A HighReliability Approach Using the QSEN Framework Transforms
A High-Reliability Approach Using the QSEN Framework Transforms Health System Initial Nursing Competency Validation Jessica M. Phillips, MSN, RN, BCNPD, Professional Development Specialist Lee Galuska, Ph. D, RN, NE-BC, Director; Nursing Practice, Education, and Research
Who We Are 2
UCLA Health Hospitals: • Ronald Reagan UCLA Medical Center – 540 inpatient rooms • Mattel Children’s Hospital UCLA – 146 inpatient rooms • Stewart and Lynda Resnick Neuropsychiatric Hospital at UCLA – 74 inpatient rooms • Santa Monica UCLA Medical Center and Orthopaedic Hospital – 266 inpatient rooms 3
Background • The overall goal for the QSEN project was to meet the challenge of preparing future nurses who will have the knowledge, skills and attitudes (KSAs) necessary to continuously improve the quality and safety of the healthcare systems within which they work • High reliability healthcare organizations provide exceptionally safe, high-quality care • Competent staff, standardization of practice, and outcome monitoring are a few elements of highly reliable organizations • Nursing professional development scope and standards support the adoption of QSEN competencies in nursing practice 4

Nursing Professional Dev. Scope and Standards • QSEN competencies accepted in academia • QSEN comp. based on IOM comp. • Academic and practice setting alignment • ANPD position acknowledges interprofessional collaboration and continuing education to achieve quality patient care Harper & Maloney, 2016. ; National Research Council, 2003 5
Introduction Purpose Why the Change: Variability in the structures and processes for unit-based nursing orientation and initial competency validation across UCLA Health • Current state: decreased reliability in practice, gaps in regulatory compliance, potential gaps in staff preparation for practice and overall retention implications • Desired state: standardization of competency assessment to establish clear expectations for new hires to succeed and provide safe quality care
Methods • A modified Delphi technique was used with a group of Nursing Professional Development (NPD) Specialists, Clinical Nurse Specialists (CNS), and clinical nurses to design a consistent process and structure for validating initial competencies • Strategies adopted to get to the desired state: (1) QSEN Competencies Framework (2) Knowledge, Skills, Attitude (KSA) Validation (3) High-Reliability Approach – structures, forms, standards 7

Strategy #1 QSEN Framework 8
System Adoption of QSEN • Nursing orientation – patient experience • Newly licensed nurse – initial unit orientation* • Preceptor development training (continuing education) • Unit leadership, CNS, and educator training 9
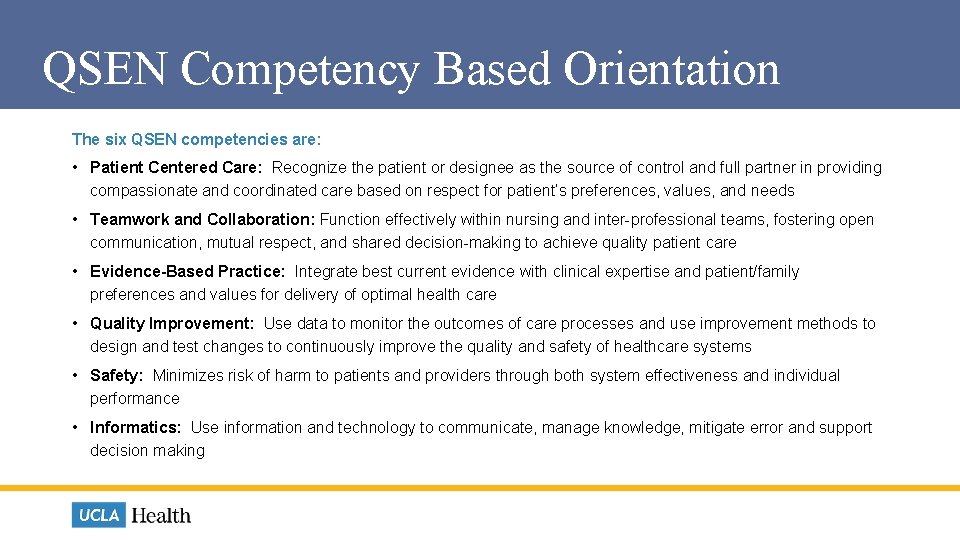
QSEN Competency Based Orientation The six QSEN competencies are: • Patient Centered Care: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs • Teamwork and Collaboration: Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care • Evidence-Based Practice: Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care • Quality Improvement: Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of healthcare systems • Safety: Minimizes risk of harm to patients and providers through both system effectiveness and individual performance • Informatics: Use information and technology to communicate, manage knowledge, mitigate error and support decision making
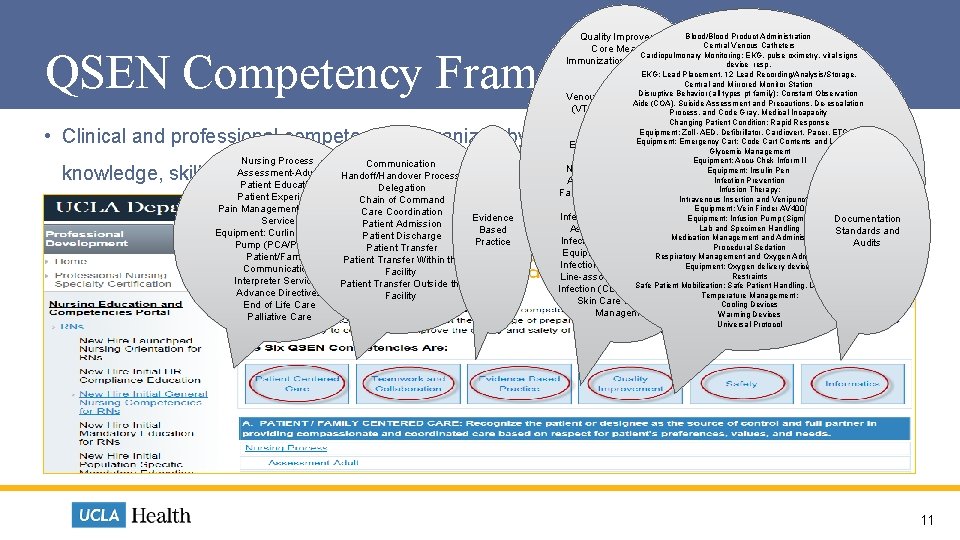
Quality Improvement Blood/Blood Product Administration Central Venous Catheters Core Measures Cardiopulmonary Monitoring: EKG, pulse oximetry, vital signs Immunization Screening in device resp. Adults EKG: Lead Placement, 12 Lead Recording/Analysis/Storage, Central and Mirrored Monitor Station Sepsis Disruptive Behavior (all types pt family): Constant Observation Venous Thromboembolism Aide (COA), Suicide Assessment and Precautions, De-escalation (VTE) Prophylaxis: VTE Process, and Code Gray, Medical Incapacity Prophylaxis and Changing Patient Condition: Rapid Response Equipment: Zoll -AED, Defibrillator, Cardiovert, Pacer, ETCO 2 Anticoagulation Equipment: VTE Devices. Emergency Cart: Code Cart Contents and Location Glycemic Management Equipment: Foot Pump Equipment: Accu-Chek Inform II Nurse Sensitive Indicators: Equipment: Insulin Pen Infection Prevention Adult Fall Prevention: Post Infusion Therapy: Fall and Post Fall Head Injury Intravenous Insertion and Venipuncture Care Equipment: Vein Finder AV 400 Infection Prevention: Catheter. Equipment: Infusion Pump (Sigma) Documentation Lab and Specimen Handling Associated Urinary Tract Standards and Medication Management and Administration Infection (CAUTI) Prevention Audits Procedural Sedation Equipment: Bladder Scanner Respiratory Management and Oxygen Administration Infections Prevention: Central Equipment: Oxygen delivery devices Restraints Line-associated Bloodstream Safe Patient Mobilization: Safe Patient Handling, UMOVE BMAT Infection (CLASBI) Prevention Temperature Management: Skin Care and Wound Cooling Devices Management Warming Devices QSEN Competency Framework • Clinical and professional competencies organized by QSEN domains including Nursing Process Communication Assessment-Adult Handoff/Handover Process Patient Education Delegation Patient Experience Chain of Command Pain Management and Pain Care Coordination Evidence Service Patient Admission Based Equipment: Curlin Pain. Smart Patient Discharge Practice Pump (PCA/PCEA) Patient Transfer Patient/Family Patient Transfer Within the Communication Facility Interpreter Services Patient Transfer Outside the Advance Directives Facility End of Life Care Palliative Care knowledge, skills, and attitudes required for competent performance Universal Protocol 11
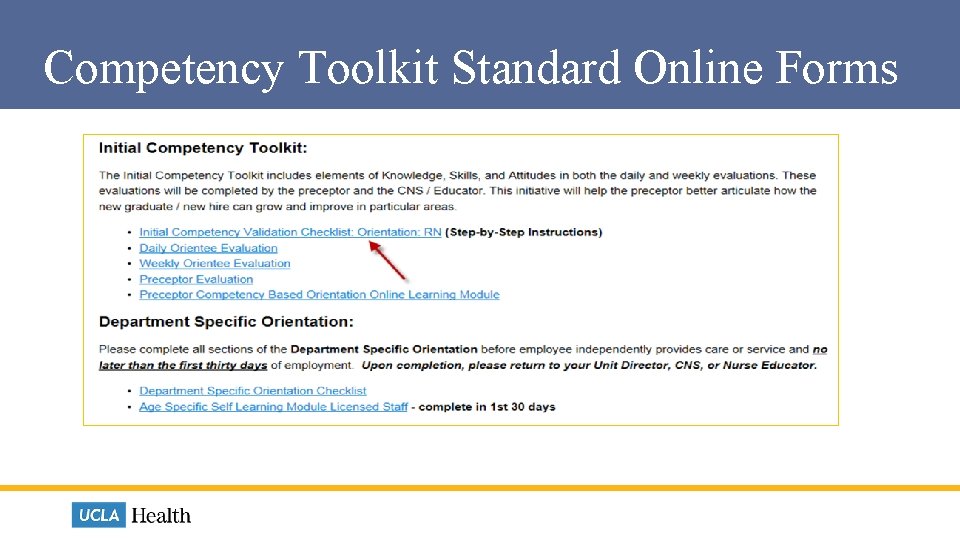
Competency Toolkit Standard Online Forms
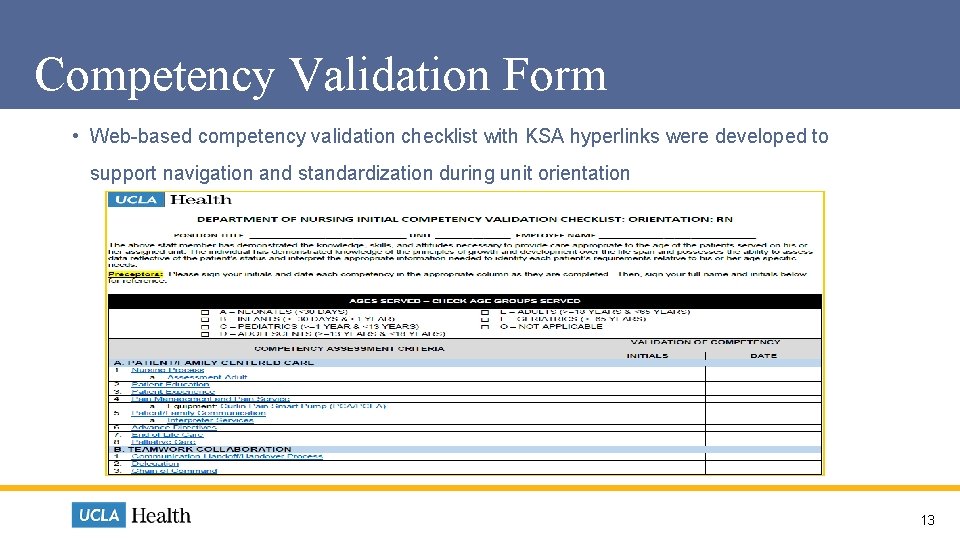
Competency Validation Form • Web-based competency validation checklist with KSA hyperlinks were developed to support navigation and standardization during unit orientation 13
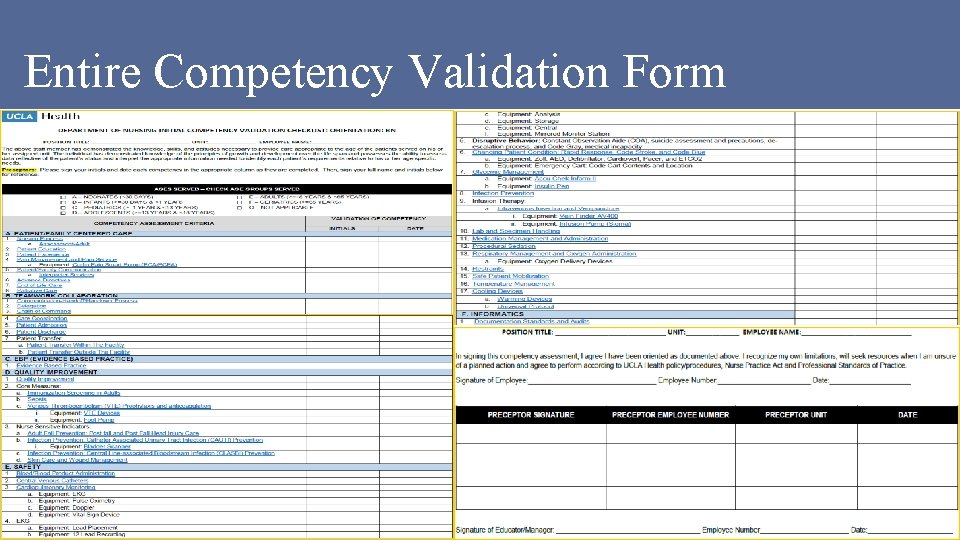
Entire Competency Validation Form 14
Strategy #2 KSA Validation 15
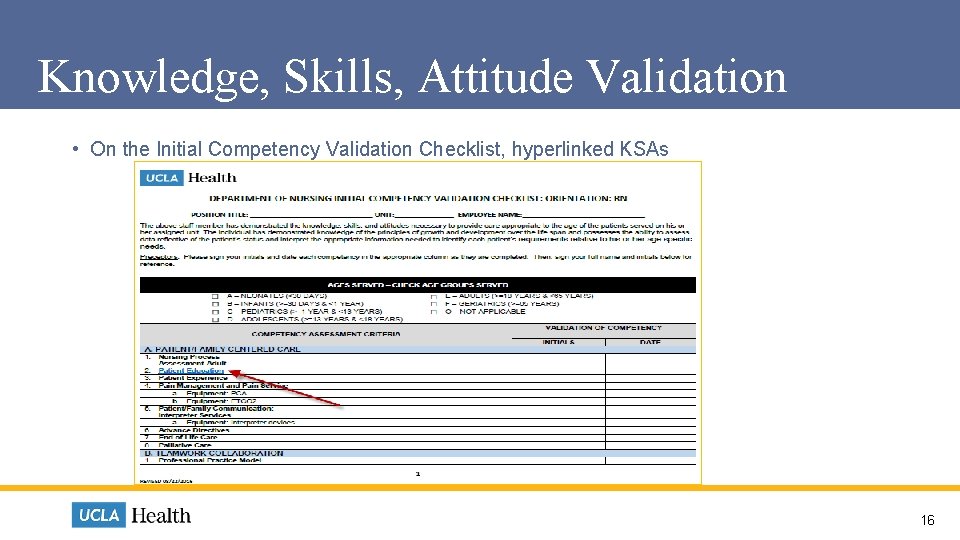
Knowledge, Skills, Attitude Validation • On the Initial Competency Validation Checklist, hyperlinked KSAs 16
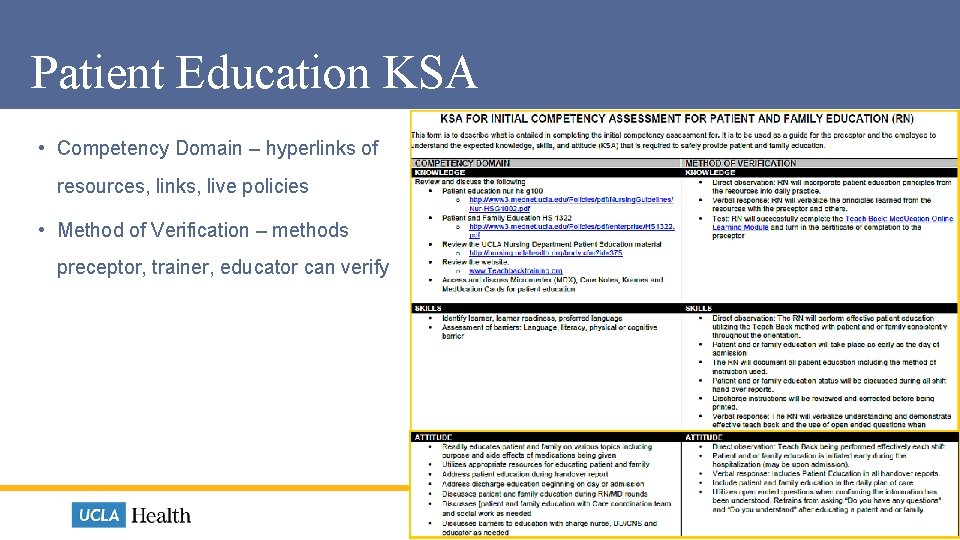
Patient Education KSA • Competency Domain – hyperlinks of resources, links, live policies • Method of Verification – methods preceptor, trainer, educator can verify 17

Strategy #3 High Reliability Approach (Standardization) 18
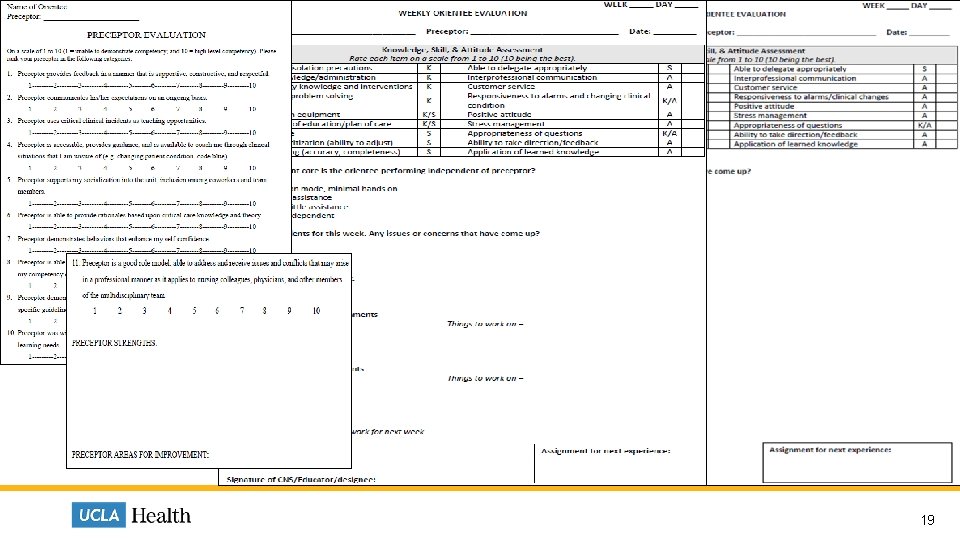
High-Reliability Approach 19
Results Preceptors (n=13) • 76% able to access forms • 86% are using the forms • 94% validate competency (validation checklist/KSAs) CNS, Educator, Manager (n=43) • 56% able to validate use of forms by preceptors • 58% meet weekly with preceptor/preceptee • 71% able to explain use of forms with preceptors 20
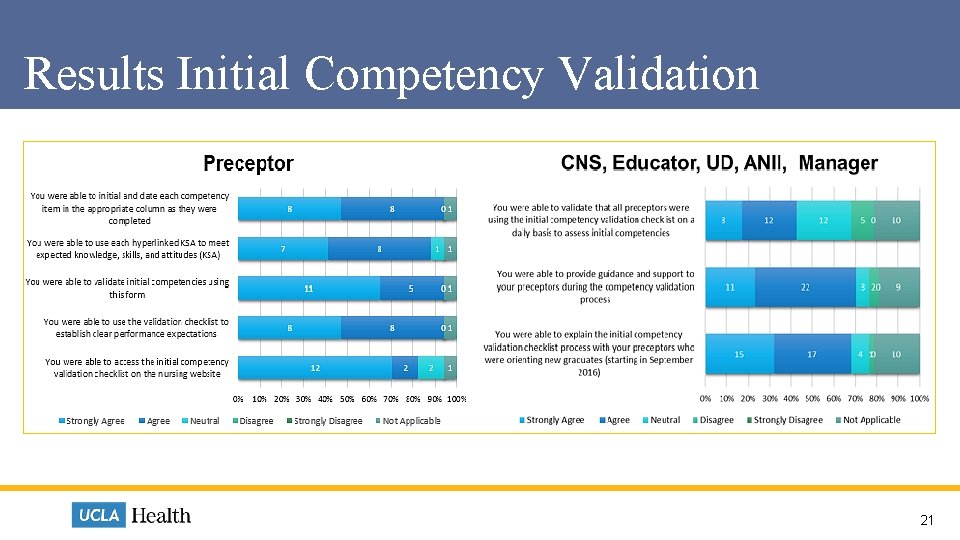
Results Initial Competency Validation 21
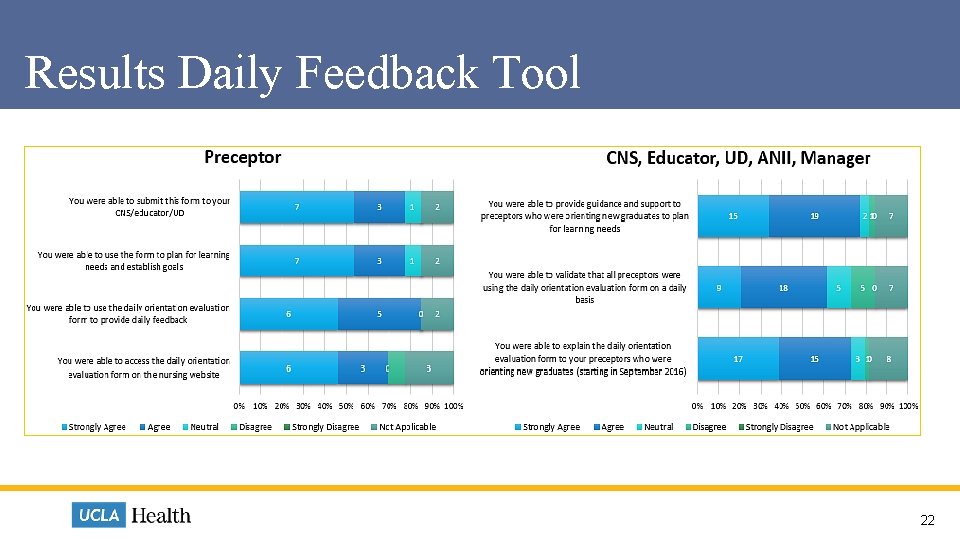
Results Daily Feedback Tool 22
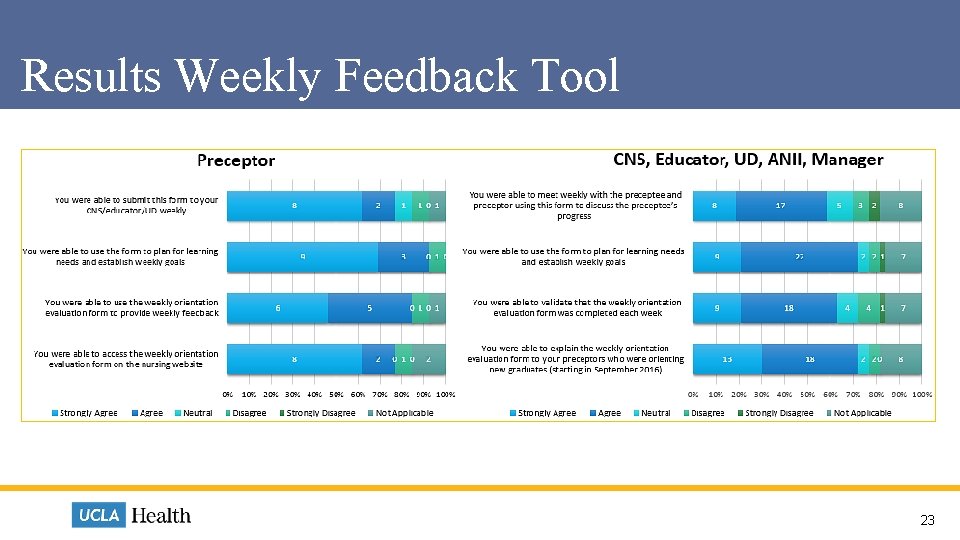
Results Weekly Feedback Tool 23
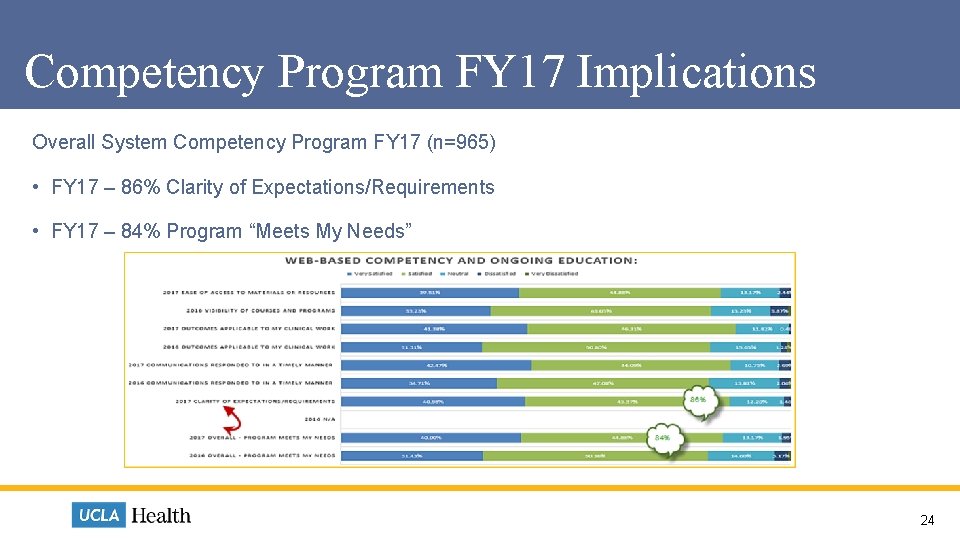
Competency Program FY 17 Implications Overall System Competency Program FY 17 (n=965) • FY 17 – 86% Clarity of Expectations/Requirements • FY 17 – 84% Program “Meets My Needs” 24

Future Direction/Next Steps • Continue to measure outcome/impact of QSEN competency framework adoption for newly licensed RNs in both system orientation and unit orientation • Develop QSEN competency framework for initial new hires (all), population specific and mandatory education • Adoption of QSEN in continuing education, educator competencies, clinical advancement programs, job descriptions, system learning needs assessment 25
References • Altmiller, G. (2013). Application of the quality and safety education for nursing competencies in orthopaedic nursing. Orthopaedic Nursing, 32(2), 98 -103. • Cronenwett, L. , Sherwood, G. , Barnsteiner, J. , Disch, J. , Johnson, J. , Mitchell, P. , Sullivan, D. T. , & Warren, J. (2007). Quality and safety education for nurses. Nursing Outlook, 55(3), 122 -131. • Harper, M. G. , & Maloney, P. (2016). Nursing professional development scope and standards of practice (3 rd ed. ). Chicago, IL: ANPD • Kirkpatrick, D. L. (1994). Evaluating training programs. San Francisco, CA: Berrett-Koehler Publishers, Inc. • Levine, J. & Johnson, J. (2014). An organizational competency validation strategy for registered nurses. Journal for Nurses in Professional Development, 30(2), 58 -65. • Melnyk, B. M. (2012). Achieving a high-reliability organization through implementation of the ARCC model for systemwide sustainability of evidence-based practice. Nursing Administration Quarterly, 36(2), 127 -135. • National Research Council. (2003). Health professions education: A bridge to quality. Washington, DC: The National Academics Press. • Wright, D. (2005). The ultimate guide to competency assessment in health care (3 rd ed. ). Minneapolis, MN: Creative Health Care Management, Inc.
Questions and Comments 27
- Slides: 27