A Trip to the Audiologist What to Expect









- Slides: 24

A Trip to the Audiologist: What to Expect When Your Child Needs a Hearing Test KATHERINE DUNCAN, AU. D. , AND STACIA THOMAS, AU. D. MAINE EDUCATIONAL CENTER FOR THE DEAF AND HARD OF HEARING/GOVERNOR BAXTER SCHOOL FOR THE DEAF

Purpose of this webinar To provide an explanation about the various test procedures used by pediatric audiologists To provide parents with expectations surrounding their child’s visit to the audiologist To provide tips on how to make the visit to the audiologist as smooth as possible
Why is my child being referred for a hearing test? Refer on newborn hearing screening Concern from daycare, preschool, or pediatrician Parental concern Ear infections Family history of hearing loss Other risk factors

Case History The audiologist will need to collect a detailed case history from the parents Some examples of questions include: Birth history (ex: hypoxia at birth) History of ear infections Family history of childhood hearing loss Presence of risk factors (in-utero infections, ear tags) Other health issues or diagnoses (syndromes, etc. ) Other audiologic evaluations (including whether the child referred on UNHS)
Otoscopy The audiologist will use an otoscope to look at the external ear, ear canal, and eardrum/middle ear This is important to allow the audiologist to rule out occlusion of earwax, or concerns with middle ear health that can contribute to reports of diminished hearing and impact test findings Depending on a child’s comfort level, the audiologist may choose to wait until the end of the appointment in order to complete this
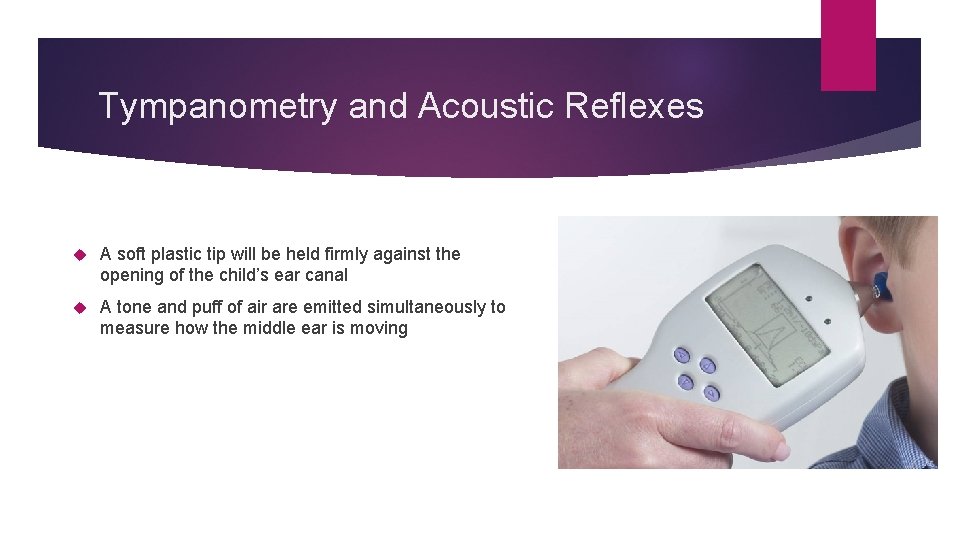
Tympanometry and Acoustic Reflexes A soft plastic tip will be held firmly against the opening of the child’s ear canal A tone and puff of air are emitted simultaneously to measure how the middle ear is moving

Tympanometry results do not tell the audiologist if the child can hear Tympanometry will tell the audiologist: If the ear drum is moving back and forth normally if the ear drum is stiff and not moving back and forth normally (this can mean fluid) if there is negative pressure in the space behind the ear drum, which is typically seen with allergies, sinus congestion, or at the beginning or end of a cold or ear infection
Acoustic Reflexes Can be completed in conjunction with tympanometry Loud tones are emitted, and the equipment looks for a response in the form of a contraction of a muscle in the middle ear called the stapedius (i. e. , the stapedius reflex) This information can be used to determine the origin of a hearing loss Is not always completed for young children due to time, need for the patient to stay still, and loudness of the presented tone
Otoacoustic Emissions A soft tip is placed in the ear canal, sending a tone to the inner ear A response from the hair cells of the cochlea (organ of hearing) is measured This response is known as an otoacoustic emission OAEs are sensitive to noise, movement, and health of the middle ear system Presence of OAEs suggests that there is no greater than a mild hearing loss
Behavioral Audiometry Dependent on the developmental age and abilities of the child Requires a response from the child in some way (head turn, block in bucket, button press, etc. ) Visual Reinforcement Audiometry Play Audiometry 6 months-2. 5 years of age 2. 5 years to 4 years of age Standard Audiometry 4 years of age and above
Visual Reinforcement Audiometry The child will sit on a parent’s lap in the booth The parent will be asked to “become part of the chair”: sit still and remain quiet at all times The audiologist will present sounds and talk quietly through speakers in the booth The audiologist will initially try to “condition” the child to the task, by presenting tones at a level they think the child will hear clearly, and reinforcing any response they receive After conditioning, tones and speech will be presented at varying intensities to determine the softest sounds to which the child will respond

Visual Reinforcement Audiometry The audiologist looks for the child to turn their head in response to a presented sound When the child turns their head successfully in a response to a sound, the audiologist will provide visual reinforcement There will be darkened boxes/screens in the corners of the booth where a brief video will play or puppet will be illuminated/move The visual reinforcement is meant to encourage the child to continue participating in the listening task

Play Audiometry The child is trained to listen for a sound and complete a task whenever they hear the sound Drop a block in a bucket, place a ring on a stacking ring toy Tones can be presented through the speakers or through headphones/inserts, depending on the child’s comfort level with headphones Children at this age may also be asked to repeat words or point to body parts to determine their ability to access speech stimuli

Standard Audiometry The child will be expected to raise their hand or press a button each time they hear a tone This typically happens through headphones or inserts The child will repeat words for the audiologist

Auditory Brainstem Response Evaluation The ABR measures the hearing nerve’s response to sound An ABR is typically performed whenever a child refers on the newborn hearing screening in order to confirm or rule out a hearing loss An ABR might also be performed on an older child if behavioral testing is inconclusive or the child cannot participate in behavioral testing The results of an ABR provide an objective measure of a child’s hearing and auditory function
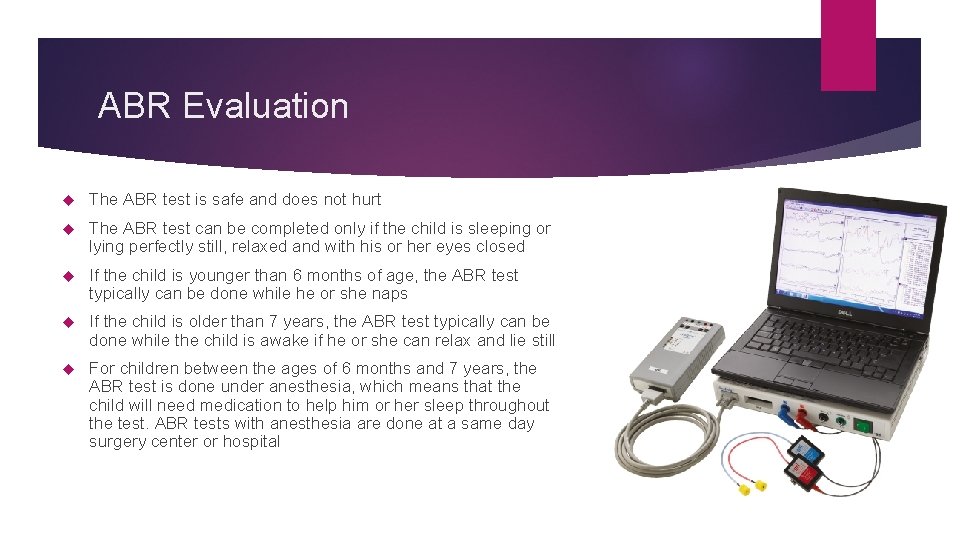
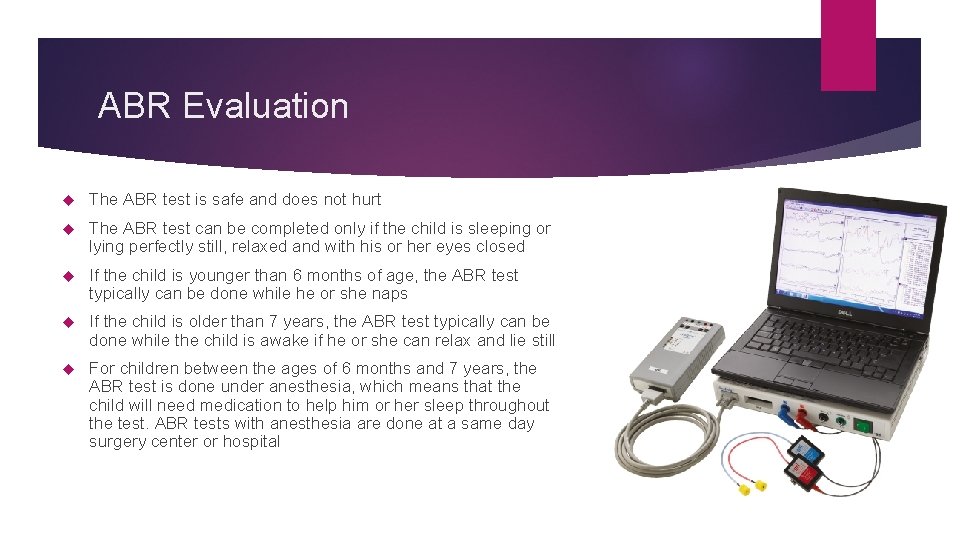
ABR Evaluation The ABR test is safe and does not hurt The ABR test can be completed only if the child is sleeping or lying perfectly still, relaxed and with his or her eyes closed If the child is younger than 6 months of age, the ABR test typically can be done while he or she naps If the child is older than 7 years, the ABR test typically can be done while the child is awake if he or she can relax and lie still For children between the ages of 6 months and 7 years, the ABR test is done under anesthesia, which means that the child will need medication to help him or her sleep throughout the test. ABR tests with anesthesia are done at a same day surgery center or hospital
ABR Evaluation 3 -4 small stickers or electrodes are placed at various points on the child’s head and in front of their ears The electrodes are connected via wires to a special computer Sound is sent to the child’s ears using insert earphones The electrodes measure how the auditory nerve and brainstem respond to the sounds sent through the inserts The audiologist interprets the responses provided by the ABR equipment by looking for certain neurological “markers” that correspond with expected areas of stimulation along the auditory system The audiologist will look for the softest loudness level at which these markers are present across multiple frequencies, which will help determine the child’s hearing levels
Parents and guardians can contribute to the success of the ABR! Babies under 6 months Testing will occur with the child asleep Ideally, should arrive with the child tired and hungry The child should be fed just before the test, with the goal to get them to nap during the test Testing can occur with the child in the car seat, or in a parent’s arms

Preparation for the ABR Children between 6 months and 7 years of age Typically, requires sedation to sleep throughout ABR Hospital/surgical center should prep parents regarding rules for eating/drinking prior to anesthesia If rules for eating/drinking are not followed, the ABR may be rescheduled
Preparation for the ABR Children older than 7 years Typically, the child can be tested while awake if they are relaxed and still If non-sedated testing is not successful, the child may be referred for a sedated ABR
Tips for having a successful trip Each trip to the audiologist may be different! Traveling far for your audiology appointment? Try to relax Siblings Cell phone Morning vs. afternoon appointment Be present during the counseling session at the end of the appointment
 Career cluster images
Career cluster images Wimbledon audiologist
Wimbledon audiologist Once upon a time there were three billy goats gruff
Once upon a time there were three billy goats gruff What to expect at resea appointment
What to expect at resea appointment Monolith etymology
Monolith etymology Womb to tomb psychology
Womb to tomb psychology Walkthrough of the parts of the entire work immersion
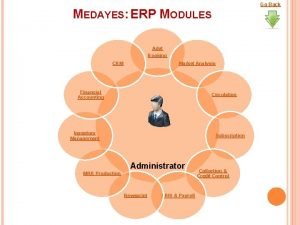
Walkthrough of the parts of the entire work immersion Alone together book review
Alone together book review Expect the unexpected
Expect the unexpected Parents impose rules and expect obedience
Parents impose rules and expect obedience Anticipation guide for the necklace
Anticipation guide for the necklace What do you expect
What do you expect Finish verb pattern
Finish verb pattern Die 2. ve 3. hali
Die 2. ve 3. hali Never expect the unexpected
Never expect the unexpected True-tone ab-700 model ultra glide
True-tone ab-700 model ultra glide What do you expect to learn
What do you expect to learn Factors of care a patient can expect
Factors of care a patient can expect Expect tool
Expect tool Parents impose rules and expect obedience
Parents impose rules and expect obedience Food and beverage directors expect a pour cost of
Food and beverage directors expect a pour cost of Dont expect more
Dont expect more đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới