A Telehealth Integrated Chronic Care Management Model CCM
- Slides: 2
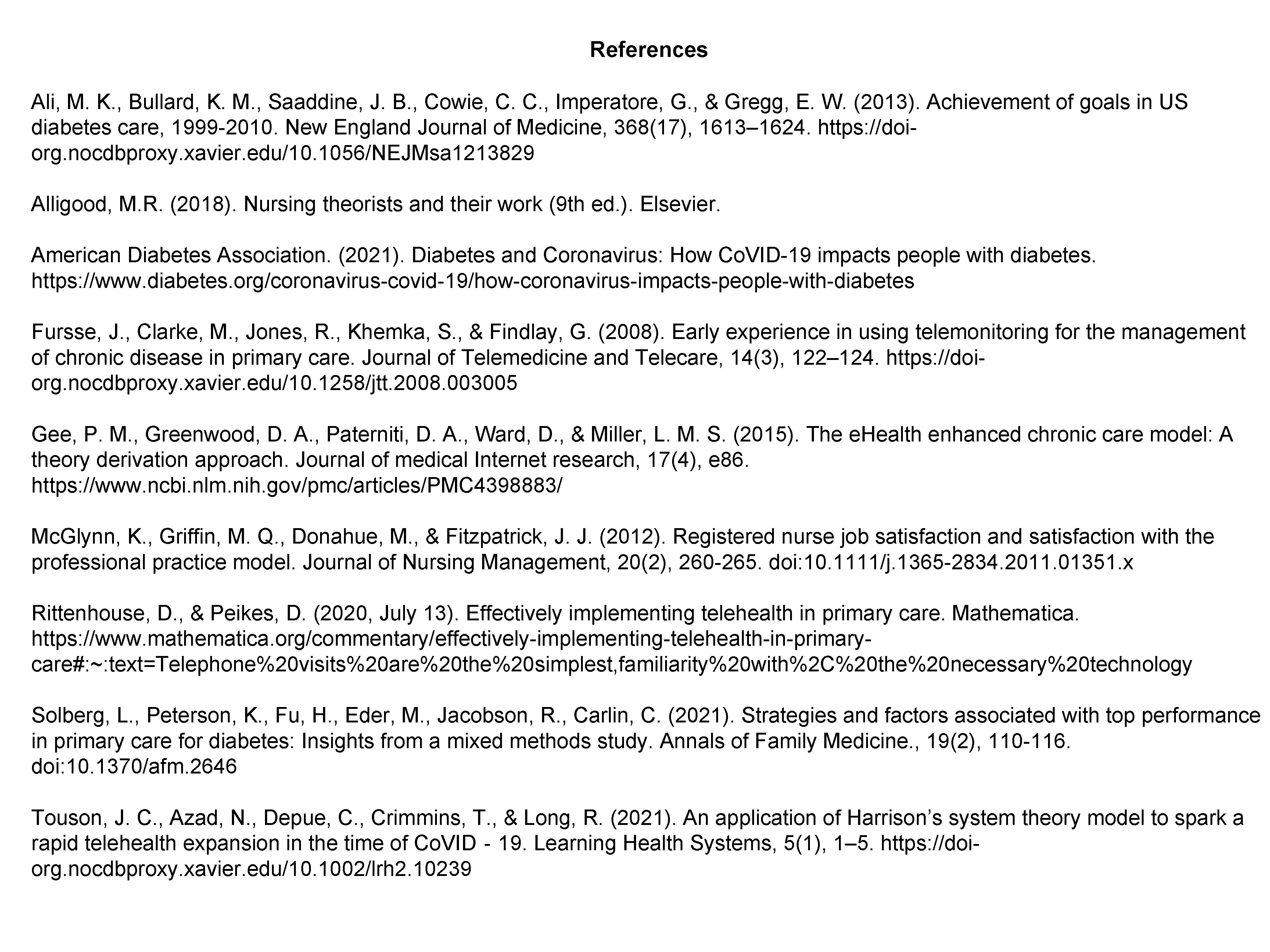
A Telehealth Integrated Chronic Care Management Model (CCM) for Type II Diabetes Ryan E. Baumgartner, B. S. N. , R. N. Xavier University College of Nursing Background Telemedicine has become a critical strategy to improve access to diabetes care during the Co. VID-19 Pandemic. The Co. VID-19 Pandemic has socially distanced the public and changed operations at the Cincinnati Health Department (CHD). Adjustments in the delivery of essential patient care had to be made and routine office appointments for CCM were suddenly canceled. CHD’s leadership searched for innovative models for providing remote diabetic care that is cost-effective, efficient, and safe. Purpose This project aims to develop a chronic care management (CCM) model that integrates telehealth services for the delivery of nursing care to the type 2 diabetic (DM 2) patient. The overarching goal is to have this model adopted and implemented into practice at the Cincinnati Health Department (CHD). A well-developed and effective diabetes care management model's objective is to control blood glucose. This objective can be accomplished in two ways using telehealth as the delivery platform. Healthy lifestyle modification, including dietary changes, regular physical exercise, weight reduction as specified by the nurse Provide medication management. Literature Review This literature review identified and evaluated high-quality, evidence-based practices (EBP) in scholarly articles, reviews, studies, and meta-analyses, providing evidence that the combination of telehealth technologies with diabetic CCM could be a practical approach to managing glycemic control in the DM 2 patient remotely. The three databases used most frequently in this literature search were Pub. Med, MEDLINE, and CINAHL, using the search words telehealth, chronic disease, patient education, and related concepts. Sufficient evidence supporting these tenets was uncovered, suggesting developing a telehealth-integrated CCM model for the DM 2 patient will be effective, cost-efficient, and safe while improving patient outcomes and clinical practices. This review examined citations from government websites that provided research strategies for finding clinical studies, EBP, and systematic reviews. Ida Jean Orlando’s 1961 Nursing Process Theory This theory offers nurses guidance for framing care delivery models when circumstances require technology in nursing practice. The development of new nursing practices to include modern technologies is essential for overcoming barriers to patient care. In Orlando's theory, the nurse's role is to seek out and meet the patient's immediate needs. As the pandemic has restricted access to care, patients experience distress in not having their needs met. Using these principles, an approach to remote diabetic care allows the nurse to appropriately and promptly respond to the patients' needs has been framed (Alligood, 2018). Projection Description The Delivery System Design element of the Tele-CCM Model assures efficient, effective care and selfmanagement support (Gee et al. , 2015). This element comes with five change concepts. These concepts are foundational to the structure of the Tele-CCM Model. They include the following: a) define roles and distribute tasks among team members, b) use planned interactions to support evidence-based care, c) provide clinical case management services for complex patients, d) ensure regular follow-up by the care team, and e) give care that patients understand, and that agrees with their cultural background. These concepts provided a framework for structuring the diabetic care management component of this new Model. Change Theory Harrison’s Model applied to Orlando’s Nursing Process Theory (below). Harrison’s Model illustrates the relationship between culture, behavior, technology, and structure related to external forces. The organization must use what resources (input) they have available to them and incorporate them (telehealth) into their processes (diabetes care) to provide essential patient services (output). From Touson et al. (2021). Measurable/Targeted outcomes Planned Evaluation Utilization: Tracking of nurse telehealth encounters will be Like the Tele-CCM Model developed for this project, reported once a week. The site champion will also be the previous models aimed to improve clinical outcomes, patient CCM-C. Initially, the target goal will be ten completed Teleexperience, nurse/provider satisfaction, and reduce costs CCM at each health center (one nurse) per week. The (Ali et al. , 2013). target goal will increase incrementally as the nurse uses the When the Tele-CCM Model is adopted and implemented, new care model. CHD administration can expect improved patient outcomes. Clinical Outcomes: Baseline values should be noted before These improvements can be used to monitor plan objectives the initial Tele-CCM visit, and these values should be using the HRSA quality measures to benchmark project reevaluated at three-month intervals. When reductions progress. (improvements) in these values are observed, program HRSA endorsed the IOM to examine the potential of effectiveness can be assumed telehealth care delivery services over two decades ago. One Profitability: Benchmarking clinical improvements and of these metrics included the Hgba 1 c. outcomes with metrics meet HRSA quality standards. When these standards are met, the organization is awarded Point-of-Care Hgb. A 1 c’s will be collected on-site every 3 federal funding. months. User Satisfaction: Feedback from point-of-care providers When reductions in this value are observed in patients and patients is critical (Mc. Glynn et al. , 2012). Semiannual provided with Tele-CCM nursing services, it will indicate the Implications, Recommendations , & Relevance to Nursing surveys will be distributed to patients receiving Tele-CCM successful implementation of the Model. Tele-CCM Services Model for Diabetes Type II Discussion In a recent study (ADA, 2021) 2, 500 individuals with DM 2 found that 9% of respondents said they could not afford medical care during the pandemic. One in five people said they had foregone getting an insulin pump or continuous glucose monitor (CGM), attributing financial strain. 15% of people with diabetes who rely on management technologies like pumps or CGMs have delayed refilling diabetic testing supplies and needles during the pandemic; 70% of these respondents, this was also due to financial strain. 12% of people with diabetes have experienced a disruption in insurance coverage since the start of the pandemic; of those who lost coverage due to the pandemic, half could not regain coverage. In a related survey (Solberg et al. 2021), researchers found that despite these setbacks faced by the DM 2 population during the pandemic, many have appeared to benefit from increased access and use of telehealth services. 73% percent of people with DM 2 have used telehealth services during the pandemic, compared to 11% before Co. VID-19. Of those who have utilized telehealth, 40% report that it has made it easier to manage their diabetes, compared with 37% who reported no change. 36% say they plan to continue seeking health care remotely after the pandemic (Solberg et al. , 2021). and the nurses who provide it. These surveys will be anonymous. Nurse Tele-CCM visits offer a broader reach to the larger communities. Giving nurses the ability to manage diabetic care via telehealth can maintain the patient-provider relationship. It also is an avenue by which nurses can reestablish relationships between the CHD and members of the community lost to care in the wake of the pandemic (Fursse et al. , 2008). The Tele-CCM Model can guide tentative payment structures that manage the current national state of emergency and help prepare the CHD’s financial officers to negotiate for future payor reimbursement plans (Rittenhouse & Peikes, 2020). Conclusion As other industries seamlessly moved to virtual interactions, healthcare organizations, like the CHD, are continually challenged with their obligations to provide patient care in a virtual capacity. The organization’s leadership continues to search for innovative models for delivering remote diabetic care that is cost-effective, efficient, and safe to the population they serve. Future adoption of the Tele-CCM Model by CHD leadership, coupled with stakeholder participation, will allow the CHD to deliver a much-needed service to those socially distanced populations further removed from access to care by the pandemic restrictions.
References Ali, M. K. , Bullard, K. M. , Saaddine, J. B. , Cowie, C. C. , Imperatore, G. , & Gregg, E. W. (2013). Achievement of goals in US diabetes care, 1999 -2010. New England Journal of Medicine, 368(17), 1613– 1624. https: //doiorg. nocdbproxy. xavier. edu/10. 1056/NEJMsa 1213829 Alligood, M. R. (2018). Nursing theorists and their work (9 th ed. ). Elsevier. American Diabetes Association. (2021). Diabetes and Coronavirus: How Co. VID-19 impacts people with diabetes. https: //www. diabetes. org/coronavirus-covid-19/how-coronavirus-impacts-people-with-diabetes Fursse, J. , Clarke, M. , Jones, R. , Khemka, S. , & Findlay, G. (2008). Early experience in using telemonitoring for the management of chronic disease in primary care. Journal of Telemedicine and Telecare, 14(3), 122– 124. https: //doiorg. nocdbproxy. xavier. edu/10. 1258/jtt. 2008. 003005 Gee, P. M. , Greenwood, D. A. , Paterniti, D. A. , Ward, D. , & Miller, L. M. S. (2015). The e. Health enhanced chronic care model: A theory derivation approach. Journal of medical Internet research, 17(4), e 86. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 4398883/ Mc. Glynn, K. , Griffin, M. Q. , Donahue, M. , & Fitzpatrick, J. J. (2012). Registered nurse job satisfaction and satisfaction with the professional practice model. Journal of Nursing Management, 20(2), 260 -265. doi: 10. 1111/j. 1365 -2834. 2011. 01351. x Rittenhouse, D. , & Peikes, D. (2020, July 13). Effectively implementing telehealth in primary care. Mathematica. https: //www. mathematica. org/commentary/effectively-implementing-telehealth-in-primarycare#: ~: text=Telephone%20 visits%20 are%20 the%20 simplest, familiarity%20 with%2 C%20 the%20 necessary%20 technology Solberg, L. , Peterson, K. , Fu, H. , Eder, M. , Jacobson, R. , Carlin, C. (2021). Strategies and factors associated with top performance in primary care for diabetes: Insights from a mixed methods study. Annals of Family Medicine. , 19(2), 110 -116. doi: 10. 1370/afm. 2646 Touson, J. C. , Azad, N. , Depue, C. , Crimmins, T. , & Long, R. (2021). An application of Harrison’s system theory model to spark a rapid telehealth expansion in the time of Co. VID‐ 19. Learning Health Systems, 5(1), 1– 5. https: //doiorg. nocdbproxy. xavier. edu/10. 1002/lrh 2. 10239