A Variety of Neurological and Muscular Disorders 2009



























- Slides: 143
A Variety of Neurological and Muscular Disorders 2009

Objectives n n n Be able to identify disease processes given clinical (H&P, lab, radiographic, etc) findings. Given a differential diagnosis be able to choose a clinical finding that helps identify the actual diagnosis. Be able to discuss the pathophysiology, treatment and prognosis of the diseases presented to the extent these characteristics are presented.
Diagnostic Catechism n n n Is there something wrong with the patient? If so, where is the abnormality? If so, what is the abnormality?
Is there something wrong with the patient? n Remember, some abnormalities are considered normal variants u u Reflexes (without clonus, asymmetry or other problems) are non-pathological even if abnormal. Aging Changes F F Decreased Reflexes Decreased Muscle Bulk Tremor Decreased Proprioception and Vibratory Sensation in LE
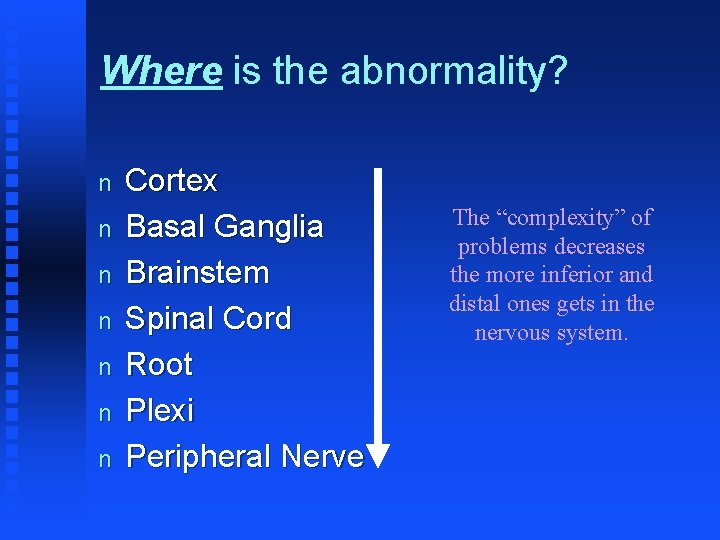
Where is the abnormality? n n n n Cortex Basal Ganglia Brainstem Spinal Cord Root Plexi Peripheral Nerve The “complexity” of problems decreases the more inferior and distal ones gets in the nervous system.
What is the abnormality? n n n Allergic CTD Congenital Defect Genetic Metabolic-Degenerative Inflammatory

n n n Physical Injury Tumors Toxic Vascular Psychiatric Remember the best diagnosis is the simplest diagnosis that explains all of the clinical findings!
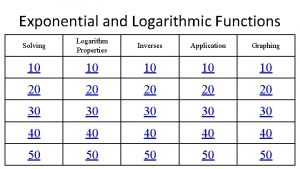
How to cover this material n Algorithms/Cases & Mini lectures u Neuro guide (demo)
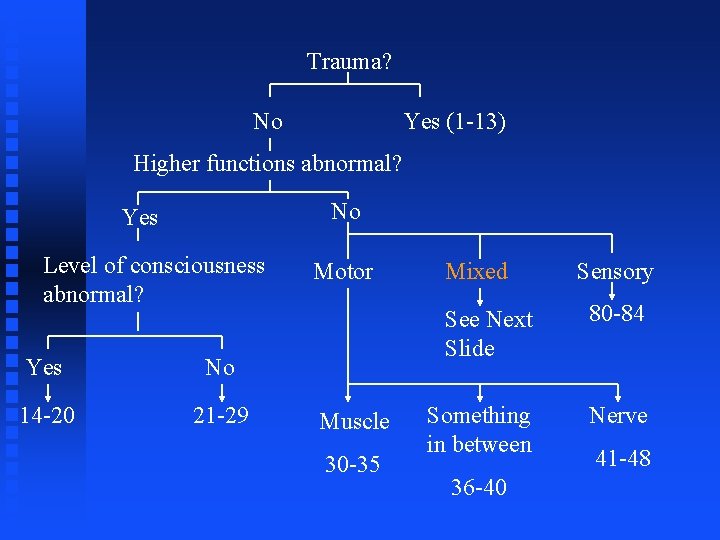
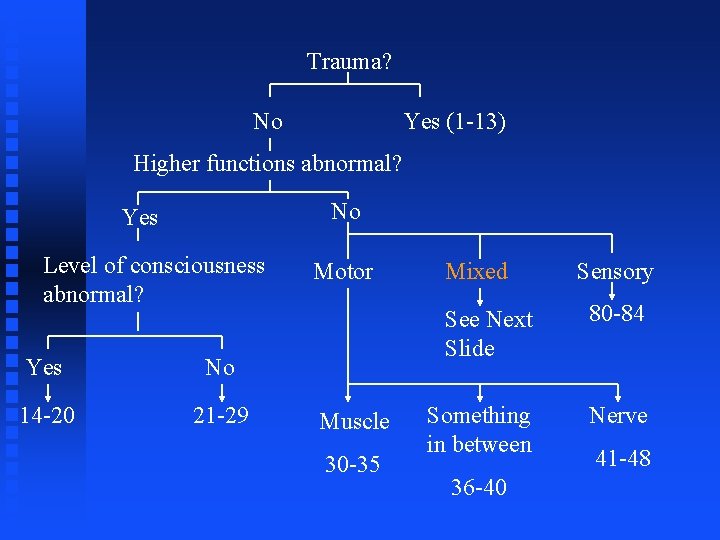
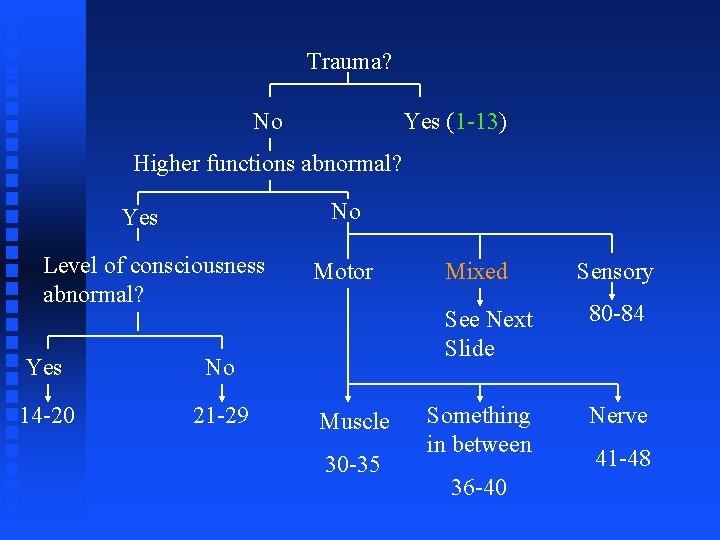
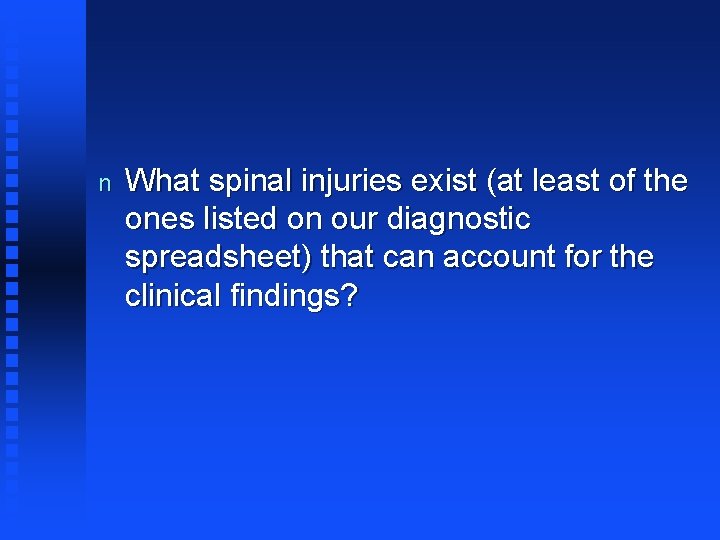
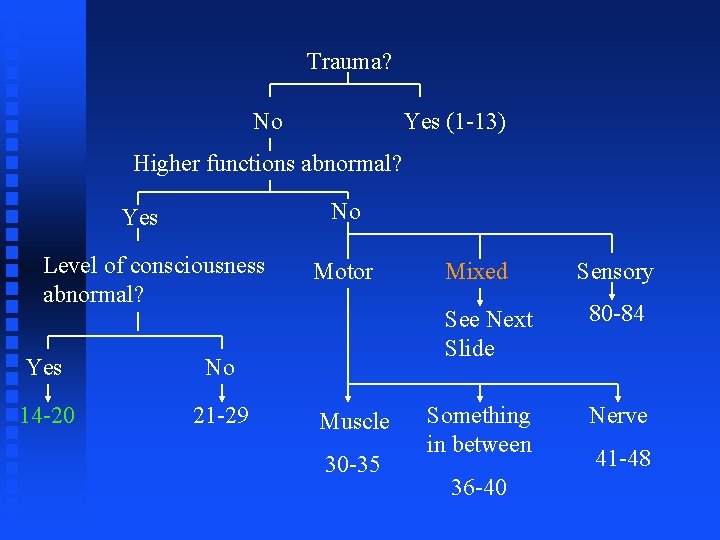
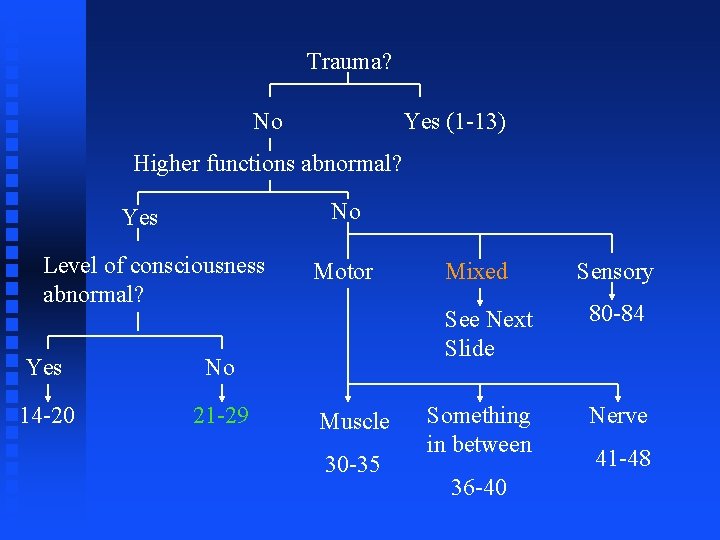
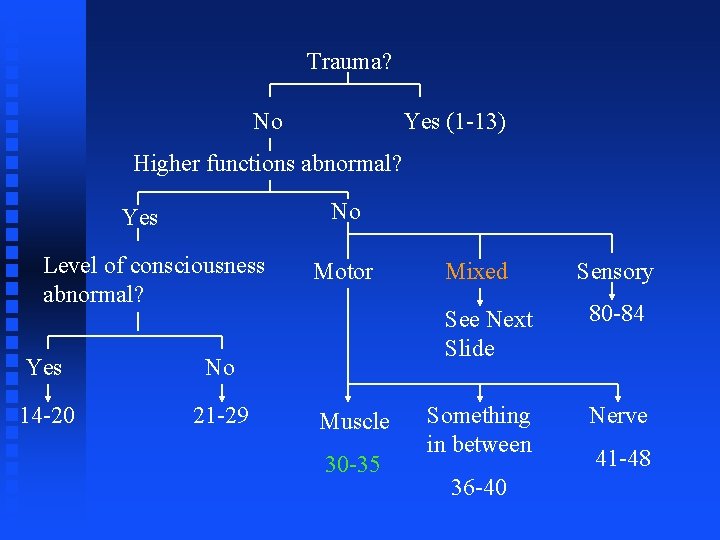
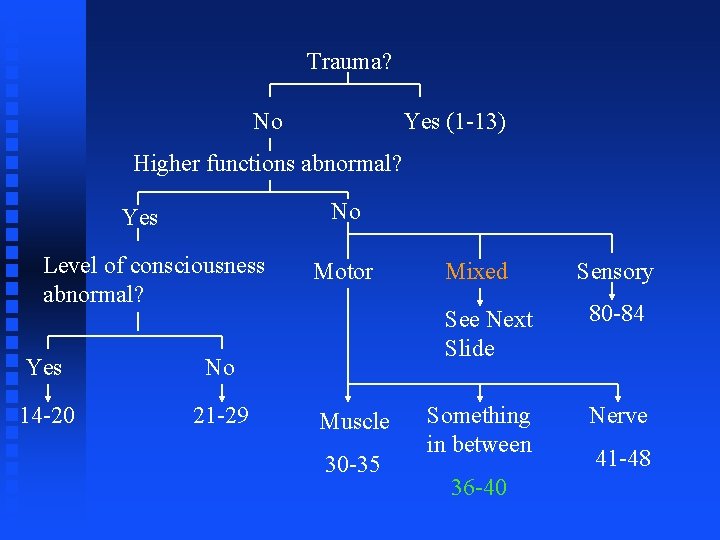
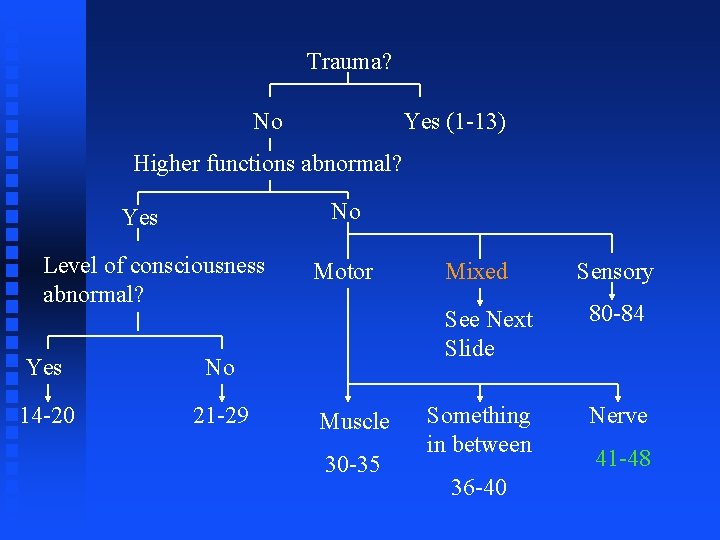
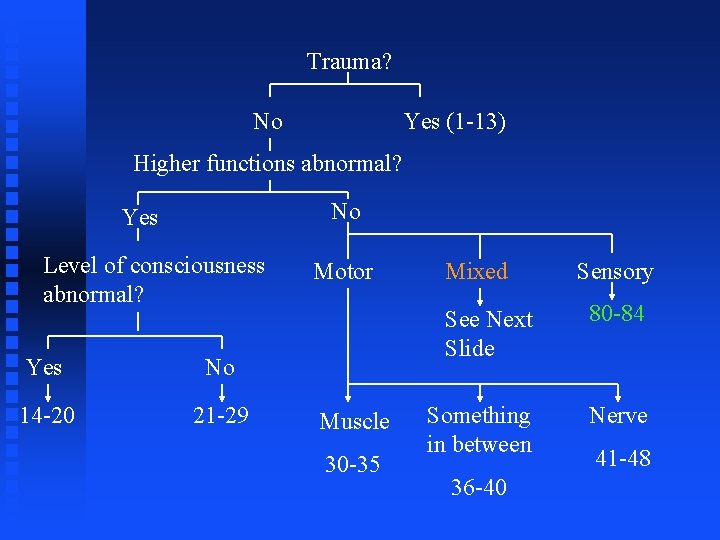
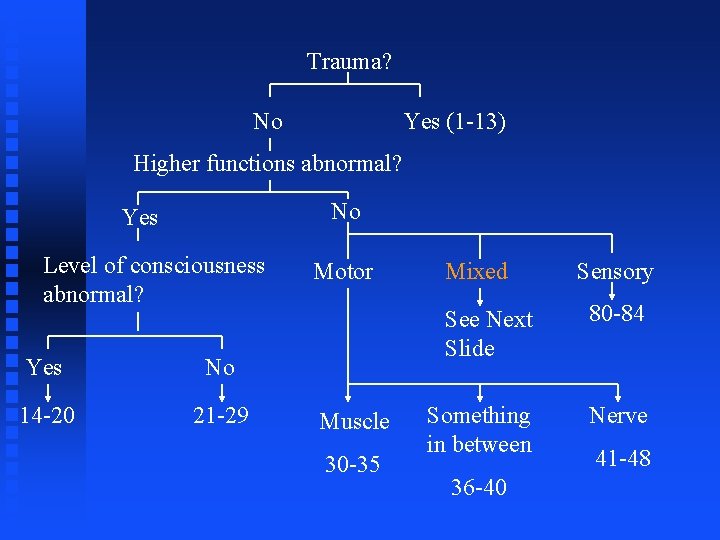
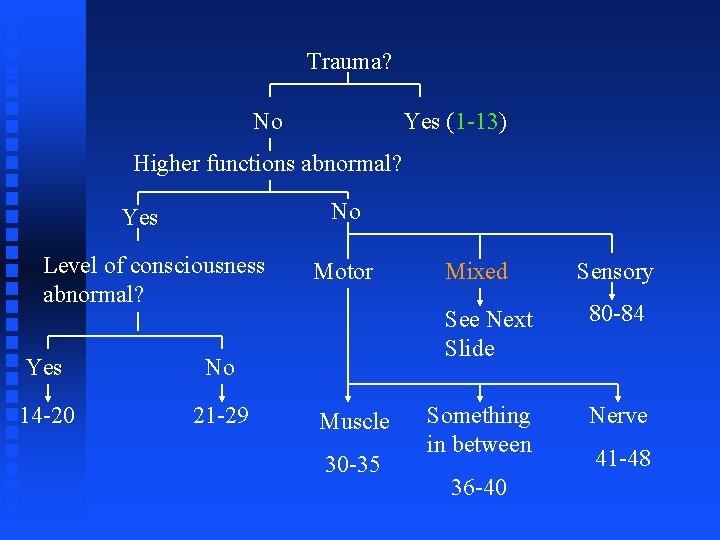
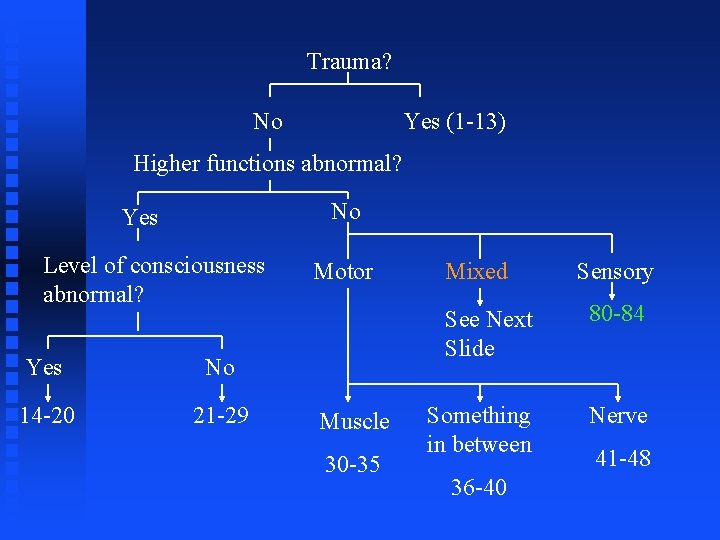
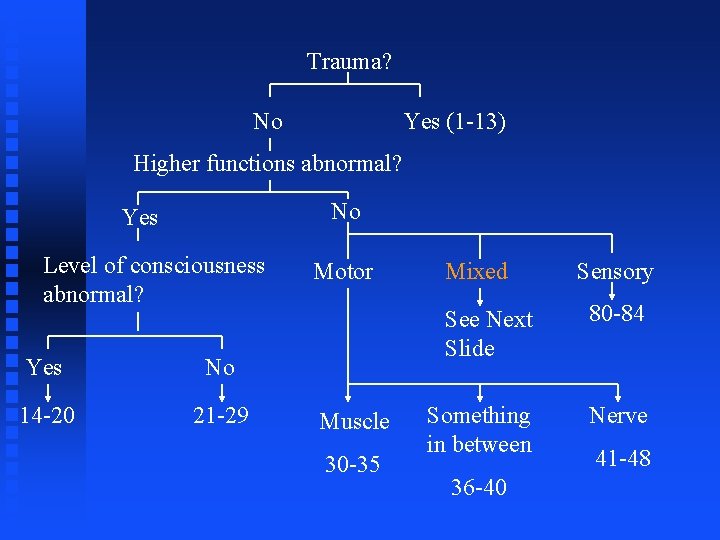
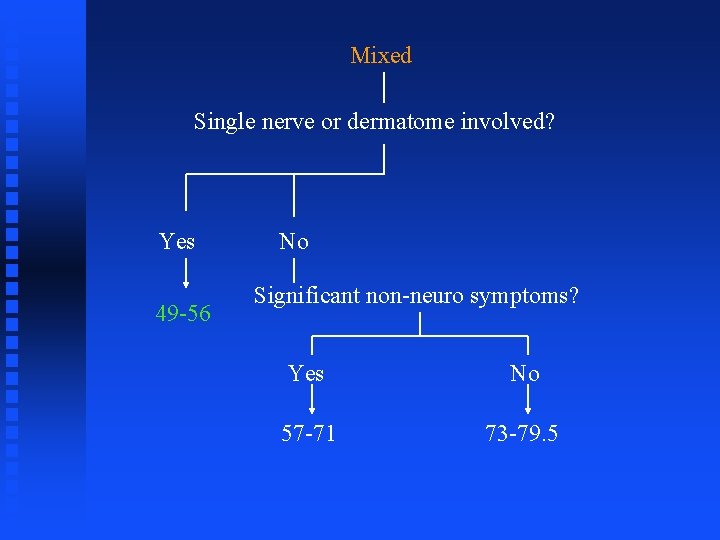
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48

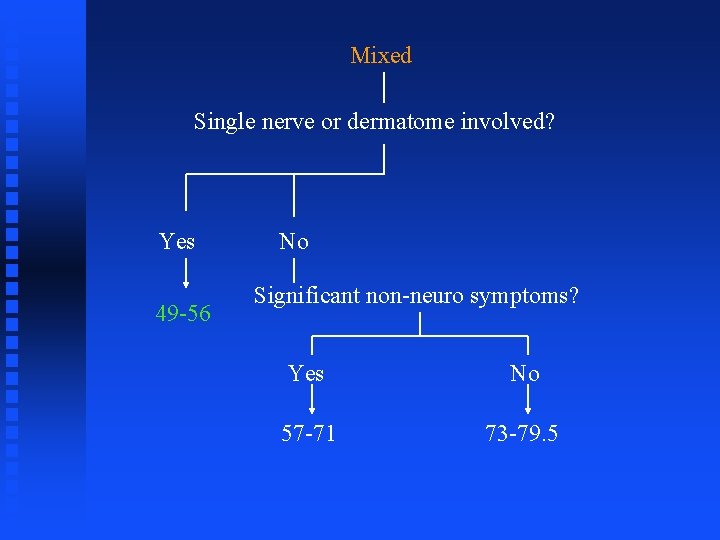
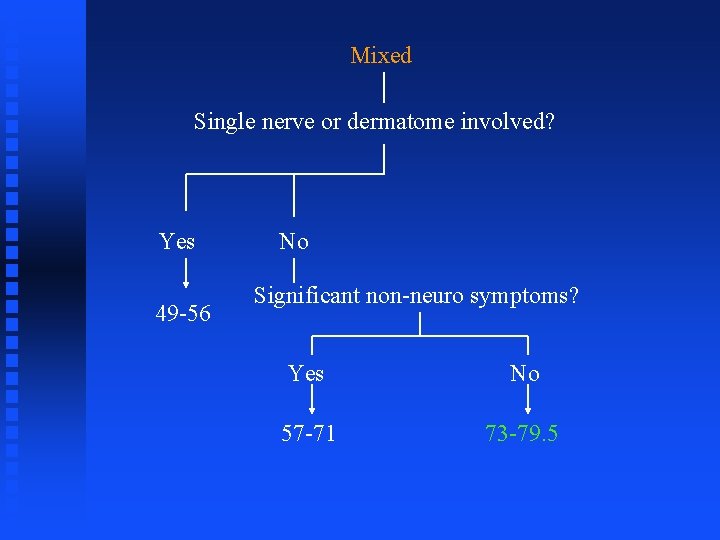
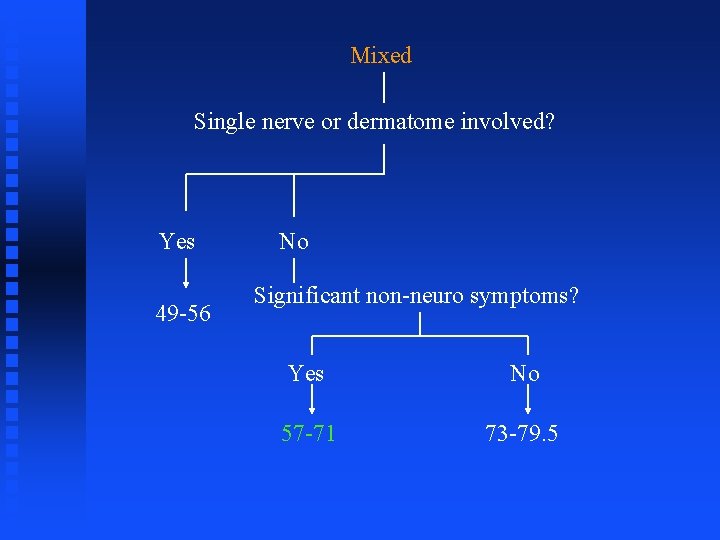
Mixed Single nerve or dermatome involved? Yes 49 -56 No Significant non-neuro symptoms? Yes No 57 -71 73 -79. 5
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48

Section 1 -13
Case #1 u u u Batter gets “beaned” without helmet on side of head LOC followed by at least a partial return of function Second depression of consciousness
What is differential diagnosis, i. e. what head injury types are associated with a depressed level of consciousness? u Ones that involve brain injury! u See Trauma (#1 -13)

n Brain injuries as seen via computed tomography. Clockwise from upper left, these CT scans show a left frontal epidural hematoma; a right frontal subdural hematoma with midline shift and ventricular compression; a subarachnoid hemorrhage in the left sylvian fissure; diffuse axonal injury with diffuse edema, obliteration of the ventricular system, and scattered hyperdense foci throughout the parenchyma (consistent with shear injury); and a second example of subdural hematoma. n mdchoice. com/emed/images/cover/12 -01 Fig. jpg
General Points about Head Injuries n n Patients who have lost consciousness for 2 minutes or more following head injury should be admitted to the hospital for observation, as should patients with focal neurologic deficits, lethargy, or skull fractures. Sometimes surgical evacuation will be necessary. Why and in whom?
n Because injury to the spine may have accompanied head trauma, cervical spine radiographs (especially in the lateral projection) should always be obtained in comatose patients and in patients with severe neck pain or a deficit possibly related to cord compression.
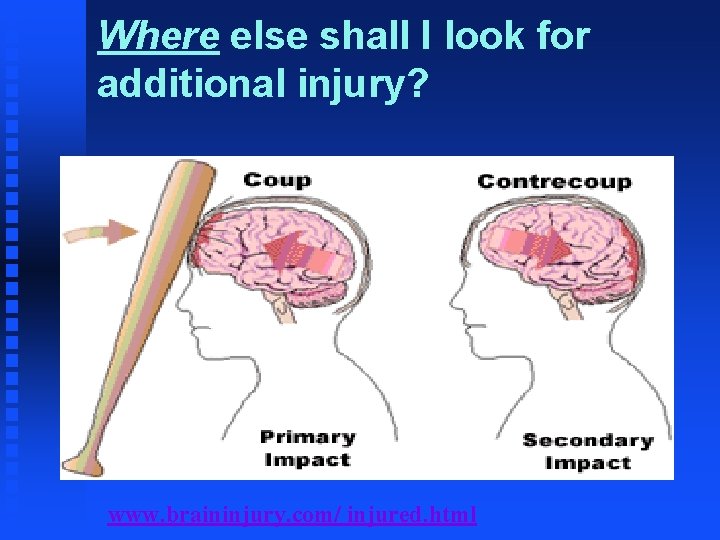
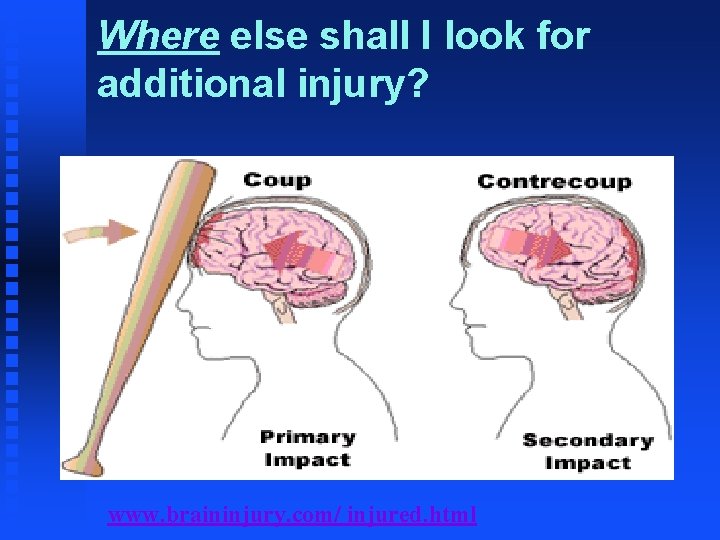
Where else shall I look for additional injury? www. braininjury. com/ injured. html
u u Increased intracranial pressure may result from ventilatory obstruction, abnormal neck position, seizures, dilutional hyponatremia, or cerebral edema; an intracranial hematoma requiring surgical evacuation may also be responsible. Why care? F F Contralateral hemiparesis with ipsilateral fixed and dilated pupil (or vice versa) (herniation) Blood flow to brain
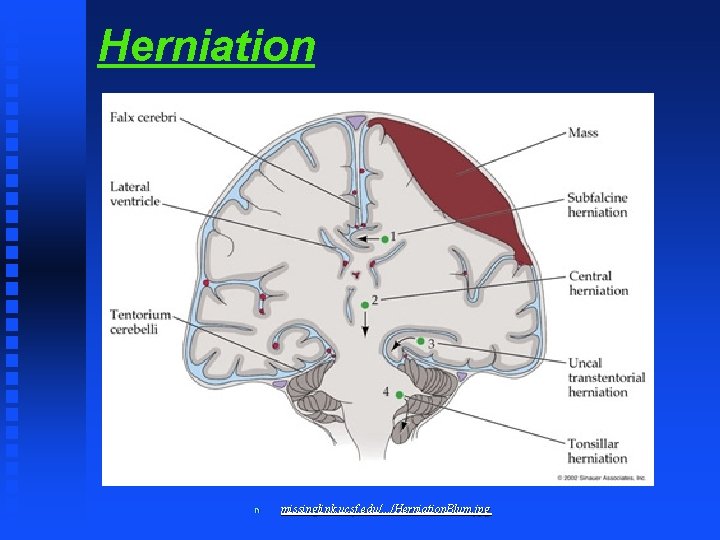
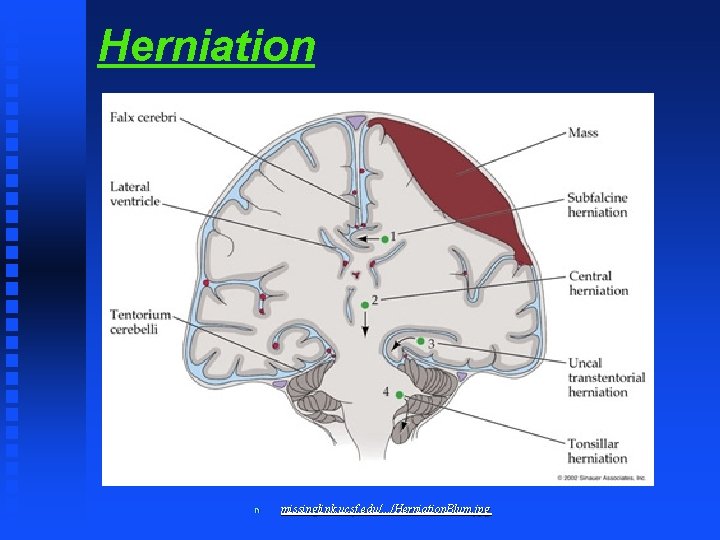
Herniation n missinglink. ucsf. edu/. . . /Herniation. Blum. jpg
n Other measures that may be necessary to reduce intracranial pressure include induced hyperventilation, intravenous mannitol infusion, and intravenous furosemide. u n How do you suppose these treatments work? Corticosteroids provide no benefit in this context.

Case #2 u u Batter gets “beaned” without helmet on side of head. Grabs head screaming in pain and falls to ground but does not lose consciousness
What is differential diagnosis, i. e. what head injury types are associated without a depressed level of consciousness?
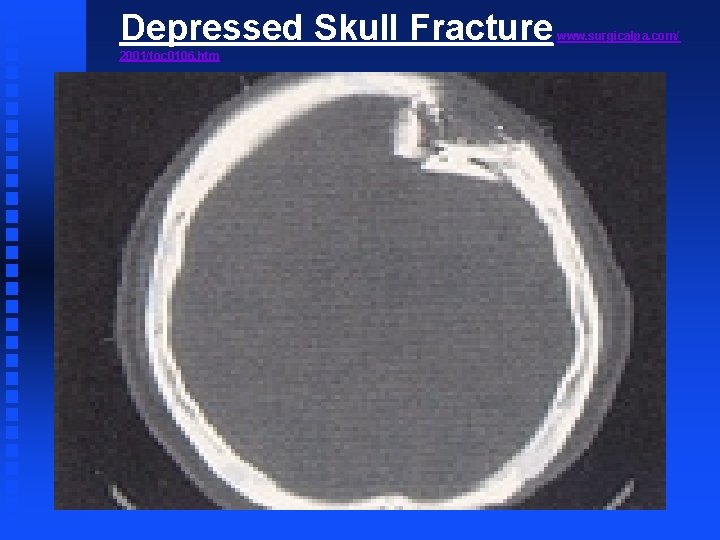
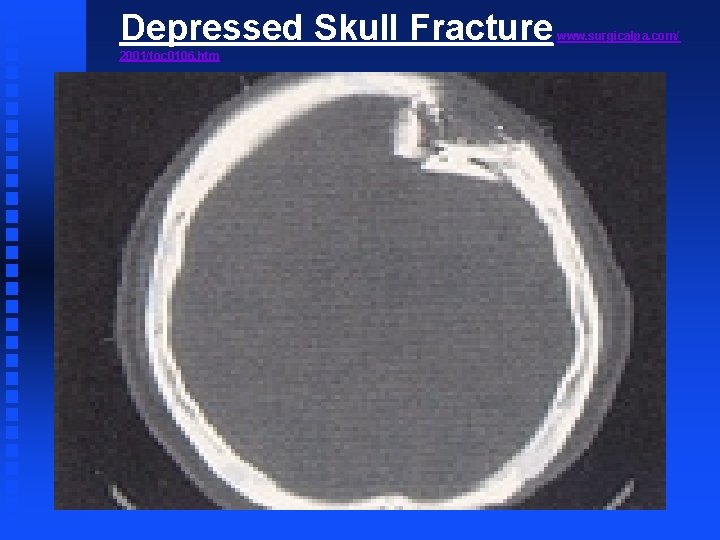
Depressed Skull Fracture 2001/toc 0106. htm www. surgicalpa. com/
n Remember there is a difference between skull injuries and brain injuries, though they can certainly occur together. n Scalp lacerations and depressed skull fractures require specific Rx.

n n Basilar skull fractures can be difficult to see radiologically Clinically suspect if: u CSF otorrhea or rhinorrhea via “ring sign” - CSF separates from blood when placed on filter paper and produces a clinically detectable sign—ring sign, double ring sign, or halo sign. F u u u Measure the level of beta-2 -transferrin in the fluid? Ecchymosis in mastoid area (Battle’s sign) Hemotympanum Raccoon eyes

Raccoon Eyes n www. surgical-tutor. org. uk/core/ trauma/head_trauma. htm
Raccoon Face www. acm. vt. edu/~clint/download/imagedump/racc. . .

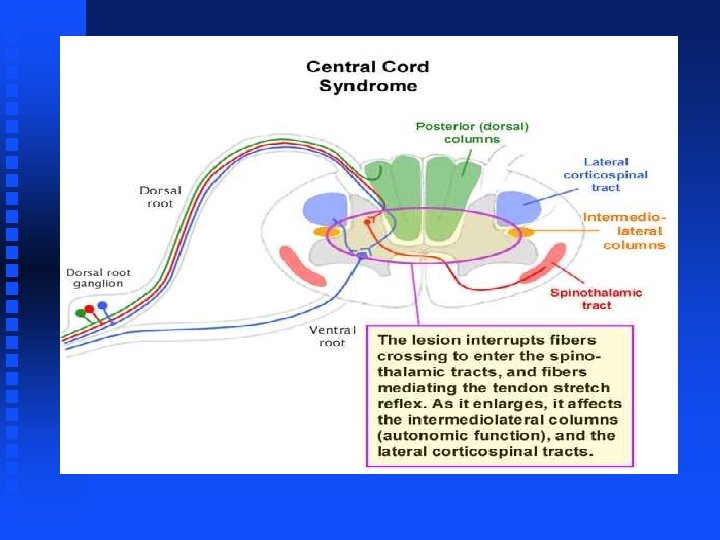
Case #3 n n A patient suffers a penetrating injury to the right thoracic spine. The patient has weakness and decreased proprioception in the right leg and decreased pain and temperature sensation in the left leg.
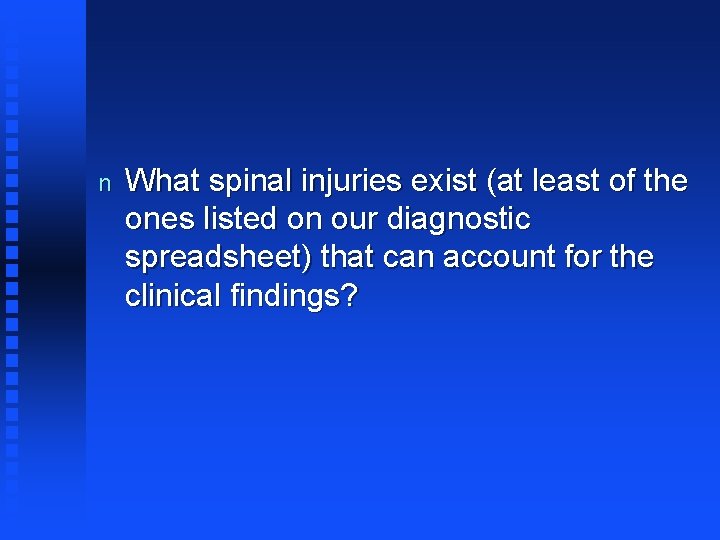
n What spinal injuries exist (at least of the ones listed on our diagnostic spreadsheet) that can account for the clinical findings?

http: //medinfo. ufl. edu/year 2/neuro/review/images/fig 02. jpg
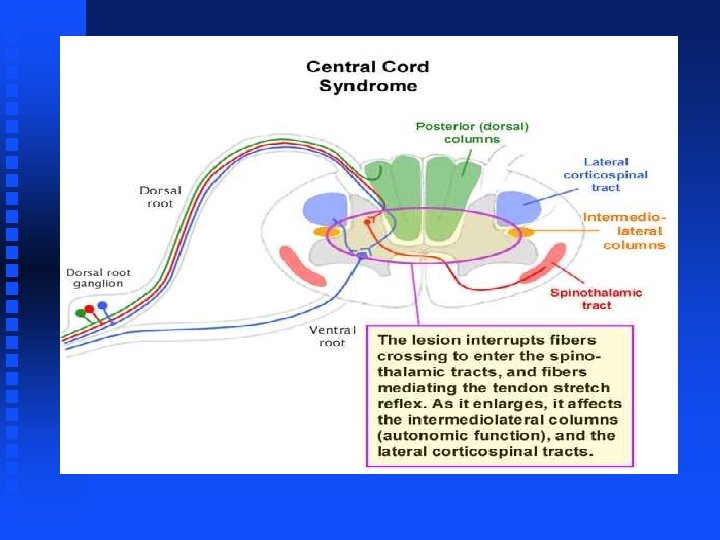
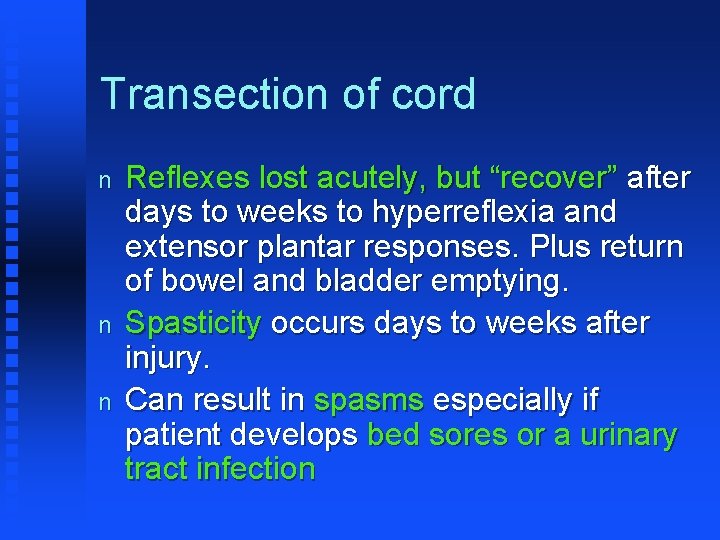
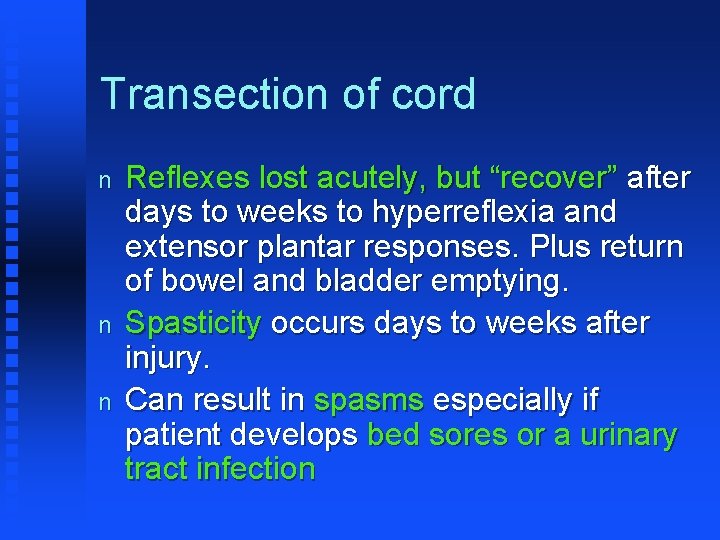
Transection of cord n n n Reflexes lost acutely, but “recover” after days to weeks to hyperreflexia and extensor plantar responses. Plus return of bowel and bladder emptying. Spasticity occurs days to weeks after injury. Can result in spasms especially if patient develops bed sores or a urinary tract infection

n n Treatment of the injury consists of immobilization and - if there is cord compression - decompressive laminectomy and fusion. Early treatment with high doses of corticosteroids has been shown to improve neurologic recovery if commenced within 8 hours after injury. Anatomic realignment of the spinal cord by traction and other orthopedic procedures is important. Subsequent care of the residual neurologic deficit paraplegia or quadriplegia - requires treatment of spasticity and care of the skin, bladder, and bowels.
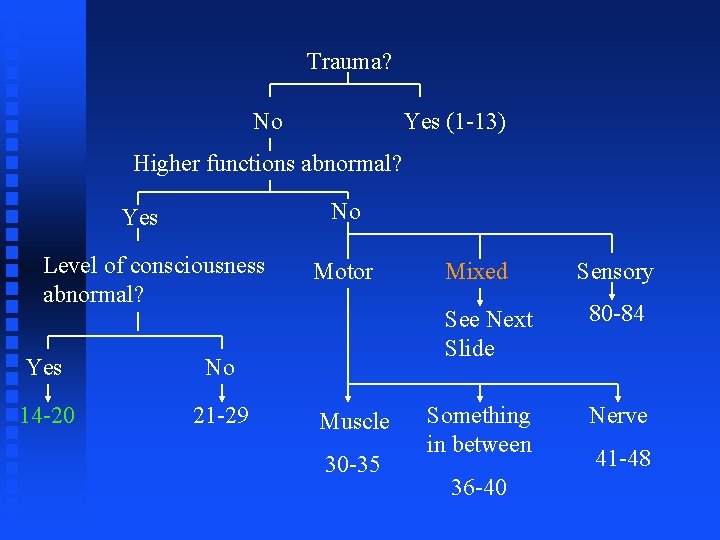
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section 14 -20
Case #1 n A 50 yo w male suffers a heart attack and cardiac arrest. A pulse is regained after 15 minutes of ACLS, but the patient has not awakened. Indeed, he is completely unresponsive (except for brainstem reflexes) and has remained so for several days. What do you think is going on?
Coma n n n Structural lesions of bilateral cerebrum or brainstem What can be learned from pupils, breathing, posturing? Only perform LP if CT negative
Breathing patterns n Cheyne-Stokes ("Torsades like") - May occur with bihemispheric or diencephalic disease or in metabolic disorders. n Central neurogenic hyperventilation - Occurs with lesions of the brainstem tegmentum. n Apneustic breathing (in which there are prominent endinspiratory pauses) - Suggests damage at the pontine level (eg, due to basilar artery occlusion). n Atactic breathing (a completely irregular pattern of breathing with deep and shallow breaths occurring randomly) - Associated with lesions of the lower pontine tegmentum and medulla.
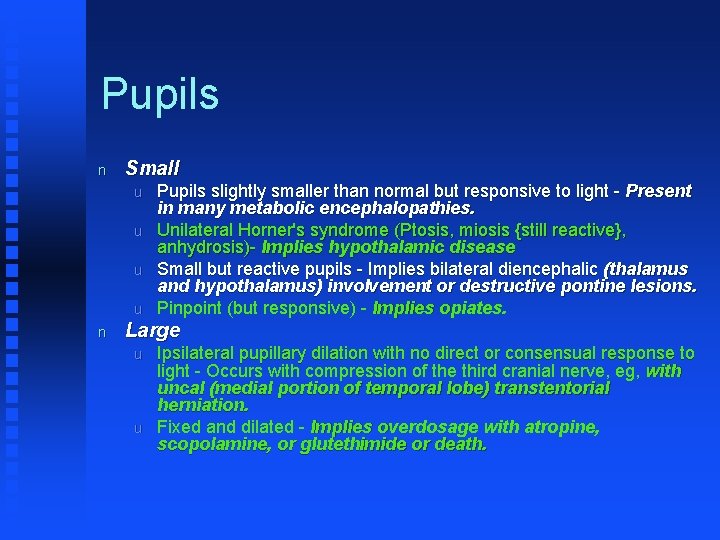
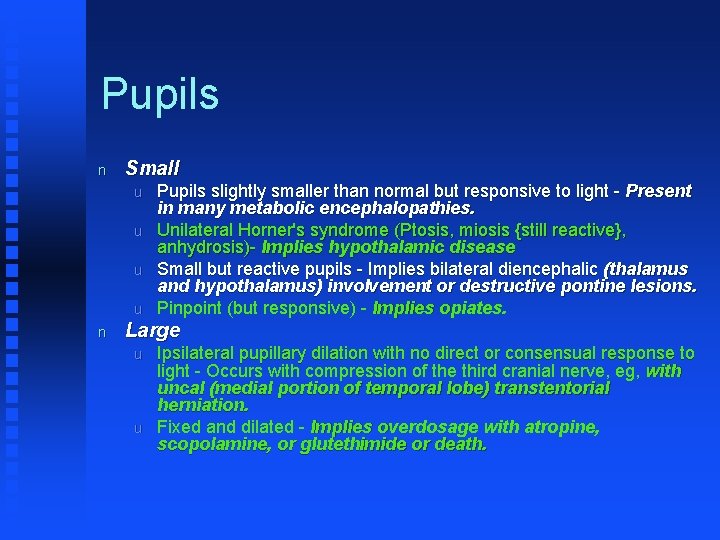
Pupils n Small u u n Pupils slightly smaller than normal but responsive to light - Present in many metabolic encephalopathies. Unilateral Horner's syndrome (Ptosis, miosis {still reactive}, anhydrosis)- Implies hypothalamic disease Small but reactive pupils - Implies bilateral diencephalic (thalamus and hypothalamus) involvement or destructive pontine lesions. Pinpoint (but responsive) - Implies opiates. Large u u Ipsilateral pupillary dilation with no direct or consensual response to light - Occurs with compression of the third cranial nerve, eg, with uncal (medial portion of temporal lobe) transtentorial herniation. Fixed and dilated - Implies overdosage with atropine, scopolamine, or glutethimide or death.
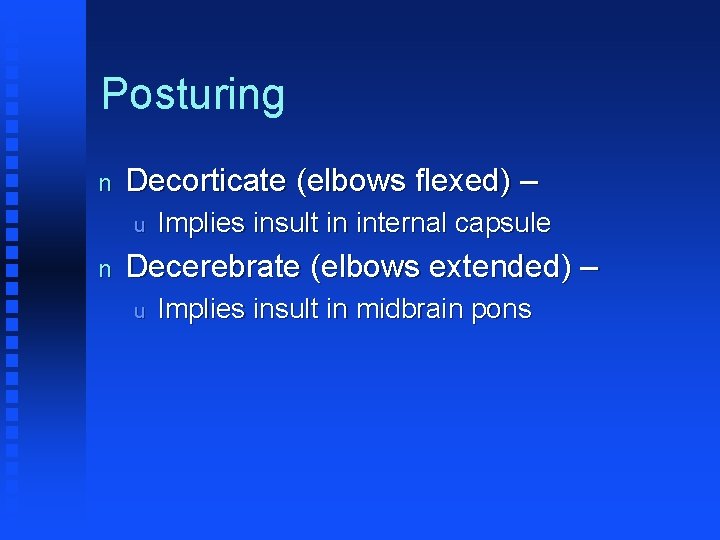
Posturing n Decorticate (elbows flexed) – u n Implies insult in internal capsule Decerebrate (elbows extended) – u Implies insult in midbrain pons
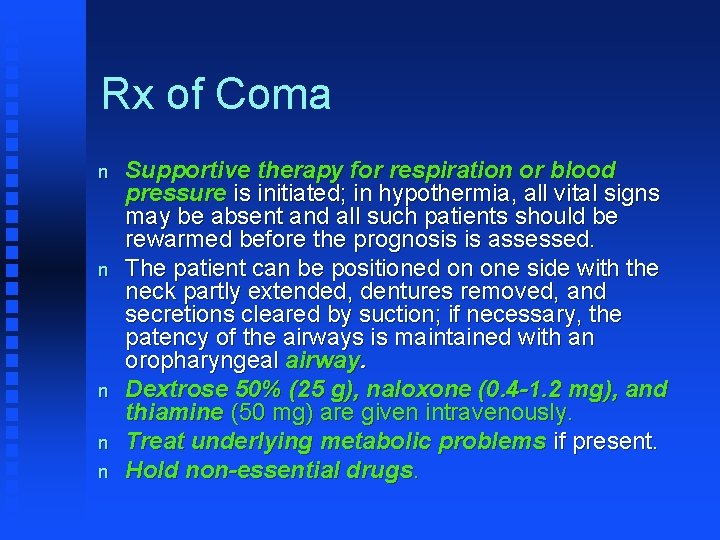
Rx of Coma n n n Supportive therapy for respiration or blood pressure is initiated; in hypothermia, all vital signs may be absent and all such patients should be rewarmed before the prognosis is assessed. The patient can be positioned on one side with the neck partly extended, dentures removed, and secretions cleared by suction; if necessary, the patency of the airways is maintained with an oropharyngeal airway. Dextrose 50% (25 g), naloxone (0. 4 -1. 2 mg), and thiamine (50 mg) are given intravenously. Treat underlying metabolic problems if present. Hold non-essential drugs.
Comments about some of the other disorders in the differential.
Stupor? n n No, because while level of consciousness is depressed in stupor, the patient will respond to repeated vigorous stimulation. Bascially stupor is like a coma but less severe; it is a “coma-lite”, if you will.
Brain Death n n n All brainstem reflexes (pupillary, corneal, oculovestibular, oculocephalic, oropharyngeal) absent for minimum of 6 hours. No posturing Spinal reflexes may be present
Locked-in State n n Patient IS conscious and alert but doesn’t look like it. Ophthalmoplegia present except for vertical plane Caused by acute destructive lesion of the pons Can also be associated with diseases of the peripheral motor nerves or paralysis produced by the administration of neuromuscular blocking agents.
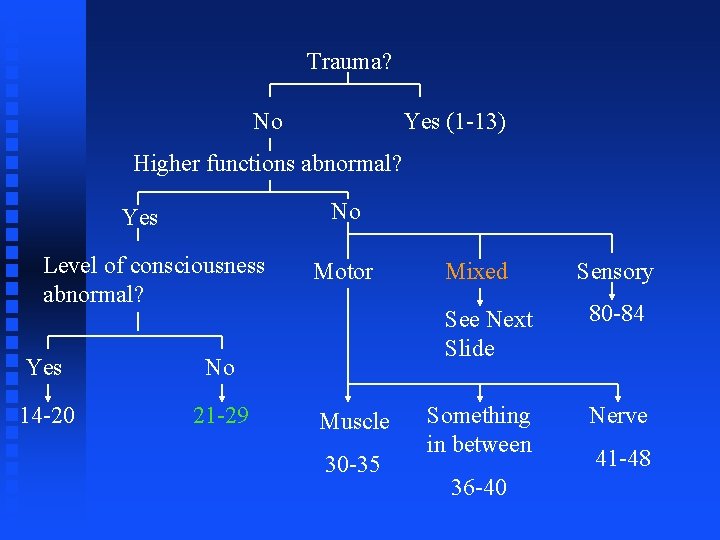
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section 21 -29
Case #1 n Patient has cognitive impairment, hallucinations, bradykinesia and muscular rigidity.
Lewy Body Dementia n Diagnosis is considered probable if 2 of 3 features are present: u u u n Supportive evidence consists of: u u u n Fluctuations in cognition, Visual hallucinations, and Parkinsonism Repeated falls, Syncope, and Sensitivity to antipsychotics Overlap of symptoms in Lewy body dementia and Parkinson's disease may complicate diagnosis. u When early cognitive impairment and behavioral disturbances predominate, Lewy body dementia is usually diagnosed.
n n CT and MRI show no characteristic changes but are helpful initially in ruling out other causes of dementia. Definitive diagnosis requires autopsy samples of brain tissue.
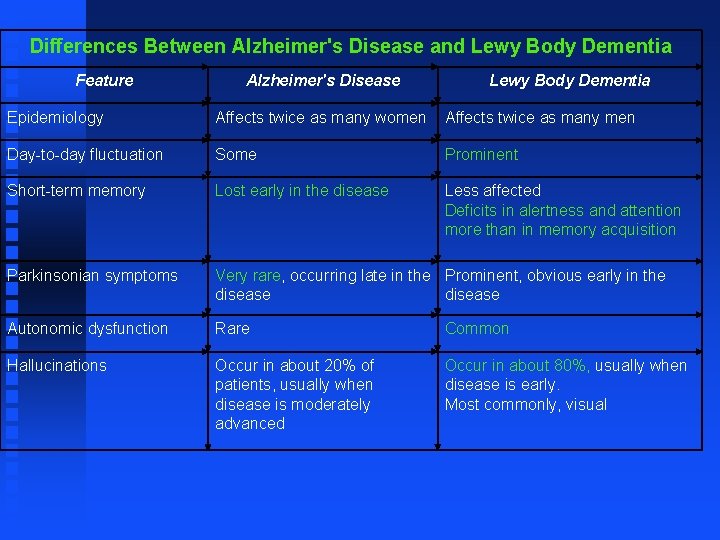
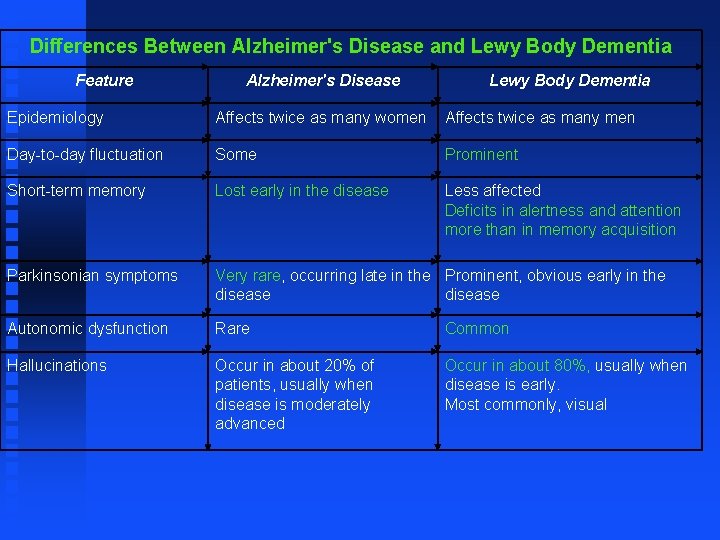
Differences Between Alzheimer's Disease and Lewy Body Dementia Feature Alzheimer's Disease Lewy Body Dementia Epidemiology Affects twice as many women Affects twice as many men Day-to-day fluctuation Some Prominent Short-term memory Lost early in the disease Less affected Deficits in alertness and attention more than in memory acquisition Parkinsonian symptoms Very rare, occurring late in the Prominent, obvious early in the disease Autonomic dysfunction Rare Common Hallucinations Occur in about 20% of patients, usually when disease is moderately advanced Occur in about 80%, usually when disease is early. Most commonly, visual
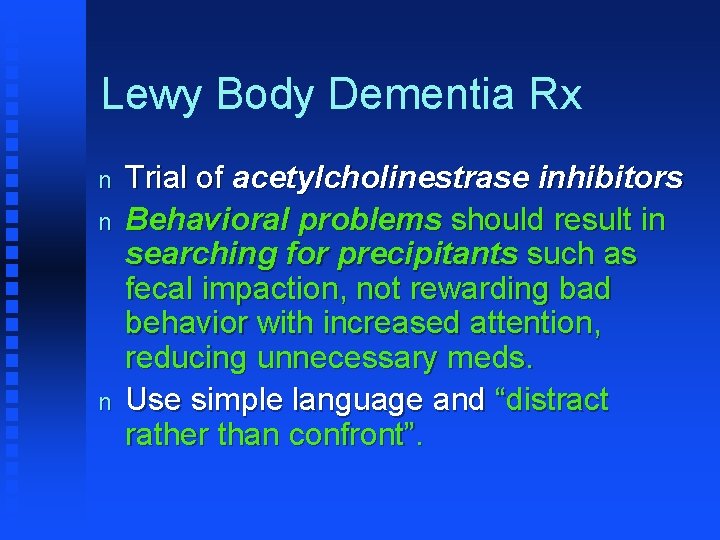
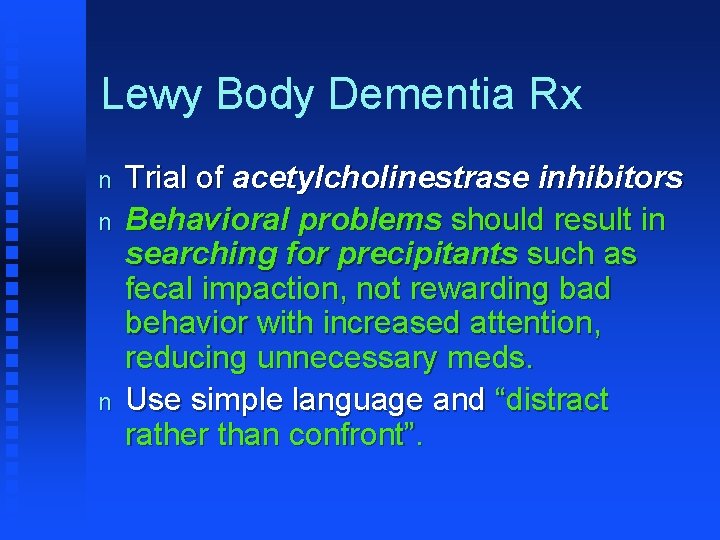
Lewy Body Dementia Rx n n n Trial of acetylcholinestrase inhibitors Behavioral problems should result in searching for precipitants such as fecal impaction, not rewarding bad behavior with increased attention, reducing unnecessary meds. Use simple language and “distract rather than confront”.

What are the other diseases in this grouping that are associated with deficits in higher functions but little muscular weakness?
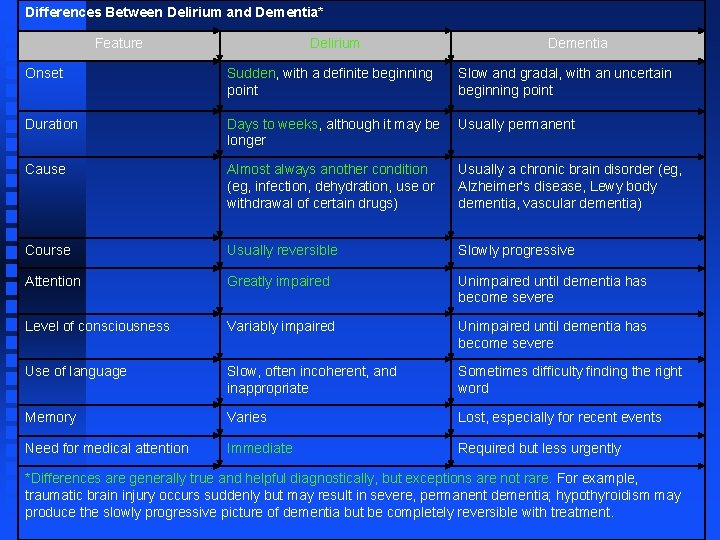
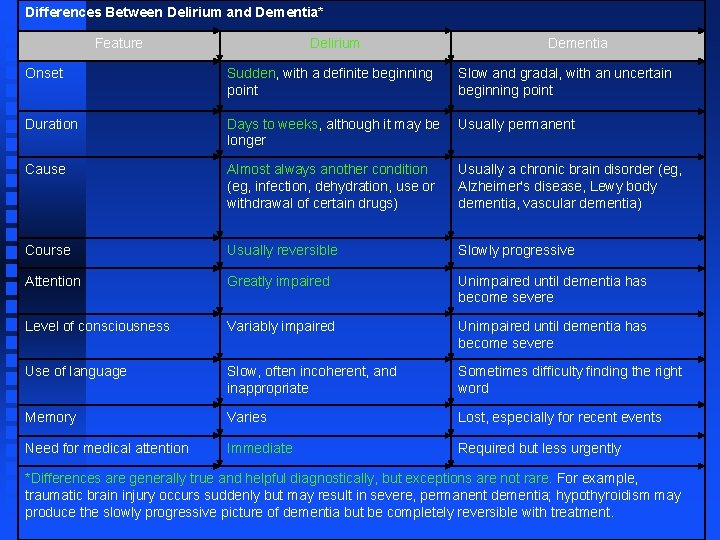
Differences Between Delirium and Dementia* Feature Delirium Dementia Onset Sudden, with a definite beginning point Slow and gradal, with an uncertain beginning point Duration Days to weeks, although it may be longer Usually permanent Cause Almost always another condition (eg, infection, dehydration, use or withdrawal of certain drugs) Usually a chronic brain disorder (eg, Alzheimer's disease, Lewy body dementia, vascular dementia) Course Usually reversible Slowly progressive Attention Greatly impaired Unimpaired until dementia has become severe Level of consciousness Variably impaired Unimpaired until dementia has become severe Use of language Slow, often incoherent, and inappropriate Sometimes difficulty finding the right word Memory Varies Lost, especially for recent events Need for medical attention Immediate Required but less urgently *Differences are generally true and helpful diagnostically, but exceptions are not rare. For example, traumatic brain injury occurs suddenly but may result in severe, permanent dementia; hypothyroidism may produce the slowly progressive picture of dementia but be completely reversible with treatment.
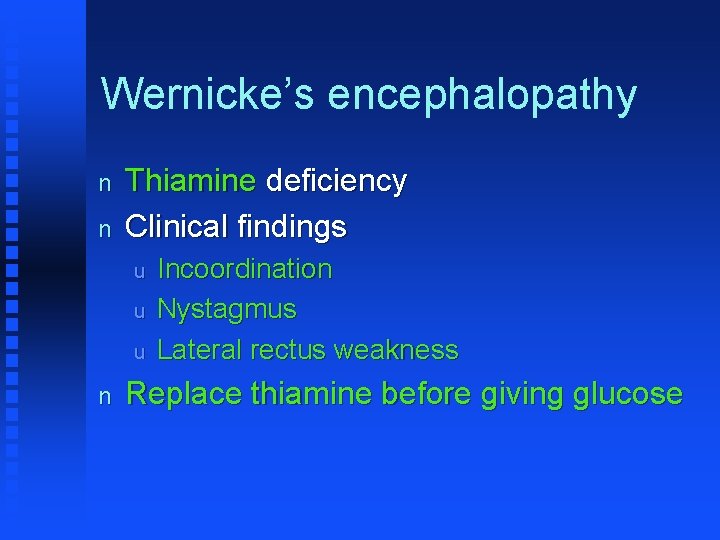
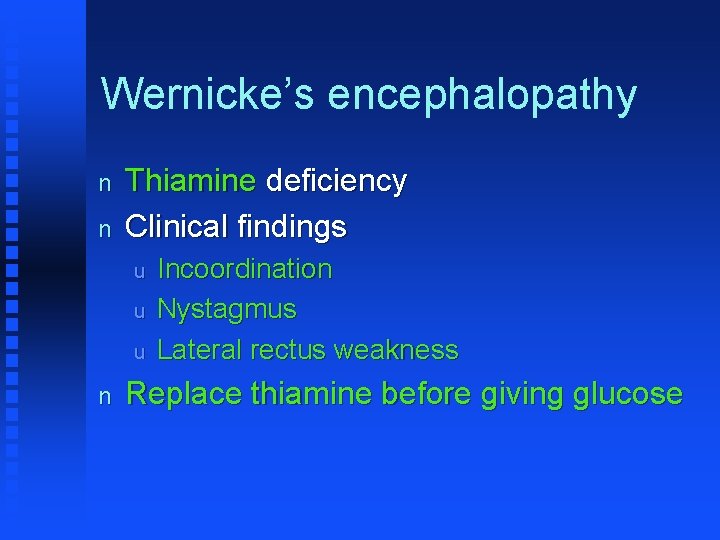
Wernicke’s encephalopathy n n Thiamine deficiency Clinical findings u u u n Incoordination Nystagmus Lateral rectus weakness Replace thiamine before giving glucose
Pick’s Disease n n Associated with shrinking of the frontal and temporal anterior lobes of the brain on a genetic(? ) basis. Depletion of seratonergic and glutamatergic neurons is present in many patients. u n n In contrast to AD, the cholinergic system is relatively spared in Pick’s. Symptoms of language disturbance, including difficulty making or understanding speech. Spatial skills and memory remain intact.
Persistent vegetative state n n Considered a partial recovery phase of coma. The vegetative state can be diagnosed according to the following criteria: u u u u n (1) no evidence of awareness of self or environment and an inability to interact with others; (2) no evidence of sustained, reproducible, purposeful, or voluntary behavioral responses to visual, auditory, tactile, or noxious stimuli; (3) no evidence of language comprehension or expression; (4) intermittent wakefulness manifested by the presence of sleepwake cycles; (5) sufficiently preserved hypothalamic and brain-stem autonomic functions to permit survival with medical and nursing care; (6) bowel and bladder incontinence; and (7) variably preserved cranial-nerve reflexes (pupillary, oculocephalic, corneal, vestibulo-ocular, and gag) and spinal reflexes. Patients in a vegetative state are usually not immobile. They may move the trunk or limbs in meaningless ways.

Binswanger’s dementia n n One of top three causes of dementia. Caused by widespread, microscopic areas of damage to the deep layers of white matter in the brain secondary to atherosclerosis of arteries that feed the subcortical areas of the brain. The most characteristic feature of BD is psychomotor slowness - an increase in the length of time it takes, for example, for the fingers to turn the thought of a letter into the shape of a letter on a piece of paper. A characteristic pattern of BD-damaged brain tissue can be seen with modern brain imaging techniques such as CT scans or magnetic resonance imaging (MRI).
Alzheimer's disease n n n Most common cause of dementia. Alzheimer's disease (AD) is a progressive, neurodegenerative disease characterized in the brain by abnormal clumps (amyloid plaques) and tangled bundles of fibers (neurofibrillary tangles) composed of misplaced proteins. Three genes have been discovered that cause early onset (familial) AD. Other genetic mutations that cause excessive accumulation of amyloid protein are associated with age-related (sporadic) AD.
n n Clinical findings: u Early loss of memory u Visuospatial abilities (ability to copy geometric designs on paper) also lost early u Mid stage F Inappropriate sexual behavior u Agitation Rx like Lewy Dementia
Case #2 n n n A 40 yo patient presents with UMN and LMN symptoms in the extremities Alterations in cognitive functions such as depression and problems with decision-making and memory. EMG is abnormal and suggests nerve loss, but NCV is OK.
ALS (Amyotrophic Lateral Sclerosis) n n Damage secondary to glutamate? The earliest symptoms are variable and may include: u u u Twitching, Cramping, or Stiffness of muscles; Muscle weakness affecting an arm or a leg; Slurred and nasal speech; or Difficulty chewing or swallowing.
ALS n n n Regardless of the part of the body first affected by the disease, muscle weakness and atrophy spread to other parts of the body as the disease progresses. Symptoms of upper motor neuron involvement include tight and stiff muscles (spasticity) and exaggerated reflexes (hyperreflexia) including an overactive gag reflex. Symptoms of lower motor neuron degeneration include muscle weakness and atrophy, muscle cramps, and fleeting twitches of muscles that can be seen under the skin (fasciculations).
ALS n To be diagnosed with ALS, patients must have signs and symptoms of both upper and lower motor neuron damage that cannot be attributed to other causes.
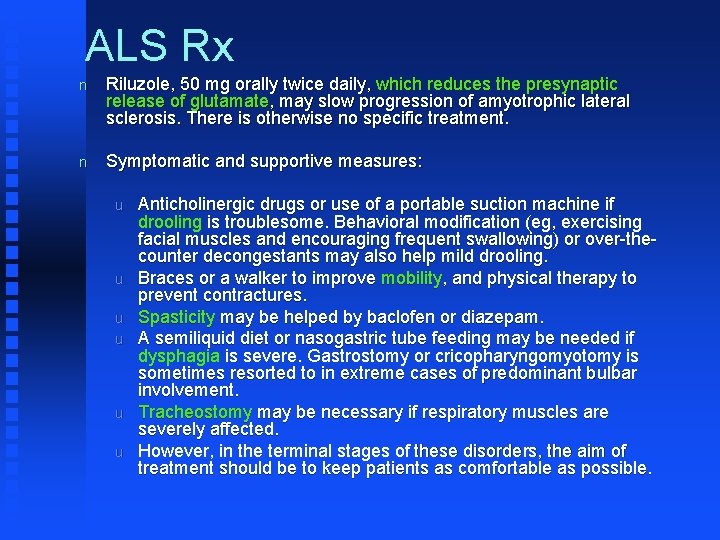
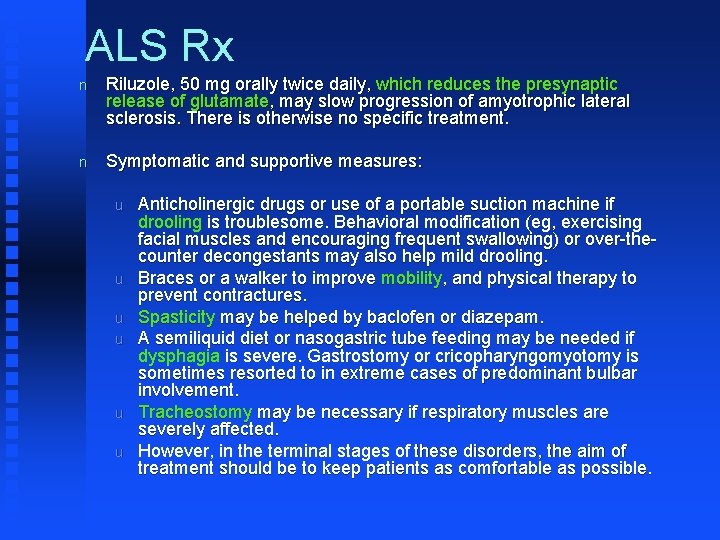
ALS Rx n Riluzole, 50 mg orally twice daily, which reduces the presynaptic release of glutamate, may slow progression of amyotrophic lateral sclerosis. There is otherwise no specific treatment. n Symptomatic and supportive measures: u u u Anticholinergic drugs or use of a portable suction machine if drooling is troublesome. Behavioral modification (eg, exercising facial muscles and encouraging frequent swallowing) or over-thecounter decongestants may also help mild drooling. Braces or a walker to improve mobility, and physical therapy to prevent contractures. Spasticity may be helped by baclofen or diazepam. A semiliquid diet or nasogastric tube feeding may be needed if dysphagia is severe. Gastrostomy or cricopharyngomyotomy is sometimes resorted to in extreme cases of predominant bulbar involvement. Tracheostomy may be necessary if respiratory muscles are severely affected. However, in the terminal stages of these disorders, the aim of treatment should be to keep patients as comfortable as possible.

Differential? i. e. What are the other diseases in this grouping that are associated with deficits in higher functions AND muscular weakness? n Myopathies u u Muscular dystrophy Mitochondrial myopathy
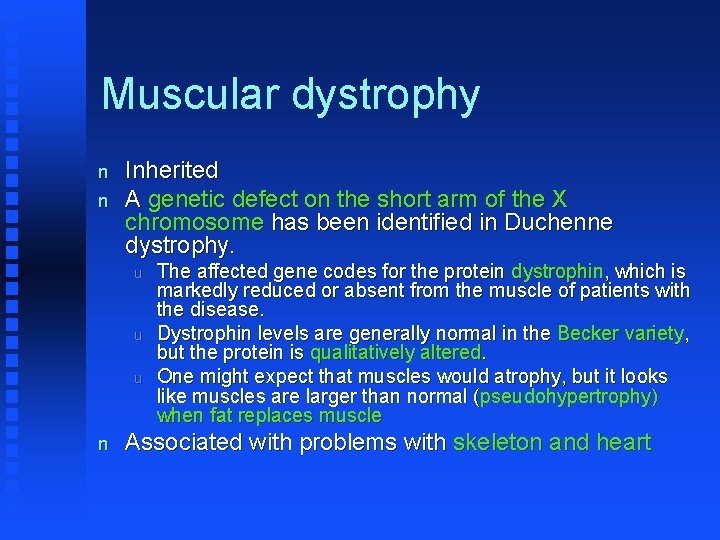
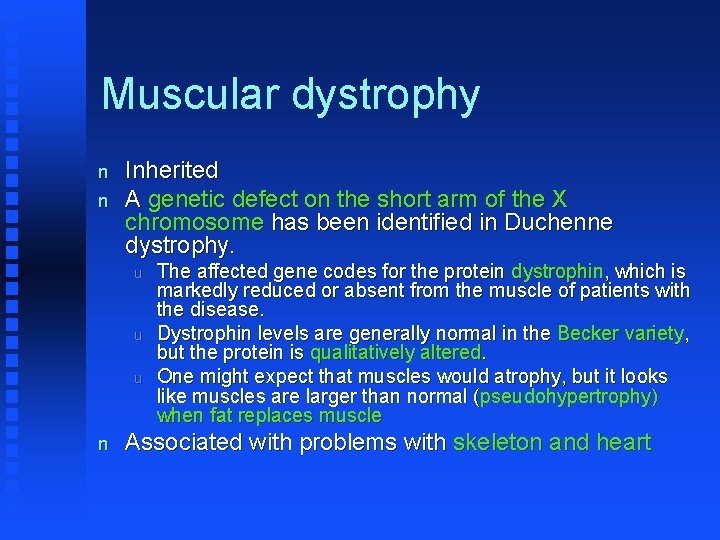
Muscular dystrophy n n Inherited A genetic defect on the short arm of the X chromosome has been identified in Duchenne dystrophy. u u u n The affected gene codes for the protein dystrophin, which is markedly reduced or absent from the muscle of patients with the disease. Dystrophin levels are generally normal in the Becker variety, but the protein is qualitatively altered. One might expect that muscles would atrophy, but it looks like muscles are larger than normal (pseudohypertrophy) when fat replaces muscle Associated with problems with skeleton and heart
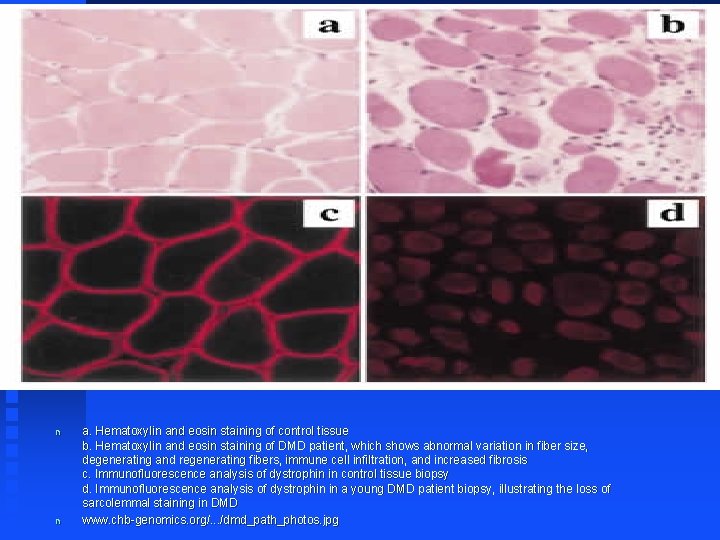
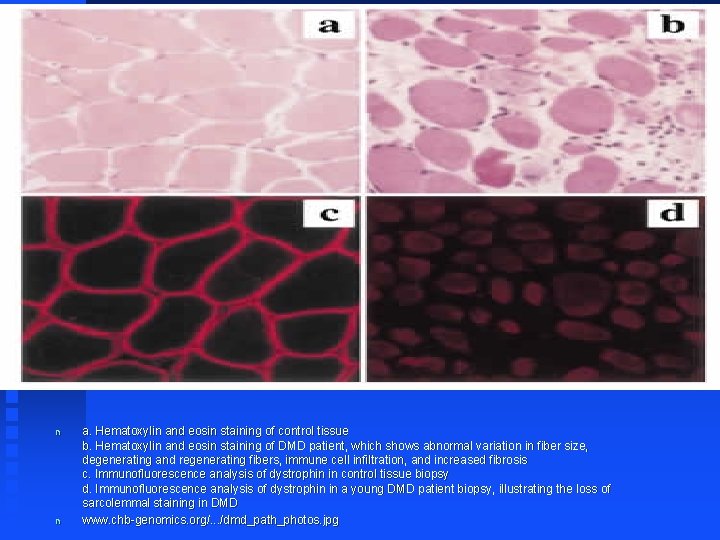
n n a. Hematoxylin and eosin staining of control tissue b. Hematoxylin and eosin staining of DMD patient, which shows abnormal variation in fiber size, degenerating and regenerating fibers, immune cell infiltration, and increased fibrosis c. Immunofluorescence analysis of dystrophin in control tissue biopsy d. Immunofluorescence analysis of dystrophin in a young DMD patient biopsy, illustrating the loss of sarcolemmal staining in DMD www. chb-genomics. org/. . . /dmd_path_photos. jpg

Mitochondrial myopathy n Pathologic examination of skeletal muscle with the modified Gomori stain show characteristic "ragged red fibers" containing accumulations of abnormal mitochondria.
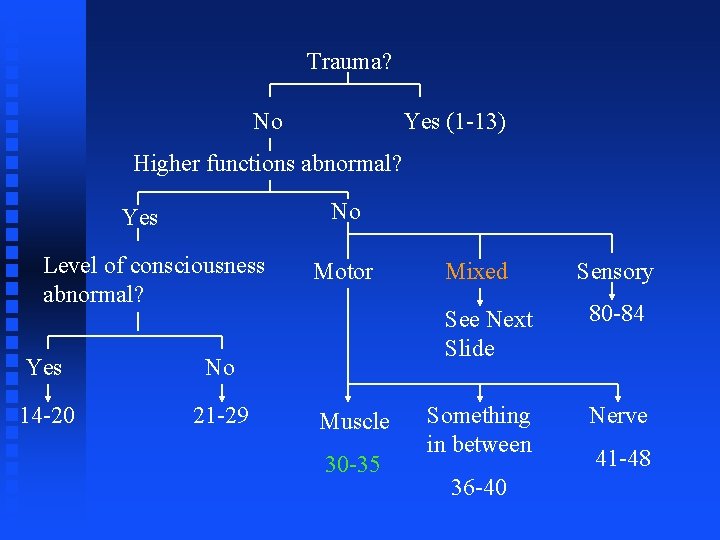
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section #30 -35
Case #1 n n 40 yo develops gradual onset of proximal muscle weakness and dysphagia. CK is elevated. Fever, AV block present
Polymyositis (PM) n n An autoimmune etiology of the inflammatory myopathies is indirectly supported. PM occurs in association with a systemic autoimmune or connective tissue disease, with a known viral or bacterial infection or with exposure to certain drugs, especially D-penicillamine or zidovudine (AZT). Biopsy provides definitive diagnosis Rx u u u Glucocorticoids Immunosuppressives Immunomodulators
PM continued n n n The 5 -year survival rate for treated patients with PM and DM is ~95% and the 10 -year survival 84%. Death is usually due to pulmonary, cardiac, or other systemic complications. Most patients improve with therapy, and many make a full functional recovery, which is often sustained with maintenance therapy. Up to 30% may be left with some residual muscle weakness. Relapses may occur at any time.
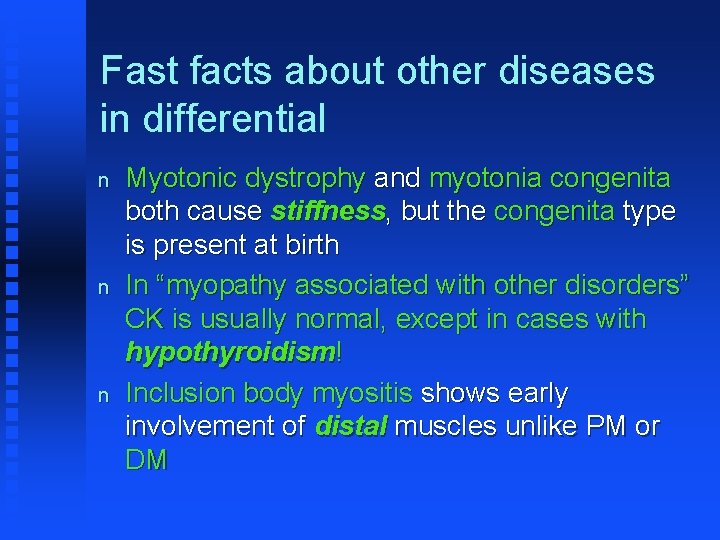
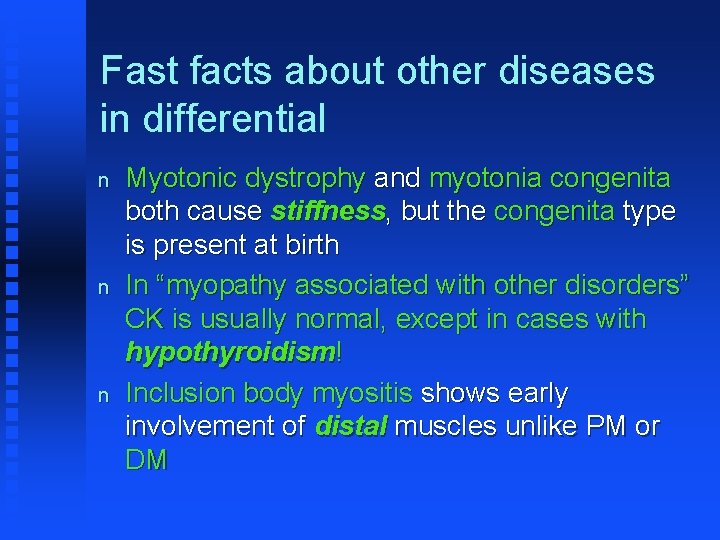
Fast facts about other diseases in differential n n n Myotonic dystrophy and myotonia congenita both cause stiffness, but the congenita type is present at birth In “myopathy associated with other disorders” CK is usually normal, except in cases with hypothyroidism! Inclusion body myositis shows early involvement of distal muscles unlike PM or DM
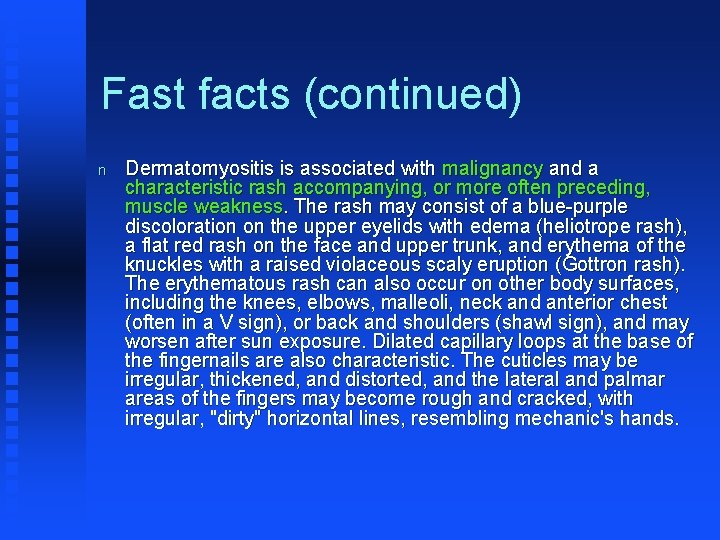
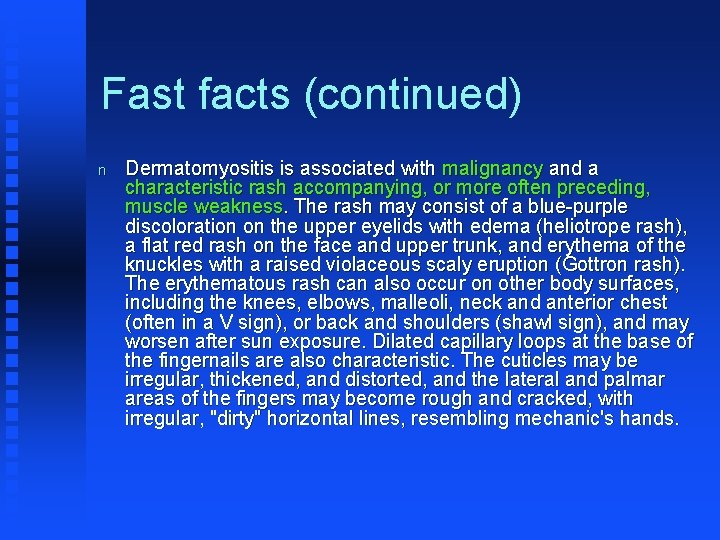
Fast facts (continued) n Dermatomyositis is associated with malignancy and a characteristic rash accompanying, or more often preceding, muscle weakness. The rash may consist of a blue-purple discoloration on the upper eyelids with edema (heliotrope rash), a flat red rash on the face and upper trunk, and erythema of the knuckles with a raised violaceous scaly eruption (Gottron rash). The erythematous rash can also occur on other body surfaces, including the knees, elbows, malleoli, neck and anterior chest (often in a V sign), or back and shoulders (shawl sign), and may worsen after sun exposure. Dilated capillary loops at the base of the fingernails are also characteristic. The cuticles may be irregular, thickened, and distorted, and the lateral and palmar areas of the fingers may become rough and cracked, with irregular, "dirty" horizontal lines, resembling mechanic's hands.
Dermatomyositis

Mechanics’ Hands

Giant mechanics’ hands n http: //www. cinemastrikesback. com/news/films/scienceofsleep/1280 -1. jpg
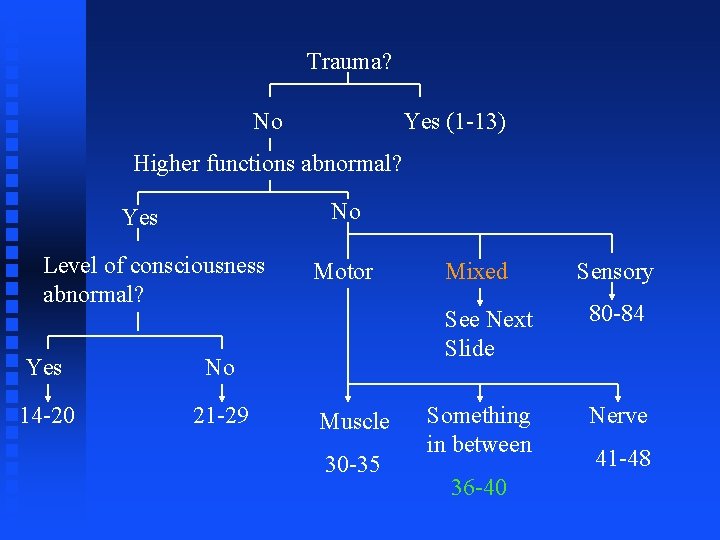
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section #36 -40
Case #1 n n A 45 yo female presents with diplopia, dilated and non-reactive pupils, ptosis, facial weakness, dysphagia, and nasal speech, followed by respiratory difficulty and finally by weakness that appears last in the limbs. She also has dry mouth, constipation, ileus, postural hypotension. She is an avid gardener and cans her own vegetables.
Botulism n n n Blood work identified the botulinum toxin Patients should be hospitalized in case respiratory assistance becomes necessary. Treatment is with trivalent antitoxin, once it is established that the patient is not allergic to horse serum.
Fast facts about other disorders in the differential
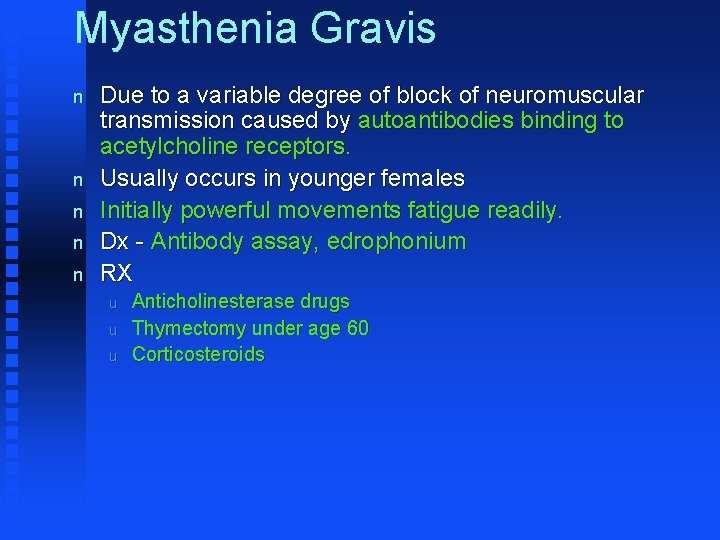
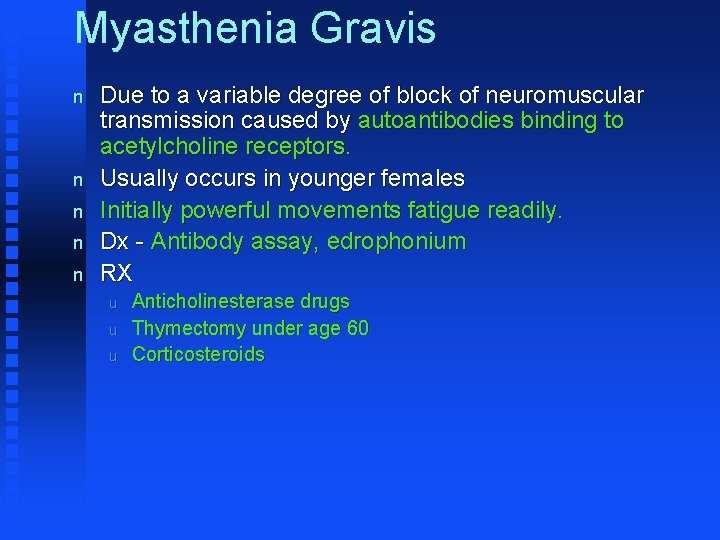
Myasthenia Gravis n n n Due to a variable degree of block of neuromuscular transmission caused by autoantibodies binding to acetylcholine receptors. Usually occurs in younger females Initially powerful movements fatigue readily. Dx - Antibody assay, edrophonium RX u u u Anticholinesterase drugs Thymectomy under age 60 Corticosteroids
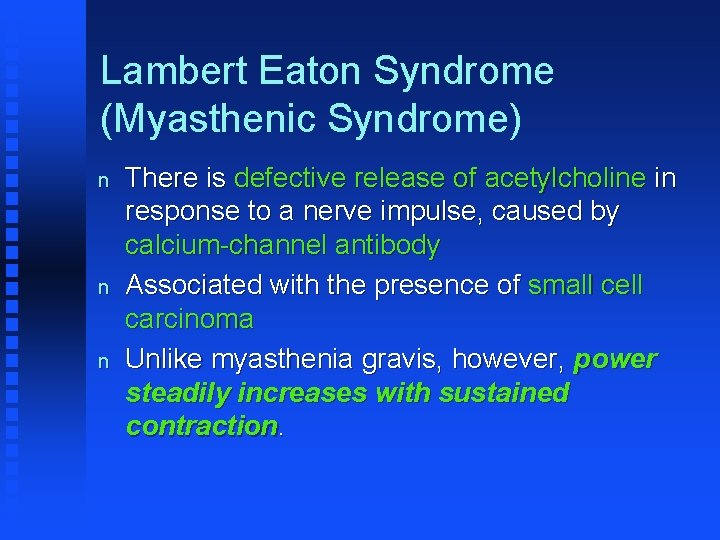
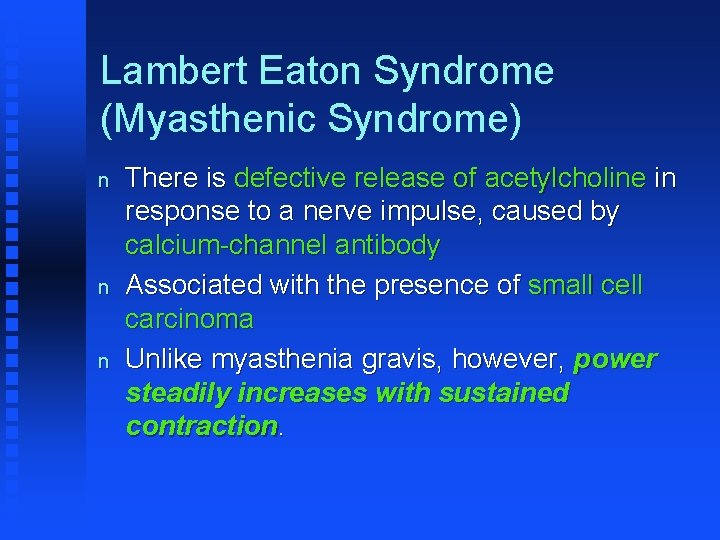
Lambert Eaton Syndrome (Myasthenic Syndrome) n n n There is defective release of acetylcholine in response to a nerve impulse, caused by calcium-channel antibody Associated with the presence of small cell carcinoma Unlike myasthenia gravis, however, power steadily increases with sustained contraction.
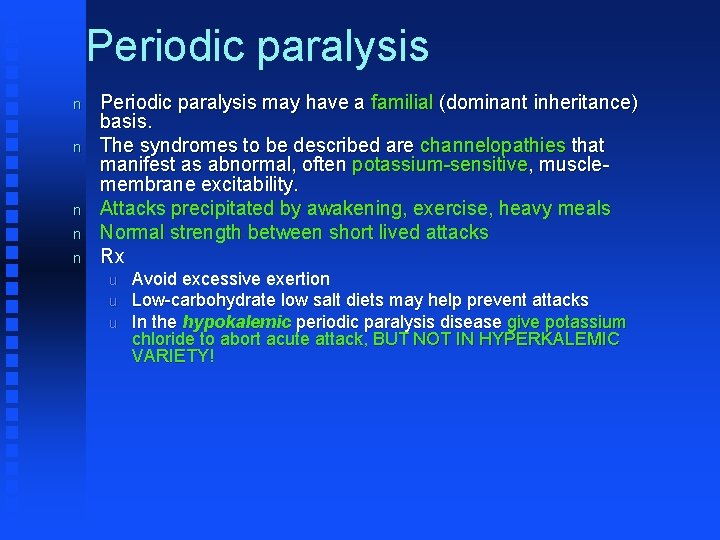
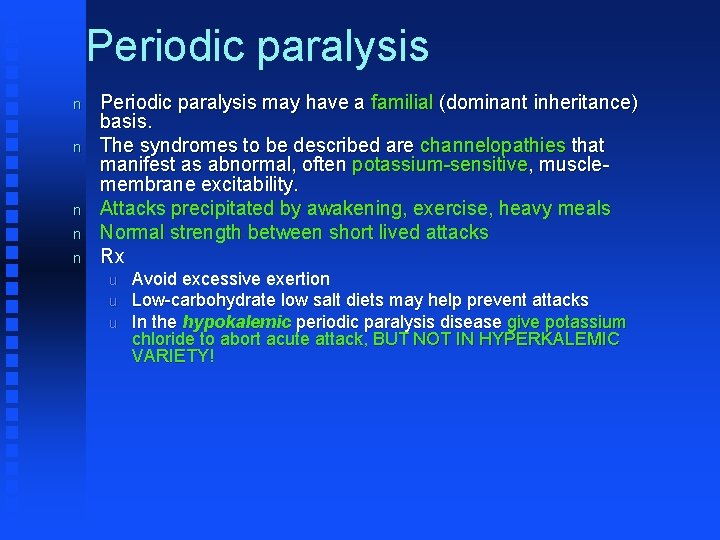
Periodic paralysis n n n Periodic paralysis may have a familial (dominant inheritance) basis. The syndromes to be described are channelopathies that manifest as abnormal, often potassium-sensitive, musclemembrane excitability. Attacks precipitated by awakening, exercise, heavy meals Normal strength between short lived attacks Rx u u u Avoid excessive exertion Low-carbohydrate low salt diets may help prevent attacks In the hypokalemic periodic paralysis disease give potassium chloride to abort acute attack, BUT NOT IN HYPERKALEMIC VARIETY!
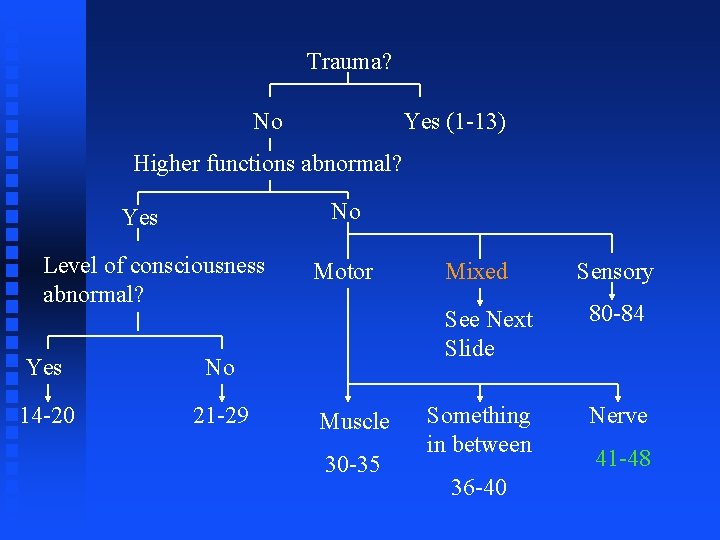
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section #41 -48 n A type 1 diabetic presents with postural hypotension, decreased cardiovascular response to Valsalva's maneuver, gastroparesis, alternating bouts of diarrhea (particularly nocturnal) and constipation, inability to empty the bladder, and impotence.

Diabetic neuropathy pathology n Metabolic theory u Hyperglycemia > Increased levels of intracellular glucose in nerves > Saturation of the normal glycolytic pathway and shunting of extra glucose into the polyol pathway > Accumulation of sorbitol and fructose lead to a whole host of neuro toxic reactions.
n Vascular (ischemic-hypoxic) theory u Endoneurial ischemia develops because of increased endoneurial vascular resistance to hyperglycemic blood.
n Altered neurotrophic support theory u u Nerve growth factor (NGF) promotes survival of sympathetic and small-fiber neural crest–derived elements in the peripheral nervous system. In animals with diabetes, both production and transport of NGF are impaired.
n Autoimmune theory u Autoimmune diabetic neuropathy is postulated to result from immunogenic alteration of endothelial capillary cells.
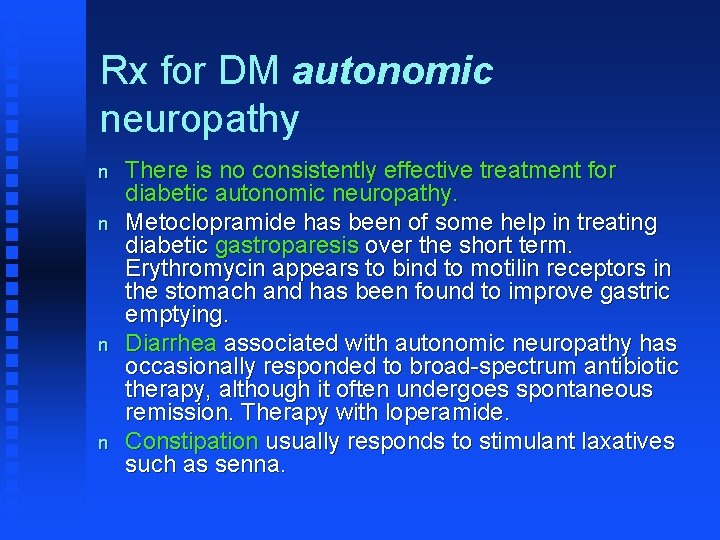
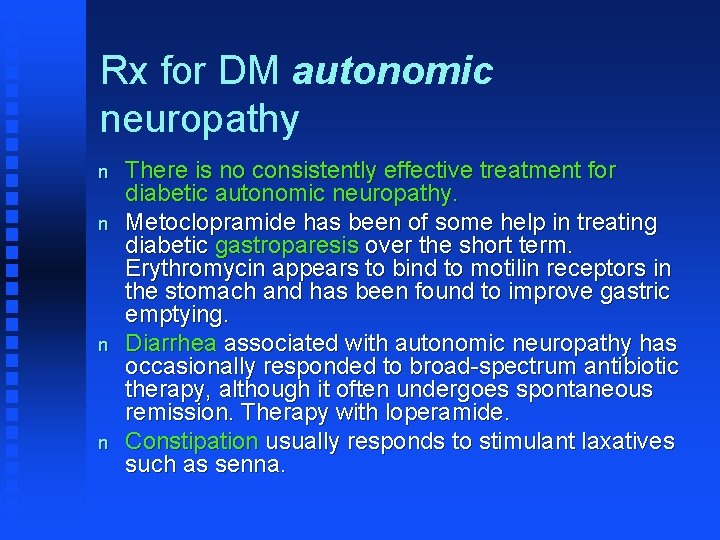
Rx for DM autonomic neuropathy n n There is no consistently effective treatment for diabetic autonomic neuropathy. Metoclopramide has been of some help in treating diabetic gastroparesis over the short term. Erythromycin appears to bind to motilin receptors in the stomach and has been found to improve gastric emptying. Diarrhea associated with autonomic neuropathy has occasionally responded to broad-spectrum antibiotic therapy, although it often undergoes spontaneous remission. Therapy with loperamide. Constipation usually responds to stimulant laxatives such as senna.

n n n Bethanechol in doses of 10 -50 mg three times a day has occasionally improved emptying of the atonic urinary bladder. Mineralocorticoid therapy with fludrocortisone, 0. 2 -0. 3 mg/d, and elastic stockings or pressure suits have reportedly been of some help in patients with orthostatic hypotension occurring as a result of loss of postural reflexes. There are medical, mechanical, and surgical treatments available for treatment of erectile dysfunction.

Motor neuropathy can be aided with appropriate splinting. Let’s try a demo!
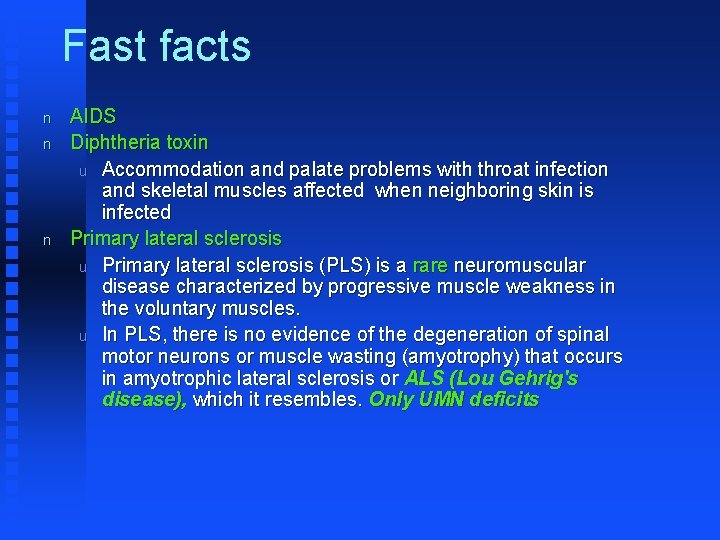
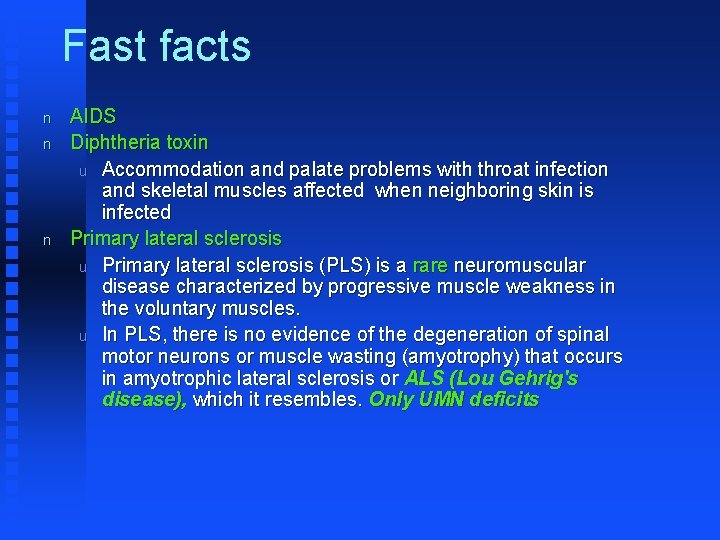
Fast facts n n n AIDS Diphtheria toxin u Accommodation and palate problems with throat infection and skeletal muscles affected when neighboring skin is infected Primary lateral sclerosis u Primary lateral sclerosis (PLS) is a rare neuromuscular disease characterized by progressive muscle weakness in the voluntary muscles. u In PLS, there is no evidence of the degeneration of spinal motor neurons or muscle wasting (amyotrophy) that occurs in amyotrophic lateral sclerosis or ALS (Lou Gehrig's disease), which it resembles. Only UMN deficits
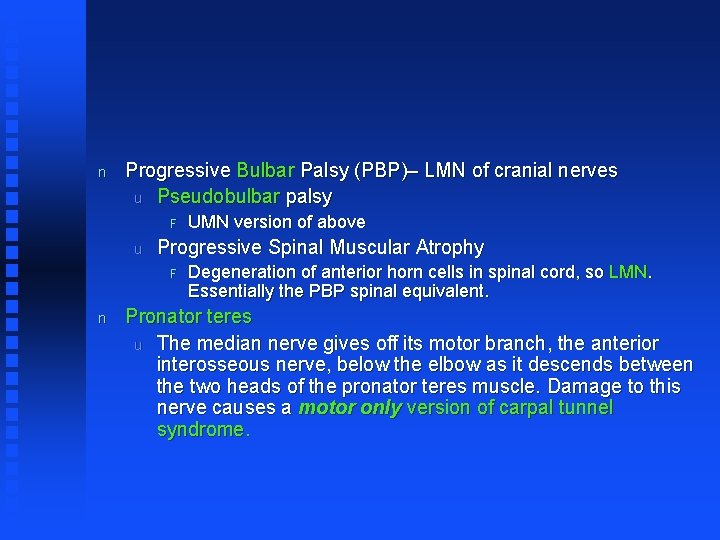
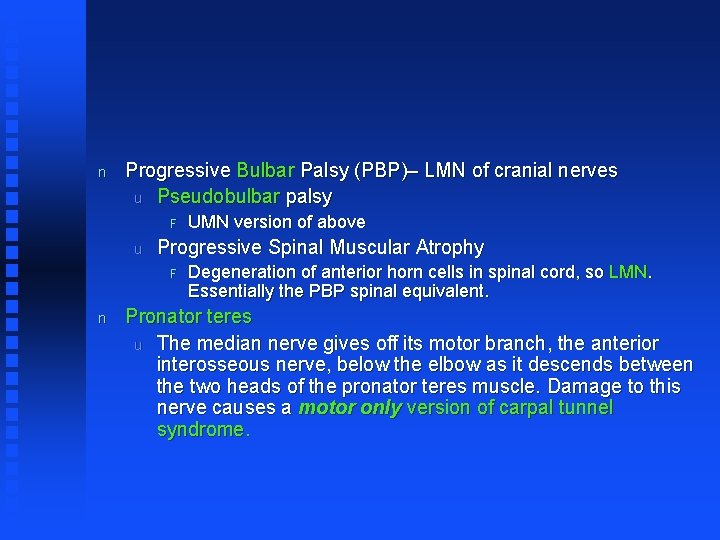
n Progressive Bulbar Palsy (PBP)– LMN of cranial nerves u Pseudobulbar palsy F u Progressive Spinal Muscular Atrophy F n UMN version of above Degeneration of anterior horn cells in spinal cord, so LMN. Essentially the PBP spinal equivalent. Pronator teres u The median nerve gives off its motor branch, the anterior interosseous nerve, below the elbow as it descends between the two heads of the pronator teres muscle. Damage to this nerve causes a motor only version of carpal tunnel syndrome.
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Section #79. 5 -84
Case #1 n n The distribution of symptoms is stronger distally and less proximally and is termed a glove-stocking distribution. The symptoms include the following: F F F Burning sensations Skin tingling Allodynia - Painful sensation on contact with something that typically would not hurt (eg, bed sheets) Hyperalgesia - Abnormally exaggerated response to painful stimuli Sensation of pins and needles

n This suggests painful diabetic neuropathy!

Fast facts n Atypical Facial Pain and Trigeminal Neuralgia (TN) both cause pain in head. u u TN more fleeting and in distribution of TGN unilaterally. ? Compression of nerve by blood vessel
n Meralgia paresthetica u u u Pain and numbness outer aspect of thigh The lateral femoral cutaneous nerve, a sensory nerve arising from the L 2 and L 3 roots, may be compressed or stretched in obese or diabetic patients and during pregnancy. The nerve usually runs under the outer portion of the inguinal ligament to reach the thigh, but the ligament sometimes splits to enclose it. Hyperextension of the hip or increased lumbar lordosis, such as occurs during pregnancy, leads to nerve compression by the posterior fascicle of the ligament.
n Postherpetic neuralgia u u May persist for months or even years Rx F F F 1) The incidence of postherpetic neuralgia may be reduced by the treatment of shingles with oral acyclovir or famciclovir 2) Zoster vaccine markedly reduces morbidity 3) If simple analgesics fail to help, a trial of a tricyclic antidepressant
Trauma? No Yes (1 -13) Higher functions abnormal? No Yes Level of consciousness abnormal? Yes No 14 -20 21 -29 Motor Muscle 30 -35 Mixed Sensory See Next Slide 80 -84 Something in between Nerve 36 -40 41 -48
Mixed Single nerve or dermatome involved? Yes 49 -56 No Significant non-neuro symptoms? Yes No 57 -71 73 -79. 5

Section #49 -56
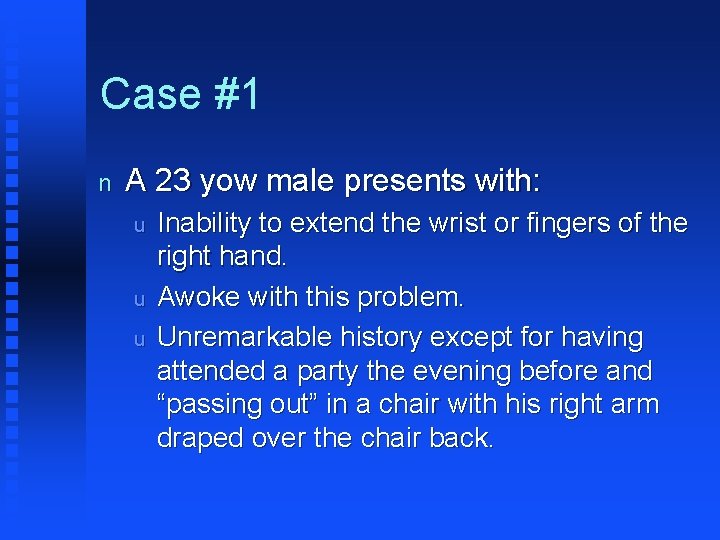
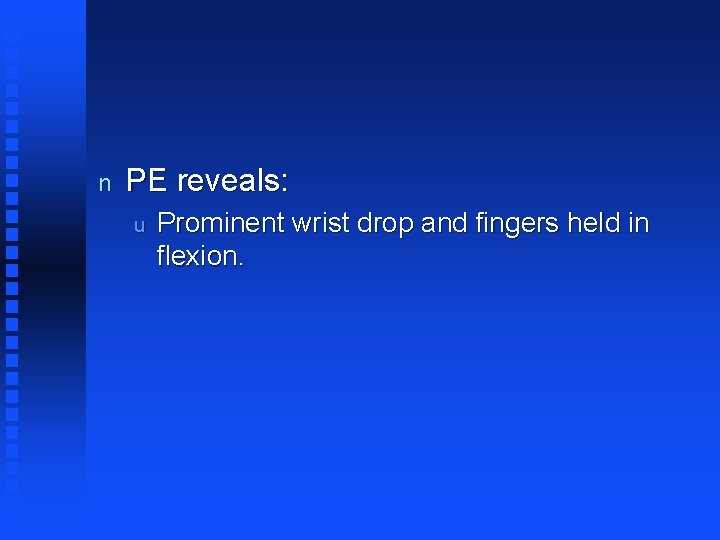
Case #1 n A 23 yow male presents with: u u u Inability to extend the wrist or fingers of the right hand. Awoke with this problem. Unremarkable history except for having attended a party the evening before and “passing out” in a chair with his right arm draped over the chair back.
n PE reveals: u Prominent wrist drop and fingers held in flexion.

Radial Nerve Palsy n n The history strongly suggests a Saturday Night Palsy (Radial Nerve Compression). Prognosis is good and recovery can be expected within 6 -8 weeks.
Fast facts n Bell’s palsy u u u Idiopathic facial paresis of lower motor neuron type that has been attributed to an inflammatory reaction involving the facial nerve. No treatment may be necessary, but the only medical treatment that may influence the outcome is administration of corticosteroids, but this is unclear. It is helpful to protect the eye with lubricating drops (or lubricating ointment at night) and a patch if eye closure is not possible. Only about 10% of all patients have permanent disfigurement or other long-term sequelae. Patients with clinically complete palsy when first seen are less likely to make a full recovery than those with an incomplete one. A poor prognosis for recovery is also associated with advanced age, hyperacusis, and severe initial pain.

n Carpal Tunnel u u Modify patient's hand activities and have the affected wrist splinted for 2 -6 weeks. NSAIDs can also be added. Patients should be referred to a specialist when they do not improve or when thenar muscle atrophy or weakness develops. Muscle strength returns gradually, but complete recovery cannot be expected when atrophy is pronounced.
n Femoral u u May occur in diabetics or from compression by retroperitoneal neoplasms or hematomas (e. g. , expanding aortic aneurysm). Symptoms occur in quads and anteromedian thigh
n Sciatic u u u Misplaced deep intramuscular injections are probably still the most common cause of sciatic nerve palsy. Trauma to the buttock, hip, or thigh may also be responsible. Clinical findings: F F Problems with dorsiflexion and eversion of foot Decreased sensation anterolateral aspect of calf and dorsum of foot
n Tarsal Tunnel u u u The tibial nerve, a branch of the sciatic, passes through the tarsal tunnel behind and below the medial malleolus, giving off calcaneal branches and the medial and lateral plantar nerves that supply small muscles of the foot and the skin on the plantar aspect of the foot and toes. Compression of the posterior tibial nerve or its branches can occur between the bony floor and ligamentous roof of the tarsal tunnel. Clinical findings: F Pain or numbness over the bottom of the foot, especially at night, with sparing of the heel.
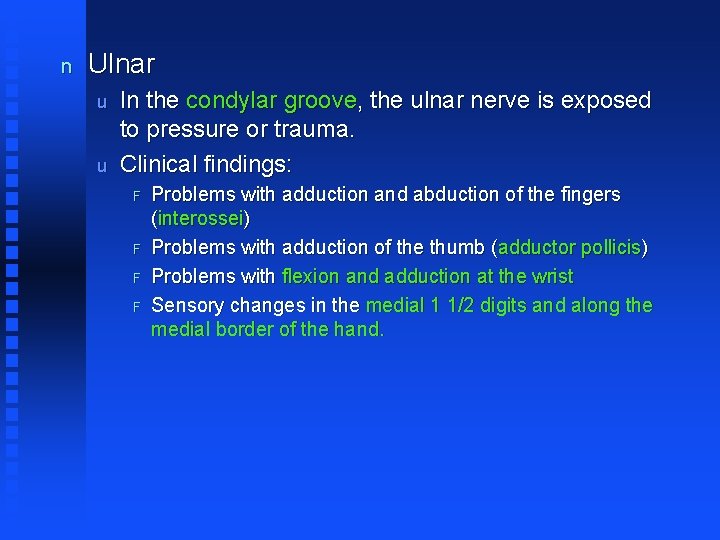
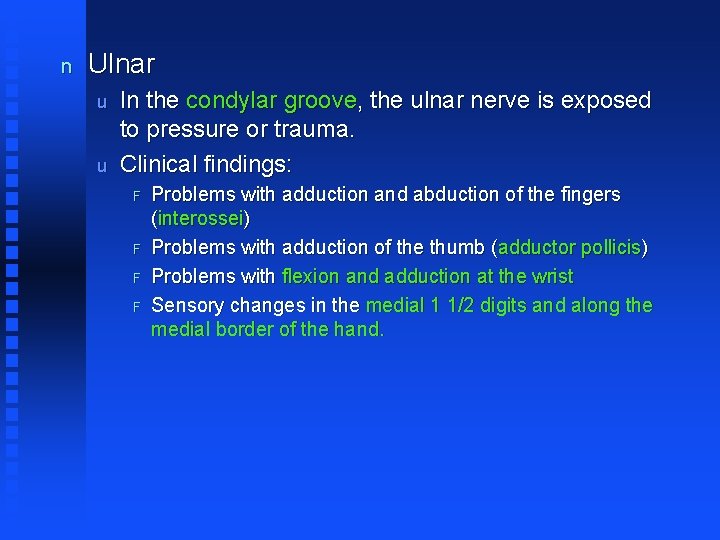
n Ulnar u u In the condylar groove, the ulnar nerve is exposed to pressure or trauma. Clinical findings: F F Problems with adduction and abduction of the fingers (interossei) Problems with adduction of the thumb (adductor pollicis) Problems with flexion and adduction at the wrist Sensory changes in the medial 1 1/2 digits and along the medial border of the hand.
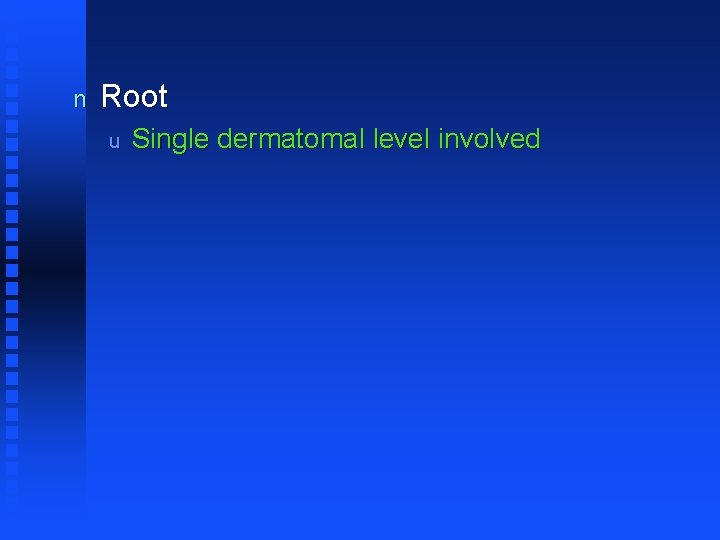
n Root u Single dermatomal level involved
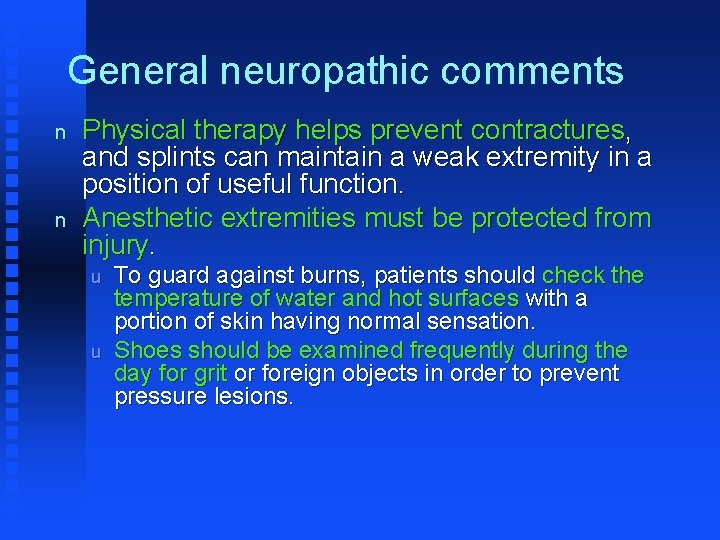
General neuropathic comments n n Physical therapy helps prevent contractures, and splints can maintain a weak extremity in a position of useful function. Anesthetic extremities must be protected from injury. u u To guard against burns, patients should check the temperature of water and hot surfaces with a portion of skin having normal sensation. Shoes should be examined frequently during the day for grit or foreign objects in order to prevent pressure lesions.
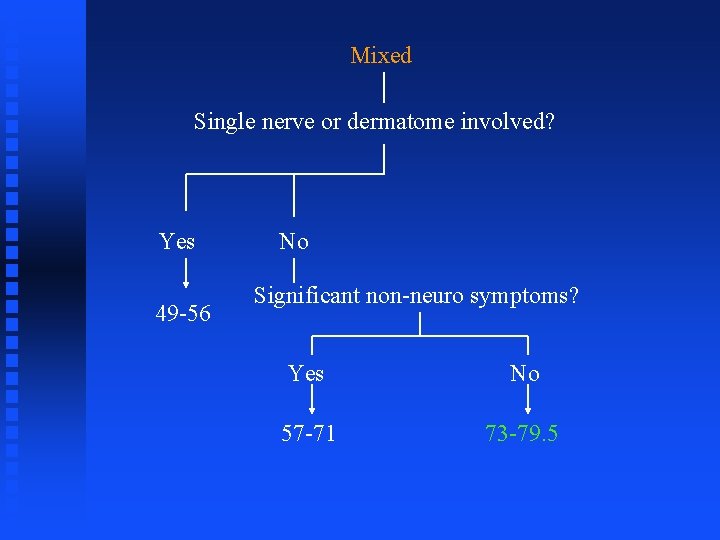
Mixed Single nerve or dermatome involved? Yes 49 -56 No Significant non-neuro symptoms? Yes No 57 -71 73 -79. 5
Section #73 -79. 5
Case #1 n A 17 yow male presents with: u u n Progressive weakness of the legs and arflexia. Spreading to the arms and face. Distal paresthesias. Abnormal sweating. PE reveals: u u Tachycardia and hypertension. Weakness as described.
n n This patient has Guillain-Barre Syndrome. Path u u u Probably immunologic Primarily demyelination Campylobacter jejuni enteritis
n Can be confused with CIDP u CIDP should be suspected when a patient presumed to have GBS deteriorates after 9 weeks
n n Most patients make a recovery over months, though 10 -20% are left with a persisting disability. Prednisone is ineffective and contraindicated.
n n Plasmaphoresis and immunoglobulin can be helpful. Intubate and admit to ICU if FVC reaches 15 ml/kg, dyspnea becomes evident or O 2 saturation declines.
Case #2 n n n Weakness, numbness, tingling, in a limb. A few month ago patient was diagnosed with retrobulbar neuritis. A few weeks before had urinary urgency with a negative UA.
Multiple Sclerosis n Path u u n Auto-immune Genetic susceptibility Focal - often perivenular - areas of demyelination with reactive gliosis found scattered in CNS and optic nerves Infection, trauma, pregnancy may precipitate exacerbations. Clinical findings: u MRI F F n Multiplicity of lesions. Two or more different areas of white matter must be affected. Rx u u u Corticosteroids hastens recovery from acute attack Beta-interferon reduces frequency of exacerbations Progression cannot be stopped, but recovery from acute relapses can be hastened.
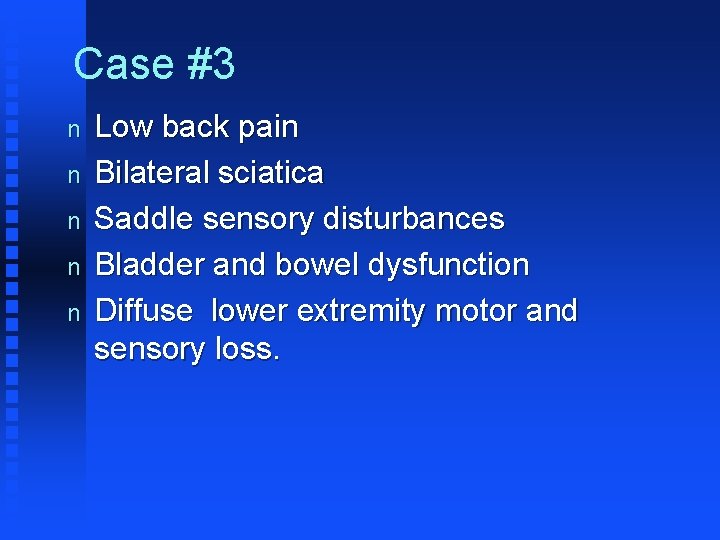
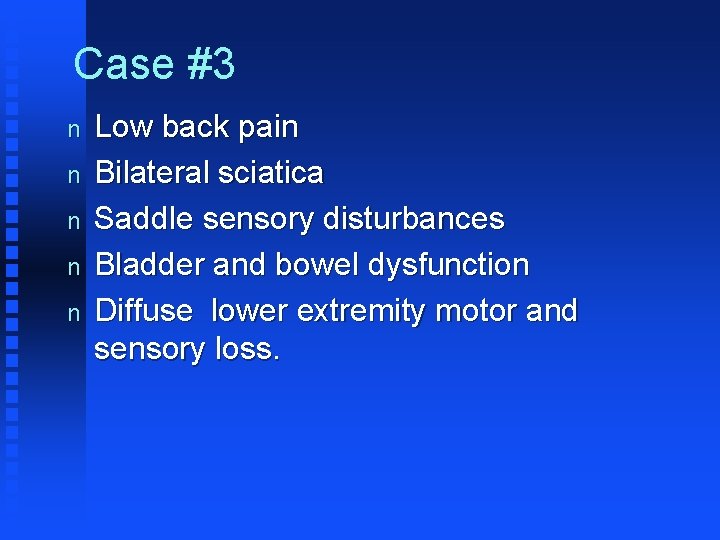
Case #3 n n n Low back pain Bilateral sciatica Saddle sensory disturbances Bladder and bowel dysfunction Diffuse lower extremity motor and sensory loss.

Cauda Equina Syndrome n No proven medical treatment exists, and therapy generally is directed at the underlying cause of CES. u Some may suggest methylprednisolone in a regimen similar to that for traumatic spinal cord injury or another regimen of steroid for the acute syndrome. F u u For penetrating trauma, steroids have not shown significant benefit. Surgery is controversial. The timing of decompression is controversial, with immediate, early, and late surgical decompression showing varying results. Consultations F Early neurosurgical, neurologic, or orthopedic consultations are recommended, depending on the suspected etiology of CES.

Fast Facts n Cervical rib u n Brachial and LS plexopathies u u u n Involves intrinsic muscles of hand on a compressive basis and can also affect pulse on the same side Can occur in association with multiple problems Brachial in the upper extremity and LS in the lower extremity Brachial can also be associated with Horner's syndrome HMSN II (Charcot-Marie-Tooth) and III (Dejerine. Sottas) u u II – Older pts, axons, lower extremities mostly III – Younger pts, myelin, palpably enlarged nerves
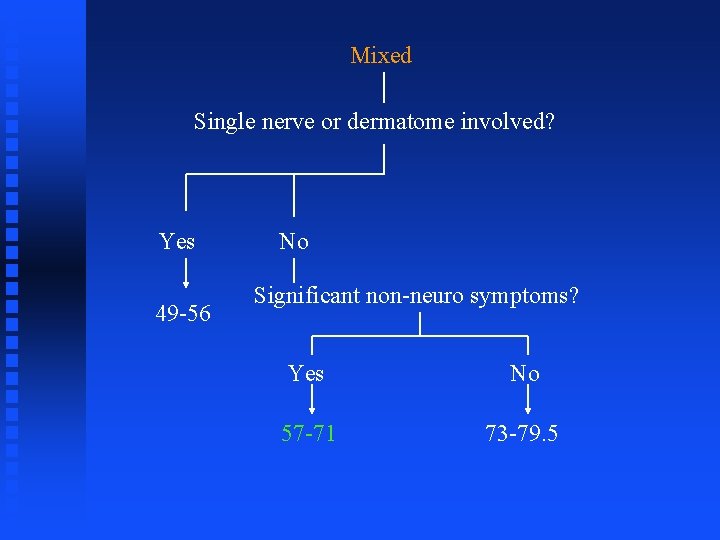
Mixed Single nerve or dermatome involved? Yes 49 -56 No Significant non-neuro symptoms? Yes No 57 -71 73 -79. 5
Section #57 -71
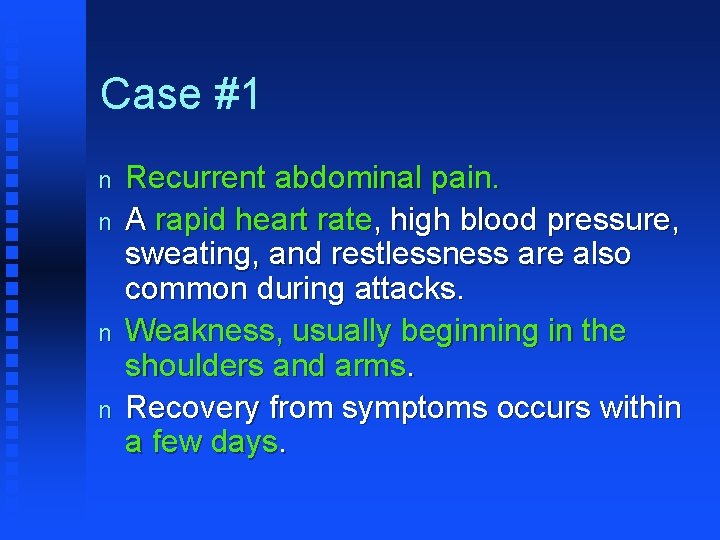
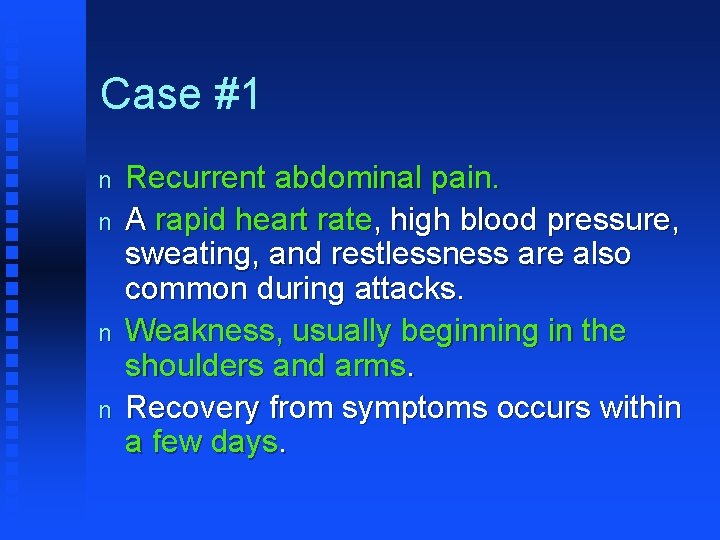
Case #1 n n Recurrent abdominal pain. A rapid heart rate, high blood pressure, sweating, and restlessness are also common during attacks. Weakness, usually beginning in the shoulders and arms. Recovery from symptoms occurs within a few days.
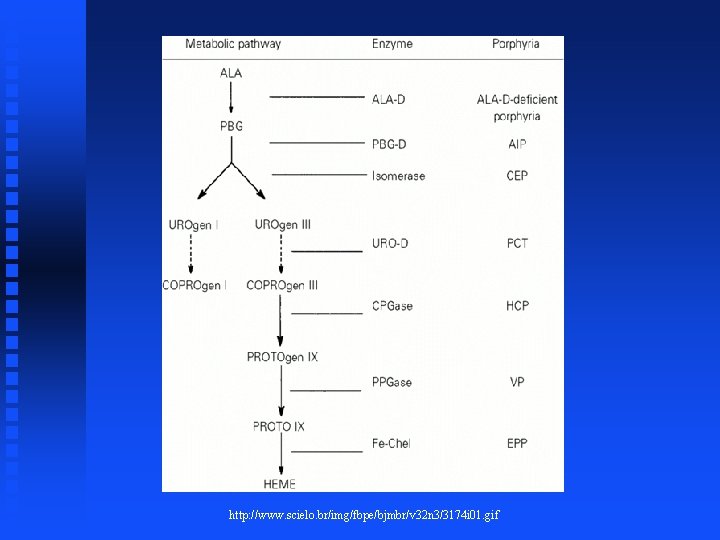
Porphyria n Dx u u Presents in adulthood is technically called “acute intermittent porphyria” Caused by deficiency of porphobilinogen deaminase with subsequent increased excretion of aminolevulinic acid and porphobilinogen in the urine.
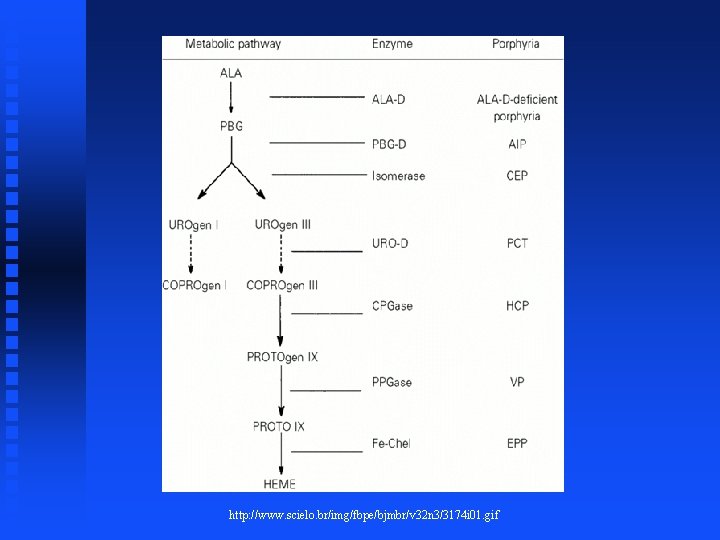
http: //www. scielo. br/img/fbpe/bjmbr/v 32 n 3/3174 i 01. gif
u u u Pain from abnormalities in autonomic innervation and causes no fever or leukocytosis Etiology of innervation pathology unclear and may result from decreased heme production or from over-stimulation of GABA receptors as ALA is structurally analogous to GABA Confirmation by increased porphobilinogen in urine during attack
n Rx u u Avoid precipitating factors like sulfonamides, barbiturates, starvation diets Suppress ALA synthetase F F F u High carbohydrate diet IV glucose Hematin administration Analgesics
Fast facts n A whole host of mixed neuropathies can be associated with “non -neuro” symptoms and/or telltale exposures: u u u Leprosy AIDS/HIV Lyme disease Sarcoid RA DM Uremia Alcohol Paraproteinemias Malignancies Industrial agents
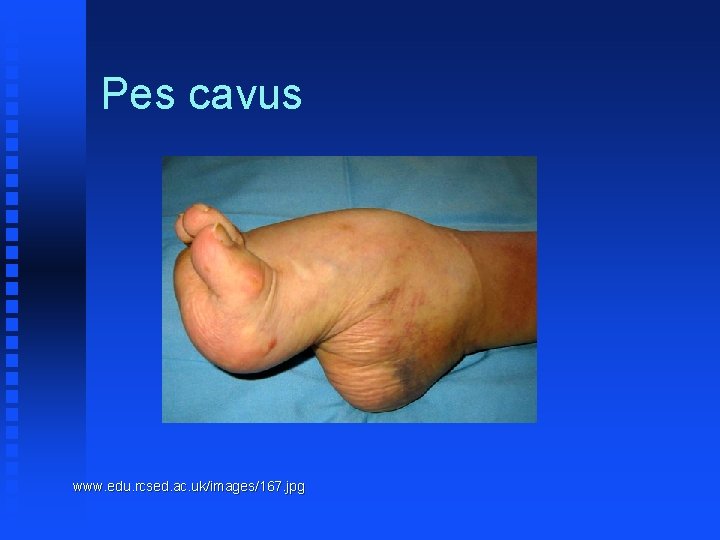
u There also genetically based neuro disease in this category F HMSN I (Also known as Charcot-Marie-Tooth) • Foot deformities (Hammertoes, high arches, tight achilles tendon) • Cold feet with hair loss and edema • Palpable nerves in 25% F Friedrich’s ataxia • Bilateral pes cavus F HMSN IV (Refsum’s disease) • • Abnormal phytanic acid metabolism Retinal degeneration Cardiomyopathy Cutaneous findings
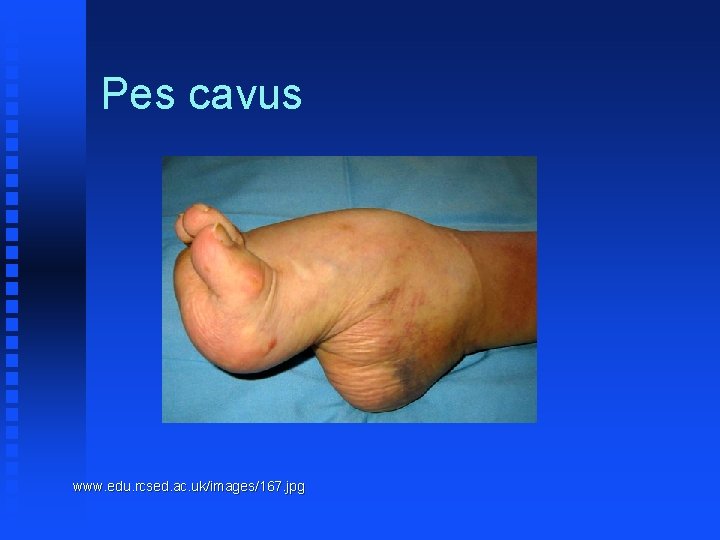
Pes cavus www. edu. rcsed. ac. uk/images/167. jpg
Pez universalis cache. halloweenmart. com/images/ip 015173. jpg
 Differentiate muscular strength from muscular endurance
Differentiate muscular strength from muscular endurance Wfns scale
Wfns scale Pupil assessment
Pupil assessment Motor function neurological assessment
Motor function neurological assessment What is focal neurological signs
What is focal neurological signs Abnormal flexion and extension
Abnormal flexion and extension Is adhd a neurological disorder
Is adhd a neurological disorder Muscle tone grading scale
Muscle tone grading scale Physio rehab centre
Physio rehab centre Neurological based behavior
Neurological based behavior Neurological examination
Neurological examination Muscle power neurological examination
Muscle power neurological examination Ao classification system
Ao classification system Neurological considerations in language acquisition
Neurological considerations in language acquisition The major premise of the neurological theory is that
The major premise of the neurological theory is that Solent nhs physiotherapy
Solent nhs physiotherapy Fudoscopy
Fudoscopy Neurological disease
Neurological disease Uw neurological surgery
Uw neurological surgery Normal pressure hydrocephalus triad
Normal pressure hydrocephalus triad Glasgow coma scale video
Glasgow coma scale video Process volume
Process volume Objectives of interior design
Objectives of interior design Limited assortment
Limited assortment Product variety and quality under monopoly
Product variety and quality under monopoly Starry night harmony unity and variety
Starry night harmony unity and variety Volume velocity variety veracity
Volume velocity variety veracity Product variety and quality under monopoly
Product variety and quality under monopoly Number and variety of pets
Number and variety of pets Variety and variability
Variety and variability Peristalsis
Peristalsis Wonnacott discrepancy matrix
Wonnacott discrepancy matrix Coroners and justice act
Coroners and justice act Saunders lewis and thornhill 2009
Saunders lewis and thornhill 2009 How to draw 1/5
How to draw 1/5 Unit 14 physiological disorders examples
Unit 14 physiological disorders examples Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Assistive technology for emotional and behavioral disorders
Assistive technology for emotional and behavioral disorders Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Physical disorders and health psychology
Physical disorders and health psychology Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Chapter 29 somatic symptom and dissociative disorders
Chapter 29 somatic symptom and dissociative disorders Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Personality disorder vs mental illness
Personality disorder vs mental illness Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Nail diseases and disorders milady
Nail diseases and disorders milady Axis 1 and 2 disorders
Axis 1 and 2 disorders Dissociative
Dissociative Unit 14 physiological disorders and their care
Unit 14 physiological disorders and their care Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Seborrheic keratoses
Seborrheic keratoses In what situation should a nail service be performed
In what situation should a nail service be performed Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Mild neurocognitive disorder
Mild neurocognitive disorder Protein metabolism mcq
Protein metabolism mcq Hypothalamus and eating disorders
Hypothalamus and eating disorders Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Difference between mendelian and chromosomal disorders
Difference between mendelian and chromosomal disorders Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Eating disorder in which people overeat compulsively
Eating disorder in which people overeat compulsively Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders What does fitt stand for
What does fitt stand for The fitt principle
The fitt principle Front loaded sentence examples
Front loaded sentence examples Prepare a variety of sandwiches
Prepare a variety of sandwiches Essentially derived variety
Essentially derived variety Variety refers to
Variety refers to What is this
What is this Principle of variety
Principle of variety Vernacular variety
Vernacular variety Pmr
Pmr Chapter 10 basics of saving and investing
Chapter 10 basics of saving and investing Variety of life in an area
Variety of life in an area Variety of perspectives
Variety of perspectives Vary variety various
Vary variety various Dr anbari
Dr anbari Combine sentences exercises
Combine sentences exercises Check variety
Check variety Language
Language Language dialect and varieties
Language dialect and varieties Bio variety
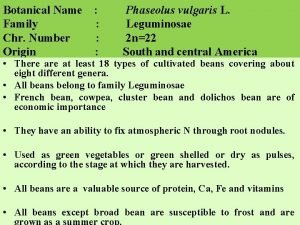
Bio variety Transverse cotyledon cracking in french bean
Transverse cotyledon cracking in french bean Gradation in art
Gradation in art Vary various variety
Vary various variety Walter cannon observed that a variety of stressors trigger
Walter cannon observed that a variety of stressors trigger Blanket family branding
Blanket family branding Prinsip variety adalah
Prinsip variety adalah Variety harmony
Variety harmony Halimbawa ng varayti ng wika
Halimbawa ng varayti ng wika Using despite in a sentence
Using despite in a sentence Name
Name Downdraft
Downdraft Product variety marketing example
Product variety marketing example 4v operation management
4v operation management Techniques of summarizing
Techniques of summarizing Numerous variety
Numerous variety What is a biome? *
What is a biome? * A variety
A variety Refers to the variety of training a performer undertakes
Refers to the variety of training a performer undertakes Cumulative sentence structure
Cumulative sentence structure Eel sentence
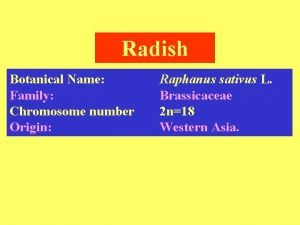
Eel sentence Radish scientific name and family
Radish scientific name and family Variety of poems
Variety of poems Volume dimension in operations management
Volume dimension in operations management Variety loving shoppers
Variety loving shoppers Language varieties
Language varieties Kitar nitrogen
Kitar nitrogen Sentence variety exercises
Sentence variety exercises Groundnut irrigation
Groundnut irrigation Walter cannon observed that a variety of stressors trigger
Walter cannon observed that a variety of stressors trigger Ndsu corn variety trials
Ndsu corn variety trials Variety of life on earth
Variety of life on earth Fitt table
Fitt table Chapter 36 skeletal muscular and integumentary systems
Chapter 36 skeletal muscular and integumentary systems Chapter 14 lesson 3 the nervous system
Chapter 14 lesson 3 the nervous system Venn diagram of muscular strength and endurance
Venn diagram of muscular strength and endurance Muscular system head and neck
Muscular system head and neck Skeletal and muscular system
Skeletal and muscular system Skeletal and muscular system
Skeletal and muscular system 2008-2009 school year
2008-2009 school year 2009 mathematics standards of learning answers
2009 mathematics standards of learning answers Sistema integral de servicio social
Sistema integral de servicio social Uma máquina fotográfica custava r$ 400
Uma máquina fotográfica custava r$ 400 Nmc record keeping guidance 2009
Nmc record keeping guidance 2009 Information services agreement intercommerce
Information services agreement intercommerce Plan nacional del buen vivir 2009 al 2013
Plan nacional del buen vivir 2009 al 2013 Permenkes no 51 tahun 2009
Permenkes no 51 tahun 2009 R.t.t. 2009
R.t.t. 2009 January 25 2018 chemistry regents answers
January 25 2018 chemistry regents answers Institutional calendar
Institutional calendar Rcfce act
Rcfce act Impaact 2009
Impaact 2009 In 2009 there were 1570 bears
In 2009 there were 1570 bears Rosa catania 2009
Rosa catania 2009