Abdominal Wall Pain An Overlooked Source of Unexplained
Abdominal Wall Pain: An Overlooked Source of Unexplained Chronic Abdominal Pain October 12 th, 2018 Donna Hoffman M. D
The Problem: 1) Chronic abdominal pain is prevalent: Up to 30% attributed to abdominal wall pain. (1) 2) Chronic abdominal pain is expensive: The cost of workup before diagnosing AWP can reach over $6000. 00 per patient. (2) 3) Chronic abdominal pain creates significant suffering and disability for patients. 4) Chronic abdominal pain can be time consuming and frustrating for providers. 1 - Srinivasan R et al. Am J Gastroenterol. 2002; 97: 824 -830 2 - Greenbaum D et al. Dig Dis Sci. 1994; 39: 1935 -1941.
“Diagnosis of Abdominal Wall Pain ( AWP) has been shown to reduce physician and emergency visits, radiologic examinations and overall costs. ” Costanza CD, et al. Clin Gastroenterol Hepatol. 2004; 2: 395 -399
Test Question #1 True or False When preforming the Carnett’s test, the supine patient is asked to raise their head while the medical provider is palpating a tender area on the abdomen. If the pain is increased, the pain is likely visceral in origin.
Test Question #2 True or False Trigger point formation is due to inadequate release of acetylcholine from the nerve terminal of the motor end plate related to trauma or abnormal stress to the muscle.
Case: 21 Year Old Female – H. G – 21 year old female with 2 year h/o of peri- umbilical pain – Pain is constant, at time dull, sharp and or cramping – Pain is worse with exercise, standing, bending, eating – Can be associated with nausea and diarrhea – Evaluation prior to our visit: – Abdominal U/S, CT of abdomen and pelvis, MRCP, Chest CT, HIDA, EGD x 2 (mild gastritis), Colonoscopy, MRI enterography, transvaginal U/S. Normal labs – She is s/p cholecystectomy, appendectomy and diagnostic laparoscopic evaluation WHAT NEXT?
Differential Diagnosis of Abdominal Wall Pain – Anterior Cutaneous Nerve Entrapment – Abdominal Myofascial Pain Syndrome (AMPS) – Hernias – Hematomas – Neuromas from scars – Endometriosis in the abdominal wall – Intra- abdominal adhesions – Rib- tip or slipped rib syndrome
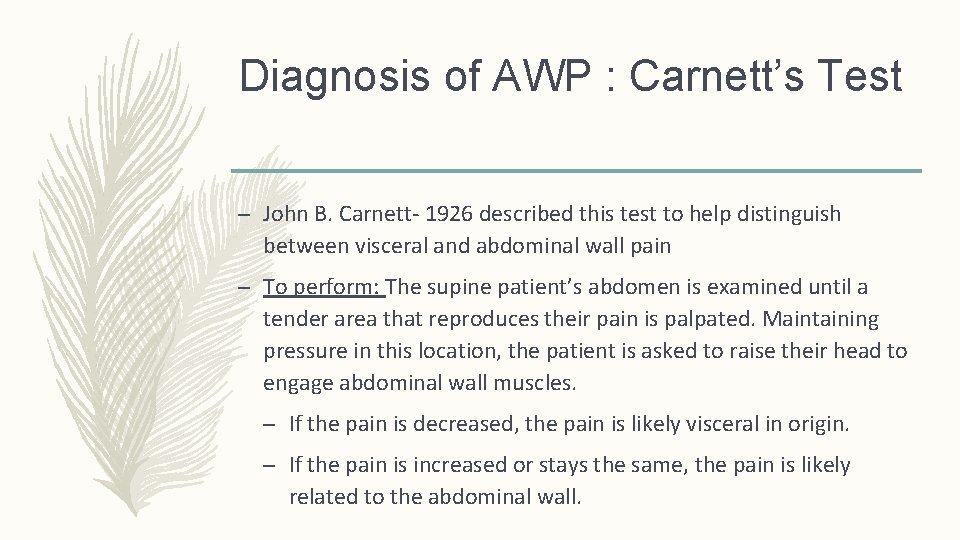
Diagnosis of AWP : Carnett’s Test – John B. Carnett- 1926 described this test to help distinguish between visceral and abdominal wall pain – To perform: The supine patient’s abdomen is examined until a tender area that reproduces their pain is palpated. Maintaining pressure in this location, the patient is asked to raise their head to engage abdominal wall muscles. – If the pain is decreased, the pain is likely visceral in origin. – If the pain is increased or stays the same, the pain is likely related to the abdominal wall.
Validity of Carnett’s Test – In 1977, Thompson and Francis investigated the utility of Carnett's sign in the evaluation of 120 patients seen in the emergency department for acute abdominal pain. – Only one of 24 patients with a positive Carnett's sign had visceral pathology on follow-up, whereas – All 96 patients with a negative Carnett's sign had visceral pathology on further testing. Thomson H. Lancet 1977; 2: 1053 -1054
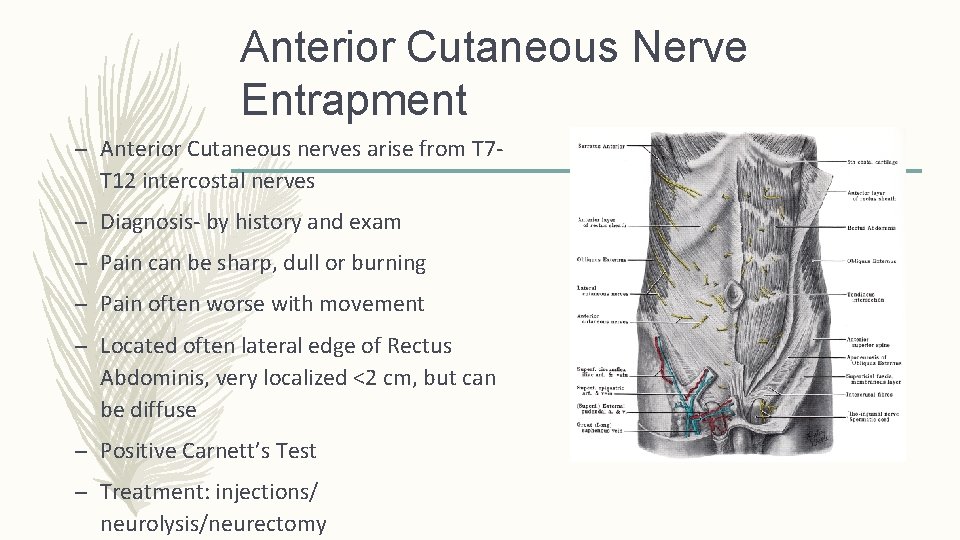
Anterior Cutaneous Nerve Entrapment – Anterior Cutaneous nerves arise from T 7 T 12 intercostal nerves – Diagnosis- by history and exam – Pain can be sharp, dull or burning – Pain often worse with movement – Located often lateral edge of Rectus Abdominis, very localized <2 cm, but can be diffuse – Positive Carnett’s Test – Treatment: injections/ neurolysis/neurectomy
Abdominal Myofascial Pain Syndrome – Pain attributed to trigger points in the abdominal wall muscles and or fascia – Diagnosis by history and exam – Pain can be sharp, dull or burning – Pain often worse with movement – Pain can be localized to an area less than 2 cm or diffuse – Positive Carnett’s Test – Treatment : Trigger Point Injections
AWP Treatment: Trigger Point Injection Efficacy – Review article quoted in Up to Date on Anterior Cutaneous Nerve Entrapment: – Injection of only local anesthetic: 83 - 91% saw immediate improvement in the pain, but pain returned in most in 2 -3 hours. – Long-term pain relief ensued after a single lidocaine injection in 2030% of patients – After repeated injections, long term relief in 40 -50% – After combined lidocaine and steroid injections in up to 80% Koop H. Chronic Abdominal Wall Pain. Dtsch Arztebl Int. 2016 Jan; 113(4): 51 -7
Nazareno et al: Long Term Follow Up of Trigger Point Injections For AWP – Criteria for AWP: 1) Localized pain 2) Point tenderness to palpation of less than 2. 5 cm 3) Positive Carnett’s test – 89 patients that met this criteria – Presence of GI Symptoms included: nausea, vomiting, hematemesis, dysphagia, odynophagia, heartburn, regurgitation, constipation, diarrhea, blood from rectum, tenesmus Nazareno J et al. Long- term follow up of trigger point injections for Abdominal wall pain. Can J Gastroentero. 2005 Sept; 19(9): 561 -5
Nazareno et al: Long Term Follow Up of Trigger Point Injections for AWP – Most common location of pain: 30% RUQ, 25% RLQ, 19% epigastric – 50% had some radiation of the pain – 73% had some GI Symptoms present, 39% had a scar in the vicinity – 88% injections were local anesthetic plus steroid – 12% anesthetic alone Nazareno J et al. Long- term follow up of trigger point injections for Abdominal wall pain. Can J Gastroentero. 2005 Sept; 19(9): 561 -5
Nazareno et al: Long Term Follow Up of Trigger Point Injections for AWP – Results: – Those that met criteria for AWP: 77% had some or complete relief – Those that did not meet criteria: 35% had some or complete relief – Without GI symptoms: 95% had some or complete relief – With GI symptoms: 71% had some or complete relief – This study found adding the steroid did not alter the amount of relief obtained. Nazareno J et al. Long- term follow up of trigger point injections for Abdominal wall pain. Can J Gastroentero. 2005 Sept; 19(9): 561 -5
Additional Studies On Abdominal Wall Trigger Point Injections – Niraj G- anesthetic with steroids provided relief at 6 months in 32%, did not study injection without steroid – Kuan LC- anesthetic with steroids 86. 5% had pain relief at 3 months – Alnahhas M- U/S guided injections at Mayo in Rochester 60% had some early improvement, at 3 months about 50%. Niraj G. Pain Med. 2018 Feb 9 (Epub ahead of print) Kuan LC. Efficany of treating Abdominal wall pain by local injection. Taiwan J Obstet Gyn. 2006 Sep; 45(3): 239 -43 Alnahhas M. Outcomes of Ultrasound –Guided Trigger Point Injection for Abdominal Wall Pain. Dig Dis Sci. 2016 61572 -577
Why The Large Variability In Response to Trigger Point Injections? Perpetuating Factors that contribute to the formation of and maintenance of trigger points/ myofascial pain
Perpetuating Factors- That Maintain AMPS 1) Mechanical Factors 2) Visceral Disease via Viscerosomatic convergence/ referred pain 3) Stress/ Behavioral Health Issues 4) Systemic Factors
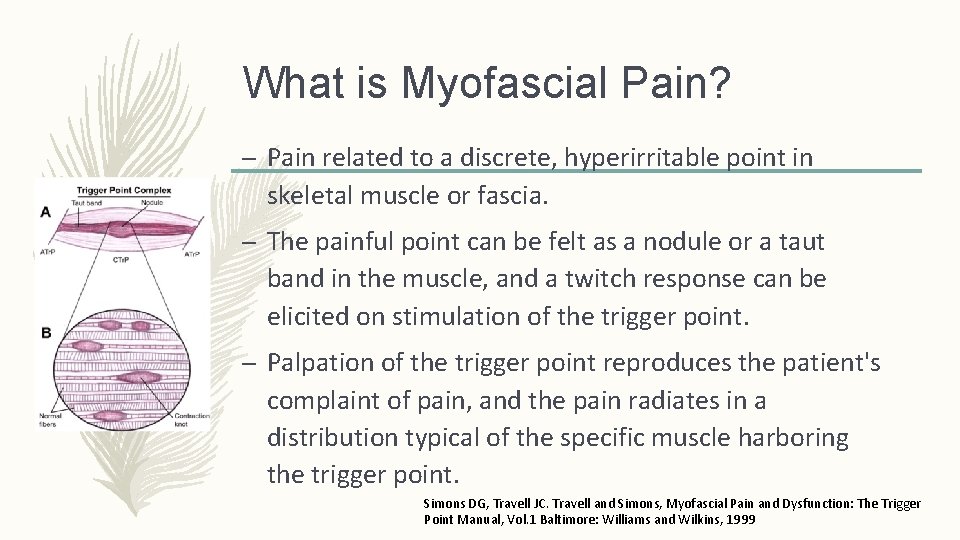
What is Myofascial Pain? – Pain related to a discrete, hyperirritable point in skeletal muscle or fascia. – The painful point can be felt as a nodule or a taut band in the muscle, and a twitch response can be elicited on stimulation of the trigger point. – Palpation of the trigger point reproduces the patient's complaint of pain, and the pain radiates in a distribution typical of the specific muscle harboring the trigger point. Simons DG, Travell JC. Travell and Simons, Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 1 Baltimore: Williams and Wilkins, 1999
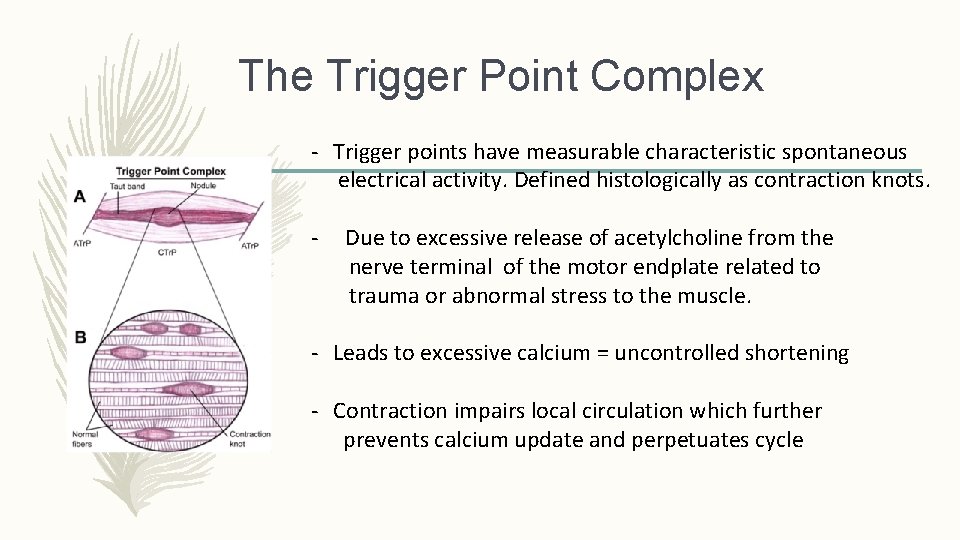
The Trigger Point Complex - Trigger points have measurable characteristic spontaneous electrical activity. Defined histologically as contraction knots. - Due to excessive release of acetylcholine from the nerve terminal of the motor endplate related to trauma or abnormal stress to the muscle. - Leads to excessive calcium = uncontrolled shortening - Contraction impairs local circulation which further prevents calcium update and perpetuates cycle
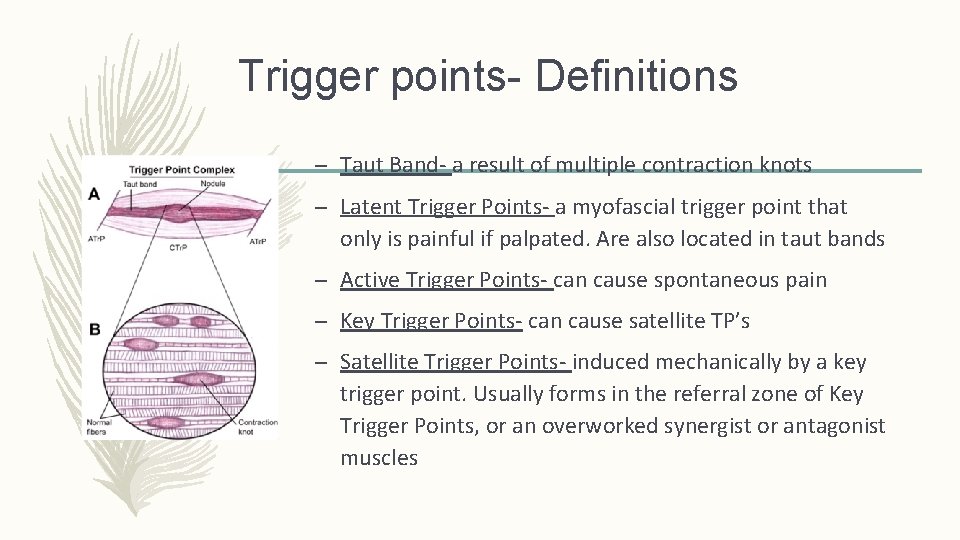
Trigger points- Definitions – Taut Band- a result of multiple contraction knots – Latent Trigger Points- a myofascial trigger point that only is painful if palpated. Are also located in taut bands – Active Trigger Points- can cause spontaneous pain – Key Trigger Points- can cause satellite TP’s – Satellite Trigger Points- induced mechanically by a key trigger point. Usually forms in the referral zone of Key Trigger Points, or an overworked synergist or antagonist muscles
What Causes Formation of Trigger Points? 1) Acute musculoskeletal injury- MVA, falls, direct blow to muscles 2) Overuse injuries/ Chronic stress on muscles 1) Postural stress, poor ergonomics, occupational 3) Secondary 1) Guarding from visceral sources of pain 2) Sexual or other forms of abuse 3) Stress/ tension/anxiety/ clenching

Myofascial Pain – History/ Symptoms – Trigger Point Pain- Can be constant, intermittent or no pain – Usually aggravated by certain movements, some relief with changing positions – Pain usually worse: strenuous use of the muscle, pressure on the Tr. P, muscle in shortened position for a long time, repeated contraction, cold, damp weather, periods of marked nervous tension, more stiff in morning – Pain usually better: short rest period, slow steady stretching of muscles, moist heat
Myofascial Pain- History / Symptoms – Abdominal wall trigger points can cause symptoms mimicking visceral disease: – External oblique- Heartburn – Lower internal oblique- detrusor spasm and urinary frequency, urinary retention, chronic diarrhea – Upper rectus abdominus- precordial pain, nausea, epigastric distress, mimic cholecystitis or peptic ulcer – Rectus at level of umbilicus- abdominal cramping – Lower rectus abdominus- dysmenorrhea – Rectus above pubis- urinary frequency or retention Ferguson, L. Clinical Mastery In The Treatment of Myofascial Pain. Lippincott Williams & Wilkins. 2005 p. 305
2) Referred Pain Of Myofascial Trigger Points – Muscles known to refer pain to the abdomen: – Thoracic iliocostalis – Quadratus Lumborum – Pelvic floor Muscles – Muscles often associated with / known to perpetuate trigger points in the abdomen: – Iliopsosas/ iliacus/ psoas ( hip flexors) – Piriformis/ Obturators/ Gluteals ( hip rotators) – Adductors – Multifidi – Pelvic floor muscles
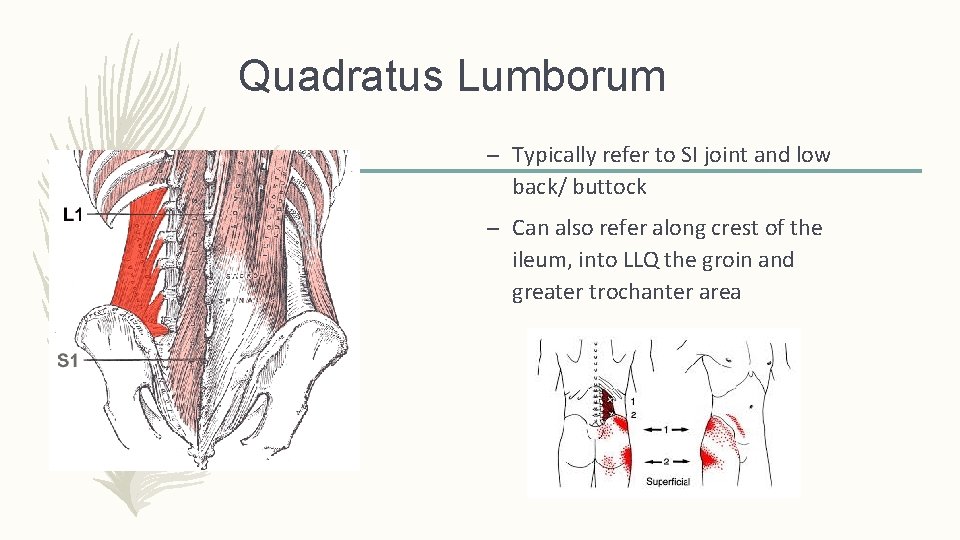
Quadratus Lumborum – Typically refer to SI joint and low back/ buttock – Can also refer along crest of the ileum, into LLQ the groin and greater trochanter area
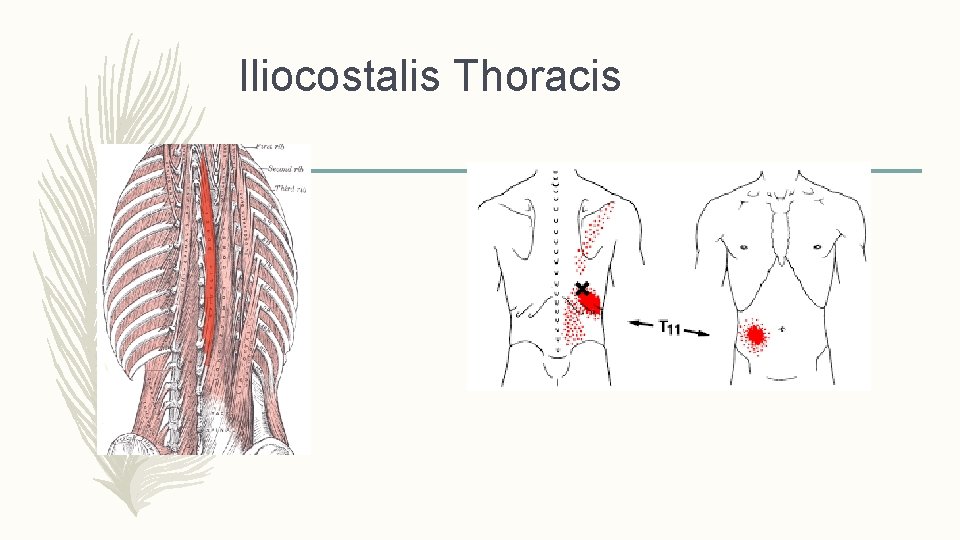
Iliocostalis Thoracis
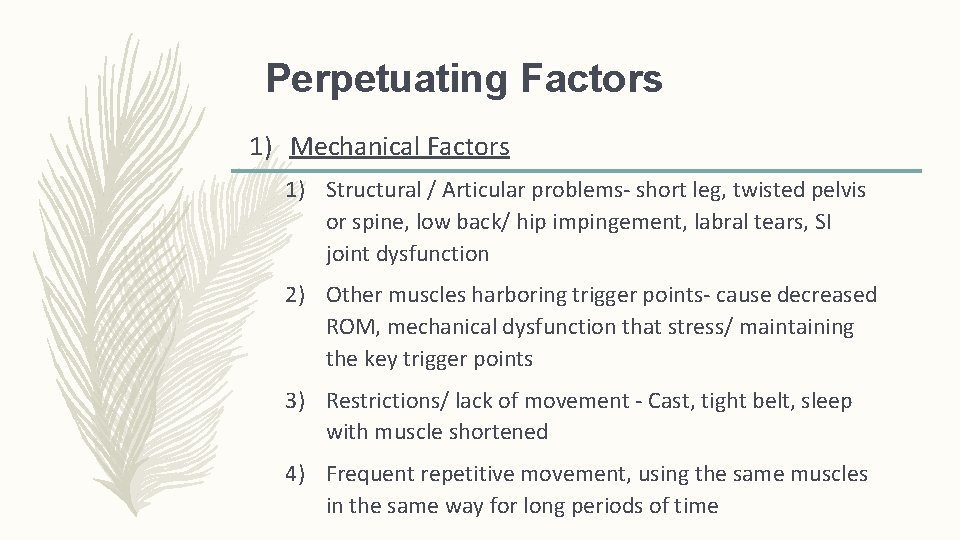
Perpetuating Factors 1) Mechanical Factors 1) Structural / Articular problems- short leg, twisted pelvis or spine, low back/ hip impingement, labral tears, SI joint dysfunction 2) Other muscles harboring trigger points- cause decreased ROM, mechanical dysfunction that stress/ maintaining the key trigger points 3) Restrictions/ lack of movement - Cast, tight belt, sleep with muscle shortened 4) Frequent repetitive movement, using the same muscles in the same way for long periods of time
Perpetuating Factors 2) Visceral Disease- can perpetuate abdominal wall myofascial pain via: a) Central sensitization b) Viscerosomatic convergence
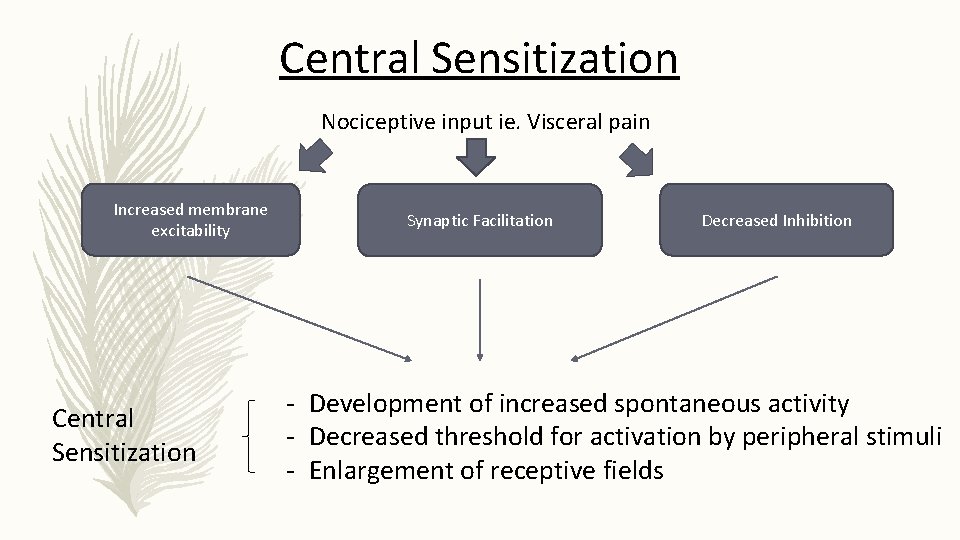
Central Sensitization Nociceptive input ie. Visceral pain Increased membrane excitability Central Sensitization Synaptic Facilitation Decreased Inhibition - Development of increased spontaneous activity - Decreased threshold for activation by peripheral stimuli - Enlargement of receptive fields
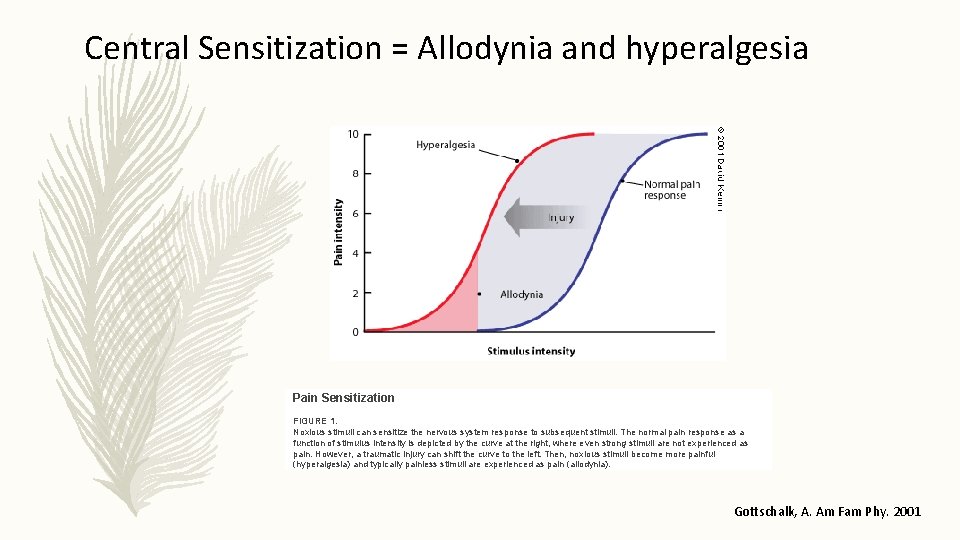
Central Sensitization = Allodynia and hyperalgesia Pain Sensitization FIGURE 1. Noxious stimuli can sensitize the nervous system response to subsequent stimuli. The normal pain response as a function of stimulus intensity is depicted by the curve at the right, where even strong stimuli are not experienced as pain. However, a traumatic injury can shift the curve to the left. Then, noxious stimuli become more painful (hyperalgesia) and typically painless stimuli are experienced as pain (allodynia). Gottschalk, A. Am Fam Phy. 2001
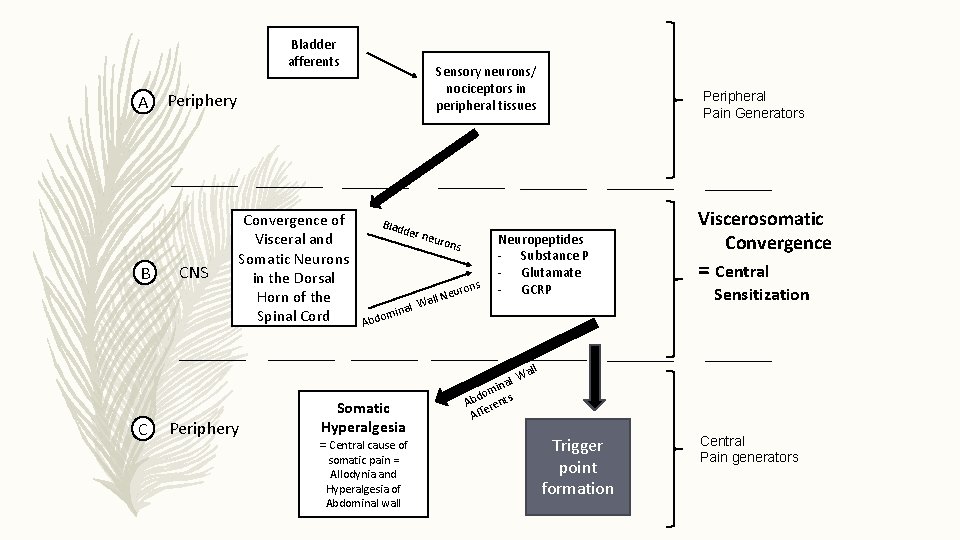
Bladder afferents A B C Sensory neurons/ nociceptors in peripheral tissues Periphery CNS Convergence of Visceral and Somatic Neurons in the Dorsal Horn of the Spinal Cord Periphery Blad der n euro ns l. N Wal inal ns euro Peripheral Pain Generators Neuropeptides - Substance P - Glutamate - GCRP Viscerosomatic Convergence = Central Sensitization om Abd Somatic Hyperalgesia = Central cause of somatic pain = Allodynia and Hyperalgesia of Abdominal wall l ina m o Abd rents e Aff ll Wa Trigger point formation Central Pain generators
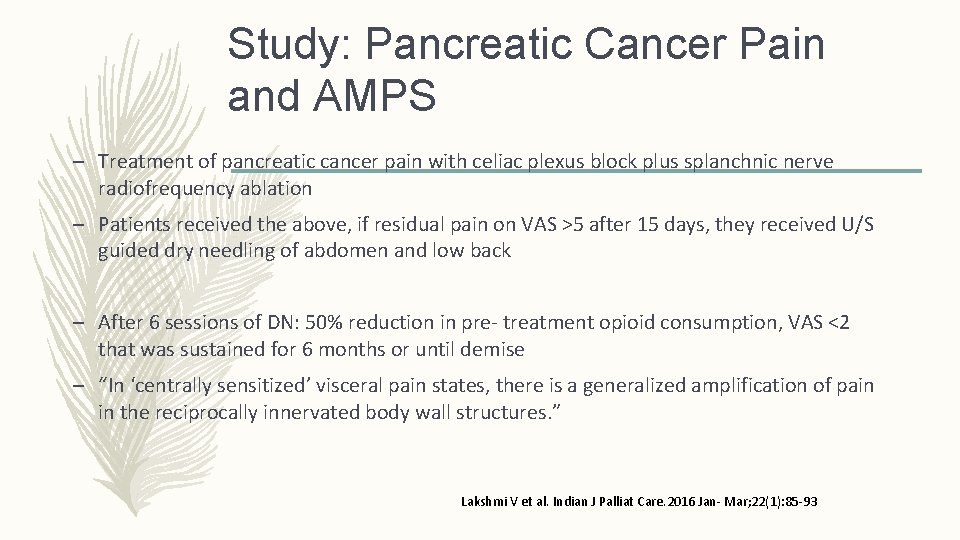
Study: Pancreatic Cancer Pain and AMPS – Treatment of pancreatic cancer pain with celiac plexus block plus splanchnic nerve radiofrequency ablation – Patients received the above, if residual pain on VAS >5 after 15 days, they received U/S guided dry needling of abdomen and low back – After 6 sessions of DN: 50% reduction in pre- treatment opioid consumption, VAS <2 that was sustained for 6 months or until demise – “In ‘centrally sensitized’ visceral pain states, there is a generalized amplification of pain in the reciprocally innervated body wall structures. ” Lakshmi V et al. Indian J Palliat Care. 2016 Jan- Mar; 22(1): 85 -93
Perpetuating Factors Continued 1) Mechanical Factors 2) Visceral Disease 3) Stress/ Behavioral Health Issues - Can contribute to tightening of muscles, - Negative thoughts and emotions (pain catastrophizing) can add to poor muscle mechanics - Can create barriers for self- management/ compliance. 4) Systemic Factors- Anything that interferes with energy metabolism of the muscle that increases muscle irritability, ie. Nutritional deficiencies
Treatment Algorithms For Myofascial Pain 1) Treat active trigger points first 2) Treat satellite trigger points in back, hip, pelvic floor 3) Assess and treat articular dysfunctions 4) Assess and treat decreases in range of motion and strength 5) Assess and treat other identifiable perpetuating factors 6) Scar Release
Treatment of Active Trigger Points – Trigger Point Injections – Dry needling – Ischemic Compression- temporarily suppress skin perfusion at Tr. P – Post isometric relaxation – Deep stroking – TENS/ Interferential current therapy – Botox injections
Dry Needling: Treatment of Myofascial Trigger Points Researchers compared superficial dry needling combined with active stretching to stretching alone. The investigators found that dry needling plus stretching was significantly more effective (P = 0. 043). The authors wrote: “Dry needling followed by active stretching is more effective than stretching alone in deactivating trigger points (reducing their sensitivity to pressure), and more effective than no treatment in reducing subjective pain. Stretching without prior deactivation may increase trigger point sensitivity. ” Edwards J, Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain – a randomized controlled trial. Acupunct Med. 2003; 21(3): 80 -86.
Acupuncture of Abdominal Wall Pain – Study of 17 women with AWP that had not responded to trigger point injections in Brazil – Patients had localized abdominal pain – Trigger points were identified by palpation and remained in situ for 25 minutes (modified acupuncture) – Once a week for ten weeks – Relief of pain after treatments that increased through the 8 th treatment, then sustained through the follow up at 1, 3 and 6 months based on VAS scale and Mc. Gill questionnaire Moreira de Souza Mitidieri, A. Medical Acupuncture Vol. 29, No. 6 2017
Manual Therapy Case Study – 16 year old male with severe chronic LLQ pain and nausea X 1 year – No injury, dull pain, bending forward and sitting made it worse – H/O Crohn’s disease- GI not feel causing pain – Had multiple imaging, laboratory and surgical evaluation negative – Treated with multiple medications and biofeedback – Diagnosis: “ Largely if not entirely psychosomatic” Muscolino, J. Abdominal wall trigger point case study. Journal of Bodywork & Movement Therapies. 2013 (17): 151 -156
Manual Therapy Case Study – Referred to Chiropractor (author of article) – On exam, left psoas was markedly tight, trigger points identified in left Rectus Abdominis (RA) one inch later to umbilicus with palpation reproduced his pain – Felt nausea was related to RA trigger points – Treatment: – 1 hour sessions twice a week: ultrasound, e-stim, moist heat, soft tissue manipulation (deep stroking) and stretching. Postural advice, home exercises 2 -3 times a day
Manual Therapy Case Study – Response: – Twice weekly treatments after 2 weeks saw an improvement, continued therapy for 3 more months. – Subjective improvement of RA 35% , of psoas 65% – Objective evaluation of tightness, RA improved 50%, psoas 80% – Referred for trigger point injections: Had 6 into RA, 4 months later patient reported 90 % improvement. – Total: 6 months of consistent hands on care with PT modalities and the Tr. P injections, he resumed functional level. Another 68 months of manual therapy was required to resolve his symptoms.
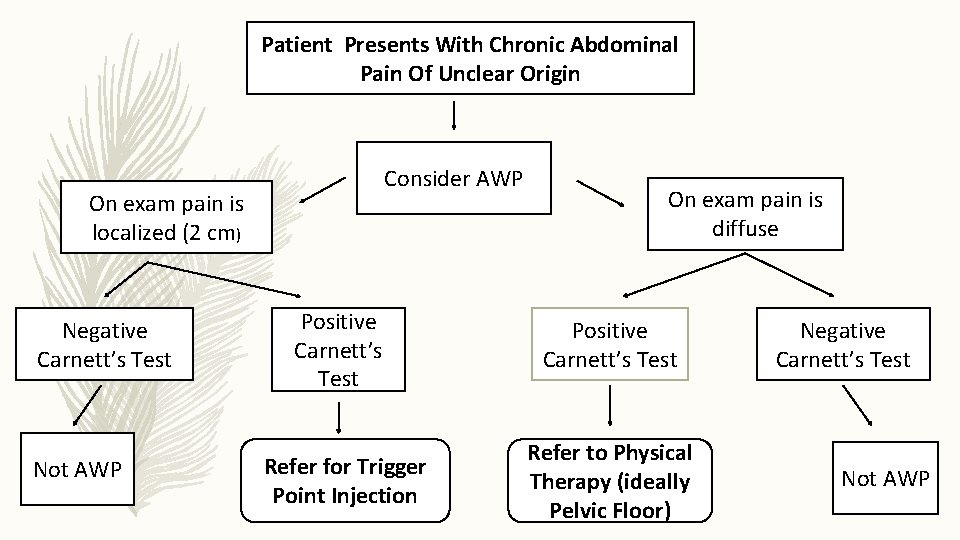
Patient Presents With Chronic Abdominal Pain Of Unclear Origin Consider AWP On exam pain is localized (2 cm) Negative Carnett’s Test Not AWP On exam pain is diffuse Positive Carnett’s Test Refer for Trigger Point Injection Refer to Physical Therapy (ideally Pelvic Floor) Negative Carnett’s Test Not AWP
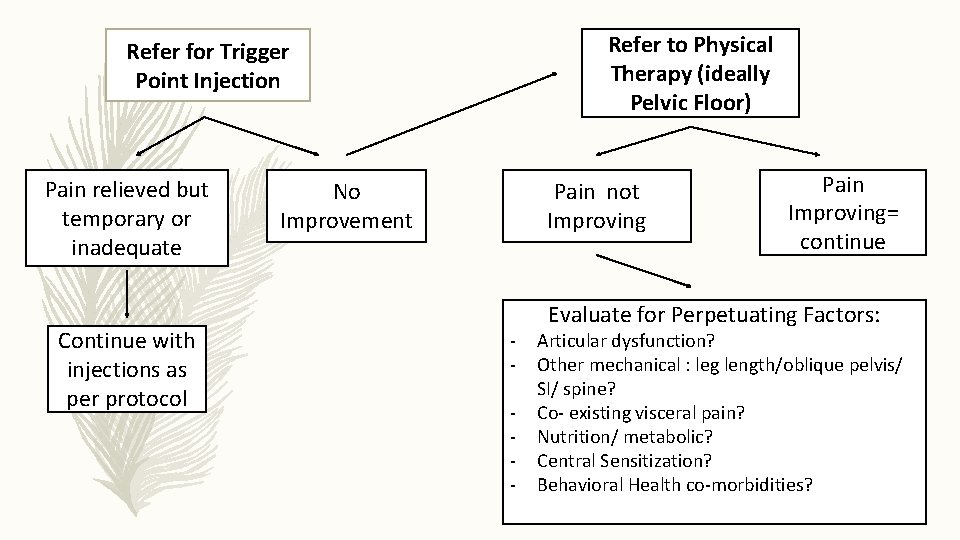
Refer to Physical Therapy (ideally Pelvic Floor) Refer for Trigger Point Injection Pain relieved but temporary or inadequate Continue with injections as per protocol No Improvement Pain not Improving - Pain Improving= continue Evaluate for Perpetuating Factors: Articular dysfunction? Other mechanical : leg length/oblique pelvis/ SI/ spine? Co- existing visceral pain? Nutrition/ metabolic? Central Sensitization? Behavioral Health co-morbidities?
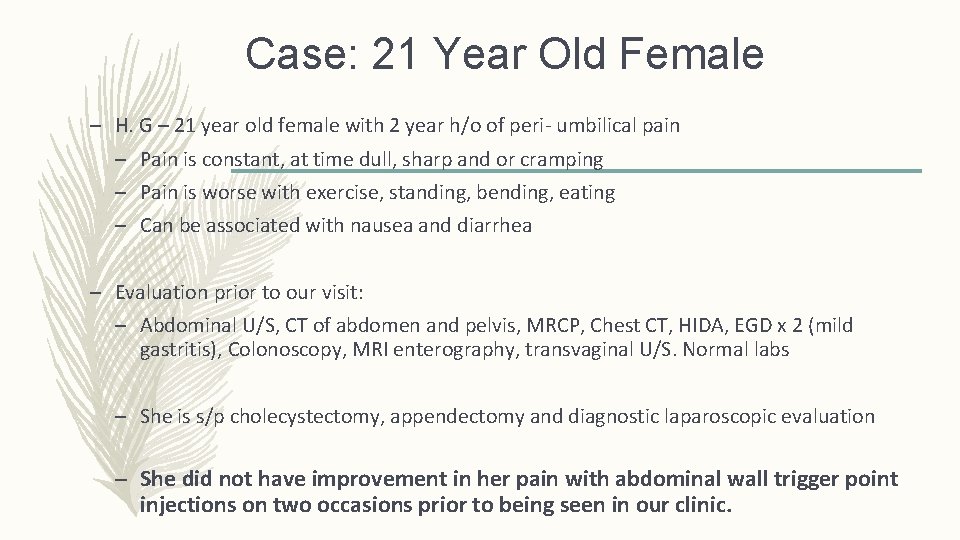
Case: 21 Year Old Female – H. G – 21 year old female with 2 year h/o of peri- umbilical pain – Pain is constant, at time dull, sharp and or cramping – Pain is worse with exercise, standing, bending, eating – Can be associated with nausea and diarrhea – Evaluation prior to our visit: – Abdominal U/S, CT of abdomen and pelvis, MRCP, Chest CT, HIDA, EGD x 2 (mild gastritis), Colonoscopy, MRI enterography, transvaginal U/S. Normal labs – She is s/p cholecystectomy, appendectomy and diagnostic laparoscopic evaluation – She did not have improvement in her pain with abdominal wall trigger point injections on two occasions prior to being seen in our clinic.
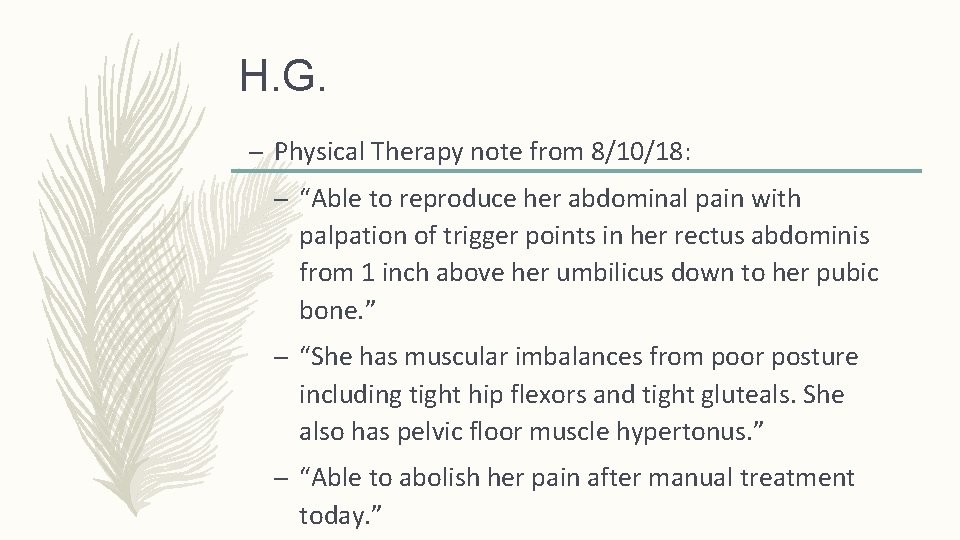
H. G. – Physical Therapy note from 8/10/18: – “Able to reproduce her abdominal pain with palpation of trigger points in her rectus abdominis from 1 inch above her umbilicus down to her pubic bone. ” – “She has muscular imbalances from poor posture including tight hip flexors and tight gluteals. She also has pelvic floor muscle hypertonus. ” – “Able to abolish her pain after manual treatment today. ”
Summary 1) Patient with abdominal pain and negative evaluation – consider abdominal wall pain. 2) If pain is localized and positive Carnett’s test – consider trigger point injections. 3) If pain is diffuse and positive Carnett’s test – refer to PT/ consider perpetuating factors. 4) When patients have “pain to palpation out of proportion to physical exam findings” – think central sensitization/ allodynia/ hyperalgesia.
Test Question #1 True or False When preforming the Carnett’s test, the supine patient is asked to raise their head while the medical provider is palpating a tender area on the abdomen. If the pain is increased, the pain is likely visceral in origin.
Answer to Question #1 FALSE
Test Question #2 True or False Trigger point formation is due to inadequate release of acetylcholine from the nerve terminal of the motor end plate related to trauma or abnormal stress to the muscle.
Answer to Question #2 FALSE

THANK YOU!
- Slides: 51