A Protocol for the Treatment of Chronic Ankle
- Slides: 1
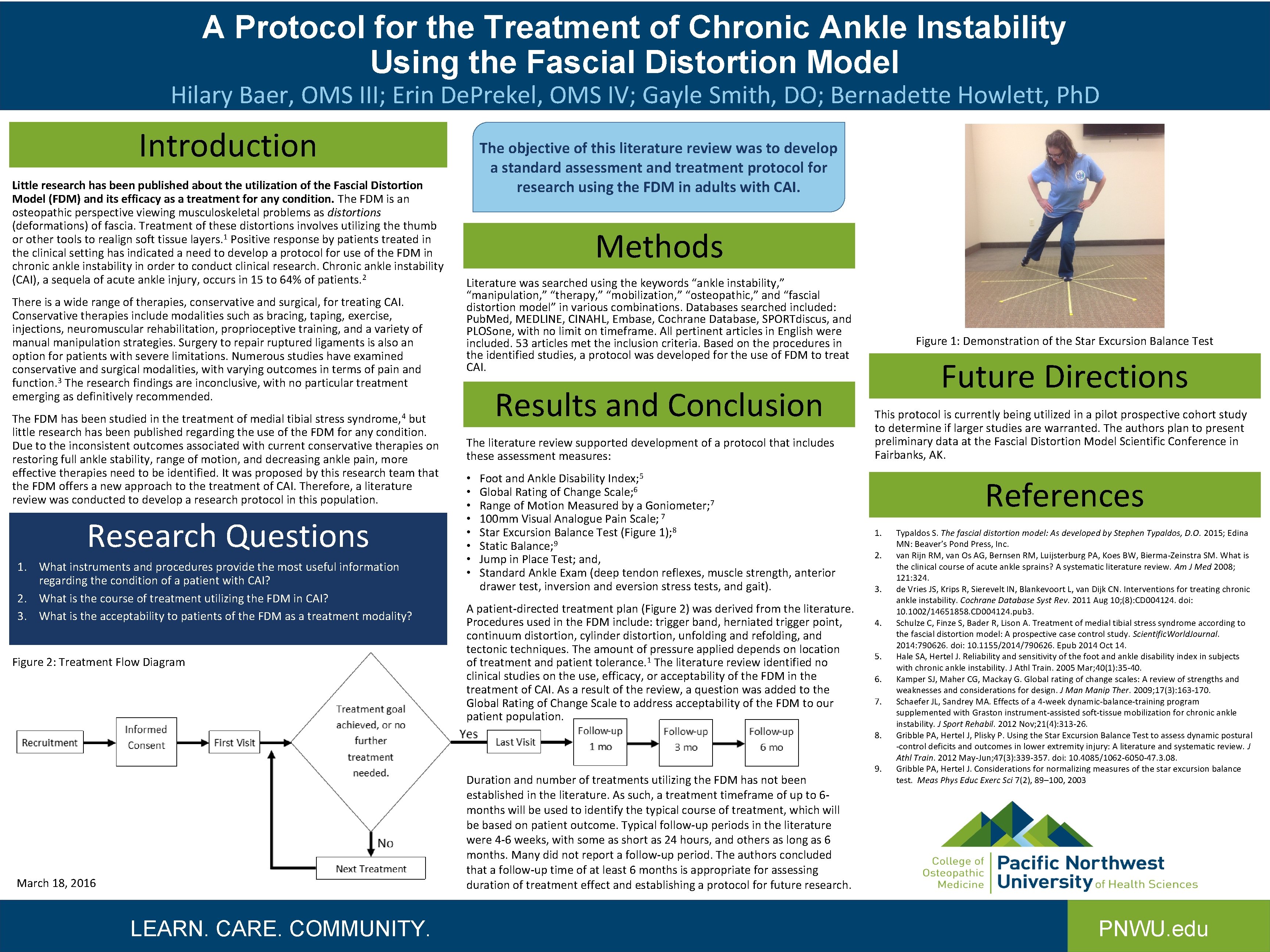
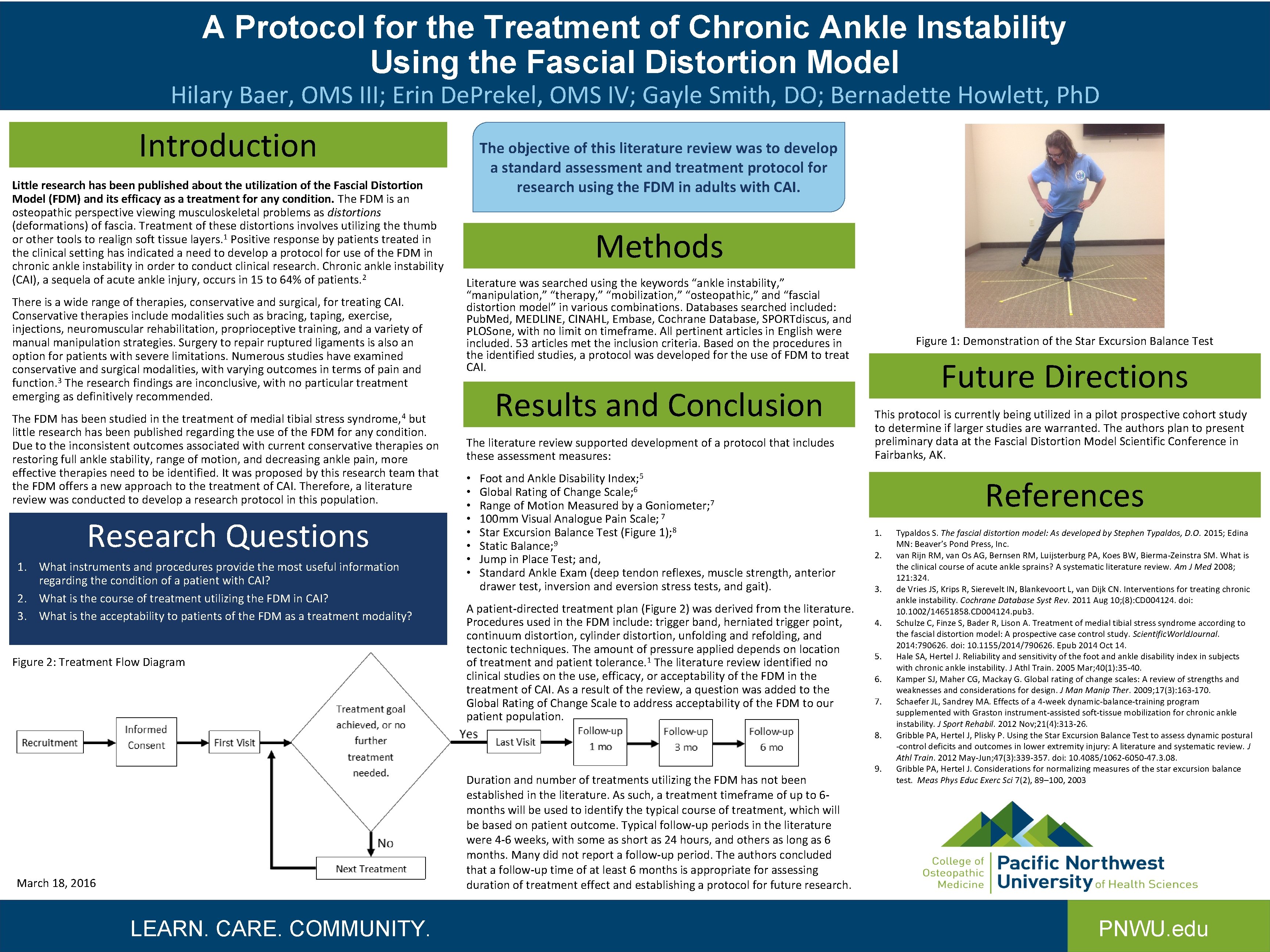
A Protocol for the Treatment of Chronic Ankle Instability Using the Fascial Distortion Model Hilary Baer, OMS III; Erin De. Prekel, OMS IV; Gayle Smith, DO; Bernadette Howlett, Ph. D Introduction Little research has been published about the utilization of the Fascial Distortion Model (FDM) and its efficacy as a treatment for any condition. The FDM is an osteopathic perspective viewing musculoskeletal problems as distortions (deformations) of fascia. Treatment of these distortions involves utilizing the thumb or other tools to realign soft tissue layers. 1 Positive response by patients treated in the clinical setting has indicated a need to develop a protocol for use of the FDM in chronic ankle instability in order to conduct clinical research. Chronic ankle instability (CAI), a sequela of acute ankle injury, occurs in 15 to 64% of patients. 2 There is a wide range of therapies, conservative and surgical, for treating CAI. Conservative therapies include modalities such as bracing, taping, exercise, injections, neuromuscular rehabilitation, proprioceptive training, and a variety of manual manipulation strategies. Surgery to repair ruptured ligaments is also an option for patients with severe limitations. Numerous studies have examined conservative and surgical modalities, with varying outcomes in terms of pain and function. 3 The research findings are inconclusive, with no particular treatment emerging as definitively recommended. The FDM has been studied in the treatment of medial tibial stress but little research has been published regarding the use of the FDM for any condition. Due to the inconsistent outcomes associated with current conservative therapies on restoring full ankle stability, range of motion, and decreasing ankle pain, more effective therapies need to be identified. It was proposed by this research team that the FDM offers a new approach to the treatment of CAI. Therefore, a literature review was conducted to develop a research protocol in this population. The objective of this literature review was to develop a standard assessment and treatment protocol for research using the FDM in adults with CAI. Methods Literature was searched using the keywords “ankle instability, ” “manipulation, ” “therapy, ” “mobilization, ” “osteopathic, ” and “fascial distortion model” in various combinations. Databases searched included: Pub. Med, MEDLINE, CINAHL, Embase, Cochrane Database, SPORTdiscus, and PLOSone, with no limit on timeframe. All pertinent articles in English were included. 53 articles met the inclusion criteria. Based on the procedures in the identified studies, a protocol was developed for the use of FDM to treat CAI. Results and Conclusion syndrome, 4 Research Questions 1. What instruments and procedures provide the most useful information regarding the condition of a patient with CAI? 2. What is the course of treatment utilizing the FDM in CAI? 3. What is the acceptability to patients of the FDM as a treatment modality? Figure 2: Treatment Flow Diagram The literature review supported development of a protocol that includes these assessment measures: • • Foot and Ankle Disability Index; 5 Global Rating of Change Scale; 6 Range of Motion Measured by a Goniometer; 7 100 mm Visual Analogue Pain Scale; 7 Star Excursion Balance Test (Figure 1); 8 Static Balance; 9 Jump in Place Test; and, Standard Ankle Exam (deep tendon reflexes, muscle strength, anterior drawer test, inversion and eversion stress tests, and gait). A patient-directed treatment plan (Figure 2) was derived from the literature. Procedures used in the FDM include: trigger band, herniated trigger point, continuum distortion, cylinder distortion, unfolding and refolding, and tectonic techniques. The amount of pressure applied depends on location of treatment and patient tolerance. 1 The literature review identified no clinical studies on the use, efficacy, or acceptability of the FDM in the treatment of CAI. As a result of the review, a question was added to the Global Rating of Change Scale to address acceptability of the FDM to our patient population. Figure 1: Demonstration of the Star Excursion Balance Test Future Directions This protocol is currently being utilized in a pilot prospective cohort study to determine if larger studies are warranted. The authors plan to present preliminary data at the Fascial Distortion Model Scientific Conference in Fairbanks, AK. References 1. 2. 3. 4. 5. 6. 7. 8. Duration and number of treatments utilizing the FDM has not been established in the literature. As such, a treatment timeframe of up to 6 months will be used to identify the typical course of treatment, which will be based on patient outcome. Typical follow-up periods in the literature were 4 -6 weeks, with some as short as 24 hours, and others as long as 6 months. Many did not report a follow-up period. The authors concluded that a follow-up time of at least 6 months is appropriate for assessing duration of treatment effect and establishing a protocol for future research. March 18, 2016 LEARN. CARE. COMMUNITY. 9. Typaldos S. The fascial distortion model: As developed by Stephen Typaldos, D. O. 2015; Edina MN: Beaver’s Pond Press, Inc. van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med 2008; 121: 324. de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011 Aug 10; (8): CD 004124. doi: 10. 1002/14651858. CD 004124. pub 3. Schulze C, Finze S, Bader R, Lison A. Treatment of medial tibial stress syndrome according to the fascial distortion model: A prospective case control study. Scientific. World. Journal. 2014: 790626. doi: 10. 1155/2014/790626. Epub 2014 Oct 14. Hale SA, Hertel J. Reliability and sensitivity of the foot and ankle disability index in subjects with chronic ankle instability. J Athl Train. 2005 Mar; 40(1): 35 -40. Kamper SJ, Maher CG, Mackay G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J Manip Ther. 2009; 17(3): 163 -170. Schaefer JL, Sandrey MA. Effects of a 4 -week dynamic-balance-training program supplemented with Graston instrument-assisted soft-tissue mobilization for chronic ankle instability. J Sport Rehabil. 2012 Nov; 21(4): 313 -26. Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural -control deficits and outcomes in lower extremity injury: A literature and systematic review. J Athl Train. 2012 May-Jun; 47(3): 339 -357. doi: 10. 4085/1062 -6050 -47. 3. 08. Gribble PA, Hertel J. Considerations for normalizing measures of the star excursion balance test. Meas Phys Educ Exerc Sci 7(2), 89– 100, 2003 PNWU. edu