Abdominal and Genitourinary Trauma Steve Lan September 25
Abdominal and Genitourinary Trauma Steve Lan September 25, 2003
Abdominal Trauma l Anatomy l History/Examination l Investigations l Blunt Trauma l Penetrating Trauma
Principles l Two questions: – Who needs an OR? – How fast do they need it? l Focus of history, physical exam and investigations

Ouch…
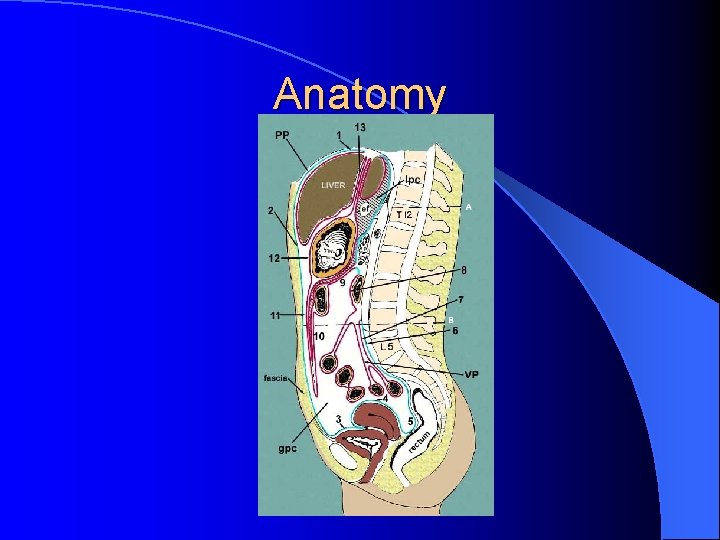
Anatomy
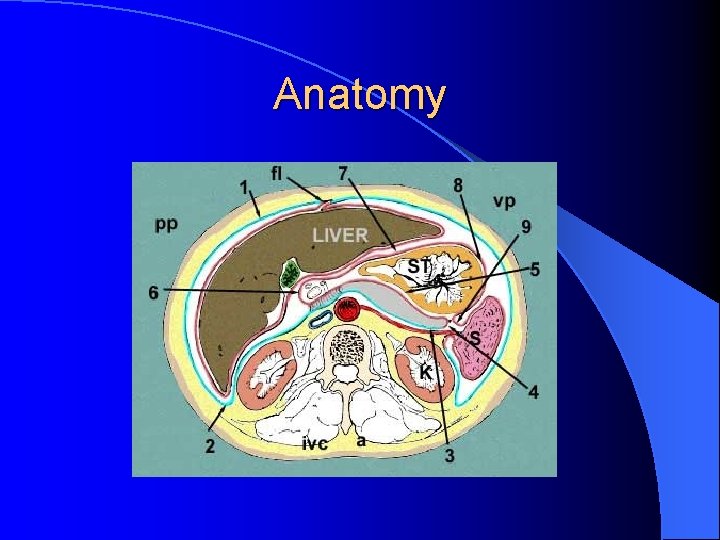
Anatomy
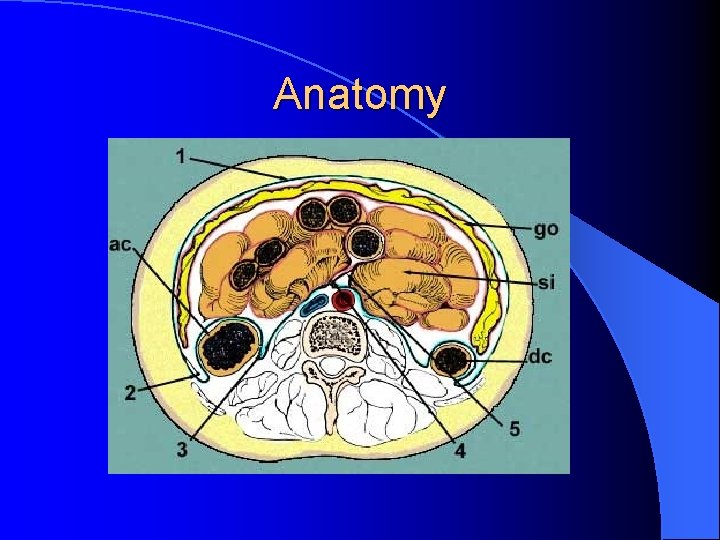
Anatomy
History l ABCDE’s l Often limited but focus on mechanism – Blunt vs penetrating – Associated injuries l Radiation of pain – – Scapula – irritation of hemidiaphragm – Testicle – irritation of retroperitoneum
Physical l Vitals l Soft/rigid/distension, bowel sounds l Turner’s (flank bruising), Cullen’s (bruising around umbilicus) **takes 12 h – several days to show l Entry/exit wounds l Rectal l Serial exams
Case #1 l 30 yo male, PMHx – 0 l MVA - Head on collision, 60 km/h l No air bags, lap belt l What type of abdo injury is this?
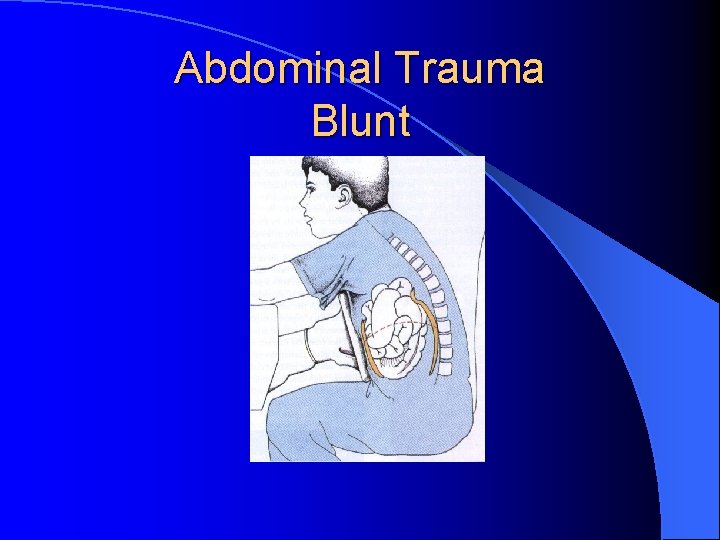
Abdominal Trauma Blunt
Blunt Abdominal Trauma l Greater mortality than penetrating – Occult injuries and associated with other trauma l Difficult to assess – ? history – Altered LOC – Other injuries – Etc.
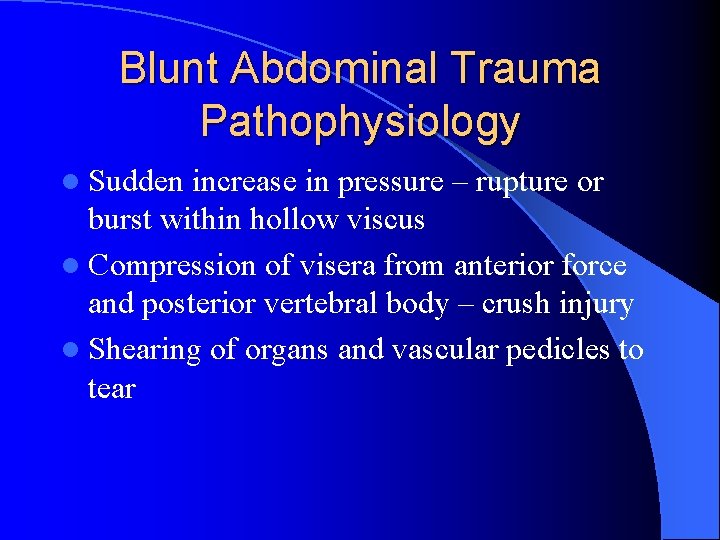
Blunt Abdominal Trauma Pathophysiology l Sudden increase in pressure – rupture or burst within hollow viscus l Compression of visera from anterior force and posterior vertebral body – crush injury l Shearing of organs and vascular pedicles to tear
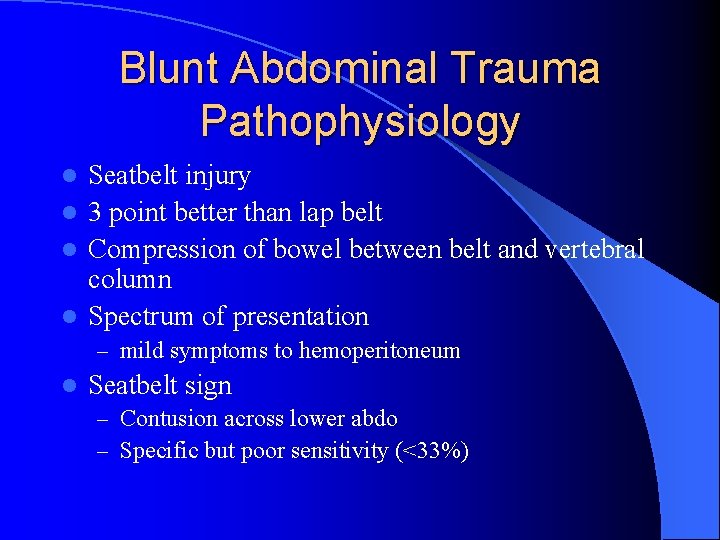
Blunt Abdominal Trauma Pathophysiology Seatbelt injury l 3 point better than lap belt l Compression of bowel between belt and vertebral column l Spectrum of presentation l – mild symptoms to hemoperitoneum l Seatbelt sign – Contusion across lower abdo – Specific but poor sensitivity (<33%)
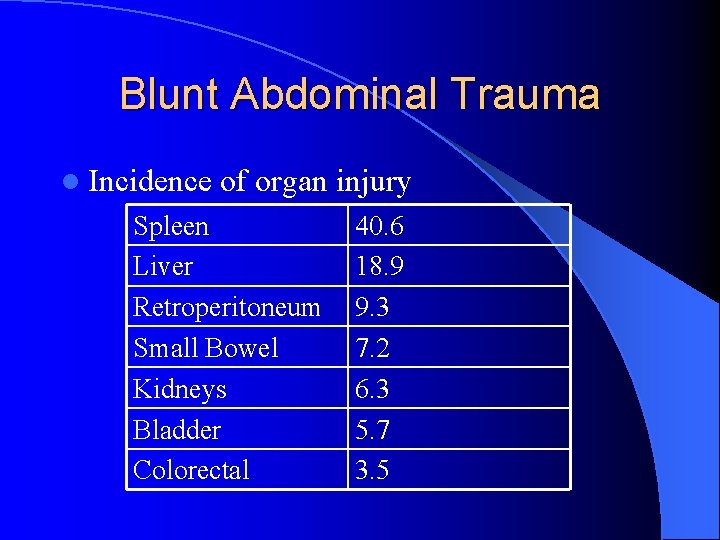
Blunt Abdominal Trauma l Incidence of organ injury Spleen Liver Retroperitoneum Small Bowel Kidneys Bladder Colorectal 40. 6 18. 9 9. 3 7. 2 6. 3 5. 7 3. 5
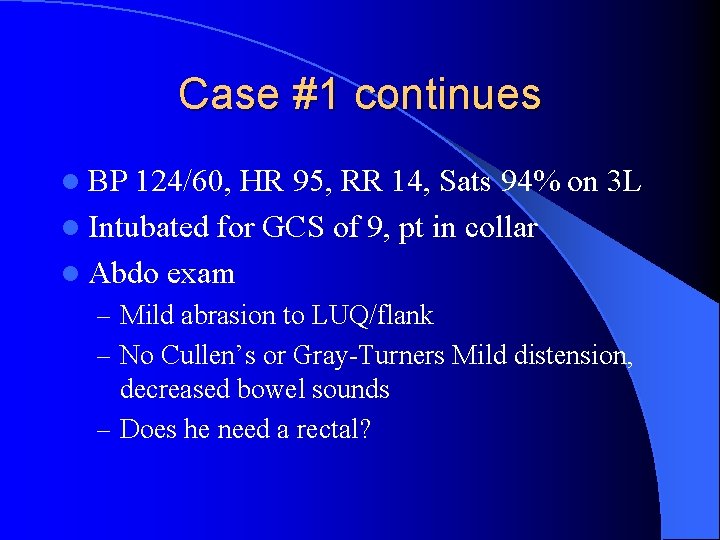
Case #1 continues l BP 124/60, HR 95, RR 14, Sats 94% on 3 L l Intubated for GCS of 9, pt in collar l Abdo exam – Mild abrasion to LUQ/flank – No Cullen’s or Gray-Turners Mild distension, decreased bowel sounds – Does he need a rectal?
“Fingers and tubes in every orifice” “The only reason not to do a rectal, is if there is no rectum or if you don’t have a finger” Hmmm? ? ?
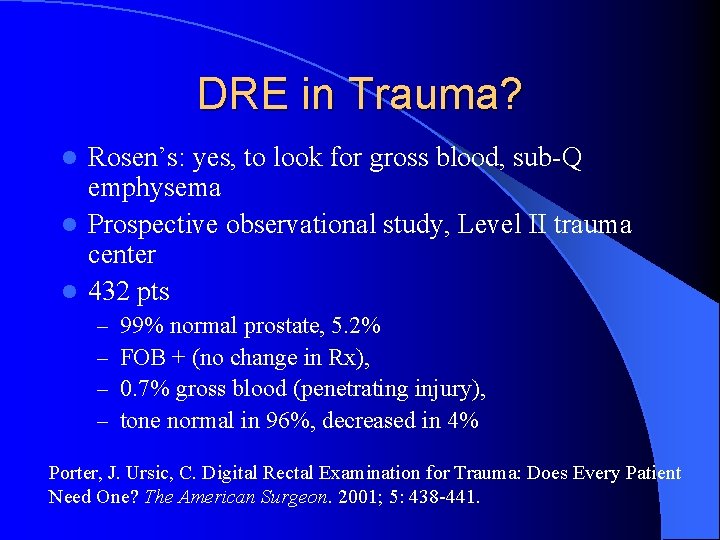
DRE in Trauma? Rosen’s: yes, to look for gross blood, sub-Q emphysema l Prospective observational study, Level II trauma center l 432 pts l – – 99% normal prostate, 5. 2% FOB + (no change in Rx), 0. 7% gross blood (penetrating injury), tone normal in 96%, decreased in 4% Porter, J. Ursic, C. Digital Rectal Examination for Trauma: Does Every Patient Need One? The American Surgeon. 2001; 5: 438 -441.
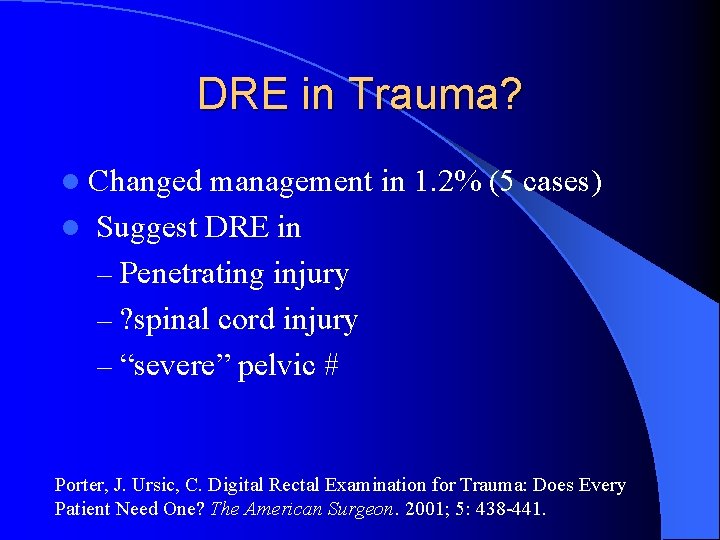
DRE in Trauma? l Changed management in 1. 2% (5 cases) l Suggest DRE in – Penetrating injury – ? spinal cord injury – “severe” pelvic # Porter, J. Ursic, C. Digital Rectal Examination for Trauma: Does Every Patient Need One? The American Surgeon. 2001; 5: 438 -441.
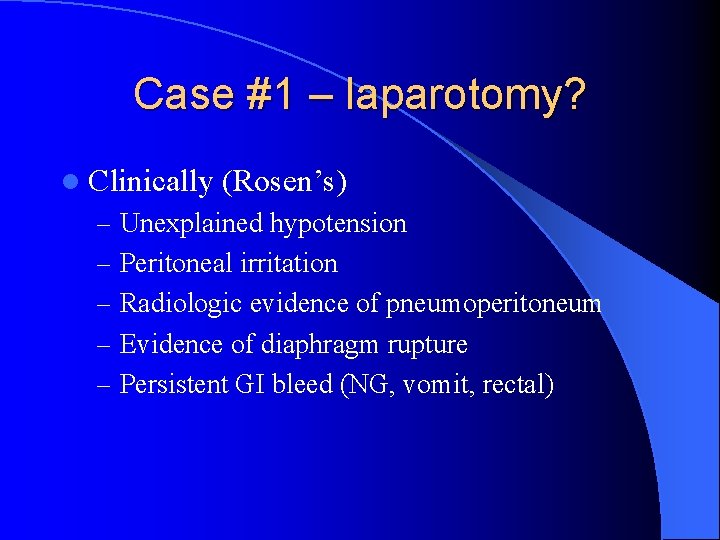
Case #1 – laparotomy? l Clinically (Rosen’s) – Unexplained hypotension – Peritoneal irritation – Radiologic evidence of pneumoperitoneum – Evidence of diaphragm rupture – Persistent GI bleed (NG, vomit, rectal)
Case #1 – Further Investigations l “What labs do you want doctor? ”
Abdominal Trauma Investigations: Labs l Most not too helpful acutely l Lipase/amylase can’t rule in/out pancreatic injury l Same with LFTs l What about in pediatric trauma?
Case #1 - Radiology l FAST or CT abdo? (DPL not used here in Calgary)
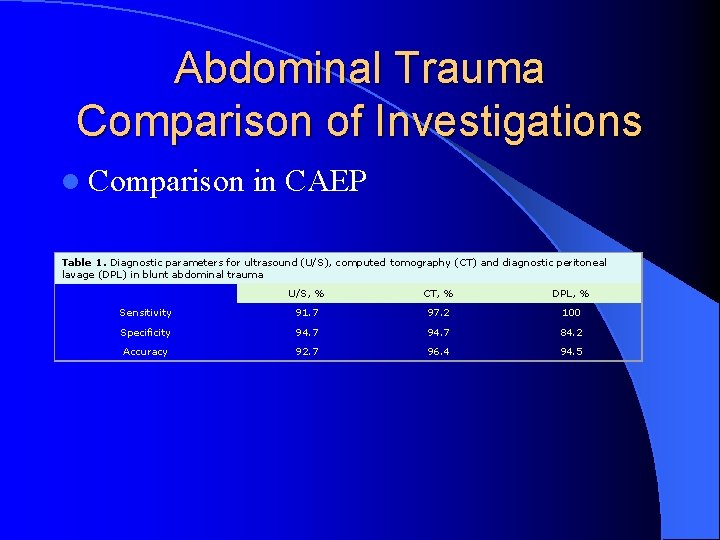
Abdominal Trauma Comparison of Investigations l Comparison in CAEP Table 1. Diagnostic parameters for ultrasound (U/S), computed tomography (CT) and diagnostic peritoneal lavage (DPL) in blunt abdominal trauma U/S, % CT, % DPL, % Sensitivity 91. 7 97. 2 100 Specificity 94. 7 84. 2 Accuracy 92. 7 96. 4 94. 5
Abdominal Trauma Investigations: FAST l Free fluid after blunt trauma – perihepatic and hepatorenal space (Morrison’s pouch) – perisplenic – pelvis (Pouch of Douglas) – pericardium l Does not look at solid organs, retroperitoneum, diaphragm
Abdominal Trauma l FAST exam of pelvis
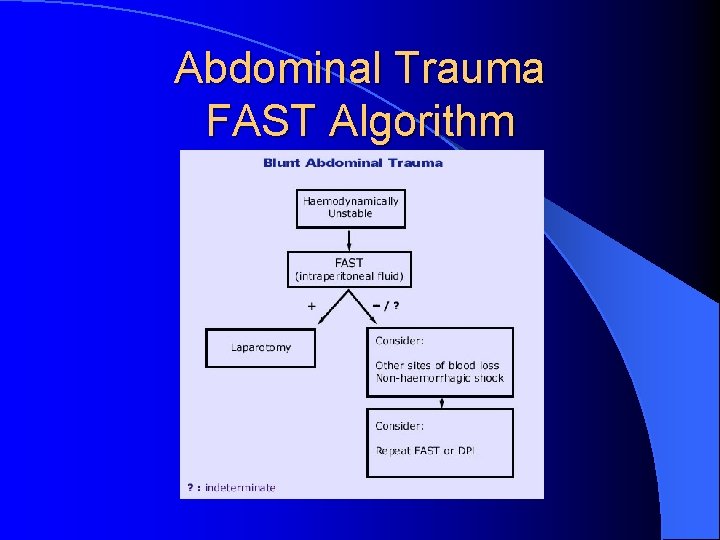
Abdominal Trauma FAST Algorithm
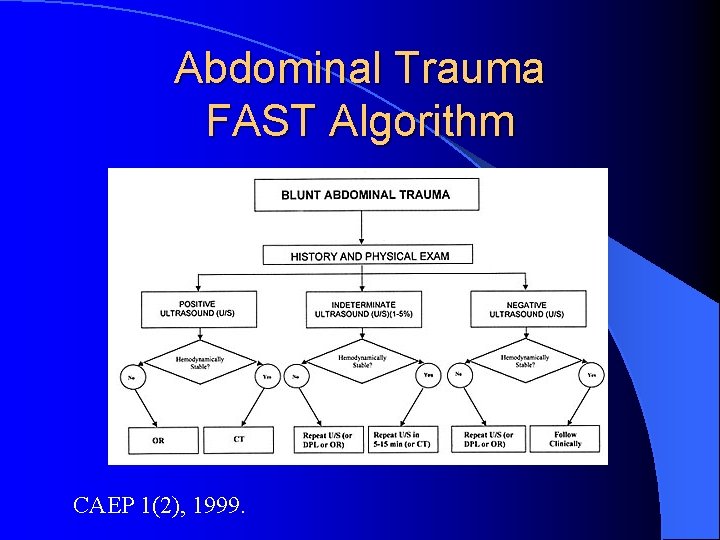
Abdominal Trauma FAST Algorithm CAEP 1(2), 1999.
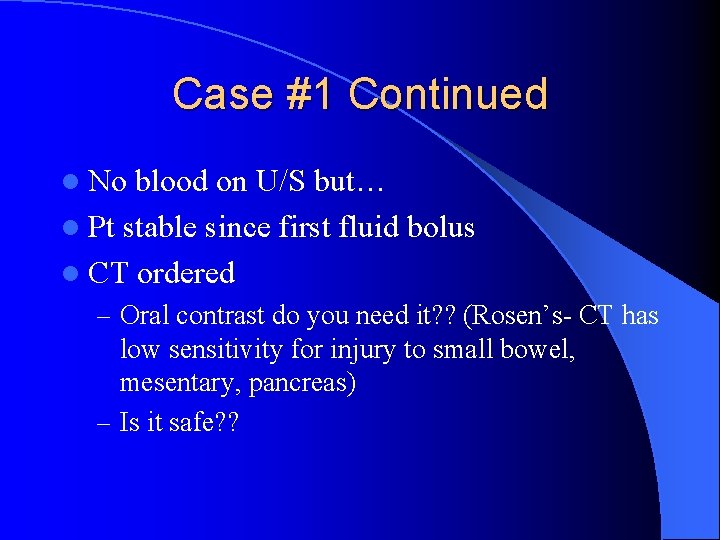
Case #1 Continued l No blood on U/S but… l Pt stable since first fluid bolus l CT ordered – Oral contrast do you need it? ? (Rosen’s- CT has low sensitivity for injury to small bowel, mesentary, pancreas) – Is it safe? ?
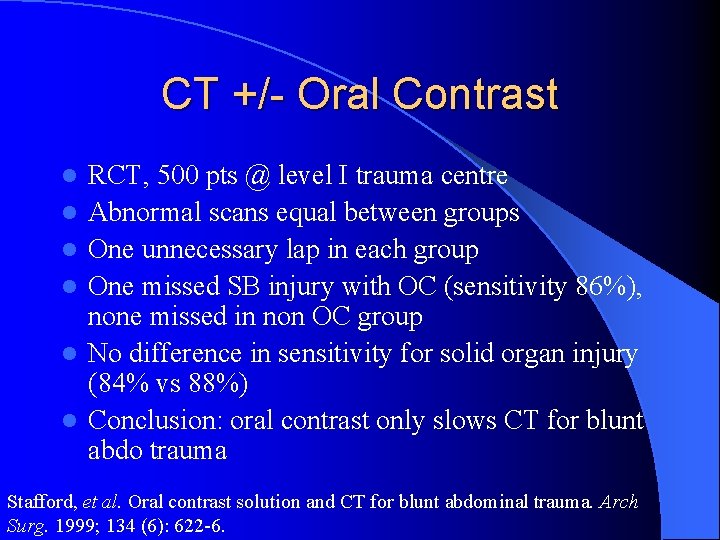
CT +/- Oral Contrast l l l RCT, 500 pts @ level I trauma centre Abnormal scans equal between groups One unnecessary lap in each group One missed SB injury with OC (sensitivity 86%), none missed in non OC group No difference in sensitivity for solid organ injury (84% vs 88%) Conclusion: oral contrast only slows CT for blunt abdo trauma Stafford, et al. Oral contrast solution and CT for blunt abdominal trauma. Arch Surg. 1999; 134 (6): 622 -6.
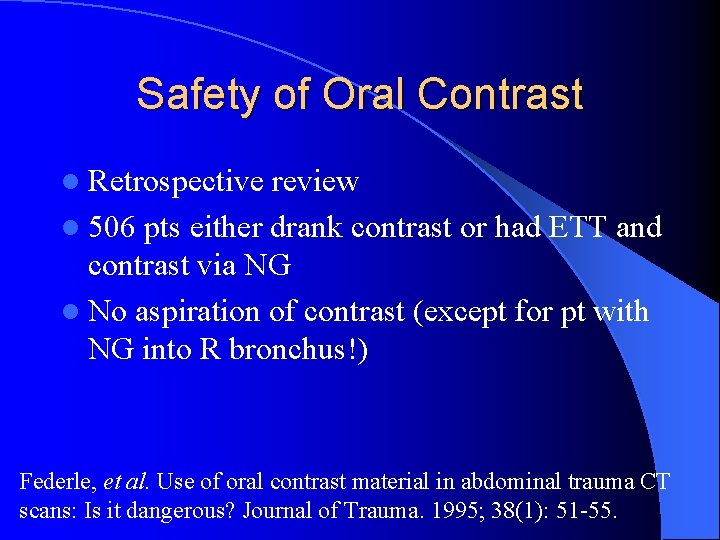
Safety of Oral Contrast l Retrospective review l 506 pts either drank contrast or had ETT and contrast via NG l No aspiration of contrast (except for pt with NG into R bronchus!) Federle, et al. Use of oral contrast material in abdominal trauma CT scans: Is it dangerous? Journal of Trauma. 1995; 38(1): 51 -55.
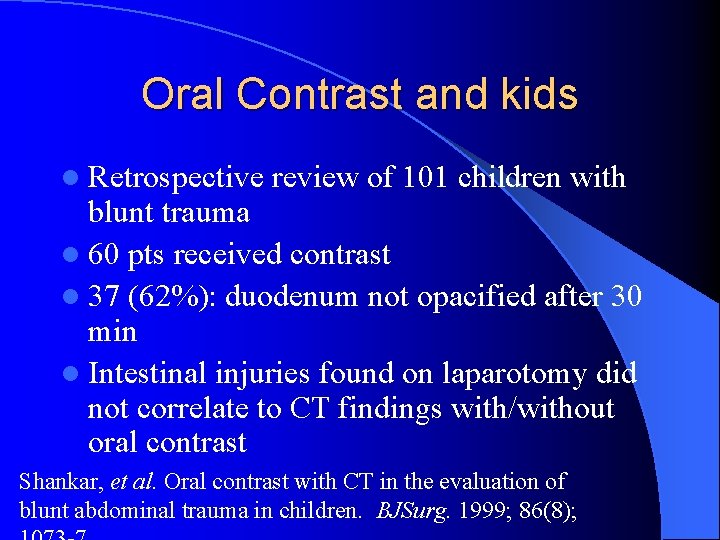
Oral Contrast and kids l Retrospective review of 101 children with blunt trauma l 60 pts received contrast l 37 (62%): duodenum not opacified after 30 min l Intestinal injuries found on laparotomy did not correlate to CT findings with/without oral contrast Shankar, et al. Oral contrast with CT in the evaluation of blunt abdominal trauma in children. BJSurg. 1999; 86(8);
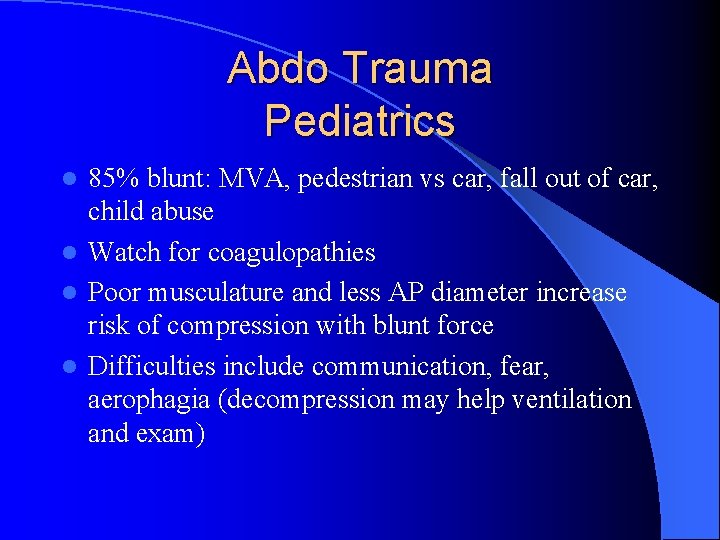
Abdo Trauma Pediatrics 85% blunt: MVA, pedestrian vs car, fall out of car, child abuse l Watch for coagulopathies l Poor musculature and less AP diameter increase risk of compression with blunt force l Difficulties include communication, fear, aerophagia (decompression may help ventilation and exam) l
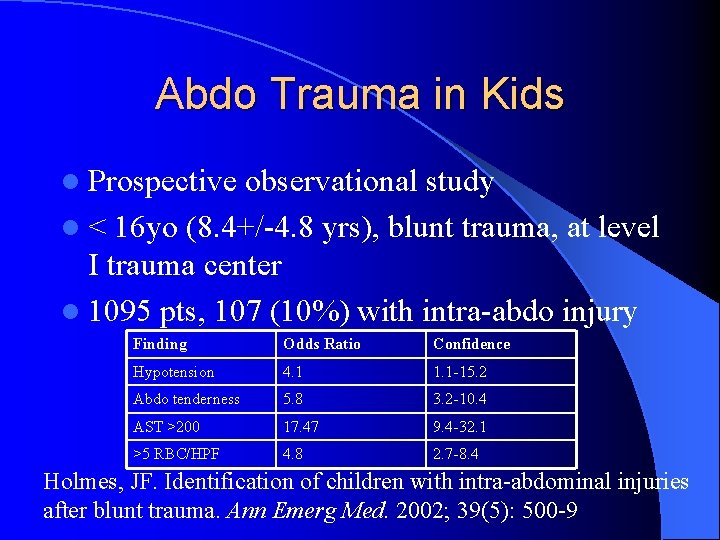
Abdo Trauma in Kids l Prospective observational study l < 16 yo (8. 4+/-4. 8 yrs), blunt trauma, at level I trauma center l 1095 pts, 107 (10%) with intra-abdo injury Finding Odds Ratio Confidence Hypotension 4. 1 1. 1 -15. 2 Abdo tenderness 5. 8 3. 2 -10. 4 AST >200 17. 47 9. 4 -32. 1 >5 RBC/HPF 4. 8 2. 7 -8. 4 Holmes, JF. Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2002; 39(5): 500 -9
Case #2 l 22 yo male presents with stab wound to abdomen l BP 155/90, HR 90, mentating “well” l What historical features are important?

Stab Wounds l Most stab wounds don’t cause intraperitoneal injury l Instrument (size, still in one piece) l # stabs l posture of patient
Stab Wounds l 3 Q’s – Urgent laparotomy? – Peritoneum violation – If peritoneum violated: laparotomy? l Clinical indications (Rosen’s): hemodynamic instability, peritoneal signs, evisceration, diaphragmatic injury, GI bleed, implement-in-situ, intraperitoneal air
Case #2 – do you want to explore the wound? l Shave and prep, local anesthetic l Extend wound and visualize layers l Do not blindly probe l Advocated for anterior abdo wounds, but all else ? ? l Watch thoracolumbar junction Markovchick. Local wound exploration of anterior abdominal stab wounds. J of Emerg Med. 1985 2(4): 287 -91.
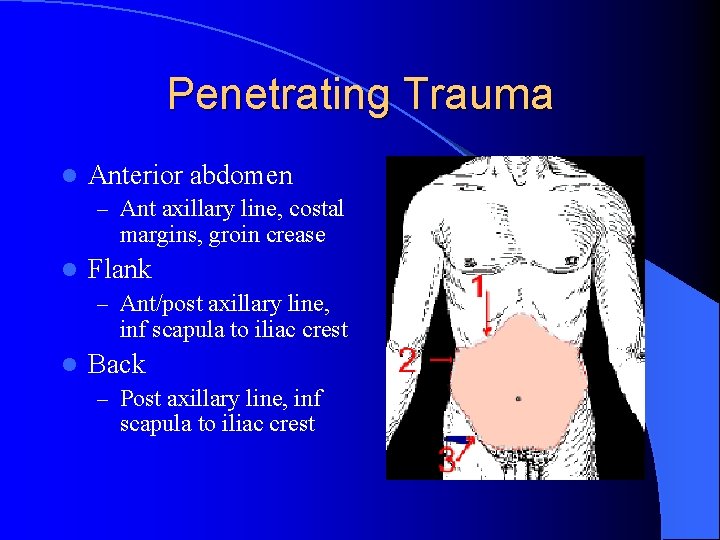
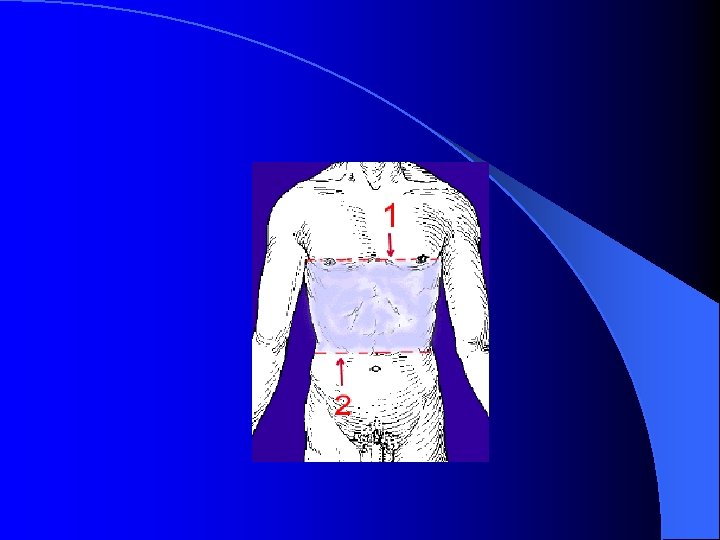
Penetrating Trauma l Anterior abdomen – Ant axillary line, costal margins, groin crease l Flank – Ant/post axillary line, inf scapula to iliac crest l Back – Post axillary line, inf scapula to iliac crest
Case #2 continued l LWE – confident that knife did not penetrate the peritoneum l Is it reasonable to stitch him up and d/c from the ED?
Selective Management l l l Retrospective review of 455 with penetrating truncal injuries (Detroit) 194 directly to OR 107 had selective w/u (triple contrast CT, LWE, observation) 136 d/c home after hx, plain films Missed 2 injuries w/o significant consequence Conclusion: stable pts with negative selective w/u can be d/c’d home Conrad, et al. Selective management of penetrating truncal injuries. Am Surg. 2003; 69(3): 266 -72.
Case #2 l No free air on upright CXR, how sensitive is this? l 13 pts with abdominal trauma (blunt and penetrating) l Upright CXR sensitivity from 0% if less than 3 pockets of 1 mm of air, to 100% if pocket of air > 13 mm Stapakis. Diagnosis of pneumoperitoneum: abdominal CT vs upright chest film. J of Comp Assist Tomo. 1992; 16(5) 713 -6.
GSW
Penetrating Trauma GSW l Ek = 1/2 mv 2 l E directly proportional to amount of injury l Other factors : resistance of tissue, stability of missle, impact velocity l Diagnostics and considerations similar to stabs
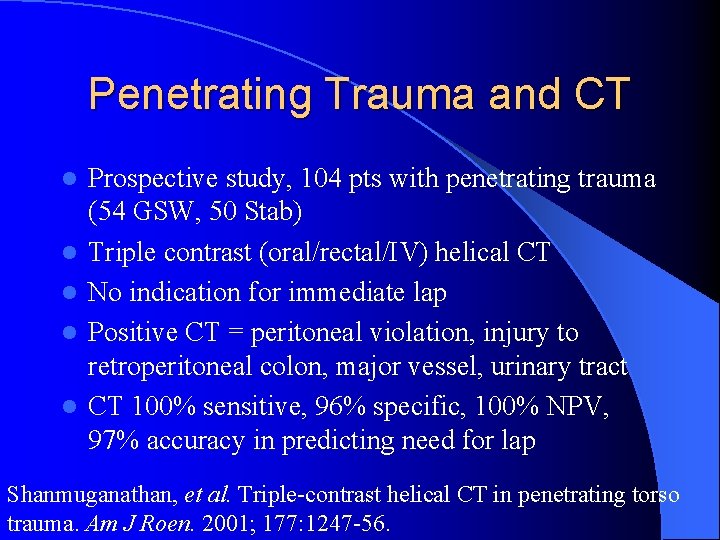
Penetrating Trauma and CT l l l Prospective study, 104 pts with penetrating trauma (54 GSW, 50 Stab) Triple contrast (oral/rectal/IV) helical CT No indication for immediate lap Positive CT = peritoneal violation, injury to retroperitoneal colon, major vessel, urinary tract CT 100% sensitive, 96% specific, 100% NPV, 97% accuracy in predicting need for lap Shanmuganathan, et al. Triple-contrast helical CT in penetrating torso trauma. Am J Roen. 2001; 177: 1247 -56.
Genitourinary Trauma l 10% of trauma has GU involvement (USA) l Lower Tract – Bladder and urethra l Upper Tract – renal and ureter l External genitalia
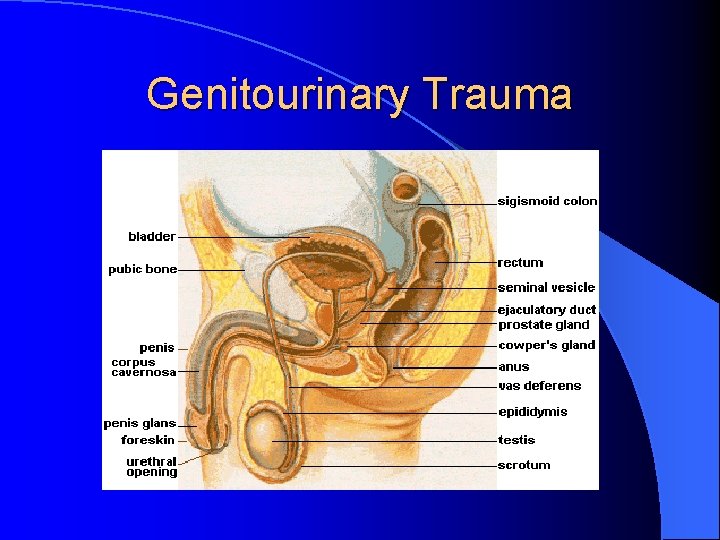
Genitourinary Trauma
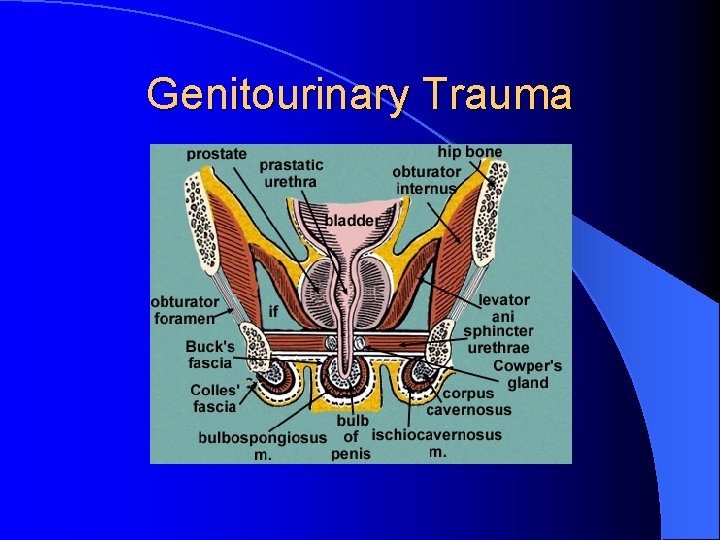
Genitourinary Trauma
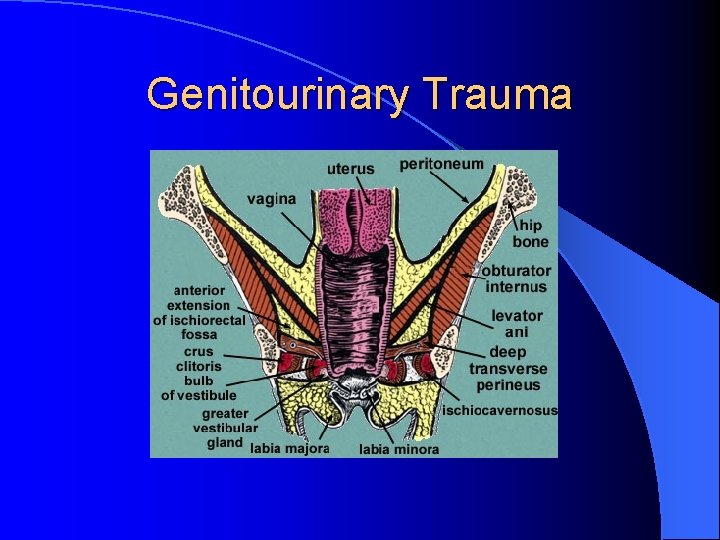
Genitourinary Trauma
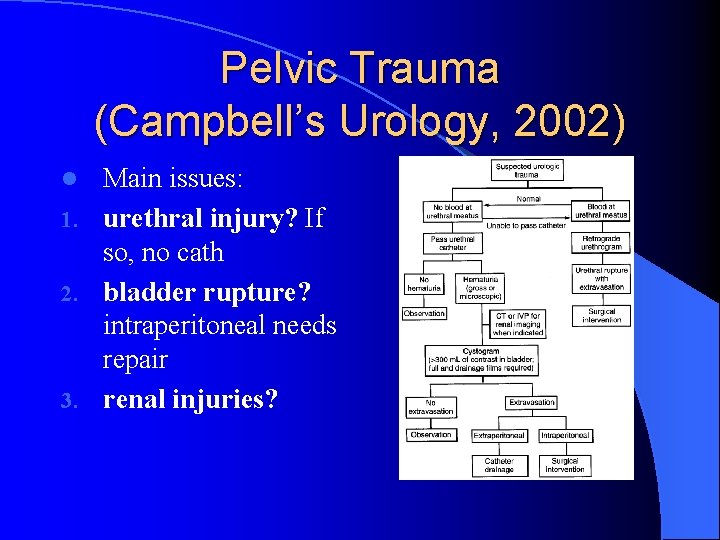
Pelvic Trauma (Campbell’s Urology, 2002) Main issues: 1. urethral injury? If so, no cath 2. bladder rupture? intraperitoneal needs repair 3. renal injuries? l
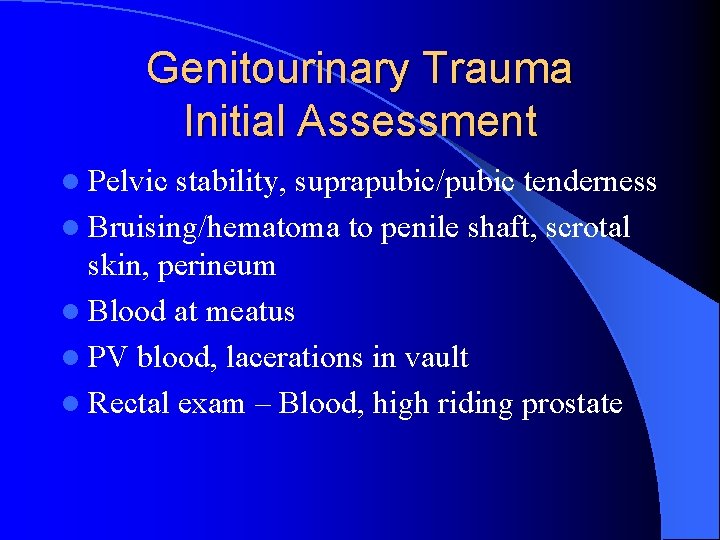
Genitourinary Trauma Initial Assessment l Pelvic stability, suprapubic/pubic tenderness l Bruising/hematoma to penile shaft, scrotal skin, perineum l Blood at meatus l PV blood, lacerations in vault l Rectal exam – Blood, high riding prostate
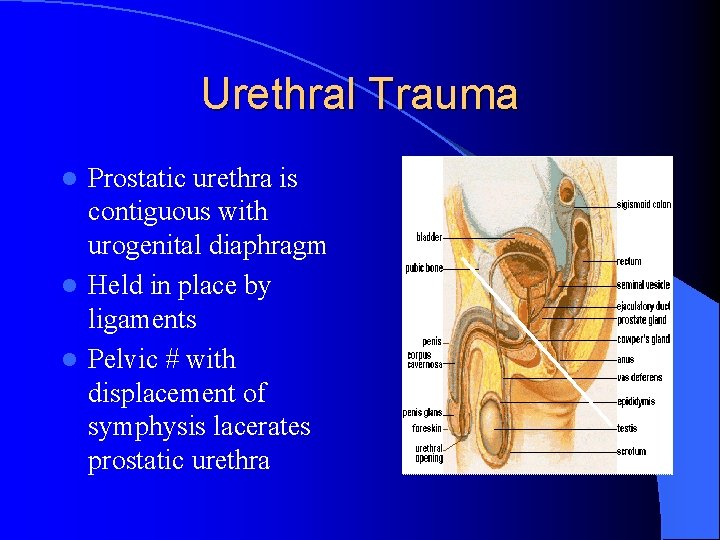
Urethral Trauma Prostatic urethra is contiguous with urogenital diaphragm l Held in place by ligaments l Pelvic # with displacement of symphysis lacerates prostatic urethra l
Urethral Trauma l Importance – Acutely: missed may convert partial to complete, difficult to assess urine output – Long term: strictures, incontinence
Urethral Trauma l Classic Triad (Campbell’s Urology, 2002) – Blood at meatus, inability to void, palpable full bladder – Blood sensitivity 50% (J Urol 1988; 140: 506– 507) – High riding prostate sensitivity only 34%, poor specificity (Br J Urol 1996; 77: 876– 880) – No study combining factors Proximal injury: pelvic # (4 -14%) l Distal injury: straddle, instrumentation, GSW l
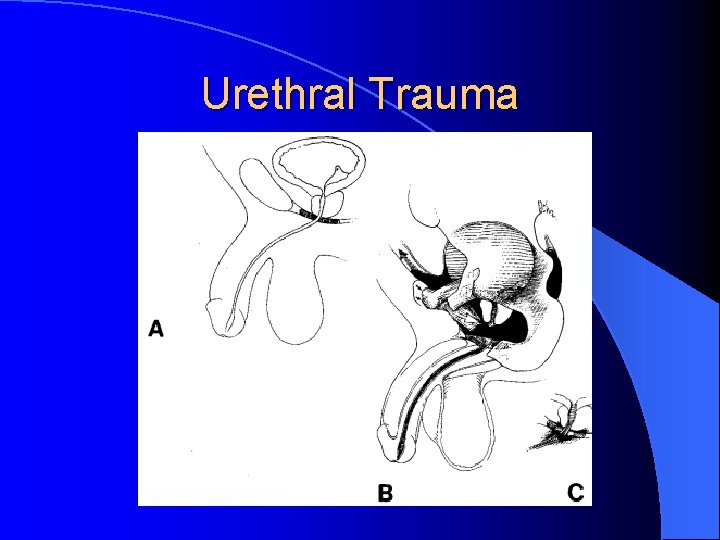
Urethral Trauma
Urethral Trauma Management l Retrograde urethrogram l If some contrast into bladder, may try one pass of Foley (Rosen’s) – may pass in partial tear l 10% associated with bladder rupture
Retrograde Urethrogram For Dummies l Patient may be supine for study l Oblique films may help l Pre-injection KUB l X-mas tree adaptor l +/- inflation of Foley balloon proximal to fossa navicularis (may leak contrast around penis)
Retrograde Urethrogram
Retrograde Urethrogram l 60 cc of full-strength or half strength contrast injected over 30 -60 sec l Repeat x-ray during last 10 cc of contrast
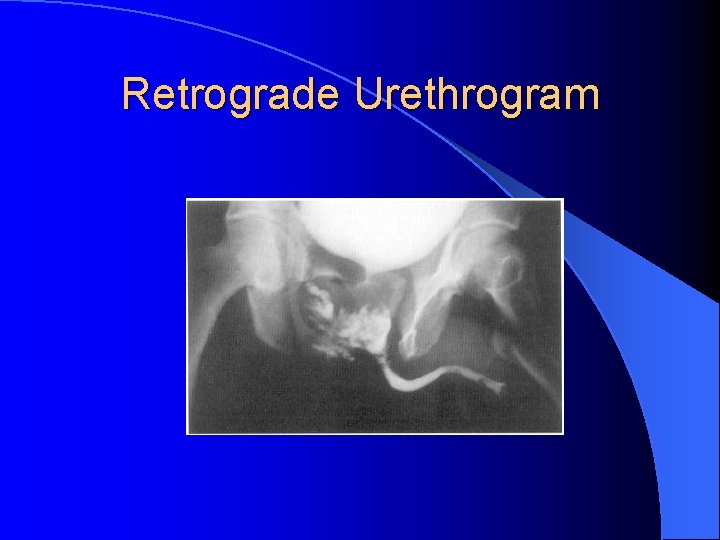
Retrograde Urethrogram
Bladder Trauma l Rare <2% of trauma l Generally associated with major injuries l When present mortality 12 -22% Carroll PR, Mc. Aninch JW: Major bladder trauma: Mechanisms of injury and a unified method of diagnosis and repair. J Urol 1984; 132: 254– 257.
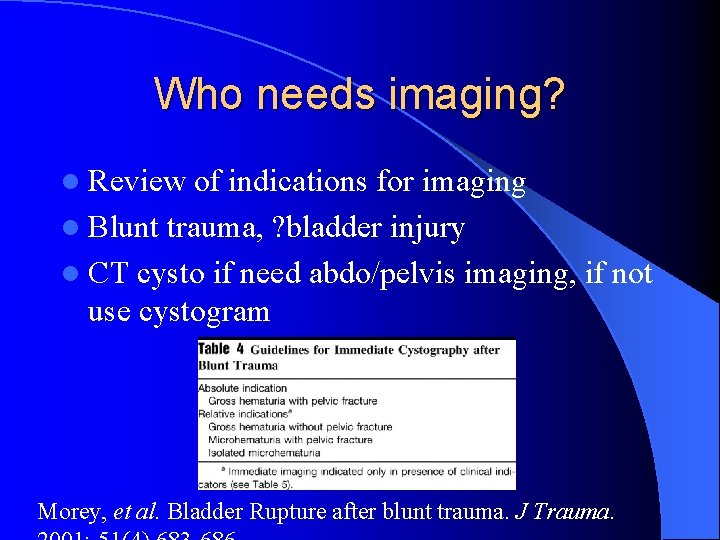
Who needs imaging? l Review of indications for imaging l Blunt trauma, ? bladder injury l CT cysto if need abdo/pelvis imaging, if not use cystogram Morey, et al. Bladder Rupture after blunt trauma. J Trauma.
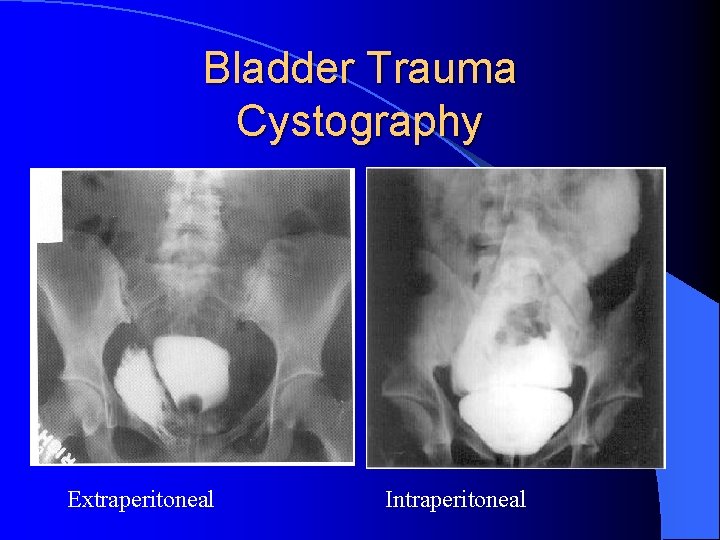
Bladder Trauma Cystography Extraperitoneal Intraperitoneal
CT Cystography l Retrospective review 316 pt with blunt trauma that received CT cysto l Radiology interpretation compared to OR report l Detection of bladder rupture sensitivity 95%, specificity 100% Deck, et al. Current experience with CT cystography and blunt trauma. W J Surg. 2001; 25(12): 1592 -6.
Bladder Trauma Management l Contusions (67% of injuries) – Hematuria w/o evidence of injury on imaging – Conservative l Intraperitoneal (usually burst injury) – Requires OR (non urgently)
Bladder Trauma Management l Extraperitoneal (penetrating or blunt) – Some controversy – Bladder drainage (J Urol 1983; 129: 946– 948) – Exceptions: bone fragment, open #, lap for other reasons
Renal Trauma l As always: The main question is who needs imaging? ? – History and Physical – Urinalysis
Case Example l 26 yo Male l Punched “in the kidneys”, yesterday l VSS, mild R flank bruising, no associated injuries l Nurse notes urine dipped positive for blood l Does this patient need further imaging?
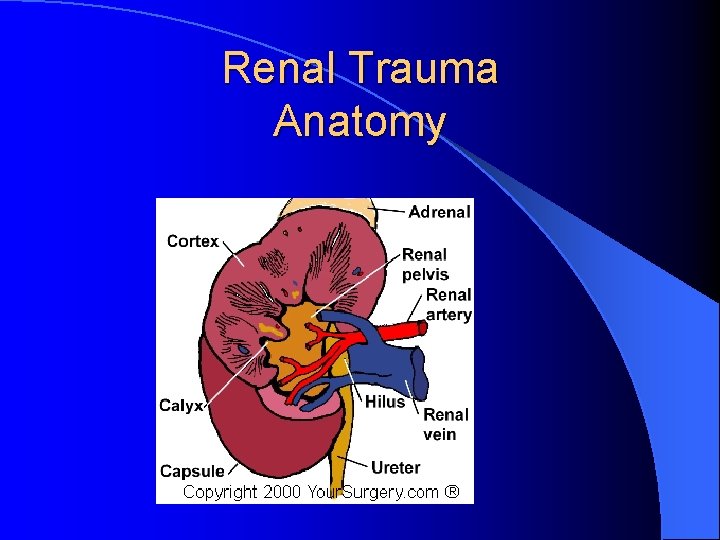
Renal Trauma Anatomy
Renal Trauma- History l More often injured in children as kidneys are relatively larger l Blunt vs Penetrating l Blunt – Fall, MVA, assault – Key info: deceleration (pedicle avulsion) l Penetrating – Stab, GSW
Renal Trauma Urinalysis • Degree of hematuria doesn’t correlate with degree of damage • 36% of renovasc injuries don’t have hematuria Cass AS: Renovascular injuries from external trauma. Urol Clin North Am 1989; 16: 213– 220
Adults and Hematuria l 1484 pts with blunt abdo trauma l Gross hematuria - 65% had significant intra-abdominal injury l Microscopic hematuria + shock - 29% had significant injury l No pts with hematuria and normotensive had significant injury l Imaging for these pts Knudson, MM, et al. Hematuria as a predictor of abdominal injury after blunt trauma. Am J Sug. 1992; 164(5): 482 -6.
Microscopic Hematuria l Review article looking at evidence for imaging in blunt trauma with microscopic hematuria l Imaging only indicated if hypotensive or have associated injuries Saunders F, Argall J. Investigating microscopic hematuria in blunt abdominal trauma. Emerg Med Journal. 2002; 19(4) 322 -3
Hematuria in Kids l Retrospective review of 110 pts (1 -18 yo) with blunt trauma + hematuria l All pts had imaging (CT abdo/pelvis) l 24 pts had significant injury l Recommend imaging if: – 50 greater RBC/HPF – Hypotension – Mechanism of injury Perez, M et al. Blunt traumatic hematuria in children – Is a simplified algorithm justified? J Urol. 2002; 167(6): 2543 -6.
Renal Trauma Investigations l IVP vs CT? l Only if no CT, no radiologist on call (Rosen’s) l No head to head comparison in Medline
CT vs IVP Major renal lacerations either have gross hematuria or microscopic hematuria (>3 -5 RBC/hpf) with shock o IV contrast CT is best o Mee, et al. Radiographic assessment of renal trauma: a ten year prospective study of patient selection. J Urol 141: 1095, 1989.
Renal Trauma Management l Penetrating injury – Presence of absence of hematuria not a factor – Location of wound is paramount l Pediatrics – Any degree of hematuria is investigated
External Genitalia Trauma l Penile trauma l Laceration, contusion, amputation, strangulation l Fracture – rupture of corpus cavernosum – During vigorous intercourse, “snap”, detumescence, hematoma – Rx - OR
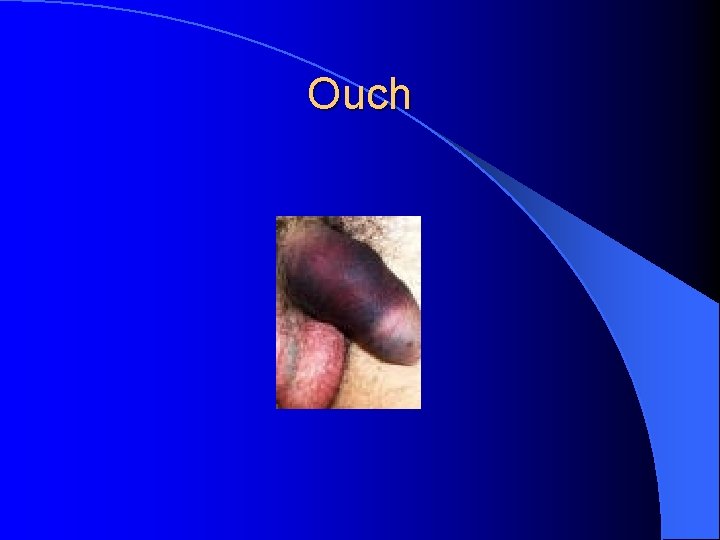
Ouch
External Genitalia Trauma l Testicular trauma l Color Doppler U/S l OR
Conclusions Mechanism of injury will help the search for damage l Abdo Trauma l – Occult injuries have worse morbidity/mortality – LWE only for anterior abdo wounds – +/- oral contrast with CT l GU Trauma – Work from bottom to top – Know how to do retrograde urethrogram – If ? renal injury: Gross blood or microscopic + hypotension are indications for imaging
- Slides: 83