ABCDEF Bundles in ICU Zohair Al Aseri FRCPC
ABCDEF Bundles in ICU Zohair Al Aseri FRCPC, EM & CCM Director of Adult Critical Care Services MOH
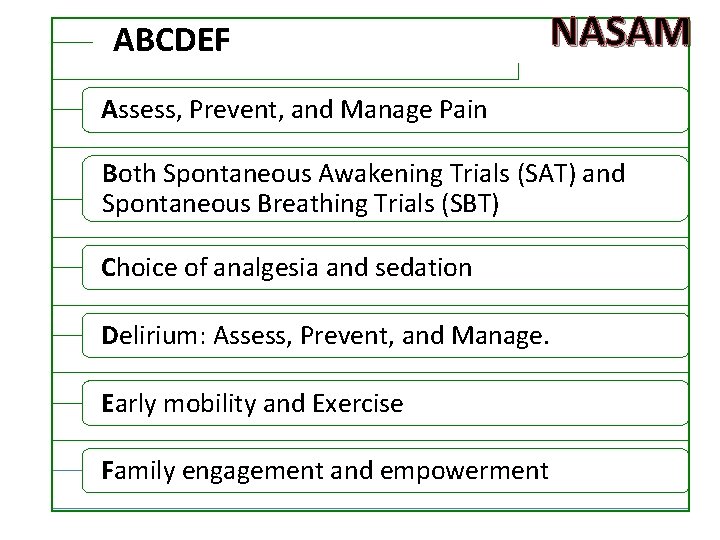
ABCDEF bundle: NASAM Assess, Prevent, and Manage Pain Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT) Choice of analgesia and sedation Delirium: Assess, Prevent, and Manage. Early mobility and Exercise Family engagement and empowerment
ABCDEF Bundle Instead of waiting for patients to get better helps ICU patients get better FASTER.
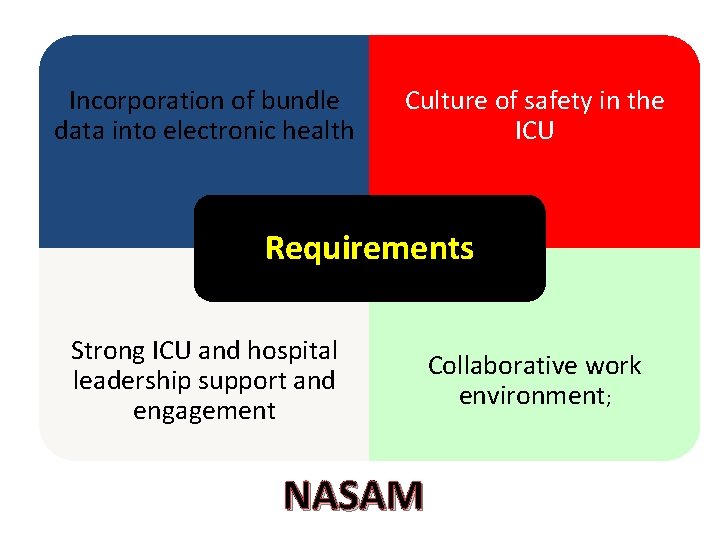
Incorporation of bundle data into electronic health Culture of safety in the ICU Requirements Strong ICU and hospital leadership support and engagement NASAM Collaborative work environment;
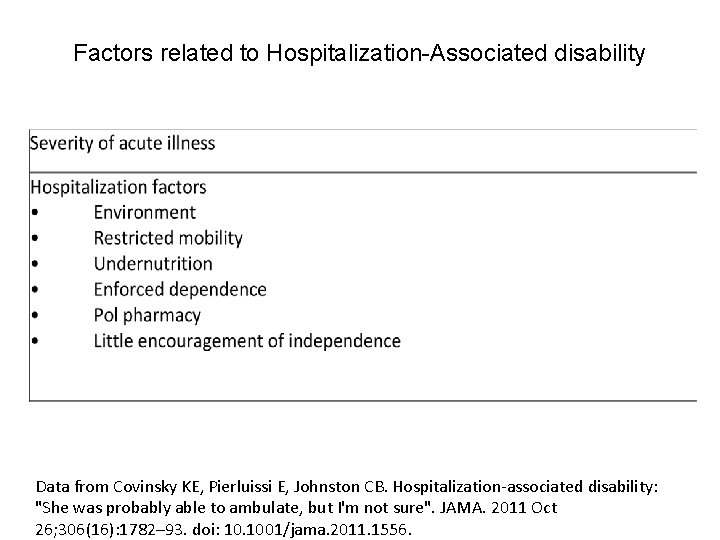
Factors related to Hospitalization-Associated disability Data from Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA. 2011 Oct 26; 306(16): 1782– 93. doi: 10. 1001/jama. 2011. 1556.
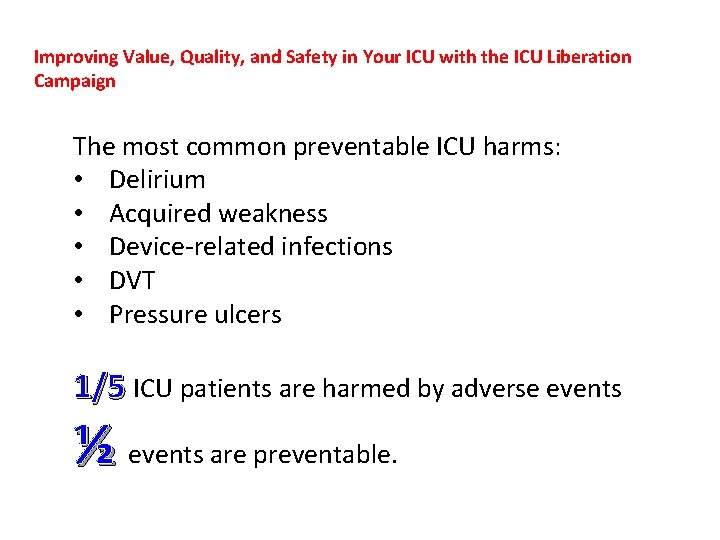
Improving Value, Quality, and Safety in Your ICU with the ICU Liberation Campaign The most common preventable ICU harms: • Delirium • Acquired weakness • Device-related infections • DVT • Pressure ulcers 1/5 ICU patients are harmed by adverse events ½ events are preventable.
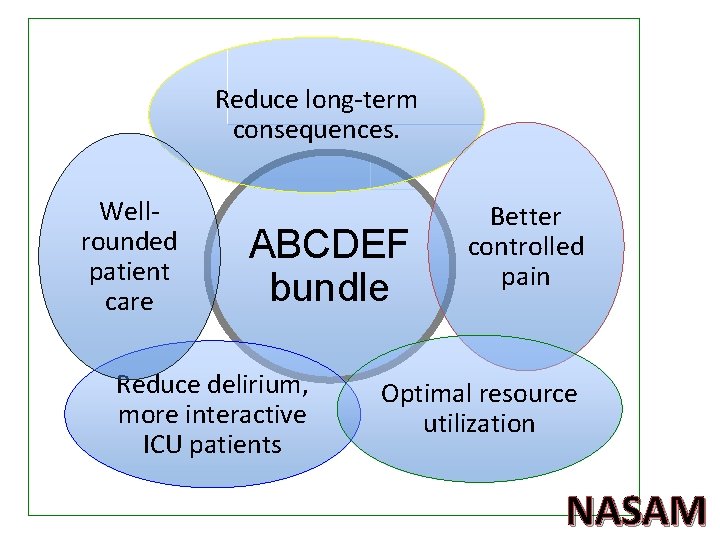
Reduce long-term consequences. Wellrounded patient care ABCDEF bundle Reduce delirium, more interactive ICU patients Better controlled pain Optimal resource utilization NASAM
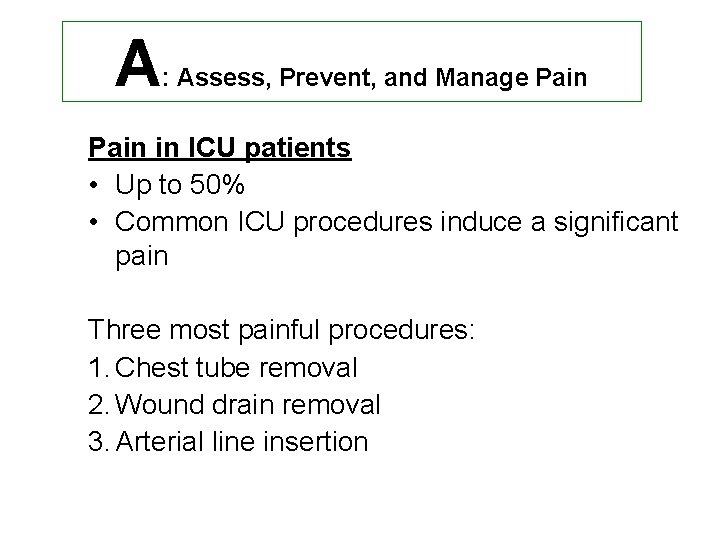
A : Assess, Prevent, and Manage Pain in ICU patients • Up to 50% • Common ICU procedures induce a significant pain Three most painful procedures: 1. Chest tube removal 2. Wound drain removal 3. Arterial line insertion
A: Assess, Prevent, and Manage Pain Assessment of pain • 1 st step before administering pain relief. • Pain and delirium interrelatedness. – Treating pain is important in the prevention and/or management of delirium • Only in 35% of the time before ICU procedures!! need improvement
A: Assess, Prevent, and Manage Pain Assessment of pain Scale • Numerical rating scale (NRS) • Gold standard: Patient's self-report 1– 10
A: Assess, Prevent, and Manage Pain For non-self reporting patient, use observable behavioral and physiological indicators 1. Behavioral Pain Scale (BPS) 1. Critical-Care Pain Observation Tool (CPOT) » Valid & Reliable. » Provide selection of pain meds. » Evaluate pain meds effectiveness.
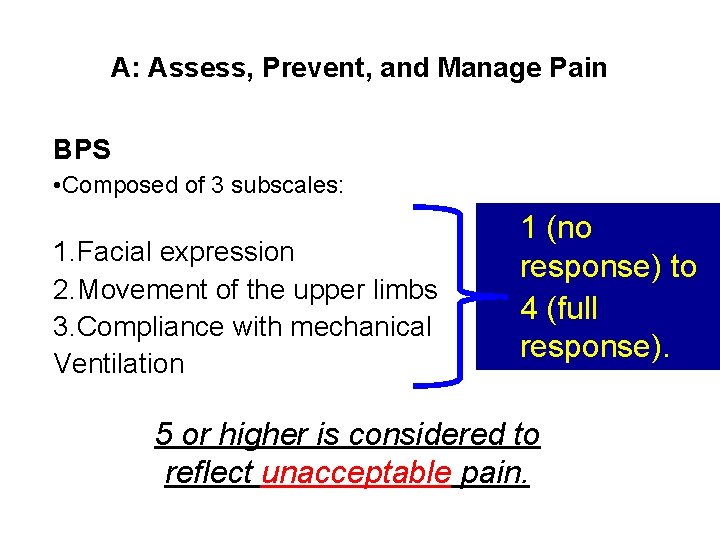
A: Assess, Prevent, and Manage Pain BPS • Composed of 3 subscales: 1. Facial expression 2. Movement of the upper limbs 3. Compliance with mechanical Ventilation 1 (no response) to 4 (full response). 5 or higher is considered to reflect unacceptable pain.
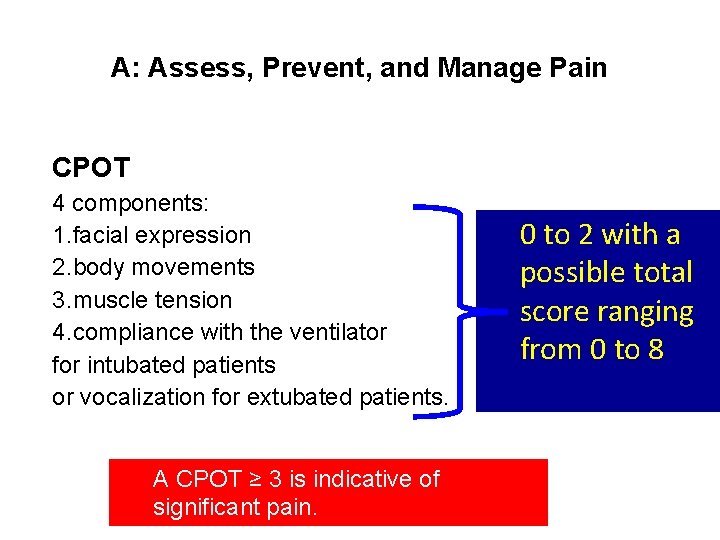
A: Assess, Prevent, and Manage Pain CPOT 4 components: 1. facial expression 2. body movements 3. muscle tension 4. compliance with the ventilator for intubated patients or vocalization for extubated patients. A CPOT ≥ 3 is indicative of significant pain. 0 to 2 with a possible total score ranging from 0 to 8
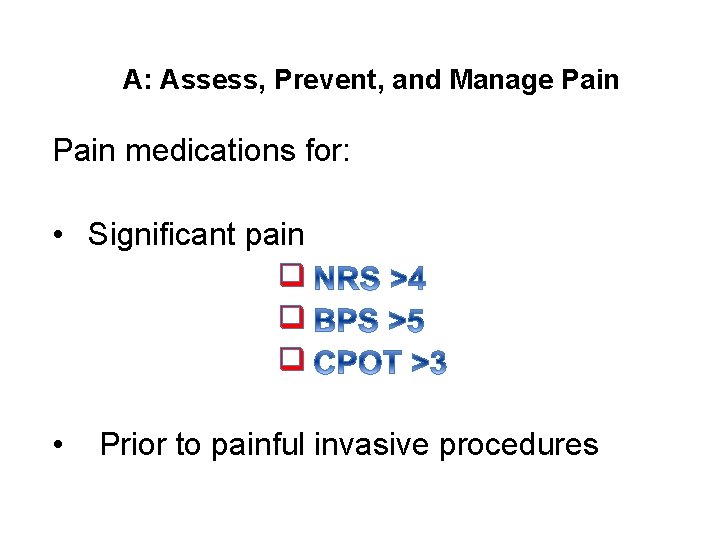
A: Assess, Prevent, and Manage Pain medications for: • Significant pain q q q • Prior to painful invasive procedures
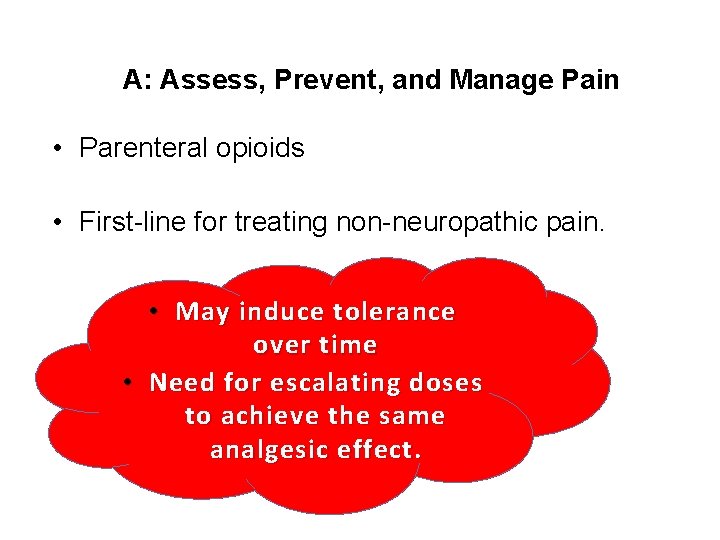
A: Assess, Prevent, and Manage Pain • Parenteral opioids • First-line for treating non-neuropathic pain. • May induce tolerance over time • Need for escalating doses to achieve the same analgesic effect.
A: Assess, Prevent, and Manage Pain • For neuropathic pain • Gabapentin • Carbamazepine • Opioids • Adjunctive medications to reduce opioid and its side effects: • Non-opioid analgesics: – Acetaminophen – NSAID – Ketamine
A: Assess, Prevent, and Manage Pain • Use of regional analgesia – Ie, epidural analgesia • surgical patients • traumatic rib fractures. • Non-pharmacological methods • Effective and safe – injury stabilization – patient repositioning – use of heat/cold
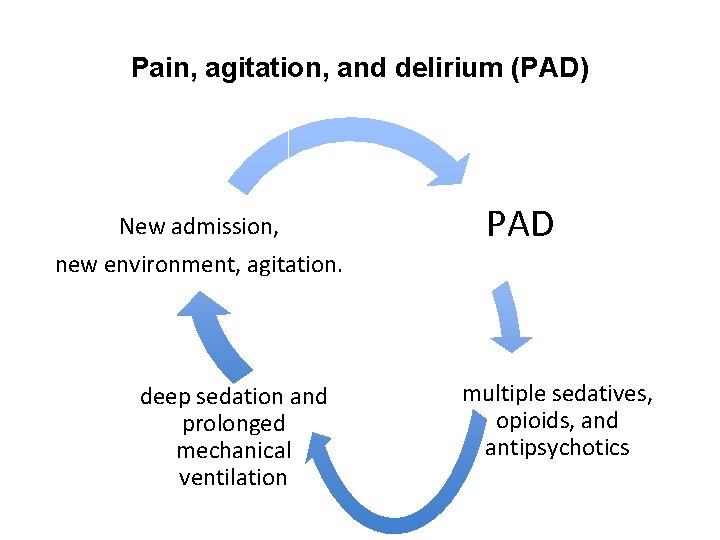
Pain, agitation, and delirium (PAD) New admission, new environment, agitation. deep sedation and prolonged mechanical ventilation PAD multiple sedatives, opioids, and antipsychotics
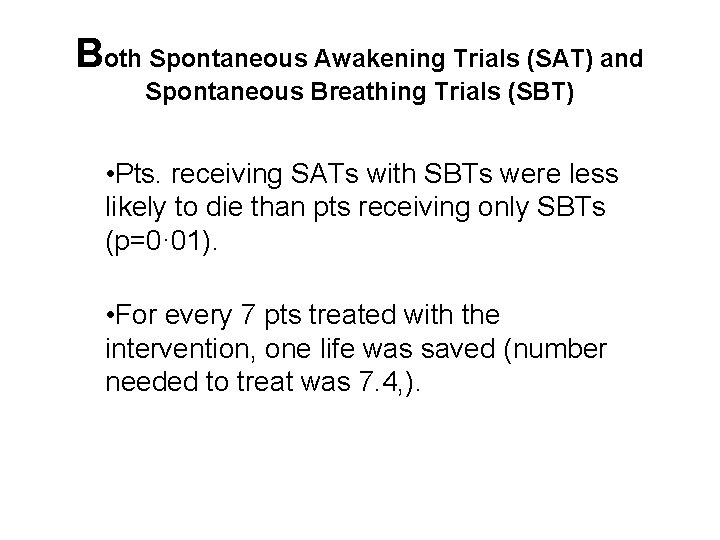
Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT) • Pts. receiving SATs with SBTs were less likely to die than pts receiving only SBTs (p=0· 01). • For every 7 pts treated with the intervention, one life was saved (number needed to treat was 7. 4, ).
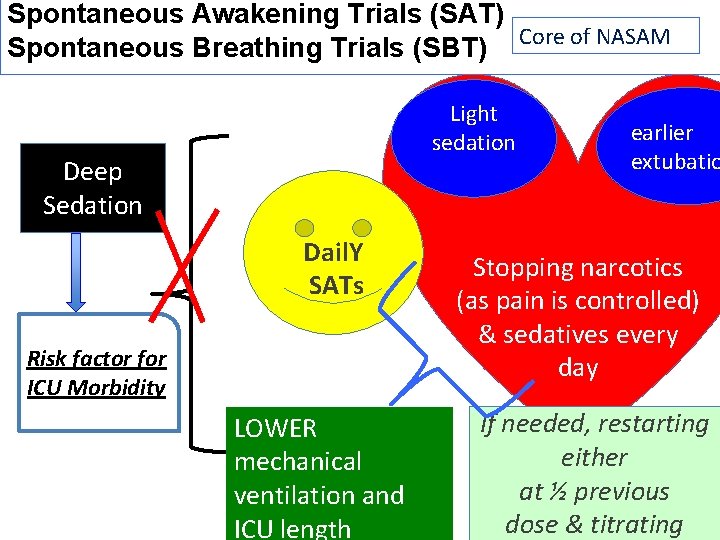
Spontaneous Awakening Trials (SAT) Core of NASAM Spontaneous Breathing Trials (SBT) Light sedation Deep Sedation Dail. Y SATs Risk factor for ICU Morbidity LOWER mechanical ventilation and ICU length earlier extubatio Stopping narcotics (as pain is controlled) & sedatives every day If needed, restarting either at ½ previous dose & titrating
C : Choice of analgesia and sedation Goal-directed delivery of psychoactive medications: By using sedation scales PAD guidelines recommend: • Richmond Agitation-Sedation Scale (RASS) • Riker Sedation-Agitation Scale (SAS).
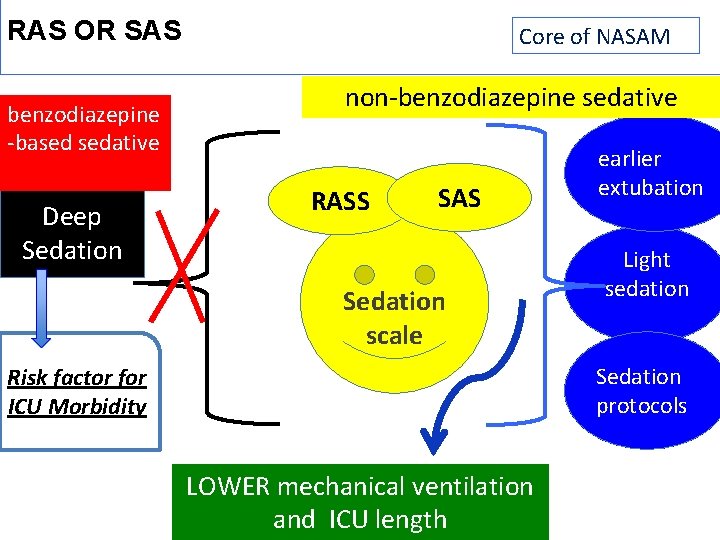
RAS OR SAS benzodiazepine -based sedative Deep Sedation Core of NASAM non-benzodiazepine sedative RASS SAS Sedation scale earlier extubation Light sedation Sedation protocols Risk factor for ICU Morbidity LOWER mechanical ventilation and ICU length
D : Delirium: Assess, Prevent, and Manage Delirium • Disturbance in attention and awareness • Develops over a short period of time, hours to day • Fluctuates over time. • Over 80% of pts developed delirium during hospita stay • Onset between 2 nd and the 3 rd day.
D: Delirium: Assess, Prevent, and Manage Tow most frequently used tools to diagnose delirium in ICU: 1. Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) 1. Intensive Care Delirium Screening Checklist (ICDSC)
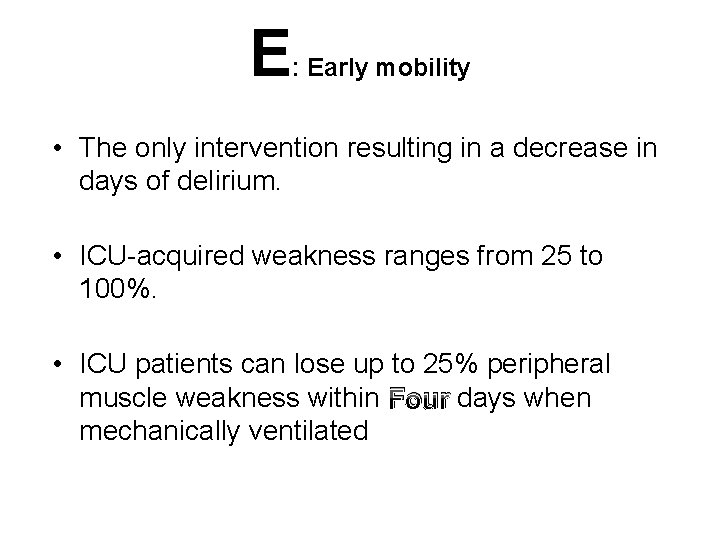
E : Early mobility • The only intervention resulting in a decrease in days of delirium. • ICU-acquired weakness ranges from 25 to 100%. • ICU patients can lose up to 25% peripheral muscle weakness within Four days when mechanically ventilated
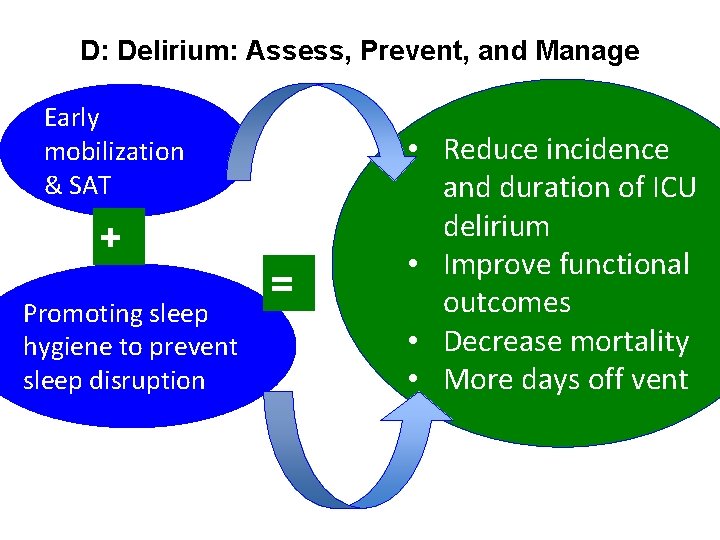
D: Delirium: Assess, Prevent, and Manage Early mobilization & SAT + Promoting sleep hygiene to prevent sleep disruption = • Reduce incidence and duration of ICU delirium • Improve functional outcomes • Decrease mortality • More days off vent
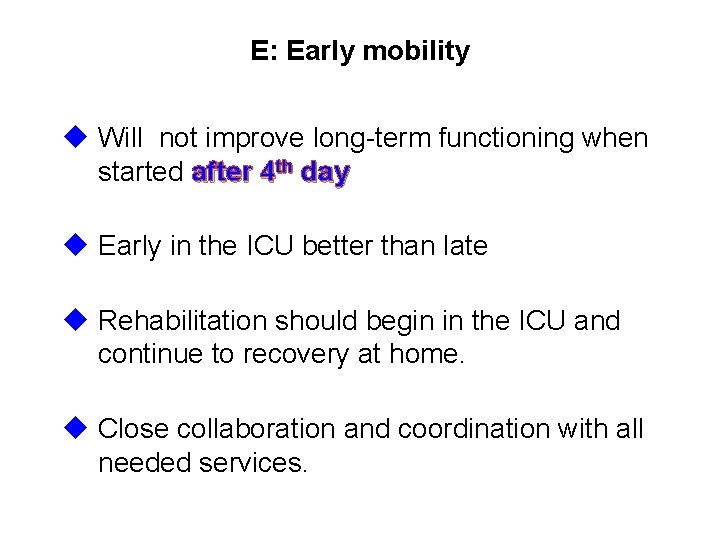
E: Early mobility u Will not improve long-term functioning when started after 4 th day u Early in the ICU better than late u Rehabilitation should begin in the ICU and continue to recovery at home. u Close collaboration and coordination with all needed services.
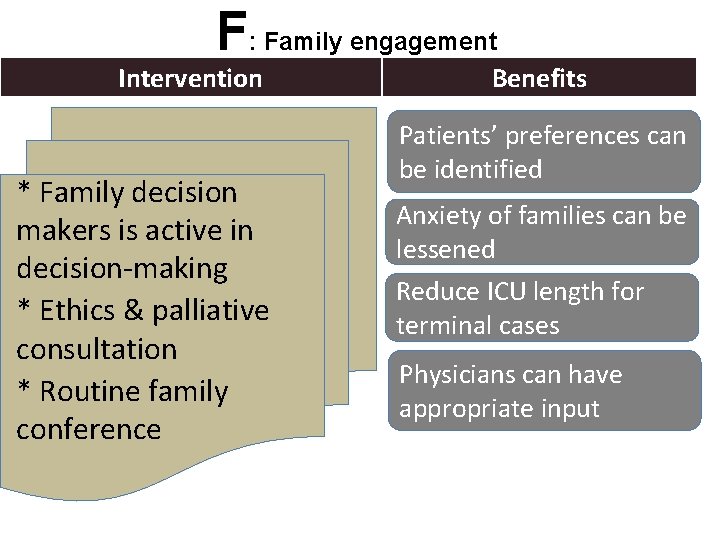
F: Family engagement Intervention * Family decision makers is active in decision-making * Ethics & palliative consultation * Routine family conference Benefits Patients’ preferences can be identified Anxiety of families can be lessened Reduce ICU length for terminal cases Physicians can have appropriate input
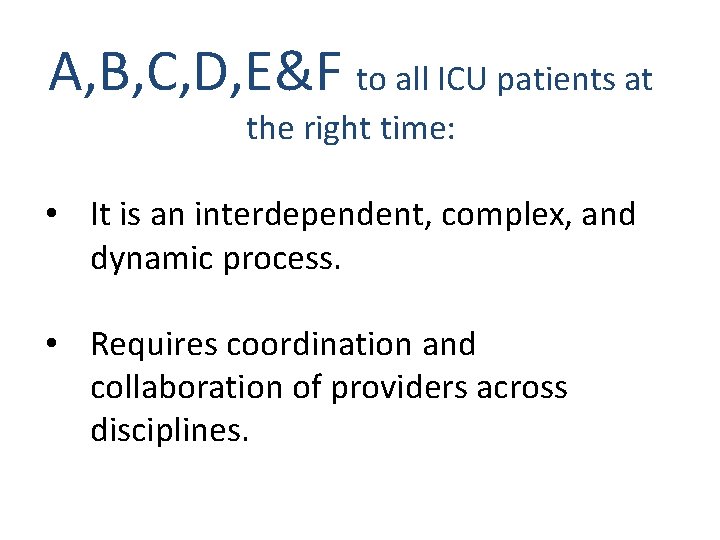
A, B, C, D, E&F to all ICU patients at the right time: • It is an interdependent, complex, and dynamic process. • Requires coordination and collaboration of providers across disciplines.
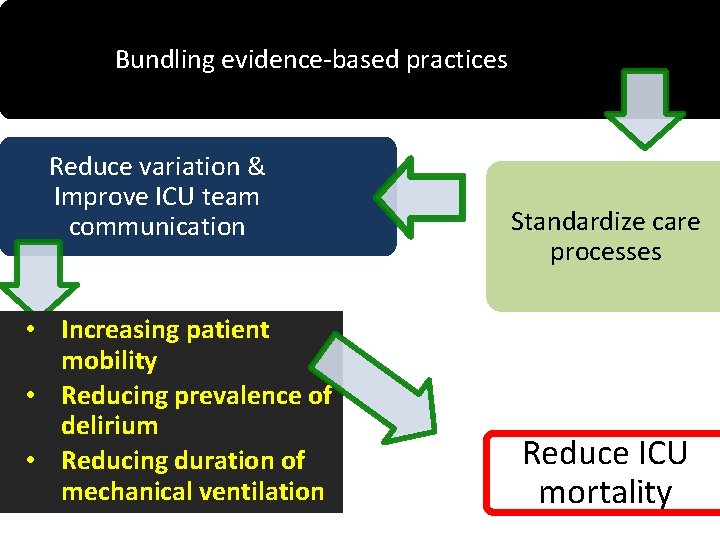
Bundling evidence-based practices Reduce variation & Improve ICU team communication • Increasing patient mobility • Reducing prevalence of delirium • Reducing duration of mechanical ventilation Standardize care processes Reduce ICU mortality
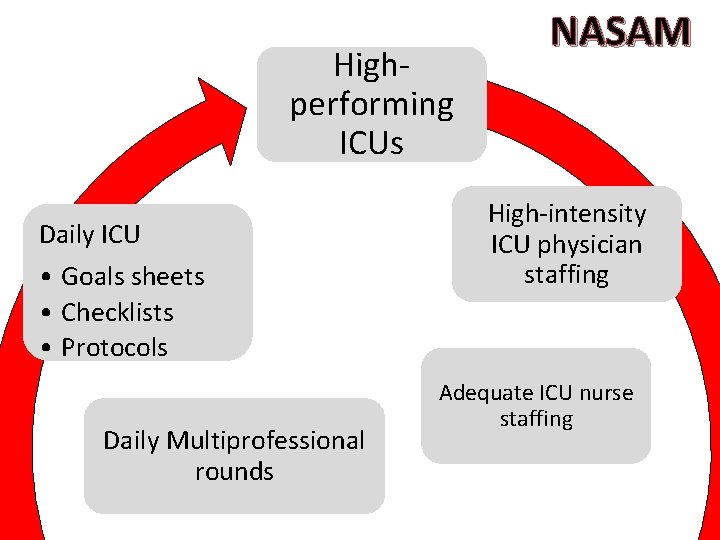
Highperforming ICUs Daily ICU • Goals sheets • Checklists • Protocols Daily Multiprofessional rounds NASAM High-intensity ICU physician staffing Adequate ICU nurse staffing
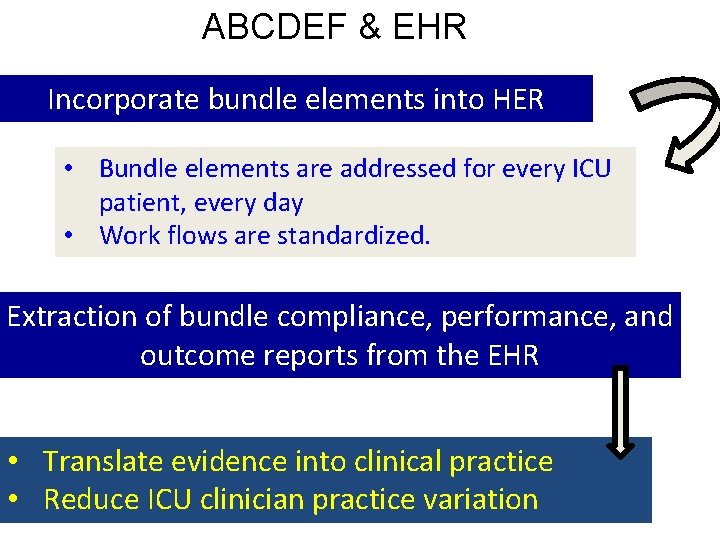
ABCDEF & EHR Incorporate bundle elements into HER • Bundle elements are addressed for every ICU patient, every day • Work flows are standardized. Extraction of bundle compliance, performance, and outcome reports from the EHR • Translate evidence into clinical practice • Reduce ICU clinician practice variation
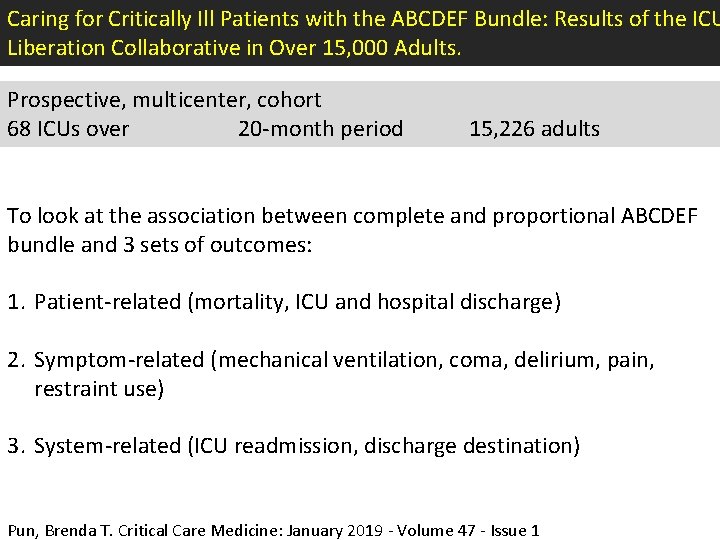
Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15, 000 Adults. Prospective, multicenter, cohort 68 ICUs over 20 -month period 15, 226 adults To look at the association between complete and proportional ABCDEF bundle and 3 sets of outcomes: 1. Patient-related (mortality, ICU and hospital discharge) 2. Symptom-related (mechanical ventilation, coma, delirium, pain, restraint use) 3. System-related (ICU readmission, discharge destination) Pun, Brenda T. Critical Care Medicine: January 2019 - Volume 47 - Issue 1
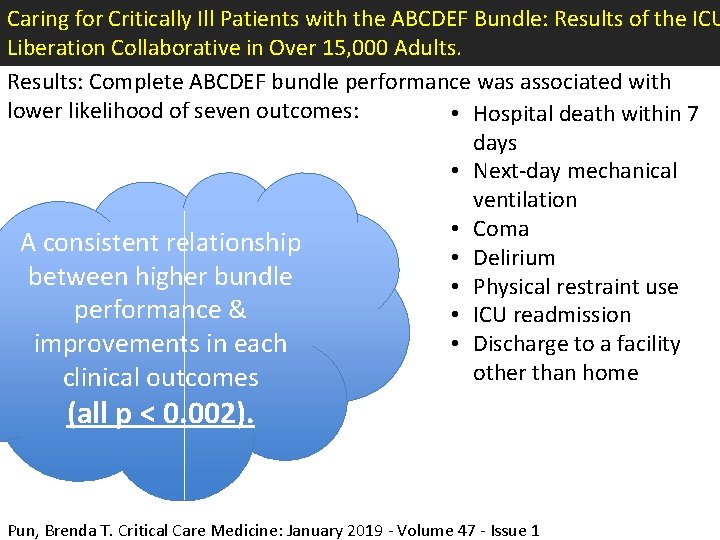
Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15, 000 Adults. Results: Complete ABCDEF bundle performance was associated with lower likelihood of seven outcomes: • Hospital death within 7 days • Next-day mechanical ventilation • Coma A consistent relationship • Delirium between higher bundle • Physical restraint use performance & • ICU readmission • Discharge to a facility improvements in each other than home clinical outcomes (all p < 0. 002). Pun, Brenda T. Critical Care Medicine: January 2019 - Volume 47 - Issue 1
• Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15, 000 Adults Pun, Brenda T. Critical Care Medicine: January 2019 - Volume 47 - Issue 1 - p 3 -14 doi: 10. 1097/CCM. 0000003482 • Society of Critical Care Medicine. Critical care statistics. Mt. Prospect, IL: Society of Critical Care Medicine. https: //www. sccm. org/Communications/Critical-Care-Statistics. Accessed July 9, 2018. • Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005 Aug; 33(8): 1694 -1700. • Kaushal R, Bates DW, Franz C, Soukup JR, Rothschild JM. Cost of adverse events in intensive care units. Crit Care Med. 2007 Nov; 35(11): 2479 -2483. • Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013 Jan; 41(1): 263 -306. • Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012 Feb; 40(2): 502 -509. • Marra A, Pandaripande PP, Girard TD, et al. Cooccurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit Care Med. 2018 May 21. [Epub ahead of print]. • • Elliott D, Davidson JE, Harvey MA, et al. Crit Care Med. 2014 Dec; 42(12): 2518 -2526. • Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014 May; 42(5): 1024 -1036. • Barnes-Daly MA, Phillips G, Ely EW. Improving hospital survival and reducing brain dysfunction at seven California community hospitals: implementing PAD guidelines via the ABCDEF bundle in 6, 064 patients. Crit Care Med. 2017 Feb; 45(2): 171 -178. • Donovan AL, Aldrich JM, Gross AK, et al; University of California San Francisco Critical Care Innovations Group. Interprofessional care and teamwork in the ICU. Crit Care Med 2018 Jun; 46(6): 980 -990. • Balas MC, Burke WJ, Gannon D, et al. Implementing the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU pain, agitation, and delirium guidelines. Crit Care Med 2013 Sep; 41(9 Suppl 1): S 116 -S 127. • Costa DK, Barg FK, Asch DA, Kahn JM. Facilitators of an interprofessional approach to care in medical and mixed medical/surgical ICUs” a multicenter qualitative study. Res Nurs Health. 2014 Aug; 37(4): 326 -335. • Harvard Business Review. Want to be a more supportive leader? Here’s how. June 25, 2018. Boston, MA: Harvard Business School Publishing Corporation. https: //www. physicianleaders. org/news/want-more-supportive-leader-heres-how. Accessed June 27, 2018. • Kambil A. Four types of executive sponsorship to catalyze change. October 11, 2017. New York, NY: Deloitte Insights. https: //www 2. deloitte. com/insights/us/en/focus/executive-transitions/four-types-of-executive-sponsorship-to-catalyze-change. html. Accessed June 27, 2018. • Institute for Healthcare Improvement. The IHI Triple Aim. Boston, MA: Institute for Healthcare Improvement; 2018. http: //www. ihi. org/Engage/Initiatives/Triple. Aim/Pages/default. aspx. Accessed July 24, 2018 references Harvey MA, Davidson JE. Postintensive care syndrome: right care, right now. . . and later. Crit Care Med. 2016 Feb; 44(2): 381 -385. Davidson JE, Harvey MA. Patient and family post-intensive care syndrome. AACN Adv Crit Care. 2016 April-June; 27(2): 184 -186. ICU Liberation. ABCDEF bundle. http: //www. iculiberation. org/Bundles/Pages/default. aspx. Mt. Prospect, IL: Society of Critical Care Medicine. Accessed June 12, 2018.
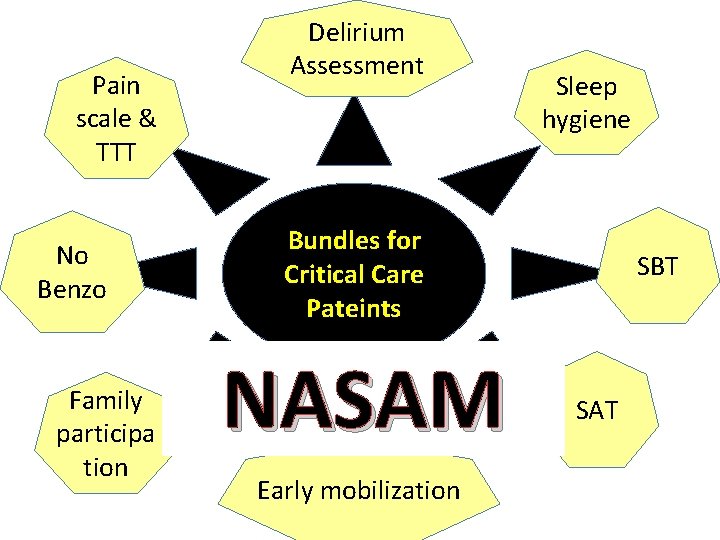
Pain scale & TTT No Benzo Family participa tion Delirium Assessment Sleep hygiene Bundles for Critical Care Pateints NASAM Early mobilization SBT SAT

Thank you Q&A
- Slides: 37