A functional Eating and Drinking Ability Classification System
A functional Eating and Drinking Ability Classification System (EDACS) for people with cerebral palsy Diane Sellers Ph. D MA BA Research Speech and Language Therapist Chailey Heritage Clinical Services
Funding Independent Research Project – funded for 3 years Commissioned by the National Institute for Health Research (NIHR) through Research for Patient Benefit Views expressed are those of author and not necessarily those of NHS, NIHR or the Department of Health
Content Background Methods Content of EDACS Reliability of EDACS Case studies Conclusion Next steps
Background Cerebral Palsy (CP) is a group of permanent, but not unchanging, disorders of movement and / or posture and of motor function, which are due to a non-progressive interference, lesion, or abnormality of the developing immature brain. (Cans et al. 2009) Prevalence 1. 5 -3 children per 1, 000 live births (Cans 2007)

Cerebral Palsy Affects many areas of function including: �Sitting, standing, walking �Speech and language development �Use of hands �Senses including vision and hearing �Eating, drinking and swallowing
Background Nutrition Team at Chailey Heritage Clinical Services: Speech and Language Therapist Dietitian Paediatrician - Neuro-developmental specialist Nutrition Nurse specialist
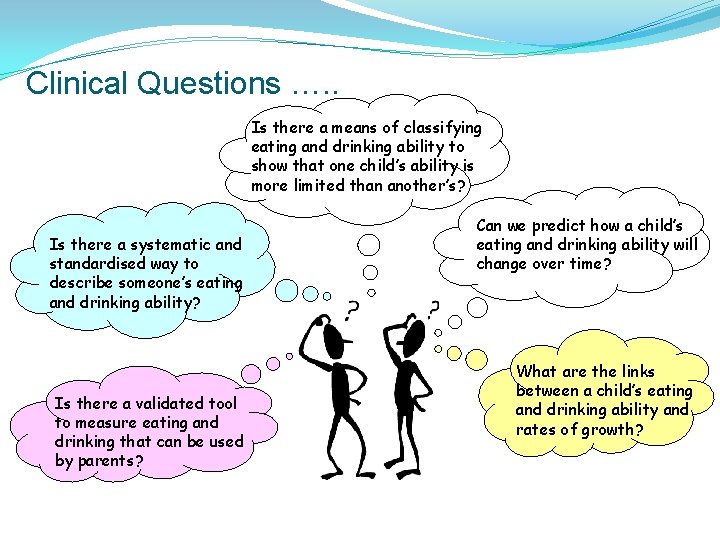
Clinical Questions …. . Is there a means of classifying eating and drinking ability to show that one child’s ability is more limited than another’s? Is there a systematic and standardised way to describe someone’s eating and drinking ability? Is there a validated tool to measure eating and drinking that can be used by parents? Can we predict how a child’s eating and drinking ability will change over time? What are the links between a child’s eating and drinking ability and rates of growth?
Cerebral Palsy 22% of identified deaths for people with CP resulted from solids or liquids in their lungs or windpipe Where difficulty swallowing was mentioned on death certificate (only 3%) cause of death in 60% of these cases was solids or liquids in the lungs or windpipe Improving Health and Lives Learning Disabilities Observatory (2010)
Gross Motor Function Classification System GMFCS – Palisano et al. (1997) Based on concepts of disability and “limitation in performance at the level of the whole person” (Nagi 1965) NOT: parts of body most involved neuro-anatomical location of lesion impairment in muscle tone, voluntary control of activity
Reasons for GMFCS Enhance communication among professionals and families Assist in determining needs of child with CP Creation of databases (CP Surveillance) Comparing and generalising results Predictive validity
Health Measurement - Ordinal Scales For example: Tumour Grading Scales (0 – 4) Cancer Staging Scales (0, I to IV) Injury severity score (1. Minor, 2. Moderate, 3. Serious, 4. Severe, 5. Critical, 6. Unsurvivable)
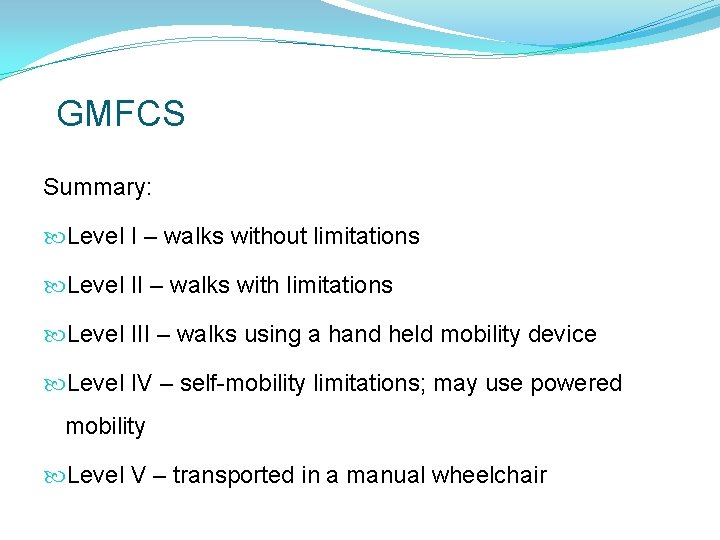
GMFCS Summary: Level I – walks without limitations Level II – walks with limitations Level III – walks using a hand held mobility device Level IV – self-mobility limitations; may use powered mobility Level V – transported in a manual wheelchair
GMFCS Standardises severity ratings of gross motor ability. Replaces terms such as “mild”, “moderate” and “severe impairment” which lack consistent definition. Use of such terms dependent upon experience. GMFCS is now well established as reliable systematic way of rating gross motor function.
Functional Classification Systems Other functional classification systems for people with CP: Manual Ability (MACS Eliasson et al. 2006) Communication Function (CFCS Hidecker et al. 2011) Viking Speech Scale (Pennington et al. 2011) Ordinal scales (I – IV or V) Measures of the extent of limitations to function Suitable for use in clinical and research contexts
Systematic Review Systematic review of ordinal scales used to classify eating and drinking ability of people with CP Ordinal scale = descriptions of eating and drinking ability placed in 3 or more ordered categories Identified 15 different measures in research literature
Systematic Review 13 / 15 scales for clinician / researcher use only 9 / 15 scales from parent interviews or questionnaires 8 / 15 scales used terms “mild”, “moderate” and “severe” differently 5 / 15 scales assessed either content validity and/or reliability O / 15 scales met psychometric quality standards Sellers, Pennington, Mandy and Morris (DMCN April 2014)
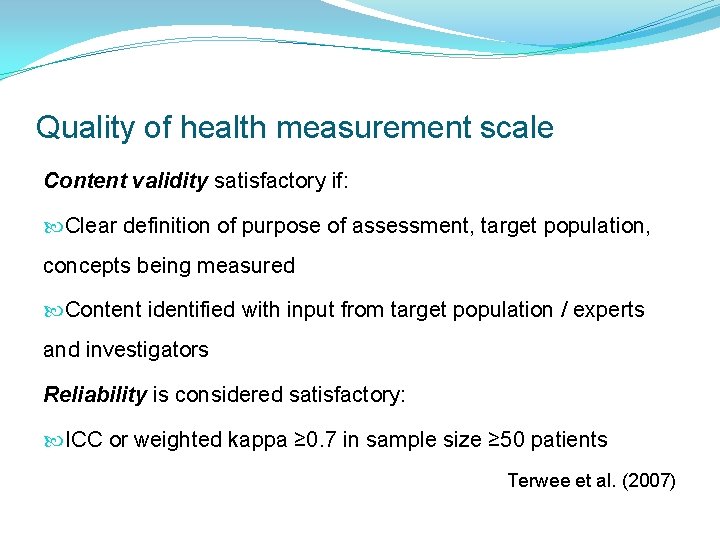
Quality of health measurement scale Content validity satisfactory if: Clear definition of purpose of assessment, target population, concepts being measured Content identified with input from target population / experts and investigators Reliability is considered satisfactory: ICC or weighted kappa ≥ 0. 7 in sample size ≥ 50 patients Terwee et al. (2007)
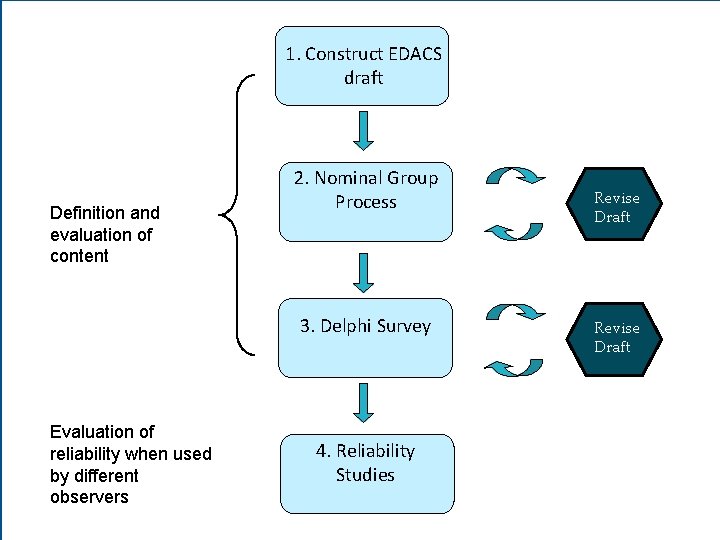
1. Construct EDACS draft Definition and evaluation of content 2. Nominal Group Process 3. Delphi Survey Evaluation of reliability when used by different observers 4. Reliability Studies Revise Draft
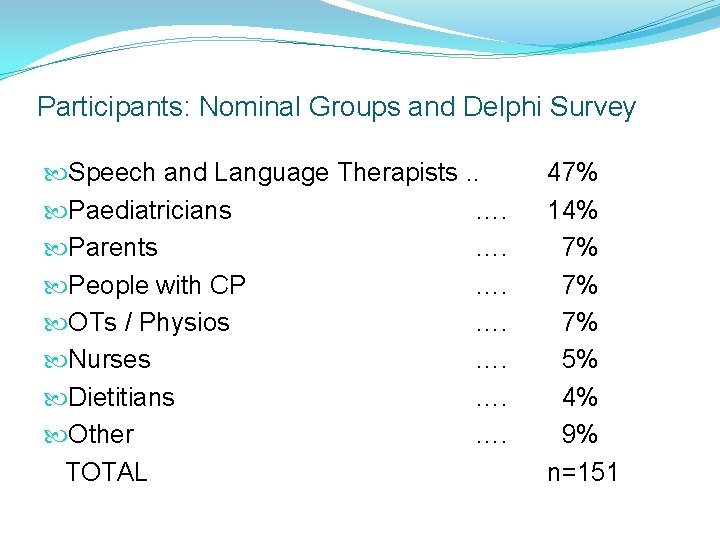
Participants: Nominal Groups and Delphi Survey Speech and Language Therapists. . Paediatricians …. Parents …. People with CP …. OTs / Physios …. Nurses …. Dietitians …. Other …. TOTAL 47% 14% 7% 7% 7% 5% 4% 9% n=151
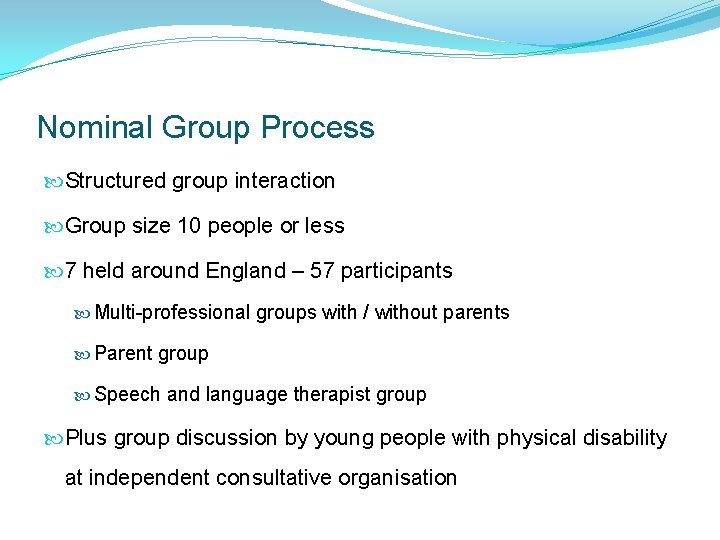
Nominal Group Process Structured group interaction Group size 10 people or less 7 held around England – 57 participants Multi-professional groups with / without parents Parent group Speech and language therapist group Plus group discussion by young people with physical disability at independent consultative organisation

Delphi Survey 95 participants in Delphi Survey over 2 rounds International group of experts with experience across 5 continents Years experience: range 2 y-52 y; median 16 y mean 19. 6 y SD 11. 8 y
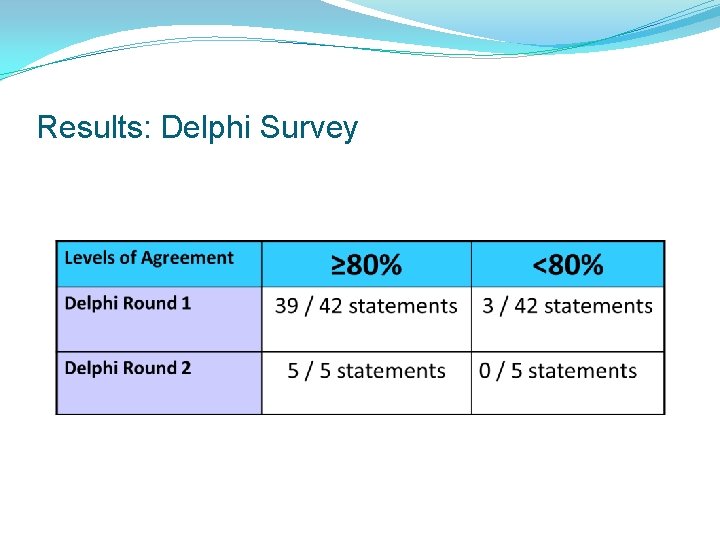
Results: Delphi Survey
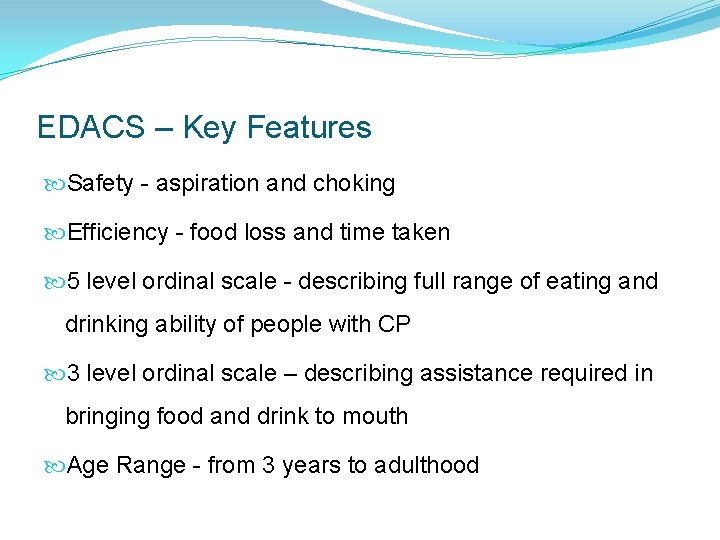
EDACS – Key Features Safety - aspiration and choking Efficiency - food loss and time taken 5 level ordinal scale - describing full range of eating and drinking ability of people with CP 3 level ordinal scale – describing assistance required in bringing food and drink to mouth Age Range - from 3 years to adulthood
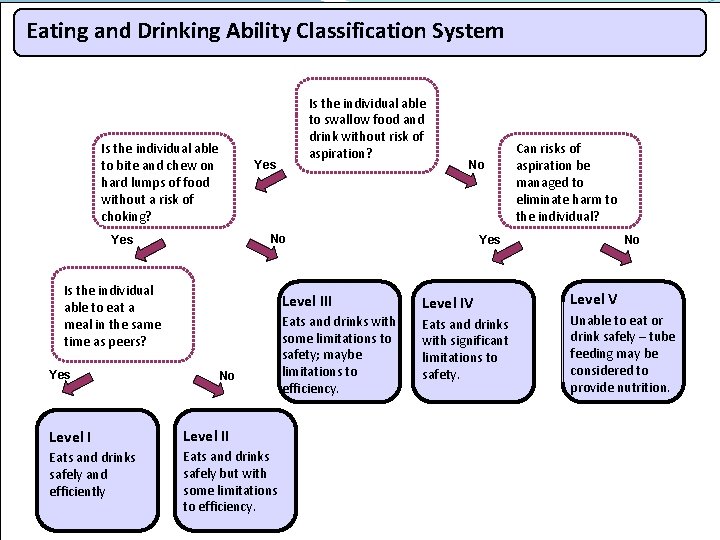
Eating and Drinking Ability Classification System Is the individual able to bite and chew on hard lumps of food without a risk of choking? Yes No No Yes Is the individual able to eat a meal in the same time as peers? Yes Is the individual able to swallow food and drink without risk of aspiration? Level III No Level II Eats and drinks safely and efficiently Eats and drinks safely but with some limitations to efficiency. Eats and drinks with some limitations to safety; maybe limitations to efficiency. Can risks of aspiration be managed to eliminate harm to the individual? Yes Level IV Eats and drinks with significant limitations to safety. No Level V Unable to eat or drink safely – tube feeding may be considered to provide nutrition.

Food textures Level I - Eats a wide range of different texture foods that are age appropriate. Level II - Eats a range of food textures that are age appropriate. Level III - Eats puree and mashed food and may bite and chew some soft chew food textures. Level IV - Eats smooth purees or well mashed food. Level V - May manage very small tastes or flavours.
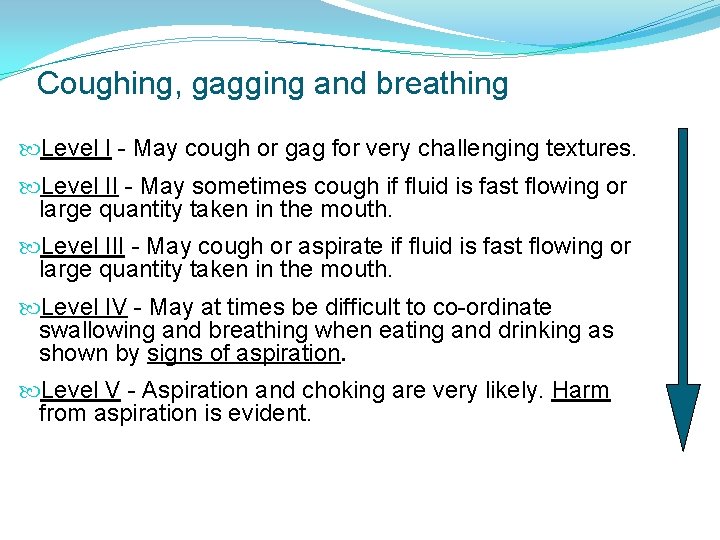
Coughing, gagging and breathing Level I - May cough or gag for very challenging textures. Level II - May sometimes cough if fluid is fast flowing or large quantity taken in the mouth. Level III - May cough or aspirate if fluid is fast flowing or large quantity taken in the mouth. Level IV - May at times be difficult to co-ordinate swallowing and breathing when eating and drinking as shown by signs of aspiration. Level V - Aspiration and choking are very likely. Harm from aspiration is evident.
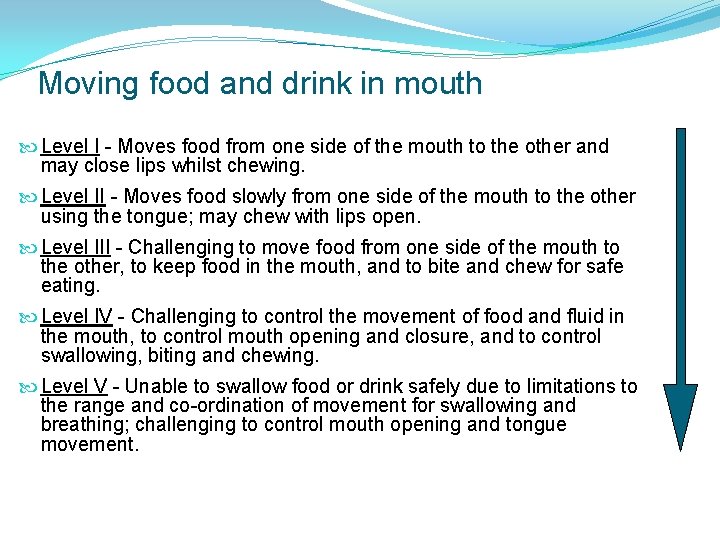
Moving food and drink in mouth Level I - Moves food from one side of the mouth to the other and may close lips whilst chewing. Level II - Moves food slowly from one side of the mouth to the other using the tongue; may chew with lips open. Level III - Challenging to move food from one side of the mouth to the other, to keep food in the mouth, and to bite and chew for safe eating. Level IV - Challenging to control the movement of food and fluid in the mouth, to control mouth opening and closure, and to control swallowing, biting and chewing. Level V - Unable to swallow food or drink safely due to limitations to the range and co-ordination of movement for swallowing and breathing; challenging to control mouth opening and tongue movement.
Distinctions between levels E. g. Distinctions between II and III Individuals in Level II manage most age appropriate food textures and drink with some slight modifications. Individuals at Level III will need more food textures to be modified in order to reduce risk of choking.
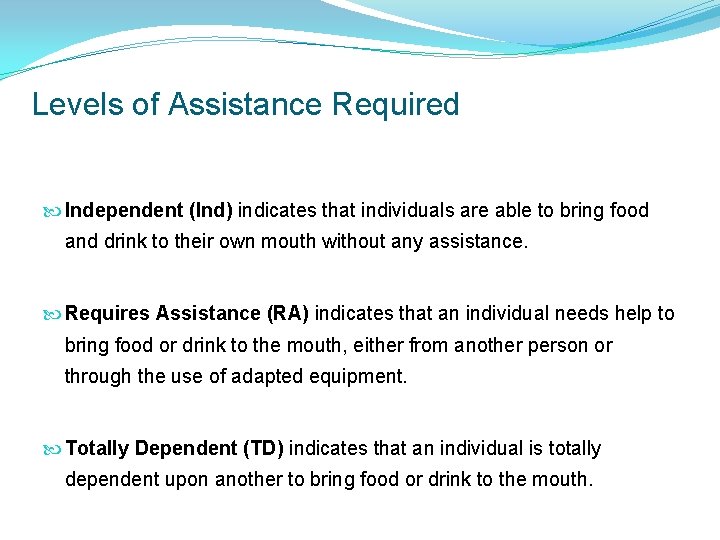
Levels of Assistance Required Independent (Ind) indicates that individuals are able to bring food and drink to their own mouth without any assistance. Requires Assistance (RA) indicates that an individual needs help to bring food or drink to the mouth, either from another person or through the use of adapted equipment. Totally Dependent (TD) indicates that an individual is totally dependent upon another to bring food or drink to the mouth.
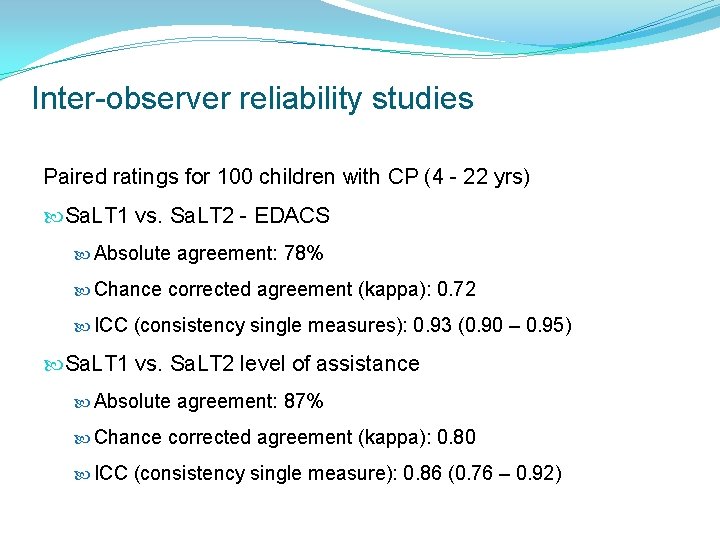
Inter-observer reliability studies Paired ratings for 100 children with CP (4 - 22 yrs) Sa. LT 1 vs. Sa. LT 2 - EDACS Absolute agreement: 78% Chance corrected agreement (kappa): 0. 72 ICC (consistency single measures): 0. 93 (0. 90 – 0. 95) Sa. LT 1 vs. Sa. LT 2 level of assistance Absolute agreement: 87% Chance corrected agreement (kappa): 0. 80 ICC (consistency single measure): 0. 86 (0. 76 – 0. 92)
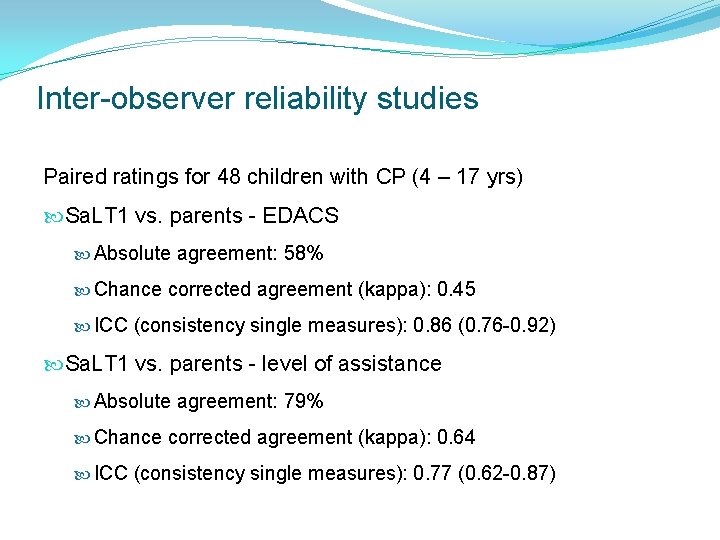
Inter-observer reliability studies Paired ratings for 48 children with CP (4 – 17 yrs) Sa. LT 1 vs. parents - EDACS Absolute agreement: 58% Chance corrected agreement (kappa): 0. 45 ICC (consistency single measures): 0. 86 (0. 76 -0. 92) Sa. LT 1 vs. parents - level of assistance Absolute agreement: 79% Chance corrected agreement (kappa): 0. 64 ICC (consistency single measures): 0. 77 (0. 62 -0. 87)
Inter-observer Reliability Studies Easy to use Parents can recognise their children Helped think more about eating and drinking Differences between Sa. LTS and parents consistent
Results Significant positive correlation between EDACS level and level of assistance – (Kendall’s Tau = 0. 69, p<0. 01) Incidence of tube feeding increased with EDACS levels although present at EDACS levels I to III Increased incidence of seizure activity with increasing limitations to eating and drinking ability
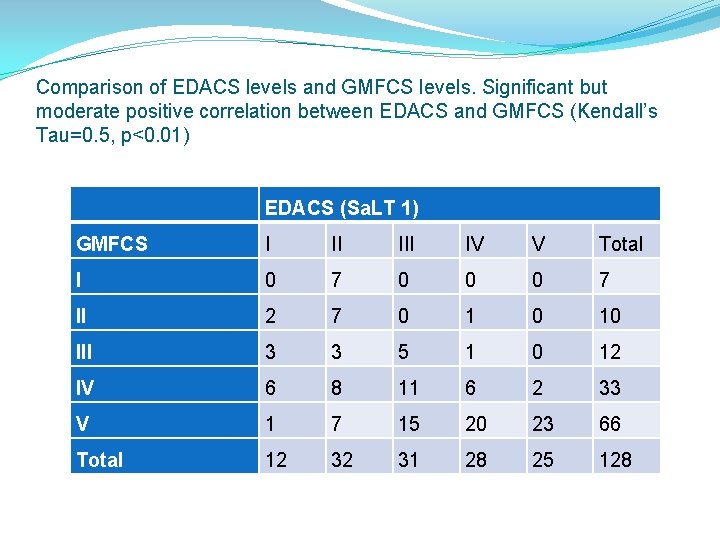
Comparison of EDACS levels and GMFCS levels. Significant but moderate positive correlation between EDACS and GMFCS (Kendall’s Tau=0. 5, p<0. 01) EDACS (Sa. LT 1) GMFCS I II IV V Total I 0 7 0 0 0 7 II 2 7 0 10 III 3 3 5 1 0 12 IV 6 8 11 6 2 33 V 1 7 15 20 23 66 Total 12 32 31 28 25 128

Case Study Toby is 8 years old and has dystonic CP. He is unable to move or sit independently or use his hands to handle any kind of object. He is unable to use speech. He is able to indicate “yes” and “no” through eye blinking when asked questions that make sense to him. Sometimes his communication signals are difficult to read unless you know him well. He has tiny tastes of food if he feels like it – recent chest infections led to a reduction in the amount of food he is now offered.
Toby – summary of function GMFCS Level V MACS Level V Viking Level IV CFCS Level III EDACS Level V
Case Study Alfie is 11 years old and has bilateral spastic CP. He is unable to move or sit independently and uses powered mobility accessed via a joy stick. He can use his hands to handle most objects. He uses speech which everyone understands. Alfie does not always understand what people say to him and conversation is not always straightforward. He has a gastrostomy for medication and fluid / nutrition if he is not interested in eating. He can bite, chew and swallow all textures of food and drink.
Alfie – summary of function GMFCS IV MACS II Viking I CFCS II EDACS I
Case Study Georgia is 14 years old with choreo-athetoid CP. She is able roll across the floor but cannot sit independently. She uses switches to access powered mobility; she can use her hands to knock objects off her tray. She expresses emotions with her voice, her family recognise some single words in some contexts. Georgia understands the language she hears around her. She can use her communication book with familiar communication partners and is an expert user of a voice output communication aid via switches to convey her meaning. She bites and chews soft lumps but chokes on hard lumps of food; she needs thickened fluids to feel safe drinking.
Georgia – summary of function GMFCS Level IV MACS Level IV Viking Level III CFCS Level II EDACS Level III
Functional Classification Systems GMFCS http: //www. canchild. ca/en/measures/gmfcs_expanded_revised. asp MACS http: //www. macs. nu/files/MACS_English_2010. pdf Viking http: //research. ncl. ac. uk/cargo-ne/measures. html CFCS http: //faculty. uca. edu/sharonr/Documents/CFCS_universal_2012_06_06. pdf EDACS www. EDACS. org
Conclusion EDACS - valid and reliable system Classifies eating and drinking performance of people with CP from age 3 years Useful in clinical and research contexts Free to download from www. EDACS. org. uk Published by Dev Med Child Neurology: Sellers et al. March 2014; Sellers et al. April 2014

Next steps Considerable interest in EDACS: 9 translation requests received (Dutch, German, Arabic, Farsi, Hebrew, Norwegian, Polish, Portuguese, Croatian) 8 requests to use in international research programmes before publication Interest from CP surveillance registers
Next steps – if NIHR grant application successful…. . Explore clinical utility of EDACS for people with CP Extend reliability studies (different users) Explore relationship between EDACS and respiratory health, and growth of people with CP Explore relationship between eating and drinking ability measured by EDACS and other areas of function NB. Research Therapist post 3 days per week for 2 ½ years…
Next steps Use EDACS in clinical practice Extend age range to include under 3 years Explore clinical utility for other client groups Explore eating and drinking ability over time Use EDACS in CP surveillance programmes

Other members of Project Team: Dr Christopher Morris Dr Anne Mandy Dr Lindsay Pennington Dr Matthew Hankins Dr Terry Pountney Mr Mike Carter Ms Sarah Ford
- Slides: 49