A Model for Community Mental Health Care in


- Slides: 24
A Model for Community Mental Health Care in Latin America The Austral Institute in Neuquén, Argentina Shannon Herndon; Lauren Ellis; Bradley Gaynes, MD MPH University of North Carolina, Chapel Hill, NC 8/16/2018 OIA Global Health Forum
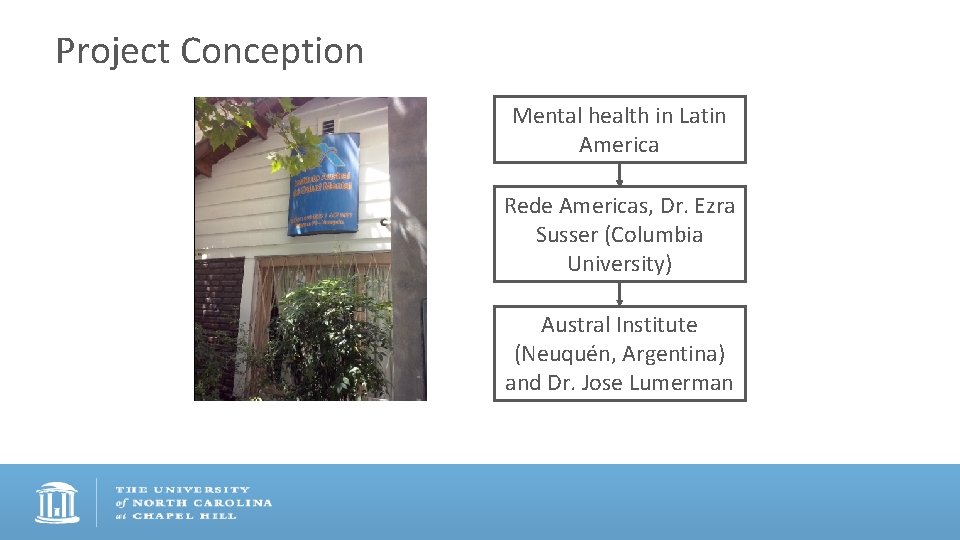
Project Conception Mental health in Latin America Rede Americas, Dr. Ezra Susser (Columbia University) Austral Institute (Neuquén, Argentina) and Dr. Jose Lumerman
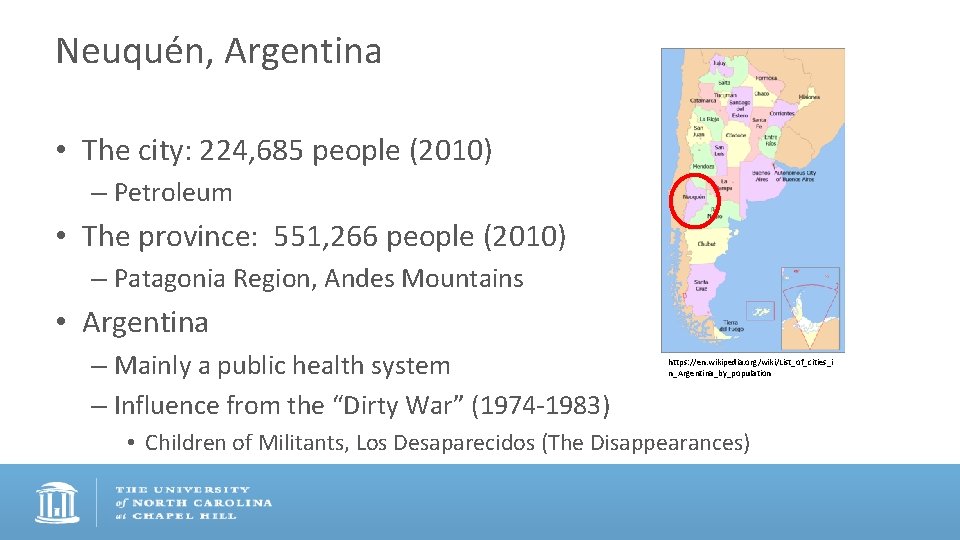
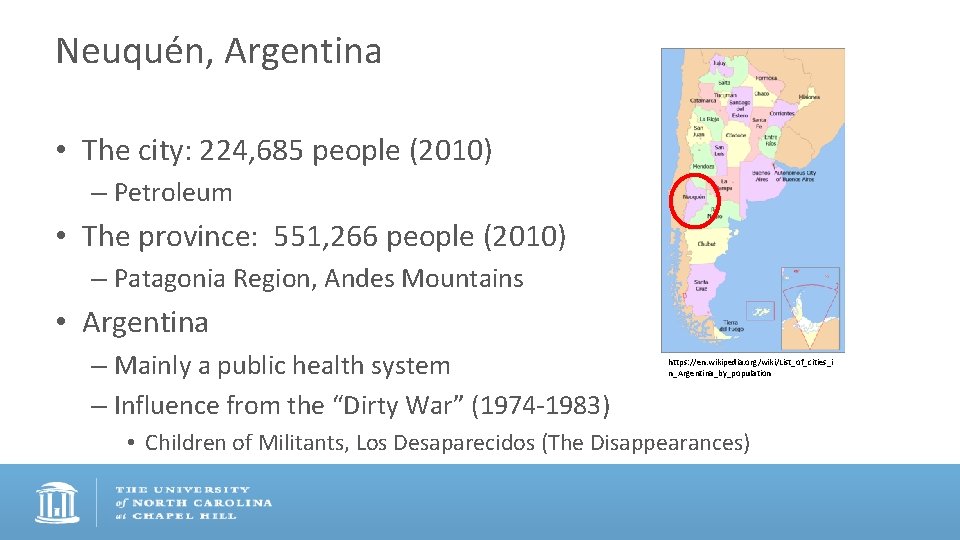
Neuquén, Argentina • The city: 224, 685 people (2010) – Petroleum • The province: 551, 266 people (2010) – Patagonia Region, Andes Mountains • Argentina – Mainly a public health system – Influence from the “Dirty War” (1974 -1983) https: //en. wikipedia. org/wiki/List_of_cities_i n_Argentina_by_population • Children of Militants, Los Desaparecidos (The Disappearances)
Clinic Background • 1987: 9 psychiatric beds for a population of 400, 000 people • Patients sent to Buenos Aires • 1993: Lumerman forms team • 1994: Austral Institute Opens • ISSN • Different clinic modalities (Day, Half-day, Ambulatory, Social Rehabilitation) • Diverse team of professionals
Research Gap – Mental health care in resource-deplete settings – Day hospitals/partial hospitalization research – Little known about the Austral Institute and it’s model of care
Project Design • Goals – Primary characteristics of the Austral Institute • • Population Services Implementation Interactions – Key aspects to success • In-person semi-structured interviews – Patients, employees, community affiliates
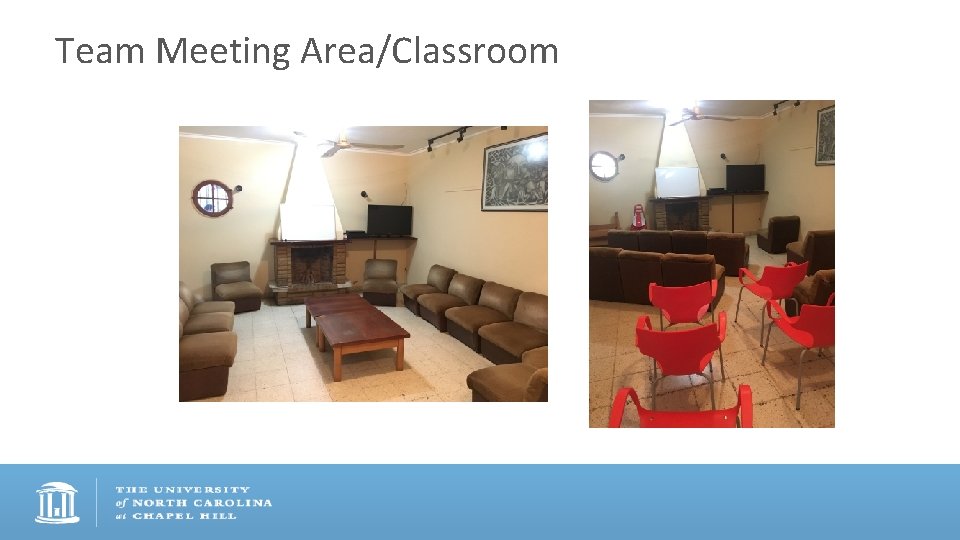
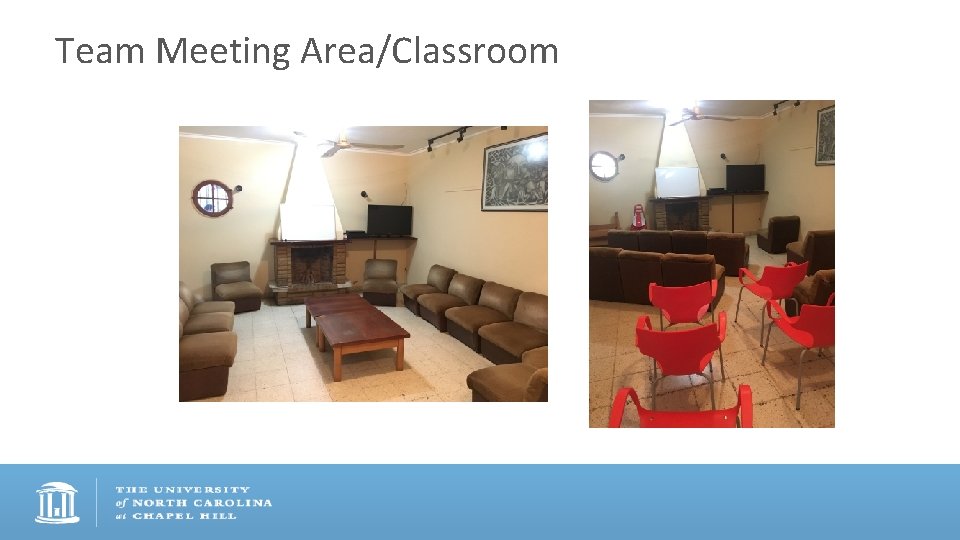
Team Meeting Area/Classroom
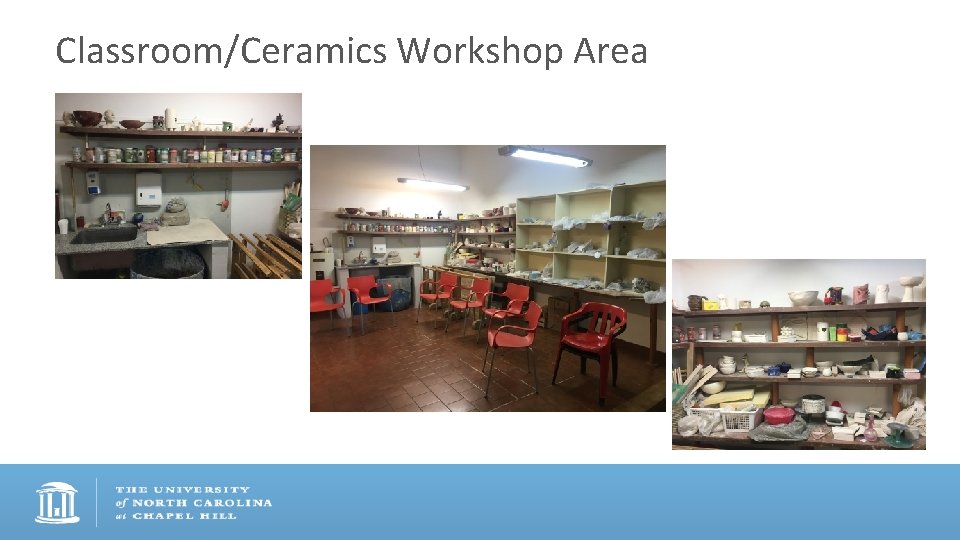
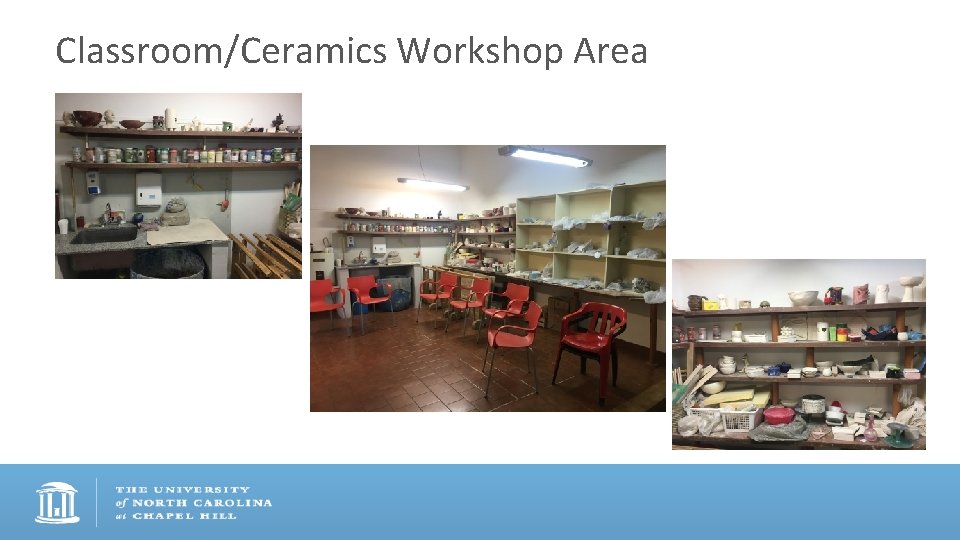
Classroom/Ceramics Workshop Area

Group therapy session
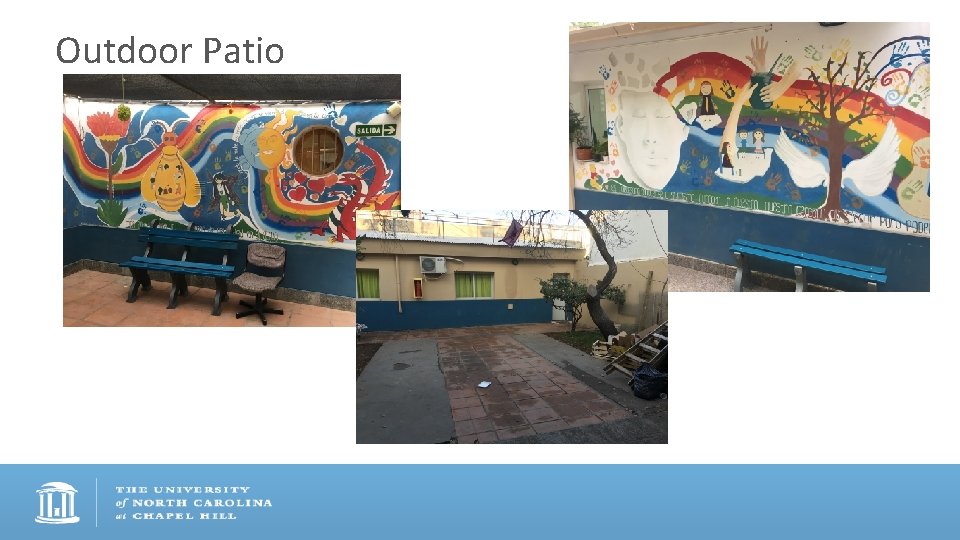
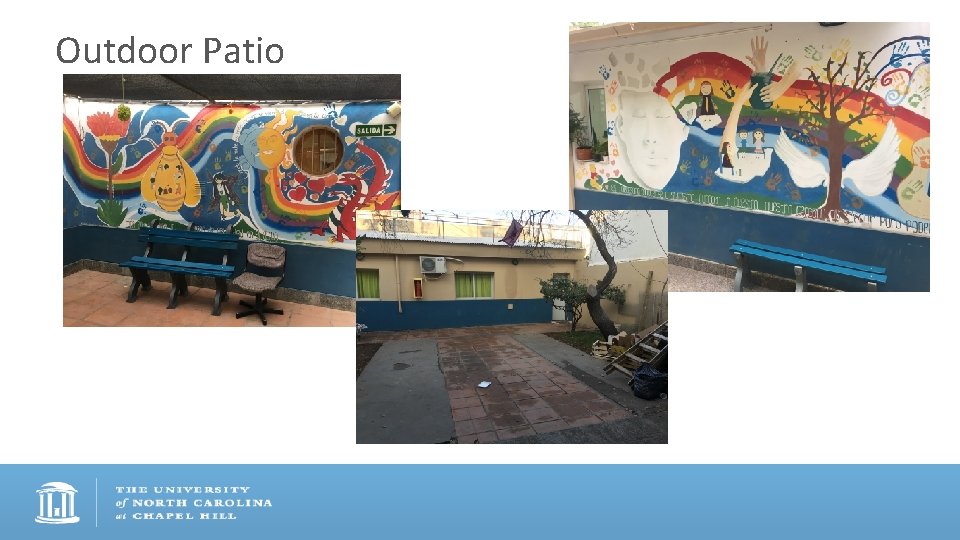
Outdoor Patio

The garden (in winter)
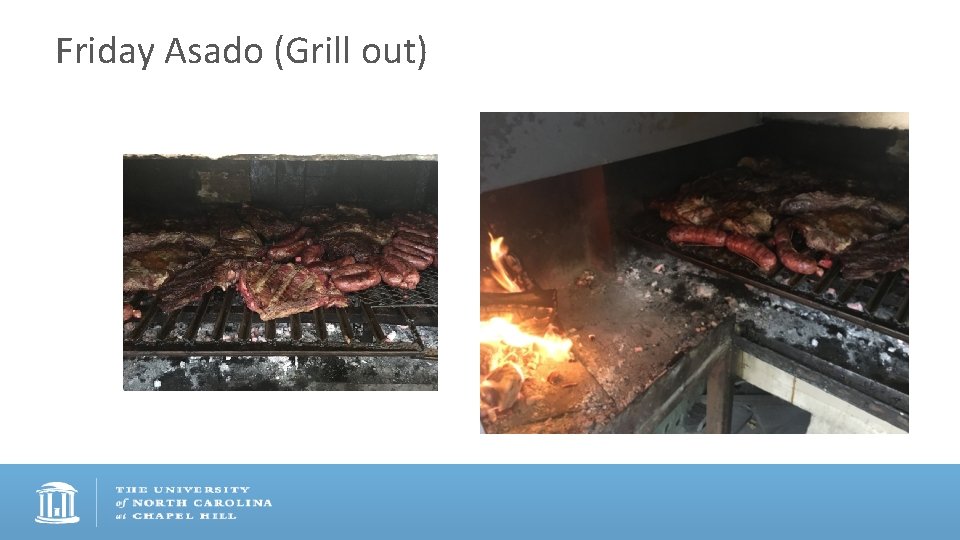
Friday Asado (Grill out)
Qualitative Analysis of Interview Data • Transcription of interviews • Developing a set of meaningful codes • Clinic structure and environment • Interpersonal relationships within the community • Mainstays of therapy • Analysis using Atlas. ti software
Primary Clinic Characteristics • Team of multi-dimensional professionals – Psychiatrists, psychologists, general physicians, therapeutic assistants, workshop professors (art, theater, mindfulness, literature) • Diverse patient population – Depression, Bipolar, Substance Abuse, Panic Disorder, Post-Traumatic Stress Disorder, Schizophrenia, Personality Disorders, Dementia • Targeted modalities for patient needs – Day Hospital as focus
Identifying Key Themes – Across all interviews • Therapeutic community • Clinic structure • Measures of patient improvement and recovery – Patient interviews • Feeling of intimacy – Employees • Equality in teamwork
Results • Differences between patient and employee perspectives – Measuring therapeutic success • Personal growth vs. functional rehabilitation – Value of unstructured time • “dead time” vs. “free time”
Unstructured Time: Employee The free time is a space that contributes to health so to be able to generate these free times where patients can learn to do activities that have to do with enjoyment, leisure, rest…it is a space to be creative, to be able to look for something, and not like the workshops…they tell you what to do…here no, you have to search for it and enjoy yourself. (Female, Therapeutic Assistant, 7 months of employment)
Unstructured Time: Patients I don’t like the dead times. After lunch we have many hours here to play ping pong, which yes I like but…I think it would be better to use this time for something more productive, let’s say the workshops. (Male, Depression, 1 year at clinic) Additionally, because I’m learning to plan my weekends, we have a planning group so that now I’m no longer in my house without anything to do, lying down if I don’t go out. (Female, Panic Disorder, 2 months at clinic)
Results • Keys to clinic success – Alta Simplicidad or “High Simplicity” • Local resources, workshops, unstructured time, community – External support vital to sustainability - “Obra Social” – Teamwork to gain comprehensive understanding of patient status
High Simplicity and Teamwork Here the novelty is the general physician, not the psychiatric physician. The general physician can take care of patients with mental illnesses and inter-consults with the psychiatrist…because if the physician works with the psychologist, the psychiatrist, the nurse, therapeutic assistant, what makes up therapeutic community…all of this forms part of the treatment that has provided much, much success. (Male, Accountant, 24 years of employment)
Limitations/Considerations • Clinic – Dependent on Obra Social • Study – One clinic director for 25 years – What will happen with a successor? – Would findings be different if there had been a few directors? – Potential bias – Selection, Social desirability, Confirmation
Future Directions • Therapeutic value of unstructured time – Other settings where this method is used – Skills acquired • Feasibility of clinic model in other Latin American communities
Acknowledgements – – – – Vivian Go, Ph. D Paul Mihas, MA Kenan Penaskovic, MD Roberto Blanco, MD Ezra Susser, MD Dr. PH Jose Lumerman, MD The Austral Institute Community The Office of International Activities at UNC
Questions? Thank you!