A Path to Successful Pathway Development Pediatric Hospital

















![Practice can change! • Ralston et al [J Hosp Med 2013]: – Reduced unnecessary Practice can change! • Ralston et al [J Hosp Med 2013]: – Reduced unnecessary](https://slidetodoc.com/presentation_image_h2/666cde3ec3672d9dacebadd372688c97/image-21.jpg)












- Slides: 34

A Path to Successful Pathway Development Pediatric Hospital Medicine Annual Conference Chicago, 2016
Disclosures • We have no relevant financial relationships with the manufacturers(s) of any commercial products(s) and/or provider of commercial services discussed in this CME activity • We do not intend to discuss an unapproved/investigative use of a commercial product/device in my presentation
Objectives 1. Define clinical pathway and review literature supporting their effectiveness 2. Demonstrate the utilization of pathways as a means to transition from volume to value 3. Outline 8 steps to pathway development and implementation 4. Discuss expansion of pathways beyond the inpatient setting 5. Small and large group discussion with attention to barriers, pitfalls, lessons learned and success stories for each step of pathway development

Agenda 1. Welcome, Introductions – 10 minutes 2. Definitions and evidence behind pathways – 5 minutes 3. Clinical effectiveness and pathways as a value proposition – 10 minutes 4. Pathway process and implementation – 15 minutes 5. Expanding pathways beyond the inpatient setting – 5 minutes 6. Small group discussion – 15 minutes 7. Large group discussion – 10 minutes 8. Wrap-up and lessons learned – 5 minutes

Introductions • • Ilana Waynik Anand Sekaran Ryan Bode Richard Engel

What is a Clinical Pathway? A clinical pathway is a structured, multidisciplinary plan which details steps in the care of patients with a specific condition. The goal of a clinical pathway is to standardize best practice, improve outcomes and reduce cost.

Related Terms • • Care Path Flow Map Clinical practice guideline Protocol Algorithm Order set Evidence based practice

Which diagnoses are ripe for a Clinical Pathway? • • • High volume High risk (even if low volume) High cost Strong evidence base High variation in practice Traverses different settings
Predictors for Pathway Success • • • Picking the right condition Local adaptation and buy-in (+ local champion!) Multi-disciplinary involvement from the start Ongoing evaluation of the pathway Real-time tracking of outcomes Sharing data in real time with end users

Literature on Pathway Outcomes • Cochrane review (2010): Clinical pathways have been shown to improve clinical outcomes 27 studies (11, 398 participants) • Clinical pathways reduce in-hospital complications and improve documentation (strength of recommendation=A) • Clinical pathways resulted in decreased LOS and reduced costs in some, but not all, studies (strength of recommendation=B)

The Evidence for Pathways Pediatric Asthma: Hsu DP et al, 2013: Pediatric asthma care pathway shortens average LOS from 61 hours to 46 hours, increased education from 48% to 89% Cunningham et al, 2007: pediatric asthma--30% reduction in prescribing errors, increase in systemic steroid use in ED, increase in education. Fever in young infants: Byington CL et al, 2012: 8, 044 febrile infants in Utah, EB-CPM, showed reduced mean LOS and costs (1. 9 M in 5 years)


Clinical Effectiveness • Value = Quality (outcome)/Cost

Waste in US Healthcare Berwick, D. M. et al. JAMA doi: 10. 1001/jama. 2012. 362

Quality Metrics – underuse improving, overuse is not Kale MS, JAMA Int Med 2013

Pediatric Overuse and Overdiagnosis • Magnesium levels – 14% of hospitalized non-ICU pediatric patients – $20 million in charges/year – <4% with an intervention • 84% within 4 disease states • HSV testing in neonatal fever Narayanan et al, Hospital Pediatrics, 2014 Gaensbauer J T et al. Pediatrics 2014; 134: e 651 -e 656

Vehicles to Value • • • Care delivery models Reimbursement models Measurement Choosing Wisely Comparative Effectiveness Research Clinical Pathways

Choosing Wisely Society of Hospital Medicine - Pediatrics 1. Don’t order chest radiographs in children with uncomplicated asthma or bronchiolitis. 2. Don’t routinely use bronchodilators in children with bronchiolitis 3. Don’t use systemic corticosteroids in children under 2 years of age with an uncomplicated lower respiratory tract infection. 4. Don’t treat gastroesophageal reflux in infants routinely with acid suppression therapy. 5. Don’t use continuous pulse oximetry routinely in children with acute respiratory illness unless they are on supplemental oxygen.

Practice Variability - Osteomyelitis Zaoutis, Pediatrics, 2009

Proportion of infants <6 months of age who received ≥ 4 days of intravenous antibiotic therapy Patrick W. Brady et al. Pediatrics 2010; 126: 196 -203 © 2010 by American Academy of Pediatrics
![Practice can change Ralston et al J Hosp Med 2013 Reduced unnecessary Practice can change! • Ralston et al [J Hosp Med 2013]: – Reduced unnecessary](https://slidetodoc.com/presentation_image_h2/666cde3ec3672d9dacebadd372688c97/image-21.jpg)
Practice can change! • Ralston et al [J Hosp Med 2013]: – Reduced unnecessary therapies in bronchiolitis (17 centers) • Schroeder et al [Arch Ped Adol Med 2011]: – Reduced VCUG utilization after UTI • Decrease in CT scan use – mild head trauma, appendicitis, kidney stones

Expansion of Hospital Pathways • Outcomes - resource utilization, readmissions, prevention strategies • ED, skilled nursing facility, ambulatory, network • Hospital committees – utilization review, antibiotic stewardship, pharmacy and therapeutics
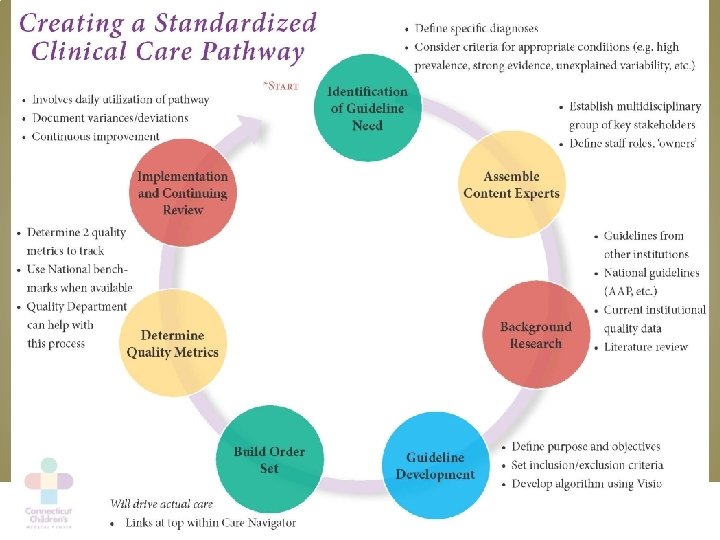

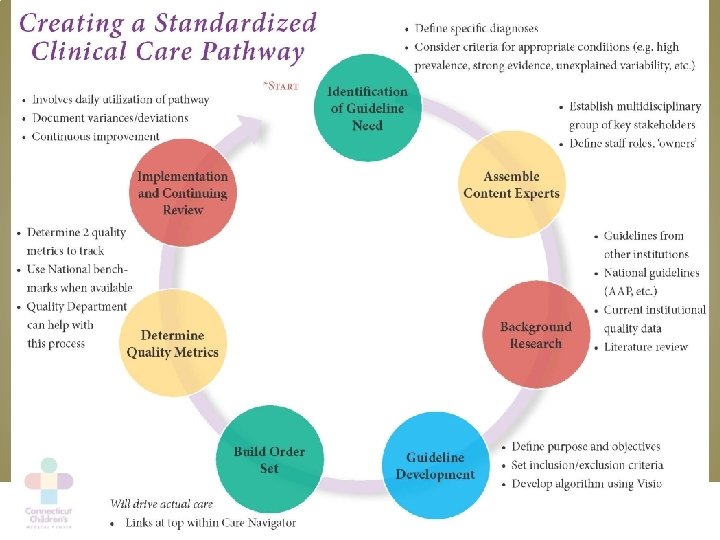
Step 1: Identify Pathway Need • Define specific diagnoses – National guidelines – Other institutions – Criteria for appropriate diagnoses • • • High prevalence Strong evidence based care Unexplained variability of care within your institution Poor outcomes Antibiotic stewardship

Step 2: Assemble Content Experts • • Multidisciplinary group Content experts/consultants Include key stakeholders Define roles, including “pathway owners”

Step 3: Perform Background Research • • • National guidelines Guidelines from other institutions National AND institutional quality data Chart review Literature review

Step 4: Develop Pathway Content • Define pathway objectives • Inclusion and exclusion criteria • Develop algorithm – Visio or other flow diagram – Keep to 1 -2 pages – Easy to follow • Discuss format (e. g. include references, resp assessment tools, etc. ) • Feasible w/in your institution

Step 5: Create Order Set • Will drive actual care – Precheck orders – Intentional omission of tests and therapies • Can monitor pathway usage • Use features of your EHR – i. e. Epic can link to the algorithm and key references

Step 6: Create Education Plan • Define pathway end-users • Determine mode of education delivery – Face-to-face meetings – Email – Formal didactic (either in person or electronic)

Step 7: Determine Quality Metrics • Define at least 2 quality metrics to track – Look back to pathway objectives • Use national benchmarks when available • Set targets for metrics • Use your institution’s quality department

Step 8: Implement Pathway • Identify resources • Obtain support • Introduce the pathway – Email, meetings, education plan • Anticipate barriers • Ongoing quality review is vital! – Document variances from pathway for review – Consider sharing quality metrics regularly w/end-users – Process for scheduled review and revision of pathway

It’s not just about you… • Think outside of your silo • Look to implement pathways outside of just your clinical area – Combine with ED, Out-Patient, Outside Care Network, etc. • Collaborate with other institutions – Why should we all re-invent the wheel?

National Collaborative Networks • PHIS • Qu. IIN – VIP Network • Stewardship in Improving Bronchiolitis (SIB) • Quality Improvement for the Management of Children Hospitalized with Urinary Tract Infection (Q-UTI) • Improving Community-Acquired Pneumonia Management Quality Improvement Project (ICAP) • A Quality Collaborative for Improving Hospitalist Compliance with the AAP Bronchiolitis Guideline (B-QIP)

Take Home Points: • Pathway development takes planning • Define clear pathway objectives at the beginning • Don’t reinvent the wheel • Collaboration is key • Plan for regular review of quality metrics • Plan for regular review/revision of pathway • Challenge your pathways to expand beyond the hospital