Abstract 11065 Efficacy of sorafenib in patients with
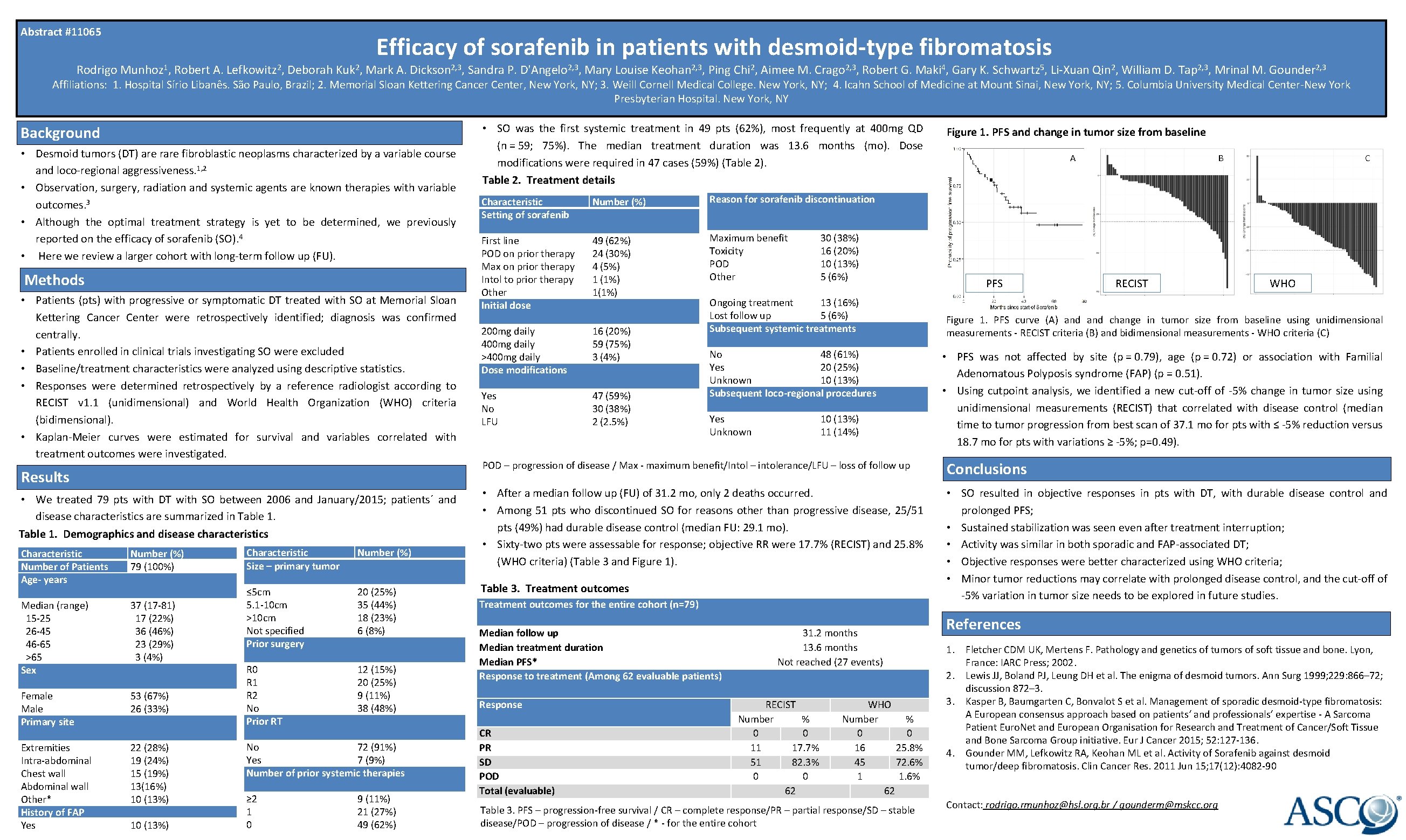
Abstract #11065 Efficacy of sorafenib in patients with desmoid-type fibromatosis Rodrigo Munhoz 1, Robert A. Lefkowitz 2, Deborah Kuk 2, Mark A. Dickson 2, 3, Sandra P. D'Angelo 2, 3, Mary Louise Keohan 2, 3, Ping Chi 2, Aimee M. Crago 2, 3, Robert G. Maki 4, Gary K. Schwartz 5, Li-Xuan Qin 2, William D. Tap 2, 3, Mrinal M. Gounder 2, 3 Affiliations: 1. Hospital Sírio Libanês. São Paulo, Brazil; 2. Memorial Sloan Kettering Cancer Center, New York, NY; 3. Weill Cornell Medical College. New York, NY; 4. Icahn School of Medicine at Mount Sinai, New York, NY; 5. Columbia University Medical Center-New York Presbyterian Hospital. New York, NY Background • Desmoid tumors (DT) are rare fibroblastic neoplasms characterized by a variable course and loco-regional aggressiveness. 1, 2 • Observation, surgery, radiation and systemic agents are known therapies with variable outcomes. 3 • Although the optimal treatment strategy is yet to be determined, we previously reported on the efficacy of sorafenib (SO). 4 • Here we review a larger cohort with long-term follow up (FU). Methods • Patients (pts) with progressive or symptomatic DT treated with SO at Memorial Sloan Kettering Cancer Center were retrospectively identified; diagnosis was confirmed centrally. • Patients enrolled in clinical trials investigating SO were excluded • Baseline/treatment characteristics were analyzed using descriptive statistics. • Responses were determined retrospectively by a reference radiologist according to RECIST v 1. 1 (unidimensional) and World Health Organization (WHO) criteria (bidimensional). • Kaplan-Meier curves were estimated for survival and variables correlated with treatment outcomes were investigated. Results • We treated 79 pts with DT with SO between 2006 and January/2015; patients´ and disease characteristics are summarized in Table 1. Demographics and disease characteristics Characteristic Number of Patients Age- years Median (range) 15 -25 26 -45 46 -65 >65 Sex Female Male Primary site Extremities Intra-abdominal Chest wall Abdominal wall Other* History of FAP Yes Number (%) 79 (100%) 37 (17 -81) 17 (22%) 36 (46%) 23 (29%) 3 (4%) 53 (67%) 26 (33%) 22 (28%) 19 (24%) 15 (19%) 13(16%) 10 (13%) Characteristic Number (%) Size – primary tumor ≤ 5 cm 20 (25%) 5. 1 -10 cm 35 (44%) >10 cm 18 (23%) Not specified 6 (8%) Prior surgery R 0 12 (15%) R 1 20 (25%) R 2 9 (11%) No 38 (48%) Prior RT No 72 (91%) Yes 7 (9%) Number of prior systemic therapies ≥ 2 9 (11%) 1 21 (27%) 0 49 (62%) • SO was the first systemic treatment in 49 pts (62%), most frequently at 400 mg QD (n = 59; 75%). The median treatment duration was 13. 6 months (mo). Dose modifications were required in 47 cases (59%) (Table 2). Table 2. Treatment details Characteristic Setting of sorafenib Number (%) First line POD on prior therapy Max on prior therapy Intol to prior therapy Other Initial dose 49 (62%) 24 (30%) 4 (5%) 1 (1%) 1(1%) 200 mg daily 400 mg daily >400 mg daily Dose modifications 16 (20%) 59 (75%) 3 (4%) Yes No LFU 47 (59%) 30 (38%) 2 (2. 5%) Figure 1. PFS and change in tumor size from baseline A B C Reason for sorafenib discontinuation Maximum benefit 30 (38%) Toxicity 16 (20%) POD 10 (13%) Other 5 (6%) Ongoing treatment 13 (16%) Lost follow up 5 (6%) Subsequent systemic treatments No 48 (61%) Yes 20 (25%) Unknown 10 (13%) Subsequent loco-regional procedures Yes 10 (13%) Unknown 11 (14%) PFS RECIST WHO Figure 1. PFS curve (A) and change in tumor size from baseline using unidimensional measurements - RECIST criteria (B) and bidimensional measurements - WHO criteria (C) • PFS was not affected by site (p = 0. 79), age (p = 0. 72) or association with Familial Adenomatous Polyposis syndrome (FAP) (p = 0. 51). • Using cutpoint analysis, we identified a new cut-off of -5% change in tumor size using unidimensional measurements (RECIST) that correlated with disease control (median time to tumor progression from best scan of 37. 1 mo for pts with ≤ -5% reduction versus 18. 7 mo for pts with variations ≥ -5%; p=0. 49). POD – progression of disease / Max - maximum benefit/Intol – intolerance/LFU – loss of follow up Conclusions • After a median follow up (FU) of 31. 2 mo, only 2 deaths occurred. • Among 51 pts who discontinued SO for reasons other than progressive disease, 25/51 pts (49%) had durable disease control (median FU: 29. 1 mo). • Sixty-two pts were assessable for response; objective RR were 17. 7% (RECIST) and 25. 8% (WHO criteria) (Table 3 and Figure 1). • SO resulted in objective responses in pts with DT, with durable disease control and prolonged PFS; • Sustained stabilization was seen even after treatment interruption; • Activity was similar in both sporadic and FAP-associated DT; • Objective responses were better characterized using WHO criteria; • Minor tumor reductions may correlate with prolonged disease control, and the cut-off of -5% variation in tumor size needs to be explored in future studies. Table 3. Treatment outcomes for the entire cohort (n=79) Median follow up Median treatment duration Median PFS* Response to treatment (Among 62 evaluable patients) Response CR PR SD POD Total (evaluable) 31. 2 months 13. 6 months Not reached (27 events) References 1. 2. RECIST Number % 0 0 11 17. 7% 51 82. 3% 0 0 62 WHO Number % 0 0 16 25. 8% 45 72. 6% 1 1. 6% 62 Table 3. PFS – progression-free survival / CR – complete response/PR – partial response/SD – stable disease/POD – progression of disease / * - for the entire cohort 3. 4. Fletcher CDM UK, Mertens F. Pathology and genetics of tumors of soft tissue and bone. Lyon, France: IARC Press; 2002. Lewis JJ, Boland PJ, Leung DH et al. The enigma of desmoid tumors. Ann Surg 1999; 229: 866– 72; discussion 872– 3. Kasper B, Baumgarten C, Bonvalot S et al. Management of sporadic desmoid-type fibromatosis: A European consensus approach based on patients‘ and professionals‘ expertise - A Sarcoma Patient Euro. Net and European Organisation for Research and Treatment of Cancer/Soft Tissue and Bone Sarcoma Group initiative. Eur J Cancer 2015; 52: 127 -136. Gounder MM, Lefkowitz RA, Keohan ML et al. Activity of Sorafenib against desmoid tumor/deep fibromatosis. Clin Cancer Res. 2011 Jun 15; 17(12): 4082 -90 Contact: rodrigo. rmunhoz@hsl. org. br / gounderm@mskcc. org
- Slides: 1