A RARE CAUSE OF ESOPHAGEAL DYSPHAGIA SECONDARY ESOPHAGEAL
- Slides: 1
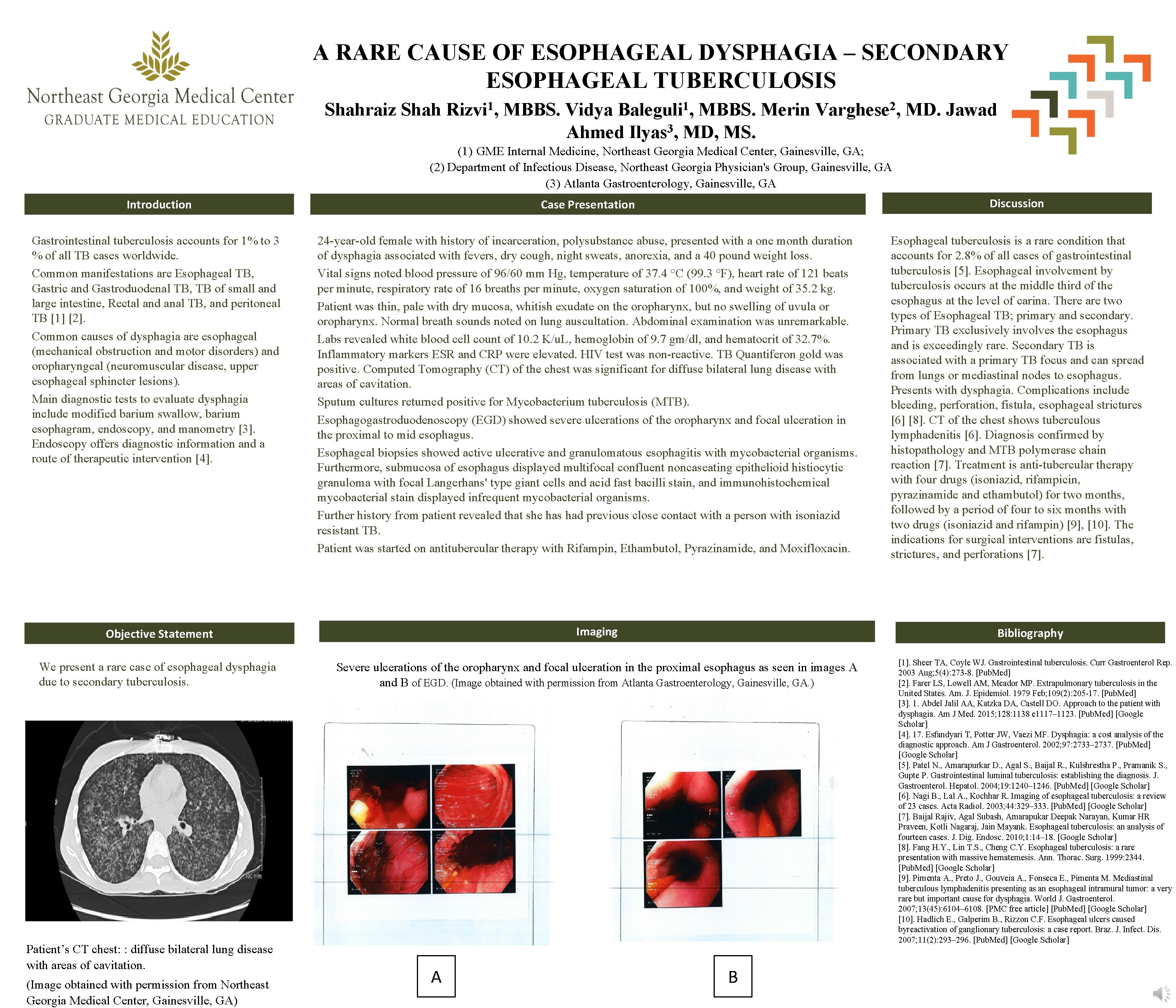
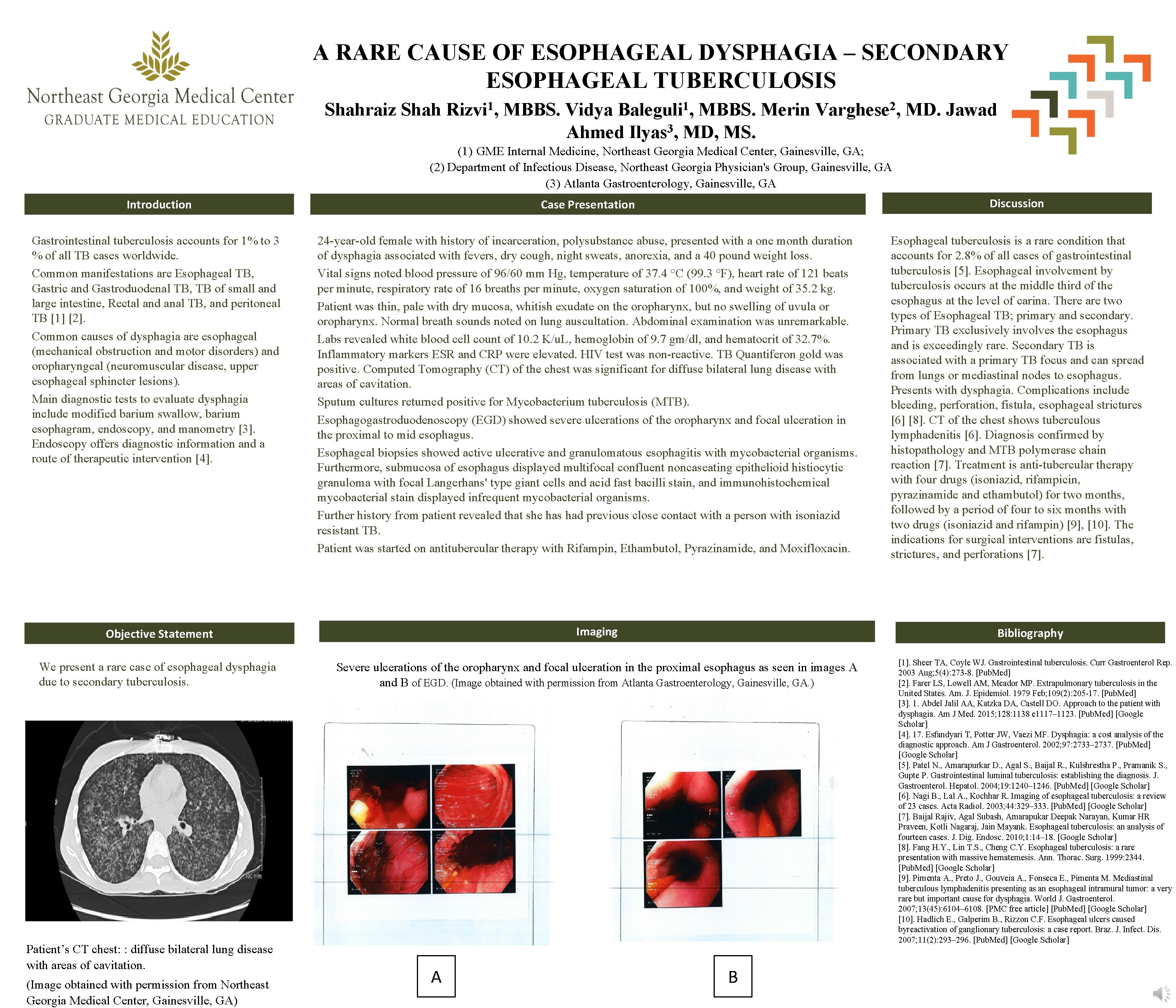
A RARE CAUSE OF ESOPHAGEAL DYSPHAGIA – SECONDARY ESOPHAGEAL TUBERCULOSIS Shahraiz Shah 1 Rizvi , 1 Baleguli , MBBS. Vidya MBBS. Merin Ahmed Ilyas 3, MD, MS. 2 Varghese , MD. Jawad (1) GME Internal Medicine, Northeast Georgia Medical Center, Gainesville, GA; (2) Department of Infectious Disease, Northeast Georgia Physician's Group, Gainesville, GA (3) Atlanta Gastroenterology, Gainesville, GA Introduction Case Presentation Discussion Gastrointestinal tuberculosis accounts for 1% to 3 % of all TB cases worldwide. Common manifestations are Esophageal TB, Gastric and Gastroduodenal TB, TB of small and large intestine, Rectal and anal TB, and peritoneal TB [1] [2]. Common causes of dysphagia are esophageal (mechanical obstruction and motor disorders) and oropharyngeal (neuromuscular disease, upper esophageal sphincter lesions). Main diagnostic tests to evaluate dysphagia include modified barium swallow, barium esophagram, endoscopy, and manometry [3]. Endoscopy offers diagnostic information and a route of therapeutic intervention [4]. 24 -year-old female with history of incarceration, polysubstance abuse, presented with a one month duration of dysphagia associated with fevers, dry cough, night sweats, anorexia, and a 40 pound weight loss. Vital signs noted blood pressure of 96/60 mm Hg, temperature of 37. 4 °C (99. 3 °F), heart rate of 121 beats per minute, respiratory rate of 16 breaths per minute, oxygen saturation of 100%, and weight of 35. 2 kg. Patient was thin, pale with dry mucosa, whitish exudate on the oropharynx, but no swelling of uvula or oropharynx. Normal breath sounds noted on lung auscultation. Abdominal examination was unremarkable. Labs revealed white blood cell count of 10. 2 K/u. L, hemoglobin of 9. 7 gm/dl, and hematocrit of 32. 7%. Inflammatory markers ESR and CRP were elevated. HIV test was non-reactive. TB Quantiferon gold was positive. Computed Tomography (CT) of the chest was significant for diffuse bilateral lung disease with areas of cavitation. Sputum cultures returned positive for Mycobacterium tuberculosis (MTB). Esophagogastroduodenoscopy (EGD) showed severe ulcerations of the oropharynx and focal ulceration in the proximal to mid esophagus. Esophageal biopsies showed active ulcerative and granulomatous esophagitis with mycobacterial organisms. Furthermore, submucosa of esophagus displayed multifocal confluent noncaseating epithelioid histiocytic granuloma with focal Langerhans' type giant cells and acid fast bacilli stain, and immunohistochemical mycobacterial stain displayed infrequent mycobacterial organisms. Further history from patient revealed that she has had previous close contact with a person with isoniazid resistant TB. Patient was started on antitubercular therapy with Rifampin, Ethambutol, Pyrazinamide, and Moxifloxacin. Esophageal tuberculosis is a rare condition that accounts for 2. 8% of all cases of gastrointestinal tuberculosis [5]. Esophageal involvement by tuberculosis occurs at the middle third of the esophagus at the level of carina. There are two types of Esophageal TB; primary and secondary. Primary TB exclusively involves the esophagus and is exceedingly rare. Secondary TB is associated with a primary TB focus and can spread from lungs or mediastinal nodes to esophagus. Presents with dysphagia. Complications include bleeding, perforation, fistula, esophageal strictures [6] [8]. CT of the chest shows tuberculous lymphadenitis [6]. Diagnosis confirmed by histopathology and MTB polymerase chain reaction [7]. Treatment is anti-tubercular therapy with four drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) for two months, followed by a period of four to six months with two drugs (isoniazid and rifampin) [9], [10]. The indications for surgical interventions are fistulas, strictures, and perforations [7]. Imaging Objective Statement We present a rare case of esophageal dysphagia due to secondary tuberculosis. Patient’s CT chest: : diffuse bilateral lung disease with areas of cavitation. (Image obtained with permission from Northeast Georgia Medical Center, Gainesville, GA) Bibliography Severe ulcerations of the oropharynx and focal ulceration in the proximal esophagus as seen in images A and B of EGD. (Image obtained with permission from Atlanta Gastroenterology, Gainesville, GA. ) A B [1]. Sheer TA, Coyle WJ. Gastrointestinal tuberculosis. Curr Gastroenterol Rep. 2003 Aug; 5(4): 273 -8. [Pub. Med] [2]. Farer LS, Lowell AM, Meador MP. Extrapulmonary tuberculosis in the United States. Am. J. Epidemiol. 1979 Feb; 109(2): 205 -17. [Pub. Med] [3]. 1. Abdel Jalil AA, Katzka DA, Castell DO. Approach to the patient with dysphagia. Am J Med. 2015; 128: 1138 e 1117– 1123. [Pub. Med] [Google Scholar] [4]. 17. Esfandyari T, Potter JW, Vaezi MF. Dysphagia: a cost analysis of the diagnostic approach. Am J Gastroenterol. 2002; 97: 2733– 2737. [Pub. Med] [Google Scholar] [5]. Patel N. , Amarapurkar D. , Agal S. , Baijal R. , Kulshrestha P. , Pramanik S. , Gupte P. Gastrointestinal luminal tuberculosis: establishing the diagnosis. J. Gastroenterol. Hepatol. 2004; 19: 1240– 1246. [Pub. Med] [Google Scholar] [6]. Nagi B. , Lal A. , Kochhar R. Imaging of esophageal tuberculosis: a review of 23 cases. Acta Radiol. 2003; 44: 329– 333. [Pub. Med] [Google Scholar] [7]. Baijal Rajiv, Agal Subash, Amarapukar Deepak Narayan, Kumar HR Praveen, Kotli Nagaraj, Jain Mayank. Esophageal tuberculosis: an analysis of fourteen cases. J. Dig. Endosc. 2010; 1: 14– 18. [Google Scholar] [8]. Fang H. Y. , Lin T. S. , Cheng C. Y. Esophageal tuberculosis: a rare presentation with massive hematemesis. Ann. Thorac. Surg. 1999: 2344. [Pub. Med] [Google Scholar] [9]. Pimenta A. , Preto J. , Gouveia A. , Fonseca E. , Pimenta M. Mediastinal tuberculous lymphadenitis presenting as an esophageal intramural tumor: a very rare but important cause for dysphagia. World J. Gastroenterol. 2007; 13(45): 6104– 6108. [PMC free article] [Pub. Med] [Google Scholar] [10]. Hadlich E. , Galperim B. , Rizzon C. F. Esophageal ulcers caused byreactivation of ganglionary tuberculosis: a case report. Braz. J. Infect. Dis. 2007; 11(2): 293– 296. [Pub. Med] [Google Scholar]