A Route Map using Theory of Change Understanding


- Slides: 19
A Route Map using Theory of Change: Understanding the impact of the Living With and Beyond Cancer model for people affected by cancer Macmillan Cancer Support in partnership with… Richard Metcalfe - Programme Lead Hayley Williams - Clinical Pathway Manager Sarah Allen - Macmillan Evidence Officer

Wi. Fi name: Wifi. Love. MCR Password: internet Join the conversation on Twitter using #Driving. Change
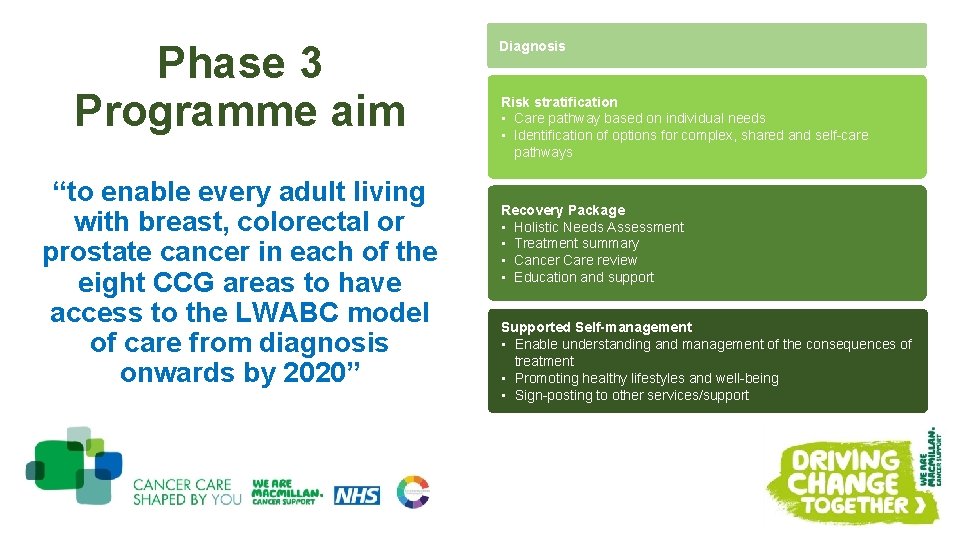
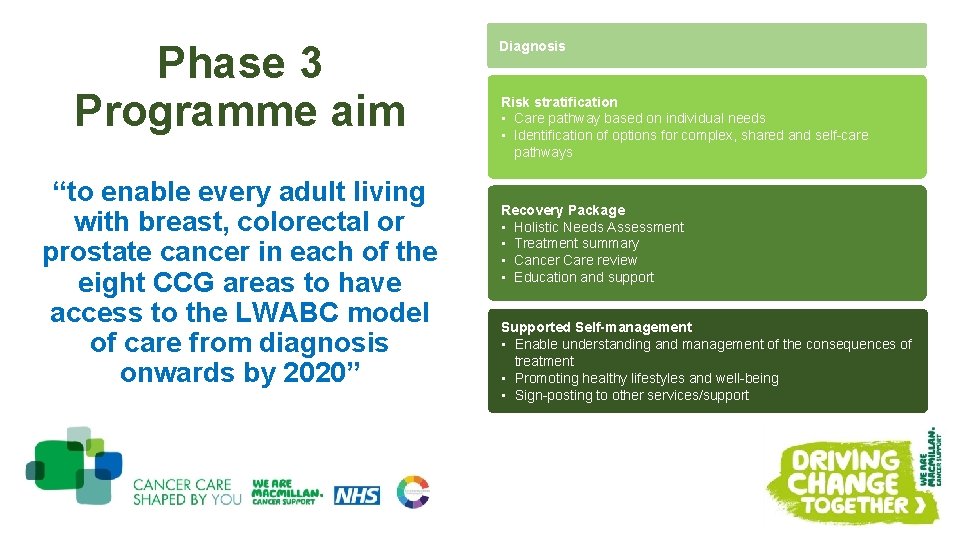
Phase 3 Programme aim “to enable every adult living with breast, colorectal or prostate cancer in each of the eight CCG areas to have access to the LWABC model of care from diagnosis onwards by 2020” Diagnosis Risk stratification • Care pathway based on individual needs • Identification of options for complex, shared and self-care pathways Recovery Package • Holistic Needs Assessment • Treatment summary • Cancer Care review • Education and support Supported Self-management • Enable understanding and management of the consequences of treatment • Promoting healthy lifestyles and well-being • Sign-posting to other services/support
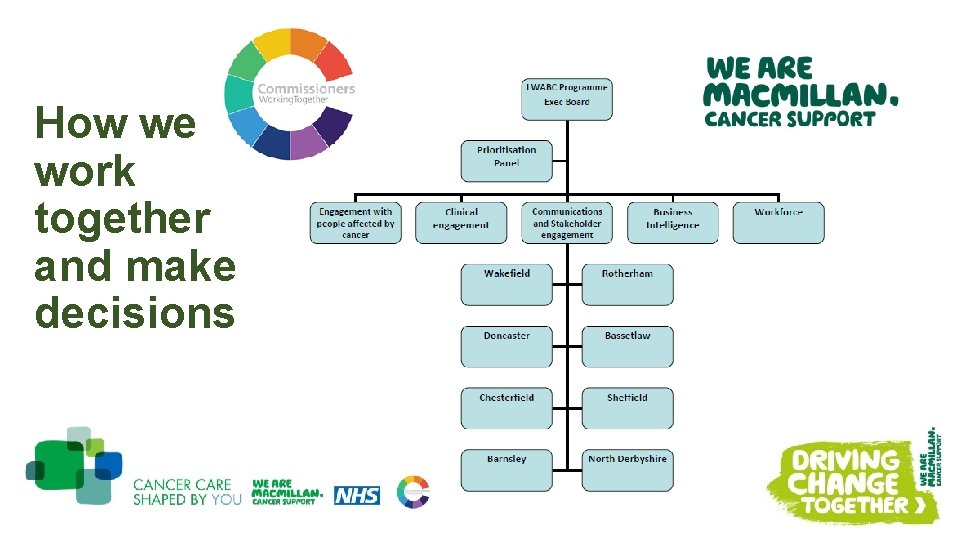
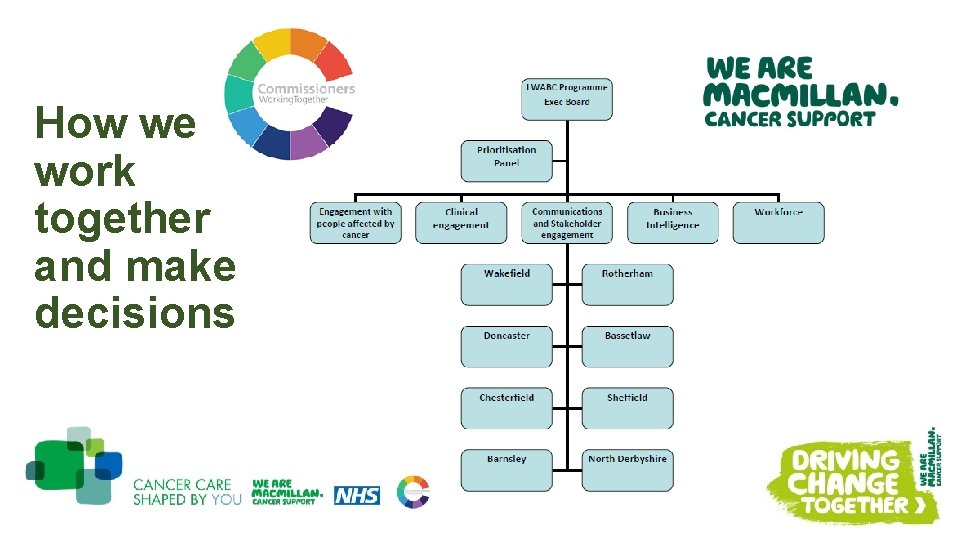
How we work together and make decisions
Programme priorities • Clinical Engagement model Risk stratification in 3 ‘Clinical Delivery Groups’ 150 clinicians & managers Lead CNS group • e-HNA/treatment summary and PROMS (x 5 acute trusts) • Programme Evaluation – testing theories of change, what is the impact so what? evidence of the RP as a coherent package? • Communications and engagement strategy • Engagement with People affected by cancer ……
• Utilising localities intelligence and what we already know from the CPES, regional and local engagement work • Principles for engagement with people affected by cancer – consulted with the public during summer 2016 • Building on co-production experience and skills across the footprint ave. 60 people affected by cancer per locality involved in co-designing solutions • Specific work via the voluntary and community sector organisations to engage reach/seldom heard groups • Using intelligence from conversations with people affected by cancer to inform a decision making framework • Development of an Advisory board of people affected by cancer – representative of the localities to support decision making • Continued involvement of PABC in recruitment
Themes from across our localities • Lots of great work, staff and services out there • Having ‘Conversations’, tools and validation: person centred conversations with a meaningful shared care plan … the elements of the LWABC model (e. g. : HNA, Treatment summary, Cancer Care review) are tools/enablers • Importance of community access, co-ordination and linking PABC to support (navigation) • Need for diverse access and delivery options e. g. : support, physical activity and information • It’s not just about specialist cancer services • Risk stratification • Cancer Care Reviews – what/how/quality? • Models of care around GP practices; local communities/neighbourhoods (primary care strategy) • Workforce development: culture, training, roles • All tumour sites/x 3 tumour sites programme
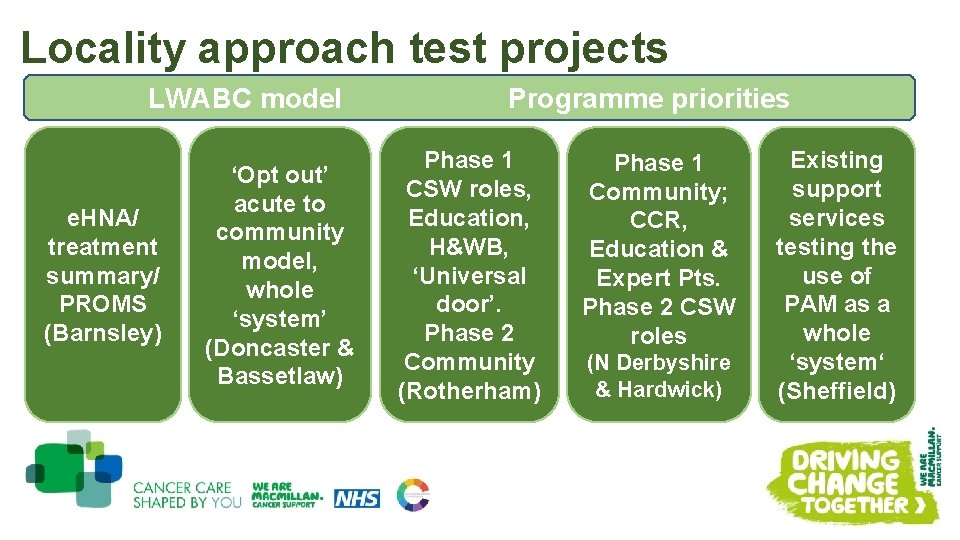
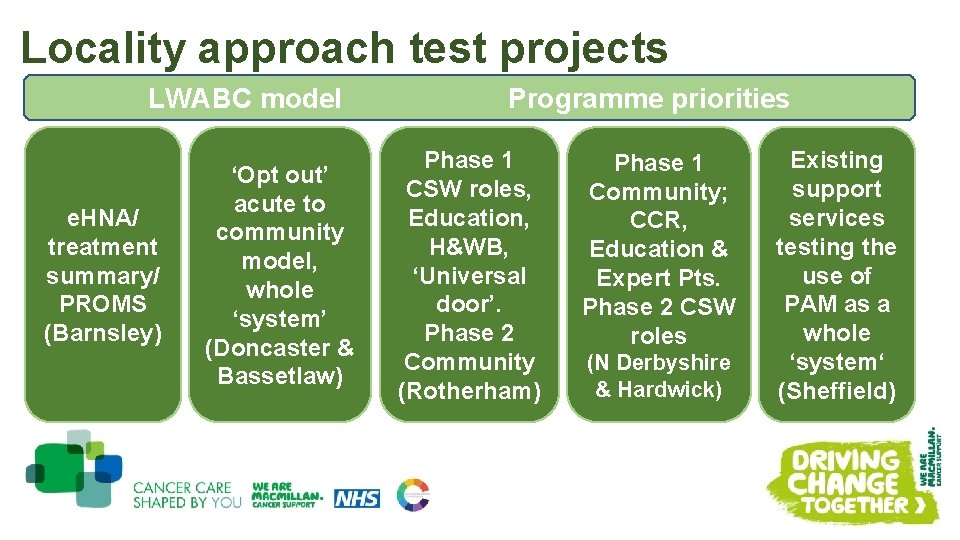
Locality approach test projects LWABC model e. HNA/ treatment summary/ PROMS (Barnsley) ‘Opt out’ acute to community model, whole ‘system’ (Doncaster & Bassetlaw) Programme priorities Phase 1 CSW roles, Education, H&WB, ‘Universal door’. Phase 2 Community (Rotherham) Phase 1 Community; CCR, Education & Expert Pts. Phase 2 CSW roles (N Derbyshire & Hardwick) Existing support services testing the use of PAM as a whole ‘system‘ (Sheffield)
Theory of change what it is and how to use it
Key messages – theory of change • It aims to provide clarity about what we think a programme will achieve and how (emphasis on causality and explicit assumptions) • It enables stronger programme design, monitoring and evaluation. • It should be revised over time as programmes evolve and evidence becomes available • It should ideally be developed at design stage but adds value at any stage of the programme cycle 10
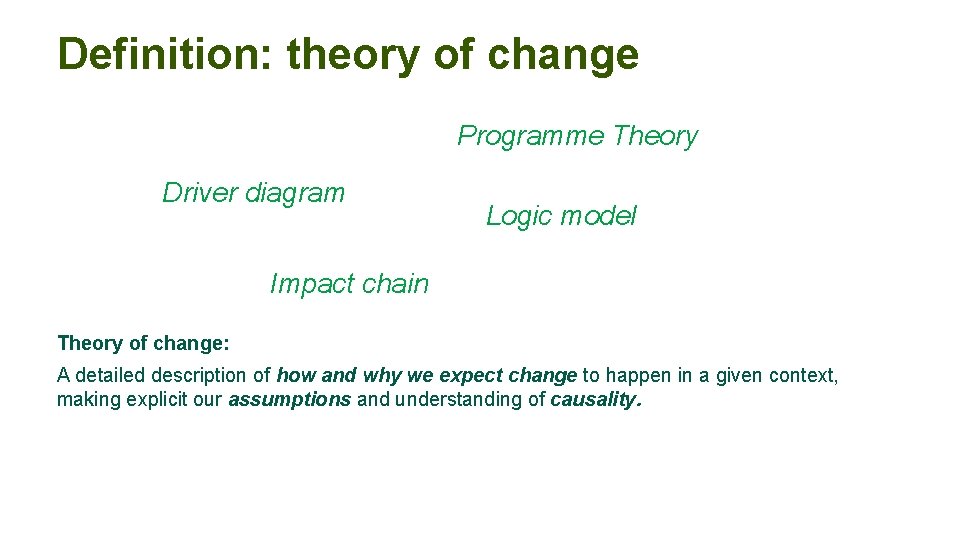
Definition: theory of change Programme Theory Driver diagram Logic model Impact chain Theory of change: A detailed description of how and why we expect change to happen in a given context, making explicit our assumptions and understanding of causality.
Why do a theory of change? How? Change happens Why? For whom?
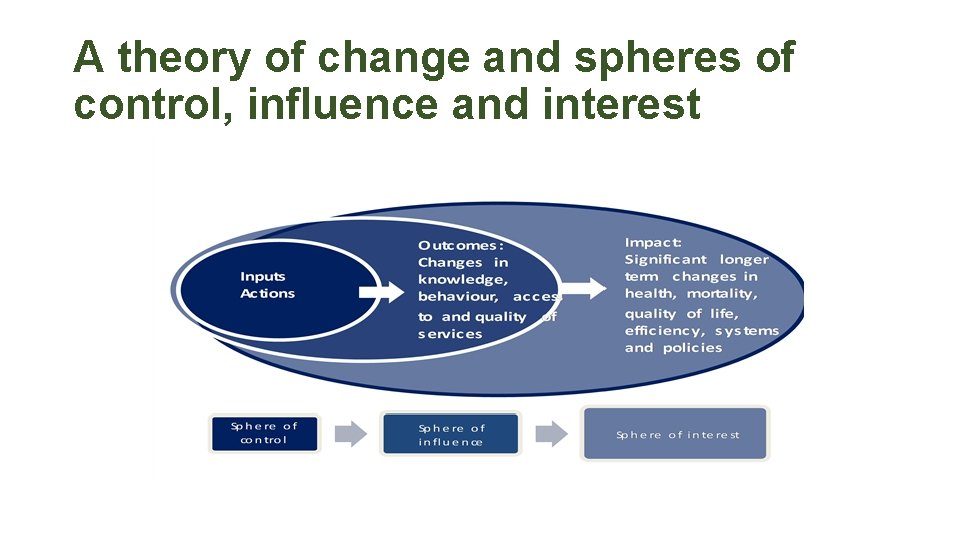
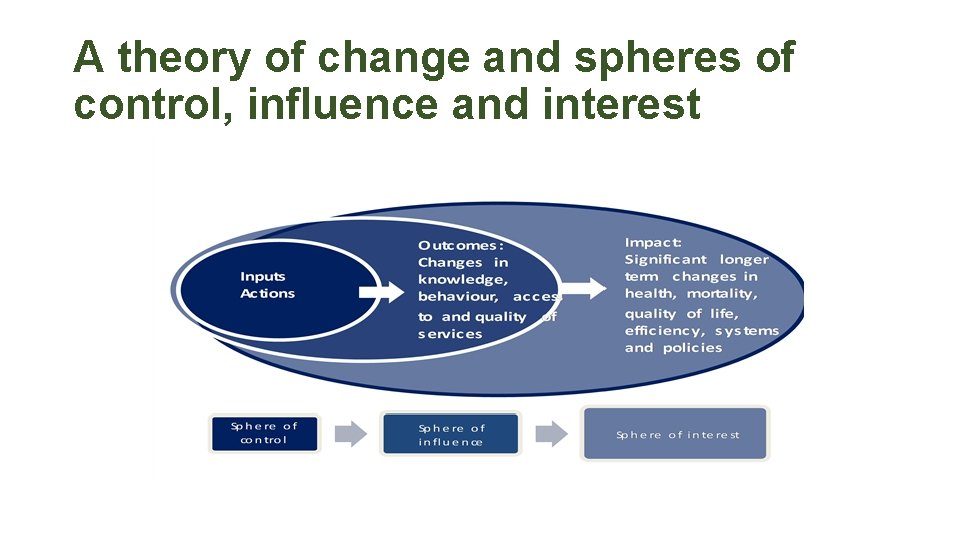
A theory of change and spheres of control, influence and interest •
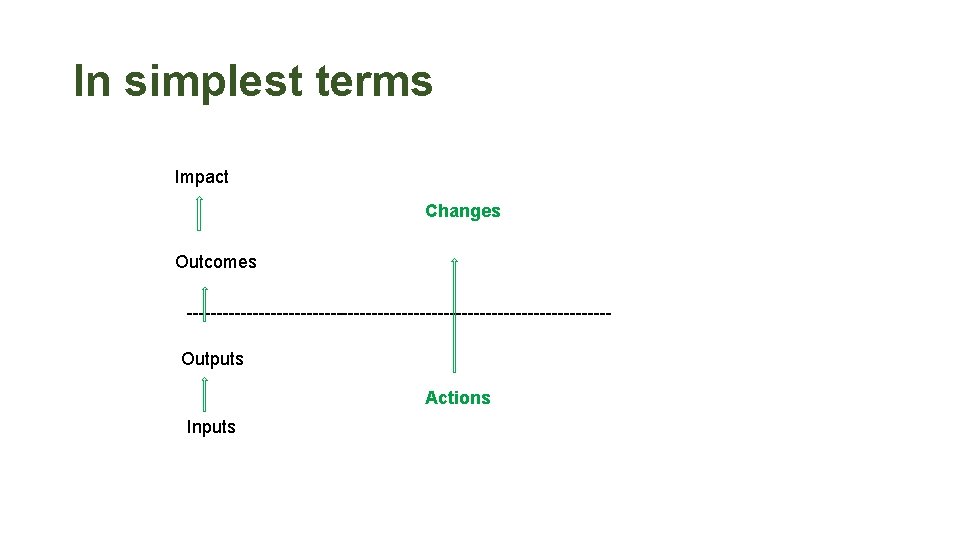
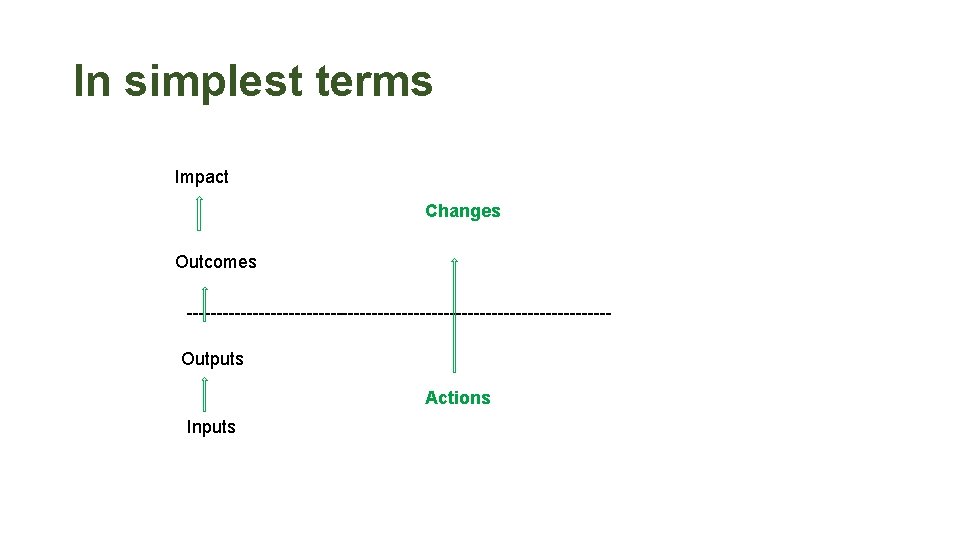
In simplest terms Impact Changes Outcomes -----------------------------------Outputs Actions Inputs
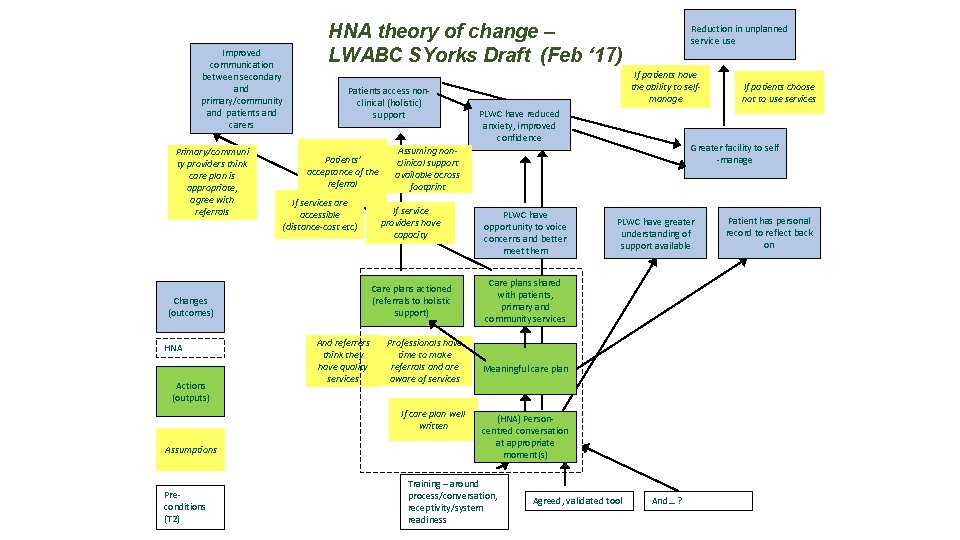
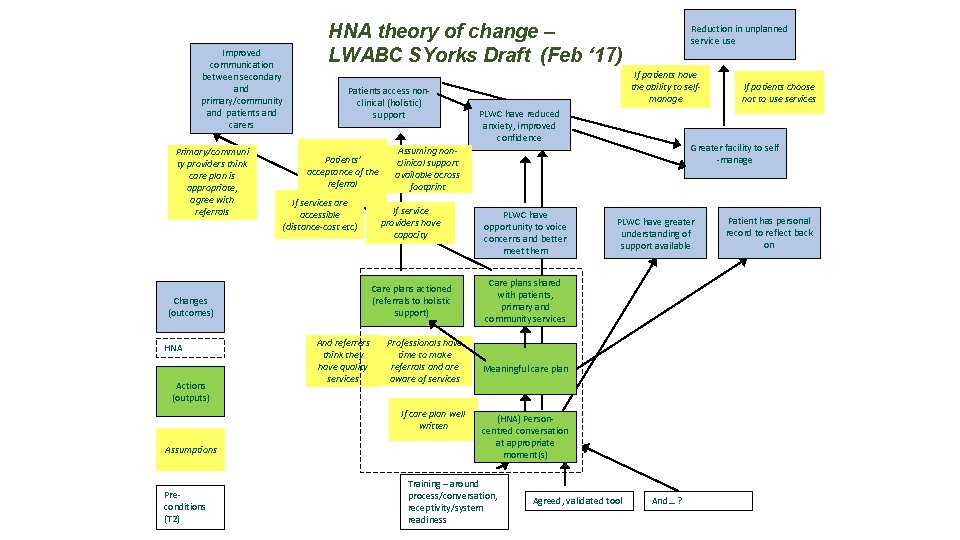
Improved communication between secondary and primary/community and patients and carers Primary/communi ty providers think care plan is appropriate, agree with referrals HNA theory of change – LWABC SYorks Draft (Feb ‘ 17) Patients access nonclinical (holistic) support Patients’ acceptance of the referral If services are accessible (distance-cost etc) HNA Actions (outputs) And referrers think they have quality services If service providers have capacity Professionals have time to make referrals and are aware of services If care plan well written Assumptions Preconditions (T 2) If patients have the ability to selfmanage PLWC have reduced anxiety, improved confidence PLWC have opportunity to voice concerns and better meet them PLWC have greater understanding of support available Care plans shared with patients, primary and community services Meaningful care plan (HNA) Personcentred conversation at appropriate moment(s) Training – around process/conversation, receptivity/system readiness If patients choose not to use services Greater facility to self -manage Assuming nonclinical support available across footprint Care plans actioned (referrals to holistic support) Changes (outcomes) Reduction in unplanned service use Agreed, validated tool And… ? Patient has personal record to reflect back on
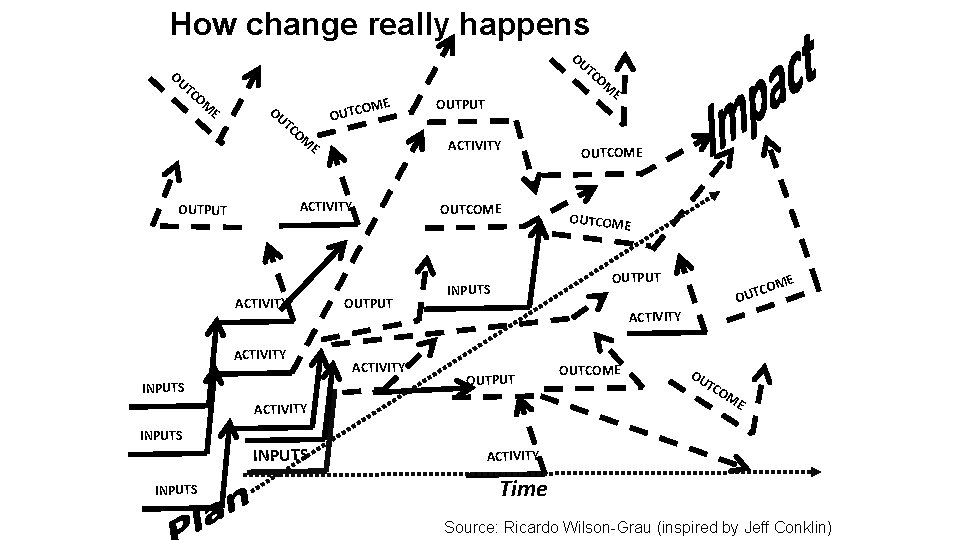
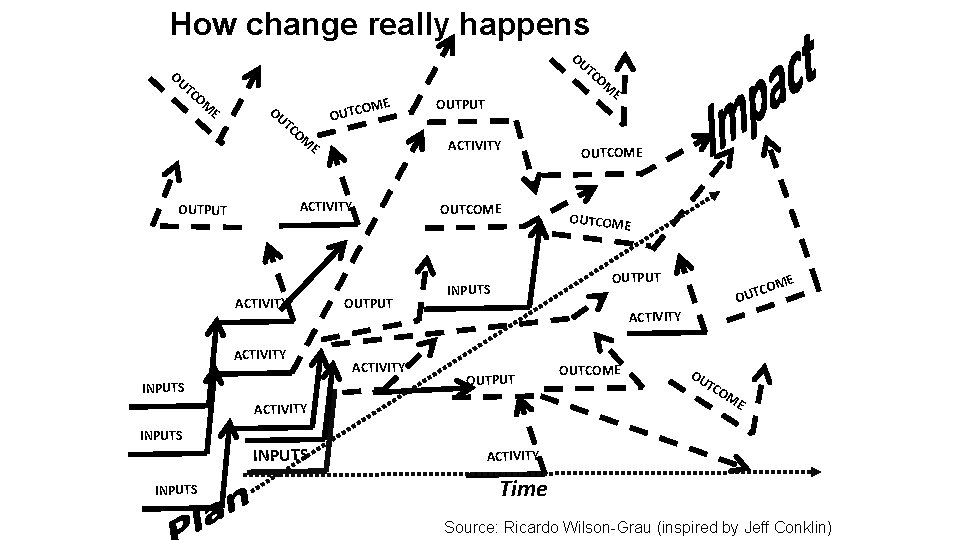
How change really happens OU TC OM E OU OME OUTC TC OM ACTIVITY OUTPUT ACTIVITY INPUTS E OUTPUT ACTIVITY OUTCOME INPUTS OUTCOME OUTPUT INPUTS COM OUT E ACTIVITY OUTPUT ACTIVITY INPUTS OM OUTCOME OU TC OM E ACTIVITY Time Source: Ricardo Wilson-Grau (inspired by Jeff Conklin)
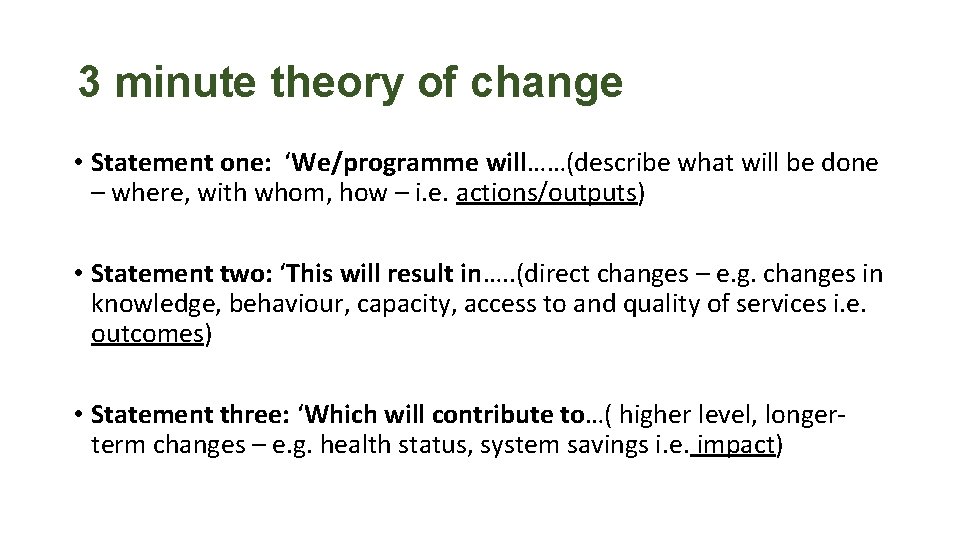
3 minute theory of change • Statement one: ‘We/programme will……(describe what will be done – where, with whom, how – i. e. actions/outputs) • Statement two: ‘This will result in…. . (direct changes – e. g. changes in knowledge, behaviour, capacity, access to and quality of services i. e. outcomes) • Statement three: ‘Which will contribute to…( higher level, longerterm changes – e. g. health status, system savings i. e. impact)
3 minute theory of change Example 1: My Party • I will…. buy food and drink, send out invitations, tidy up my house, pick out music (activities-outputs) • This will result in …. . my friends coming to my party, eating, drinking and dancing (outcomes – changes in behaviour) • And will contribute to…. . them having a good weekend (impact – wider change to their well-being)

Richard Metcalfe – richard. metcalfe 1@nhs. net Hayley Williams - hwilliams 2@nhs. net Sarah Allen - SAllen@macmillan. org. uk