A retrospective audit of compliance and validity of


- Slides: 11

A retrospective audit of compliance and validity of consent in a tertiary teaching hospital Dr Jonathan Roddy Department of Anaesthesiology Children’s University Hospital, Temple Street
Background o Legal and ethical requirement o Guidance has been issued by the Medical Council and the HSE[1][2] o Valid consent; o Comprehension - Informed o Voluntary o Capacity o Remarkable heterogeneity in obtaining consent for children presenting to theatre [1] Irish Medical Council, “Good medical practice in seeking informed consent to treatment” (2008) [2] HSE national consent policy (https: //www. hse. ie/eng/about/who/qid/other-quality-improvement-programmes/consent/nationalconsent-policy-hse-v 1 -3 -june-2019. pdf)
Aim o To assess the current practice of obtaining informed consent in our institution o To determine compliance with the HSE guidelines on obtaining informed consent o To identify any appropriate remedial action required to ensure a suitable standard of care is achieved o The implementation of any remediation which become apparent o To ultimately re-audit the consent process to determine the effectiveness of our interventions
Methods o Information collected over 4 weeks o Every child who presented to theatre between 0800 -1700 o Consent form compared under the headings of; o Disclosure o Comprehension o Voluntariness o Capacity o 408 charts reviewed
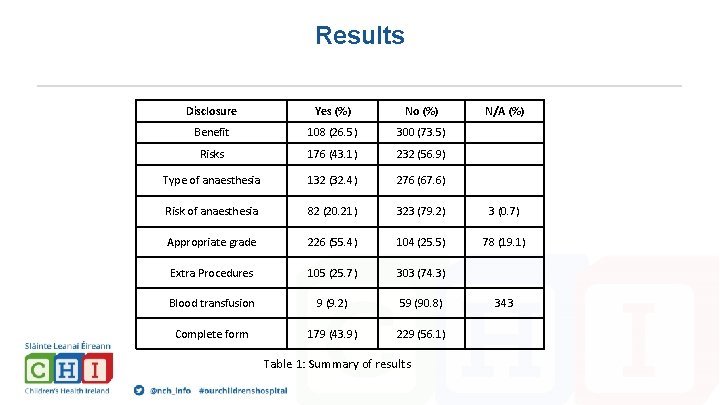
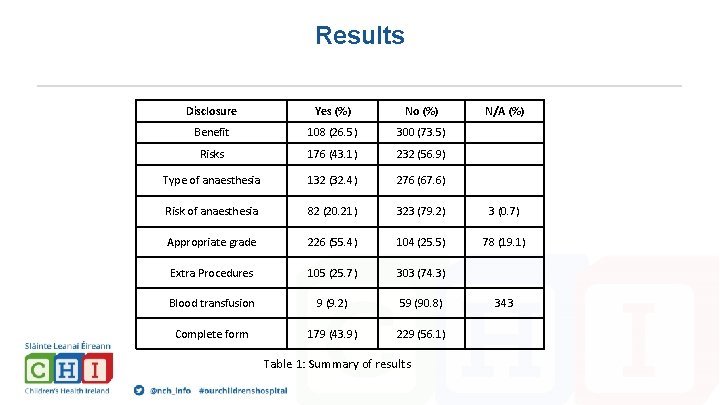
Results Disclosure Yes (%) No (%) Benefit 108 (26. 5) 300 (73. 5) Risks 176 (43. 1) 232 (56. 9) Type of anaesthesia 132 (32. 4) 276 (67. 6) Risk of anaesthesia 82 (20. 21) 323 (79. 2) 3 (0. 7) Appropriate grade 226 (55. 4) 104 (25. 5) 78 (19. 1) Extra Procedures 105 (25. 7) 303 (74. 3) Blood transfusion 9 (9. 2) 59 (90. 8) Complete form 179 (43. 9) 229 (56. 1) Table 1: Summary of results N/A (%) 343
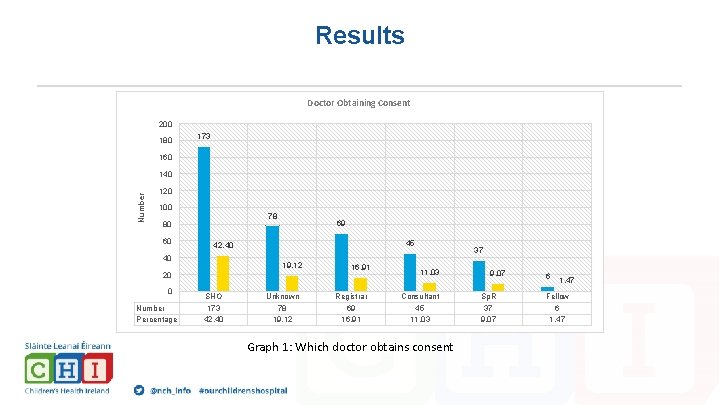
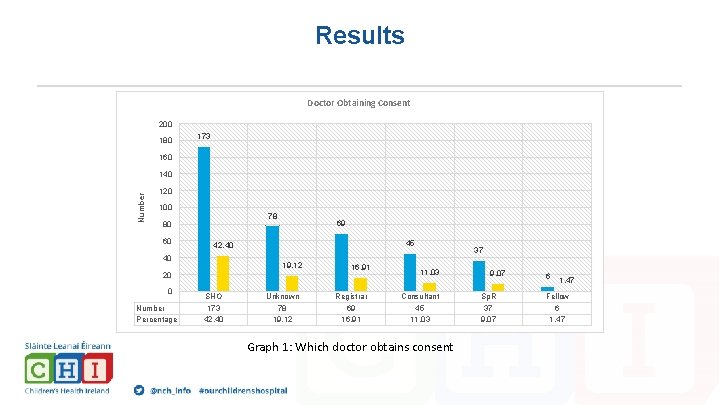
Results Doctor Obtaining Consent 200 180 173 160 Number 140 120 100 78 80 60 69 45 42, 40 40 19, 12 20 0 Number Percentage SHO 173 42, 40 Unknown 78 19, 12 16, 91 Registrar 69 16, 91 37 11, 03 Consultant 45 11, 03 Graph 1: Which doctor obtains consent 9, 07 Sp. R 37 9, 07 6 1, 47 Fellow 6 1, 47
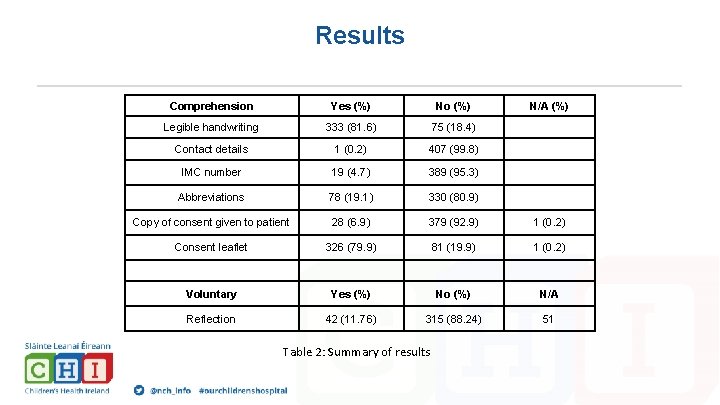
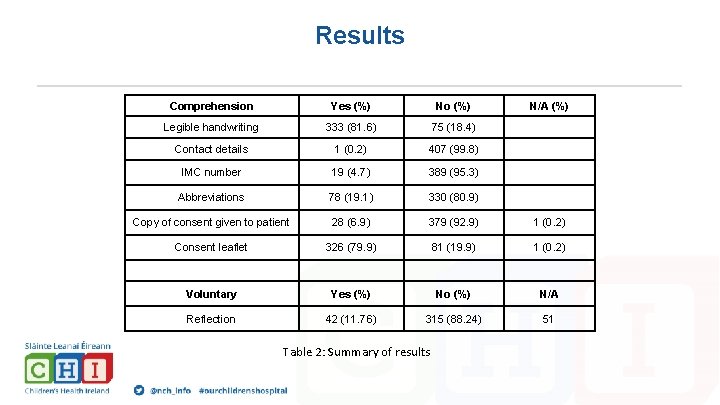
Results Comprehension Yes (%) No (%) Legible handwriting 333 (81. 6) 75 (18. 4) Contact details 1 (0. 2) 407 (99. 8) IMC number 19 (4. 7) 389 (95. 3) Abbreviations 78 (19. 1) 330 (80. 9) Copy of consent given to patient 28 (6. 9) 379 (92. 9) 1 (0. 2) Consent leaflet 326 (79. 9) 81 (19. 9) 1 (0. 2) Voluntary Yes (%) No (%) N/A Reflection 42 (11. 76) 315 (88. 24) 51 Table 2: Summary of results N/A (%)
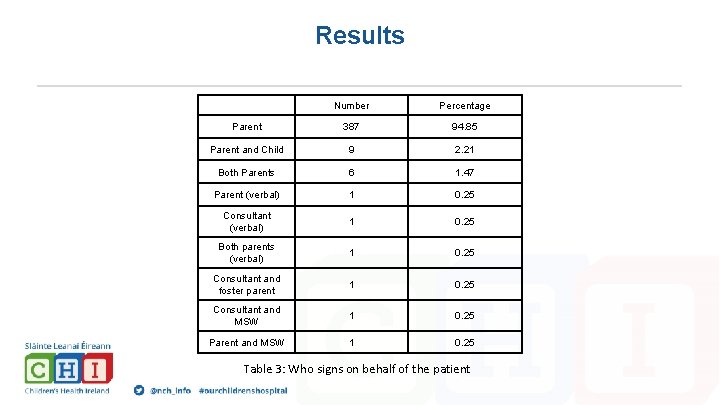
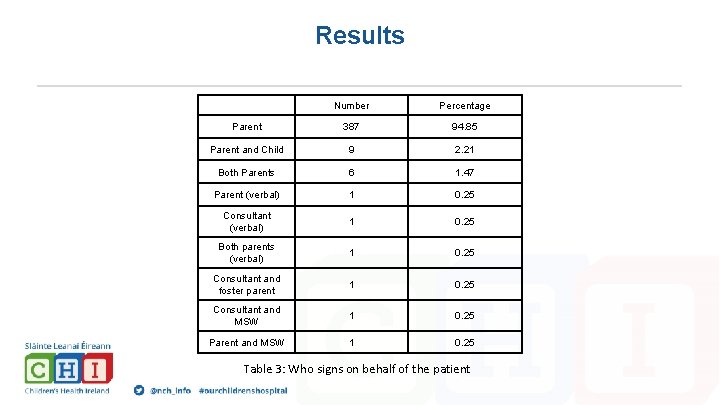
Results Number Percentage Parent 387 94. 85 Parent and Child 9 2. 21 Both Parents 6 1. 47 Parent (verbal) 1 0. 25 Consultant (verbal) 1 0. 25 Both parents (verbal) 1 0. 25 Consultant and foster parent 1 0. 25 Consultant and MSW 1 0. 25 Parent and MSW 1 0. 25 Table 3: Who signs on behalf of the patient
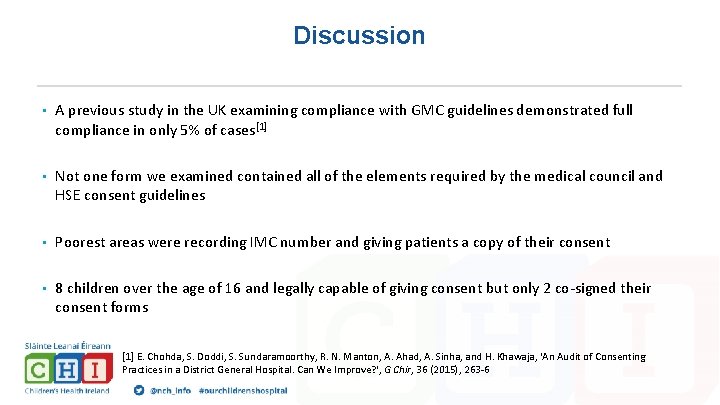
Discussion • A previous study in the UK examining compliance with GMC guidelines demonstrated full compliance in only 5% of cases[1] • Not one form we examined contained all of the elements required by the medical council and HSE consent guidelines • Poorest areas were recording IMC number and giving patients a copy of their consent • 8 children over the age of 16 and legally capable of giving consent but only 2 co-signed their consent forms [1] E. Chohda, S. Doddi, S. Sundaramoorthy, R. N. Manton, A. Ahad, A. Sinha, and H. Khawaja, 'An Audit of Consenting Practices in a District General Hospital. Can We Improve? ', G Chir, 36 (2015), 263 -6
Conclusion • Potential medico-legal ramifications • Provision of education sessions to NCHDs about the processes for obtaining valid informed consent with subsequent re-audit to close the loop • Should we move to a model of signing specific consent forms? • Should anaesthesia have a specific form?

Questions?