ACC Phase II Laurel Karabatsos Deputy Medicaid Director
ACC Phase II Laurel Karabatsos Deputy Medicaid Director 1

Our Mission Improving health care access and outcomes for the people we serve while demonstrating sound stewardship of financial resources 2

coordinated and integrated care that Moving toward more increasingly rewards improved health 3
Accountable Care Collaborative Improve Health and Reduce Costs Medical Home Regional Coordination Data Ensure Medicaid members have a focal point of care. Medicaid members have complex needs and are served by multiple systems. Regional umbrella organizations help to coordinate across systems. Members, providers and the system receive the data needed to make real-time decisions that improve care, increase coordination of services and improve overall efficiencies. 4

Phase I Goals • To improve member health & reduce costs Phase I Objectives • Expand access to comprehensive primary care. • Provide a focal point of care. • Ensure a positive member and provider experience and promote engagement. • Effectively apply an unprecedented level of statewide data and analytics functionality. 5

Phase II Goals • To improve member health & reduce costs Phase II Objectives • Join physical and behavioral health under one accountable entity • Strengthen coordination of services by advancing team-based care and health neighborhoods • Promote member choice and engagement • Pay providers for the increased value they deliver • Ensure greater accountability and transparency 6

Regional Accountable Entity Physical Health Care Behavioral Health Care Per Member/ Per Month Behavioral Health Capitation 7
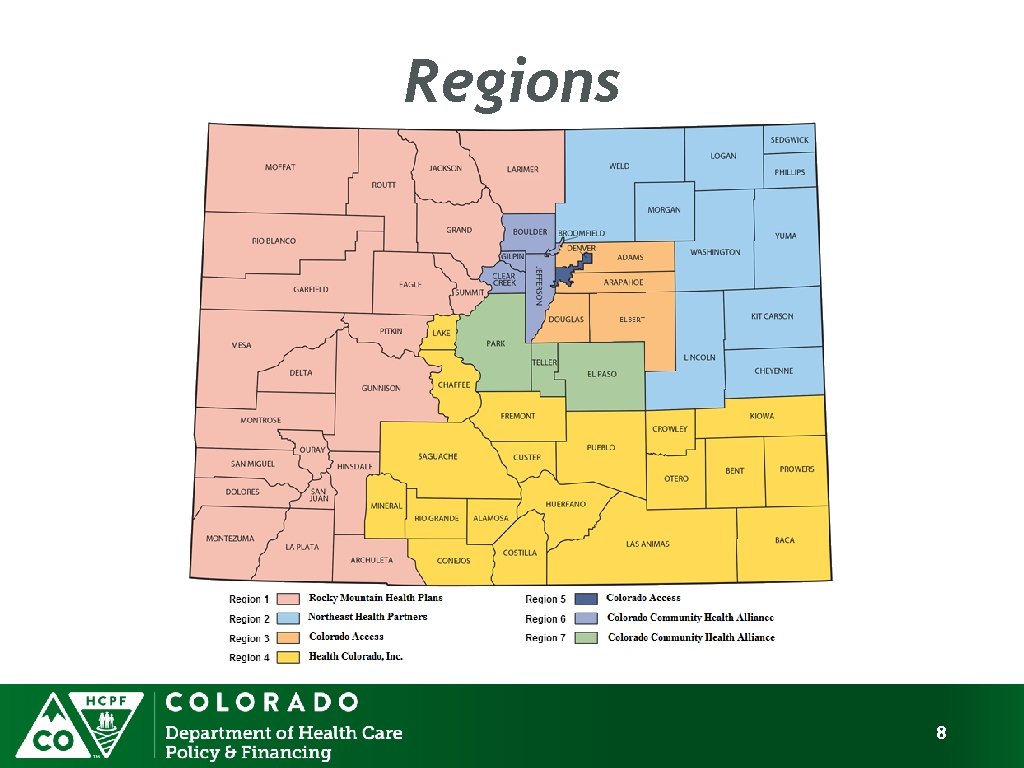
Regions 8

Objectives Continued. . . Strengthen Coordination • Population Health Management • Increase PCMP standards • Neighborhood • Community • Increase RAE Authority to support activities Promote Member Choice • Immediate Enrollment • Choice of PCMP • PCMP Selection Drives RAE Assignment • Health Needs Survey • Behavioral Health Services in Primary Care Pay for Value • Pay for Performance § Key Performance Indicators § Public Reporting § Flexible Funding Pool § Behavioral Health Incentives • RAE Increased Flexibility • Alignment with Alternative Payment Model Accountability/Transparency • Increase Financial Transparency and Reporting § Utilization Management § Provider Network Decisions § Conflict of Interest in Governance § Financial Reporting • Increase Funding Tied to Value • Matrix Team Management 9
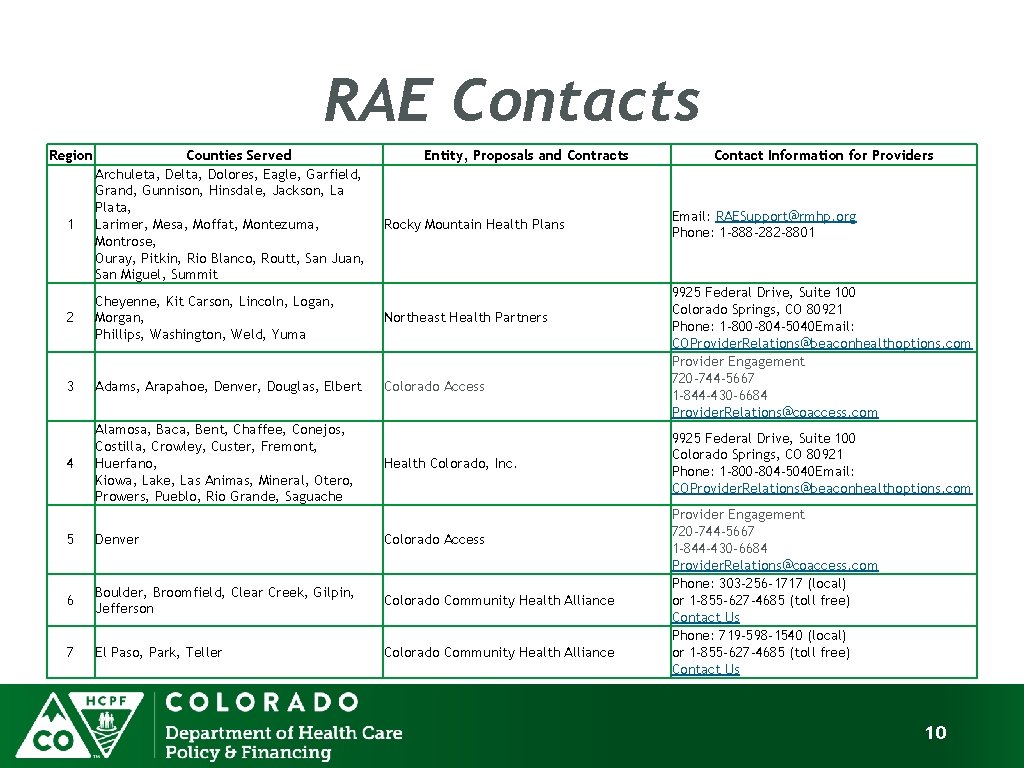
RAE Contacts Region 1 Counties Served Archuleta, Delta, Dolores, Eagle, Garfield, Grand, Gunnison, Hinsdale, Jackson, La Plata, Larimer, Mesa, Moffat, Montezuma, Montrose, Ouray, Pitkin, Rio Blanco, Routt, San Juan, San Miguel, Summit Entity, Proposals and Contracts Rocky Mountain Health Plans 2 Cheyenne, Kit Carson, Lincoln, Logan, Morgan, Phillips, Washington, Weld, Yuma Northeast Health Partners 3 Adams, Arapahoe, Denver, Douglas, Elbert Colorado Access 4 Alamosa, Baca, Bent, Chaffee, Conejos, Costilla, Crowley, Custer, Fremont, Huerfano, Kiowa, Lake, Las Animas, Mineral, Otero, Prowers, Pueblo, Rio Grande, Saguache Health Colorado, Inc. 5 Denver Colorado Access 6 Boulder, Broomfield, Clear Creek, Gilpin, Jefferson Colorado Community Health Alliance 7 El Paso, Park, Teller Colorado Community Health Alliance Contact Information for Providers Email: RAESupport@rmhp. org Phone: 1 -888 -282 -8801 9925 Federal Drive, Suite 100 Colorado Springs, CO 80921 Phone: 1 -800 -804 -5040 Email: COProvider. Relations@beaconhealthoptions. com Provider Engagement 720 -744 -5667 1 -844 -430 -6684 Provider. Relations@coaccess. com Phone: 303 -256 -1717 (local) or 1 -855 -627 -4685 (toll free) Contact Us Phone: 719 -598 -1540 (local) or 1 -855 -627 -4685 (toll free) Contact Us 10
- Slides: 10