Abnormal agranular granulocytes may be confused with monocytes
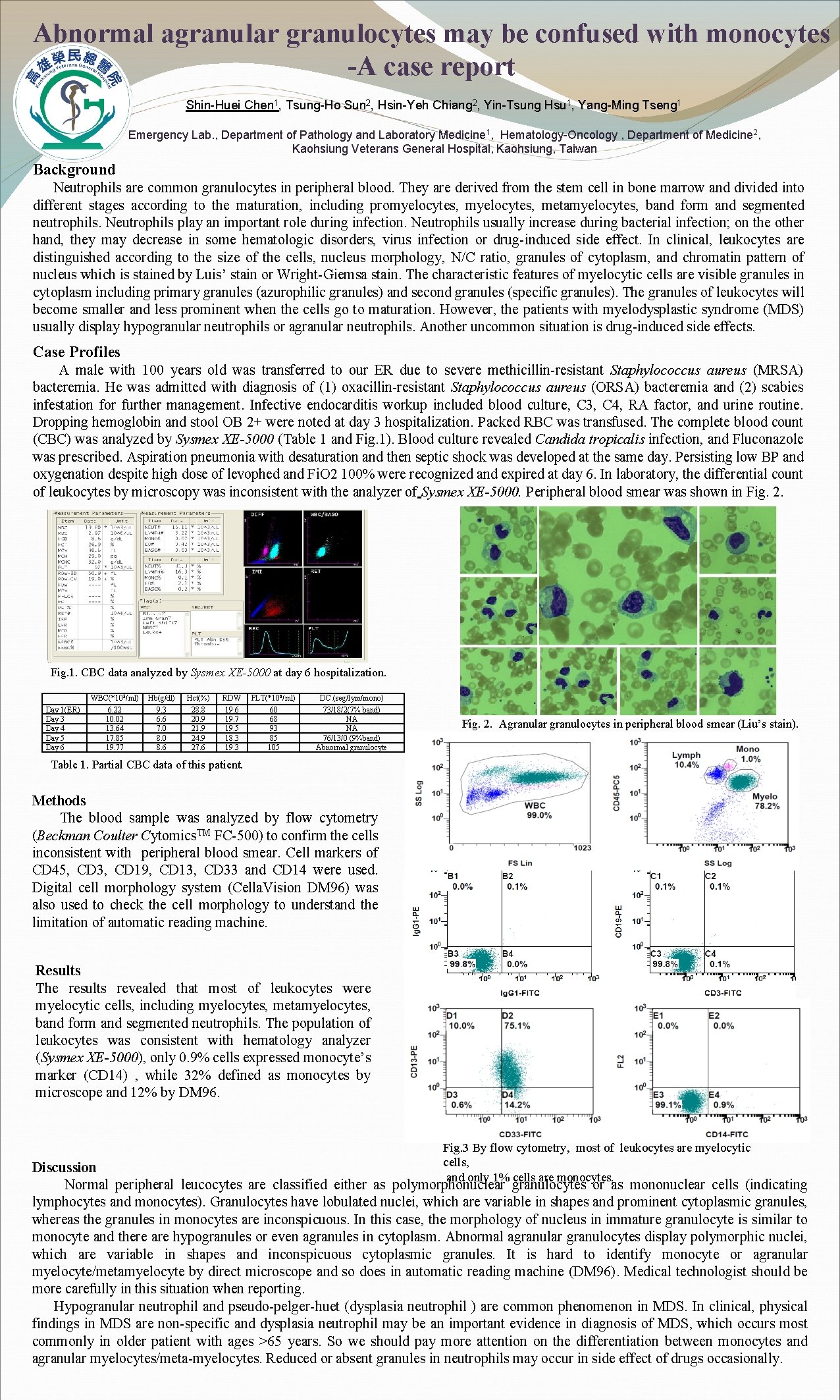
Abnormal agranular granulocytes may be confused with monocytes -A case report Shin-Huei Chen 1, Tsung-Ho Sun 2, Hsin-Yeh Chiang 2, Yin-Tsung Hsu 1, Yang-Ming Tseng 1 Emergency Lab. , Department of Pathology and Laboratory Medicine 1, Hematology-Oncology , Department of Medicine 2, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan Background Neutrophils are common granulocytes in peripheral blood. They are derived from the stem cell in bone marrow and divided into different stages according to the maturation, including promyelocytes, metamyelocytes, band form and segmented neutrophils. Neutrophils play an important role during infection. Neutrophils usually increase during bacterial infection; on the other hand, they may decrease in some hematologic disorders, virus infection or drug-induced side effect. In clinical, leukocytes are distinguished according to the size of the cells, nucleus morphology, N/C ratio, granules of cytoplasm, and chromatin pattern of nucleus which is stained by Luis’ stain or Wright-Giemsa stain. The characteristic features of myelocytic cells are visible granules in cytoplasm including primary granules (azurophilic granules) and second granules (specific granules). The granules of leukocytes will become smaller and less prominent when the cells go to maturation. However, the patients with myelodysplastic syndrome (MDS) usually display hypogranular neutrophils or agranular neutrophils. Another uncommon situation is drug-induced side effects. Case Profiles A male with 100 years old was transferred to our ER due to severe methicillin-resistant Staphylococcus aureus (MRSA) bacteremia. He was admitted with diagnosis of (1) oxacillin-resistant Staphylococcus aureus (ORSA) bacteremia and (2) scabies infestation for further management. Infective endocarditis workup included blood culture, C 3, C 4, RA factor, and urine routine. Dropping hemoglobin and stool OB 2+ were noted at day 3 hospitalization. Packed RBC was transfused. The complete blood count (CBC) was analyzed by Sysmex XE-5000 (Table 1 and Fig. 1). Blood culture revealed Candida tropicalis infection, and Fluconazole was prescribed. Aspiration pneumonia with desaturation and then septic shock was developed at the same day. Persisting low BP and oxygenation despite high dose of levophed and Fi. O 2 100% were recognized and expired at day 6. In laboratory, the differential count of leukocytes by microscopy was inconsistent with the analyzer of Sysmex XE-5000. Peripheral blood smear was shown in Fig. 2. Fig. 1. CBC data analyzed by Sysmex XE-5000 at day 6 hospitalization. Day 1(ER) Day 3 Day 4 Day 5 Day 6 WBC(*103/ml) 6. 22 10. 02 13. 64 17. 85 19. 77 Hb(g/dl) 9. 3 6. 6 7. 0 8. 6 Hct(%) 28. 8 20. 9 21. 9 24. 9 27. 6 RDW 19. 6 19. 7 19. 5 18. 3 19. 3 PLT(*106/ml) 60 68 93 85 105 DC. (seg/lym/mono) 73/18/2(7% band) NA NA 76/13/0 (9%band) Abnormal granulocyte Fig. 2. Agranular granulocytes in peripheral blood smear (Liu’s stain). Table 1. Partial CBC data of this patient. Methods The blood sample was analyzed by flow cytometry (Beckman Coulter Cytomics. TM FC-500) to confirm the cells inconsistent with peripheral blood smear. Cell markers of CD 45, CD 3, CD 19, CD 13, CD 33 and CD 14 were used. Digital cell morphology system (Cella. Vision DM 96) was also used to check the cell morphology to understand the limitation of automatic reading machine. Results The results revealed that most of leukocytes were myelocytic cells, including myelocytes, metamyelocytes, band form and segmented neutrophils. The population of leukocytes was consistent with hematology analyzer (Sysmex XE-5000), only 0. 9% cells expressed monocyte’s marker (CD 14) , while 32% defined as monocytes by microscope and 12% by DM 96. Fig. 3 By flow cytometry, most of leukocytes are myelocytic cells, and only 1% cells are monocytes. Discussion Normal peripheral leucocytes are classified either as polymorphonuclear granulocytes or as mononuclear cells (indicating lymphocytes and monocytes). Granulocytes have lobulated nuclei, which are variable in shapes and prominent cytoplasmic granules, whereas the granules in monocytes are inconspicuous. In this case, the morphology of nucleus in immature granulocyte is similar to monocyte and there are hypogranules or even agranules in cytoplasm. Abnormal agranular granulocytes display polymorphic nuclei, which are variable in shapes and inconspicuous cytoplasmic granules. It is hard to identify monocyte or agranular myelocyte/metamyelocyte by direct microscope and so does in automatic reading machine (DM 96). Medical technologist should be more carefully in this situation when reporting. Hypogranular neutrophil and pseudo-pelger-huet (dysplasia neutrophil ) are common phenomenon in MDS. In clinical, physical findings in MDS are non-specific and dysplasia neutrophil may be an important evidence in diagnosis of MDS, which occurs most commonly in older patient with ages >65 years. So we should pay more attention on the differentiation between monocytes and agranular myelocytes/meta-myelocytes. Reduced or absent granules in neutrophils may occur in side effect of drugs occasionally.
- Slides: 1