorted ascending aorta Need to preserve radial for free graft Need to preserve radial for arterial monitoring line especially for immediately upcoming surgery Contraindication to heparin and/or anticoagulation Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Contraindications – relative Massively obese patients Patients with difficulty lying flat Patients unable to remain still post procedure Unobtainable femoral access Anticoagulated (except IV heparin) Peripheral arterial disease especially prior femoral grafts or know occlusion iliacs and/or femoral Ipsilateral kidney transplant Symptomatic descending aortic disease Andre Lapeyre, MD © Mayo Clinic
Access Basics Anatomy Know the anatomy Entire Aorta Specific attention to: Arch variants Abdominal Aorta Ileofemoral arteries and branches Andre Lapeyre, MD © Mayo Clinic
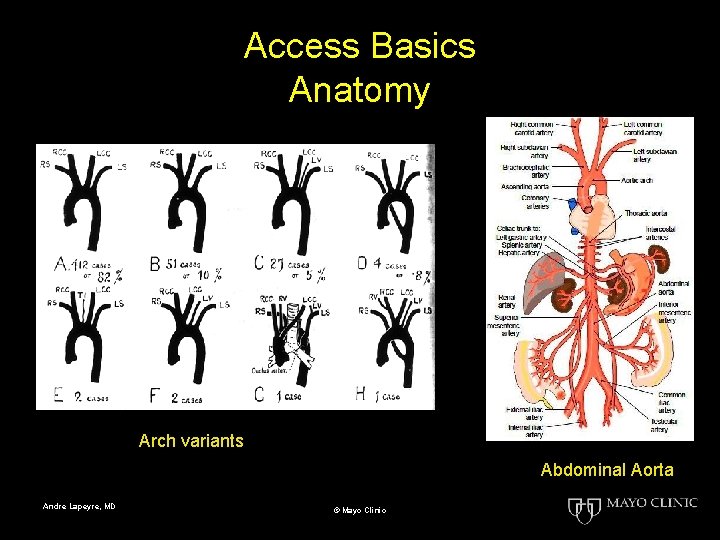
Access Basics Anatomy Arch variants Abdominal Aorta Andre Lapeyre, MD © Mayo Clinic
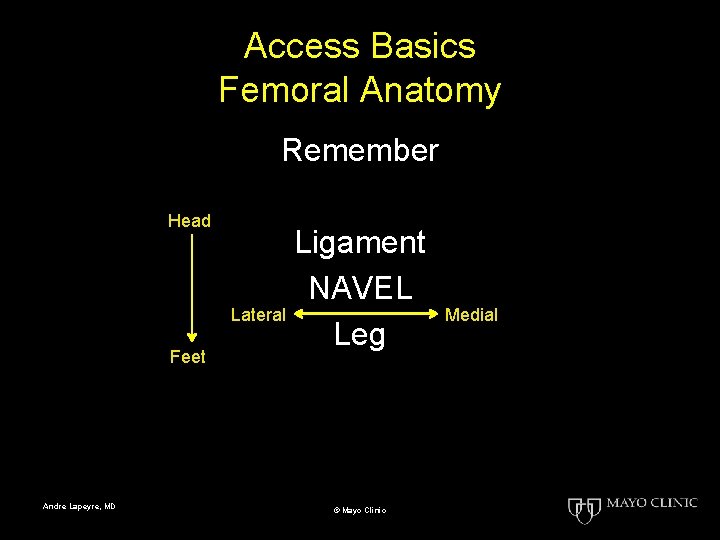
Access Basics Femoral Anatomy Remember Head Feet Andre Lapeyre, MD Ligament NAVEL Lateral Leg © Mayo Clinic Medial
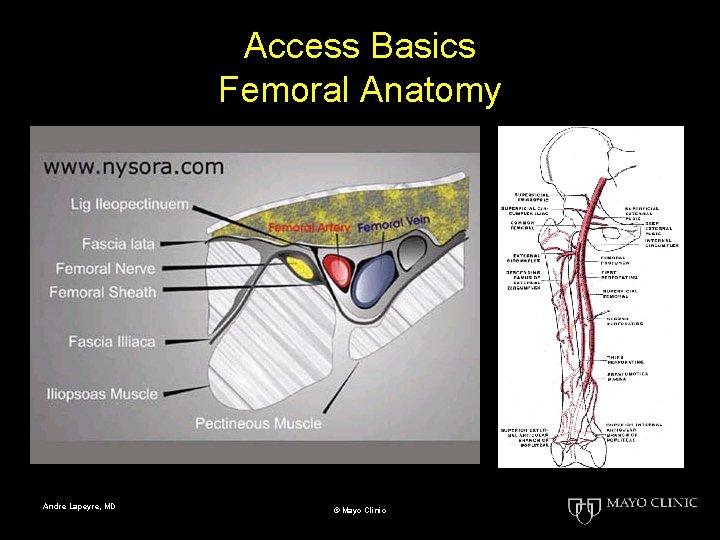
Access Basics Femoral Anatomy Andre Lapeyre, MD © Mayo Clinic
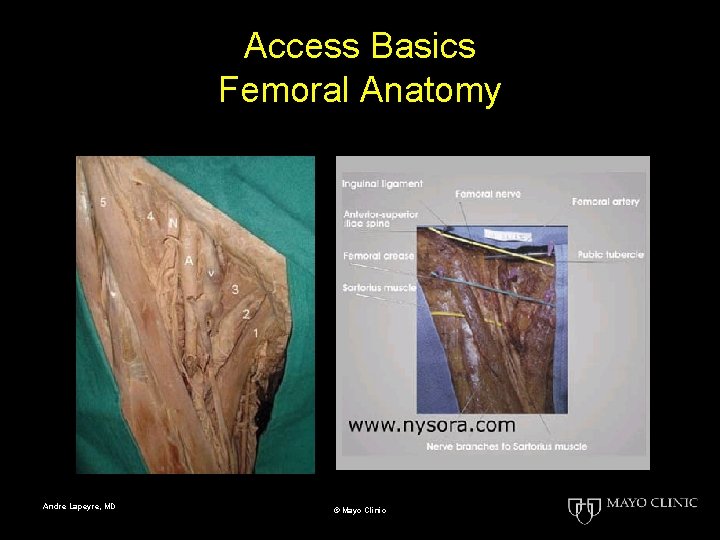
Access Basics Femoral Anatomy Andre Lapeyre, MD © Mayo Clinic
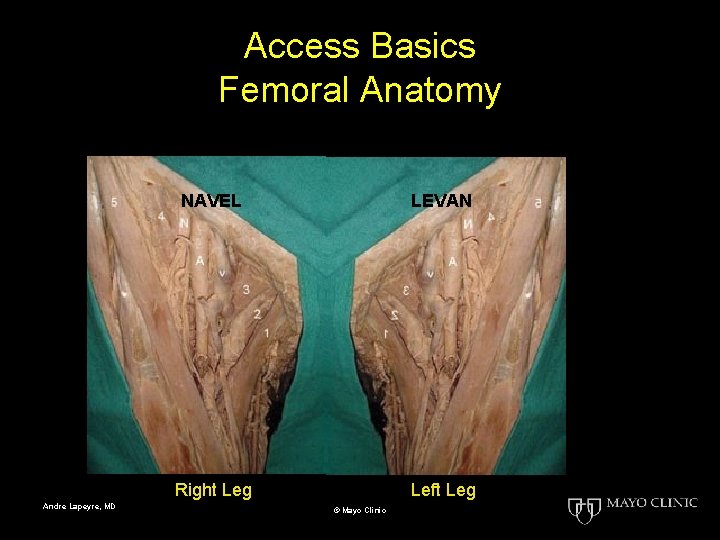
Access Basics Femoral Anatomy Andre Lapeyre, MD NAVEL LEVAN Right Leg Left Leg © Mayo Clinic
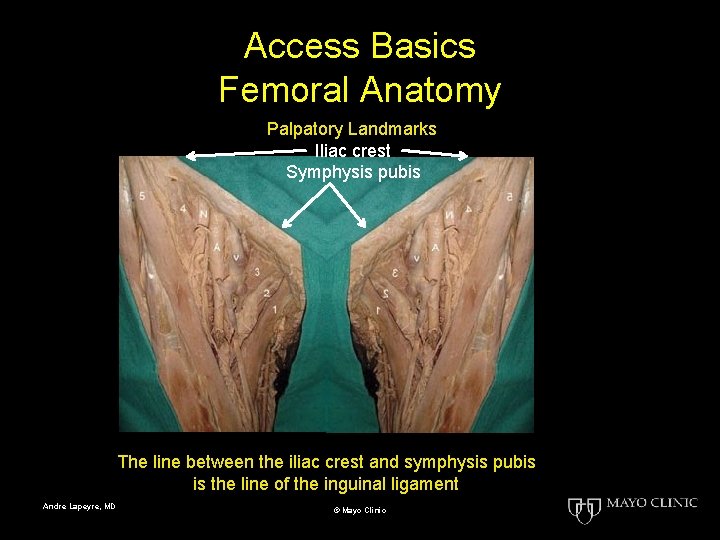
Access Basics Femoral Anatomy Palpatory Landmarks Iliac crest Symphysis pubis The line between the iliac crest and symphysis pubis is the line of the inguinal ligament Andre Lapeyre, MD © Mayo Clinic
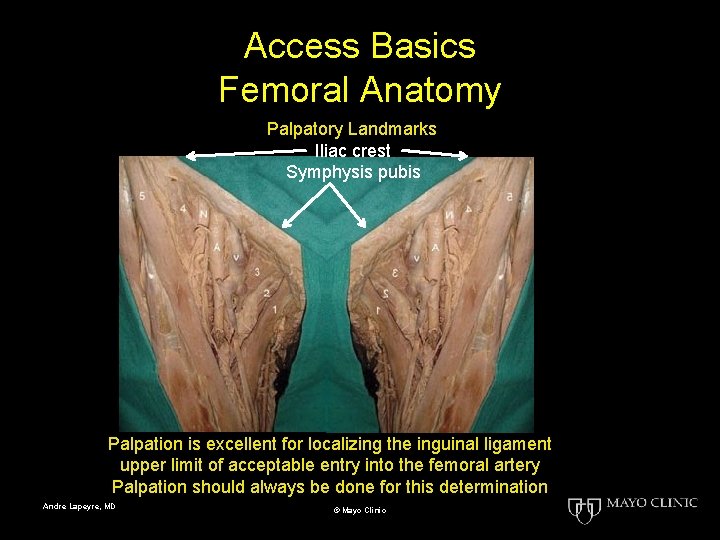
Access Basics Femoral Anatomy Palpatory Landmarks Iliac crest Symphysis pubis Palpation is excellent for localizing the inguinal ligament upper limit of acceptable entry into the femoral artery Palpation should always be done for this determination Andre Lapeyre, MD © Mayo Clinic
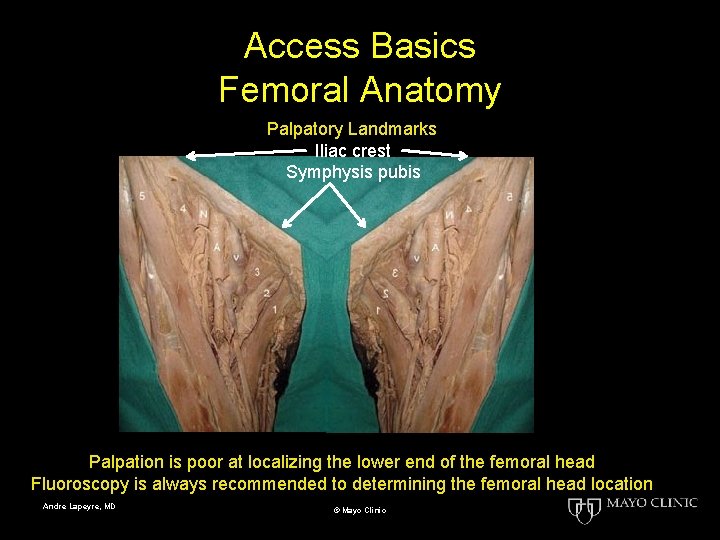
Access Basics Femoral Anatomy Palpatory Landmarks Iliac crest Symphysis pubis Palpation is poor at localizing the lower end of the femoral head Fluoroscopy is always recommended to determining the femoral head location Andre Lapeyre, MD © Mayo Clinic
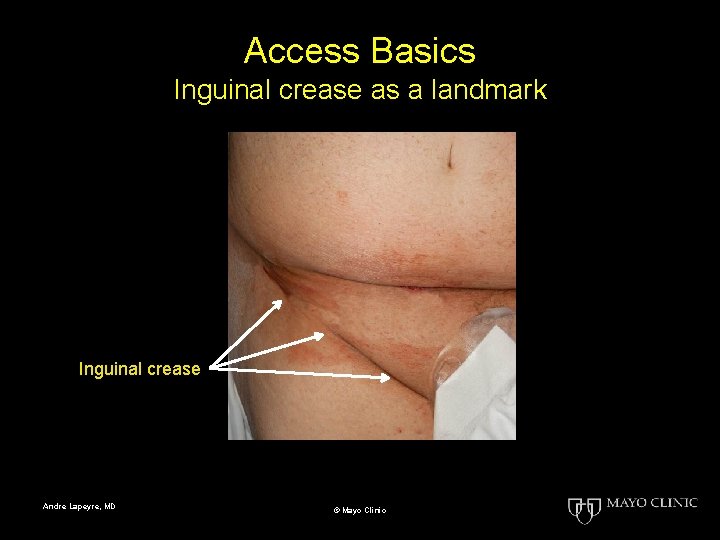
Access Basics Inguinal crease as a landmark Inguinal crease Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Skin Crease Some teach – always stick in the crease Andre Lapeyre, MD © Mayo Clinic
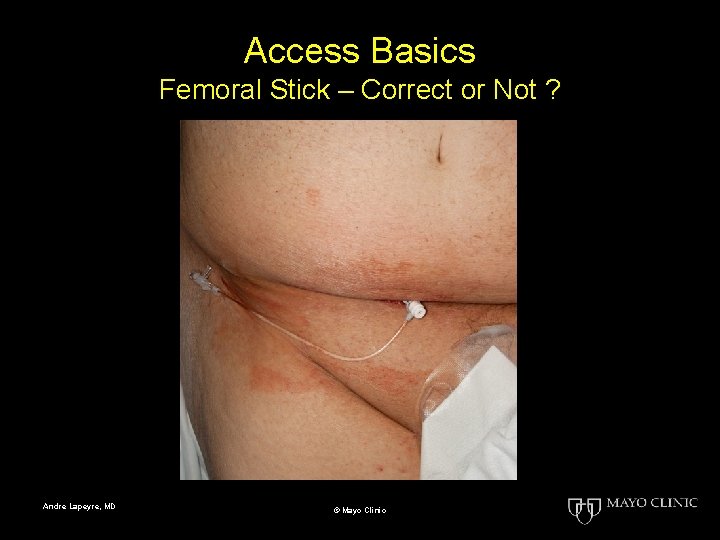
Access Basics Femoral Stick – Correct or Not ? Andre Lapeyre, MD © Mayo Clinic
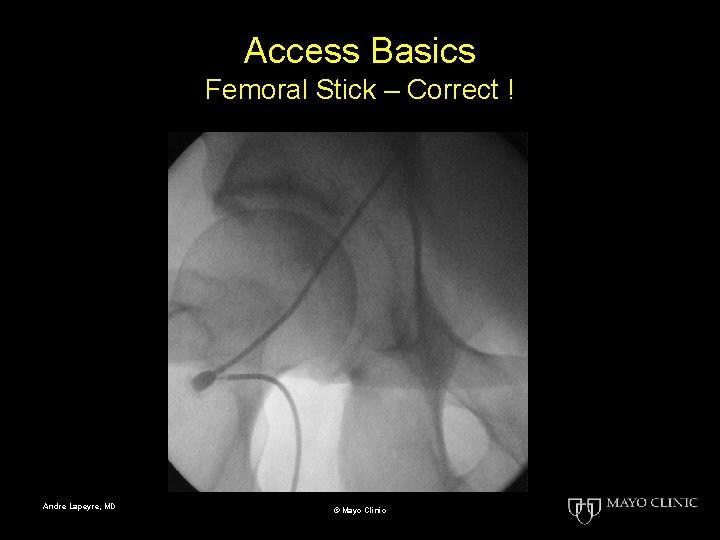
Access Basics Femoral Stick – Correct ! Andre Lapeyre, MD © Mayo Clinic
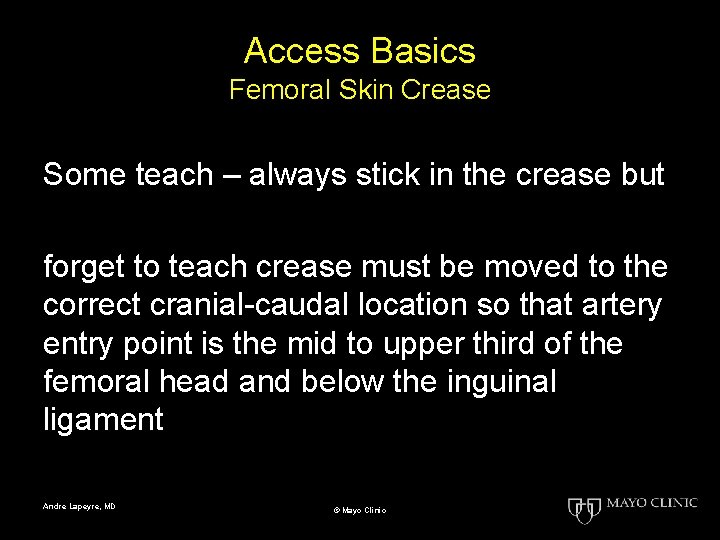
Access Basics Femoral Skin Crease Some teach – always stick in the crease but forget to teach crease must be moved to the correct cranial-caudal location so that artery entry point is the mid to upper third of the femoral head and below the inguinal ligament Andre Lapeyre, MD © Mayo Clinic
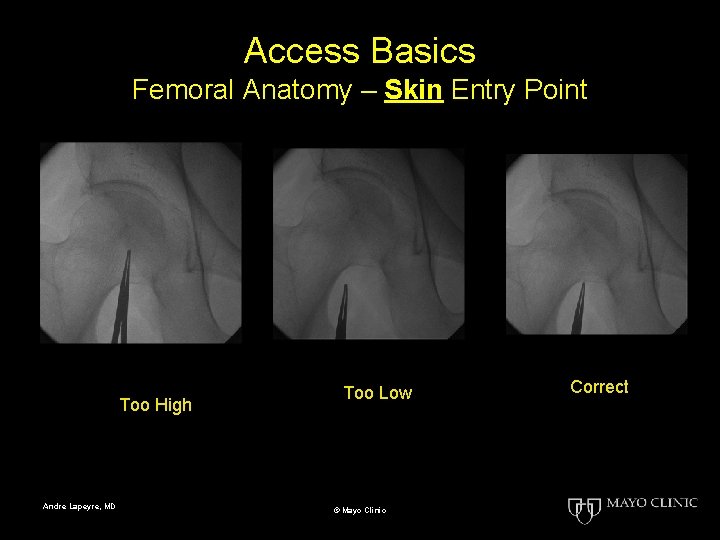
Access Basics Femoral Anatomy – Skin Entry Point Too High Andre Lapeyre, MD Too Low © Mayo Clinic Correct
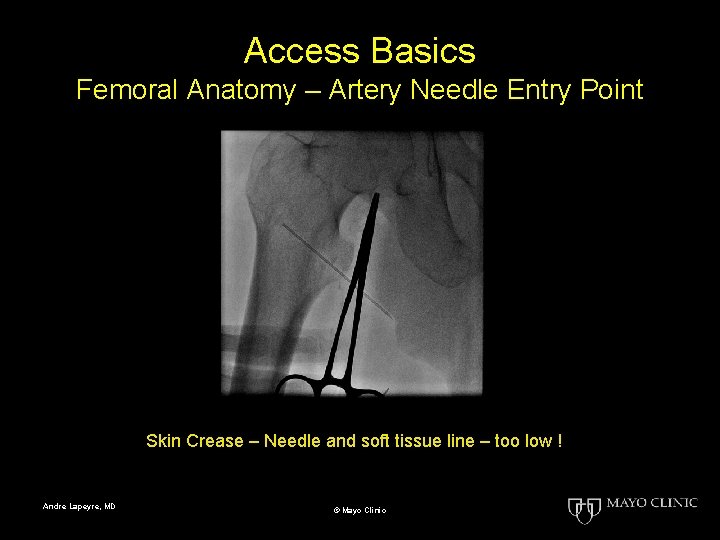
Access Basics Femoral Anatomy – Artery Needle Entry Point Skin Crease – Needle and soft tissue line – too low ! Andre Lapeyre, MD © Mayo Clinic
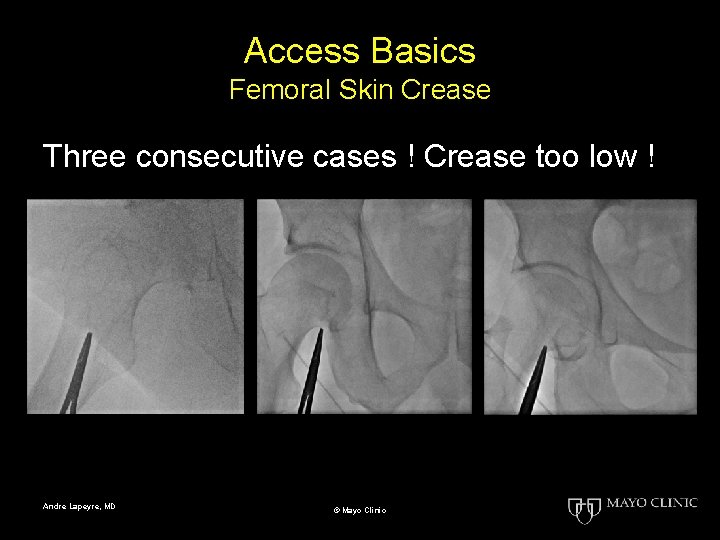
Access Basics Femoral Skin Crease Three consecutive cases ! Crease too low ! Andre Lapeyre, MD © Mayo Clinic
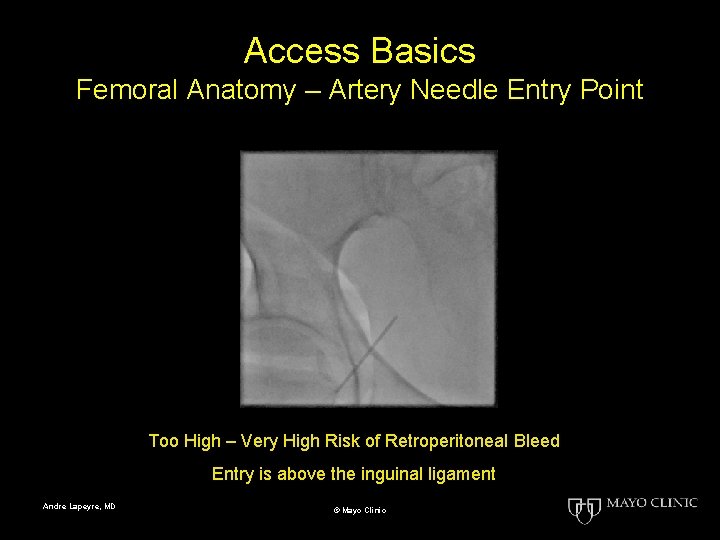
Access Basics Femoral Anatomy – Artery Needle Entry Point Too High – Very High Risk of Retroperitoneal Bleed Entry is above the inguinal ligament Andre Lapeyre, MD © Mayo Clinic
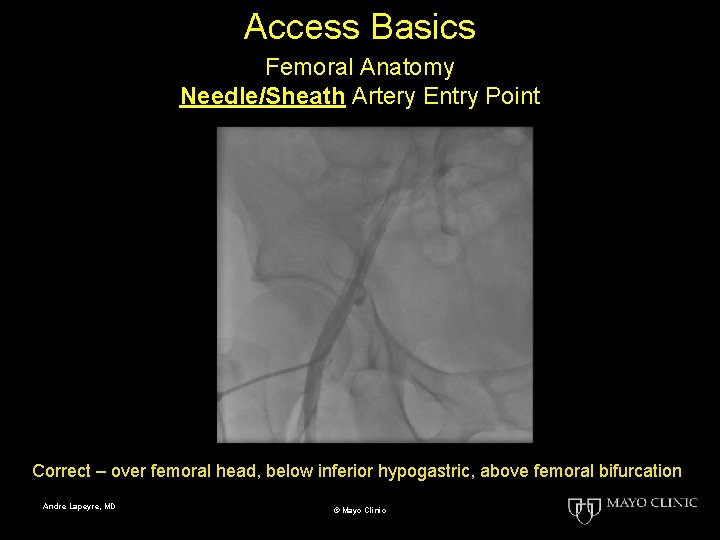
Access Basics Femoral Anatomy Needle/Sheath Artery Entry Point Correct – over femoral head, below inferior hypogastric, above femoral bifurcation Andre Lapeyre, MD © Mayo Clinic
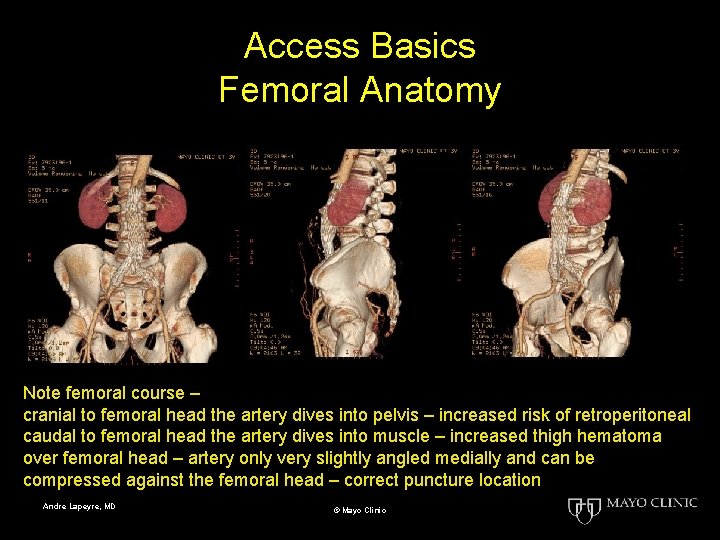
Access Basics Femoral Anatomy Note femoral course – cranial to femoral head the artery dives into pelvis – increased risk of retroperitoneal caudal to femoral head the artery dives into muscle – increased thigh hematoma over femoral head – artery only very slightly angled medially and can be compressed against the femoral head – correct puncture location Andre Lapeyre, MD © Mayo Clinic
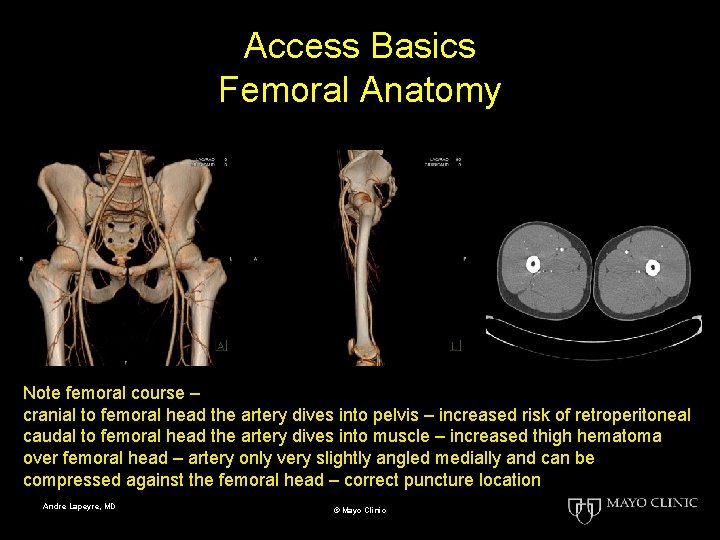
Access Basics Femoral Anatomy Note femoral course – cranial to femoral head the artery dives into pelvis – increased risk of retroperitoneal caudal to femoral head the artery dives into muscle – increased thigh hematoma over femoral head – artery only very slightly angled medially and can be compressed against the femoral head – correct puncture location Andre Lapeyre, MD © Mayo Clinic
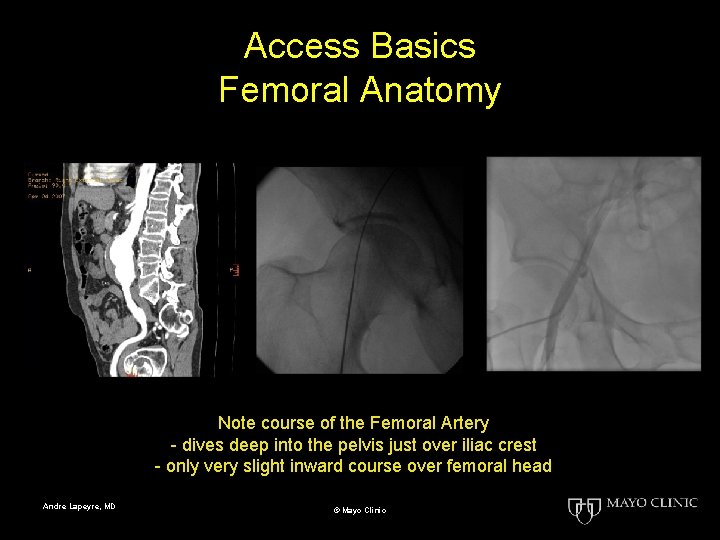
Access Basics Femoral Anatomy Note course of the Femoral Artery - dives deep into the pelvis just over iliac crest - only very slight inward course over femoral head Andre Lapeyre, MD © Mayo Clinic
Access Basics Fluoroscopy ? vs ? Ultrasound • Femoral artery ultrasound excellent for ensuring access above the femoral bifurcation. • Ultrasound very poor at preventing access above the femoral head/inguinal ligament • Ultrasound should be used as a complimentary and adjunctive technique along with fluoroscopic visualization. Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Anesthesia • Large skin wheal – skin hurts • Needle • straight in with gentle aspiration • straight out injecting track of local anesthesia deep to superficial • Avoid injecting blood if possible • Increases s. q. fibrosis for future procedures • Mini-regional block technique • Most of local just lateral to vessel • dermatome innervation • Note: 10 cc of 1% lidocaine = 100 mg Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Skin Nicks • • • ≤ 5 F sheath – skin nick unnecessary If needed At fluoro skin entry site, over pulse (arterial) Venous is medial to pulse and slightly below fluoro skin arterial entry site Just large enough for sheath DO NOT go deep !!!!! Blunt dilation to open track Andre Lapeyre, MD © Mayo Clinic
Access Basics Femoral Arterial Puncture • In line with artery – easier and reduces risk of side wall stick • Straight in – straight out • NO wiggle, redirecting, reaiming • NO roll or coring • NO leveraging • Bevel toward head of patient • ~45 degree angle to enter artery over upper 1/2 to 1/3 of the femoral head Andre Lapeyre, MD © Mayo Clinic
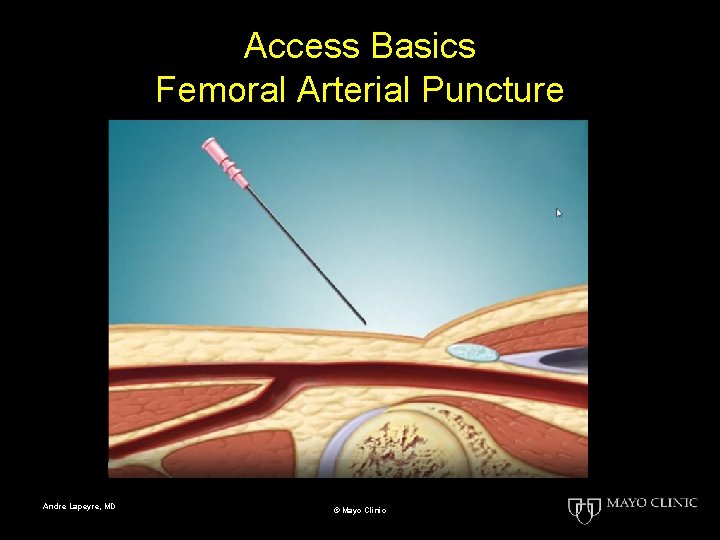
Access Basics Femoral Arterial Puncture Andre Lapeyre, MD © Mayo Clinic
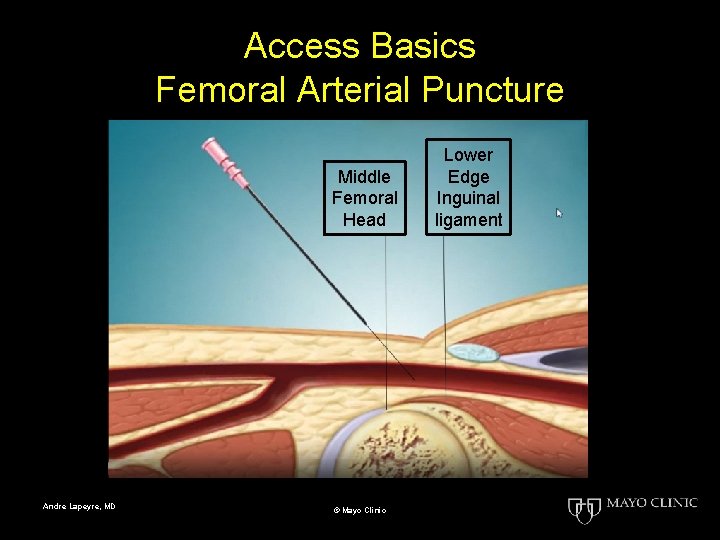
Access Basics Femoral Arterial Puncture Middle Femoral Head Andre Lapeyre, MD © Mayo Clinic Lower Edge Inguinal ligament
Access Basics Femoral Venous Puncture • One and one-half finger breath medial to pulse • Slightly below arterial skin entry site • If miss – miss medial • Slightly steeper vertical angle • Aspirate gentle as entering and withdrawing • Other as per arterial Andre Lapeyre, MD © Mayo Clinic
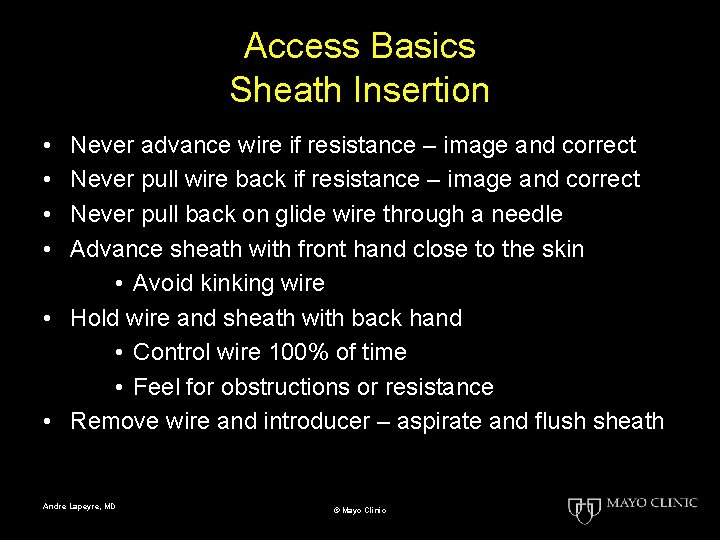
Access Basics Sheath Insertion • • Never advance wire if resistance – image and correct Never pull wire back if resistance – image and correct Never pull back on glide wire through a needle Advance sheath with front hand close to the skin • Avoid kinking wire • Hold wire and sheath with back hand • Control wire 100% of time • Feel for obstructions or resistance • Remove wire and introducer – aspirate and flush sheath Andre Lapeyre, MD © Mayo Clinic
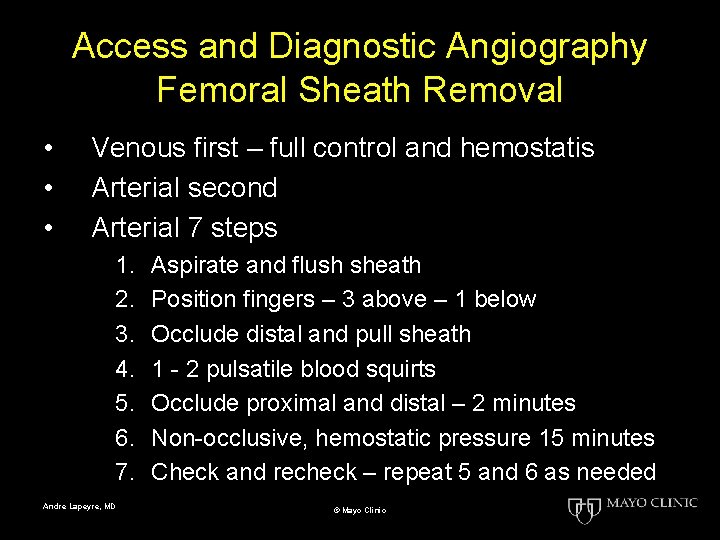
Access and Diagnostic Angiography Femoral Sheath Removal • • • Venous first – full control and hemostatis Arterial second Arterial 7 steps 1. 2. 3. 4. 5. 6. 7. Andre Lapeyre, MD Aspirate and flush sheath Position fingers – 3 above – 1 below Occlude distal and pull sheath 1 - 2 pulsatile blood squirts Occlude proximal and distal – 2 minutes Non-occlusive, hemostatic pressure 15 minutes Check and recheck – repeat 5 and 6 as needed © Mayo Clinic
- End of this slide set - Andre Lapeyre, MD © Mayo Clinic
- Slides: 35