ABNORMAL PRESENTATION by Noha Eid Mohamed Hassan Lecturer
ABNORMAL PRESENTATION by Noha Eid Mohamed Hassan Lecturer OB/GYN El-Shatby Maternity University Hospital Faculty of Medicine University of Alexandria
INTRODUCTION AND OCCIPITO-POSTERIOR POSITION
INTRODUCTION
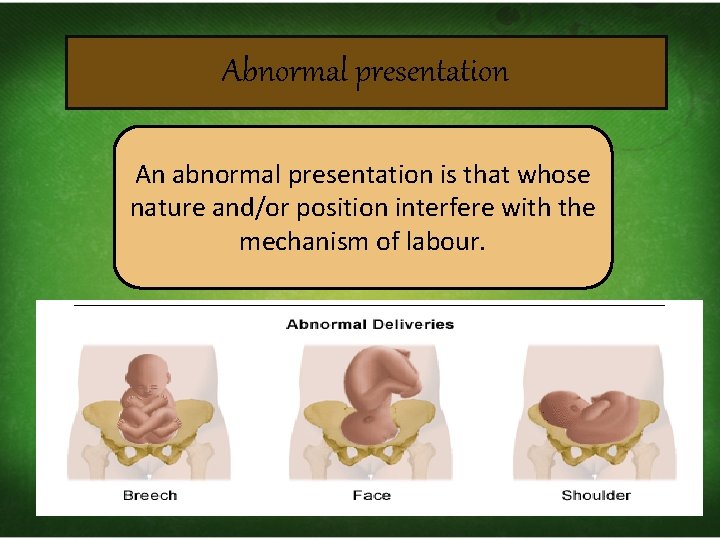
Abnormal presentation An abnormal presentation is that whose nature and/or position interfere with the mechanism of labour.

OCCIPITO POSTERIOR POSITION
Definition: It is a vertex presentation with foetal back directed posteriorly.
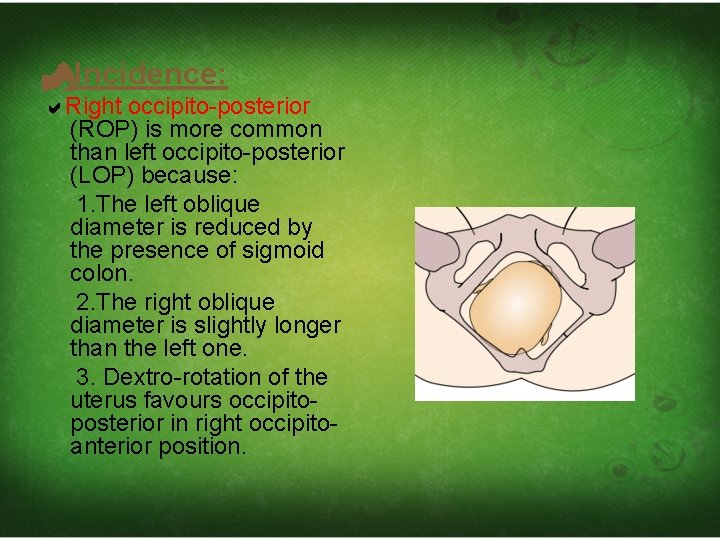
Incidence: Right occipito-posterior (ROP) is more common than left occipito-posterior (LOP) because: 1. The left oblique diameter is reduced by the presence of sigmoid colon. 2. The right oblique diameter is slightly longer than the left one. 3. Dextro-rotation of the uterus favours occipitoposterior in right occipitoanterior position.
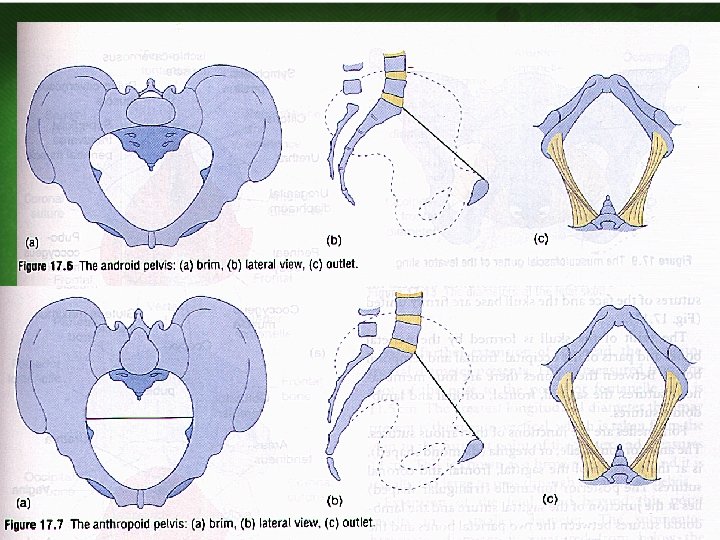
AETIOLOGY 1)Shape of pelvis
2)Maternal kyphosis: The convexity of the foetal back fits with the concavity of the lumbar kyphosis. 3)Other causes of malpresentations: as – placenta praevia, – pelvic tumours, – pendulous abdomen, – polyhydramnios, – multiple pregnancy.
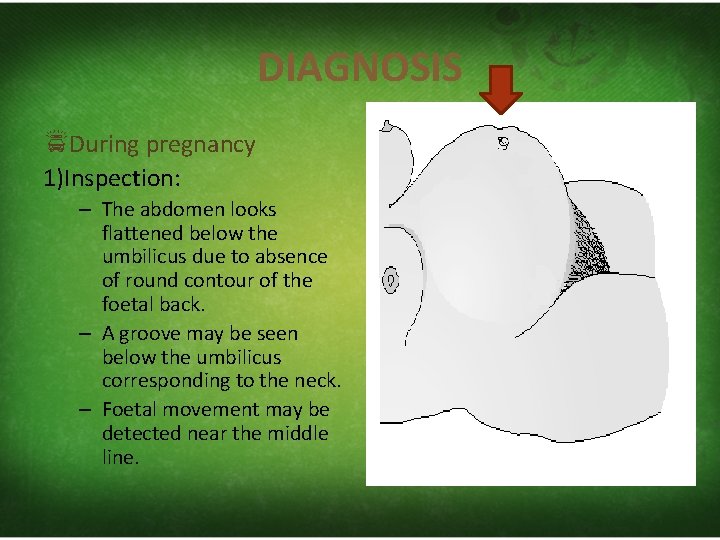
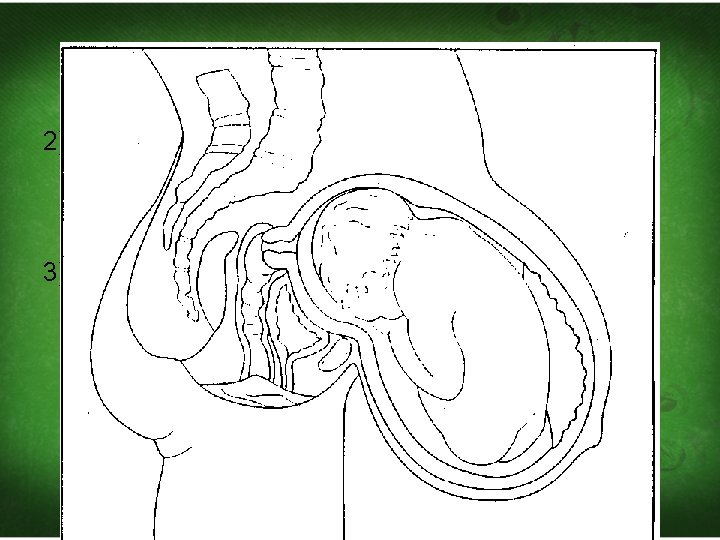
DIAGNOSIS During pregnancy 1)Inspection: – The abdomen looks flattened below the umbilicus due to absence of round contour of the foetal back. – A groove may be seen below the umbilicus corresponding to the neck. – Foetal movement may be detected near the middle line.
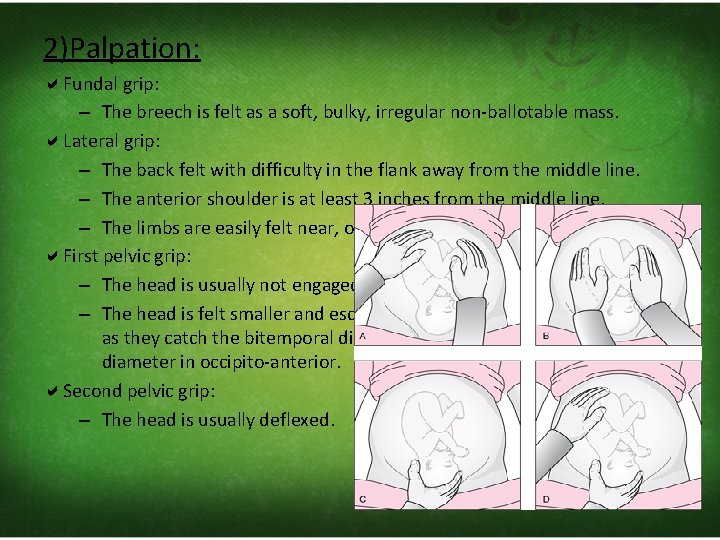
2)Palpation: Fundal grip: – The breech is felt as a soft, bulky, irregular non‐ballotable mass. Lateral grip: – The back felt with difficulty in the flank away from the middle line. – The anterior shoulder is at least 3 inches from the middle line. – The limbs are easily felt near, or on both sides, of the middle line. First pelvic grip: – The head is usually not engaged due to deflexion. – The head is felt smaller and escapes easily from the palpating fingers as they catch the bitemporal diameter instead of the biparietal diameter in occipito‐anterior. Second pelvic grip: – The head is usually deflexed.
• Auscultation: – FHS are heard in the flank away from the middle line. – In major degree of deflexion, the FHS may be heard in middle line. • Ultrasonography or lateral view x‐ray.
• During labour
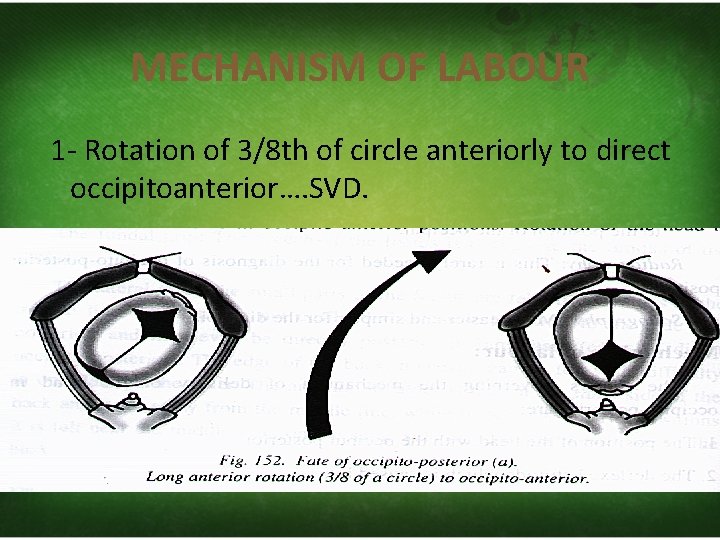
MECHANISM OF LABOUR 1‐ Rotation of 3/8 th of circle anteriorly to direct occipitoanterior…. SVD.
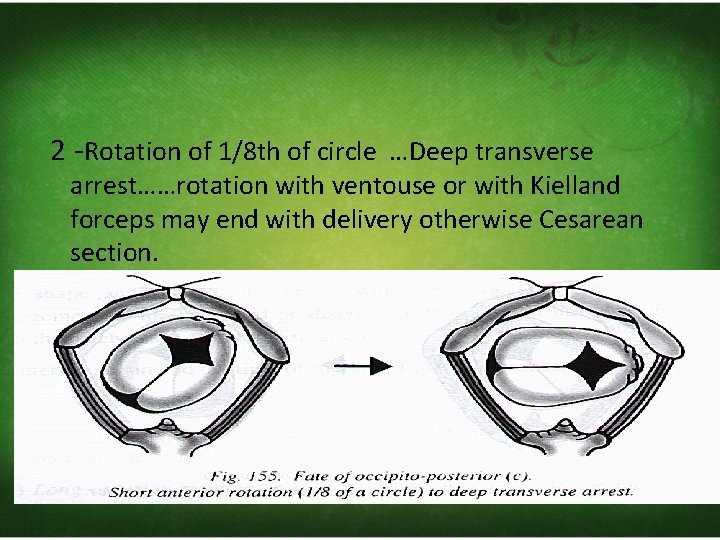
2 ‐Rotation of 1/8 th of circle …Deep transverse arrest……rotation with ventouse or with Kielland forceps may end with delivery otherwise Cesarean section.
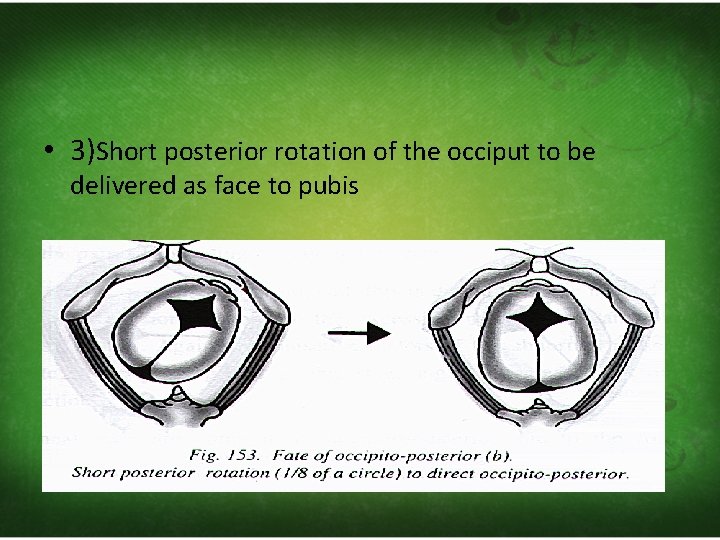
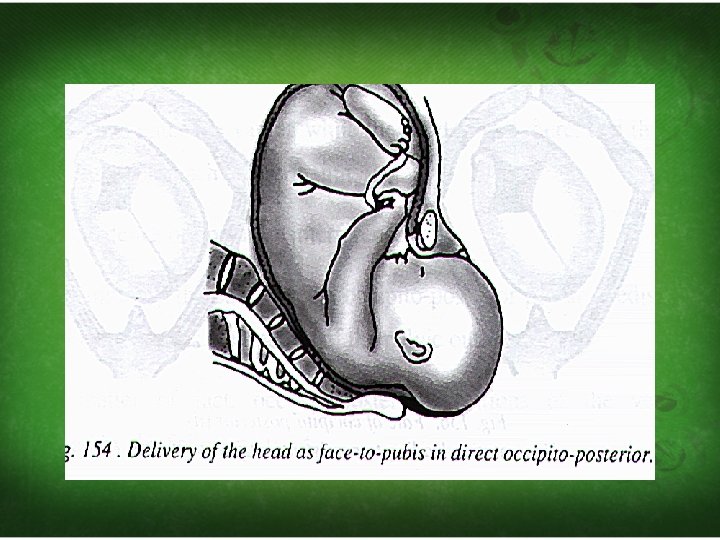
• 3)Short posterior rotation of the occiput to be delivered as face to pubis
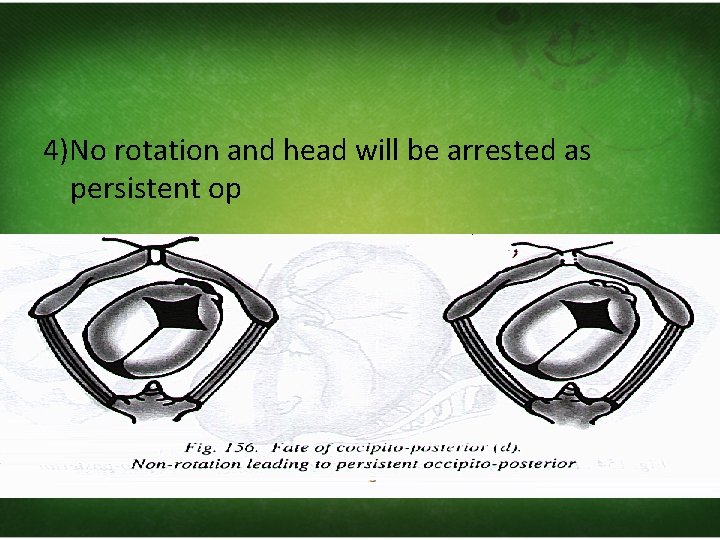
4)No rotation and head will be arrested as persistent op
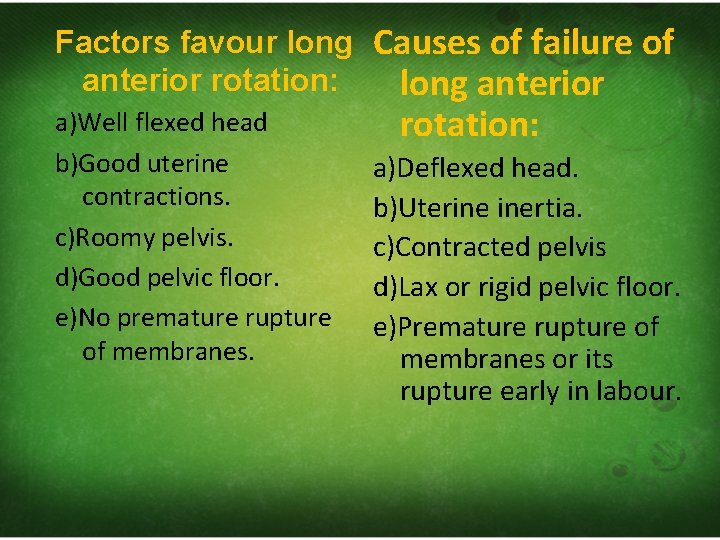
Factors favour long Causes of failure of anterior rotation: long anterior a)Well flexed head b)Good uterine contractions. c)Roomy pelvis. d)Good pelvic floor. e)No premature rupture of membranes. rotation: a)Deflexed head. b)Uterine inertia. c)Contracted pelvis d)Lax or rigid pelvic floor. e)Premature rupture of membranes or its rupture early in labour.
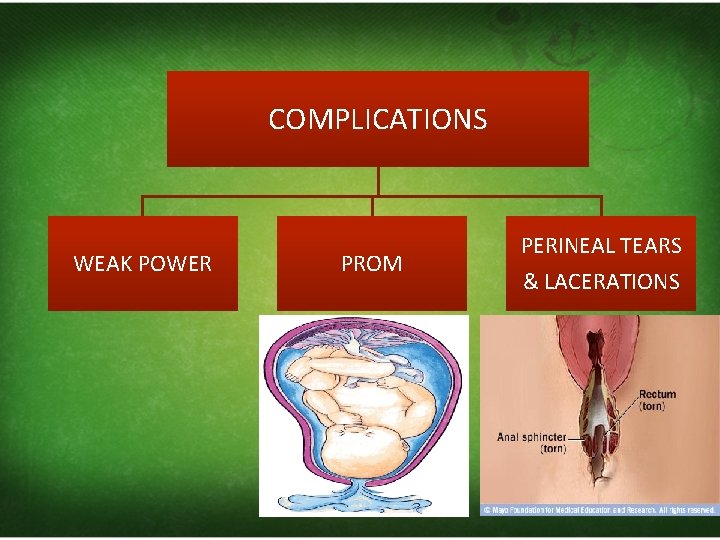
COMPLICATIONS WEAK POWER PROM PERINEAL TEARS & LACERATIONS
MANAGEMENT During pregnancy : positional treatment by lying on the side (lateral position opposite to the direction of the back)
1 st STAGE • Exclude contracted pelvis. • Exclude presentation or prolapse of the cord. • Inertia and prolonged labour are expected so oxytocin may be indicated unless there is contraindication. • Contractions are sustained, irregular and accompanied by marked backache which needs analgesia as pethidine or epidural analgesia. • Avoid premature rupture of membranes by: ‐ – – rest in bed, no straining, avoid high enema, minimise vaginal examinations.
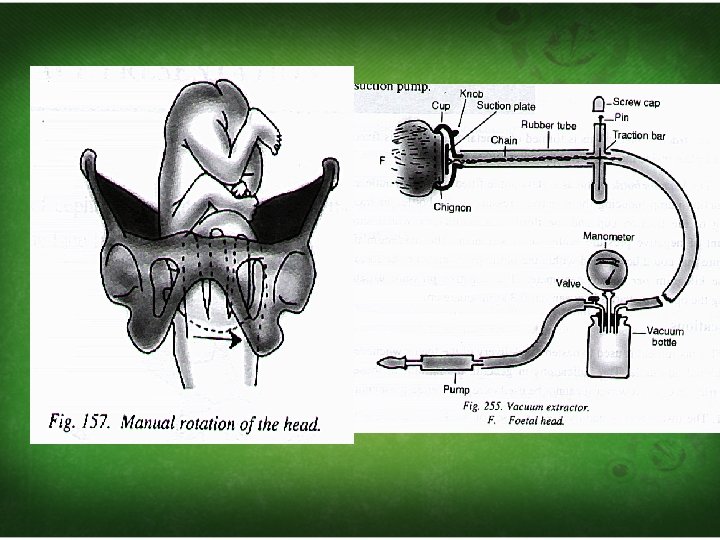
2 nd STAGE Wait for 60‐ 90 minutes. One of the following will occur: – Long internal rotation 3/8 circle: • occurs in about 90% of cases and delivery is completed as in normal labour. – Direct occipito-posterior (face to pubis): • occurs in about 6% of cases. – Deep transverse arrest (1%) and persistent occipito-posterior (3%): • The labour is obstructed and one of the following should be done: – Vacuum extraction (ventouse) – Manual rotation and extraction by forceps
CAESARIAN SECTION Indications a)Prolapse pulsating cord b)Elderly primigravida c)Contracted pelvis d)Placenta praevia
BROW, FACE AND COMPLEX PRESENTATION
BROW PRESENTATION
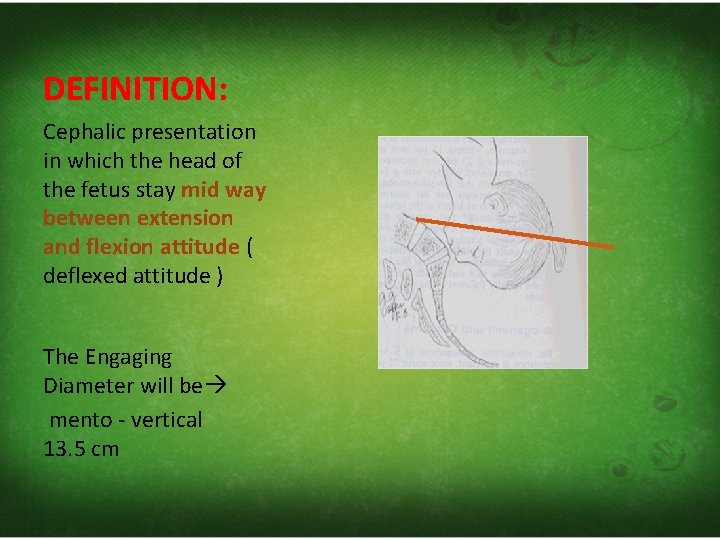
DEFINITION: Cephalic presentation in which the head of the fetus stay mid way between extension and flexion attitude ( deflexed attitude ) The Engaging Diameter will be mento ‐ vertical 13. 5 cm
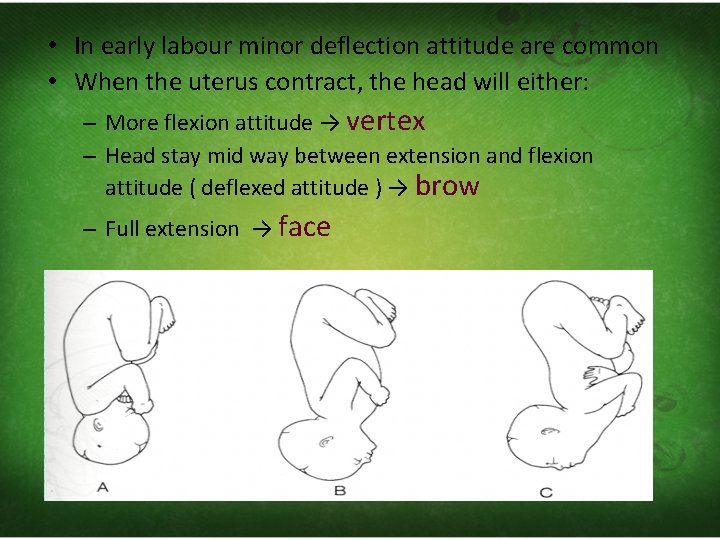
• In early labour minor deflection attitude are common • When the uterus contract, the head will either: – More flexion attitude → vertex – Head stay mid way between extension and flexion attitude ( deflexed attitude ) → brow – Full extension → face
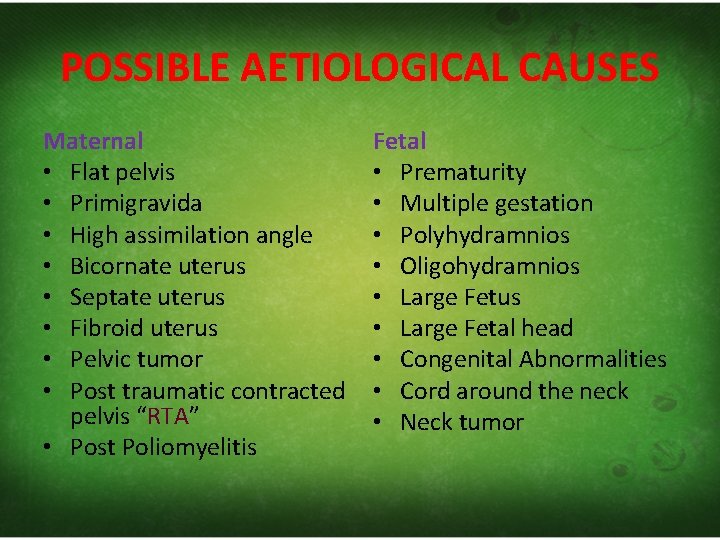
POSSIBLE AETIOLOGICAL CAUSES Maternal • Flat pelvis • Primigravida • High assimilation angle • Bicornate uterus • Septate uterus • Fibroid uterus • Pelvic tumor • Post traumatic contracted pelvis “RTA” • Post Poliomyelitis Fetal • Prematurity • Multiple gestation • Polyhydramnios • Oligohydramnios • Large Fetus • Large Fetal head • Congenital Abnormalities • Cord around the neck • Neck tumor
DENOMINATOR AND POSITION • Fronto‐anterior • Fronto‐posterior
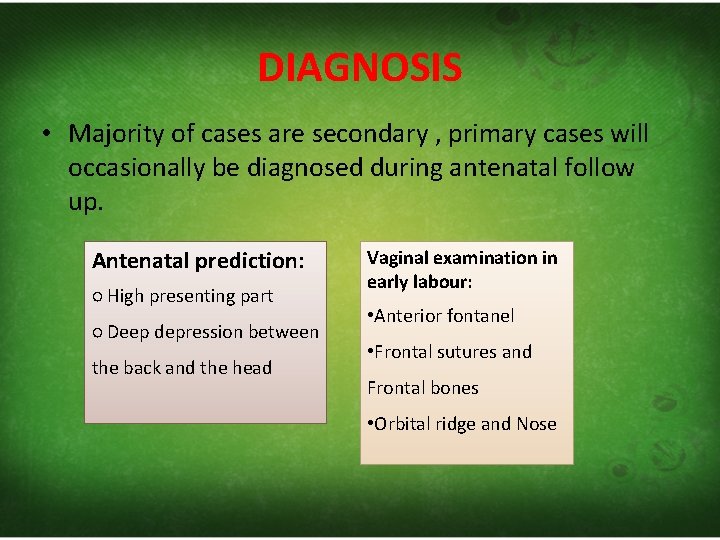
DIAGNOSIS • Majority of cases are secondary , primary cases will occasionally be diagnosed during antenatal follow up. Antenatal prediction: ○ High presenting part ○ Deep depression between the back and the head Vaginal examination in early labour: • Anterior fontanel • Frontal sutures and Frontal bones • Orbital ridge and Nose
MANAGEMENT • Brow presentation is not suitable for vaginal delivery because of the large longitudinal diameter (undeliverable cephalic presentation). If brow presentation diagnosed in early labour with no maternal of fetal compromise we may wait and review the condition after 2 hours if still brow … emergency cesarean section If brow presentation diagnosed in established labour with signs of obstructed labour ……. emergency cesarean section
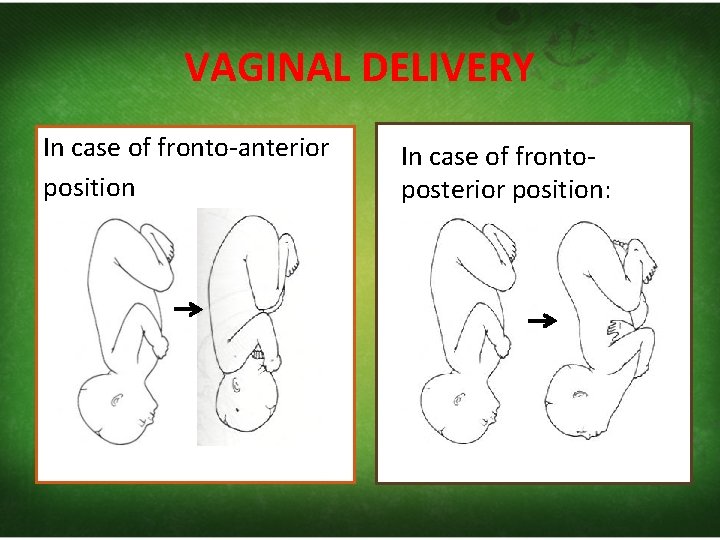
VAGINAL DELIVERY In case of fronto‐anterior position In case of fronto‐ posterior position:
FACE PRESENTATION
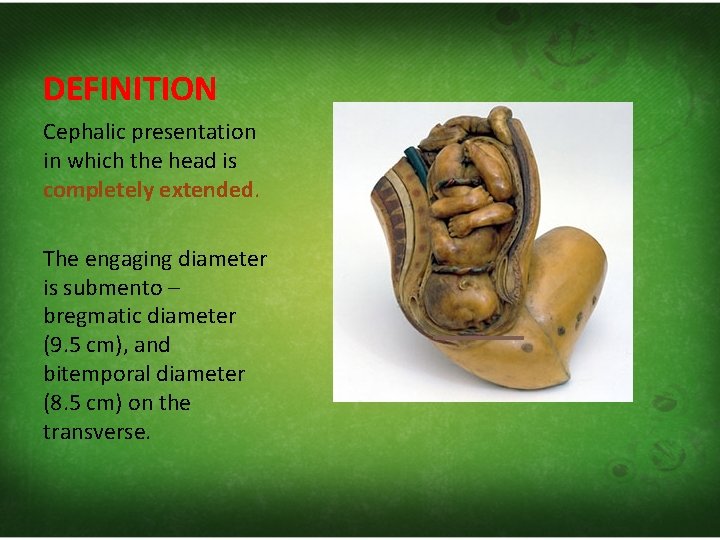
DEFINITION Cephalic presentation in which the head is completely extended. The engaging diameter is submento – bregmatic diameter (9. 5 cm), and bitemporal diameter (8. 5 cm) on the transverse.
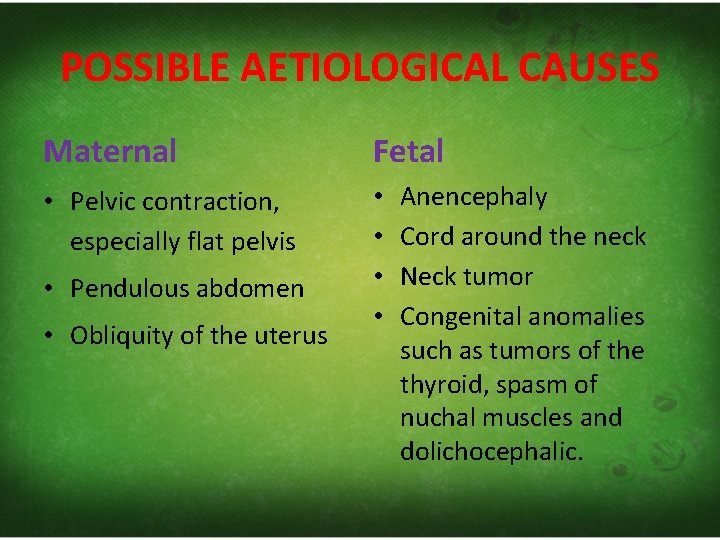
POSSIBLE AETIOLOGICAL CAUSES Maternal Fetal • Pelvic contraction, especially flat pelvis • • • Pendulous abdomen • Obliquity of the uterus Anencephaly Cord around the neck Neck tumor Congenital anomalies such as tumors of the thyroid, spasm of nuchal muscles and dolichocephalic.
TYPES Secondary face presentation Primary face presentation • The head is completely extended prior to the onset of labour • Due to fetal causes • More common • Head become extended during descent in the pelvis. • Due to maternal causes.
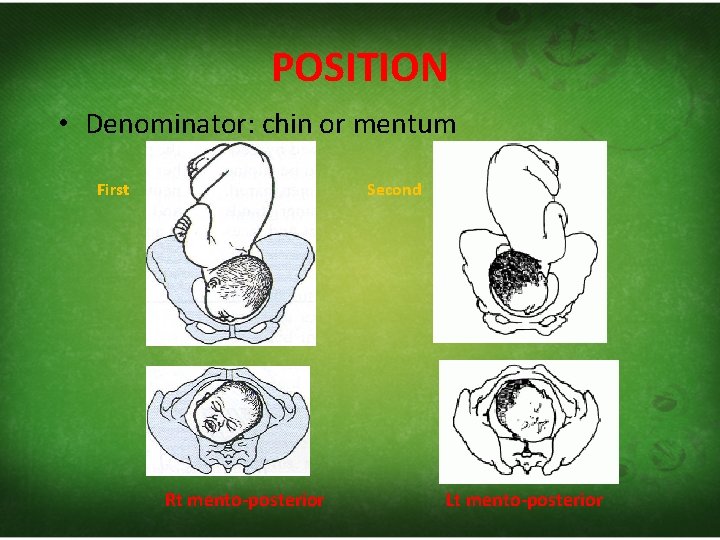
POSITION • Denominator: chin or mentum First Second Rt mento-posterior Lt mento-posterior
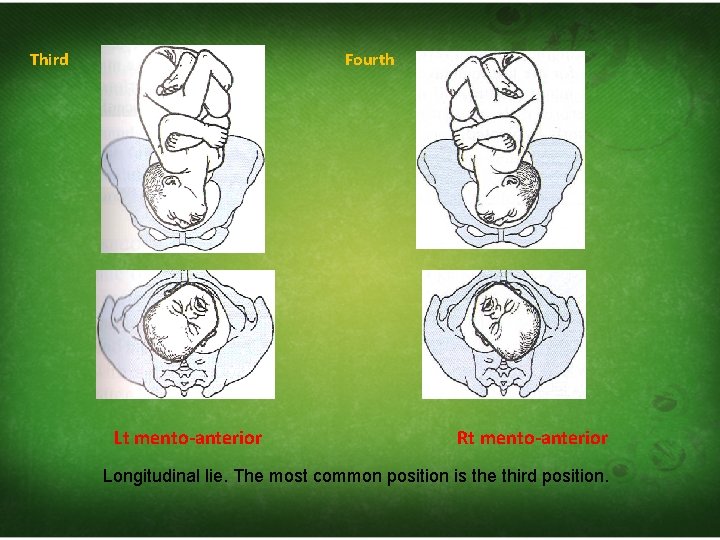
Third Fourth Lt mento-anterior Rt mento-anterior Longitudinal lie. The most common position is the third position.
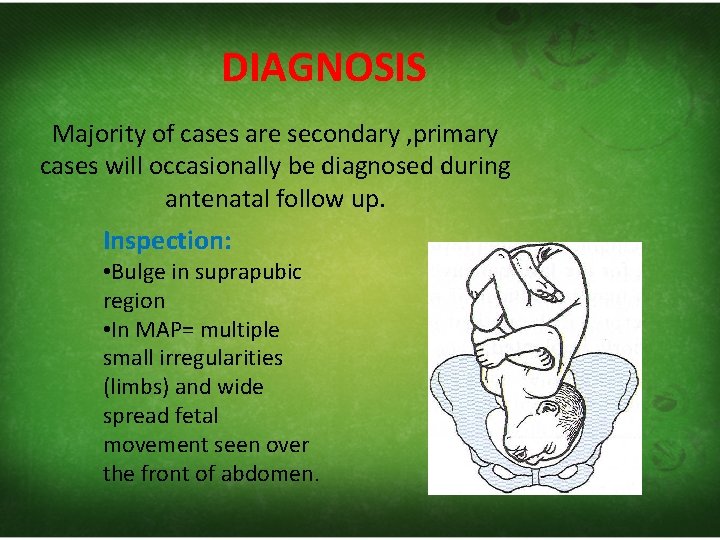
DIAGNOSIS Majority of cases are secondary , primary cases will occasionally be diagnosed during antenatal follow up. Inspection: • Bulge in suprapubic region • In MAP= multiple small irregularities (limbs) and wide spread fetal movement seen over the front of abdomen.
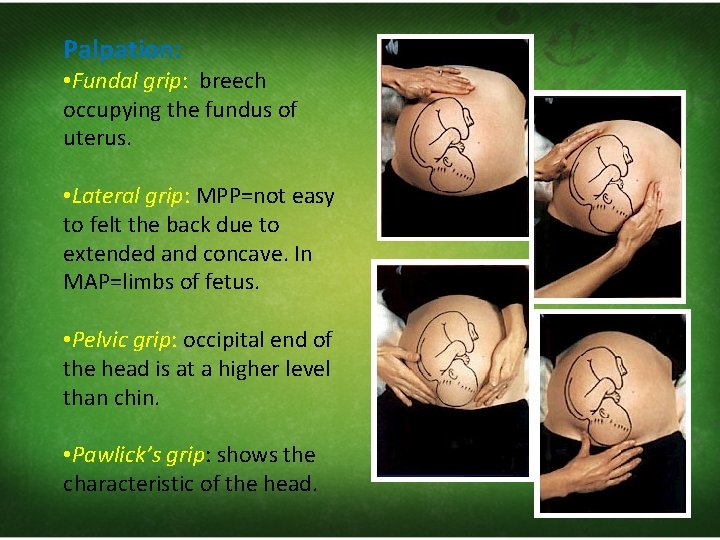
Palpation: • Fundal grip: breech occupying the fundus of uterus. • Lateral grip: MPP=not easy to felt the back due to extended and concave. In MAP=limbs of fetus. • Pelvic grip: occipital end of the head is at a higher level than chin. • Pawlick’s grip: shows the characteristic of the head.
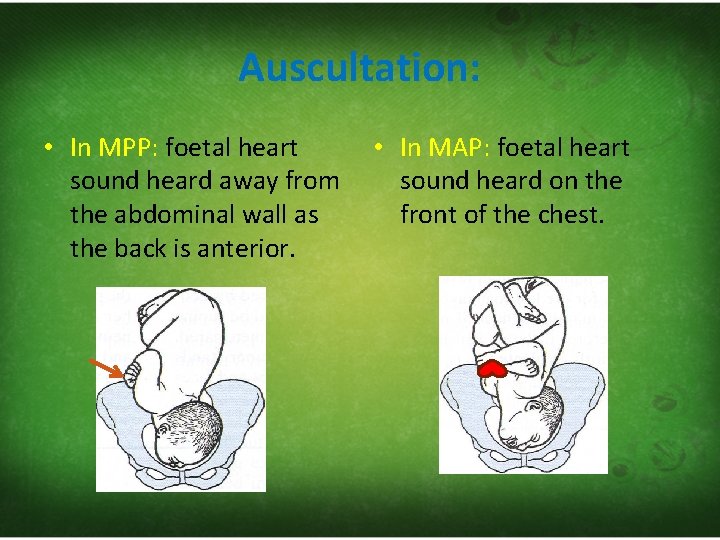
Auscultation: • In MPP: foetal heart sound heard away from the abdominal wall as the back is anterior. • In MAP: foetal heart sound heard on the front of the chest.
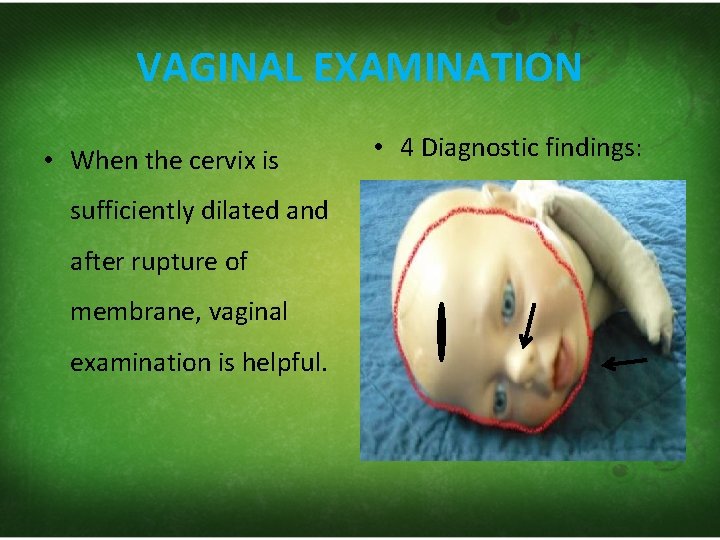
VAGINAL EXAMINATION • When the cervix is sufficiently dilated and after rupture of membrane, vaginal examination is helpful. • 4 Diagnostic findings:
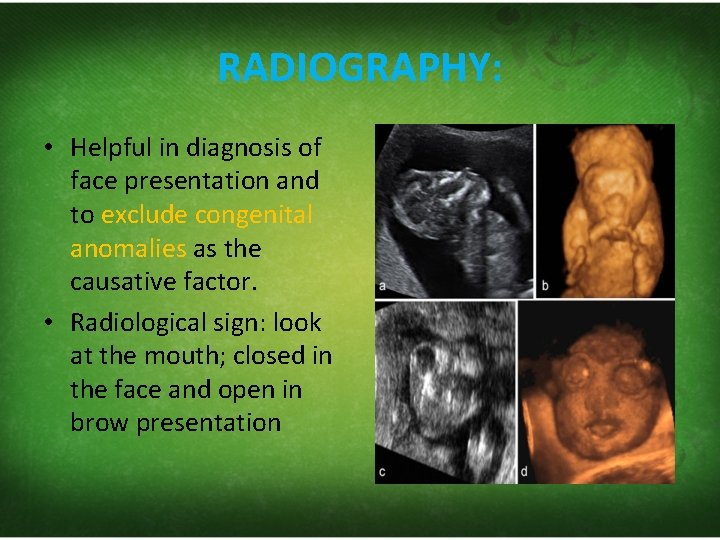
RADIOGRAPHY: • Helpful in diagnosis of face presentation and to exclude congenital anomalies as the causative factor. • Radiological sign: look at the mouth; closed in the face and open in brow presentation

MECHANISM OF LABOUR • Mento‐anterior position can be delivered vaginally. • Mento‐posterior position undeliverable cephalic presentation.
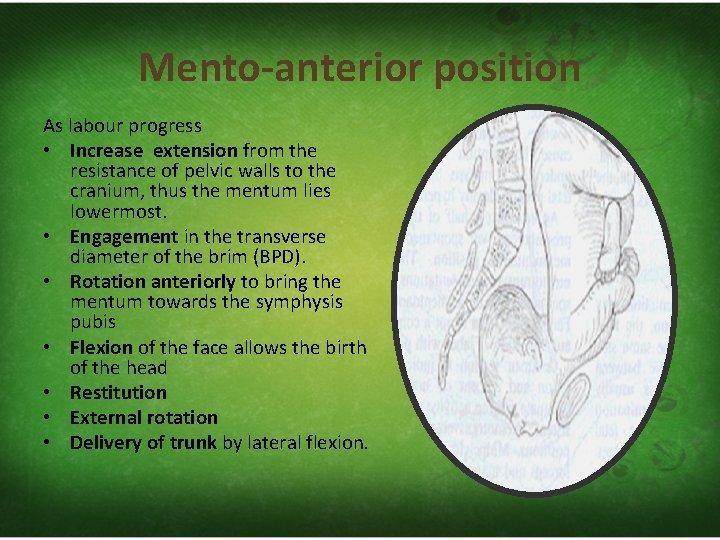
Mento-anterior position As labour progress • Increase extension from the resistance of pelvic walls to the cranium, thus the mentum lies lowermost. • Engagement in the transverse diameter of the brim (BPD). • Rotation anteriorly to bring the mentum towards the symphysis pubis • Flexion of the face allows the birth of the head • Restitution • External rotation • Delivery of trunk by lateral flexion.
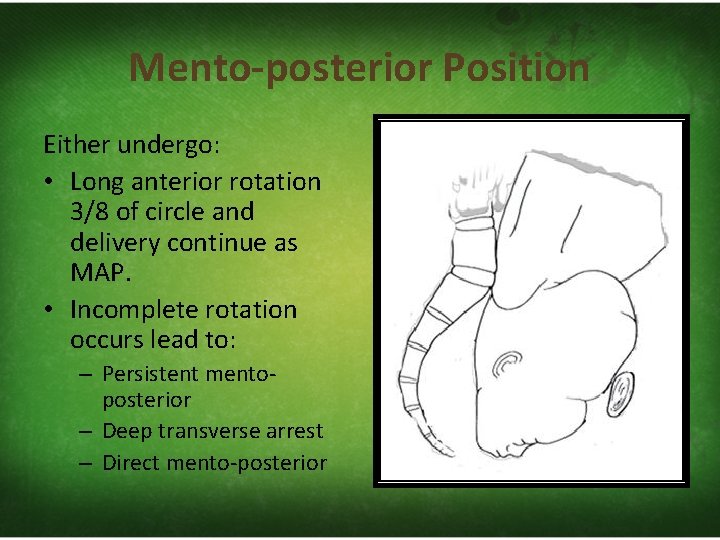
Mento-posterior Position Either undergo: • Long anterior rotation 3/8 of circle and delivery continue as MAP. • Incomplete rotation occurs lead to: – Persistent mento‐ posterior – Deep transverse arrest – Direct mento‐posterior
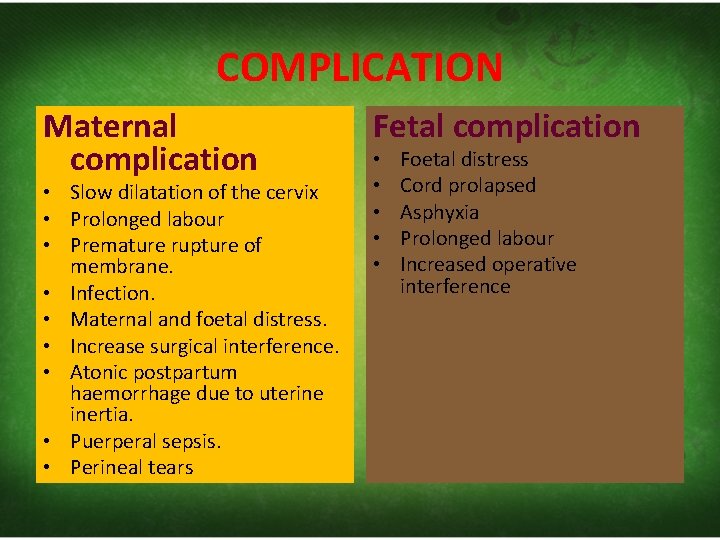
COMPLICATION Maternal complication • Slow dilatation of the cervix • Prolonged labour • Premature rupture of membrane. • Infection. • Maternal and foetal distress. • Increase surgical interference. • Atonic postpartum haemorrhage due to uterine inertia. • Puerperal sepsis. • Perineal tears Fetal complication • • • Foetal distress Cord prolapsed Asphyxia Prolonged labour Increased operative interference
MANAGEMENT In mento anterior position: • Labour is left to progress normally • If have foetal or maternal distress, use forceps or caesarean section. In mento-posterior position: • If the mentum not rotate anteriorly, we can do the followings: – Manual rotation to bring chin anteriorly and delivery by forceps or – Caesarean section
COMPLEX PRESENTATION
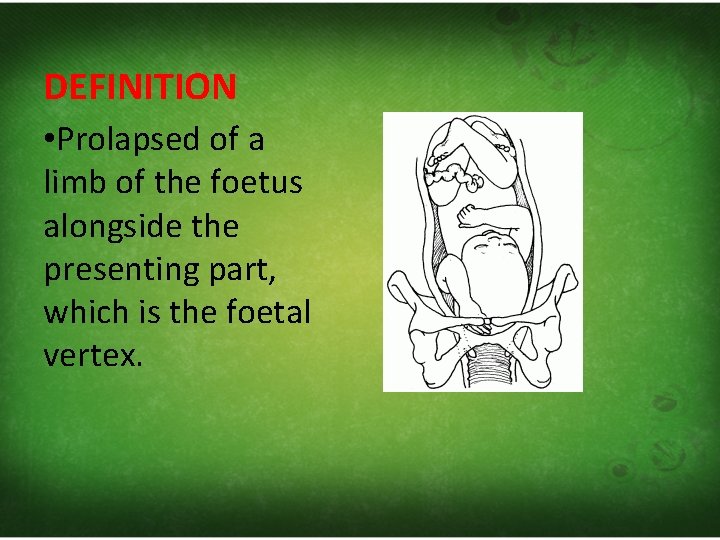
DEFINITION • Prolapsed of a limb of the foetus alongside the presenting part, which is the foetal vertex.
Aetiology: This event usually occur especially at the time of rupture membrane with sudden gush of liquor amnii especially in the following conditions: Cephalo‐pelvic disproportion Cephalic malpresentation; face and brow presentation Premature labour Multiple pregnancy Polyhydramnios Anencephaly and microcephaly
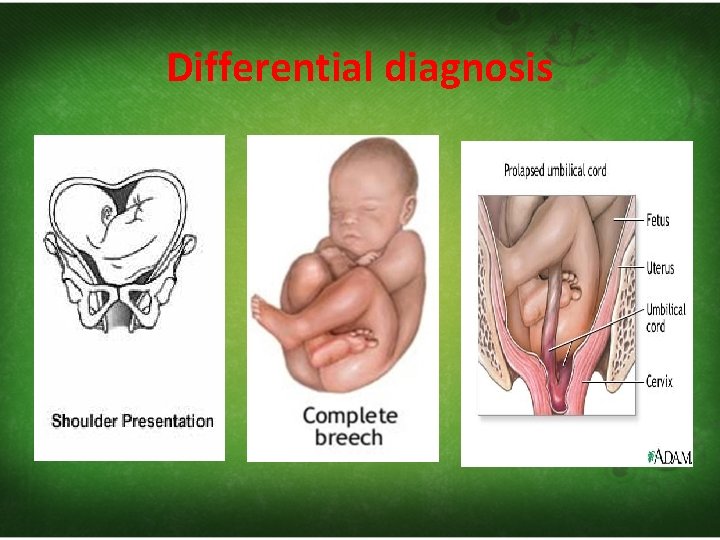
Differential diagnosis
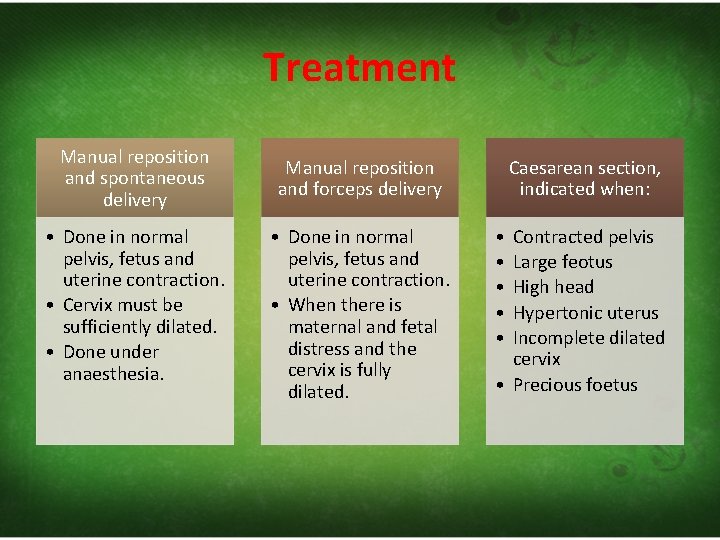
Treatment Manual reposition and spontaneous delivery Manual reposition and forceps delivery • Done in normal pelvis, fetus and uterine contraction. • Cervix must be sufficiently dilated. • Done under anaesthesia. • Done in normal pelvis, fetus and uterine contraction. • When there is maternal and fetal distress and the cervix is fully dilated. Caesarean section, indicated when: • • • Contracted pelvis Large feotus High head Hypertonic uterus Incomplete dilated cervix • Precious foetus

BREECH PRESENTATION
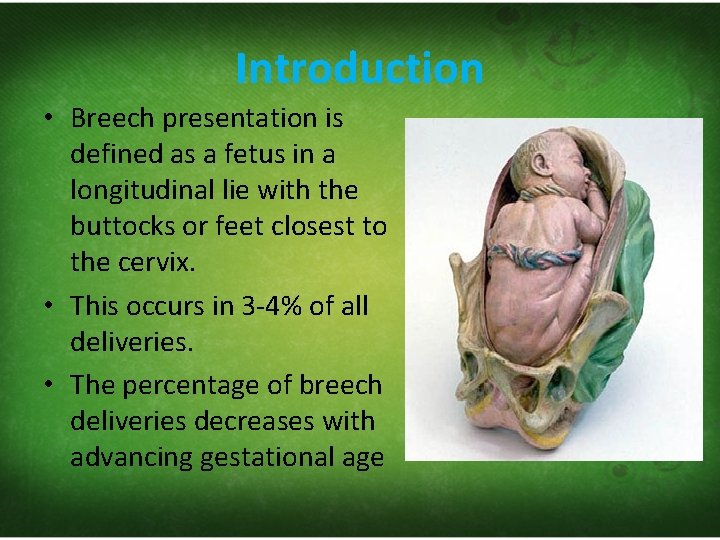
Introduction • Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. • This occurs in 3‐ 4% of all deliveries. • The percentage of breech deliveries decreases with advancing gestational age
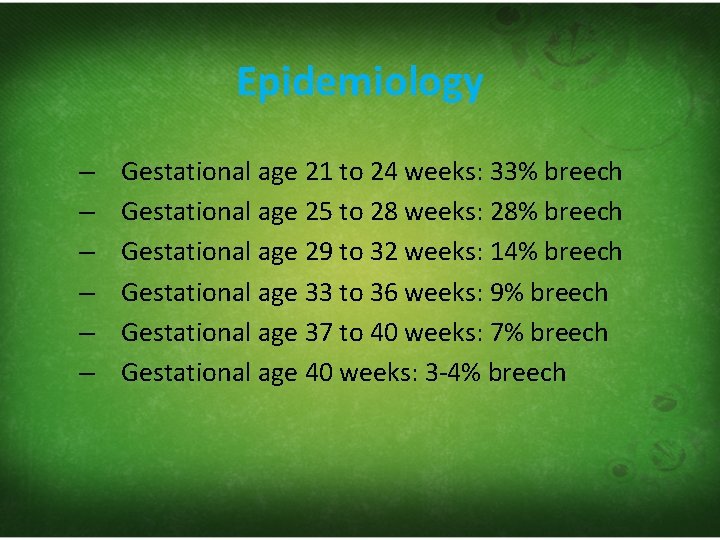
Epidemiology – – – Gestational age 21 to 24 weeks: 33% breech Gestational age 25 to 28 weeks: 28% breech Gestational age 29 to 32 weeks: 14% breech Gestational age 33 to 36 weeks: 9% breech Gestational age 37 to 40 weeks: 7% breech Gestational age 40 weeks: 3‐ 4% breech
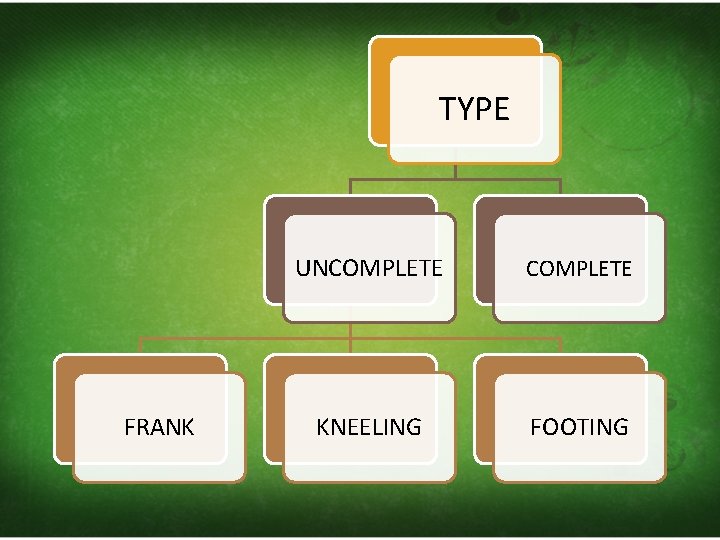
TYPE FRANK UNCOMPLETE KNEELING FOOTING
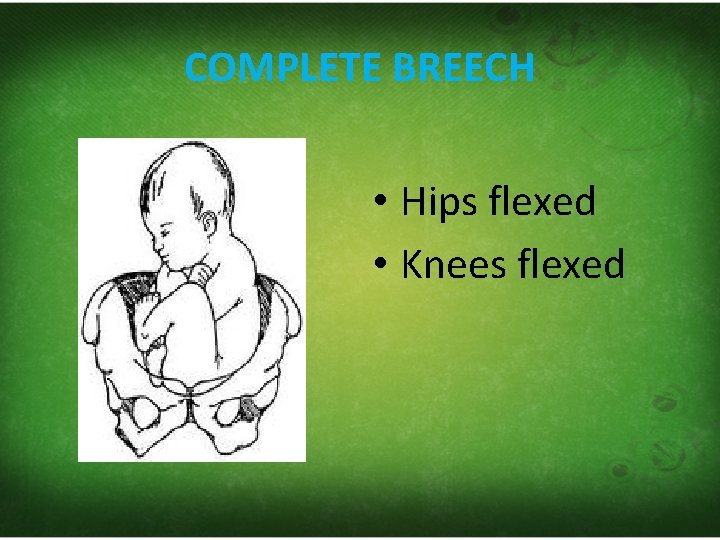
COMPLETE BREECH • Hips flexed • Knees flexed
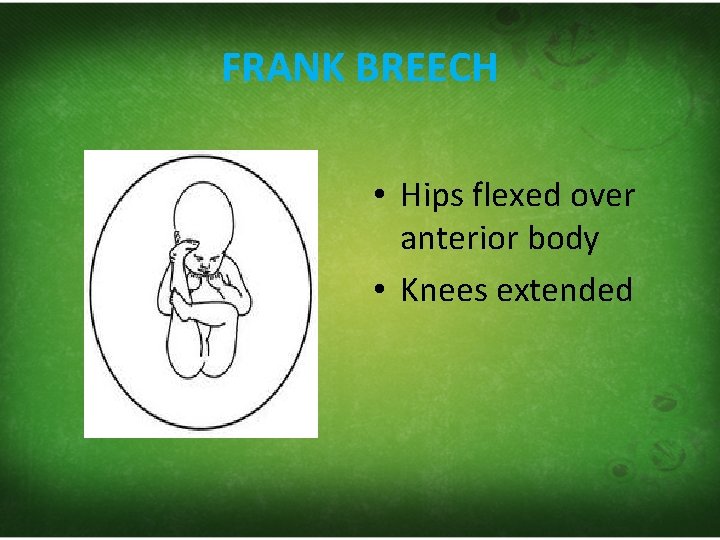
FRANK BREECH • Hips flexed over anterior body • Knees extended
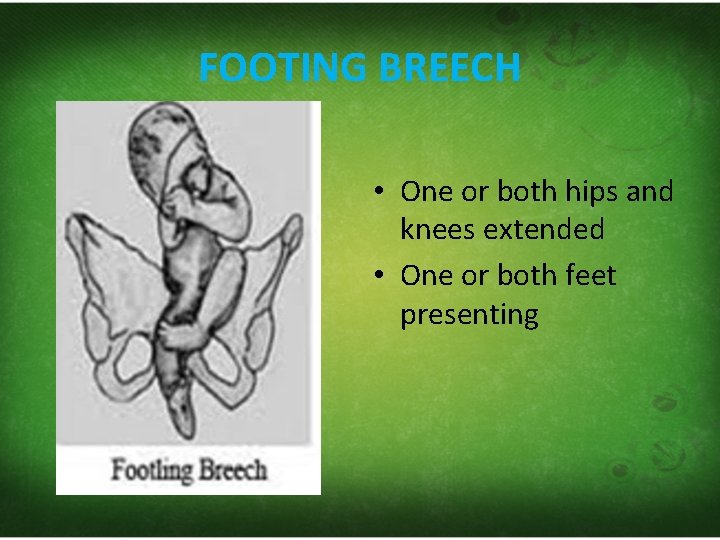
FOOTING BREECH • One or both hips and knees extended • One or both feet presenting

KNEELING BREECH • The thigh are extended • Legs are flexed on the thighs
Aetiology Maternal causes Foetal causes • Pelvic contraction • Congenital anomalies of the uterus • Pelvic tumor , either bony or soft tissue like fibroid or ovarian cysts • • Prematurity Multiple pregnancy Intra uterine fetal death Congenital anomalies particularly hydrocephalus • Placenta previa • polyhydramions
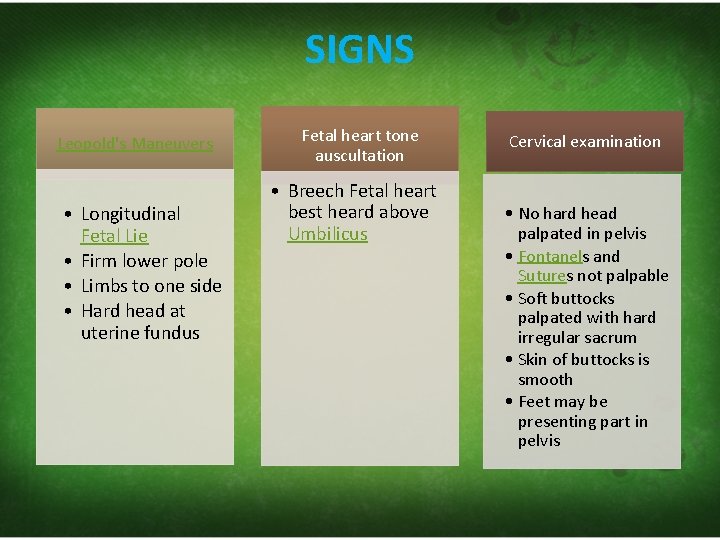
SIGNS Leopold's Maneuvers • Longitudinal Fetal Lie • Firm lower pole • Limbs to one side • Hard head at uterine fundus Fetal heart tone auscultation • Breech Fetal heart best heard above Umbilicus Cervical examination • No hard head palpated in pelvis • Fontanels and Sutures not palpable • Soft buttocks palpated with hard irregular sacrum • Skin of buttocks is smooth • Feet may be presenting part in pelvis
RADIOLOGY Obstetric Ultrasound
MANAGEMENT 1. General • Evaluate for cause in all breech presentation • Consider postural Exercises for patient – Technique 1: Knee chest » Knee‐chest position for 15 minutes » Repeat 3 times daily for 5 days » Consider pelvic rocking while performing – Technique 2: Deep trendelenburg position » Patient supine with hips elevated 9‐ 12 inches » Perform 10 minute, once to twice daily » Consider pelvic rocking while performing – Questionable efficacy but considered safe
2. Footling or Incomplete Breech • Cesarean Section 3. Frank or Complete Breech • Attempt External Cephalic Version • If external version fails – Cesarean section or – Breech Delivery 4. Complete Breech with foot protruding through cervix • Dangerous! (Very high risk) • Emergent Cesarean section
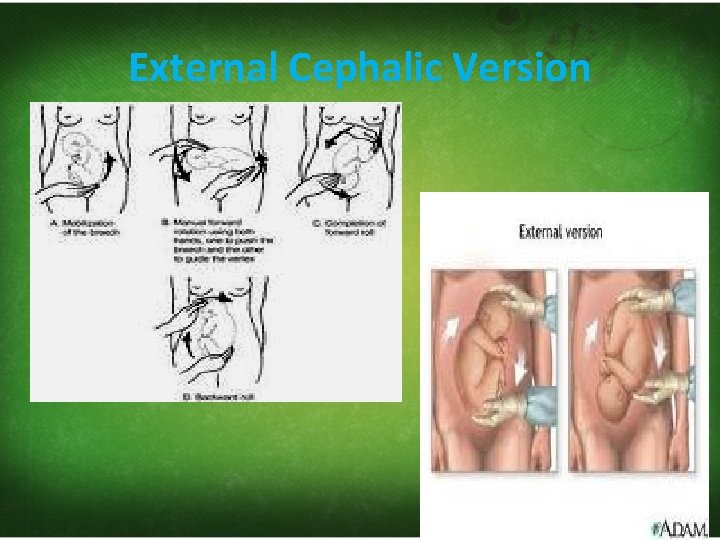
External Cephalic Version
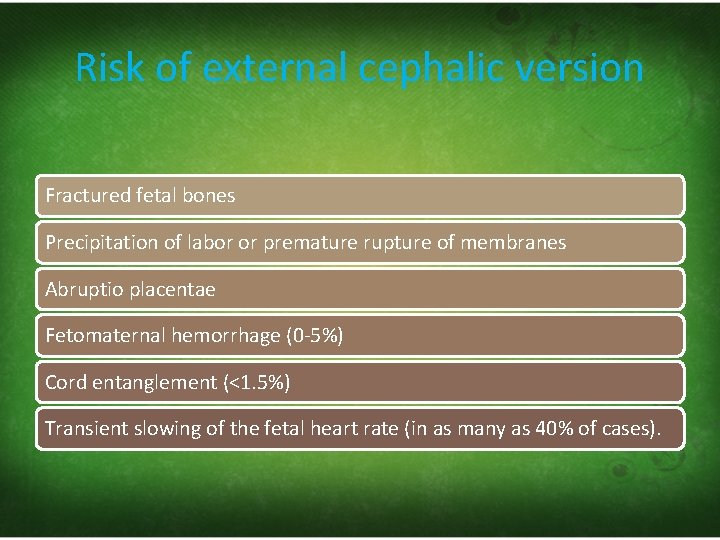
Risk of external cephalic version Fractured fetal bones Precipitation of labor or premature rupture of membranes Abruptio placentae Fetomaternal hemorrhage (0‐ 5%) Cord entanglement (<1. 5%) Transient slowing of the fetal heart rate (in as many as 40% of cases).
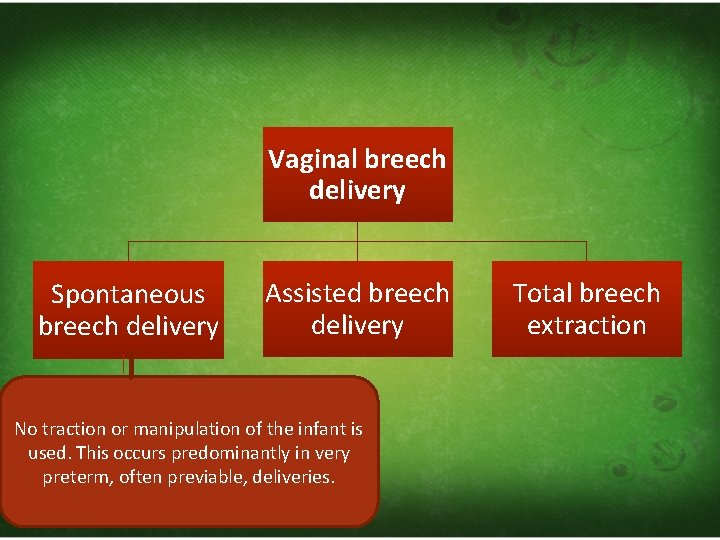
Vaginal breech delivery Spontaneous breech delivery Assisted breech delivery No traction or manipulation of the infant is used. This occurs predominantly in very preterm, often previable, deliveries. Total breech extraction
Total breech extraction • The fetal feet are grasped, • the entire fetus is extracted. • Total breech extraction should be used only for a noncephalic second twin; it should not be used for a singleton fetus because the cervix may not be adequately dilated to allow passage of the fetal head.
Assisted breech delivery • Thick meconium passage is common as the breech is squeezed through the birth canal. This is usually not associated with meconium aspiration because the meconium passes out of the vagina and does not mix with the amniotic fluid.

• The Ritgen maneuver is applied to take pressure off the perineum during vaginal delivery. Episiotomies are often performed for assisted vaginal breech deliveries, even in multiparous women, to prevent soft tissue dystocia.
• No downward or outward traction is applied to the fetus until the umbilicus has been reached.
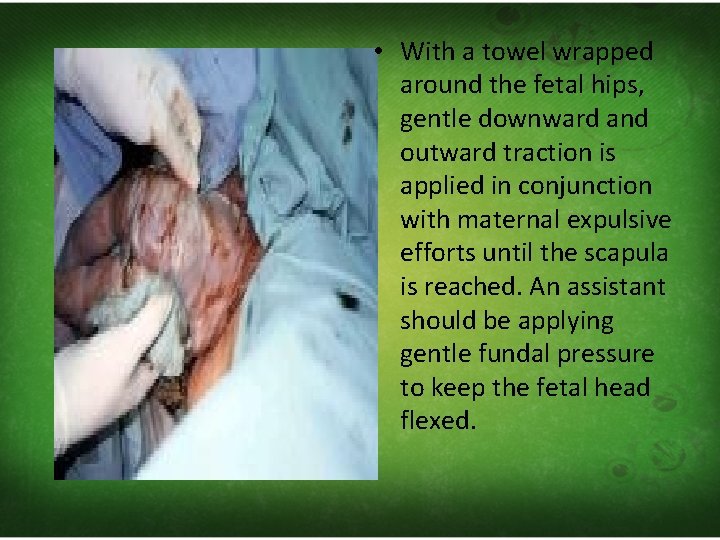
• With a towel wrapped around the fetal hips, gentle downward and outward traction is applied in conjunction with maternal expulsive efforts until the scapula is reached. An assistant should be applying gentle fundal pressure to keep the fetal head flexed.
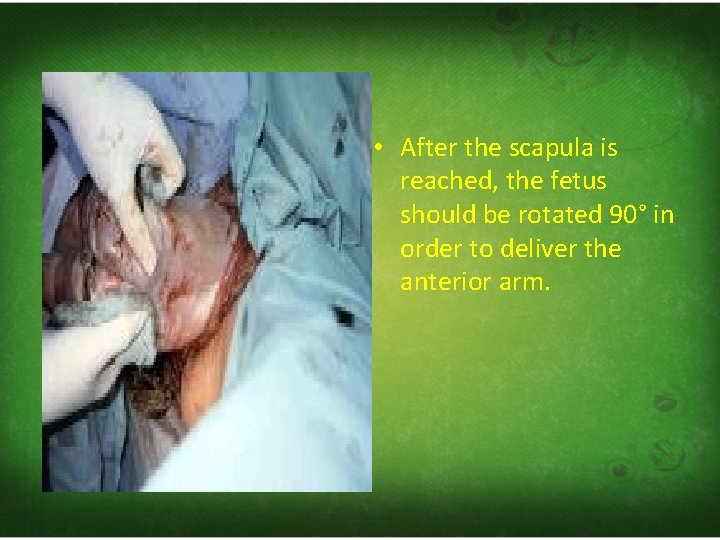
• After the scapula is reached, the fetus should be rotated 90° in order to deliver the anterior arm.
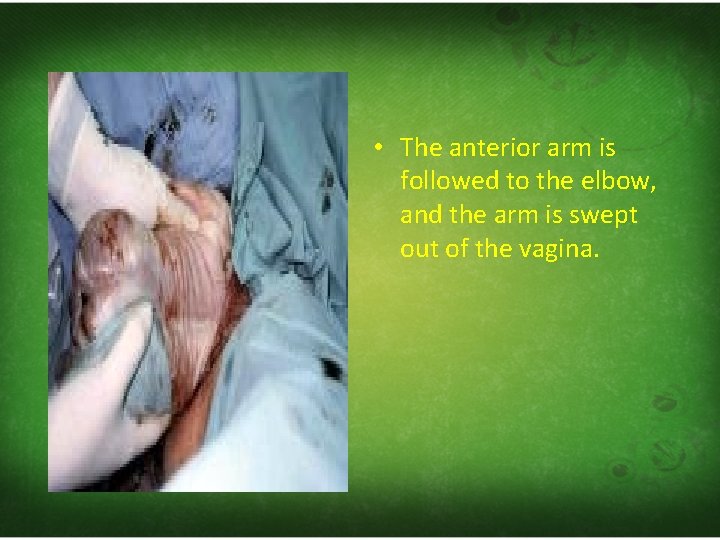
• The anterior arm is followed to the elbow, and the arm is swept out of the vagina.
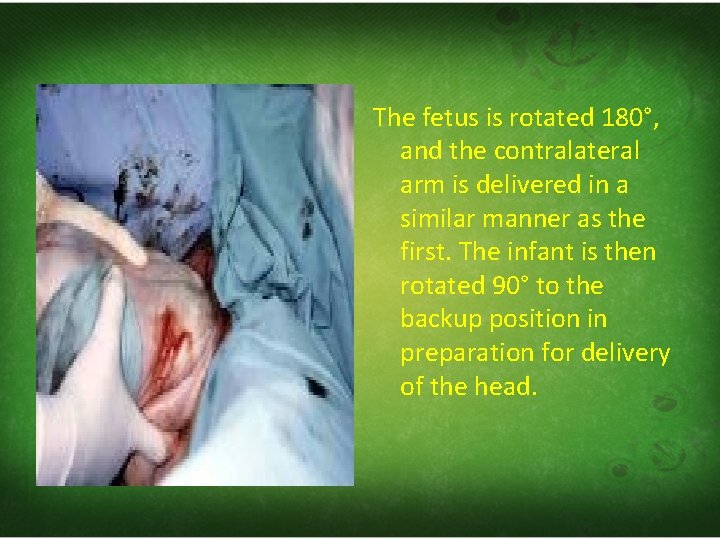
The fetus is rotated 180°, and the contralateral arm is delivered in a similar manner as the first. The infant is then rotated 90° to the backup position in preparation for delivery of the head.
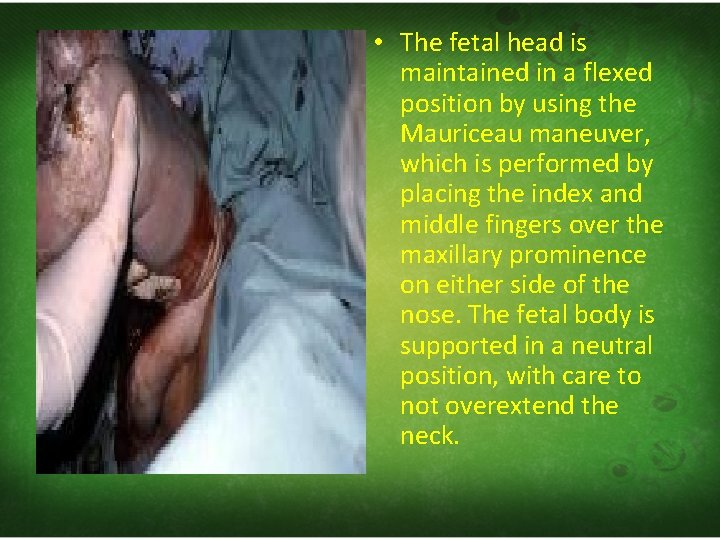
• The fetal head is maintained in a flexed position by using the Mauriceau maneuver, which is performed by placing the index and middle fingers over the maxillary prominence on either side of the nose. The fetal body is supported in a neutral position, with care to not overextend the neck.
Piper forceps application. Piper forceps are specialized forceps used only for the after‐coming head of a breech presentation. They are used to keep the fetal head flexed during extraction of the head. An assistant is needed to hold the infant while the operator gets on one knee to apply the forceps from below.

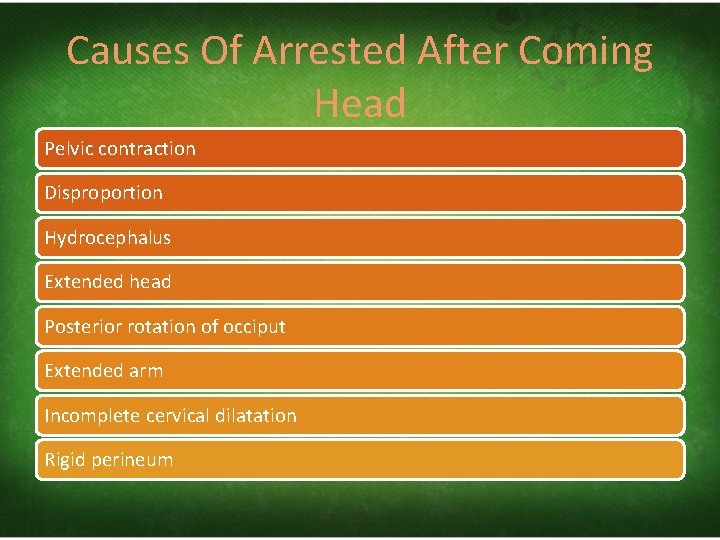
Causes Of Arrested After Coming Head Pelvic contraction Disproportion Hydrocephalus Extended head Posterior rotation of occiput Extended arm Incomplete cervical dilatation Rigid perineum
Obstruction in after coming head during vaginal delivery 1. Conservative methods, if fail 2. Symphysiotomy or 3. Caesarean section should be performed.
SHOULDER AND CORD PRESENTATION AND PROLAPSE
SHOULDER PRESENTATION
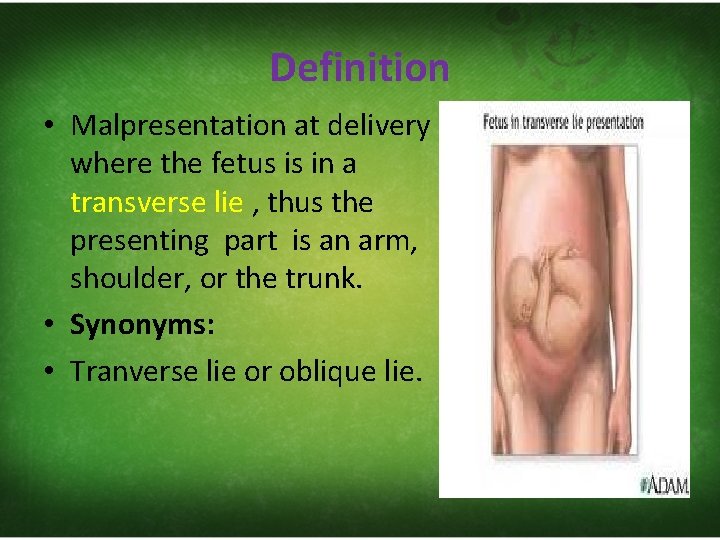
Definition • Malpresentation at delivery where the fetus is in a transverse lie , thus the presenting part is an arm, shoulder, or the trunk. • Synonyms: • Tranverse lie or oblique lie.
Aetilogy Maternal Grand multiparity Bony abnormalities of the pelvis Other pelvic mass uterine abnormalities : malformations or tumors (fibroids) • weak abdominal musculature, • uterine overdistension (i. e. polyhydramnion). • • •
• • Fetal small fetus congenital anomaly Placenta previa
Position • • • The denominator are the head and the back. Left dorso‐anterior (LDA)(first position) Right dorso‐anterior (RDA)(second position) Right dorso‐posterior (RDP)(third position) Left dorso‐posterior (LDP)(forth position)
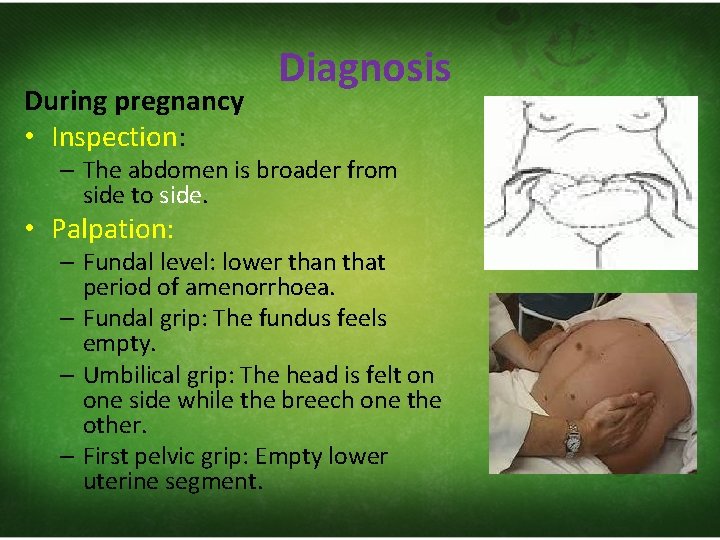
During pregnancy • Inspection: Diagnosis – The abdomen is broader from side to side. • Palpation: – Fundal level: lower than that period of amenorrhoea. – Fundal grip: The fundus feels empty. – Umbilical grip: The head is felt on one side while the breech one the other. – First pelvic grip: Empty lower uterine segment.
• Auscultation: – FHS are best heard on one side of the umbilicus towards the foetal head. • Ultrasound or X‐ray: – Confirms the diagnosis and may identify the cause as multiple pregnancy or placenta praevia.
During labour Vaginal examination reveals: • The presenting part is high. • Membranes are bulging. • Premature rupture of membranes. • When the cervix is sufficiently dilated particularly after rupture of the membranes : scapula, acromion, clavicle, ribs or axilla can be felt.
Mechanism of Labour • As a rule: • no mechanism of labour should be anticipated. • Undeliverable
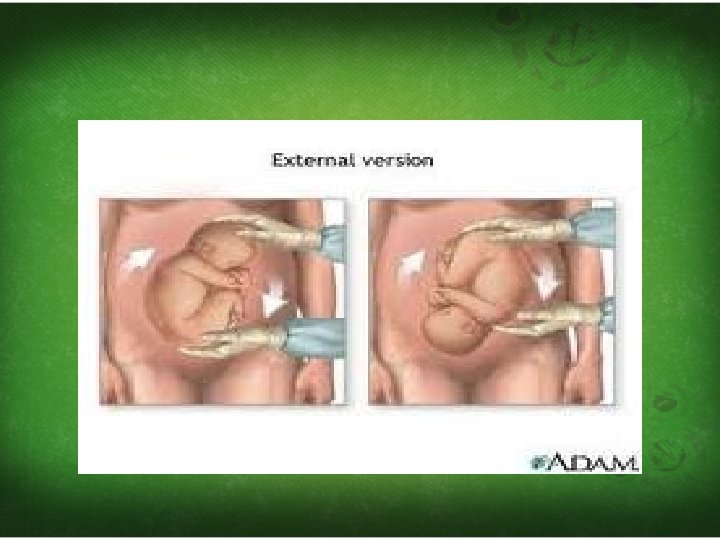
Management • During pregnancy • External cephalic version. • External podalic version can be try. • In early labour, if version succeeded apply abdominal binder and rupture the membranes as if there are uterine contractions.
• During labour: • With intact membranes: • Keep the membrane intact for as long as possible by raising the root of the bed and avoid repeated vaginal examination • close observation and immediate vaginal examination once the membranes is rupture.
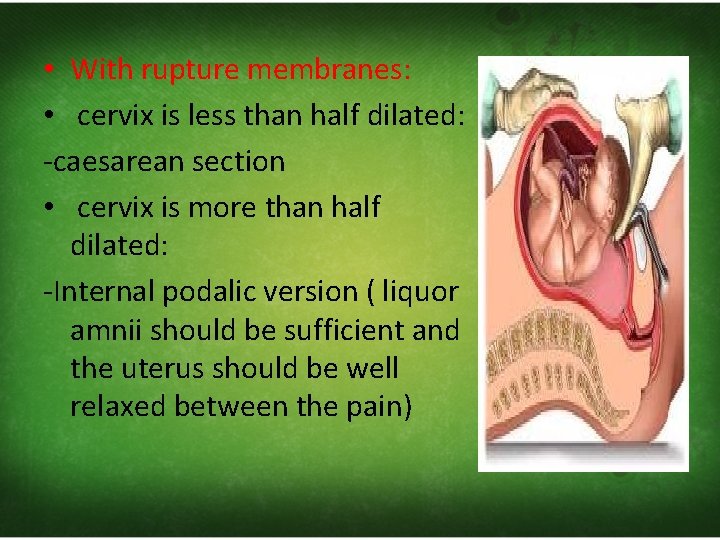
• With rupture membranes: • cervix is less than half dilated: ‐caesarean section • cervix is more than half dilated: ‐Internal podalic version ( liquor amnii should be sufficient and the uterus should be well relaxed between the pain)
Neglected (Impacted) shoulder: • Definition: • Undiagnosed shoulder presentation until labour is advanced and became obstructed.
Clinical picture (impending rupture uterus): v. Exhaustion and distress of the mother and showing sign of obstructed labour : • tachycardia • raised temperature • dry tongue • complain of pain and tenderness over the lower part of uterus.
v. Shoulder is impacted may be with prolapsed arm and / or cord. v. Membranes are already ruptured. v. Liquor is drained. v. The uterus is tonically contracted and shows bandl’s ring. v. The foetus is severely distressed or dead. v. The vagina is hot and dry and the cervical lips are edematous.
Prognosis: • Fetal death is usually the rule. • Rupture uterus is easy to happen either spontaneous or traumatic.
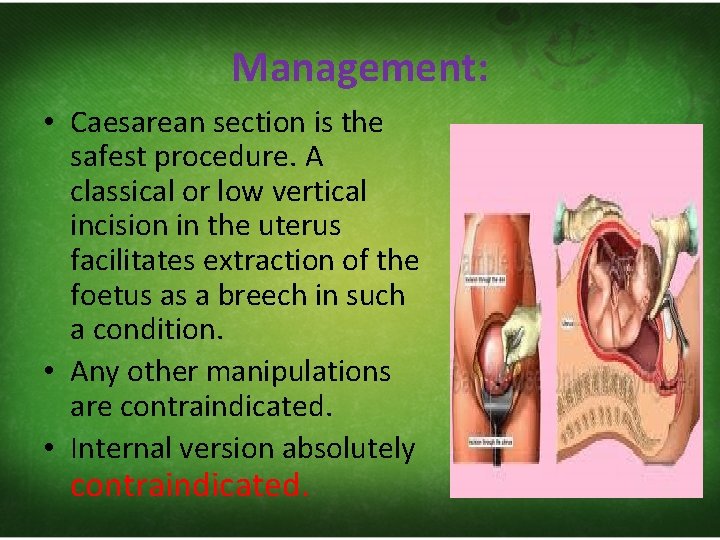
Management: • Caesarean section is the safest procedure. A classical or low vertical incision in the uterus facilitates extraction of the foetus as a breech in such a condition. • Any other manipulations are contraindicated. • Internal version absolutely contraindicated.
CORD PRESENTATION AND PROLAPSED
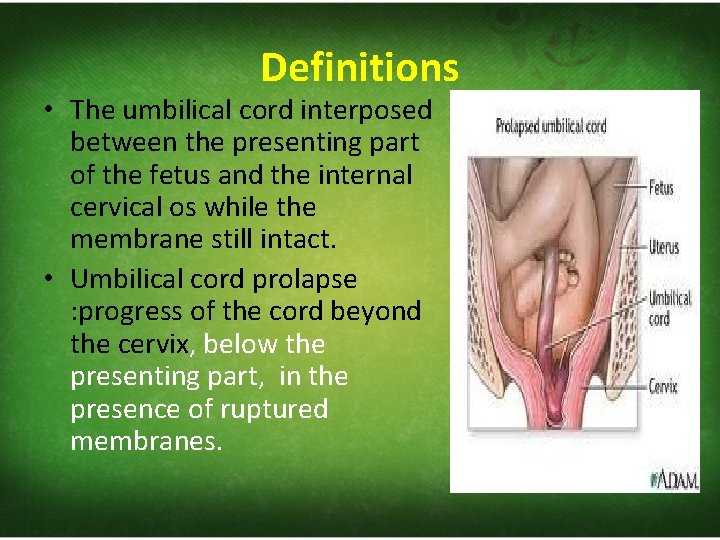
Definitions • The umbilical cord interposed between the presenting part of the fetus and the internal cervical os while the membrane still intact. • Umbilical cord prolapse : progress of the cord beyond the cervix, below the presenting part, in the presence of ruptured membranes.
Etiology Abnormal cephalic presentation Breech presentation and transverse lie long umbilical cord Polyhydramnios Prematurity Unengaged presenting part
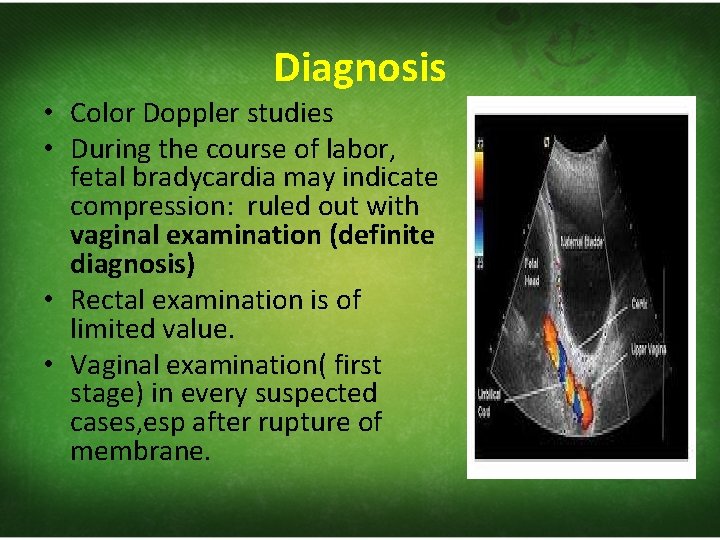
Diagnosis • Color Doppler studies • During the course of labor, fetal bradycardia may indicate compression: ruled out with vaginal examination (definite diagnosis) • Rectal examination is of limited value. • Vaginal examination( first stage) in every suspected cases, esp after rupture of membrane.
Differential diagnosis • Nothing can be mistaken for the pulsating cord. • If the cord is not pulsating, the fetal toe or finger may stimulate it
Prognosis • Maternal: no added dangers. • Fetal: in the presentation ( danger is minimal ): needed to interfere quickly before the cord became prolapsed. Which have a grave effect.
• If pulsation is not felt, it does not always mean that the feotus is dead, it can be cause by uterine contraction and it will recur again. • 8 minutes window period • Cord prolapsed with cephalic presentation is more dangerous than others.
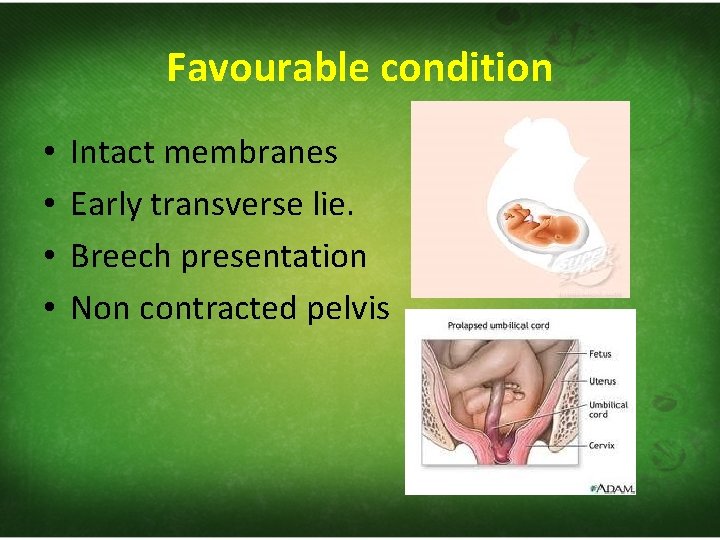
Favourable condition • • Intact membranes Early transverse lie. Breech presentation Non contracted pelvis
Management • If the feotus is dead , there is nothing need to be done for the prolapsed cord itself. • If the feotus is alive, some measures can be done according to the situation:
Deliver as Intrauterine Fetal demise if fetus has died • Check for cord pulsations • Check for fetal heart sounds • Obstetric Ultrasound to assess heart activity
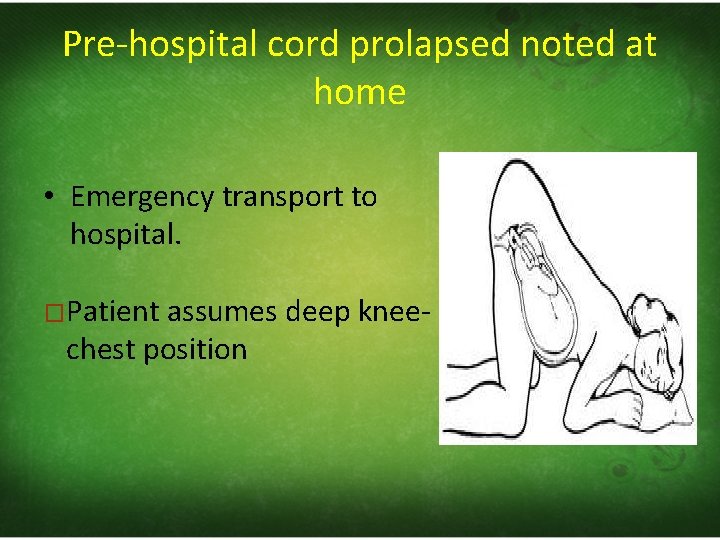
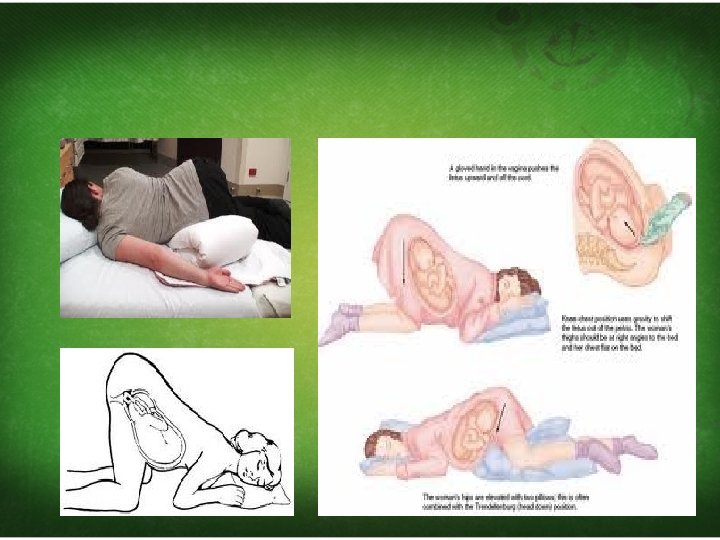
Pre‐hospital cord prolapsed noted at home • Emergency transport to hospital. �Patient assumes deep knee‐ chest position
Temporally measures to relieve cord pressure – Tocolysis with Terbutaline 0. 25 mg SC – Manual reposition of the cord back into vagina and maintain with gauze pack( cervix is already fully dilated. ) – Vaginal retrograde pressure applied to presenting part • Hand in vagina elevates presenting part – Consider filling bladder with 500‐ 700 cc Saline
– Minimize handling of the cord – Adjust maternal position to reduce cord pressure. • Raise foot of the bed (Trendelenburg's Position) • Sims' position – left lateral decubitus position • Genu‐pectoral position – knee‐chest position
• Keep the membrane intact until the cervix is fully dilated. • After fully dilated cervix : artificial rupture of the membrane and immediate extraction of the feotus by forceps or internal podalic version and breech extraction.
Complication • Fetal distress • Fetal anoxia • Fetal death • Emergency operative intervention

THANK YOU
- Slides: 121