AAC Assessment Speech and Language Assessment vs AAC

- Slides: 55
AAC Assessment
Speech and Language Assessment vs AAC Assessment �Traditional evaluation focus is on describing nature and severity of communication disability, estimating prognosis, and designing initial framework for intervention �AAC assessment assumes communication disorder is chronic and natural language is not likely to occur.
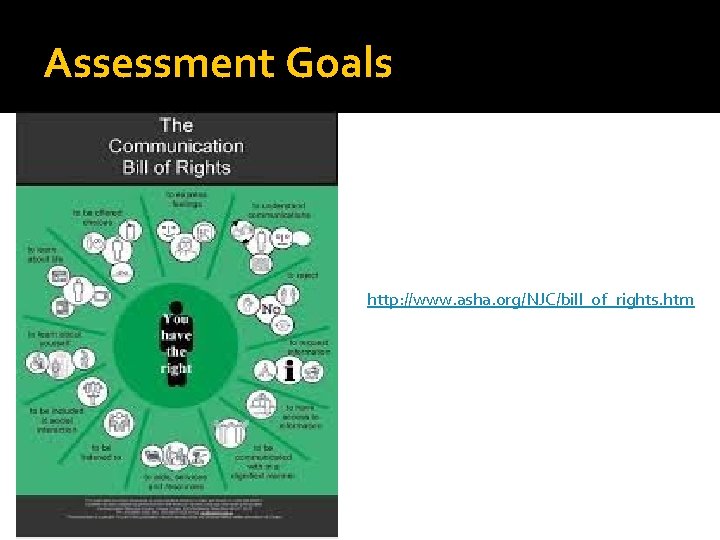
Assessment Goals To assist the individual in meeting: 1. Their current communication needs 2. Their future communication needs To assist the individual in becoming communicatively competent (Light, 1989) To facilitate the most effective communication possible across a variety of communication environments, situations or frameworks
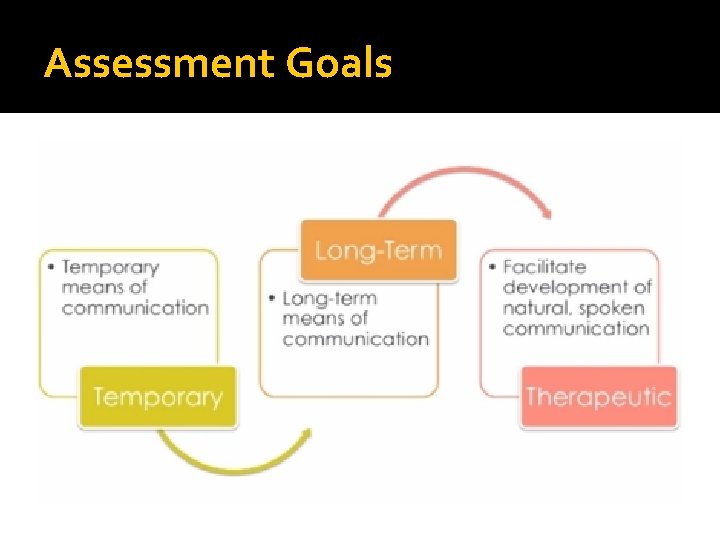
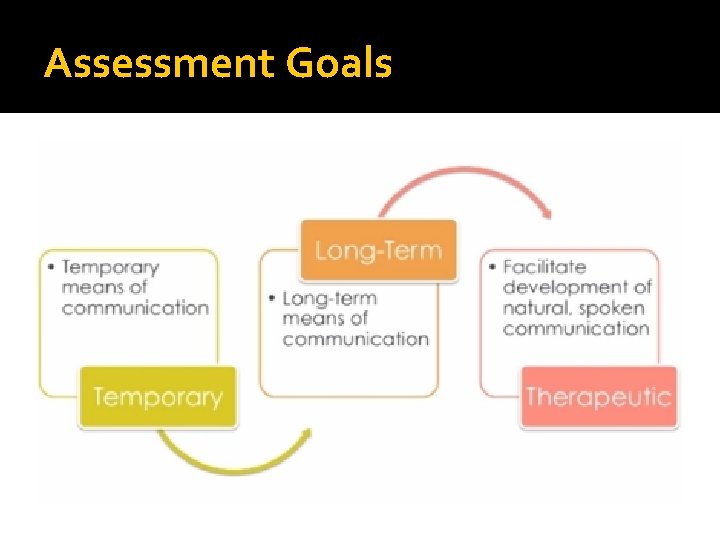
Assessment Goals
Assessment Goals http: //www. asha. org/NJC/bill_of_rights. htm
Basis for Successful Outcomes �Knowledge about client �Information about devices and AAC systems �EBP Best Practices
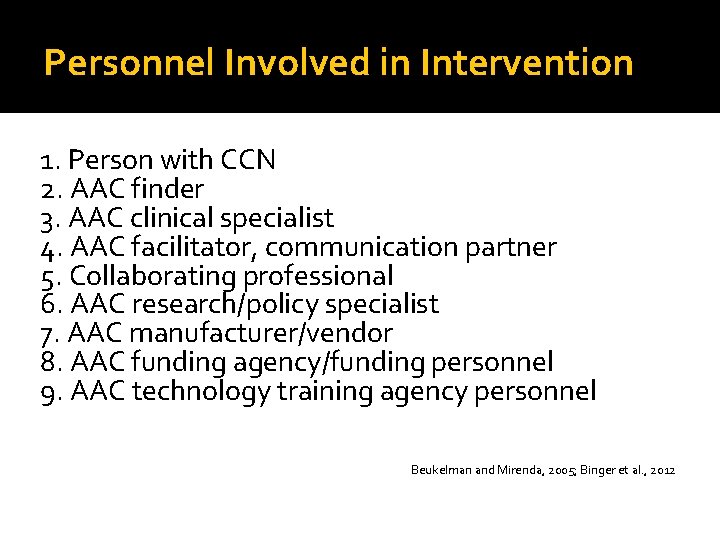
Personnel Involved in Intervention 1. Person with CCN 2. AAC finder 3. AAC clinical specialist 4. AAC facilitator, communication partner 5. Collaborating professional 6. AAC research/policy specialist 7. AAC manufacturer/vendor 8. AAC funding agency/funding personnel 9. AAC technology training agency personnel Beukelman and Mirenda, 2005; Binger et al. , 2012
Assessment Models �Candidacy Model �Participation Model
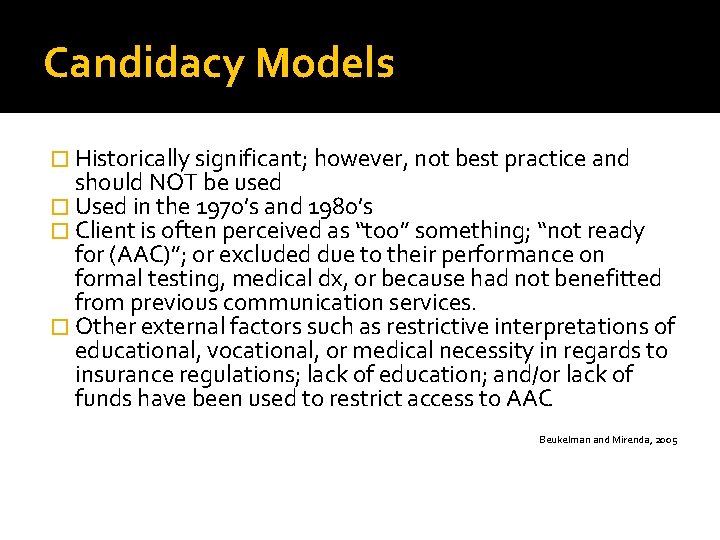
Candidacy Models � Historically significant; however, not best practice and should NOT be used � Used in the 1970’s and 1980’s � Client is often perceived as “too” something; “not ready for (AAC)”; or excluded due to their performance on formal testing, medical dx, or because had not benefitted from previous communication services. � Other external factors such as restrictive interpretations of educational, vocational, or medical necessity in regards to insurance regulations; lack of education; and/or lack of funds have been used to restrict access to AAC Beukelman and Mirenda, 2005
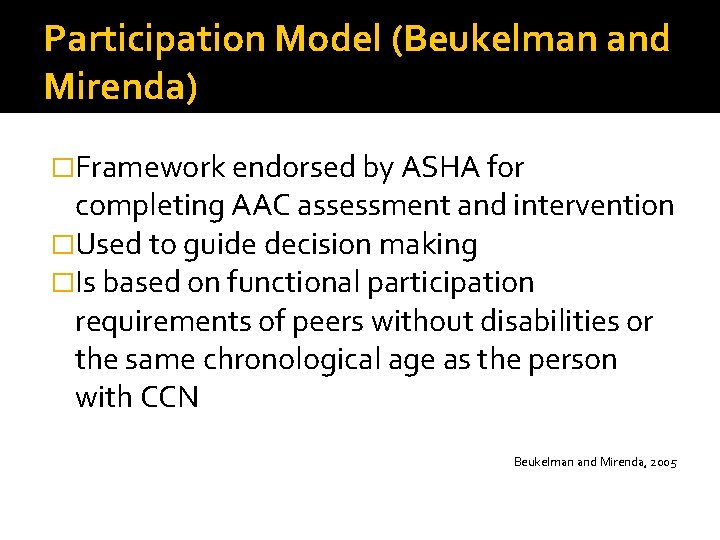
Participation Model (Beukelman and Mirenda) �Framework endorsed by ASHA for completing AAC assessment and intervention �Used to guide decision making �Is based on functional participation requirements of peers without disabilities or the same chronological age as the person with CCN Beukelman and Mirenda, 2005
Principles of Participation Model �Principle 1: Assessment is on-going �Principle 2: Intervention to facilitate meaningful communication and participation �Principle 3: Identification of actual and potential opportunity barriers �Principle 4: Everyone can communication. Everyone does communicate. �Principle 5: Technology alone does not make a competent communicator
Assessment �Dynamic Process �Usually consists of four phases
Phases 1. 2. 3. 4. Referral for AAC Assessment and Intervention for Today Detailed Assessment for Tomorrow Follow-up Assessment

Opportunity Barriers �Policy Barriers �Practice Barriers �Knowledge Barriers �Skill Barriers �Attitude Barriers
Access Barriers �Capabilities, attitudes and resources of potential AAC users �Lack of mobility, difficulty with fine motor control, cognitive limitations, sensoryperceptual impairments
Family Preferences Most important constraint May include concerns about -System portability, durability, and appearance -Time and skills required to learn system -Quality and intelligibility of speech output -The “naturalness” of the communication exchange � Family and potential AAC user may not share same concerns � �
Limitations of Norm-Referenced Tests �Usually can’t be delivered in a standardized manner �Must adapt �Norms are NOT appropriate for severe disabilities
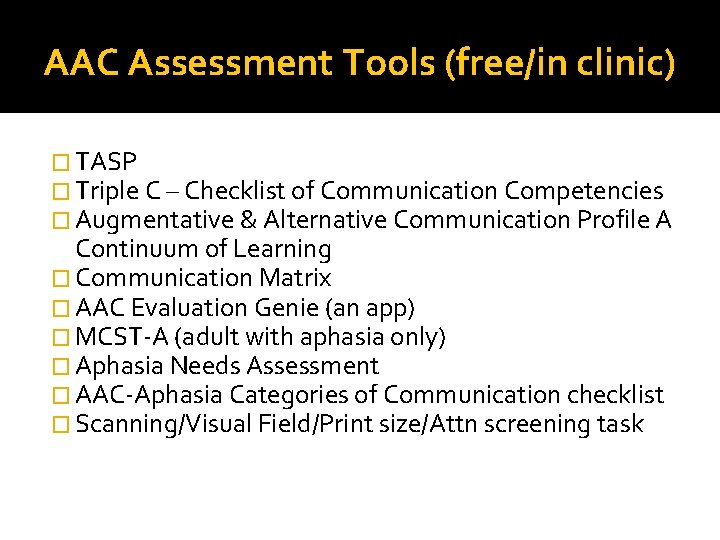
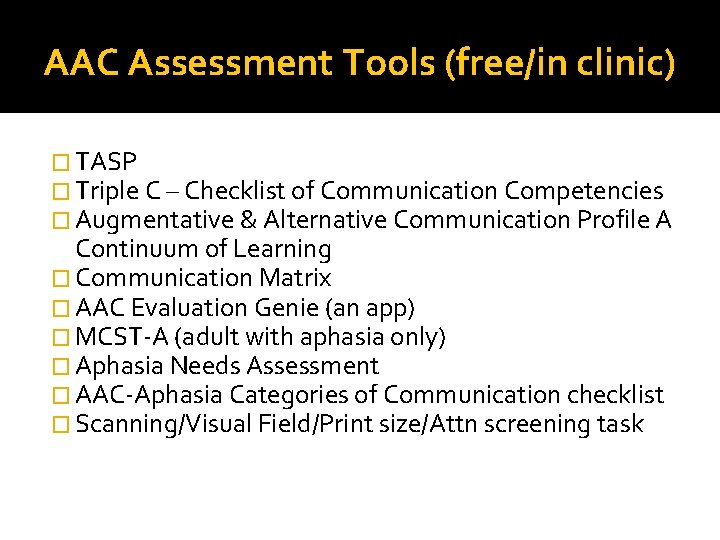
AAC Assessment Tools (free/in clinic) � TASP � Triple C – Checklist of Communication Competencies � Augmentative & Alternative Communication Profile A Continuum of Learning � Communication Matrix � AAC Evaluation Genie (an app) � MCST-A (adult with aphasia only) � Aphasia Needs Assessment � AAC-Aphasia Categories of Communication checklist � Scanning/Visual Field/Print size/Attn screening task
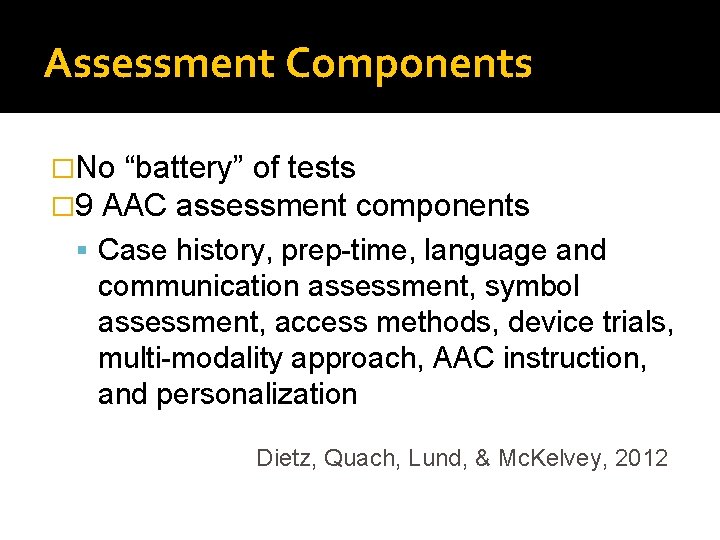
Assessment Components �No “battery” of tests � 9 AAC assessment components Case history, prep-time, language and communication assessment, symbol assessment, access methods, device trials, multi-modality approach, AAC instruction, and personalization Dietz, Quach, Lund, & Mc. Kelvey, 2012
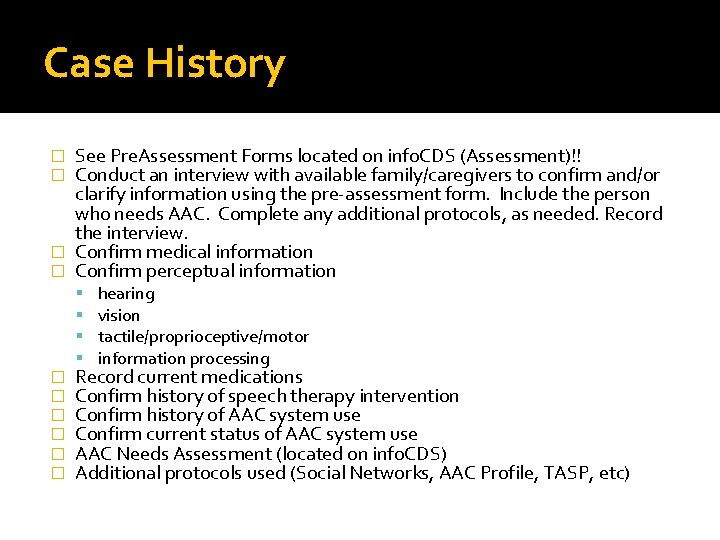
Case History See Pre. Assessment Forms located on info. CDS (Assessment)!! Conduct an interview with available family/caregivers to confirm and/or clarify information using the pre-assessment form. Include the person who needs AAC. Complete any additional protocols, as needed. Record the interview. � Confirm medical information � Confirm perceptual information � � � � hearing vision tactile/proprioceptive/motor information processing Record current medications Confirm history of speech therapy intervention Confirm history of AAC system use Confirm current status of AAC system use AAC Needs Assessment (located on info. CDS) Additional protocols used (Social Networks, AAC Profile, TASP, etc)
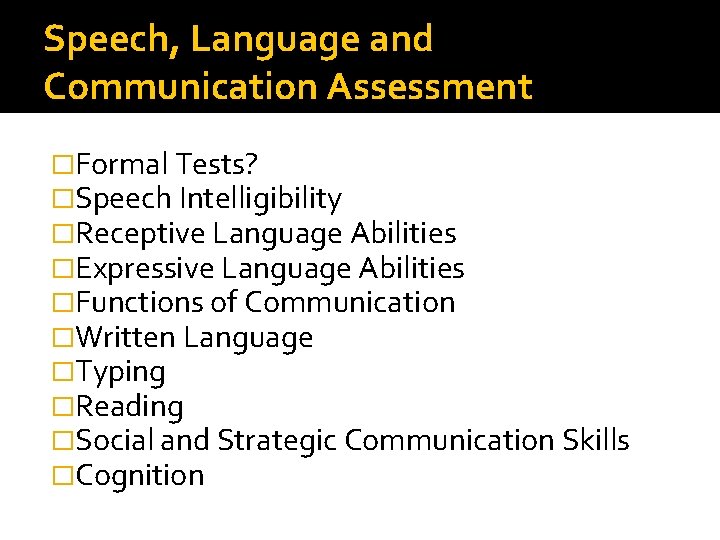
Speech, Language and Communication Assessment �Formal Tests? �Speech Intelligibility �Receptive Language Abilities �Expressive Language Abilities �Functions of Communication �Written Language �Typing �Reading �Social and Strategic Communication Skills �Cognition
Assessment of Individual �Linguistic Emergent Context-Dependent Independent
Assessment Goals �Emergent �Context-Dependent �Independent �Literacy
Symbol Selection �Symbols are learned! �Dependent on sensory, cognitive, and perceptual issues, as well as individual preference �Consider representational skills �No hierarchy
Sensory and perceptual �Vision Unaided and functional Corrected with glasses? Accommodations needed? Concerns in absence of acuity difficulty �Hearing Unaided and functional Hearing aids? Modifications needed?
Positioning and Access �Positioning for Access �Hand Use �Head use �Means of Mobility �Anticipated transportation of AAC system
Communication partners �Collect this information through observation and informal assessment �Social Networks
Environments �Work with communication partners to ID all environments and what needs to be communicated in each of these
Communication Topics �Consider topics person needs to communicate about �Consider functions person needs to communicate about
Feature Matching �First assess capabilities of user �Then predict devices that may work for individual based on language representation, hardware, access methods, feedback methods, and current needs/capabilities of person �See info. CDS form
Feature Matching (How might it fail the person with CCN? ) � Focus is solely on current needs and abilities without considering anticipated future needs and capabilities. � AAC team overemphasizes (caughtup) with device features. � Fails to take into account the user’s preferences while negotiating a device recommendation that will support current or future abilities for generative communication. � A “match” and capabilities to use a device does not account for all of the components needed for success. The whole is more than the sum of it’s parts. Rush-Helling
Device Trials If appropriate, can contact vendors, utilize lending library, etc… 30 day trial options If asking a representative to join your session, familiarize yourself with the software by downloading and trialing the free editing software or apps provided by the companies. Remember that the representative is there to introduce their equipment and the features of the equipment. S/he is NOT there to do the evaluation for you. � Consider: � � � Length of trial Techniques used to elicit communication Operational skills Size of display and symbols Access methods Cognitive Access (navigation, support, size, number of symbols, etc)
Personalization �Customization should include placing highly motivating photographs, videos, or sound effects on the devices. Highly motivating activities/items should be gathered to present to the client.
AAC instruction � Introduce motivating activities/highly interesting topics of conversation. Model appropriate use of the device without pressure to perform. Invite the client to try out the device following your model to meet communication functions (requesting, commenting, responding). Offer suggestions of possible messages the patient could try out. Model navigation to desired messages. Avoid “show me the __” language for this portion of the assessment. Model and expect functional, purposeful communication. With time, assess the client’s ability to remember and reproduce your model for direct communication, navigation, and various functions of language (greeting, commenting, requesting. . . ).
Complete the AAC Evaluation Per Medicare and most funding sources, your evaluation report must include: -Current communication impairment (type, severity, rec/exp language skills, speech, cognitive ability, and anticipated course of tx) -Mobility status and physical abilities, hearing and vision **Must state that client possesses cognitive and physical abilities to effectively use the SGD and accessories** -Assessment of individual’s daily communication needs and why they could not be met using other natural modes of communication -Other SGDs and modes considered/trialed -Rationale for recommended SGD and accessories -Description of functional communication goals -Treatment plan that includes schedule -If client has a previously issued SGD, must include info regarding functional benefit of new system -Disclosure and signature
Post-Evaluation Recommendations and Follow-Up Planning �Recommended strategies and tools �Recommended accessories and equipment �Treatment plan and follow up Intervention Schedule If follow up services are not available, a high tech speech generating device is not recommended TREATMENT GOALS: See Dynamic AAC Goals Grid and Planning Guide (DAGG-2) The Goals Grid should be completed to determine areas of strength and need. Partners should be consulted regarding priority goals targeting increasing function and independence.
Patient/Family Support �Patient, Family, Caregiver, Therapist, Manufacturer �Who will provide: Therapy to address goals? Initial training? Initial Customization? Ongoing Training and Modifications? Maintenance of Device? Warranty Maintenance Management?
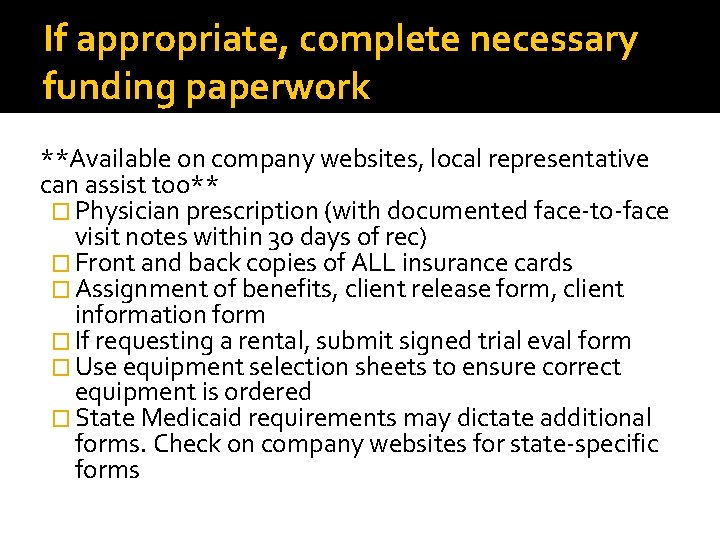
If appropriate, complete necessary funding paperwork **Available on company websites, local representative can assist too** � Physician prescription (with documented face-to-face visit notes within 30 days of rec) � Front and back copies of ALL insurance cards � Assignment of benefits, client release form, client information form � If requesting a rental, submit signed trial eval form � Use equipment selection sheets to ensure correct equipment is ordered � State Medicaid requirements may dictate additional forms. Check on company websites for state-specific forms
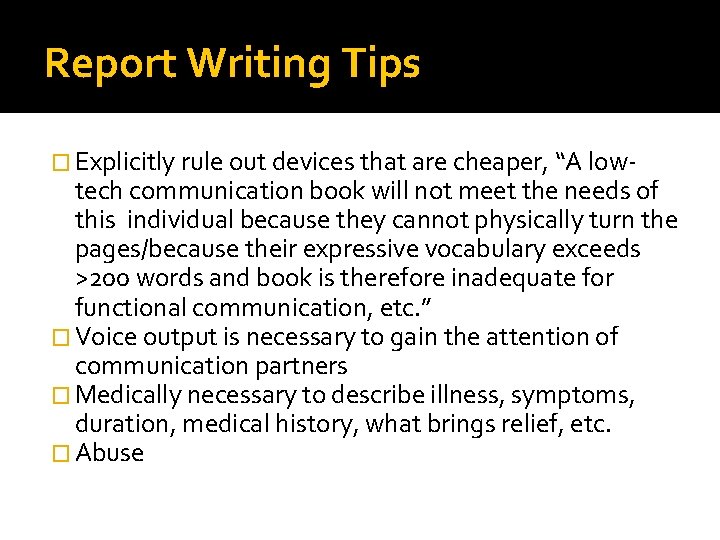
Report Writing Tips � Explicitly rule out devices that are cheaper, “A low- tech communication book will not meet the needs of this individual because they cannot physically turn the pages/because their expressive vocabulary exceeds >200 words and book is therefore inadequate for functional communication, etc. ” � Voice output is necessary to gain the attention of communication partners � Medically necessary to describe illness, symptoms, duration, medical history, what brings relief, etc. � Abuse
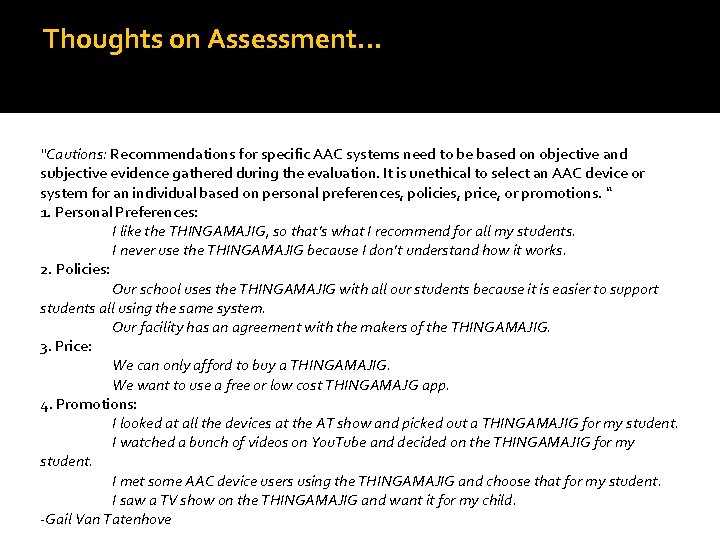
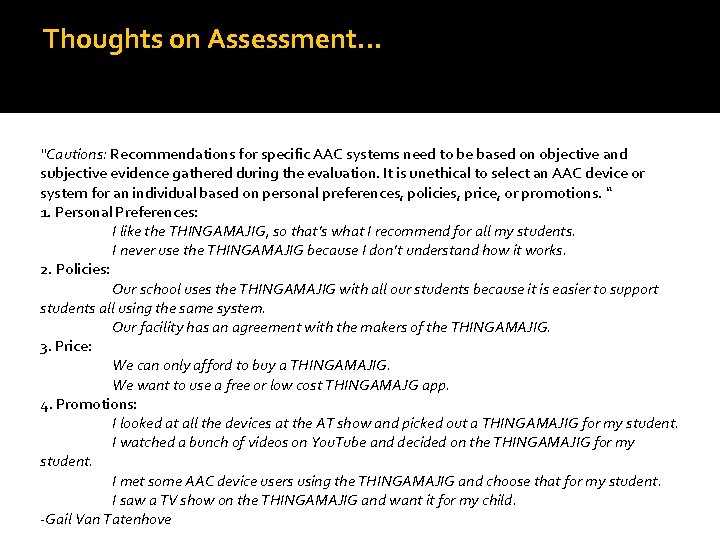
Thoughts on Assessment… “Cautions: Recommendations for specific AAC systems need to be based on objective and subjective evidence gathered during the evaluation. It is unethical to select an AAC device or system for an individual based on personal preferences, policies, price, or promotions. “ 1. Personal Preferences: I like the THINGAMAJIG, so that’s what I recommend for all my students. I never use the THINGAMAJIG because I don’t understand how it works. 2. Policies: Our school uses the THINGAMAJIG with all our students because it is easier to support students all using the same system. Our facility has an agreement with the makers of the THINGAMAJIG. 3. Price: We can only afford to buy a THINGAMAJIG. We want to use a free or low cost THINGAMAJG app. 4. Promotions: I looked at all the devices at the AT show and picked out a THINGAMAJIG for my student. I watched a bunch of videos on You. Tube and decided on the THINGAMAJIG for my student. I met some AAC device users using the THINGAMAJIG and choose that for my student. I saw a TV show on the THINGAMAJIG and want it for my child. -Gail Van Tatenhove
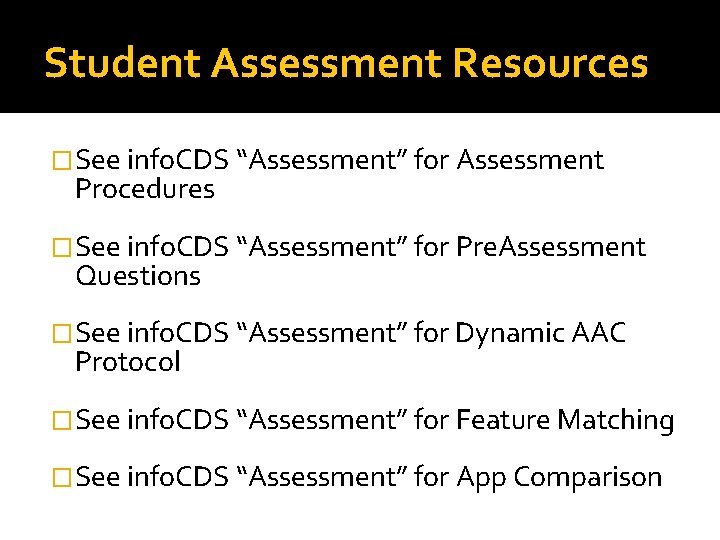
Student Assessment Resources �See info. CDS “Assessment” for Assessment Procedures �See info. CDS “Assessment” for Pre. Assessment Questions �See info. CDS “Assessment” for Dynamic AAC Protocol �See info. CDS “Assessment” for Feature Matching �See info. CDS “Assessment” for App Comparison
Funding �Medical necessity The “medical purpose” of SGDs and the “medical need” for SGDs, is to treat severe expressive communication impairment that precludes individuals from meeting all daily communication needs using natural communication methods
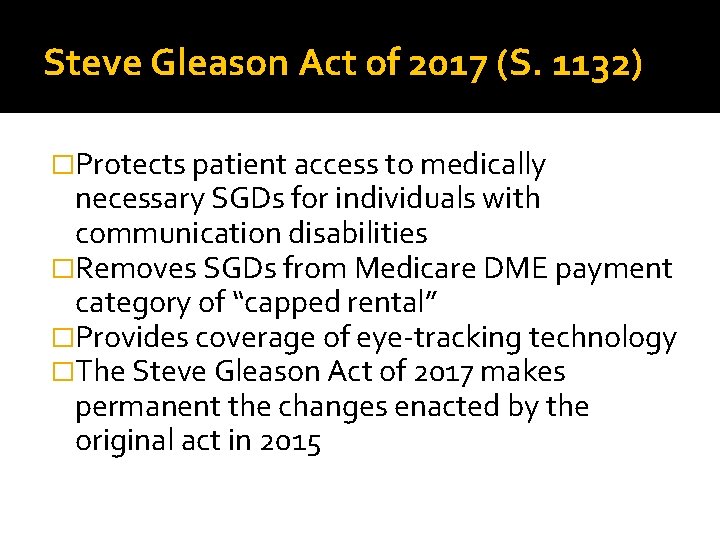
Steve Gleason Act of 2017 (S. 1132) �Protects patient access to medically necessary SGDs for individuals with communication disabilities �Removes SGDs from Medicare DME payment category of “capped rental” �Provides coverage of eye-tracking technology �The Steve Gleason Act of 2017 makes permanent the changes enacted by the original act in 2015
How do I help my patient obtain an SGD? �The process for getting a device has not changed. The speech-language pathologist performs a comprehensive evaluation and sends the report to the patient’s physician. The physician attaches this report to the order for the SGD. The manufacturer provides the device and submits the claim to Medicare for reimbursement. The SLP should work with the manufacturer to ensure that the evaluation meets the coverage guidelines.
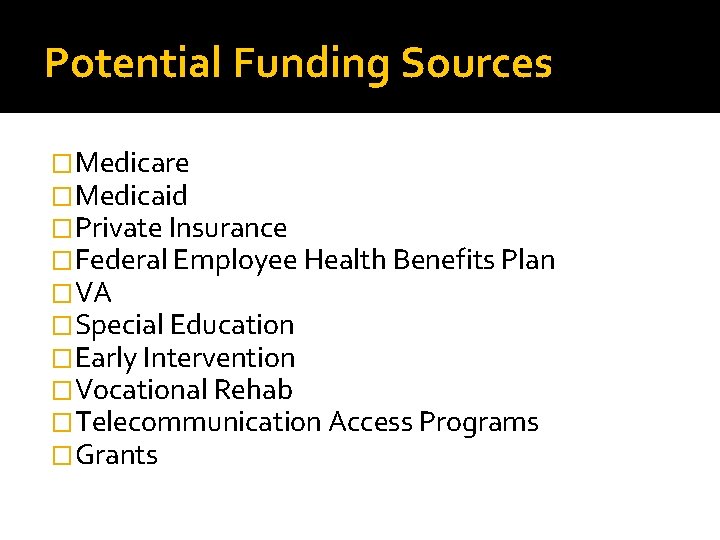
Potential Funding Sources �Medicare �Medicaid �Private Insurance �Federal Employee Health Benefits Plan �VA �Special Education �Early Intervention �Vocational Rehab �Telecommunication Access Programs �Grants
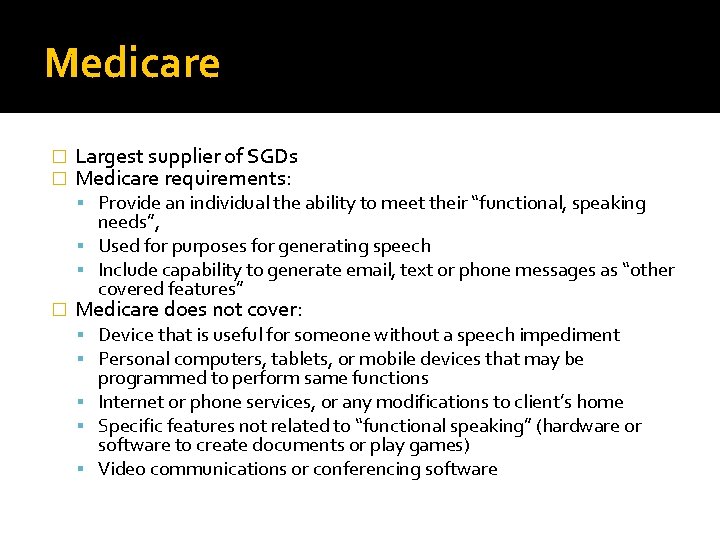
Medicare � � Largest supplier of SGDs Medicare requirements: Provide an individual the ability to meet their “functional, speaking � needs”, Used for purposes for generating speech Include capability to generate email, text or phone messages as “other covered features” Medicare does not cover: Device that is useful for someone without a speech impediment Personal computers, tablets, or mobile devices that may be programmed to perform same functions Internet or phone services, or any modifications to client’s home Specific features not related to “functional speaking” (hardware or software to create documents or play games) Video communications or conferencing software
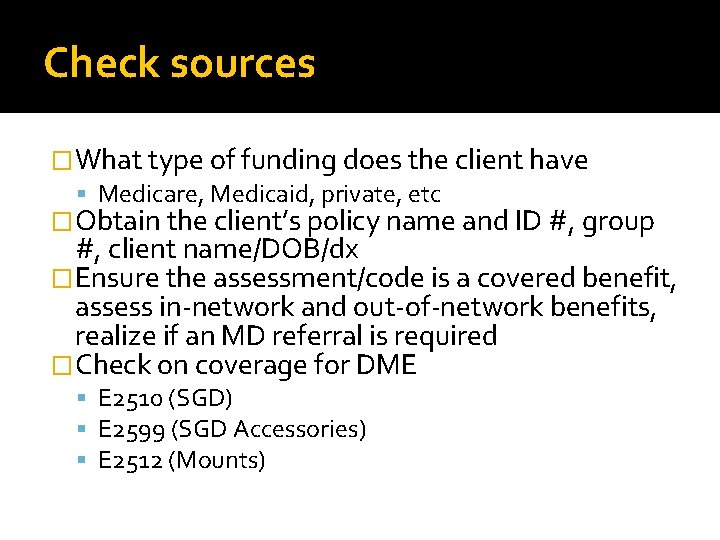
Check sources �What type of funding does the client have Medicare, Medicaid, private, etc �Obtain the client’s policy name and ID #, group #, client name/DOB/dx �Ensure the assessment/code is a covered benefit, assess in-network and out-of-network benefits, realize if an MD referral is required �Check on coverage for DME E 2510 (SGD) E 2599 (SGD Accessories) E 2512 (Mounts)
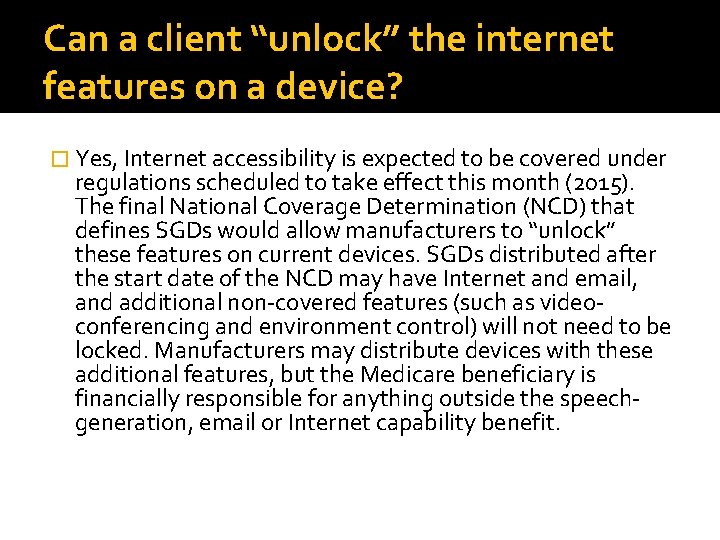
Can a client “unlock” the internet features on a device? � Yes, Internet accessibility is expected to be covered under regulations scheduled to take effect this month (2015). The final National Coverage Determination (NCD) that defines SGDs would allow manufacturers to “unlock” these features on current devices. SGDs distributed after the start date of the NCD may have Internet and email, and additional non-covered features (such as videoconferencing and environment control) will not need to be locked. Manufacturers may distribute devices with these additional features, but the Medicare beneficiary is financially responsible for anything outside the speechgeneration, email or Internet capability benefit.
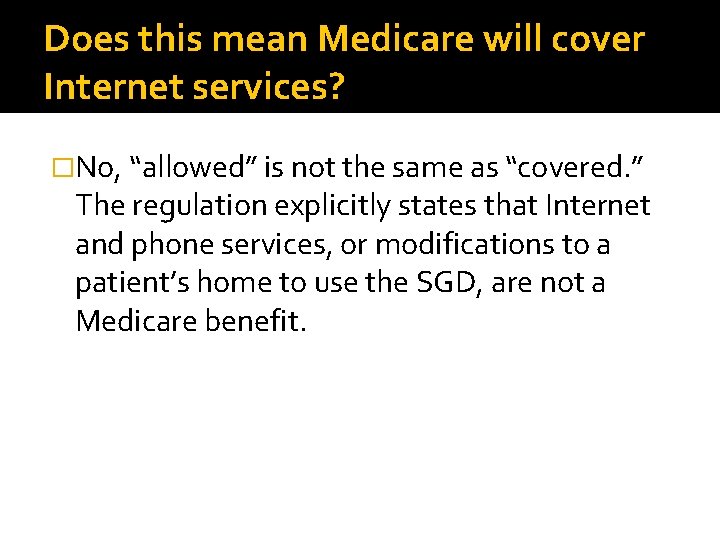
Does this mean Medicare will cover Internet services? �No, “allowed” is not the same as “covered. ” The regulation explicitly states that Internet and phone services, or modifications to a patient’s home to use the SGD, are not a Medicare benefit.
Will Medicare cover eye-tracking accessories? �Yes, eye-tracking will be covered. Although the rule was not explicit, Medicare officials have assured ASHA that medically necessary accessories are a covered benefit. Regional Medicare policies state that accessories are covered when reasonable and necessary.
Can my currently hospitalized patient get an SGD? �The hospital/inpatient facility is responsible for ensuring that patients have the medical equipment they need. However, an SGD for home use cannot be ordered while the patient is under the inpatient (Part A) benefit. Medicare covers SGDs for home use as an outpatient (Part B) benefit.
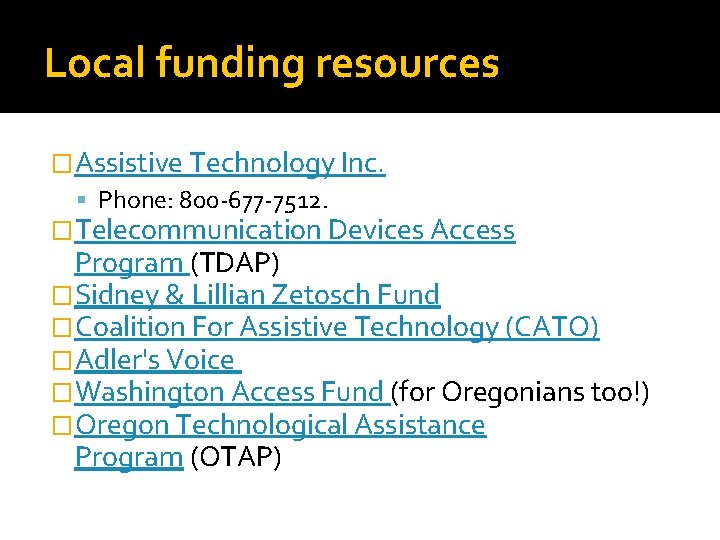
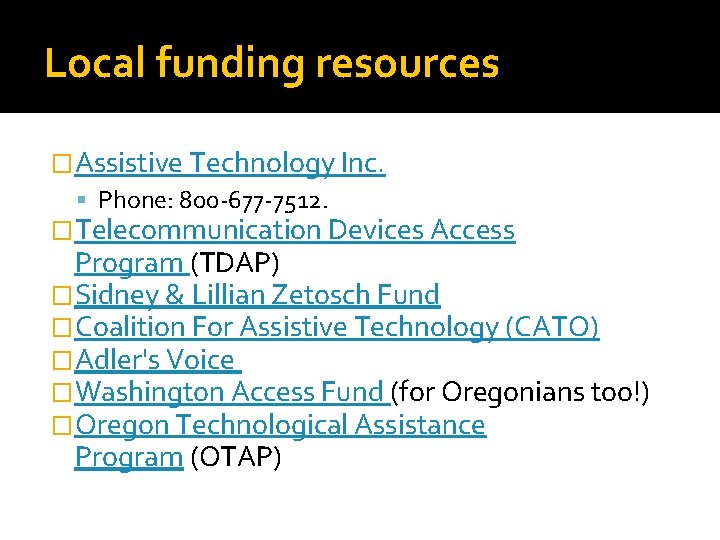
Local funding resources �Assistive Technology Inc. Phone: 800 -677 -7512. �Telecommunication Devices Access Program (TDAP) �Sidney & Lillian Zetosch Fund �Coalition For Assistive Technology (CATO) �Adler's Voice �Washington Access Fund (for Oregonians too!) �Oregon Technological Assistance Program (OTAP)
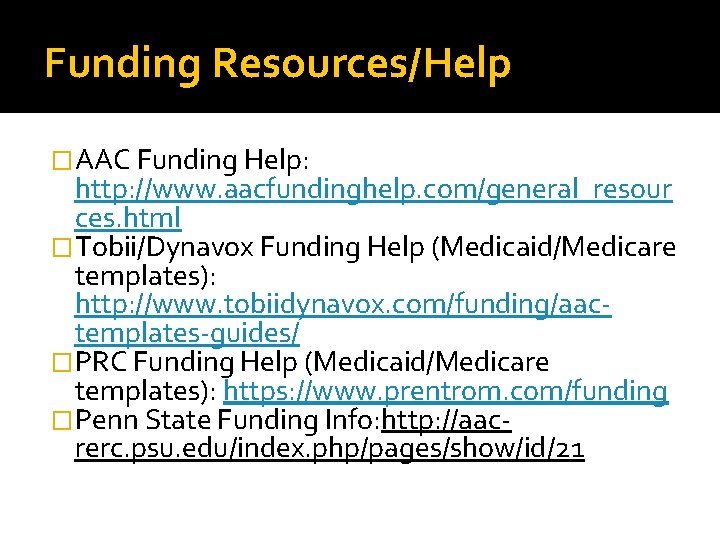
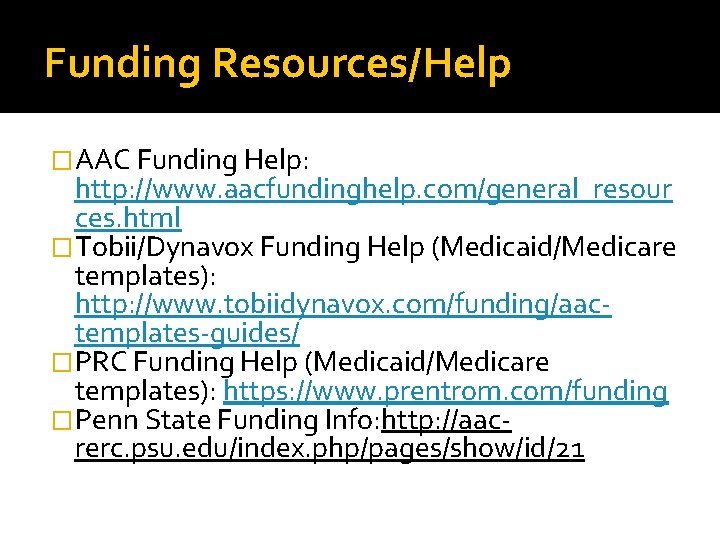
Funding Resources/Help �AAC Funding Help: http: //www. aacfundinghelp. com/general_resour ces. html �Tobii/Dynavox Funding Help (Medicaid/Medicare templates): http: //www. tobiidynavox. com/funding/aactemplates-guides/ �PRC Funding Help (Medicaid/Medicare templates): https: //www. prentrom. com/funding �Penn State Funding Info: http: //aacrerc. psu. edu/index. php/pages/show/id/21
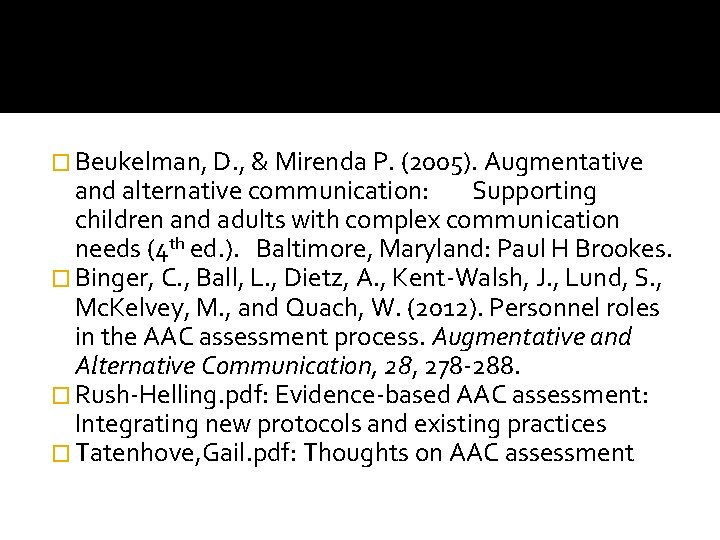
� Beukelman, D. , & Mirenda P. (2005). Augmentative and alternative communication: Supporting children and adults with complex communication needs (4 th ed. ). Baltimore, Maryland: Paul H Brookes. � Binger, C. , Ball, L. , Dietz, A. , Kent-Walsh, J. , Lund, S. , Mc. Kelvey, M. , and Quach, W. (2012). Personnel roles in the AAC assessment process. Augmentative and Alternative Communication, 28, 278 -288. � Rush-Helling. pdf: Evidence-based AAC assessment: Integrating new protocols and existing practices � Tatenhove, Gail. pdf: Thoughts on AAC assessment
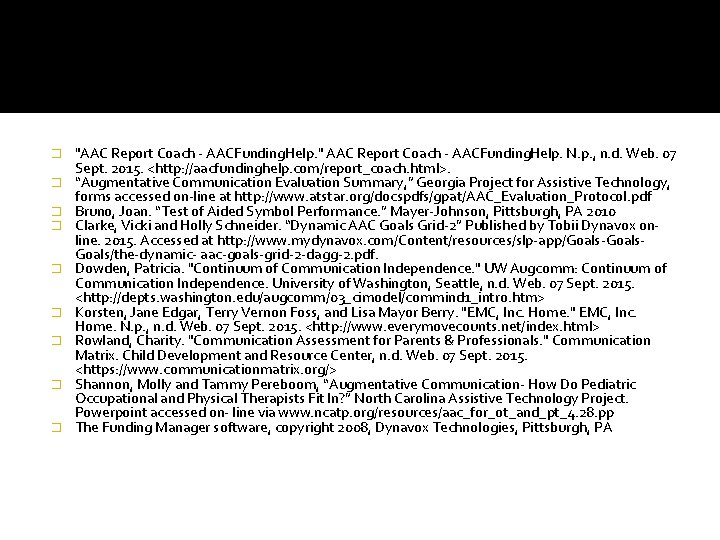
� � � � � "AAC Report Coach - AACFunding. Help. " AAC Report Coach - AACFunding. Help. N. p. , n. d. Web. 07 Sept. 2015. <http: //aacfundinghelp. com/report_coach. html>. “Augmentative Communication Evaluation Summary, ” Georgia Project for Assistive Technology, forms accessed on-line at http: //www. atstar. org/docspdfs/gpat/AAC_Evaluation_Protocol. pdf Bruno, Joan. “Test of Aided Symbol Performance. ” Mayer-Johnson, Pittsburgh, PA 2010 Clarke, Vicki and Holly Schneider. “Dynamic AAC Goals Grid-2” Published by Tobii Dynavox online. 2015. Accessed at http: //www. mydynavox. com/Content/resources/slp-app/Goals-Goals/the-dynamic- aac-goals-grid-2 -dagg-2. pdf. Dowden, Patricia. "Continuum of Communication Independence. " UW Augcomm: Continuum of Communication Independence. University of Washington, Seattle, n. d. Web. 07 Sept. 2015. <http: //depts. washington. edu/augcomm/03_cimodel/commind 1_intro. htm> Korsten, Jane Edgar, Terry Vernon Foss, and Lisa Mayor Berry. "EMC, Inc. Home. " EMC, Inc. Home. N. p. , n. d. Web. 07 Sept. 2015. <http: //www. everymovecounts. net/index. html> Rowland, Charity. "Communication Assessment for Parents & Professionals. " Communication Matrix. Child Development and Resource Center, n. d. Web. 07 Sept. 2015. <https: //www. communicationmatrix. org/> Shannon, Molly and Tammy Pereboom, “Augmentative Communication- How Do Pediatric Occupational and Physical Therapists Fit In? ” North Carolina Assistive Technology Project. Powerpoint accessed on- line via www. ncatp. org/resources/aac_for_ot_and_pt_4. 28. pp The Funding Manager software, copyright 2008, Dynavox Technologies, Pittsburgh, PA