A Practical Guide for the NHS Benefits Driven
A Practical Guide for the NHS Benefits Driven Change Using some examples from the ISIP Demonstrator Programme, this guide shows how a benefits approach to change can be used to deliver sustainable service transformation more quickly. It also helps the care community, including external partnerships, to be more flexible in responding to changing circumstances.
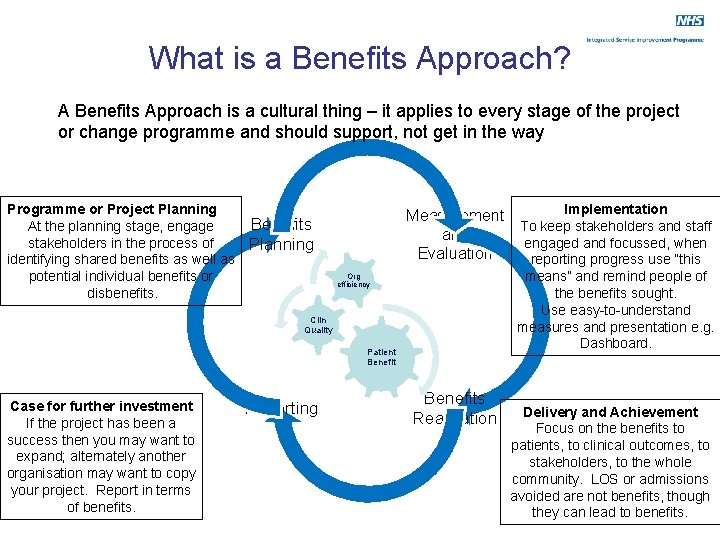
What is a Benefits Approach? A Benefits Approach is a cultural thing – it applies to every stage of the project or change programme and should support, not get in the way Programme or Project Planning At the planning stage, engage stakeholders in the process of identifying shared benefits as well as potential individual benefits or disbenefits. Measurement and Evaluation Benefits Planning Org efficiency Clin Quality Patient Benefit Case for further investment If the project has been a success then you may want to expand; alternately another organisation may want to copy your project. Report in terms of benefits. Reporting Benefits Realisation Implementation To keep stakeholders and staff engaged and focussed, when reporting progress use “this means” and remind people of the benefits sought. Use easy-to-understand measures and presentation e. g. Dashboard. Delivery and Achievement Focus on the benefits to patients, to clinical outcomes, to stakeholders, to the whole community. LOS or admissions avoided are not benefits, though they can lead to benefits.
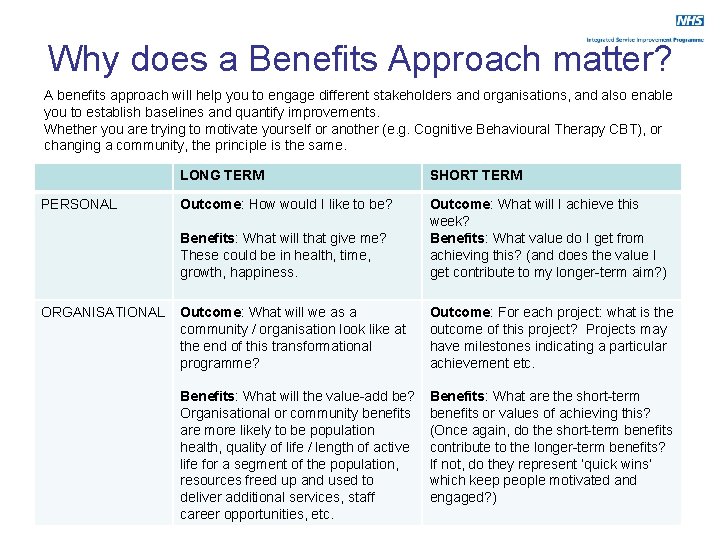
Why does a Benefits Approach matter? A benefits approach will help you to engage different stakeholders and organisations, and also enable you to establish baselines and quantify improvements. Whether you are trying to motivate yourself or another (e. g. Cognitive Behavioural Therapy CBT), or changing a community, the principle is the same. PERSONAL ORGANISATIONAL LONG TERM SHORT TERM Outcome: How would I like to be? Benefits: What will that give me? These could be in health, time, growth, happiness. Outcome: What will I achieve this week? Benefits: What value do I get from achieving this? (and does the value I get contribute to my longer-term aim? ) Outcome: What will we as a community / organisation look like at the end of this transformational programme? Outcome: For each project: what is the outcome of this project? Projects may have milestones indicating a particular achievement etc. Benefits: What will the value-add be? Organisational or community benefits are more likely to be population health, quality of life / length of active life for a segment of the population, resources freed up and used to deliver additional services, staff career opportunities, etc. Benefits: What are the short-term benefits or values of achieving this? (Once again, do the short-term benefits contribute to the longer-term benefits? If not, do they represent ‘quick wins’ which keep people motivated and engaged? )

Stakeholder Benefits Stakeholder 2 Stakeholder 1 Priority Objective Benefit Outcomes Projects, Actions to Change Progress isn’t always direct, but it should always be progress Stakeholder 3 Stakeholder 4 See also NHS ISIP Practical Guide on Stakeholder Engagement Priority Objectives are national or local targets e. g. “reducing inequalities” Benefits may be stakeholder-specific or shared, and are the motivating force Outcomes represent the future state of the service, what it has to be like to deliver the benefits Projects and Actions to Change are what you do to achieve the outcomes New Economics Foundation – Measuring real value: A DIY guide to Social Return on Investment
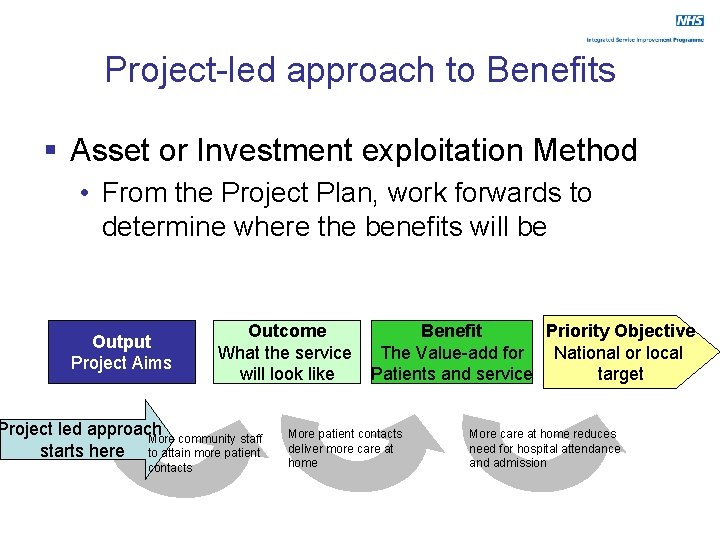
Project-led approach to Benefits § Asset or Investment exploitation Method • From the Project Plan, work forwards to determine where the benefits will be Output Project Aims Outcome What the service will look like Project led approach More community staff starts here to attain more patient contacts Priority Objective Benefit National or local The Value-add for target Patients and service More patient contacts deliver more care at home More care at home reduces need for hospital attendance and admission
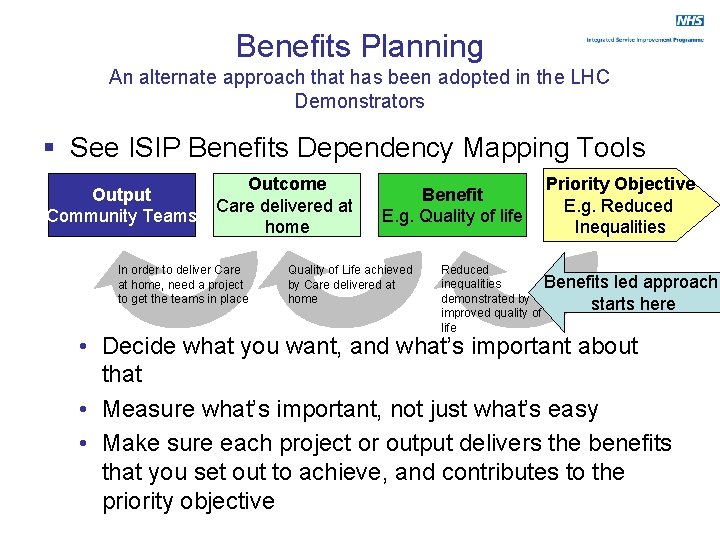
Benefits Planning An alternate approach that has been adopted in the LHC Demonstrators § See ISIP Benefits Dependency Mapping Tools Output Community Teams Outcome Care delivered at home In order to deliver Care at home, need a project to get the teams in place Benefit E. g. Quality of life Quality of Life achieved by Care delivered at home Priority Objective E. g. Reduced Inequalities Reduced inequalities Benefits led approach demonstrated by starts here improved quality of life • Decide what you want, and what’s important about that • Measure what’s important, not just what’s easy • Make sure each project or output delivers the benefits that you set out to achieve, and contributes to the priority objective
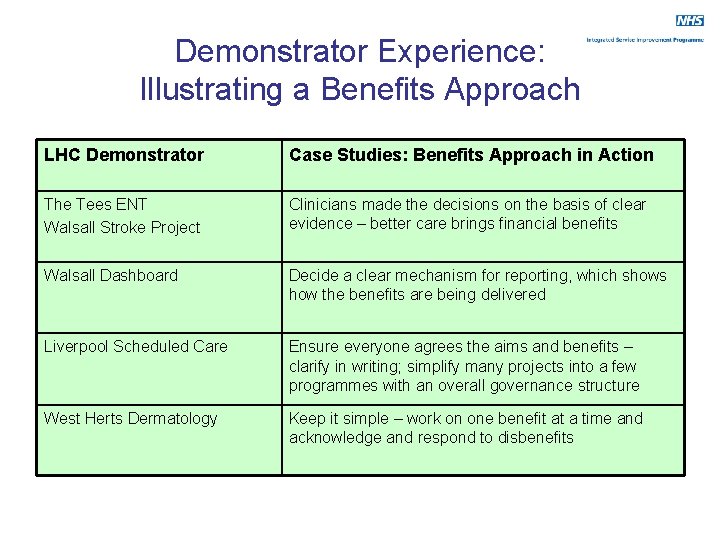
Demonstrator Experience: Illustrating a Benefits Approach LHC Demonstrator Case Studies: Benefits Approach in Action The Tees ENT Walsall Stroke Project Clinicians made the decisions on the basis of clear evidence – better care brings financial benefits Walsall Dashboard Decide a clear mechanism for reporting, which shows how the benefits are being delivered Liverpool Scheduled Care Ensure everyone agrees the aims and benefits – clarify in writing; simplify many projects into a few programmes with an overall governance structure West Herts Dermatology Keep it simple – work on one benefit at a time and acknowledge and respond to disbenefits
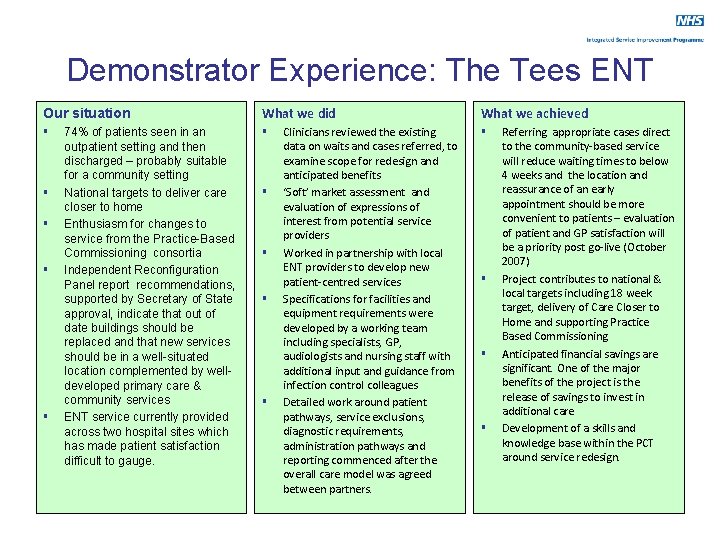
Demonstrator Experience: The Tees ENT Our situation What we did § § § 74% of patients seen in an outpatient setting and then discharged – probably suitable for a community setting National targets to deliver care closer to home Enthusiasm for changes to service from the Practice-Based Commissioning consortia Independent Reconfiguration Panel report recommendations, supported by Secretary of State approval, indicate that out of date buildings should be replaced and that new services should be in a well-situated location complemented by welldeveloped primary care & community services ENT service currently provided across two hospital sites which has made patient satisfaction difficult to gauge. § § Clinicians reviewed the existing data on waits and cases referred, to examine scope for redesign and anticipated benefits ‘Soft’ market assessment and evaluation of expressions of interest from potential service providers Worked in partnership with local ENT providers to develop new patient-centred services Specifications for facilities and equipment requirements were developed by a working team including specialists, GP, audiologists and nursing staff with additional input and guidance from infection control colleagues Detailed work around patient pathways, service exclusions, diagnostic requirements, administration pathways and reporting commenced after the overall care model was agreed between partners. What we achieved § § Referring appropriate cases direct to the community-based service will reduce waiting times to below 4 weeks and the location and reassurance of an early appointment should be more convenient to patients – evaluation of patient and GP satisfaction will be a priority post go-live (October 2007) Project contributes to national & local targets including 18 week target, delivery of Care Closer to Home and supporting Practice Based Commissioning Anticipated financial savings are significant. One of the major benefits of the project is the release of savings to invest in additional care Development of a skills and knowledge base within the PCT around service redesign.
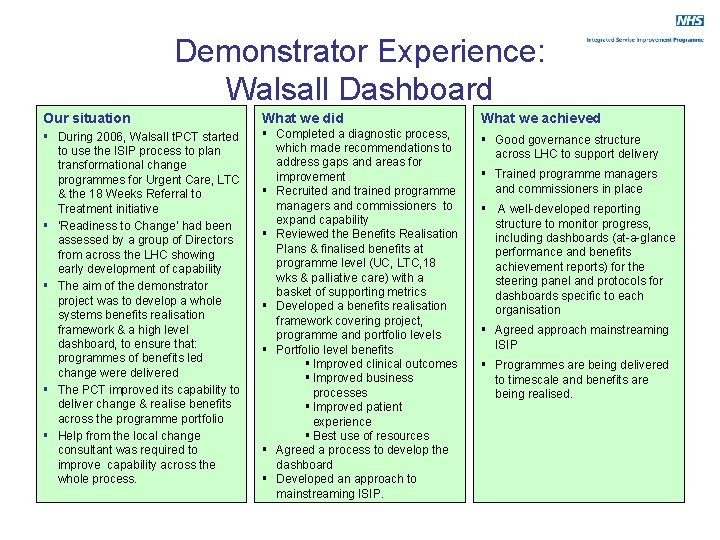
Demonstrator Experience: Walsall Dashboard Our situation What we did What we achieved § During 2006, Walsall t. PCT started to use the ISIP process to plan transformational change programmes for Urgent Care, LTC & the 18 Weeks Referral to Treatment initiative § ‘Readiness to Change’ had been assessed by a group of Directors from across the LHC showing early development of capability § The aim of the demonstrator project was to develop a whole systems benefits realisation framework & a high level dashboard, to ensure that: programmes of benefits led change were delivered § The PCT improved its capability to deliver change & realise benefits across the programme portfolio § Help from the local change consultant was required to improve capability across the whole process. § Completed a diagnostic process, which made recommendations to address gaps and areas for improvement § Recruited and trained programme managers and commissioners to expand capability § Reviewed the Benefits Realisation Plans & finalised benefits at programme level (UC, LTC, 18 wks & palliative care) with a basket of supporting metrics § Developed a benefits realisation framework covering project, programme and portfolio levels § Portfolio level benefits § Improved clinical outcomes § Improved business processes § Improved patient experience § Best use of resources § Agreed a process to develop the dashboard § Developed an approach to mainstreaming ISIP. § Good governance structure across LHC to support delivery § Trained programme managers and commissioners in place § A well-developed reporting structure to monitor progress, including dashboards (at-a-glance performance and benefits achievement reports) for the steering panel and protocols for dashboards specific to each organisation § Agreed approach mainstreaming ISIP § Programmes are being delivered to timescale and benefits are being realised.
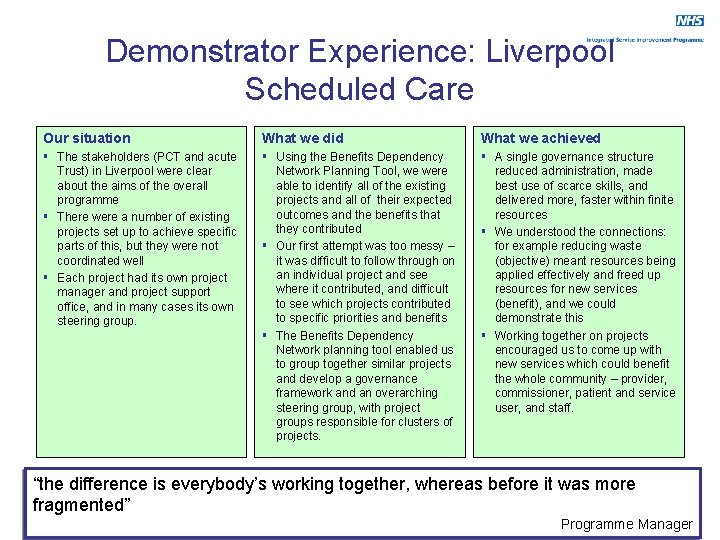
Demonstrator Experience: Liverpool Scheduled Care Our situation What we did What we achieved § The stakeholders (PCT and acute Trust) in Liverpool were clear about the aims of the overall programme § There were a number of existing projects set up to achieve specific parts of this, but they were not coordinated well § Each project had its own project manager and project support office, and in many cases its own steering group. § Using the Benefits Dependency Network Planning Tool, we were able to identify all of the existing projects and all of their expected outcomes and the benefits that they contributed § Our first attempt was too messy – it was difficult to follow through on an individual project and see where it contributed, and difficult to see which projects contributed to specific priorities and benefits § The Benefits Dependency Network planning tool enabled us to group together similar projects and develop a governance framework and an overarching steering group, with project groups responsible for clusters of projects. § A single governance structure reduced administration, made best use of scarce skills, and delivered more, faster within finite resources § We understood the connections: for example reducing waste (objective) meant resources being applied effectively and freed up resources for new services (benefit), and we could demonstrate this § Working together on projects encouraged us to come up with new services which could benefit the whole community – provider, commissioner, patient and service user, and staff. “the difference is everybody’s working together, whereas before it was more fragmented” Programme Manager
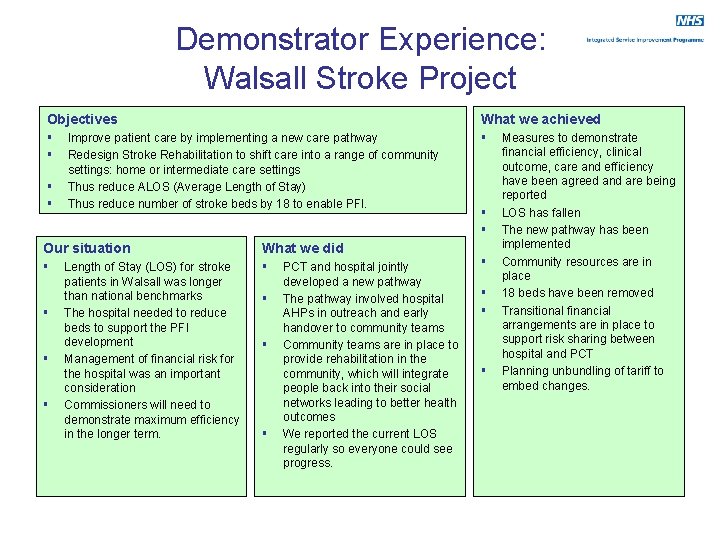
Demonstrator Experience: Walsall Stroke Project Objectives What we achieved § § § Improve patient care by implementing a new care pathway Redesign Stroke Rehabilitation to shift care into a range of community settings: home or intermediate care settings Thus reduce ALOS (Average Length of Stay) Thus reduce number of stroke beds by 18 to enable PFI. Our situation What we did § § § Length of Stay (LOS) for stroke patients in Walsall was longer than national benchmarks The hospital needed to reduce beds to support the PFI development Management of financial risk for the hospital was an important consideration Commissioners will need to demonstrate maximum efficiency in the longer term. § § § PCT and hospital jointly developed a new pathway The pathway involved hospital AHPs in outreach and early handover to community teams Community teams are in place to provide rehabilitation in the community, which will integrate people back into their social networks leading to better health outcomes We reported the current LOS regularly so everyone could see progress. § § § Measures to demonstrate financial efficiency, clinical outcome, care and efficiency have been agreed and are being reported LOS has fallen The new pathway has been implemented Community resources are in place 18 beds have been removed Transitional financial arrangements are in place to support risk sharing between hospital and PCT Planning unbundling of tariff to embed changes.
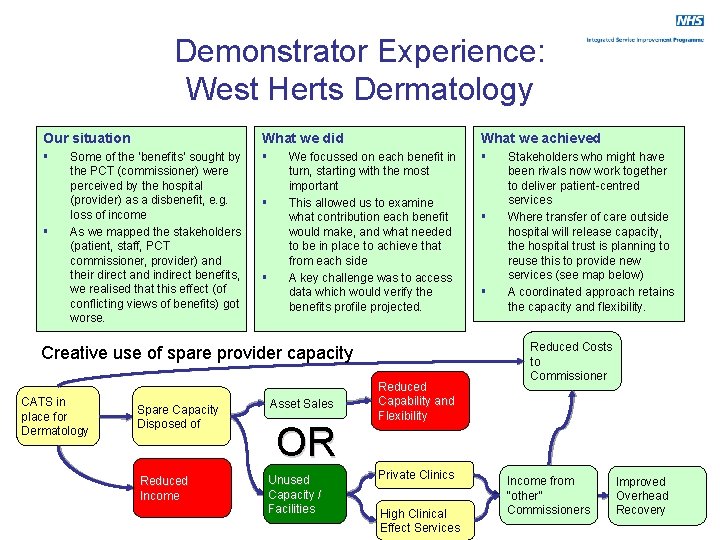
Demonstrator Experience: West Herts Dermatology Our situation What we did What we achieved § § Some of the ‘benefits’ sought by the PCT (commissioner) were perceived by the hospital (provider) as a disbenefit, e. g. loss of income As we mapped the stakeholders (patient, staff, PCT commissioner, provider) and their direct and indirect benefits, we realised that this effect (of conflicting views of benefits) got worse. § § We focussed on each benefit in turn, starting with the most important This allowed us to examine what contribution each benefit would make, and what needed to be in place to achieve that from each side A key challenge was to access data which would verify the benefits profile projected. Creative use of spare provider capacity CATS in place for Dermatology Spare Capacity Disposed of Asset Sales Reduced Income Unused Capacity / Facilities OR Reduced Capability and Flexibility Private Clinics High Clinical Effect Services § § Stakeholders who might have been rivals now work together to deliver patient-centred services Where transfer of care outside hospital will release capacity, the hospital trust is planning to reuse this to provide new services (see map below) A coordinated approach retains the capacity and flexibility. Reduced Costs to Commissioner Income from “other” Commissioners Improved Overhead Recovery
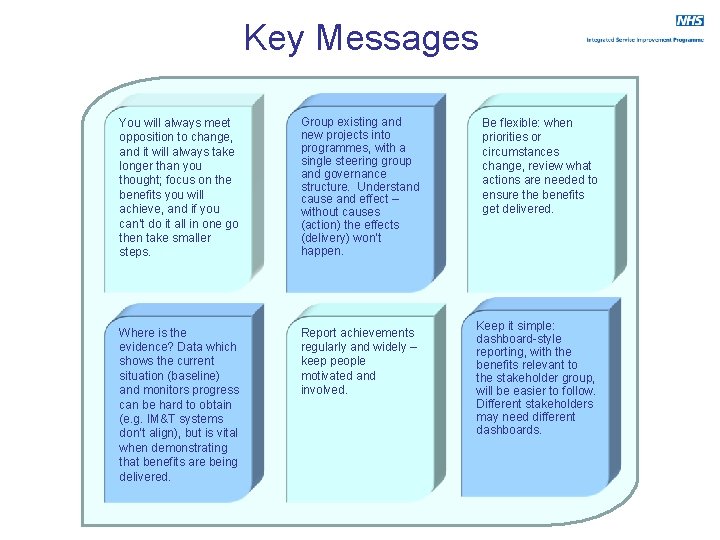
Key Messages You will always meet opposition to change, and it will always take longer than you thought; focus on the benefits you will achieve, and if you can’t do it all in one go then take smaller steps. Group existing and new projects into programmes, with a single steering group and governance structure. Understand cause and effect – without causes (action) the effects (delivery) won’t happen. Where is the evidence? Data which shows the current situation (baseline) and monitors progress can be hard to obtain (e. g. IM&T systems don’t align), but is vital when demonstrating that benefits are being delivered. Report achievements regularly and widely – keep people motivated and involved. Be flexible: when priorities or circumstances change, review what actions are needed to ensure the benefits get delivered. Keep it simple: dashboard-style reporting, with the benefits relevant to the stakeholder group, will be easier to follow. Different stakeholders may need different dashboards.
Where to go for more information External references: Delivering Quality and Value: ISIP Guide: http: //www. isip. nhs. uk/guidance ISIP Practical Guide: Developing a Shared Vision: http: //www. isip. nhs. uk ISIP Practical Guide: Stakeholder Engagement: : http: //www. isip. nhs. uk RTC Stage I Benefits Planning: http: //www. isip. nhs. uk/roadmap Measuring real value: A DIY guide to Social Return on Investment (New Economics Foundation): http: //www. neweconomics. org/gen/z_sys_Publication. Detail. aspx? pid=241 Named contacts: Leonie Beavers, Director of Strategy / SRO, Liverpool PCT, leonie. beavers@liverpoolpct. nhs. uk Nicola Allen, Head of Planned Care Commissioning / Programme Manager, Liverpool PCT, nicola. allen@liverpoolpct. nhs. uk Andrea Bigmore, Head of Change Programmes, Walsall t. PCT, andrea. bigmore@walsall. nhs. uk Julia Schofield, Consultant Dermatologist, West Herts Healthcare Trust, julia. schofield@whht. nhs. uk Amanda Yeates, Project Manager, West Herts Healthcare Trust, amanda. yeates@whht. nhs. uk Phil Whitfield, Associate Director of Planning and Performance, Hartlepool PCT, philip. whitfield@hartlepoolpct. nhs. uk
- Slides: 14