A clinically led whole systems approach to redesigning


















- Slides: 47
A clinically led whole systems approach to redesigning end of life care in Worcestershire Dr Felix Blaine- Clinical Champion Debbie Westwood – programme Lead
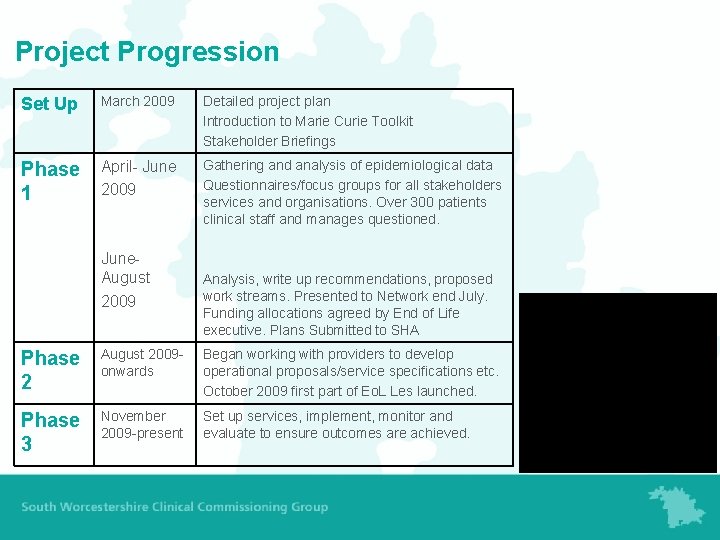
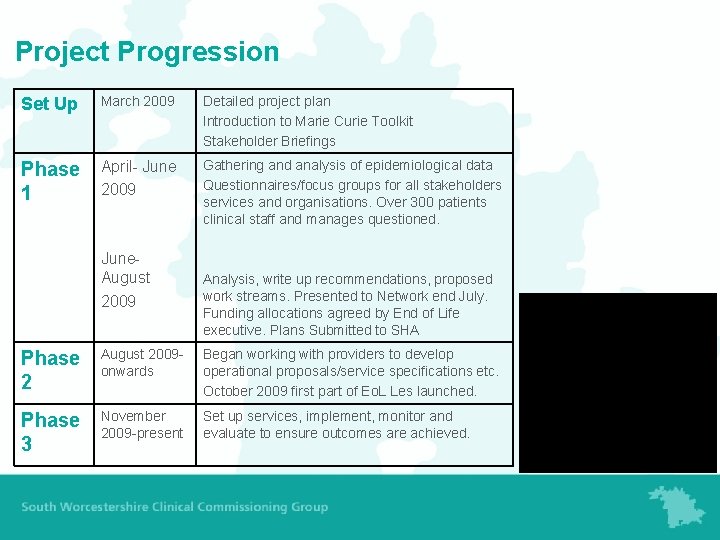
Project Progression Set Up March 2009 Detailed project plan Introduction to Marie Curie Toolkit Stakeholder Briefings Phase 1 April- June 2009 Gathering and analysis of epidemiological data Questionnaires/focus groups for all stakeholders services and organisations. Over 300 patients clinical staff and manages questioned. June. August 2009 Analysis, write up recommendations, proposed work streams. Presented to Network end July. Funding allocations agreed by End of Life executive. Plans Submitted to SHA Phase 2 August 2009 onwards Began working with providers to develop operational proposals/service specifications etc. October 2009 first part of Eo. L Les launched. Phase 3 November 2009 -present Set up services, implement, monitor and evaluate to ensure outcomes are achieved.
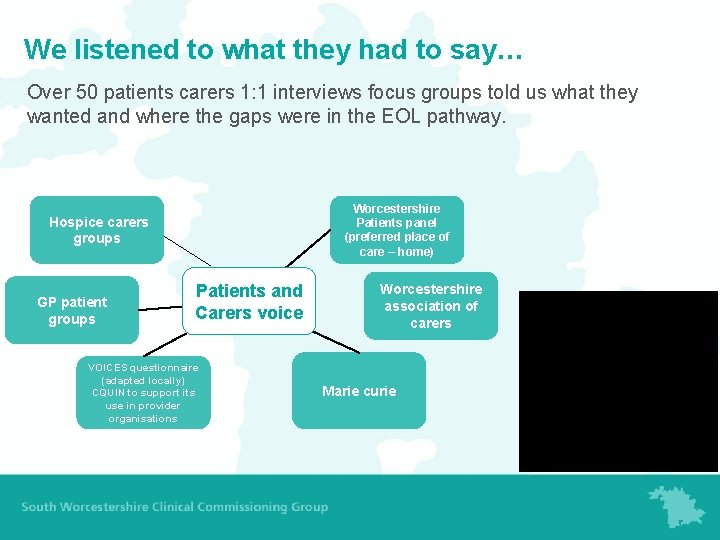
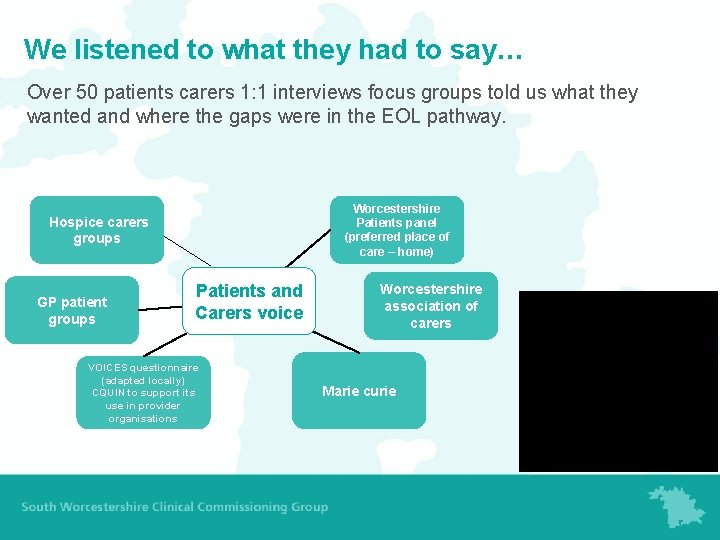
We listened to what they had to say… Over 50 patients carers 1: 1 interviews focus groups told us what they wanted and where the gaps were in the EOL pathway. Worcestershire Patients panel (preferred place of care – home) Hospice carers groups GP patient groups Patients and Carers voice VOICES questionnaire (adapted locally) CQUIN to support its use in provider organisations Worcestershire association of carers Marie curie
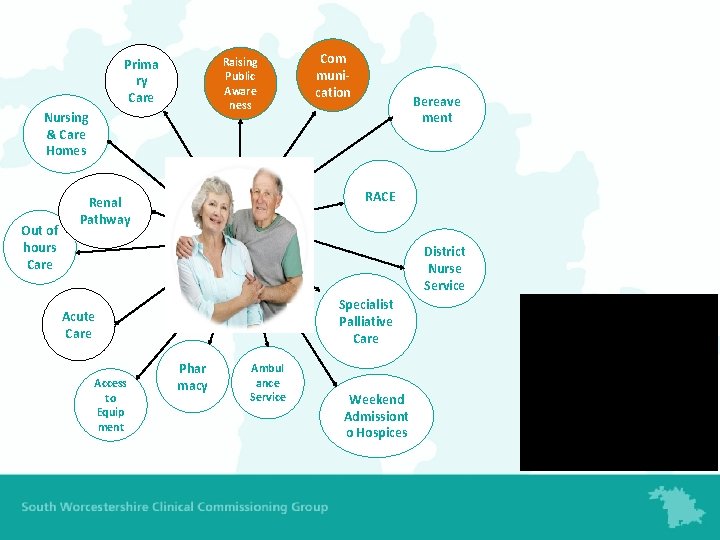
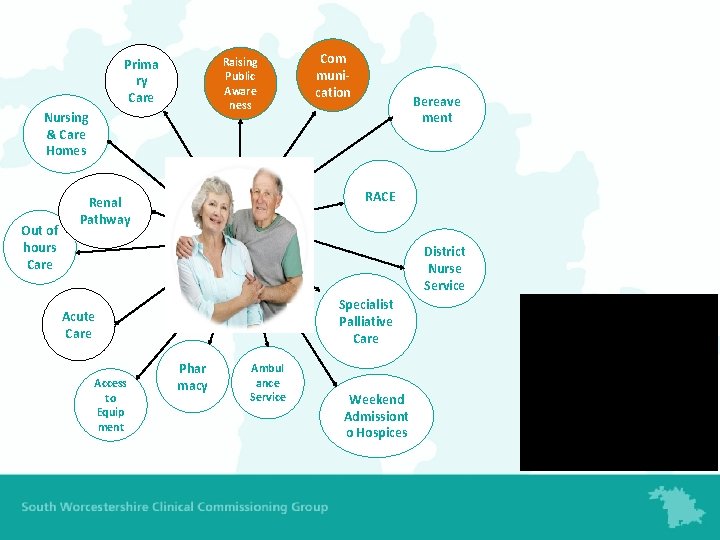
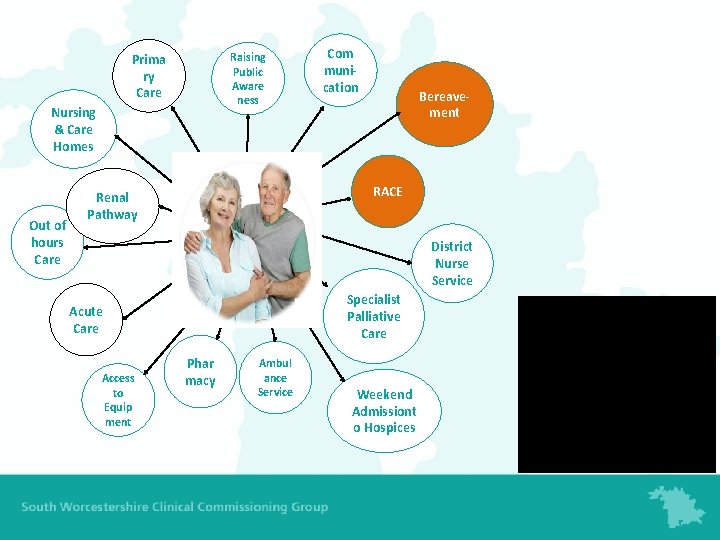
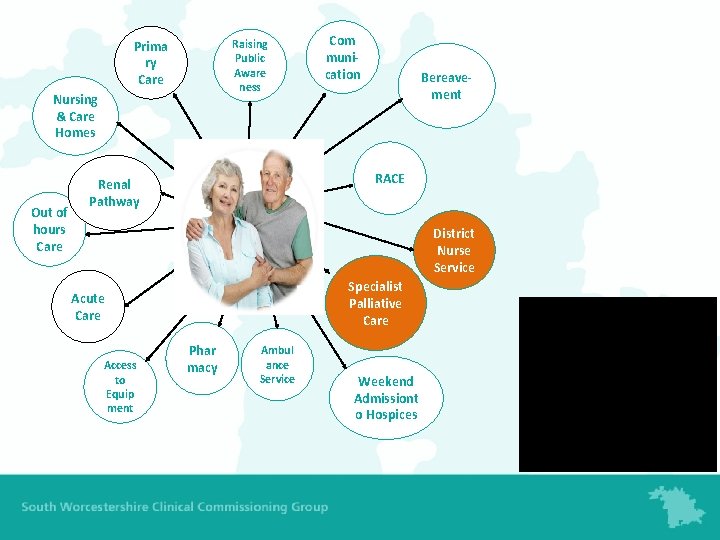
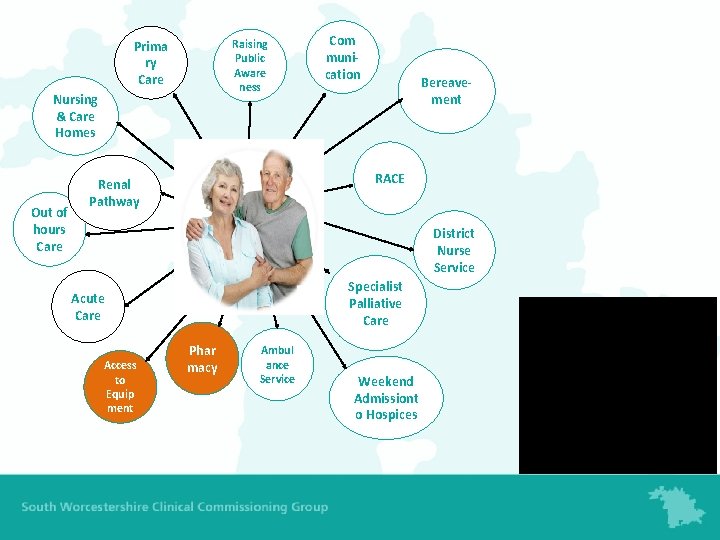
Raising Public Aware ness Prima ry Care Nursing & Care Homes Out of hours Care Com munication Bereave ment RACE Renal Pathway District Nurse Service Specialist Palliative Care Acute Care Access to Equip ment Phar macy Ambul ance Service Weekend Admissiont o Hospices
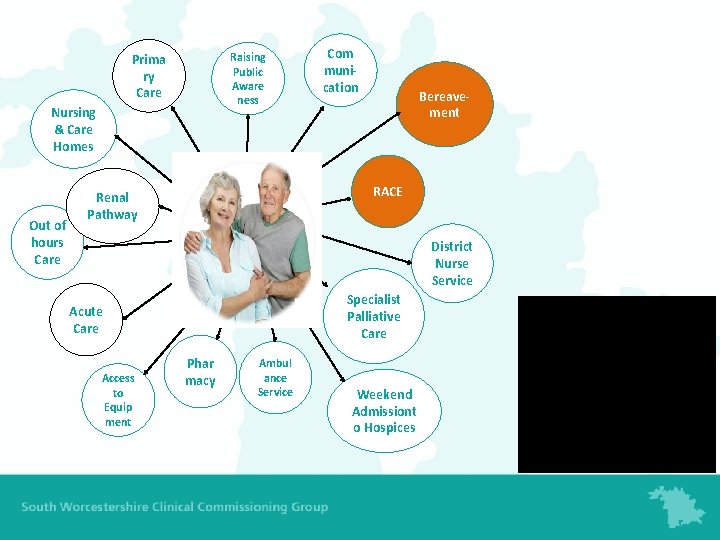
Raising Public Aware ness Prima ry Care Nursing & Care Homes Out of hours Care Com munication Bereavement RACE Renal Pathway District Nurse Service Specialist Palliative Care Acute Care Access to Equip ment Phar macy Ambul ance Service Weekend Admissiont o Hospices
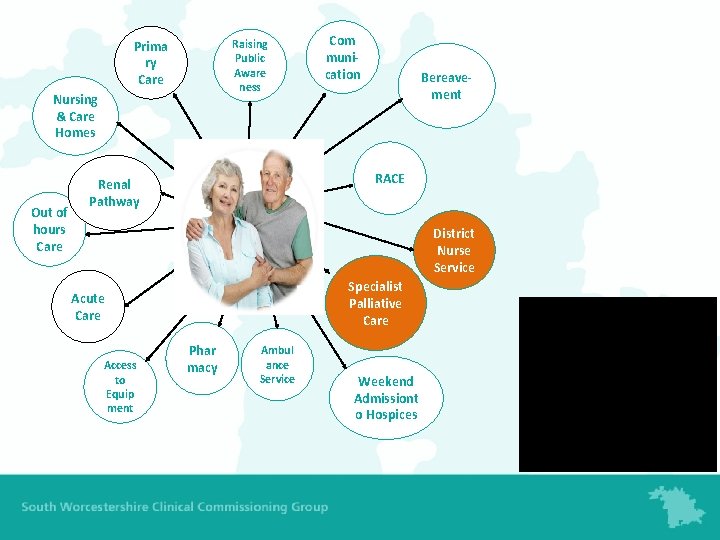
Raising Public Aware ness Prima ry Care Nursing & Care Homes Out of hours Care Com munication Bereavement RACE Renal Pathway District Nurse Service Specialist Palliative Care Acute Care Access to Equip ment Phar macy Ambul ance Service Weekend Admissiont o Hospices

Raising Public Aware ness Prima ry Care Nursing & Care Homes Out of hours Care Com munication Bereavement RACE Renal Pathway District Nurse Service Specialist Palliative Care Acute Care Access to Equip ment Phar macy Ambul ance Service Weekend Admission to Hospices
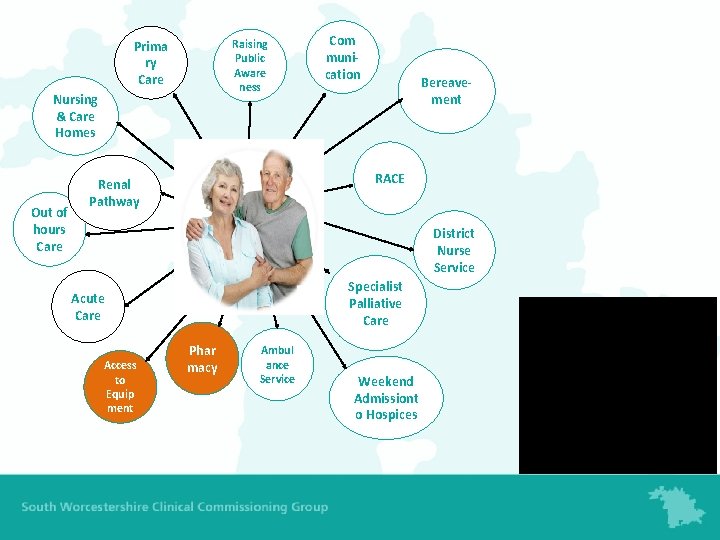
Raising Public Aware ness Prima ry Care Nursing & Care Homes Out of hours Care Com munication Bereavement RACE Renal Pathway District Nurse Service Specialist Palliative Care Acute Care Access to Equip ment Phar macy Ambul ance Service Weekend Admissiont o Hospices
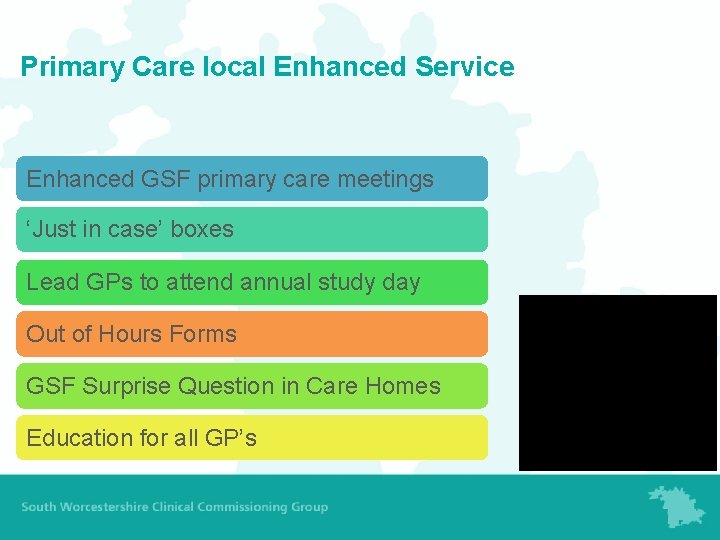
Primary Care local Enhanced Service Enhanced GSF primary care meetings ‘Just in case’ boxes Lead GPs to attend annual study day Out of Hours Forms GSF Surprise Question in Care Homes Education for all GP’s

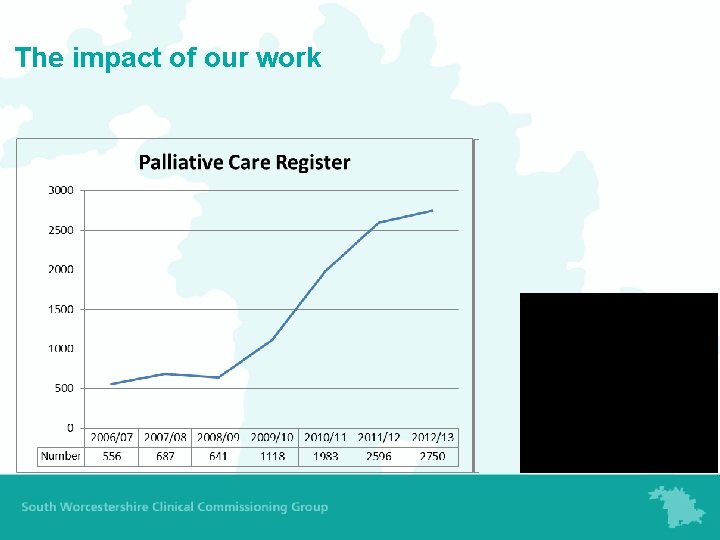
The impact of our work
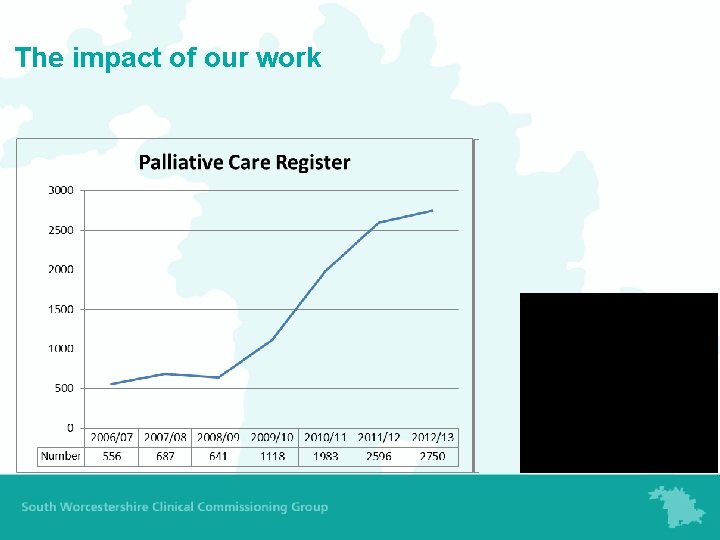
The impact of our work
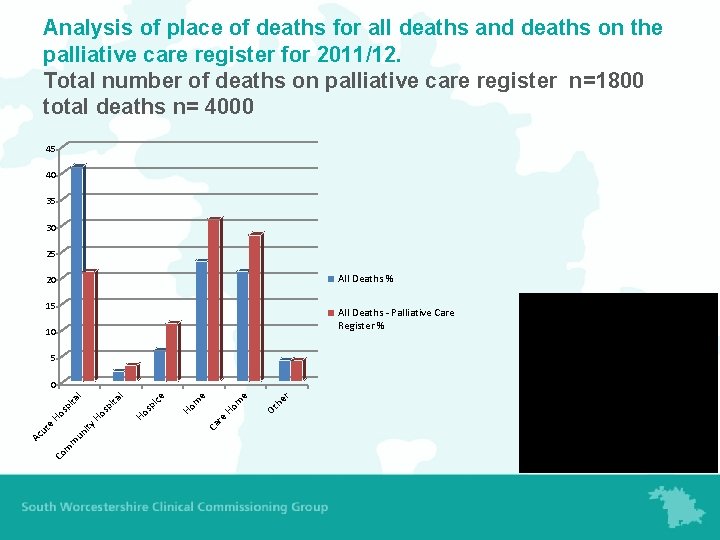
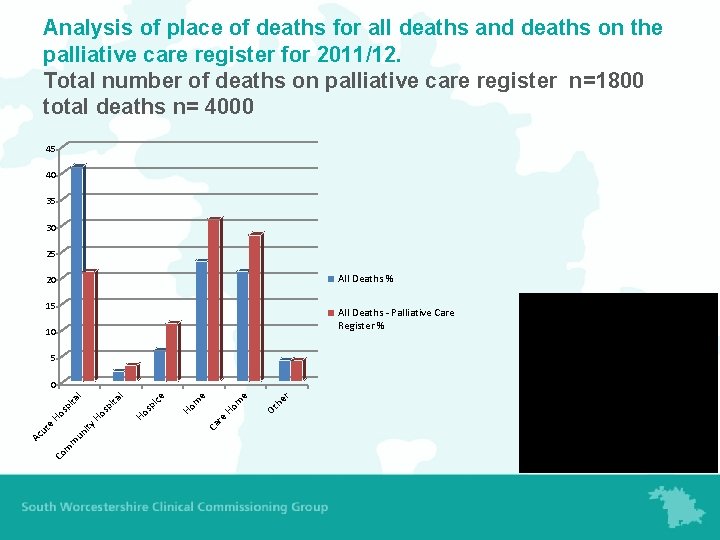
Analysis of place of deaths for all deaths and deaths on the palliative care register for 2011/12. Total number of deaths on palliative care register n=1800 total deaths n= 4000 45 40 35 30 25 All Deaths % 20 15 All Deaths - Palliative Care Register % 10 5 om H re Ca r Ot he e e m Ho ice sp Ho ita sp H o un ity m m Co Ac ut e Ho sp ita l l 0

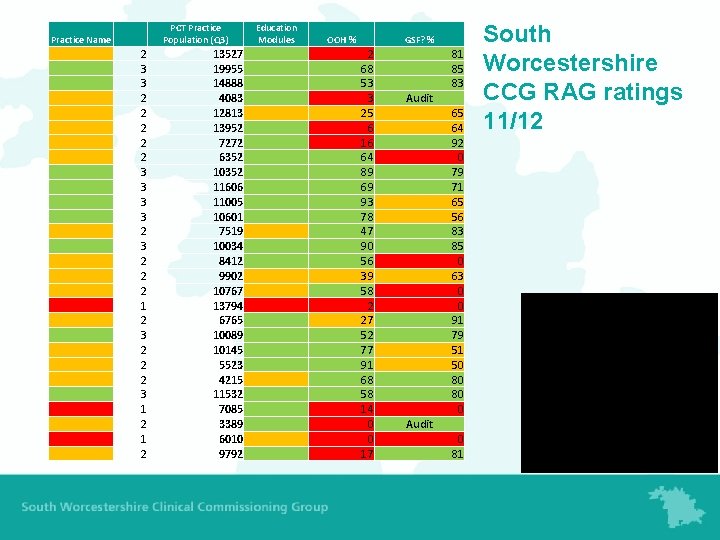
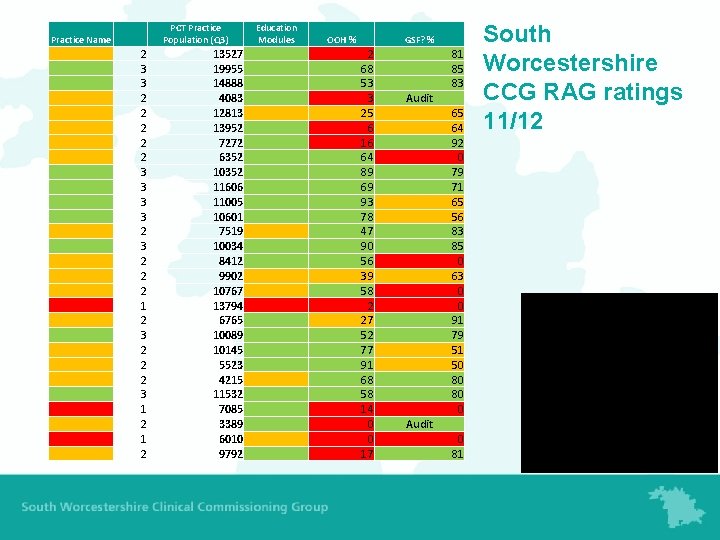
Practice Name PCT Practice Population (Q 3) 2 3 3 2 2 2 3 3 2 3 2 2 2 1 2 3 2 2 2 3 1 2 13527 19955 14888 4083 12813 13952 7272 6352 10352 11606 11005 10601 7519 10034 8412 9902 10767 13794 6765 10089 10145 5523 4215 11532 7085 3389 6010 9792 Education Modules OOH % GSF? % 2 68 53 3 25 6 16 64 89 69 93 78 47 90 56 39 58 2 27 52 77 91 68 58 14 0 0 17 81 85 83 Audit 65 64 92 0 79 71 65 56 83 85 0 63 0 0 91 79 51 50 80 80 0 Audit 0 81 South Worcestershire CCG RAG ratings 11/12

Wyre Forest CCG RAG ratings 11/12
Case Study 1 • 99 year old lady living in a lovely residential home for 8 years • Heart failure and breathless • Possible underlying diagnosis of Pulmonary fibrosis
Practical planning • • Discussion with the patient or relative Discussion with the home DNAR decision Advanced Care planning - Symptomatic treatment only - A ceiling on treatment - Full treatment options (palliative care register, just in case box) Communicate the plan
OOH Care • Bimonthly reviews of cases • Set KPI’s • Training module developed • Feedback to primary care and Ooh from reviews • Information fed into study days and two modules for all GP’s
Case Study 2 • Case 2 68 year old man with MND wanted to die at home, main fear was choking to death. Had an OOH form, DNAR, Just in case box. • OOH form read ‘patient has motor neurone disease, patient unable to speak and uses a text machine (i. Pad) to communicate increasing weakness in limbs.

Case Study 3 • 86 year old gentleman with bowel cancer wanting to die in his residential home. OOH form. • No Just in case box

Care Homes The National Audit Office report on End of Life Care (Nov 2008).

Care Homes • GSF surprise question • Rolling programme of education • Nursing home support nurses • Average life expectancy on entering a care home< 1 year

Using the evidence- Causes of death

Why is non cancer so difficult? • Patient Expectations • Lack of Consultant decision making • Holistic support • Recognised disease trajectory ‘How do you tell someone they are dying in a busy cardiology clinic in a 10 minute appointment when youare running late? ’
Innovation and new ways of working: The renal clinic When we started: • No clear pathway for patient support • All died in the acute trust At the end of the first year: • 27 patients with a mean age of 84 • 90% died in the community • Multidisciplinary support • Carers support and gentle advance care planning
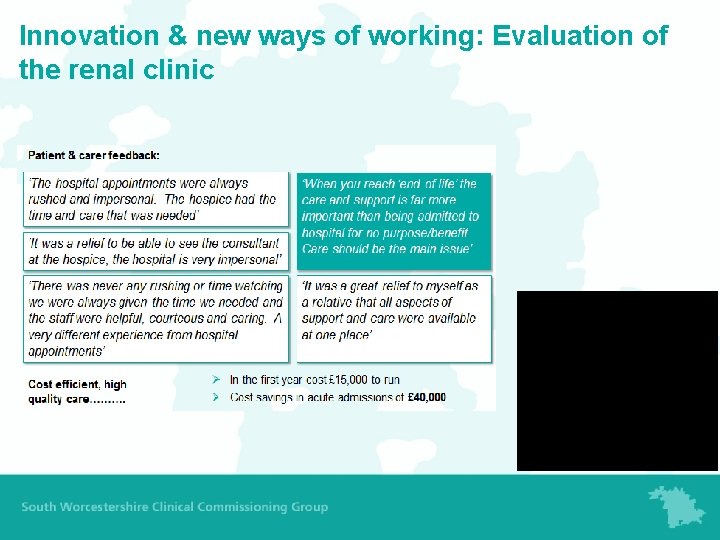
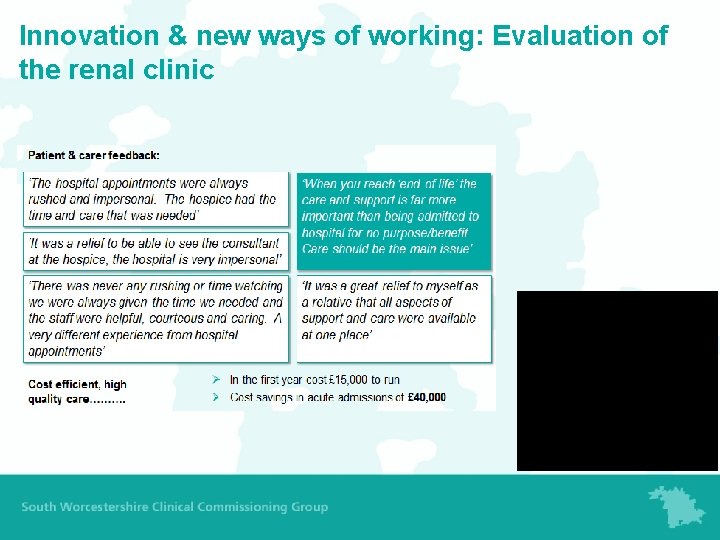
Innovation & new ways of working: Evaluation of the renal clinic
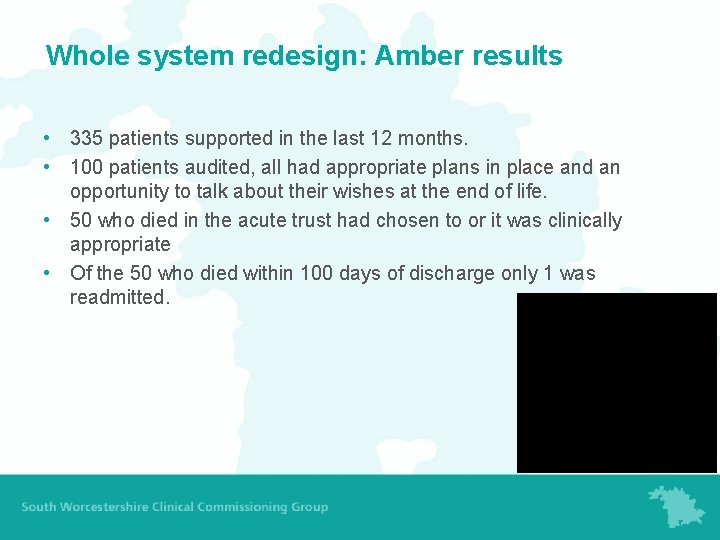
Whole systems redesign: Working with our Acute Trust • 2012/13 Amber care bundle in 12 wardsmore to follow. • Use by Health and care trust in community hospitals. • One of the first to pilot in the community. • Recognised nationally
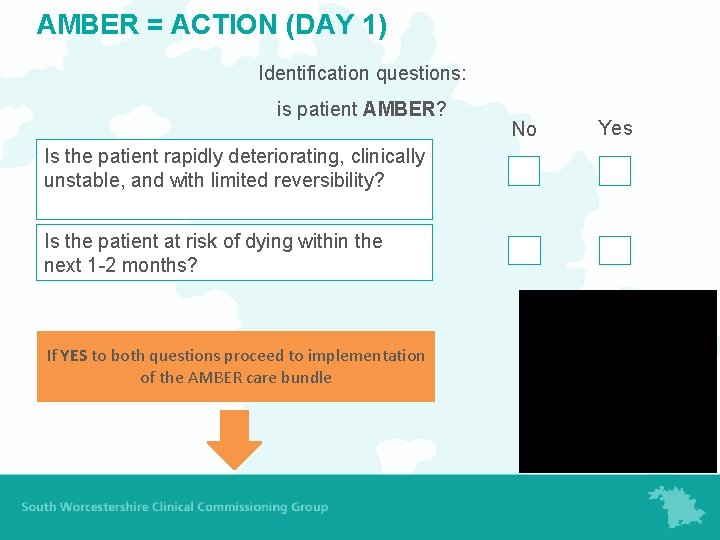
AMBER = Action • Assessment • Management • Best Practice • Engagement • Recovery uncertain
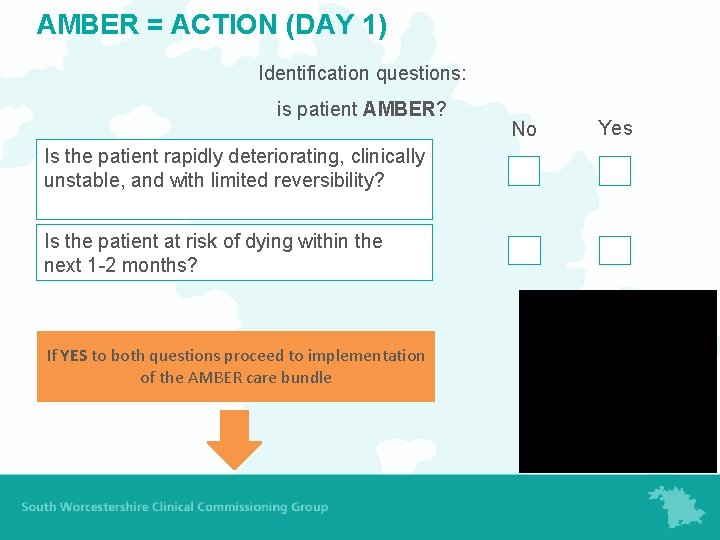
AMBER = ACTION (DAY 1) Identification questions: is patient AMBER? Is the patient rapidly deteriorating, clinically unstable, and with limited reversibility? Is the patient at risk of dying within the next 1 -2 months? If YES to both questions proceed to implementation of the AMBER care bundle No Yes

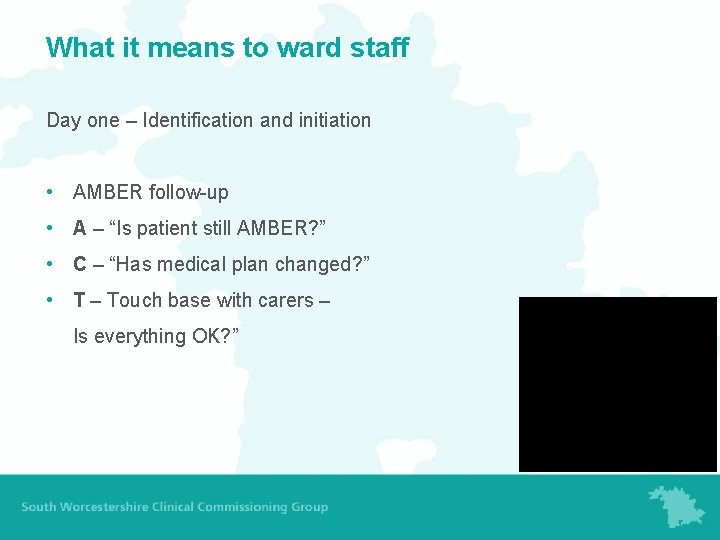
What it means to ward staff Day one – Identification and initiation • AMBER follow-up • A – “Is patient still AMBER? ” • C – “Has medical plan changed? ” • T – Touch base with carers – Is everything OK? ”
Whole system redesign: Amber results • 335 patients supported in the last 12 months. • 100 patients audited, all had appropriate plans in place and an opportunity to talk about their wishes at the end of life. • 50 who died in the acute trust had chosen to or it was clinically appropriate • Of the 50 who died within 100 days of discharge only 1 was readmitted.


Building on Success, planned investment 2012/13
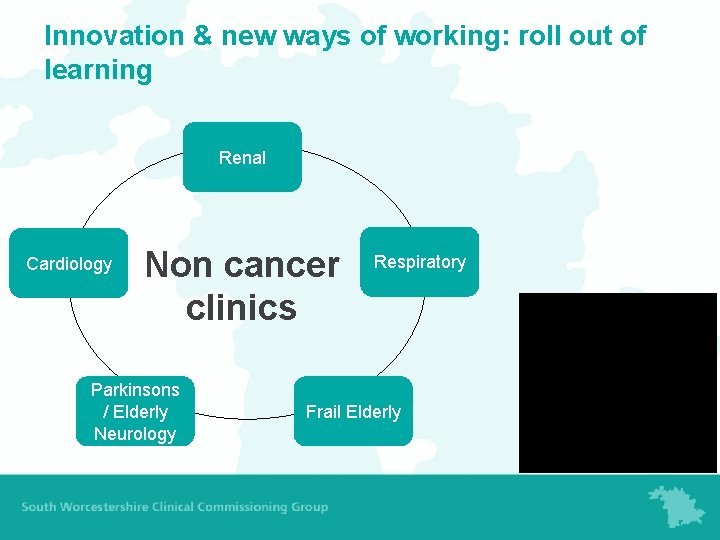
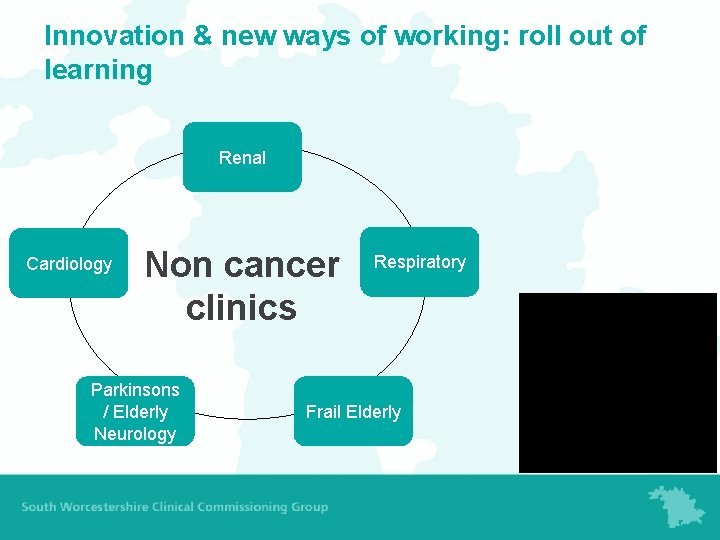
Innovation & new ways of working: roll out of learning Renal Cardiology Non cancer clinics Parkinsons / Elderly Neurology Respiratory Frail Elderly
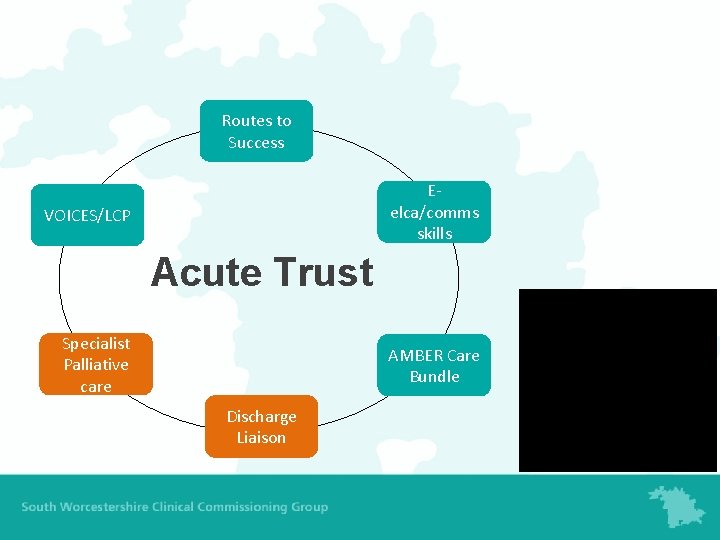
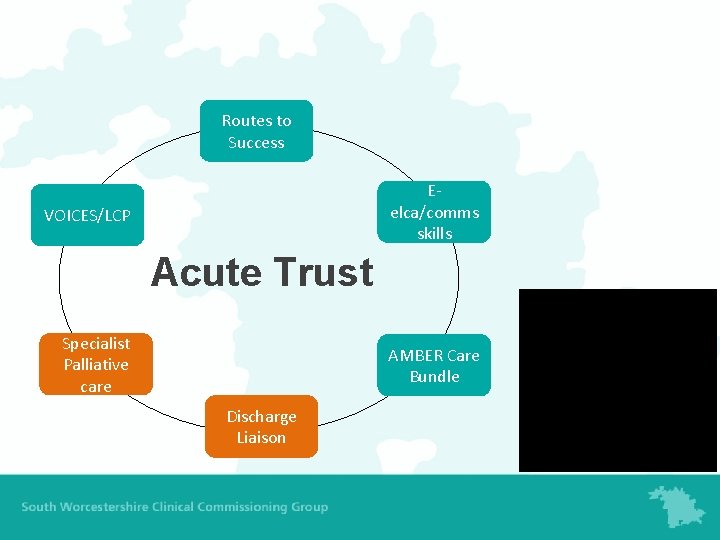
Routes to Success Eelca/comms skills VOICES/LCP Acute Trust Specialist Palliative care AMBER Care Bundle Discharge Liaison
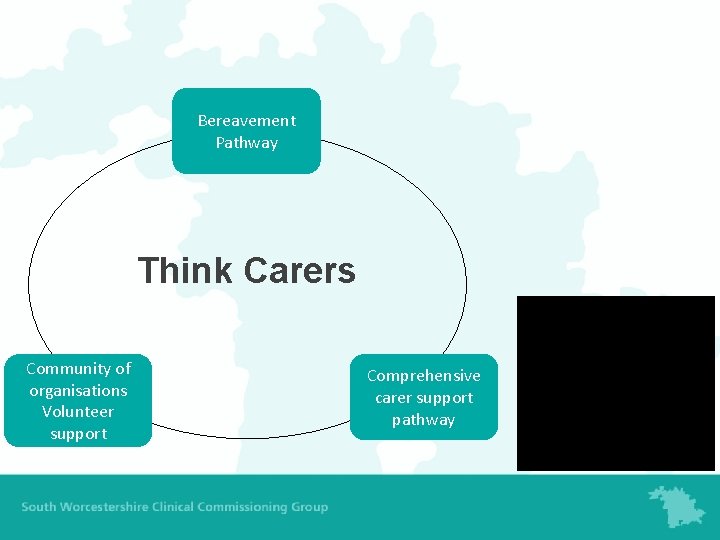
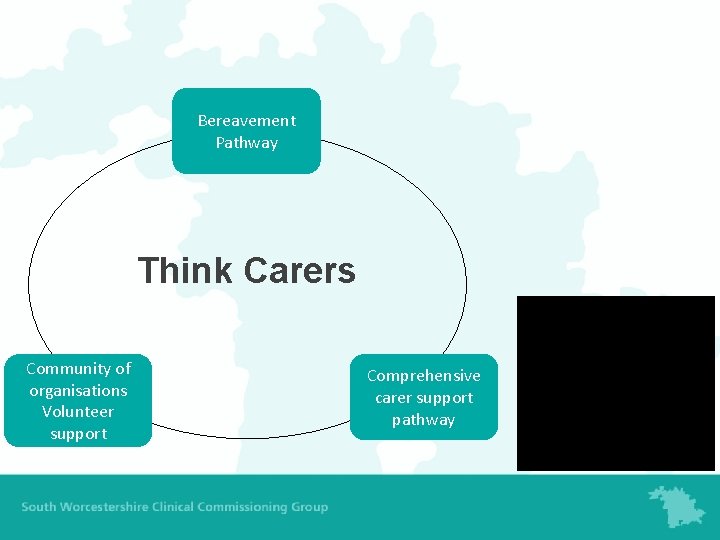
Bereavement Pathway Think Carers Community of organisations Volunteer support Comprehensive carer support pathway
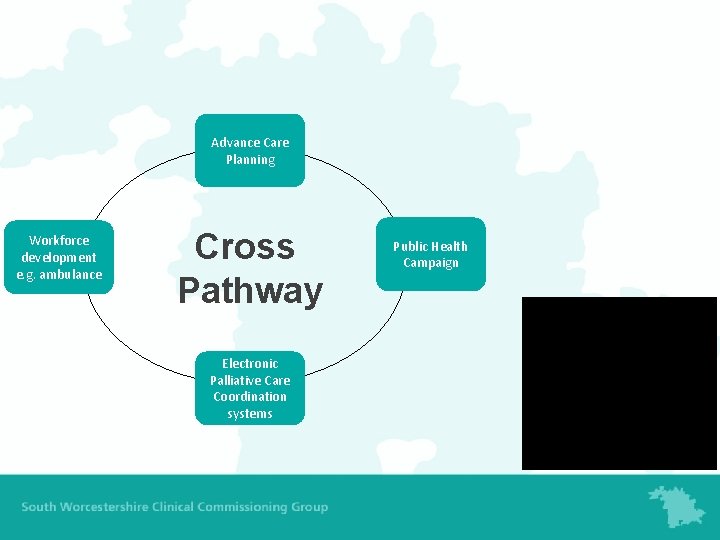
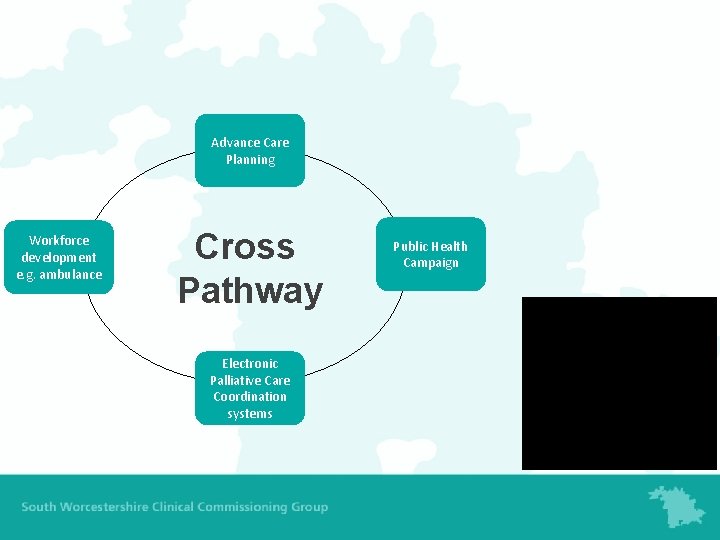
Advance Care Planning Workforce development e. g. ambulance Cross Pathway Electronic Palliative Care Coordination systems Public Health Campaign






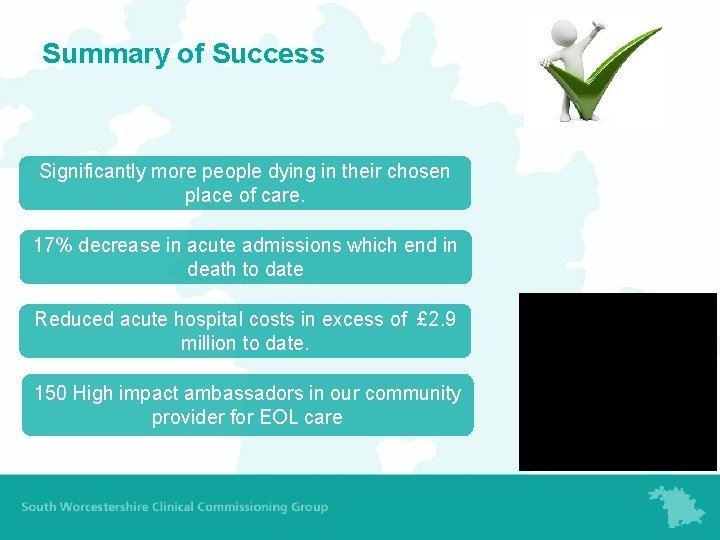
Summary of Success Significantly more people dying in their chosen place of care. 17% decrease in acute admissions which end in death to date Reduced acute hospital costs in excess of £ 2. 9 million to date. 150 High impact ambassadors in our community provider for EOL care
Thank you for watching! Please submit your name here to download your certificate.