ABO ANTIGENS n n n The ABO system
ABO ANTIGENS
n n n The ABO system was described in 1901 by Karl Landsteiner and was the first blood group system to be discovered. By 1902, the four major groups had been identified as A, B, AB and O. Landsteiner showed that the serum of certain healthy people agglutinated the red cells of others, this being a constant characteristic.
This information gave rise to Landsteiner's Law, i. e. : ‘’Whenever an (A and/or B) antigen is not present on the red cells, the corresponding antibody is found in the serum’’ n
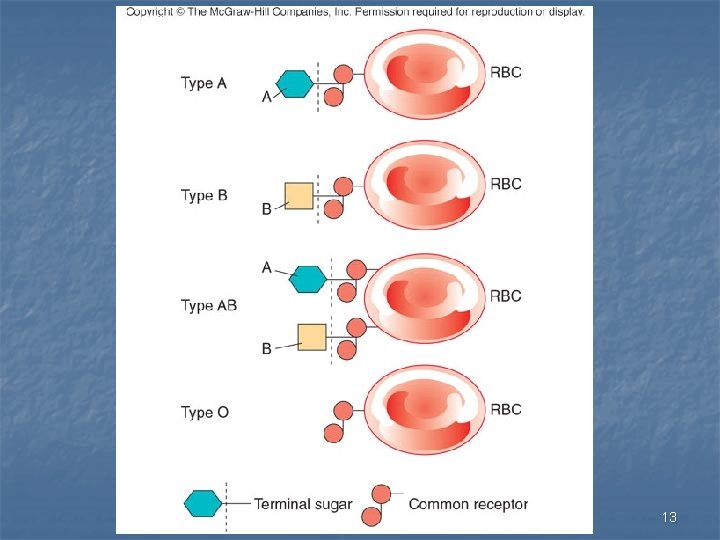
ABO ANTIGENS n n n The ABO genes do not actually code for the production of ABO antigens but, produce specific Glycosyltransferases. ABO blood groups dependant upon the formation of H antigen from the H gene. The H gene produces H antigen, then the A gene or B gene add to the H antigen to produce A antigen or B antigen. Since O gene is blank gene (does not produce a product), O cells contain only H substance. The H gene is very common in the random population, with greater than 99. 99 %.
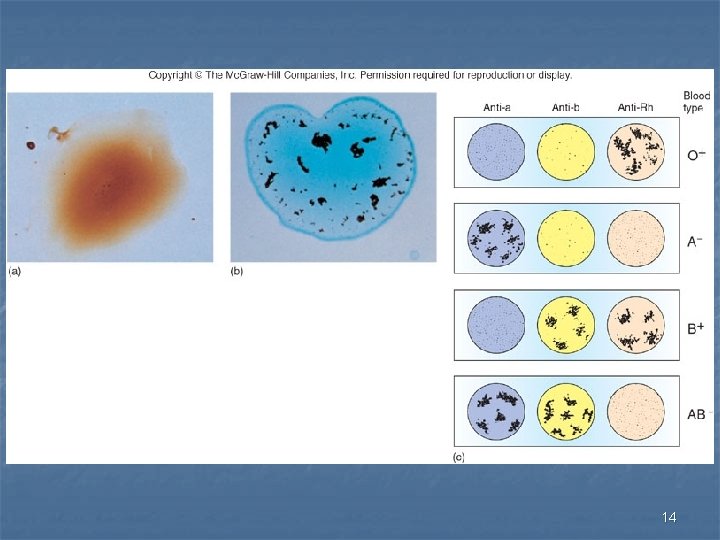
n n n The genotype ‘hh’ is extremely rare, this ‘hh’ genotype is called the “Bombay” blood group. Bombay cells have no A, B or H antigens and develop anti-A, anti-B and anti-H antibodies. They are compatible only to Bombay individuals will be type as an O. There are 4 main blood groups: A, B, AB and O. Landsteiner identified that if a person’s red cells lack either one or both of the A and B antigens, their serum always contains the corresponding anti-A and/or anti-B antibodies.
n n n Therefore : Group A: - Have the A antigen on their red cells and anti-B in their serum. Group B: - Have the B antigen on their red cells and anti-A in their serum. Group AB: - Have both A and B antigens on their red cells and no antibodies in their serum. Therefore it called Universal Recipient Group O: - Have no antigen on their red cells and have both anti-A and anti-B in their serum. Therefore it called Universal Donor
ABO SUBGROUP n n The major subgroups of A are A 1 and A 2; the difference between them is partly quantitative and partly qualitative. These subgroups can be distinguished using specific anti–A 1 reagents. Group A red cells that react with both anti. A and anti- A 1 are classified as A 1. The red cells that react with anti-A only and not with anti- A 1 are classified as A 2.
n n n Subgroups of B are very rare, they are less common than subgroups of A. Some of these subgroups are B 3, Bx, Bel and Bm. No commercial antisera are available for typing of these Subgroups.
ABO ANTIBODIES n n n ABO antibodies are described as being "naturally acquired" because they are present in the plasma of all healthy adults, except group AB. ABO antibodies are usually of both Ig. M and rarely Ig. G group. Children under the age of 3 months usually have little or no antibody present in their plasma. Any antibody present in a baby's plasma at birth is likely to be of maternal origin, due to placental transfer of Ig. G antibody.
n n . Antibody strength reaches normal adult levels at approximately 5 years of age, remaining relatively stable during adult life, then usually declining in old age. The routine presence of antibodies in the serum/plasma is unique to the ABO system.
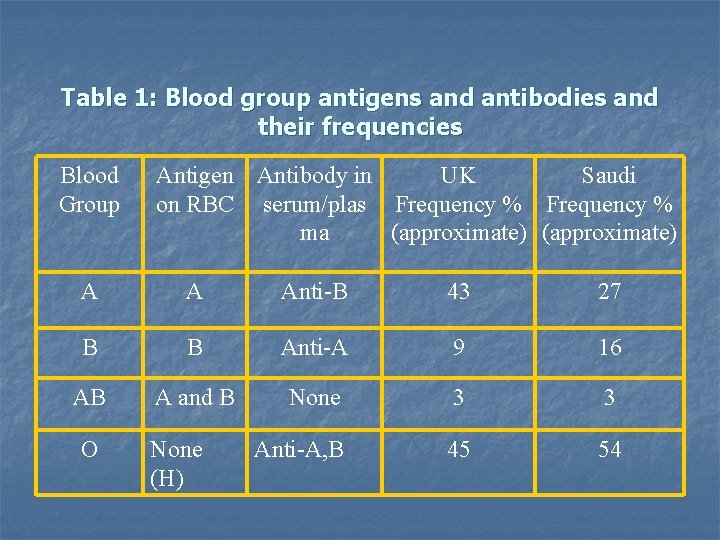
Table 1: Blood group antigens and antibodies and their frequencies Blood Group Antigen Antibody in UK Saudi on RBC serum/plas Frequency % ma (approximate) A A Anti-B 43 27 B B Anti-A 9 16 AB A and B None 3 3 Anti-A, B 45 54 O None (H)
13
14
15
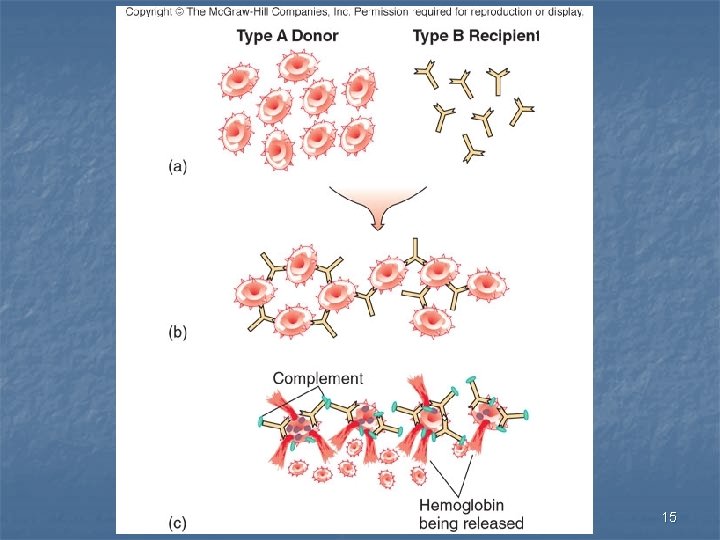
CLINICAL SIGNIFICANCE OF ABO blood group I- ABO incompatible reactions: n n transfusion Usually resulting from the transfusion of group A or B red cells to a group O person Capable of producing acute intravascular haemolysis. Clinical effects are frequently severe and potentially fatal, even when only small volumes of transfused cells are involved. The frequency of such reactions is low, but all errors (i. e. technical, clerical or patient identification) are avoidable.
n n n Pregnancy ABO is a common cause of Haemolytic Disease of the Newborn (HDN), i. e. in group O mothers (with Ig. G anti-A, B) who have group A or B children. The effect of ABO HDN is invariably always mild due to the limitations of the ability of the maternal antibody to cause fetal red cell damage.
n n n Transplantation ABO antigens are expressed on a variety of tissue cells within the body and as a consequence some transplanted organs (e. g. kidney) must be ABO compatible. Bone marrow transplants can be performed across either 'major' (i. e. group A donor and a group O patient) or `minor' (i. e. group O donor and a group A patient) ABO differences, though this may require manipulation of the marrow to removed red cells (antigen) and/or plasma (antibody).
Any Questions? ?

Thank YOU
- Slides: 20