Abdominal Imaging of Liver Chuan Lu School of
Abdominal Imaging of Liver Chuan Lu School of Radiology Taishan Medical University
Anatomy l Protocols and Normal Ultrasound Findings l Pathology l
Anatomy of the Liver l The Liver occupies all of the right hypochondrium, the greater part of the epigastrium, and left hypochondrium. The ribs cover the greater part of the right lobe. In the epigastric region, the liver extends several centimeters below the xiphoid process. Most of the left lobe of the liver is covered by the rib cage.
Lobes of the Liver l l l Right lobe: The right lobe of the liver is the largest of the liver’s lobes. It extends the left lobe by a ratio of 6: 1. It occupies the right hypochodrium. Left lobe: The left lobe of the liver lies in the epigastric and left hypochondriac region. Caudate lobe: The caudate lobe is a small lobe situated on the posterosuperior surface of the left lobe opposite the tenth and eleventh thoracic vertebrae.
Hepatic Nomenclature l Couinaud’s system of hepatic nomenclature provides the anatomic basis for hepatic surgical resection. By using this system , the radiologist may be able to precisely isolate the location of a lesion for the surgical team
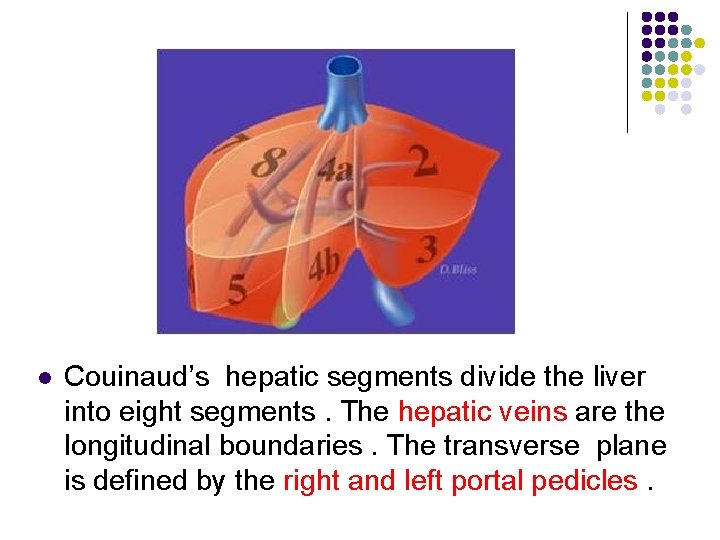
l Couinaud’s hepatic segments divide the liver into eight segments. The hepatic veins are the longitudinal boundaries. The transverse plane is defined by the right and left portal pedicles.
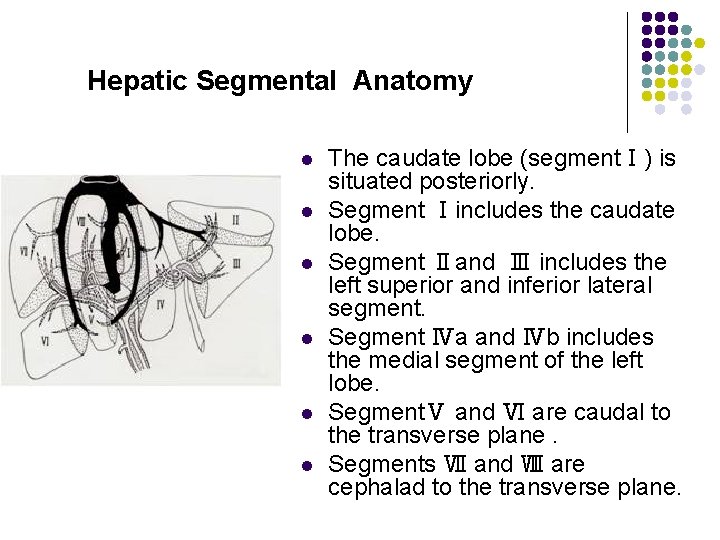
Hepatic Segmental Anatomy l l l The caudate lobe (segmentⅠ) is situated posteriorly. Segment Ⅰincludes the caudate lobe. Segment Ⅱand Ⅲ includes the left superior and inferior lateral segment. Segment Ⅳa and Ⅳb includes the medial segment of the left lobe. SegmentⅤ and Ⅵ are caudal to the transverse plane. Segments Ⅶ and Ⅷ are cephalad to the transverse plane.
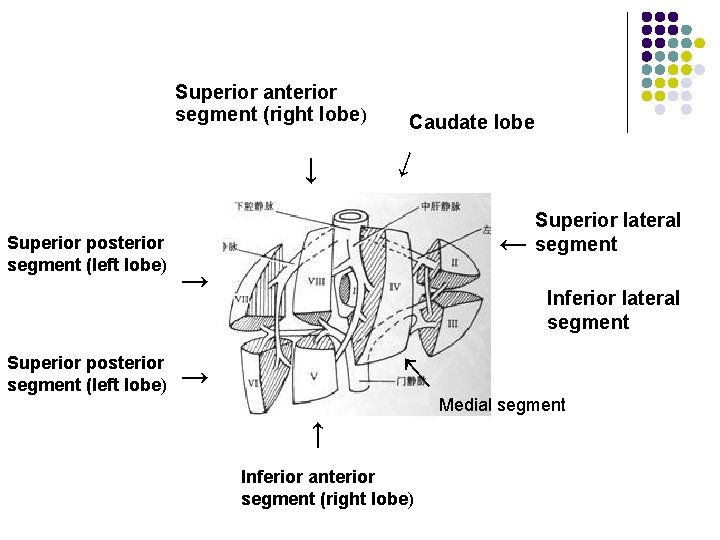
Superior anterior segment (right lobe) → → Superior lateral segment → Inferior lateral segment → Medial segment → Superior posterior segment (left lobe) → → Superior posterior segment (left lobe) Caudate lobe Inferior anterior segment (right lobe)
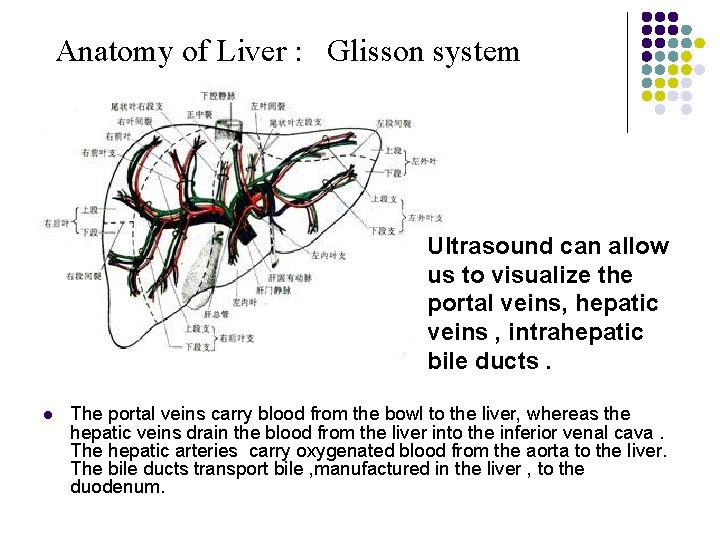
Anatomy of Liver : Glisson system Ultrasound can allow us to visualize the portal veins, hepatic veins , intrahepatic bile ducts. l The portal veins carry blood from the bowl to the liver, whereas the hepatic veins drain the blood from the liver into the inferior venal cava. The hepatic arteries carry oxygenated blood from the aorta to the liver. The bile ducts transport bile , manufactured in the liver , to the duodenum.
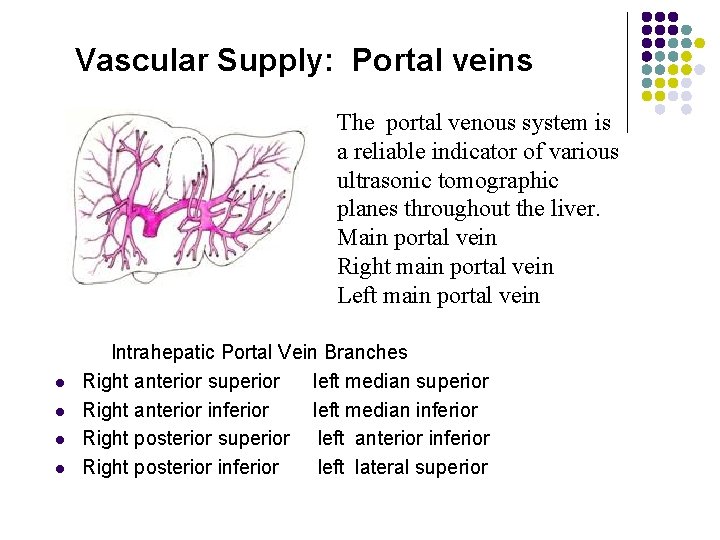
Vascular Supply: Portal veins The portal venous system is a reliable indicator of various ultrasonic tomographic planes throughout the liver. Main portal vein Right main portal vein Left main portal vein l l Intrahepatic Portal Vein Branches Right anterior superior left median superior Right anterior inferior left median inferior Right posterior superior left anterior inferior Right posterior inferior left lateral superior
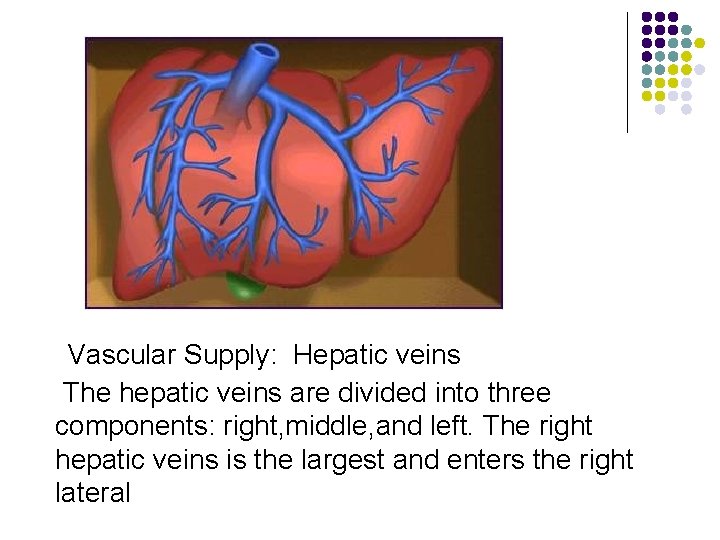
Vascular Supply: Hepatic veins The hepatic veins are divided into three components: right, middle, and left. The right hepatic veins is the largest and enters the right lateral
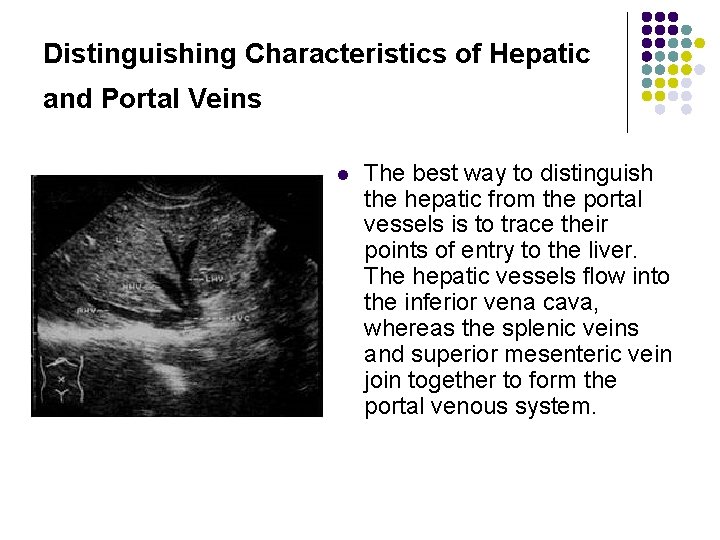
Distinguishing Characteristics of Hepatic and Portal Veins l The best way to distinguish the hepatic from the portal vessels is to trace their points of entry to the liver. The hepatic vessels flow into the inferior vena cava, whereas the splenic veins and superior mesenteric vein join together to form the portal venous system.
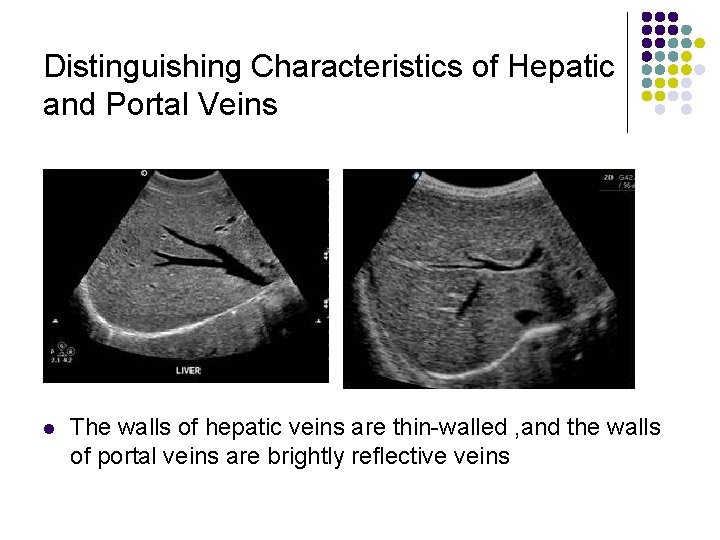
Distinguishing Characteristics of Hepatic and Portal Veins l The walls of hepatic veins are thin-walled , and the walls of portal veins are brightly reflective veins
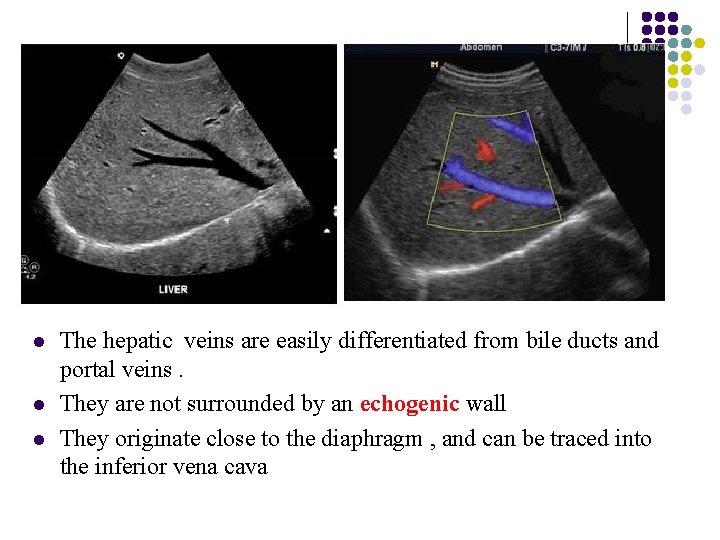
l l l The hepatic veins are easily differentiated from bile ducts and portal veins. They are not surrounded by an echogenic wall They originate close to the diaphragm , and can be traced into the inferior vena cava
Sonographic Evaluation of the Liver l Evaluation of the hepatic structure is one of the most important procedures in sonography for many reasons. The normal , basiclly homogenerous parenchyma of the liver allows imaging of the neighboring anatomic structures in the upper abdomen.
Sonographic Evaluation of The Liver l l l The system gain should be adjusted to adequately penetrate the entire right lobe of the liver as a smooth , homogeneous echo-texture pattern The time gain compensation should be adjusted to balance the far-gain and the near-gain echo signals. The far time -gain control pods should gradually be increased until the posterior aspect of the liver is well seen.
l l The appropriate transducer depends on the patient’s body habitus and size The average adult abdomen usually requires a 3. 5 MHz
l l l The basic instrumentation should be adjusted in the following parameters : Time gain compensation Overall gain Transducer frequency and type Depth and focus

Longitudinal Scan Plane l The longitudinal , or sagittal, scan offers an excellent window to visualize the hepatic structure. With the patient in full inspiration , the transducer may be swept under the costal margin to record the liver parenchyma from the anterior abdominal wall to the diaphragm.
Longitudinal Scan Plane l l Scan Ⅰ Scan Ⅱ Scan Ⅲ Scan Ⅳ, Ⅴ, Ⅵ
Longitudinal Scan Plane l Scan Ⅰ The initial scan should be made slightly to the left of the midline to record the left lobe of the liver and the abdominal aorta. The left hepatic and portal veins may be seen as small circular structures in this view.
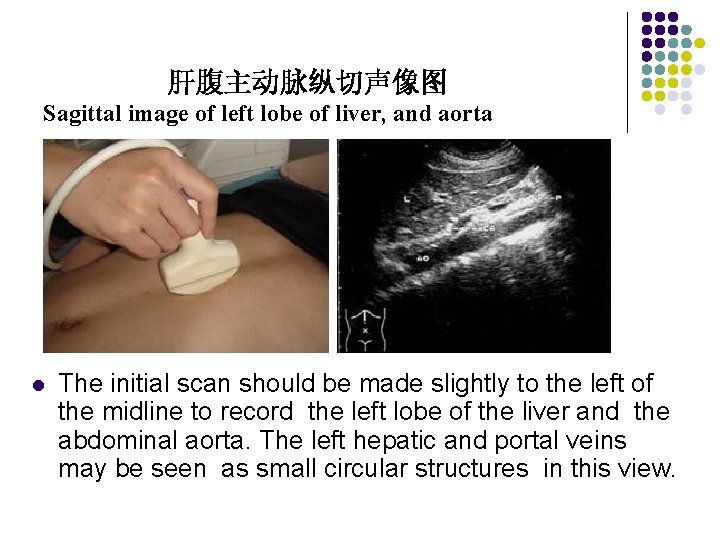
肝腹主动脉纵切声像图 Sagittal image of left lobe of liver, and aorta l The initial scan should be made slightly to the left of the midline to record the left lobe of the liver and the abdominal aorta. The left hepatic and portal veins may be seen as small circular structures in this view.
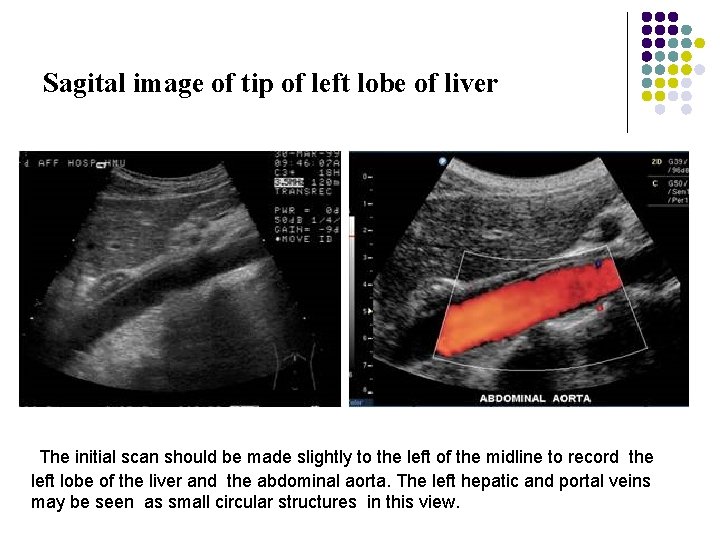
Sagital image of tip of left lobe of liver The initial scan should be made slightly to the left of the midline to record the left lobe of the liver and the abdominal aorta. The left hepatic and portal veins may be seen as small circular structures in this view.
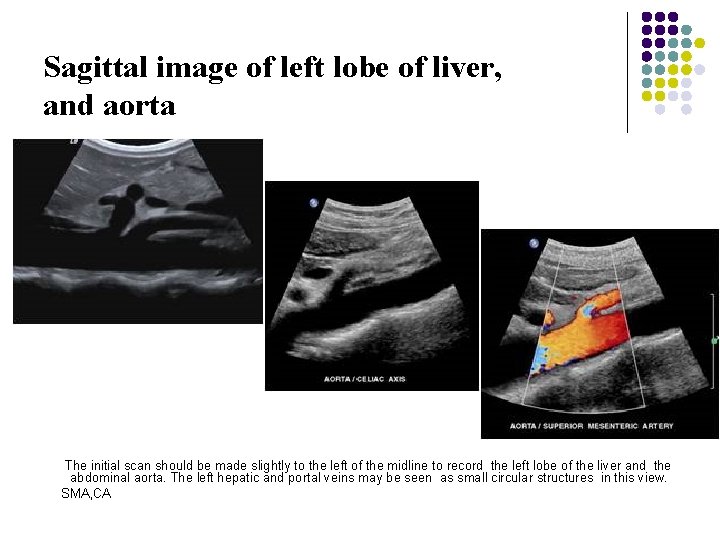
Sagittal image of left lobe of liver, and aorta The initial scan should be made slightly to the left of the midline to record the left lobe of the liver and the abdominal aorta. The left hepatic and portal veins may be seen as small circular structures in this view. SMA, CA
Longitudinal Scan Plane l l Scan Ⅱ As the sonographer scans at midline or slightly to the right of midline , a larger segment of the left lobe and the inferior vena cava may be seen posteriorly. In this view , it is useful to record the inferior vena cana as it is dilated near the end of inspiration. The left or midline hepatic vein may be imaged as it drain into the inferior vena cava near the level of the diaghram. The area of the portal hepatis is shown anterior to the inferior vena cava as the superior mesenteric vein and splenic vein converge to form the main portal vein. The common bile duct may be seen just anterior to the main portal vein. The head of the pancreas may be seen just inferior to the right lobe of the liver and main portal vein and anterior to the inferior vena cava.
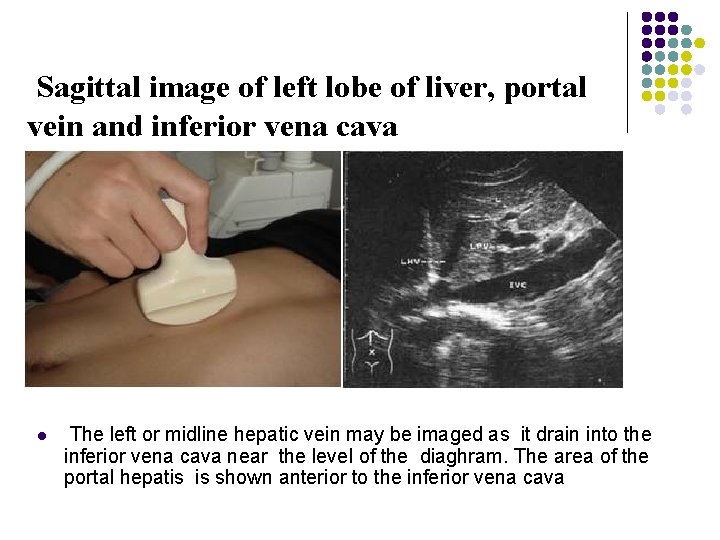
Sagittal image of left lobe of liver, portal vein and inferior vena cava l The left or midline hepatic vein may be imaged as it drain into the inferior vena cava near the level of the diaghram. The area of the portal hepatis is shown anterior to the inferior vena cava
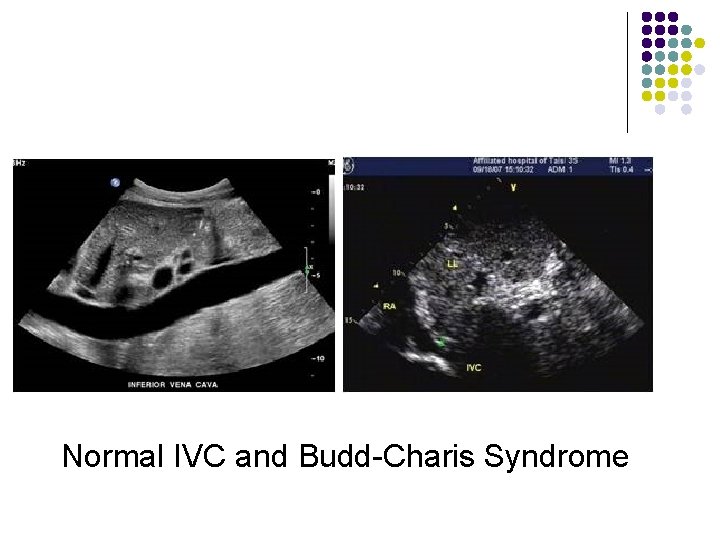
Normal IVC and Budd-Charis Syndrome
Longitudinal Scan Plane l Scan Ⅲ The next image should be made slightly lateral to this saggital plane to record part of the right portal vein and right lobe of liver. The caudate lobe is often seen in this view.
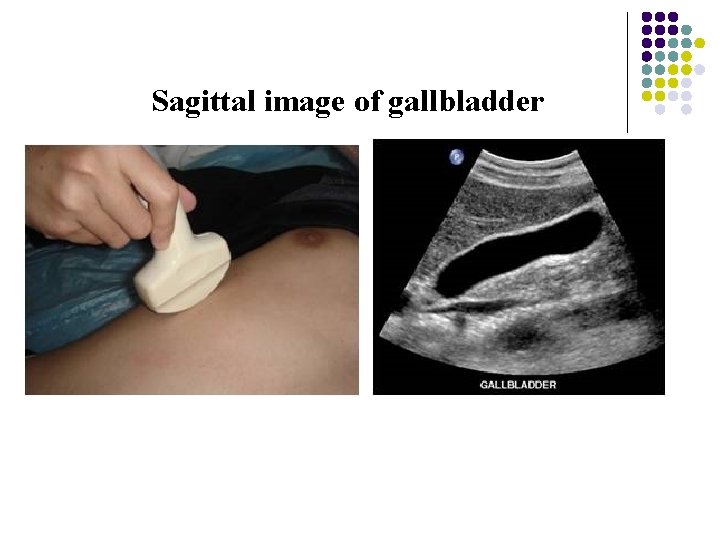
Sagittal image of gallbladder
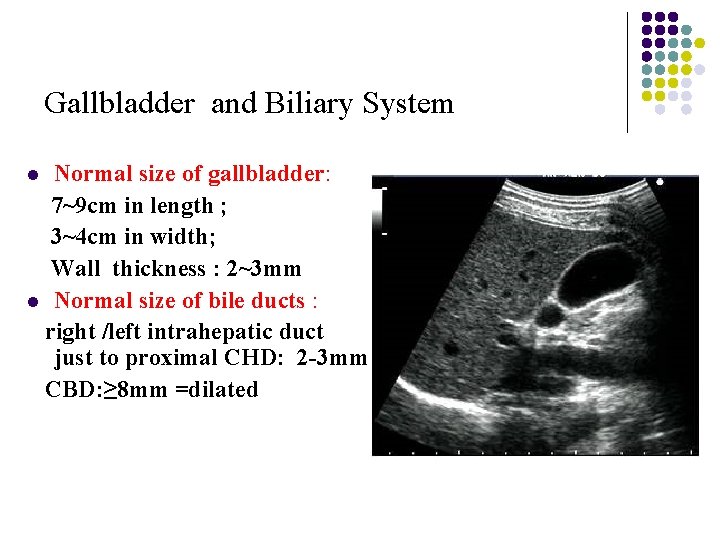
Gallbladder and Biliary System Normal size of gallbladder: 7~9 cm in length ; 3~4 cm in width; Wall thickness : 2~3 mm l Normal size of bile ducts : right /left intrahepatic duct just to proximal CHD: 2 -3 mm ; CBD: ≥ 8 mm =dilated l
Longitudinal Scan Plane l Scan Ⅳ, Ⅴ, Ⅵ The nest three scans should be made in small increment through the right lobe of the liver. The last scan is usually made to show the right kidney and lateral segment of the right lobe of the liver. The liver texture is compared with the renal parenchyma. The normal liver parenchyma should have a softer , more homogenerous texture than the dense medulla and hypoechoic renal cortex. Liver size may be measured from the tip of the liver to the diaphragm. Generally this measurement is less than 15 cm, with 15 to 20 cm representing the upper limits of normal. Hepatomegaly is present when the liver measurement exceed 20 cm.
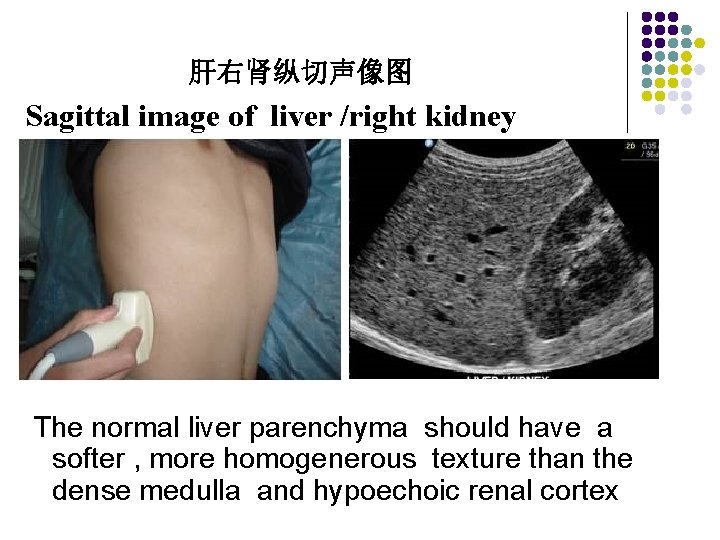
肝右肾纵切声像图 Sagittal image of liver /right kidney The normal liver parenchyma should have a softer , more homogenerous texture than the dense medulla and hypoechoic renal cortex
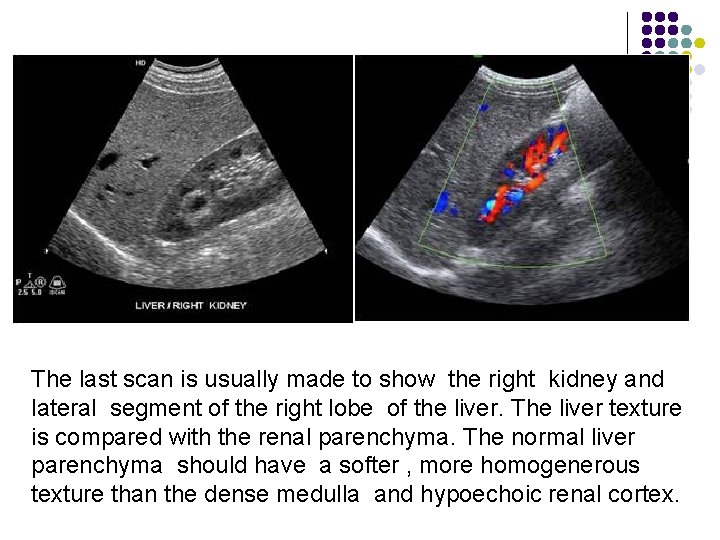
The last scan is usually made to show the right kidney and lateral segment of the right lobe of the liver. The liver texture is compared with the renal parenchyma. The normal liver parenchyma should have a softer , more homogenerous texture than the dense medulla and hypoechoic renal cortex.
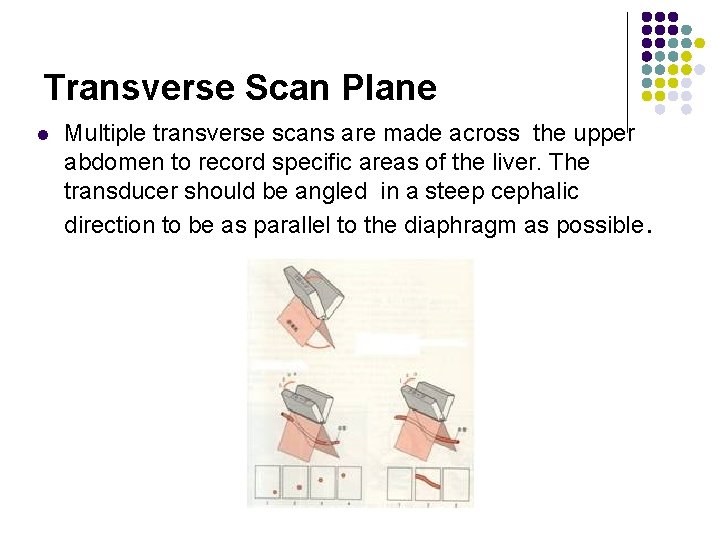
Transverse Scan Plane l Multiple transverse scans are made across the upper abdomen to record specific areas of the liver. The transducer should be angled in a steep cephalic direction to be as parallel to the diaphragm as possible.
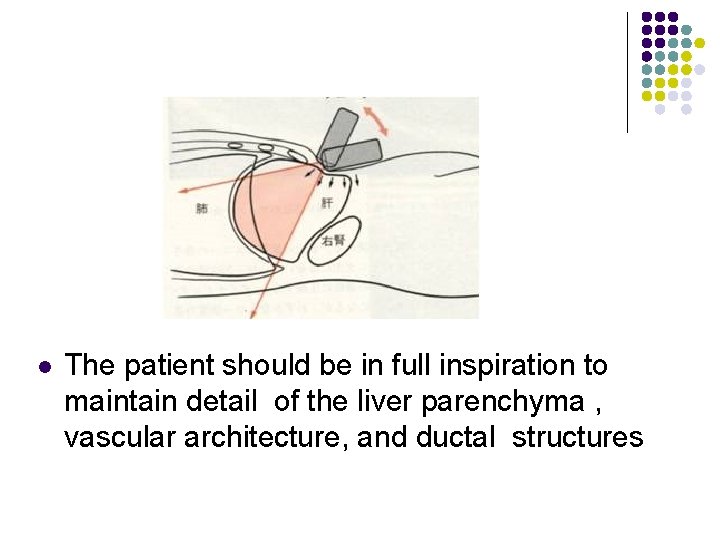
l The patient should be in full inspiration to maintain detail of the liver parenchyma , vascular architecture, and ductal structures
Transverse Scan Plane l l l Scan Ⅰ Scan Ⅱ Scan Ⅲ Scan Ⅳ Scan Ⅴ, Ⅵ
Transverse Scan Plane l Scan Ⅰ The initial transverse scan is made with the transducer under the costal margin at a steep angel perpenducular to the diaphragm. The patient should be in deep inspiration to adequately record the dome of the liver. The sonographer should identify the inferior vena cava and three hepatic veins as they drain into the cava. This pattern has sometimes been referred to as “reindeer sign” or “Playboy bunny” sign.

l The sonographer should identify the inferior vena cava and three hepatic veins as they drain into the cava. This pattern has sometimes been referred to as “reindeer sign” or “Playboy bunny” sign.
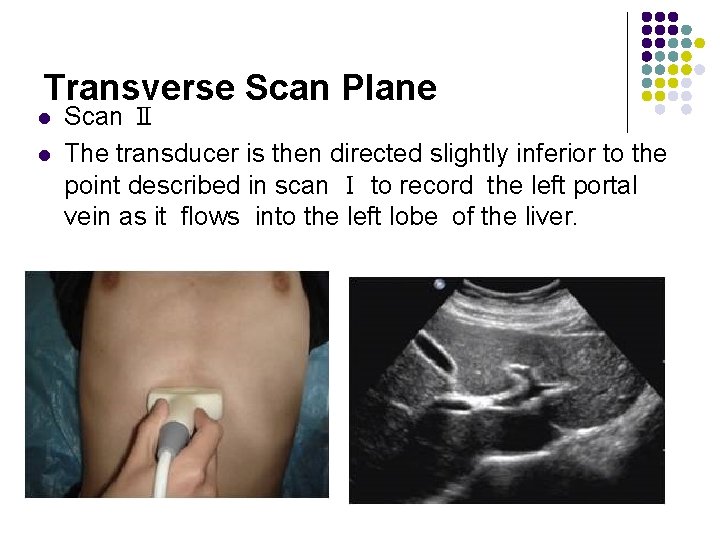
Transverse Scan Plane l l Scan Ⅱ The transducer is then directed slightly inferior to the point described in scan Ⅰ to record the left portal vein as it flows into the left lobe of the liver.
Transverse Scan Plane l Scan Ⅲ The porta hepatis is seen as a tubular structure within the central part of the liver. Sometimes the left or right portal vein can be identified. The caudate lobe may be seen just superior to the porta hepatis ; thus , depending on the angel , either the caudate lobe is shown anterior to the inferior vena cava, or as the transducer moves inferior , the porta hepatis is identified anterior to the inferior vena cava.
Transverse Scan Plane l Scan Ⅳ The fourth scan should show the right portal vein as it divides into the anterior and posterior segments of the right lobe of the liver. The gallbladder may be seen in this scan as an anechoic structure medial to the right lobe and anterior to the right kidney.
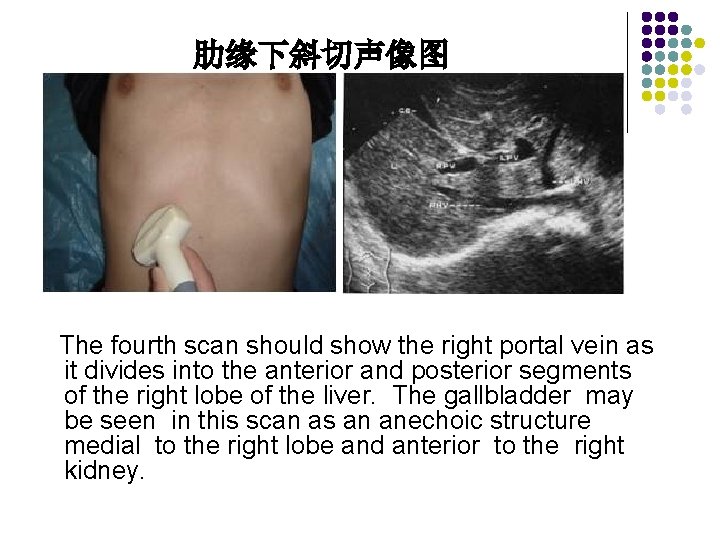
肋缘下斜切声像图 The fourth scan should show the right portal vein as it divides into the anterior and posterior segments of the right lobe of the liver. The gallbladder may be seen in this scan as an anechoic structure medial to the right lobe and anterior to the right kidney.
Transverse Scan Plane l Scan Ⅴ, Ⅵ These two scans are made through the lower segment of the right lobe of the liver. The right kidney is the posterior border. Usually intrahepatic vascular structures are not identified in these views
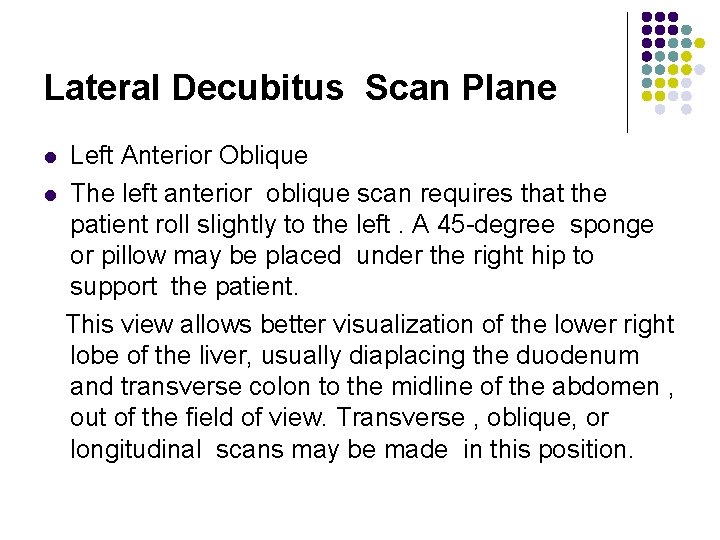
Lateral Decubitus Scan Plane Left Anterior Oblique l The left anterior oblique scan requires that the patient roll slightly to the left. A 45 -degree sponge or pillow may be placed under the right hip to support the patient. This view allows better visualization of the lower right lobe of the liver, usually diaplacing the duodenum and transverse colon to the midline of the abdomen , out of the field of view. Transverse , oblique, or longitudinal scans may be made in this position. l
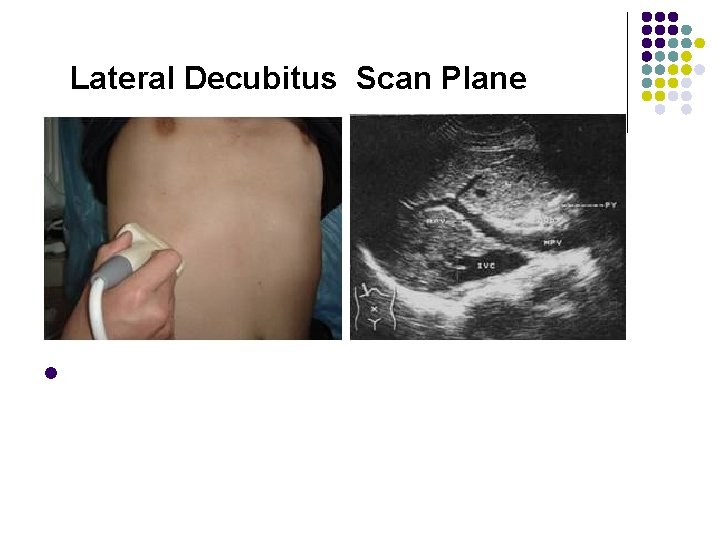
Lateral Decubitus Scan Plane l
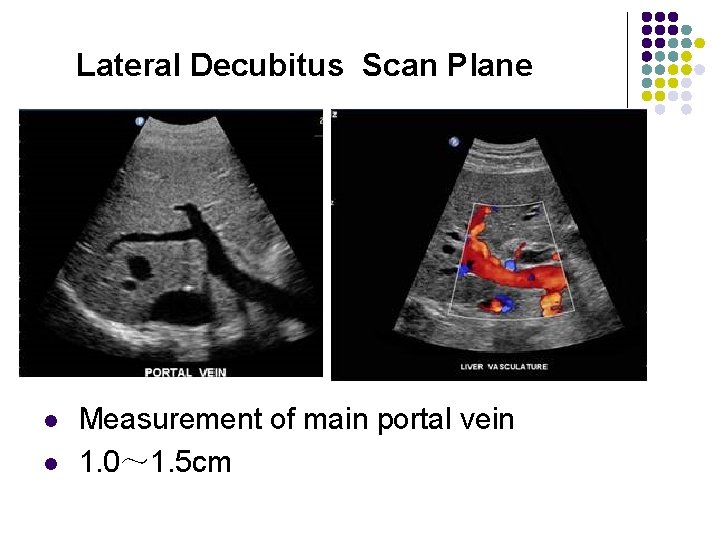
Lateral Decubitus Scan Plane l l Measurement of main portal vein 1. 0~ 1. 5 cm
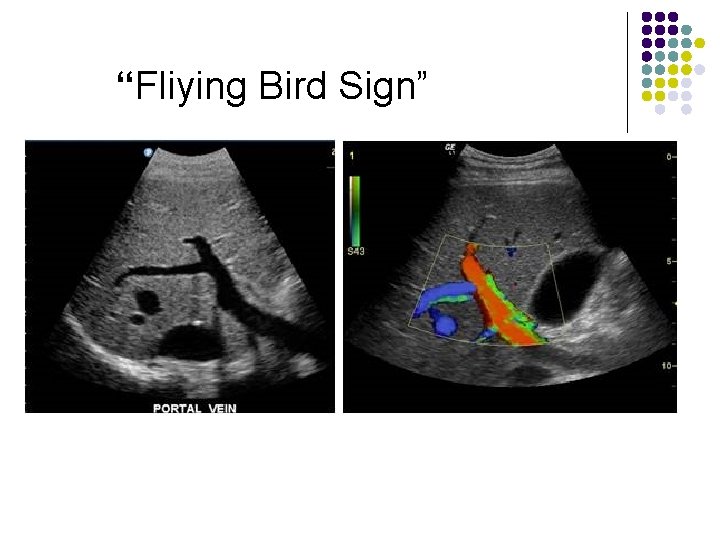
“Fliying Bird Sign”
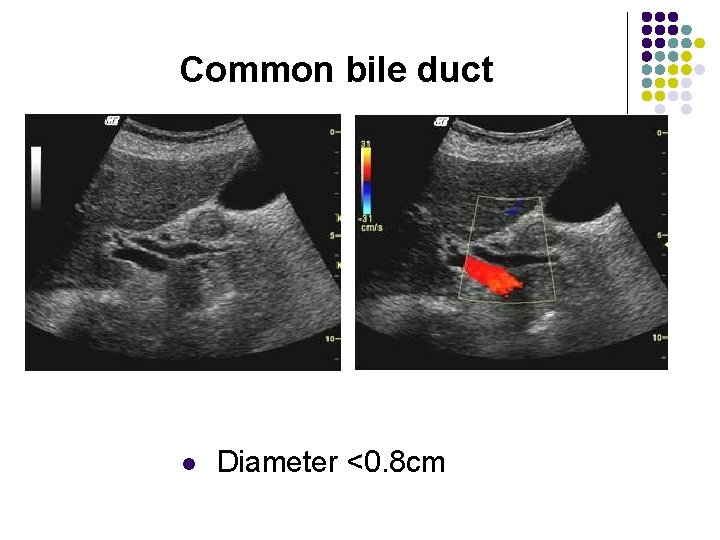
Common bile duct l Diameter <0. 8 cm
Sonographic Evaluation of The Liver l l l Adequate scanning technique demands that each patient be examined with the following assessment The size of the liver in the longitudinal plane The attenuation of the liver parenchyma Liver texture The presence of hepatic vascular structures, ligaments , and fissures
Pathology of the Live l Evaluation of the liver parenchyma includes the assessment of its size , configuration, homogeneity , and contour.
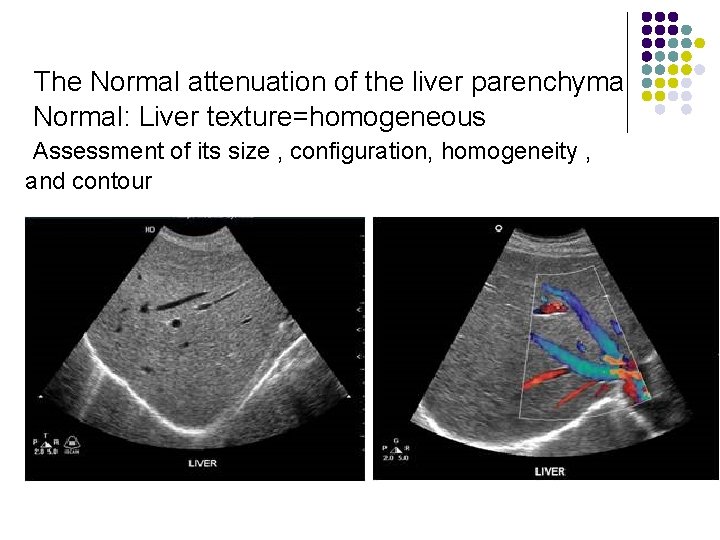
The Normal attenuation of the liver parenchyma Normal: Liver texture=homogeneous Assessment of its size , configuration, homogeneity , and contour
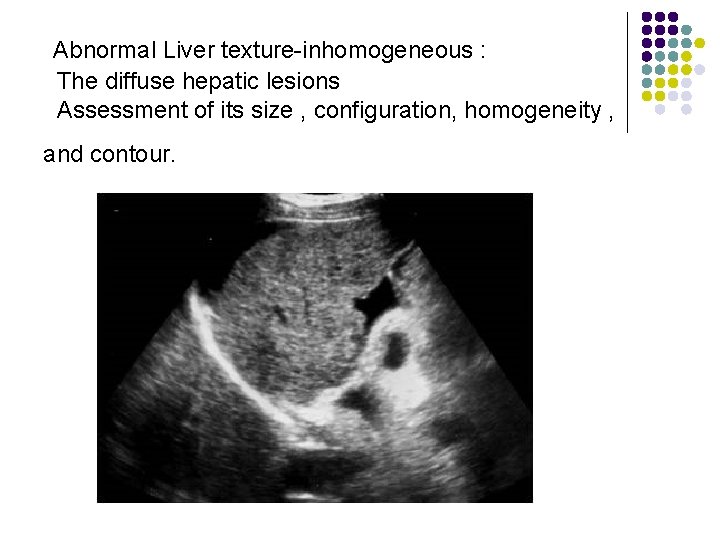
Abnormal Liver texture-inhomogeneous : The diffuse hepatic lesions Assessment of its size , configuration, homogeneity , and contour.
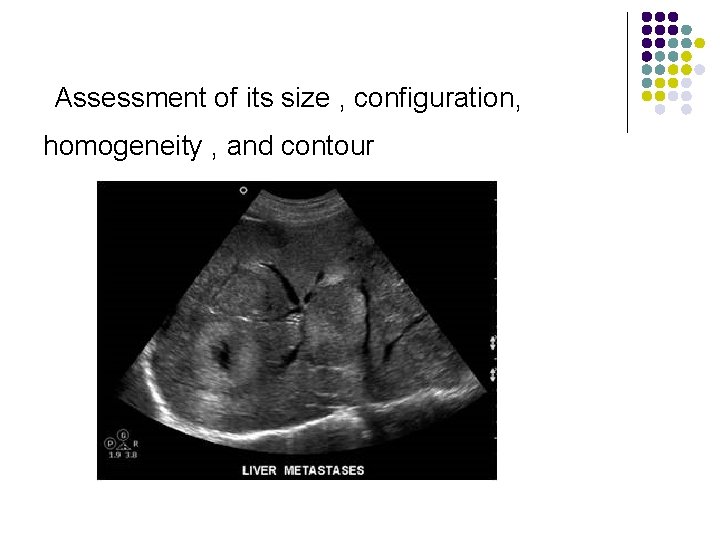
Assessment of its size , configuration, homogeneity , and contour
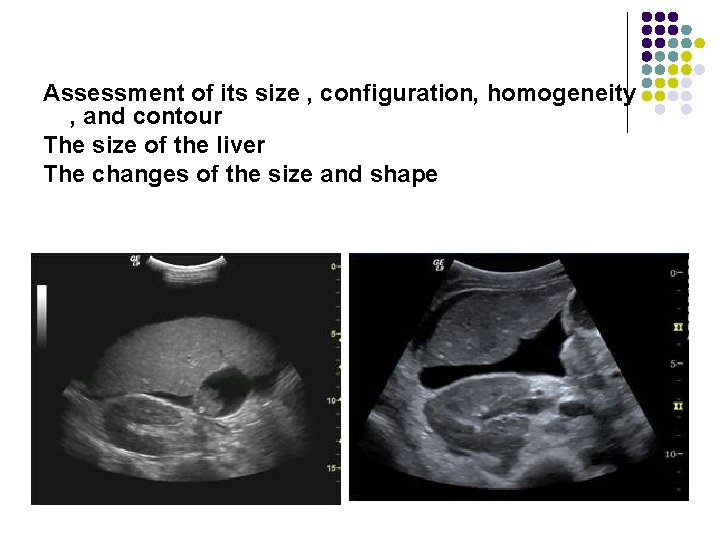
Assessment of its size , configuration, homogeneity , and contour The size of the liver The changes of the size and shape
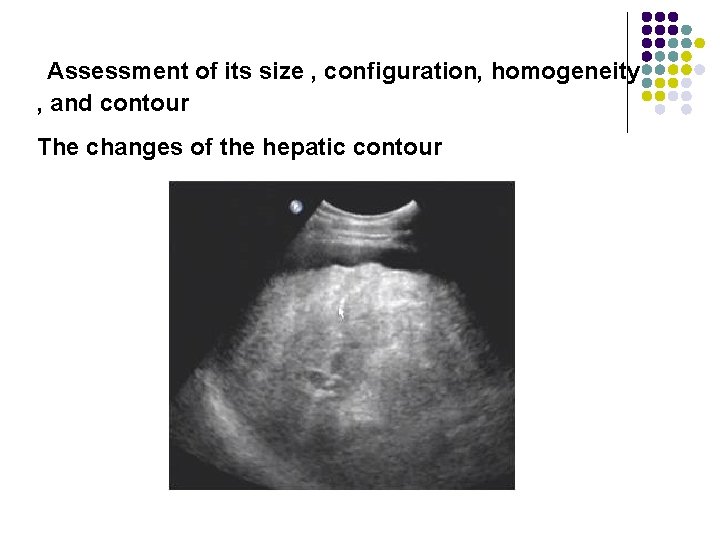
Assessment of its size , configuration, homogeneity , and contour The changes of the hepatic contour
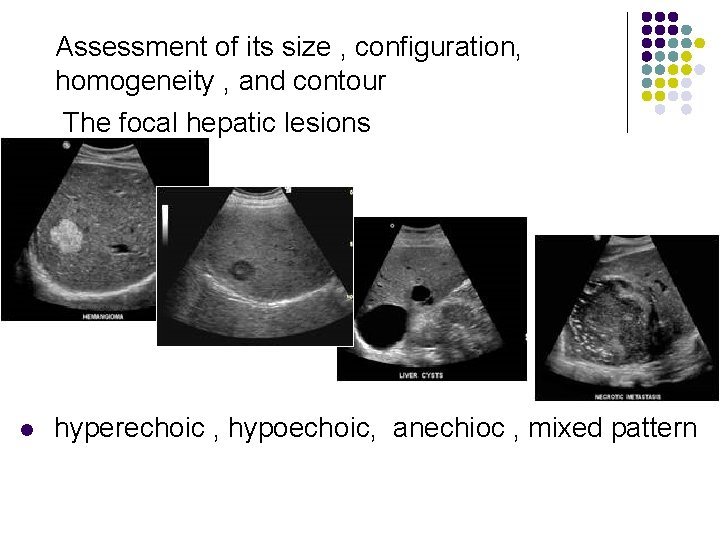
Assessment of its size , configuration, homogeneity , and contour The focal hepatic lesions l hyperechoic , hypoechoic, anechioc , mixed pattern
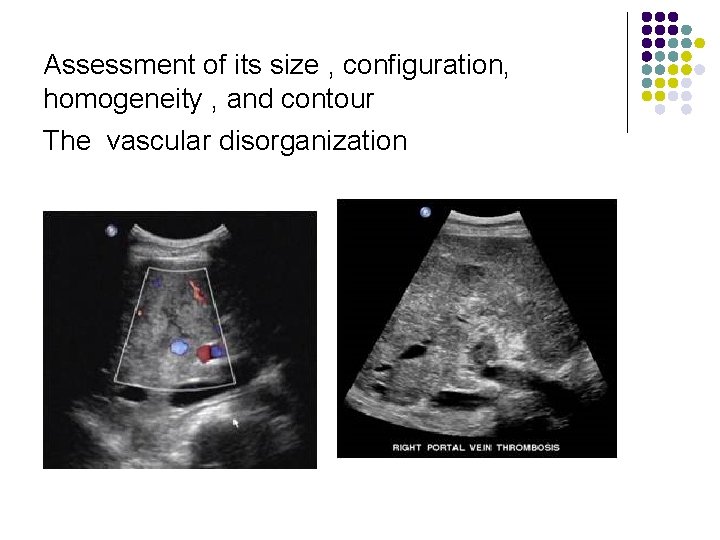
Assessment of its size , configuration, homogeneity , and contour The vascular disorganization
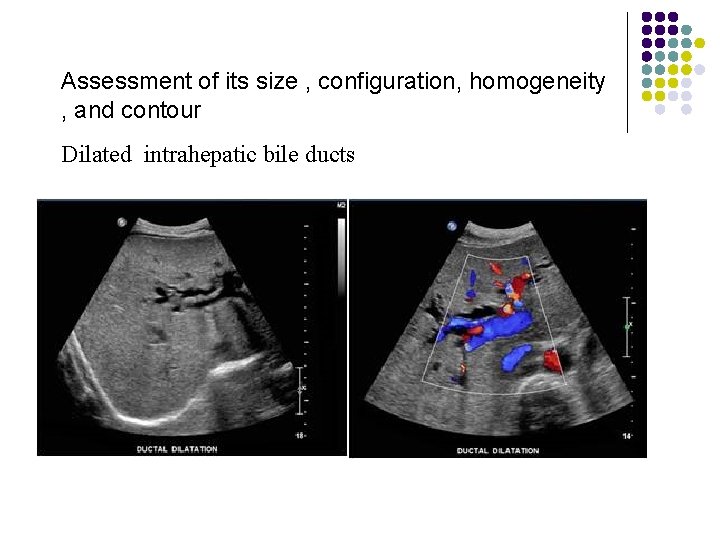
Assessment of its size , configuration, homogeneity , and contour Dilated intrahepatic bile ducts
Pathology of the Live Subsequent sections discuss the pathology of liver disease in the following categories : l Diffuse disease l Hepatic Tumors Benign disease Malignant disease l Abscess formation l Functional disease l Tranplantation l Vascular problems
Pathology of the Live Diffuse Fatty Infiltration US l increased sound attenuation =poor definition of posterior aspect of liver ( bright liver) l fine/coarsened hyperechogenicity (compared with kidney) l impaired visualization of borders of hepatic vessels l Attenuation of sound beam
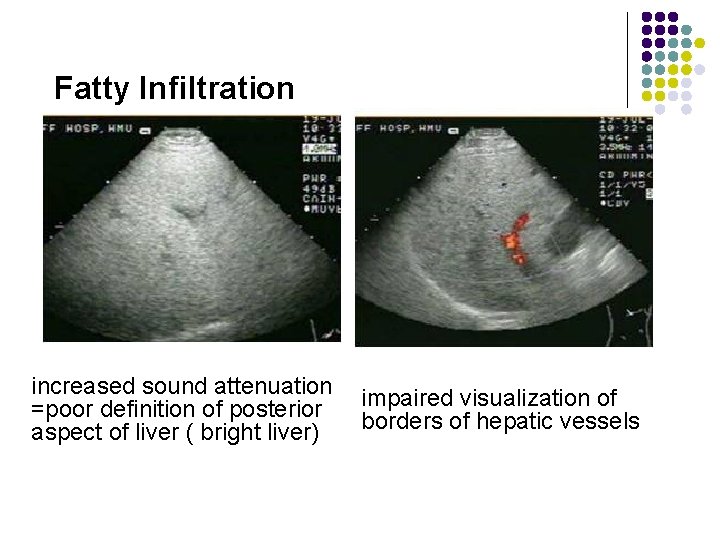
Fatty Infiltration increased sound attenuation =poor definition of posterior aspect of liver ( bright liver) impaired visualization of borders of hepatic vessels
Diffuse Fatty Infiltration—CT l l l Areas of lower attenuation than normal portal vein/IVC density Reversal of liver spleen density relationship (liver density is normal 612 HU greater than spleen) Hyperdense intrahepatic vessels
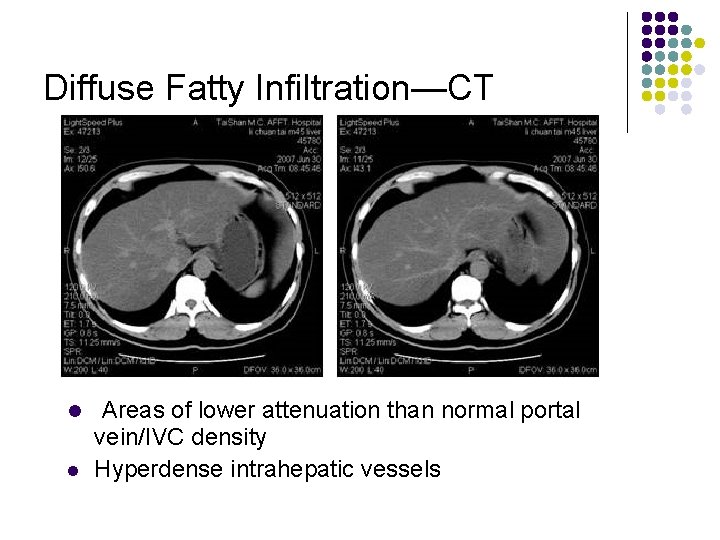
Diffuse Fatty Infiltration—CT l l Areas of lower attenuation than normal portal vein/IVC density Hyperdense intrahepatic vessels
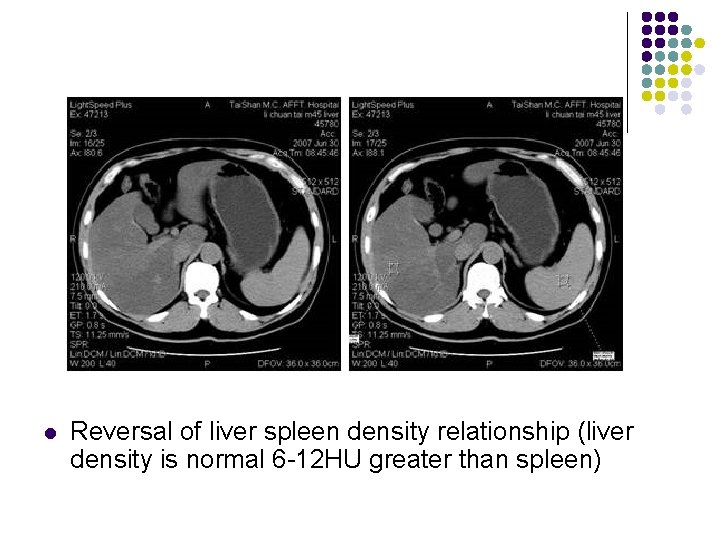
l Reversal of liver spleen density relationship (liver density is normal 6 -12 HU greater than spleen)
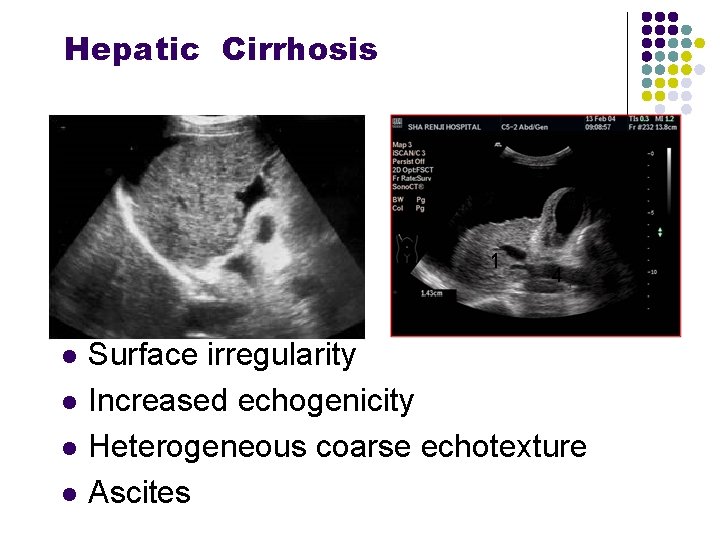
Hepatic Cirrhosis l l Surface irregularity Increased echogenicity Heterogeneous coarse echotexture Ascites
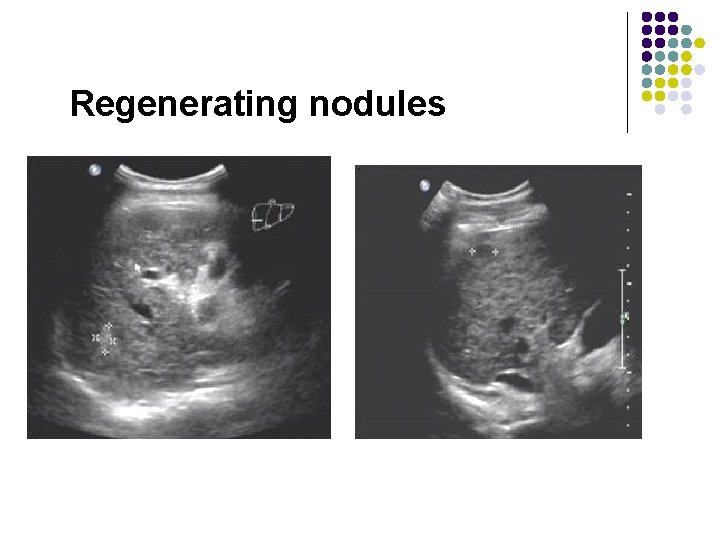
Regenerating nodules
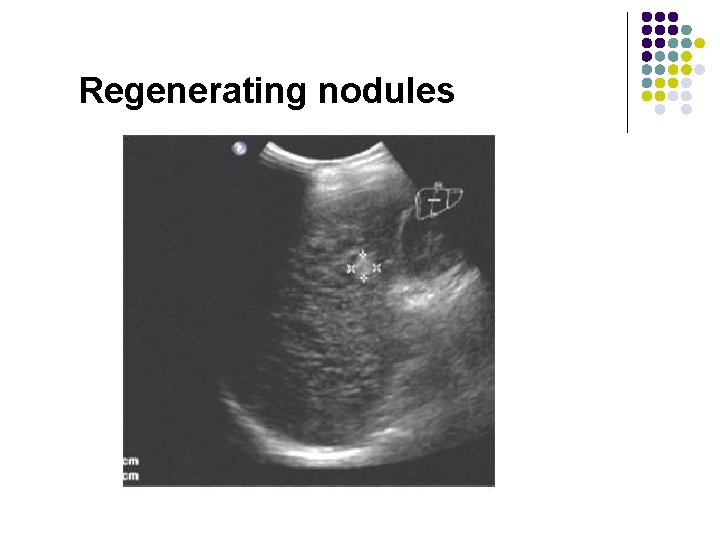
Regenerating nodules
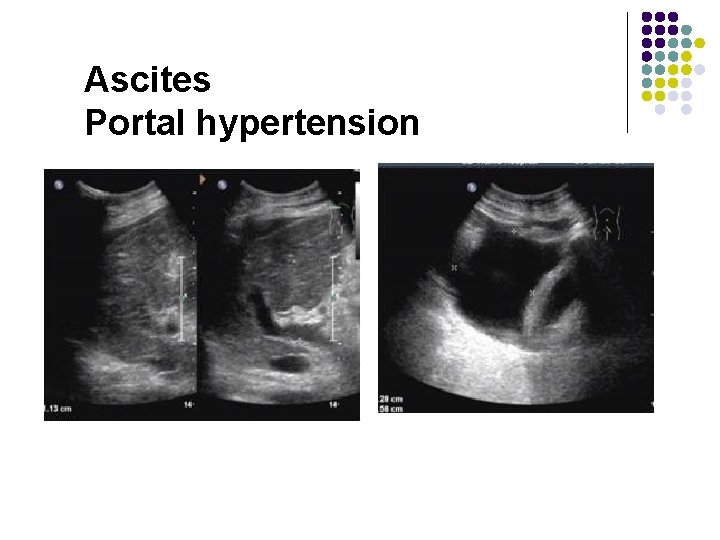
Ascites Portal hypertension
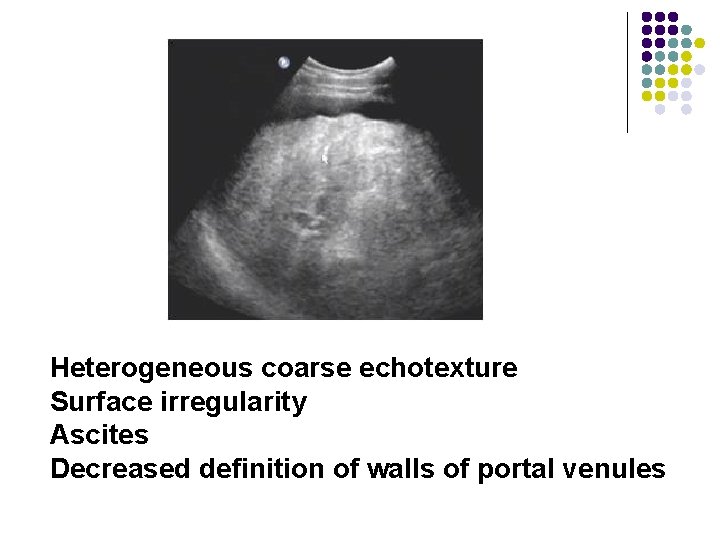
Heterogeneous coarse echotexture Surface irregularity Ascites Decreased definition of walls of portal venules
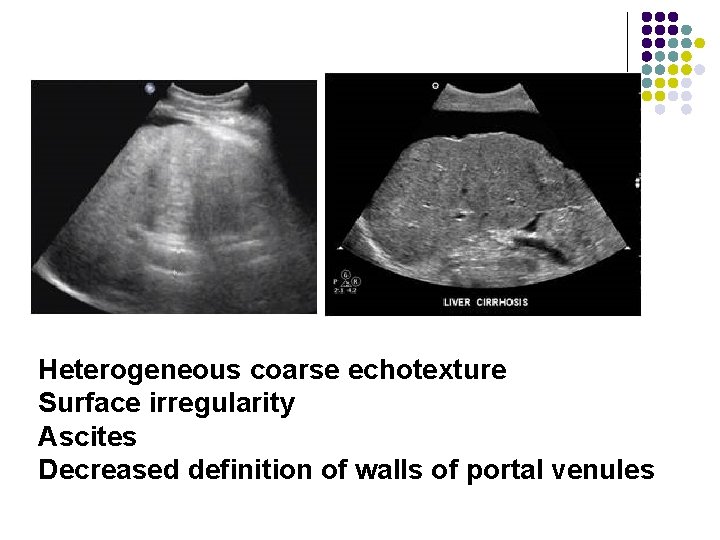
Heterogeneous coarse echotexture Surface irregularity Ascites Decreased definition of walls of portal venules
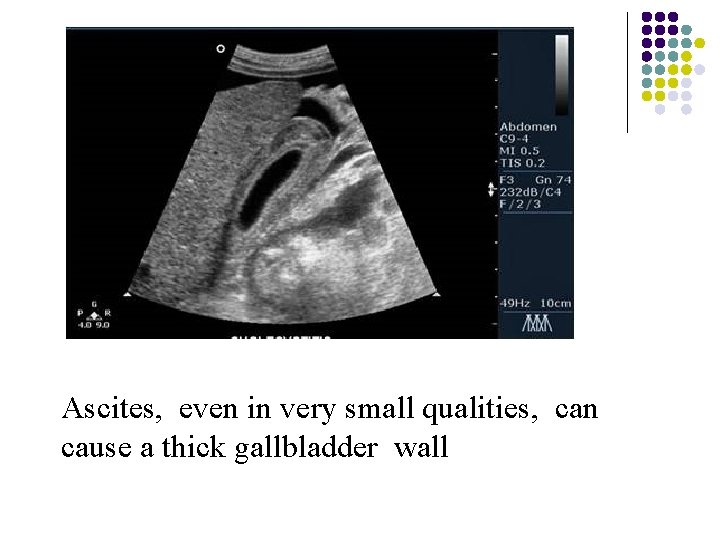
Ascites, even in very small qualities, can cause a thick gallbladder wall

Ascites
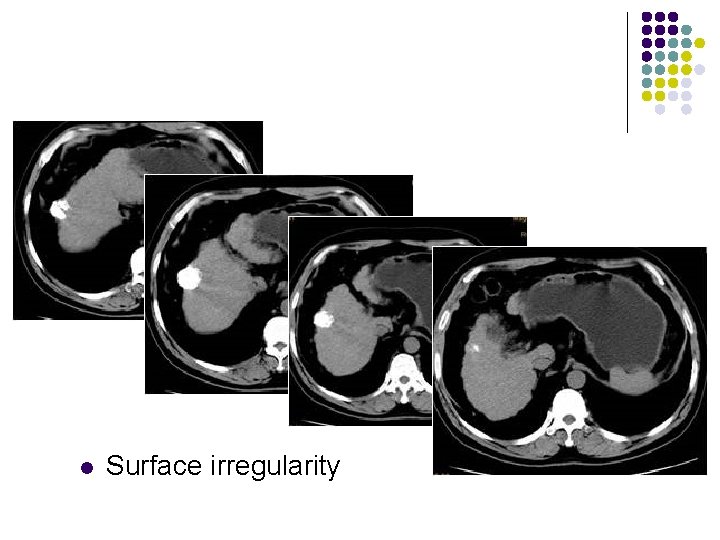
l Surface irregularity
Pathology of the Live Focal Hepatic Disease l Cystic Lesions l Hepatic cysts may be congenital or acquired , solitary , or multiple. Patients are often asymptomatic, except patients who have large cysts , which can compress the hepatic vasculature or ductal system.
Pathology of the Live Focal Hepatic Disease l Cystic Lesions within the liver include the following : l Simple or congenital hepatic cysts l Traumatic cysts l Parasitic cysts l Inflammatory cysts l Polycystic disease l Pseudo-cysts
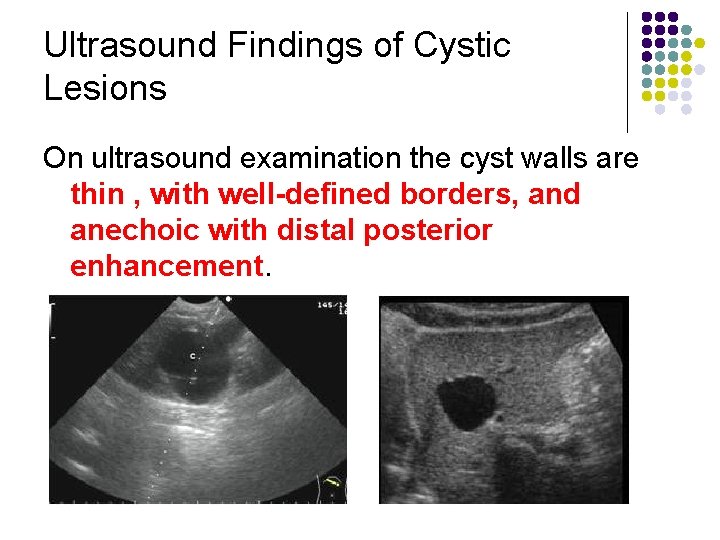
Ultrasound Findings of Cystic Lesions On ultrasound examination the cyst walls are thin , with well-defined borders, and anechoic with distal posterior enhancement.
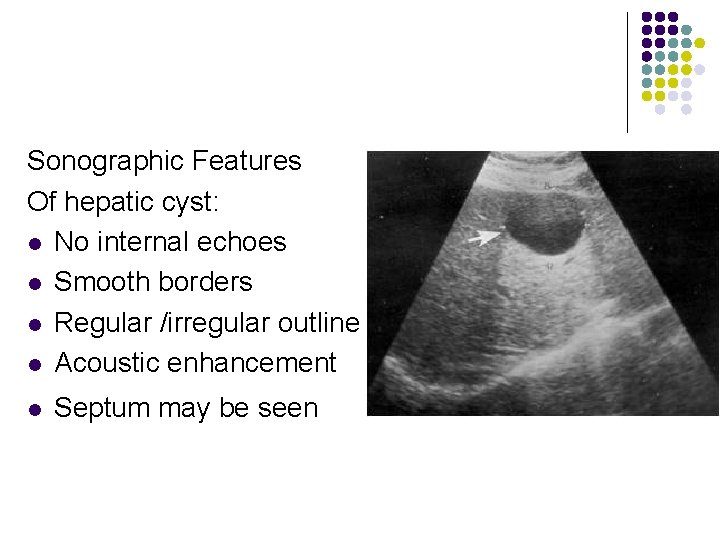
Sonographic Features Of hepatic cyst: l No internal echoes l Smooth borders l Regular /irregular outline l Acoustic enhancement l Septum may be seen
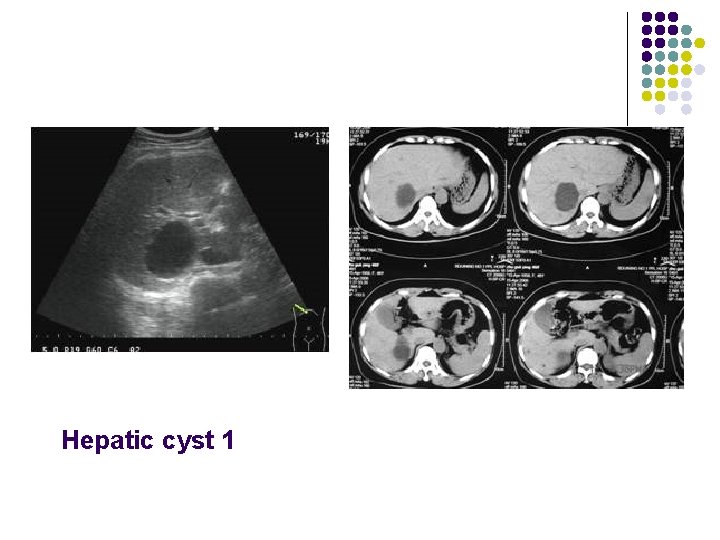
Hepatic cyst 1
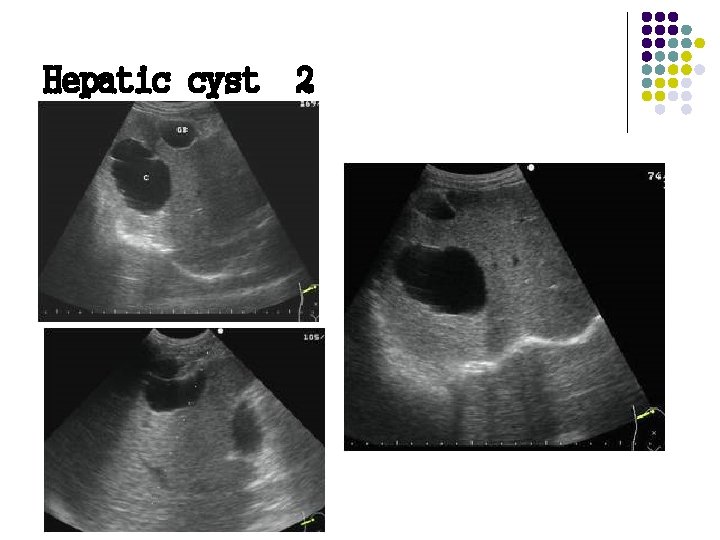
Hepatic cyst 2
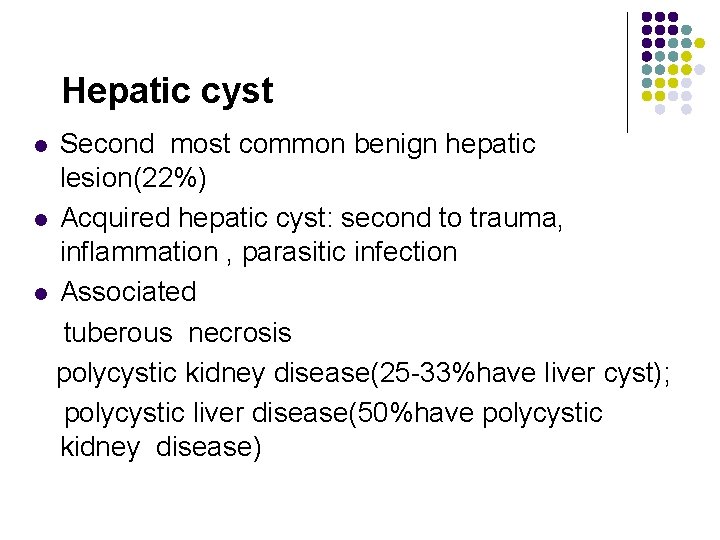
Hepatic cyst Second most common benign hepatic lesion(22%) l Acquired hepatic cyst: second to trauma, inflammation , parasitic infection l Associated tuberous necrosis polycystic kidney disease(25 -33%have liver cyst); polycystic liver disease(50%have polycystic kidney disease) l
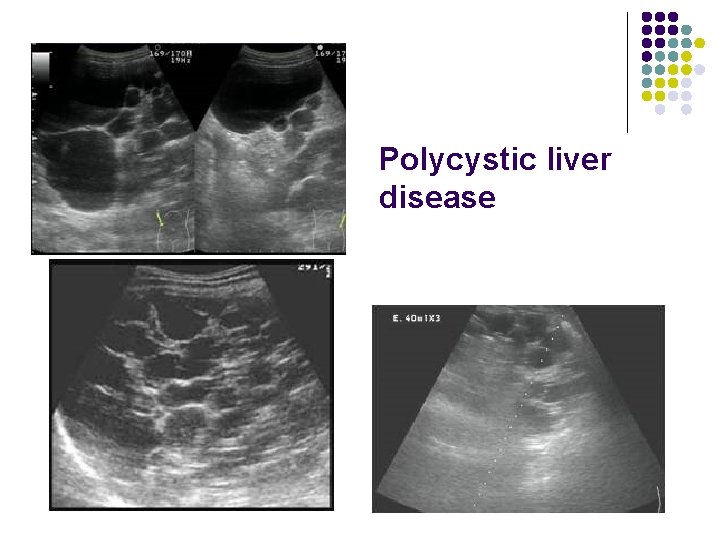
Polycystic liver disease
Hepatic abscess l l l Types pyogenic(88%) amebic(10%) fungal(2%)
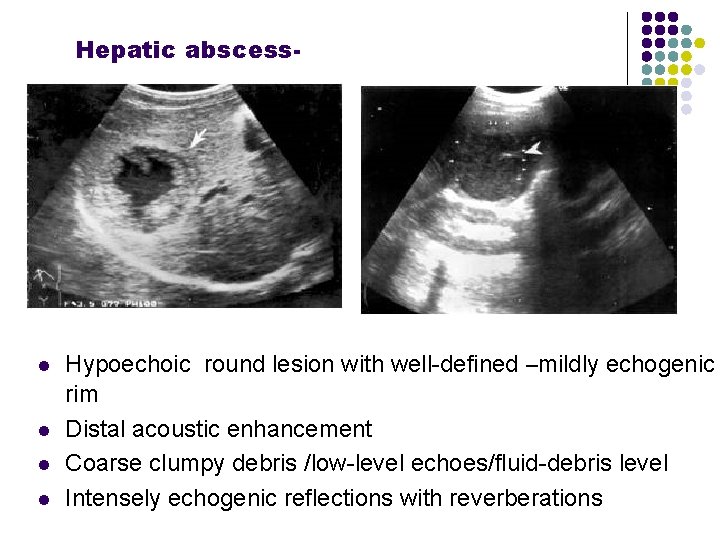
Hepatic abscess- l l Hypoechoic round lesion with well-defined –mildly echogenic rim Distal acoustic enhancement Coarse clumpy debris /low-level echoes/fluid-debris level Intensely echogenic reflections with reverberations
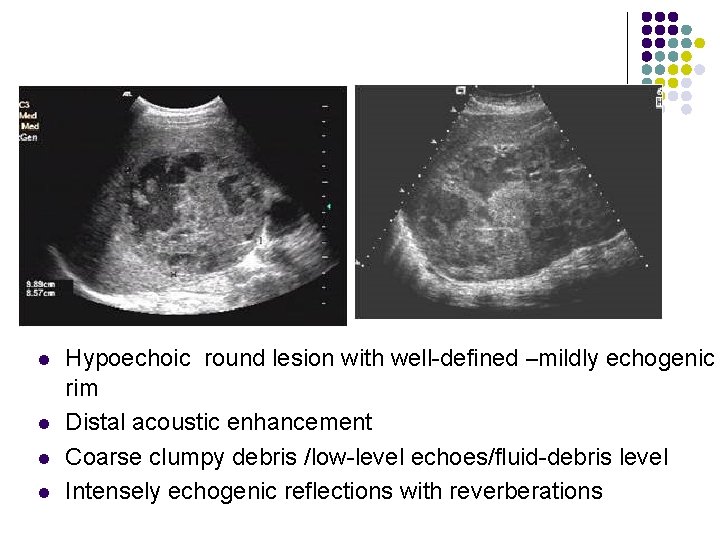
l l Hypoechoic round lesion with well-defined –mildly echogenic rim Distal acoustic enhancement Coarse clumpy debris /low-level echoes/fluid-debris level Intensely echogenic reflections with reverberations
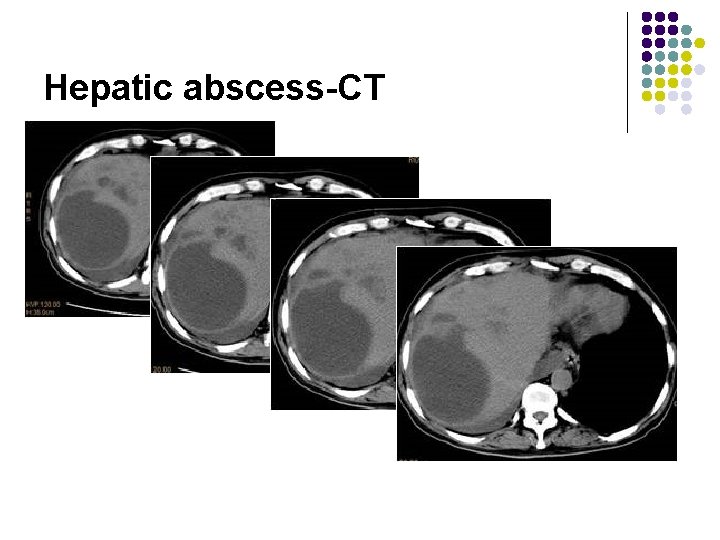
Hepatic abscess-CT
Pathology of the Live l Hepatic Tumors Benign disease Malignant disease
Pathology of Liver l l l Primary Hepatic Carcinoma (PHC) Metastases to liver Hepatic hemangioma
Hepatocellular Carcinoma(HCC) Primary Hepatic Carcinoma (PHC) l l Etiology: cirrhosis, hepatitis B and C infection and carcinogens Solitary, multifocal or more rarely diffusely infiltrating
Hepatocellular Carcinoma(HCC) l Growth pattern: l solitary massive (27 -59%): l bulk in one (most often right) lobe with satellite nodules multifocal small nodular (15 -25%): l small foci of usually <2 cm (up to 5 cm) in both hepatic lobes diffuse microscopic infiltrating form (10 -26%): l tiny indistinct nodules closely resembling cirrhosis Vascular supply: hepatic artery, portal vein in 6% l l l
HCC l l l l Metastases to: lung (most common = 8%), adrenal, lymph nodes, bone portal vein invasion (25 -48%) arterioportal shunting (4 -63%) invasion of hepatic vein (16%)/IVC (= Budd-Chiari syndrome) occasionally invasion of bile ducts calcifications in ordinary HCC (2 -25%); however, common in fibrolamellar (30 -40%) and sclerosing HCC hepatomegaly and ascites tumor fatty metamorphosis (2 -17%)
Sonographic Features of HCC l l l 86 -99% sensitivity; 90 -93% specificity; 65 -94% accuracy; Hyperechoic HCC(13%)due to fatty metamophosis or marked dilatation of sinusoids Hypoechoic HCC(26%)due to solid tumor HCC of mixed echogenicity (61%)due to nonliquefactive tumor necrosis
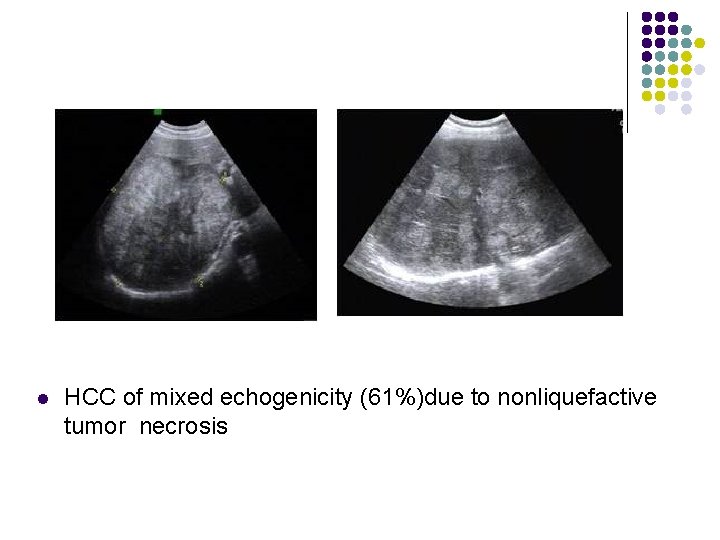
l HCC of mixed echogenicity (61%)due to nonliquefactive tumor necrosis
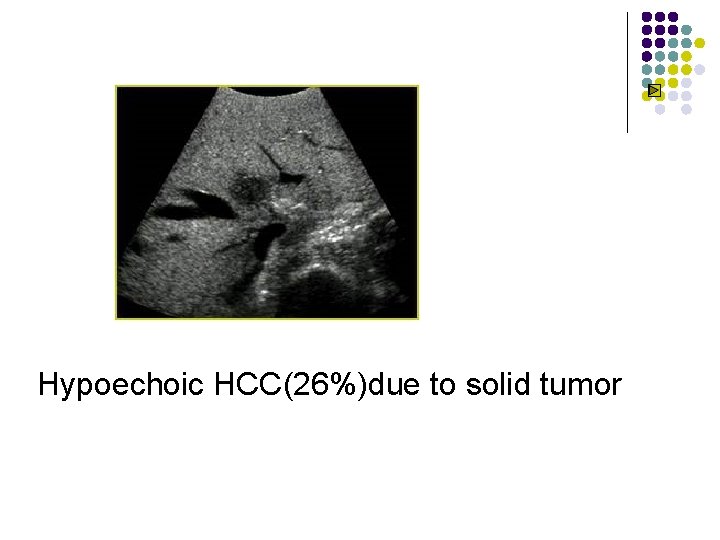
Hypoechoic HCC(26%)due to solid tumor
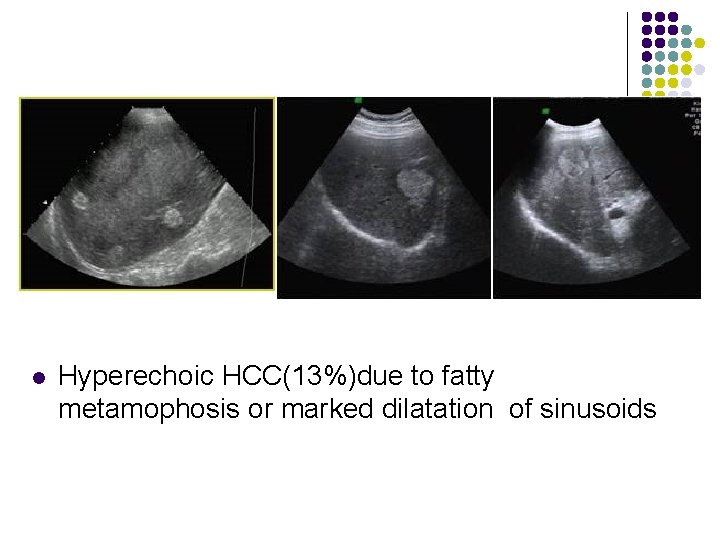
l Hyperechoic HCC(13%)due to fatty metamophosis or marked dilatation of sinusoids
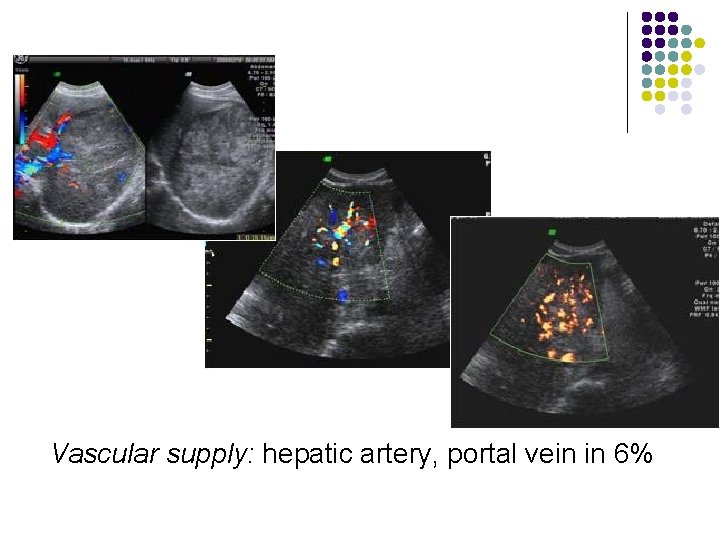
Vascular supply: hepatic artery, portal vein in 6%

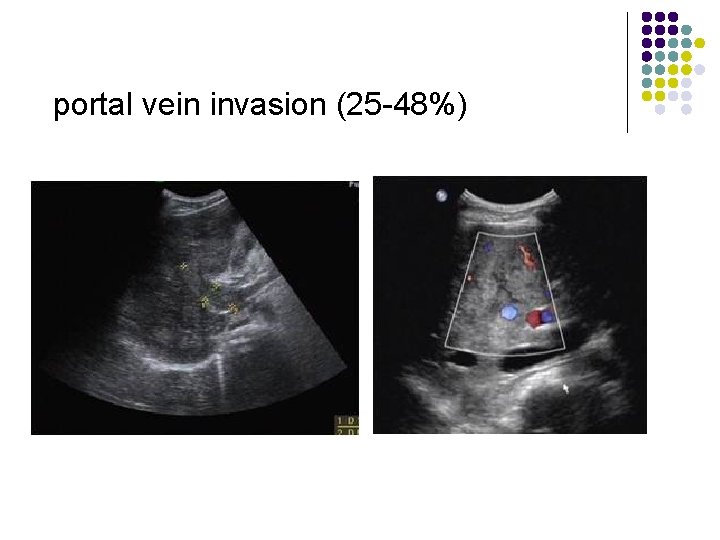
portal vein invasion (25 -48%)
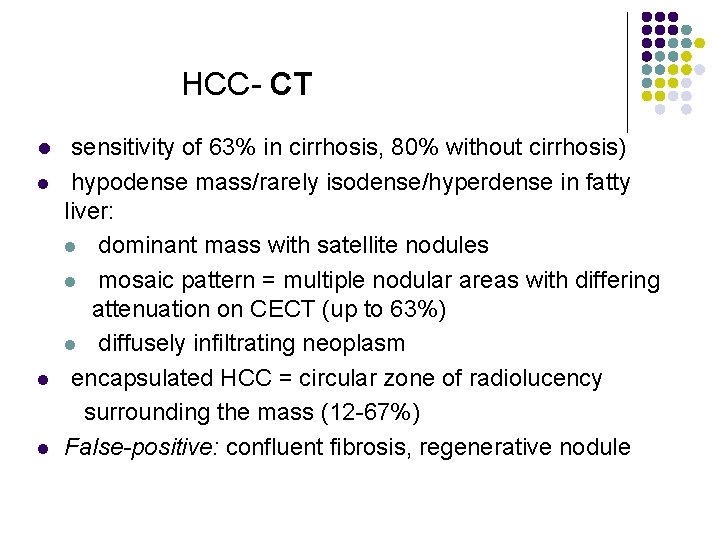
HCC- CT l l sensitivity of 63% in cirrhosis, 80% without cirrhosis) hypodense mass/rarely isodense/hyperdense in fatty liver: l dominant mass with satellite nodules l mosaic pattern = multiple nodular areas with differing attenuation on CECT (up to 63%) l diffusely infiltrating neoplasm encapsulated HCC = circular zone of radiolucency surrounding the mass (12 -67%) False-positive: confluent fibrosis, regenerative nodule
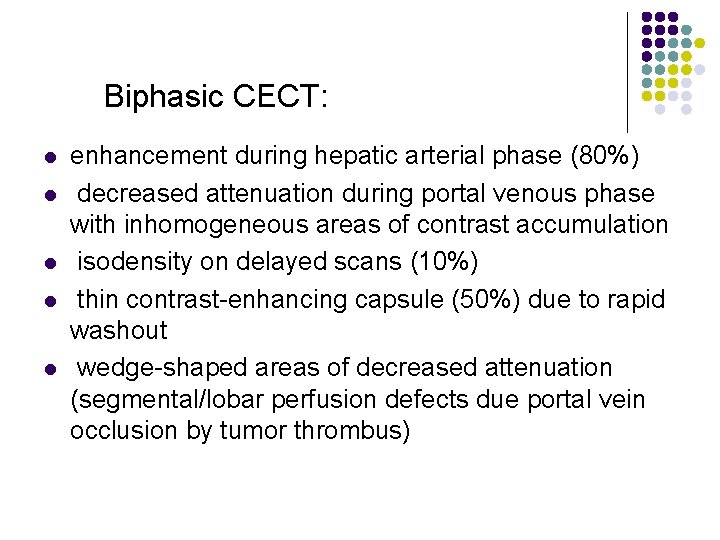
Biphasic CECT: l l l enhancement during hepatic arterial phase (80%) decreased attenuation during portal venous phase with inhomogeneous areas of contrast accumulation isodensity on delayed scans (10%) thin contrast-enhancing capsule (50%) due to rapid washout wedge-shaped areas of decreased attenuation (segmental/lobar perfusion defects due portal vein occlusion by tumor thrombus)
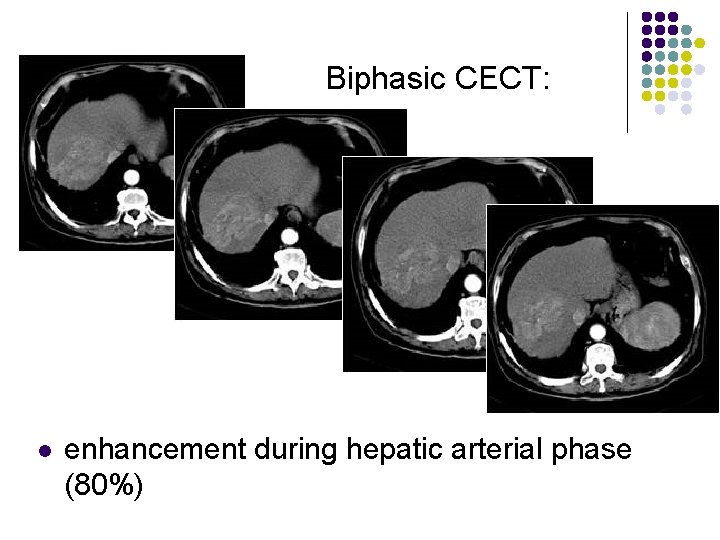
Biphasic CECT: l enhancement during hepatic arterial phase (80%)
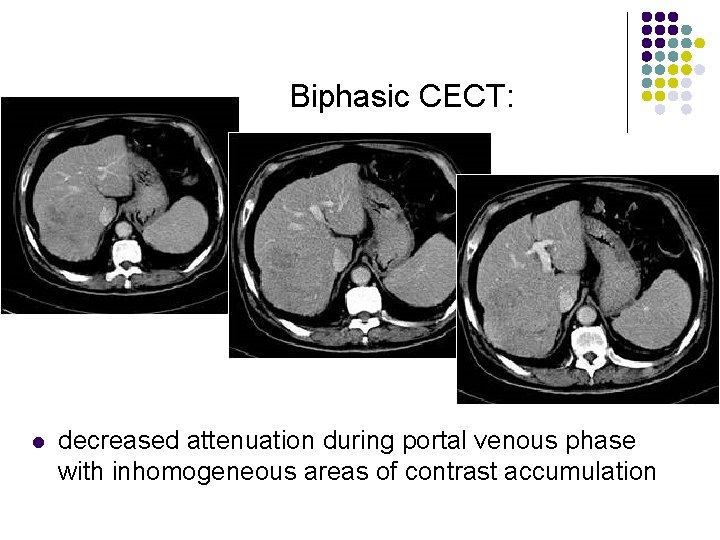
Biphasic CECT: l decreased attenuation during portal venous phase with inhomogeneous areas of contrast accumulation
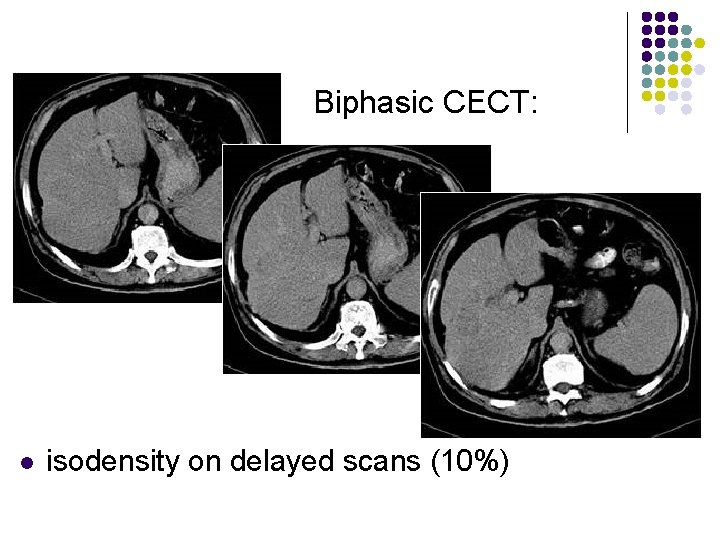
Biphasic CECT: l isodensity on delayed scans (10%)
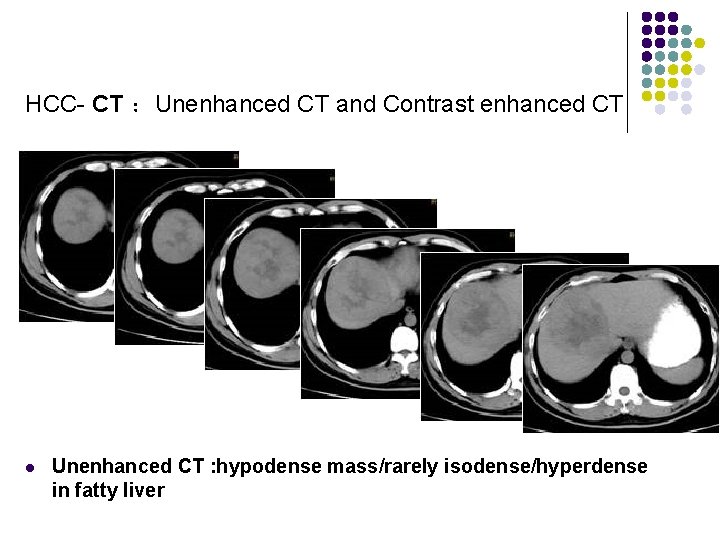
HCC- CT :Unenhanced CT and Contrast enhanced CT l Unenhanced CT : hypodense mass/rarely isodense/hyperdense in fatty liver
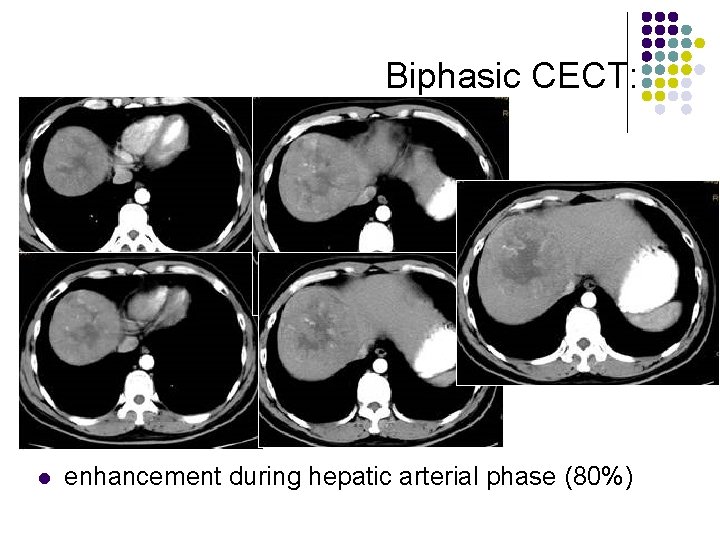
Biphasic CECT: l enhancement during hepatic arterial phase (80%)
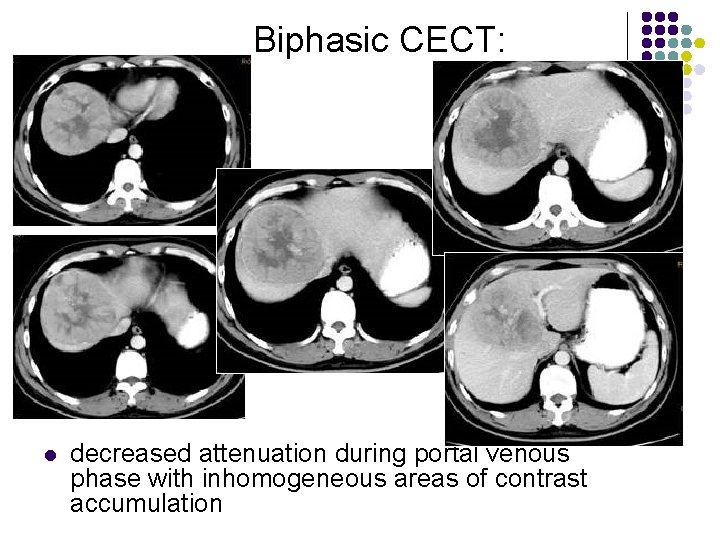
Biphasic CECT: l decreased attenuation during portal venous phase with inhomogeneous areas of contrast accumulation
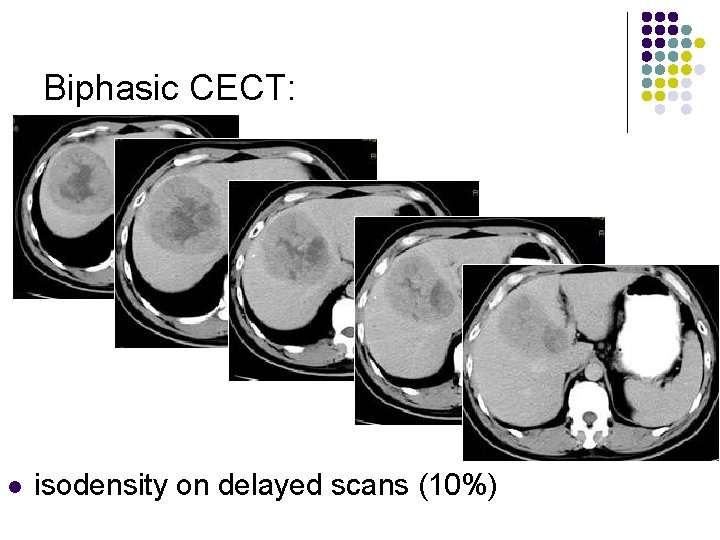
Biphasic CECT: l isodensity on delayed scans (10%)
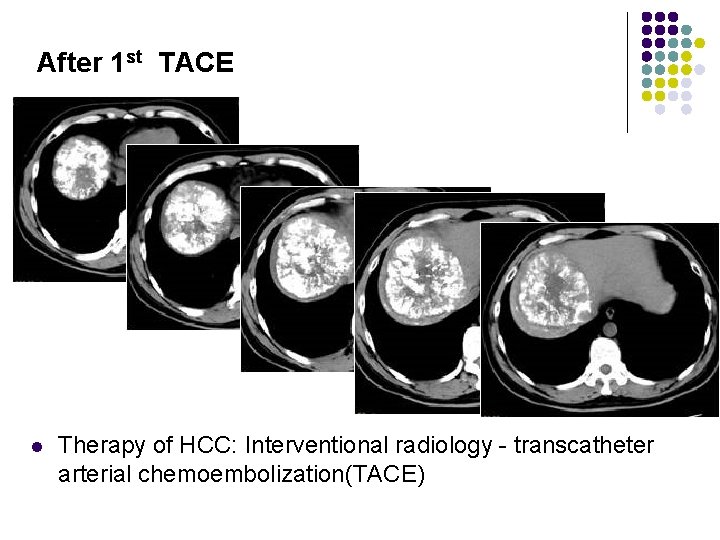
After 1 st TACE l Therapy of HCC: Interventional radiology - transcatheter arterial chemoembolization(TACE)
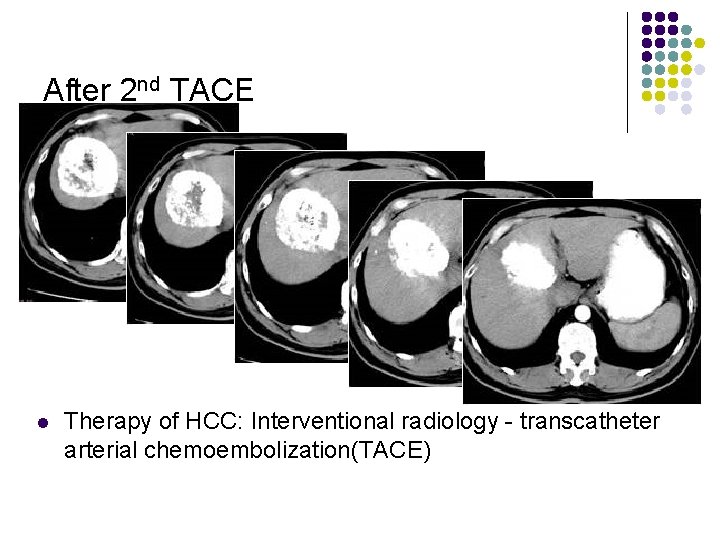
After 2 nd TACE l Therapy of HCC: Interventional radiology - transcatheter arterial chemoembolization(TACE)
Metastases to liver l l l Organ of origin: colon(42%); stomach(23%); pancreas(21%); breast(14%); lung(13%) Number : multiple(98%); solitary(2%) “Bullseye”:An echogenic center with a surrounding echopenic area Echopenic : Less echogenic than the surrounding liver Echogenic More echogenic than the surrounding liver
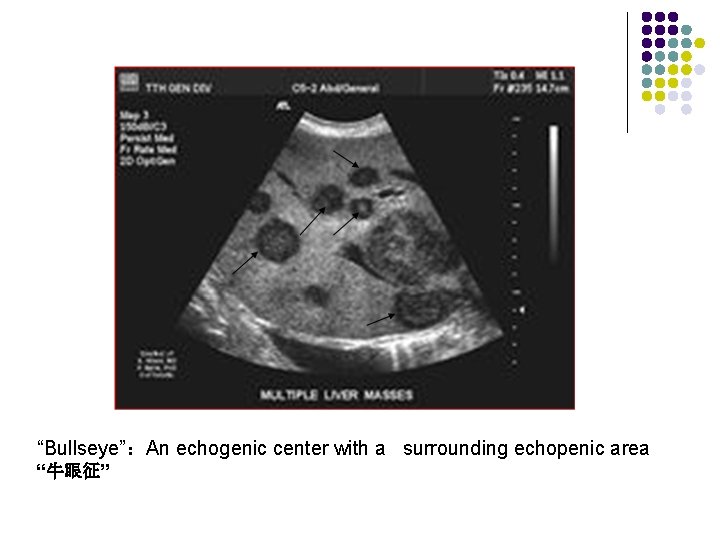
“Bullseye”:An echogenic center with a surrounding echopenic area “牛眼征”
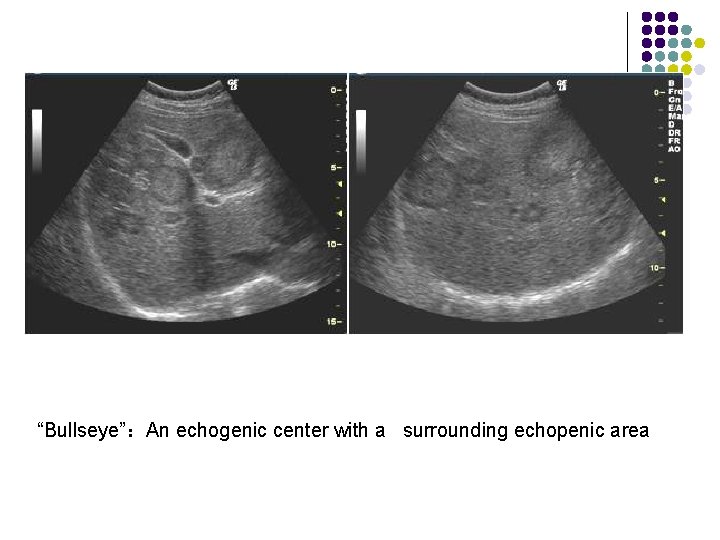
“Bullseye”:An echogenic center with a surrounding echopenic area
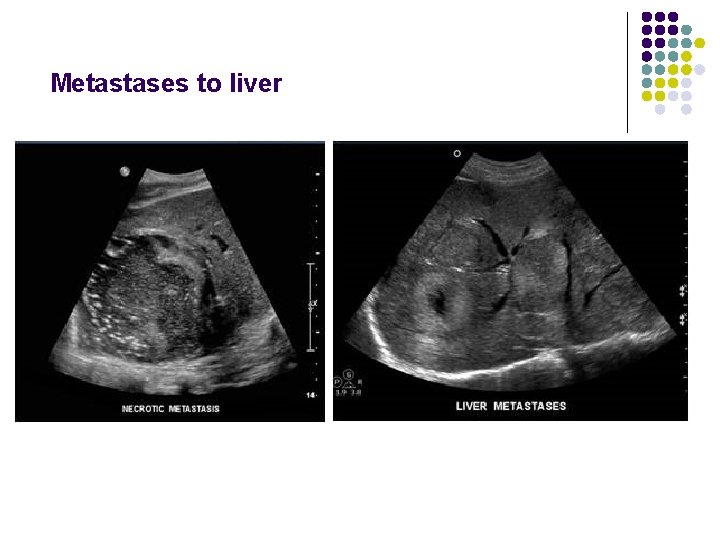
Metastases to liver
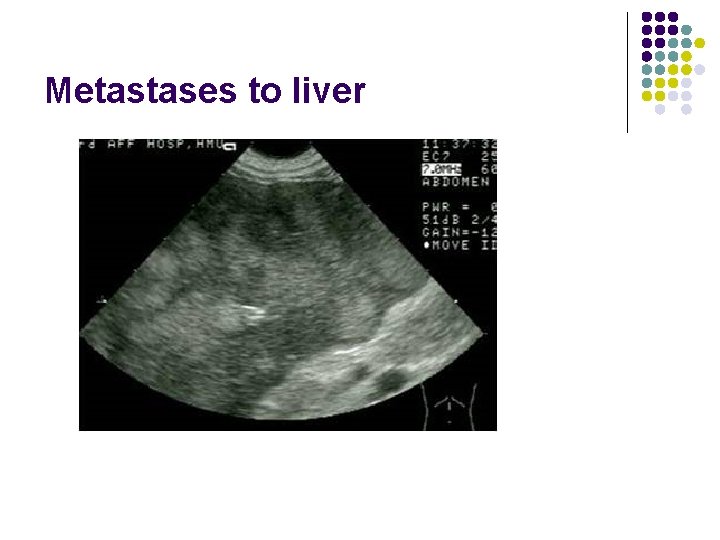
Metastases to liver
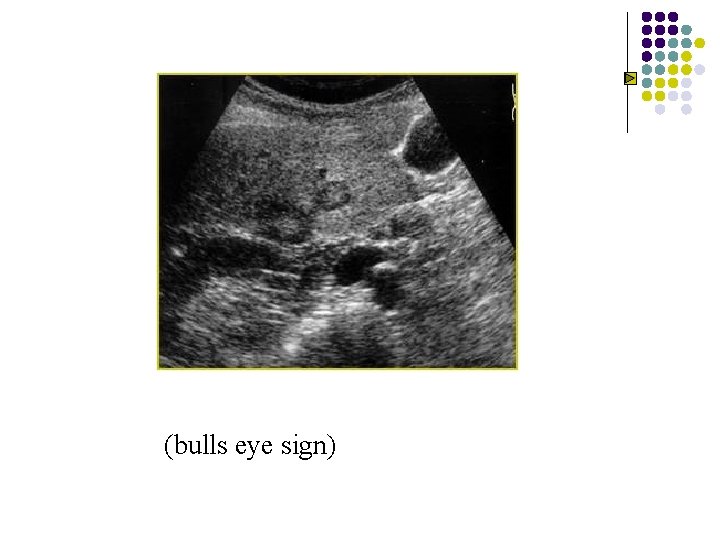
(bulls eye sign)
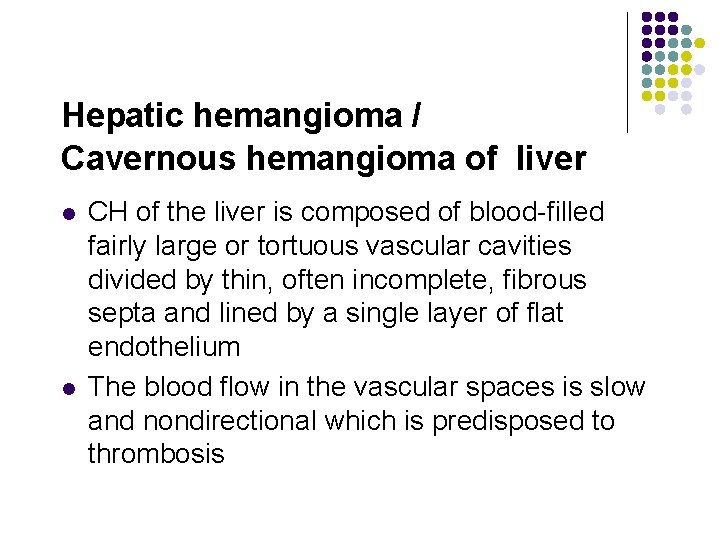
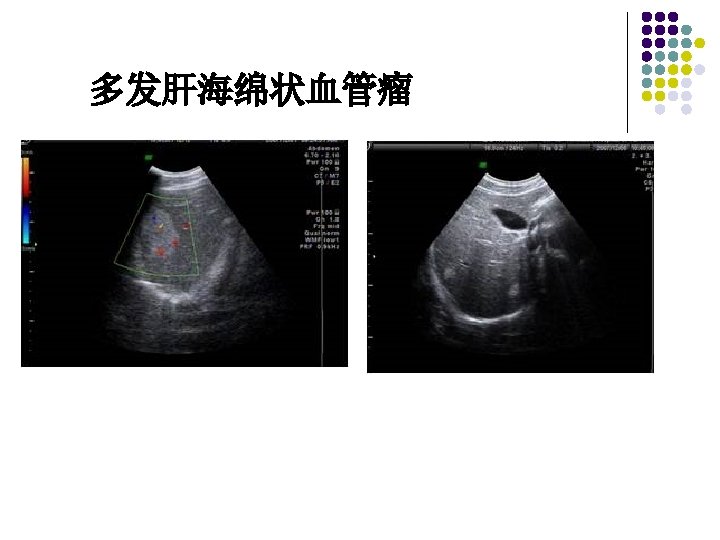
Hepatic hemangioma / Cavernous hemangioma of liver l l CH of the liver is composed of blood-filled fairly large or tortuous vascular cavities divided by thin, often incomplete, fibrous septa and lined by a single layer of flat endothelium The blood flow in the vascular spaces is slow and nondirectional which is predisposed to thrombosis
Ultrasonic features of Hepatic hemangioma l l l Uniformly hyperechoic mass(60 -70%) Inhomogeneous hypoechoic mass (up to 40%) Homogeneous(58 -73%) /heterogeneous May show acoustic enhancement(37 -77%) Unchanged in size/appearance(82)on 1 -to-6 year follow-up No Doppler signals/signals with peak velocity of <50 cm/cm
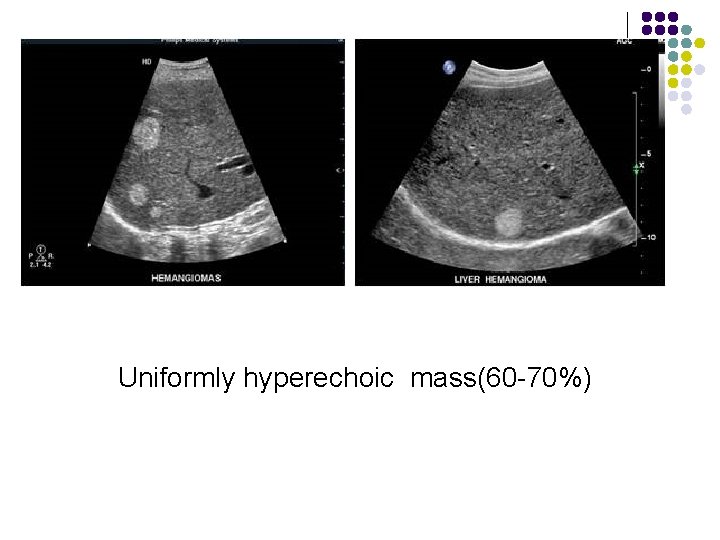
。 Uniformly hyperechoic mass(60 -70%)
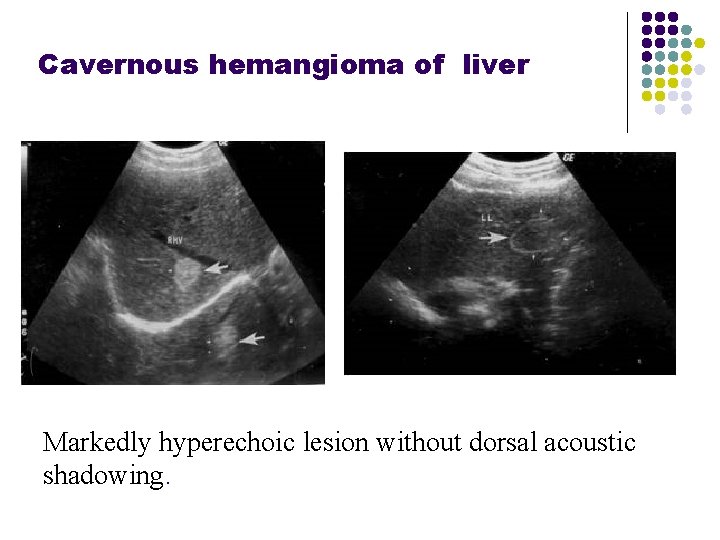
Cavernous hemangioma of liver Markedly hyperechoic lesion without dorsal acoustic shadowing.
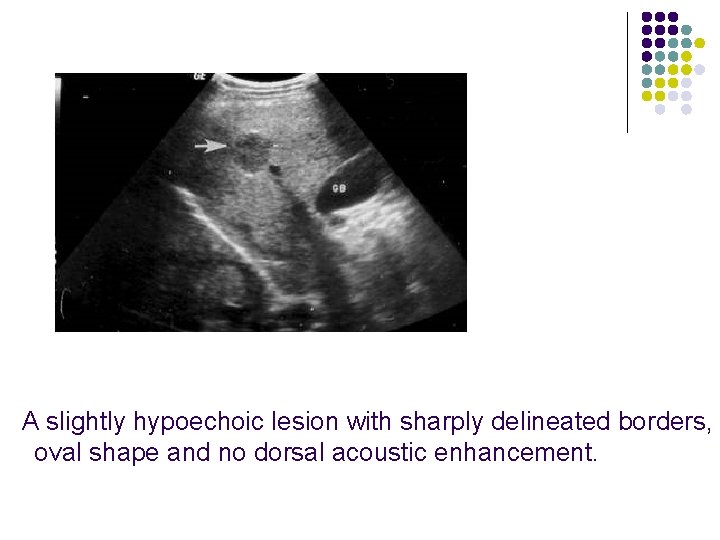
A slightly hypoechoic lesion with sharply delineated borders, oval shape and no dorsal acoustic enhancement.
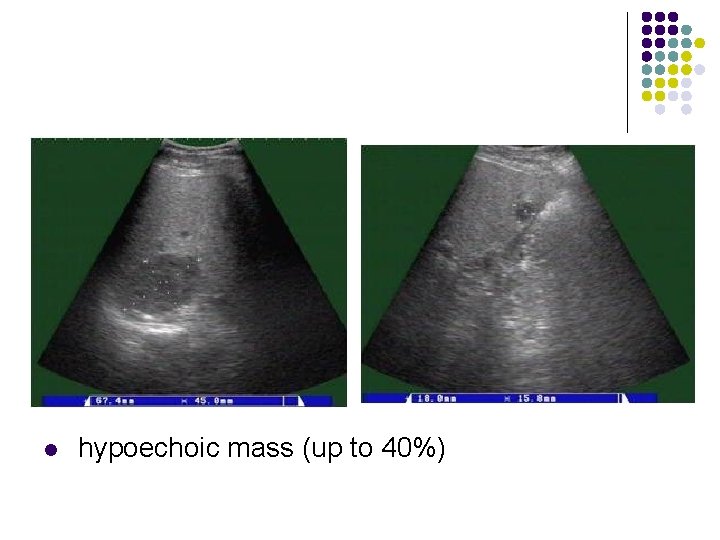
l hypoechoic mass (up to 40%)

- Slides: 124