A Balancing Act The Resident Panel Reassignment Process

A Balancing Act: The Resident Panel Reassignment Process At Academic Year-end STFM Annual Spring Conference April 26, 2012 Brian Arndt, MD Assistant Professor University of Wisconsin School of Medicine & Public Health
Session Objectives 1. Define various different types of handoffs in healthcare. 2. Discuss the importance of balance in resident panels. 3. Review some ways to adjust for patient complexity or comorbidity. 4. Discuss how to include complexity in a proposed algorithm for resident panel reassignment. 5. Review the logistics of an outpatient panel handoff from one resident to another.
What is a Handoff (Transition)? § Transfers of patient care & responsibility from one clinician/staff person (RNs, NP/PAs, MDs, PT/OT, etc) or care setting to another – Typically informal, unstructured, idiosyncratic – Synchronous: real-time interactive communication that allows for questioning between the giver & the receiver of patient information (in-person, over the phone, etc) – Asynchronous: not real time – desktop Excel doc, In. Basket message, phone call, etc)
To Err is Human § According to the Institute of Medicine, 44, 000 – 98, 000 deaths occur annually due to medical errors (November 1999) § Private & public purchasers, health care organizations, clinicians, & patients should work together to redesign health care processes (including transitions) § According to rule #6: § Safety as a system property. Patients should be safe from injury caused by the care system. Reducing risk & ensuring safety require greater attention to systems that help prevent & mitigate errors. Institute of Medicine. To Err is Human: Building a Safer Health System. http: //www. iom. edu/~/media/Files/Report%20 Files/1999/To-Err-is. Human/To%20 Err%20 is%20 Human%201999%20%20 report%20 brief. pdf
Handoff Errors are Common § Omission errors occur at a rate of 1 per every 100 – Most are content omissions § Failure prone communication – Failure in communication is more likely with absence of face-to-face communication processes § Faulty or inconsistent format is at the heart of most handoff problems Arora V, et al. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005; 14: 401 -407. Nolan TW. System changes to improve patient safety. BMJ. 2000; 320: 771 -773.
Handoff Requirements § The Joint Commission has mandated standardized approaches to handoff communications – JCAHO National Patient Safety Goal 2 E: All health care providers must “implement a standardized approach to handoff communications including an opportunity to ask & respond to questions. ” § The 2010 ACGME standards require that residents receive formal training in patient handoff communication – Resident faculty must monitor their residents’ patient handoffs to ensure that residents are competent in handoff communications The Joint Commission. Accreditation Standards. Oakbrook, IL: The Joint Commission; 2010. Nasca TJ, Day SH, Amis ES Jr; ACGME Duty Hour Taskforce. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010; 363: e 3.
Outpatient Panel Handoffs (vs. Inpatient Care Transitions) § Panel handoffs: – Clinician transitions (eg, leaving system) or patient transitions (insurance changes, peds to adult clinics, etc) • How difficult is it for you to interpret “signal” vs “noise” in internal & external record review? – Academic year-end transfers from one resident to another § Are there formal (synchronous or asynchronous) handoff processes for transferring panels in your practices?
Importance of Panel Balance § Educational experience – Need to balance multiple factors including age, acuity, payer mix, chronic conditions, etc … • 65+yo, 18 -65 yo with Medicare/MA, <3 yo, etc • DM, CHF, behavioral, social issues, etc • … while maintaining a high percent continuity – A difficult case mix could overwhelm a resident → ↑ patient risk while simultaneously preventing other residents from receiving experience managing difficult cases if not balanced appropriately – An easier case mix may not be challenging enough for a resident to truly appreciate how to help patients navigate the system
Importance of Panel Balance § ACGME minimum visit requirements: 1650 over 3 years – Must consider mental demands – can’t have all patients that require “extra time” vs only seeing urgent care visits to meet those requirements § Patient safety – continuum of experience – R 1 vs R 3 ability to manage complexity? § Clinical support / team structure § Faculty capacity to provide oversight § Impact on faculty compensation – Pay for performance § Others?
Current reassignment process… § “R 3 s: Here are your current patient lists. Let us know who you would like them reassigned to after you graduate. We will reassign those you don’t specify. ” – Some residents do not specify any … – Do the residents really know (all? ) patients? – Do they attempt to keep patients on the same team or with the same provider gender (if patient has a preference) as previous?

Current reassignment process… § continued from previous … – Do panels get more unbalanced over time due to certain clinical interests? • • • MD vs DO (eg, MSK/sports) Specific interests (eg, womens health, DM groups) Practice style (eg, “pushover” for controlled meds) Clinician gender (eg, female clinician w/80% females) Others? – Do incoming R 1 s get included or do they get whoever is left? • How do we ensure spread of complexity across the continuum of learning?

Original Reassignment Lists
Are there ways to remind the current resident PCP about characteristics of each individual patient in a summary format on the patient lists to be used when reassigning patients to another resident PCP? Is so, what characteristics would you show them?
How about complexity? § Our original reassignment process only adjusted for the following: – Age (0 -3, 4 -14, 15 -39, 40 -59, 60 -74, ≥ 75) – Sex – Payer § Original process did not account for: – Frequency of non-office visit encounters – Chronic conditions – Other demographics (ie, homelessness, interpreter needs, etc)
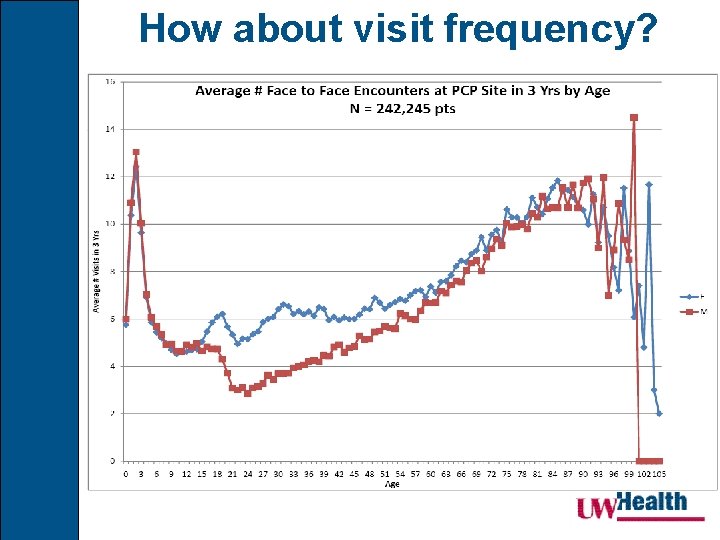
How about visit frequency?
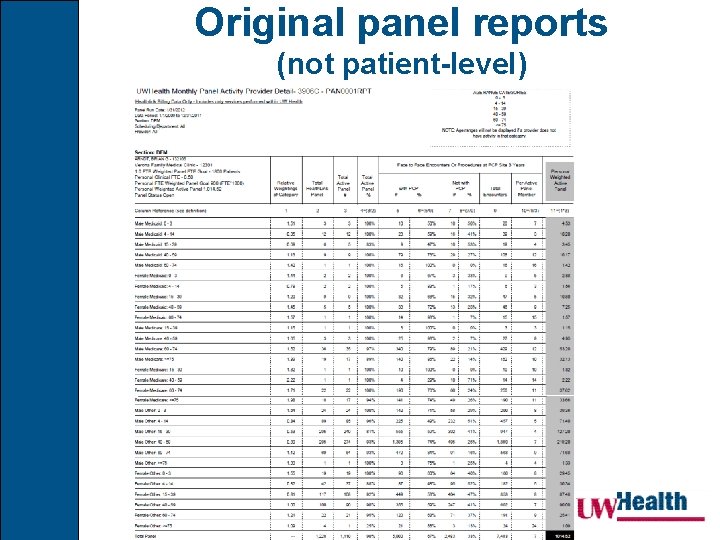
Original panel reports (not patient-level)
Panel balancing: It makes sense to include age, sex, payer, visit frequency, & clinically complex conditions. But what clinic conditions matter? Acute or chronic, major or minor, etc?
Which diagnoses? § Charlson Comorbidity Index (1987 …) – Predicts 10 year mortality based on presence of 18 different comorbidities – Each condition = 1, 2, 3 or 6 depending on risk of dying associated with the condition: • 1: MI, CHF, PVD, dementia, CVD, chronic lung disease, connective tissue disease, ulcer, chronic liver disease • 2: Hemiplegia, CKD, diabetes, tumor, leukemia, lymphoma • 3: Moderate or severe liver disease • 6: Malignant tumor, metastasis, AIDS – Charlson does not account for other conditions … Charlson ME, Pompei P, Ales KL, Mac. Kenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5): 373 -83.
Accounting for all diagnoses? § AHRQ’s Clinical Classifications Software (CCS) – A tool for clustering patient diagnoses and procedures into a manageable number of clinically meaningful categories – Researchers use CCS in risk adjustment models and as a way to predict future health resource utilization – Available for downloading http: //www. hcup-us. ahrq. gov/toolssoftware/ccsfactsheet. jsp
Adjusting for diagnoses § Diagnostic-based risk-adjustment systems (DBRAS) – Allows for comparisons between patients that may differ significantly in terms of their overall health (morbidity burden) – Can be used to estimate future expenses for groups of people with same age and sex and similar diagnosis mix (conditions) – Can be used to identify high-cost patients for case management – Could a DBRAS be useful in the resident patient reassignment process? Berlinguet M, Preyra M, Dean M. Comparing the Value of Three Main Diagnostic-Based Risk-Adjustment Systems (DBRAS). Canadian Health Services Research Foundation. http: //www. chsrf. ca/Migrated/PDF/Research. Reports/OGC/berlinguet_e. pdf
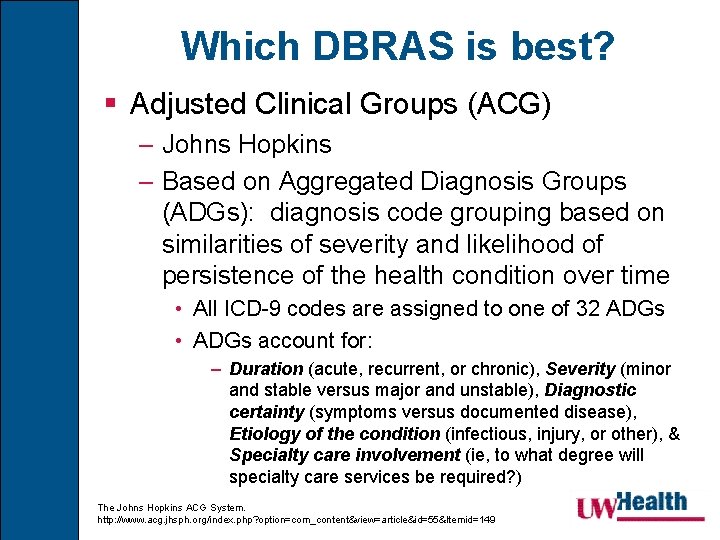
Which DBRAS is best? § Adjusted Clinical Groups (ACG) – Johns Hopkins – Based on Aggregated Diagnosis Groups (ADGs): diagnosis code grouping based on similarities of severity and likelihood of persistence of the health condition over time • All ICD-9 codes are assigned to one of 32 ADGs • ADGs account for: – Duration (acute, recurrent, or chronic), Severity (minor and stable versus major and unstable), Diagnostic certainty (symptoms versus documented disease), Etiology of the condition (infectious, injury, or other), & Specialty care involvement (ie, to what degree will specialty care services be required? ) The Johns Hopkins ACG System. http: //www. acg. jhsph. org/index. php? option=com_content&view=article&id=55&Itemid=149
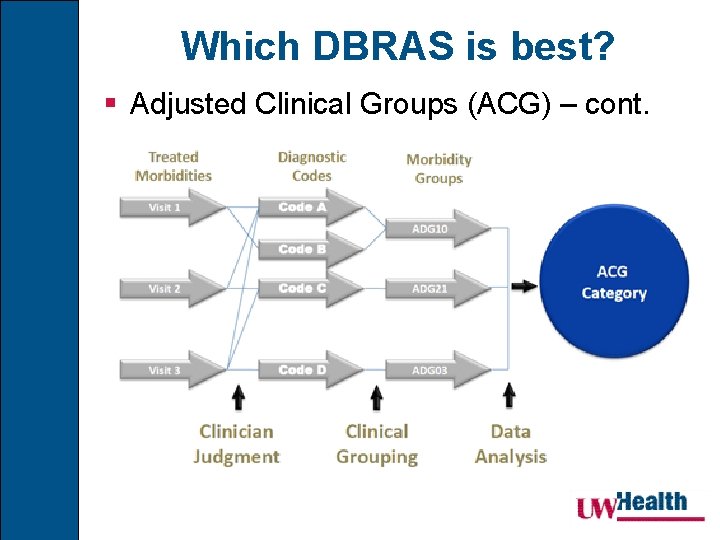
Which DBRAS is best? § Adjusted Clinical Groups (ACG) – cont.
Which DBRAS is best? § Adjusted Clinical Groups (ACG) – cont. – Individuals may have >one ADG → one ACG – ACG methodology places people into one of 102 discrete categories based on their assigned ADGs, age, and sex – Individuals within a given ACG have a similar pattern of morbidity and resource use over the course of a given year – ACGs outperform age and sex adjustment alone, which has been the traditional riskadjustment mechanism used within the health insurance industry The Johns Hopkins ACG System. http: //www. acg. jhsph. org/index. php? option=com_content&view=article&id=55&Itemid=149
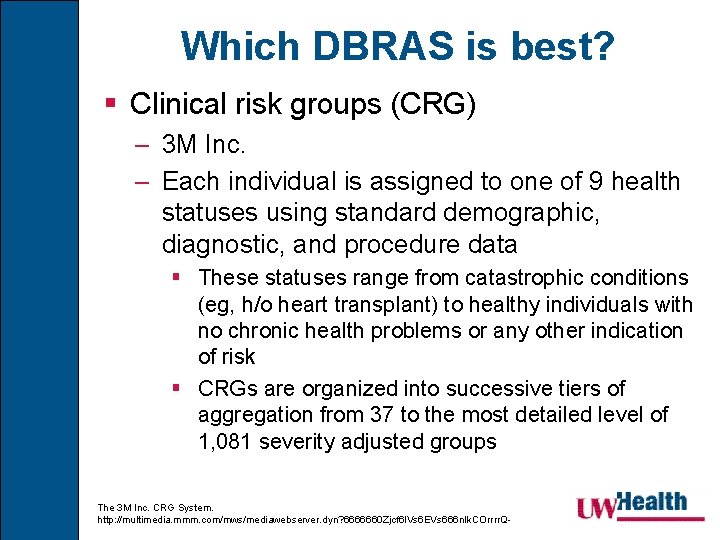
Which DBRAS is best? § Clinical risk groups (CRG) – 3 M Inc. – Each individual is assigned to one of 9 health statuses using standard demographic, diagnostic, and procedure data § These statuses range from catastrophic conditions (eg, h/o heart transplant) to healthy individuals with no chronic health problems or any other indication of risk § CRGs are organized into successive tiers of aggregation from 37 to the most detailed level of 1, 081 severity adjusted groups The 3 M Inc. CRG System. http: //multimedia. mmm. com/mws/mediawebserver. dyn? 6666660 Zjcf 6 l. Vs 6 EVs 666 n. Ik. COrrrr. Q-
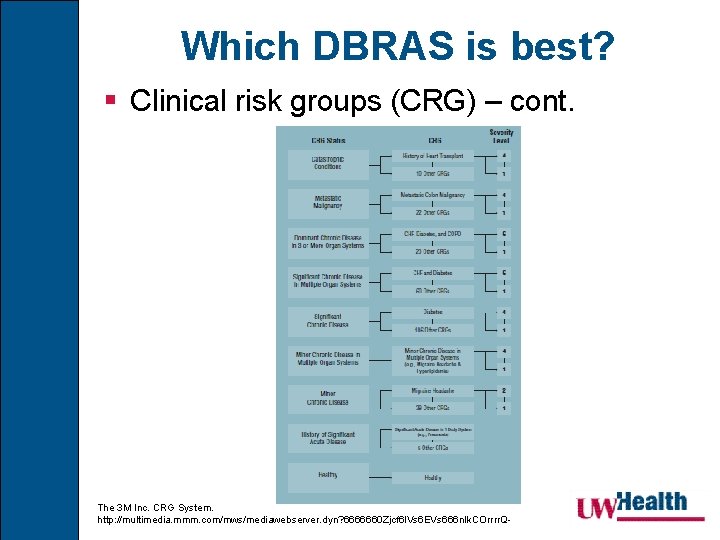
Which DBRAS is best? § Clinical risk groups (CRG) – cont. The 3 M Inc. CRG System. http: //multimedia. mmm. com/mws/mediawebserver. dyn? 6666660 Zjcf 6 l. Vs 6 EVs 666 n. Ik. COrrrr. Q-
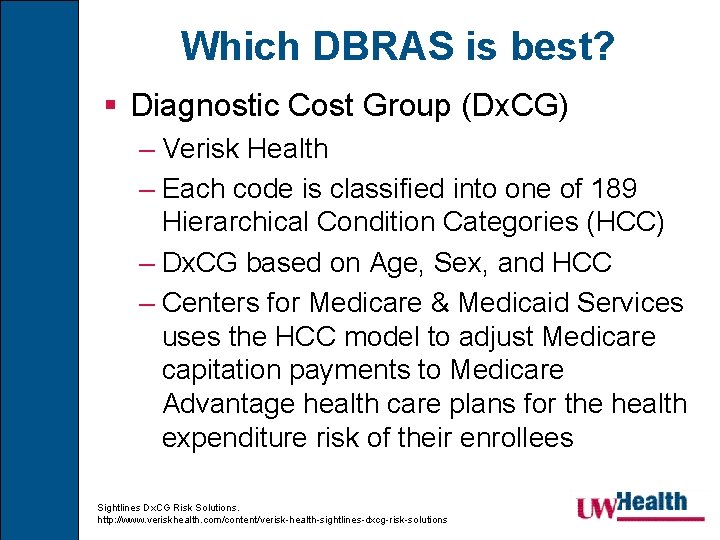
Which DBRAS is best? § Diagnostic Cost Group (Dx. CG) – Verisk Health – Each code is classified into one of 189 Hierarchical Condition Categories (HCC) – Dx. CG based on Age, Sex, and HCC – Centers for Medicare & Medicaid Services uses the HCC model to adjust Medicare capitation payments to Medicare Advantage health care plans for the health expenditure risk of their enrollees Sightlines Dx. CG Risk Solutions. http: //www. veriskhealth. com/content/verisk-health-sightlines-dxcg-risk-solutions
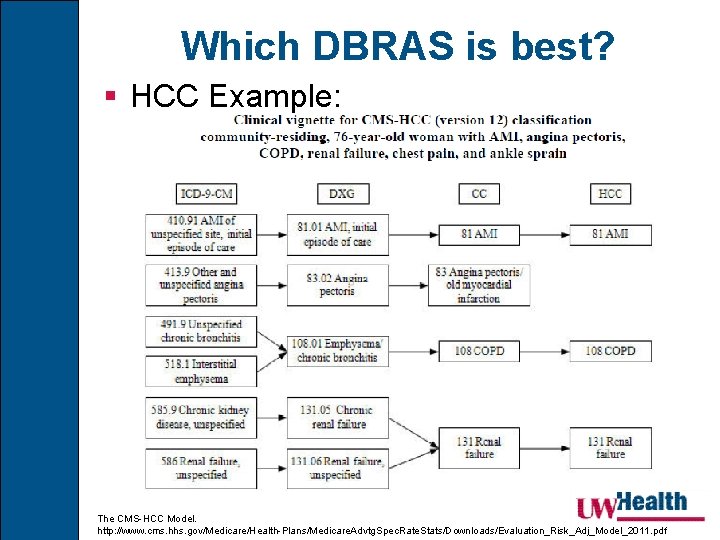
Which DBRAS is best? § HCC Example: The CMS-HCC Model. http: //www. cms. hhs. gov/Medicare/Health-Plans/Medicare. Advtg. Spec. Rate. Stats/Downloads/Evaluation_Risk_Adj_Model_2011. pdf
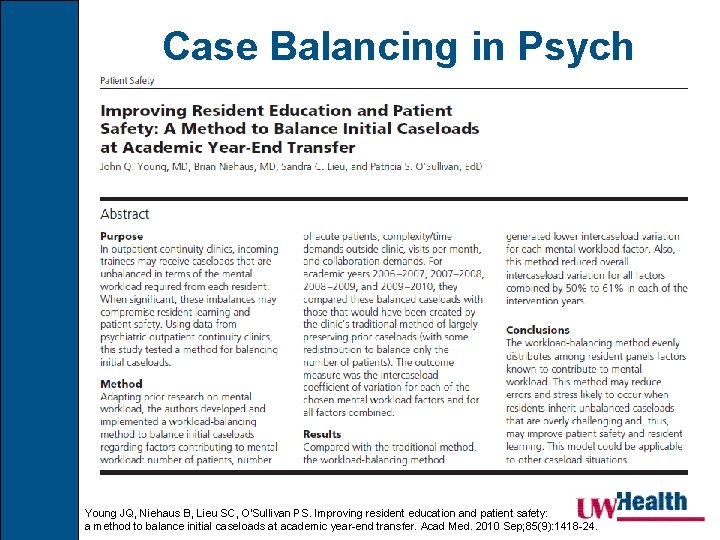
Case Balancing in Psych Young JQ, Niehaus B, Lieu SC, O'Sullivan PS. Improving resident education and patient safety: a method to balance initial caseloads at academic year-end transfer. Acad Med. 2010 Sep; 85(9): 1418 -24.
So how should family medicine residencies balance patient panels? § … and what is our baseline balance? (or more likely lack of balance? …) – Are our panels balanced in size? – Are our panels balanced in complexity? – When does the balancing occur/recur? • Academic year-end? • Should it also happen in mid-academic year sometime to ensure balance is maintained?
Where are UW residents?
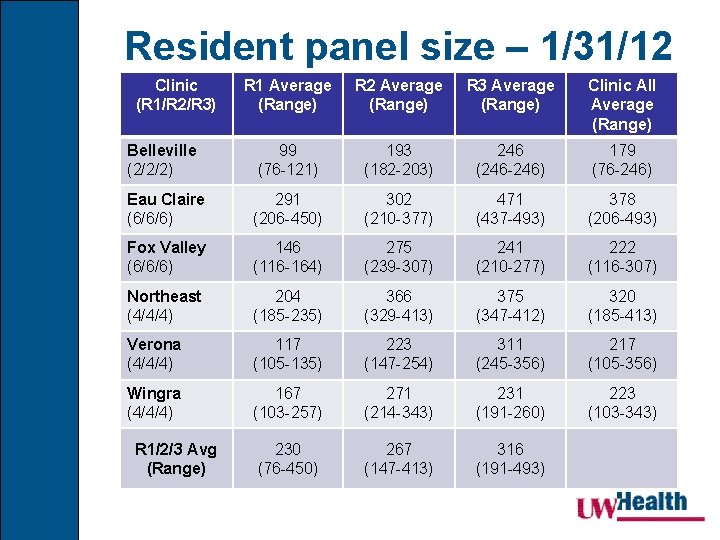
Resident panel size – 1/31/12 Clinic (R 1/R 2/R 3) R 1 Average (Range) R 2 Average (Range) R 3 Average (Range) Clinic All Average (Range) Belleville (2/2/2) 99 (76 -121) 193 (182 -203) 246 (246 -246) 179 (76 -246) Eau Claire (6/6/6) 291 (206 -450) 302 (210 -377) 471 (437 -493) 378 (206 -493) Fox Valley (6/6/6) 146 (116 -164) 275 (239 -307) 241 (210 -277) 222 (116 -307) Northeast (4/4/4) 204 (185 -235) 366 (329 -413) 375 (347 -412) 320 (185 -413) Verona (4/4/4) 117 (105 -135) 223 (147 -254) 311 (245 -356) 217 (105 -356) Wingra (4/4/4) 167 (103 -257) 271 (214 -343) 231 (191 -260) 223 (103 -343) 230 (76 -450) 267 (147 -413) 316 (191 -493) R 1/2/3 Avg (Range)
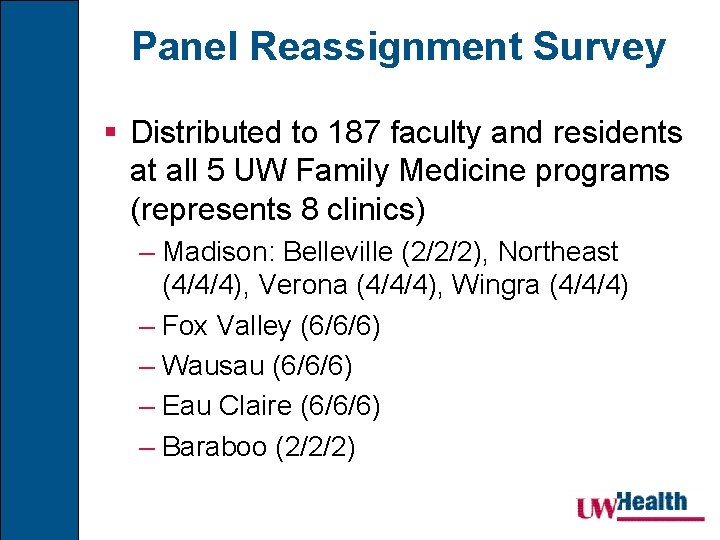
Panel Reassignment Survey § Distributed to 187 faculty and residents at all 5 UW Family Medicine programs (represents 8 clinics) – Madison: Belleville (2/2/2), Northeast (4/4/4), Verona (4/4/4), Wingra (4/4/4) – Fox Valley (6/6/6) – Wausau (6/6/6) – Eau Claire (6/6/6) – Baraboo (2/2/2)
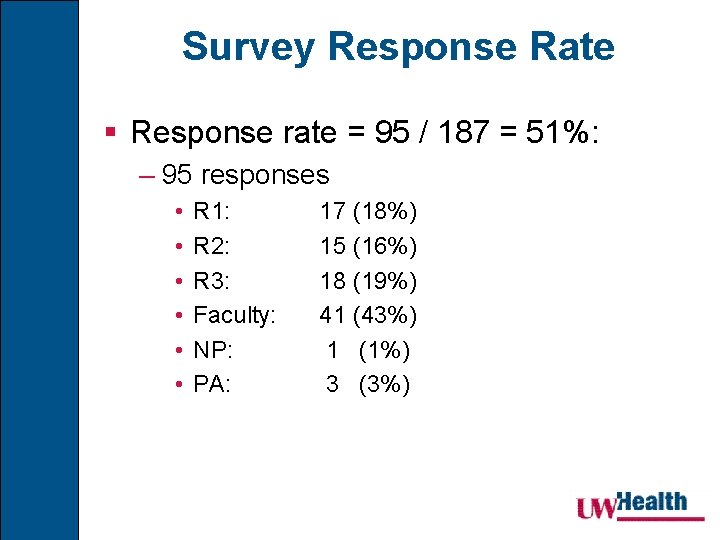
Survey Response Rate § Response rate = 95 / 187 = 51%: – 95 responses • • • R 1: R 2: R 3: Faculty: NP: PA: 17 (18%) 15 (16%) 18 (19%) 41 (43%) 1 (1%) 3 (3%)
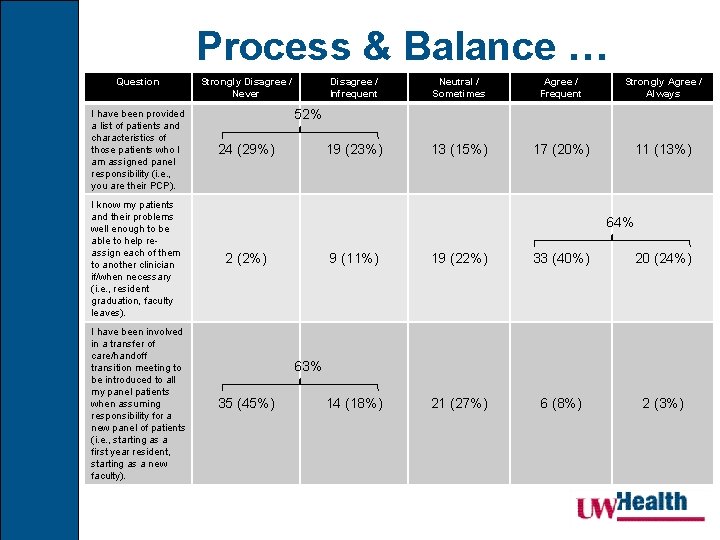
Process & Balance … Question I have been provided a list of patients and characteristics of those patients who I am assigned panel responsibility (i. e. , you are their PCP). I know my patients and their problems well enough to be able to help reassign each of them to another clinician if/when necessary (i. e. , resident graduation, faculty leaves). I have been involved in a transfer of care/handoff transition meeting to be introduced to all my panel patients when assuming responsibility for a new panel of patients (i. e. , starting as a first year resident, starting as a new faculty). Strongly Disagree / Never Disagree / Infrequent Neutral / Sometimes Agree / Frequent Strongly Agree / Always 19 (23%) 13 (15%) 17 (20%) 11 (13%) 52% 24 (29%) 64% 2 (2%) 9 (11%) 19 (22%) 33 (40%) 20 (24%) 14 (18%) 21 (27%) 6 (8%) 2 (3%) 63% 35 (45%)
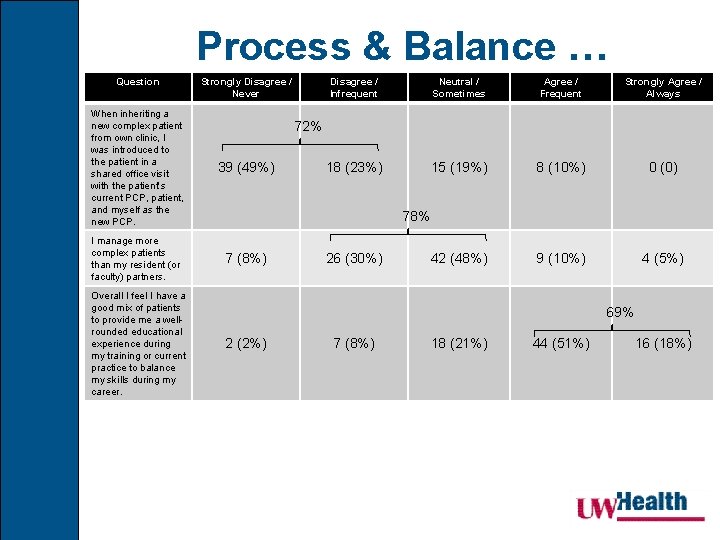
Process & Balance … Question Strongly Disagree / Never When inheriting a new complex patient from own clinic, I was introduced to the patient in a shared office visit with the patient’s current PCP, patient, and myself as the new PCP. 39 (49%) I manage more complex patients than my resident (or faculty) partners. 7 (8%) Overall I feel I have a good mix of patients to provide me a wellrounded educational experience during my training or current practice to balance my skills during my career. Disagree / Infrequent Neutral / Sometimes Agree / Frequent Strongly Agree / Always 18 (23%) 15 (19%) 8 (10%) 0 (0) 42 (48%) 9 (10%) 4 (5%) 72% 78% 26 (30%) 69% 2 (2%) 7 (8%) 18 (21%) 44 (51%) 16 (18%)
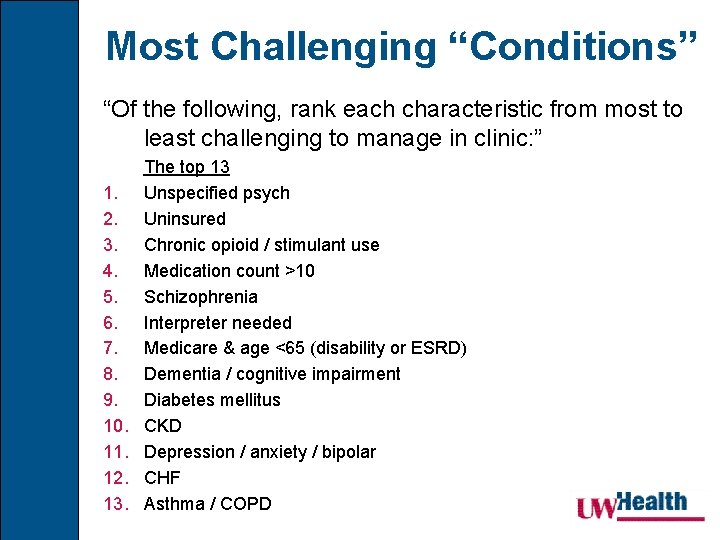
Most Challenging “Conditions” “Of the following, rank each characteristic from most to least challenging to manage in clinic: ” 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. The top 13 Unspecified psych Uninsured Chronic opioid / stimulant use Medication count >10 Schizophrenia Interpreter needed Medicare & age <65 (disability or ESRD) Dementia / cognitive impairment Diabetes mellitus CKD Depression / anxiety / bipolar CHF Asthma / COPD
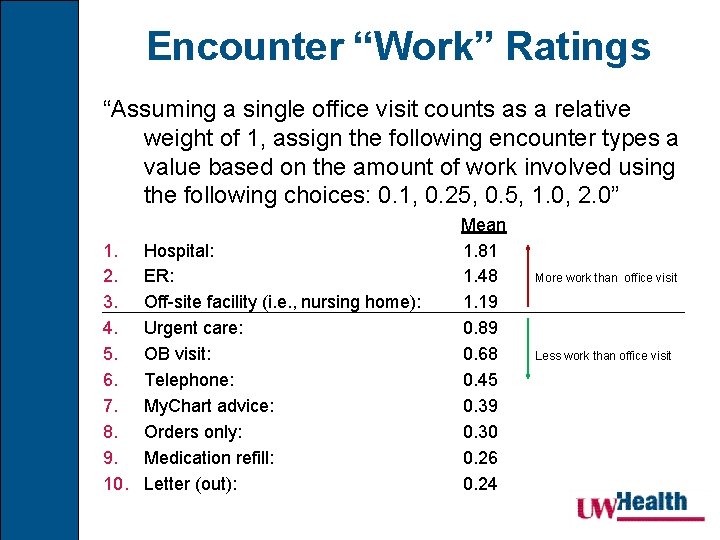
Encounter “Work” Ratings “Assuming a single office visit counts as a relative weight of 1, assign the following encounter types a value based on the amount of work involved using the following choices: 0. 1, 0. 25, 0. 5, 1. 0, 2. 0” 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Hospital: ER: Off-site facility (i. e. , nursing home): Urgent care: OB visit: Telephone: My. Chart advice: Orders only: Medication refill: Letter (out): Mean 1. 81 1. 48 1. 19 0. 89 0. 68 0. 45 0. 39 0. 30 0. 26 0. 24 More work than office visit Less work than office visit
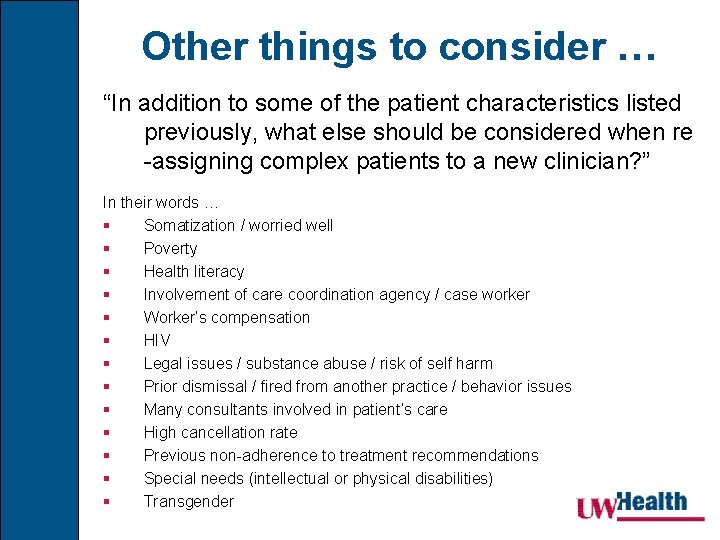
Other things to consider … “In addition to some of the patient characteristics listed previously, what else should be considered when re -assigning complex patients to a new clinician? ” In their words … § Somatization / worried well § Poverty § Health literacy § Involvement of care coordination agency / case worker § Worker’s compensation § HIV § Legal issues / substance abuse / risk of self harm § Prior dismissal / fired from another practice / behavior issues § Many consultants involved in patient’s care § High cancellation rate § Previous non-adherence to treatment recommendations § Special needs (intellectual or physical disabilities) § Transgender
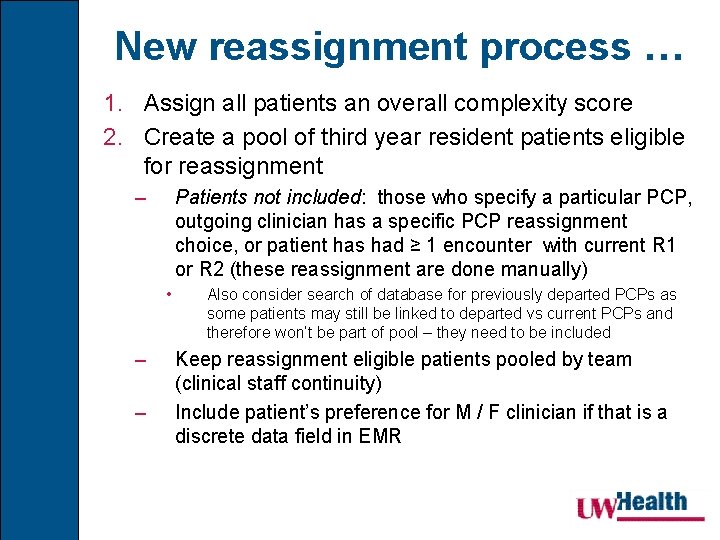
New reassignment process … 1. Assign all patients an overall complexity score 2. Create a pool of third year resident patients eligible for reassignment – Patients not included: those who specify a particular PCP, outgoing clinician has a specific PCP reassignment choice, or patient has had ≥ 1 encounter with current R 1 or R 2 (these reassignment are done manually) • – – Also consider search of database for previously departed PCPs as some patients may still be linked to departed vs current PCPs and therefore won’t be part of pool – they need to be included Keep reassignment eligible patients pooled by team (clinical staff continuity) Include patient’s preference for M / F clinician if that is a discrete data field in EMR
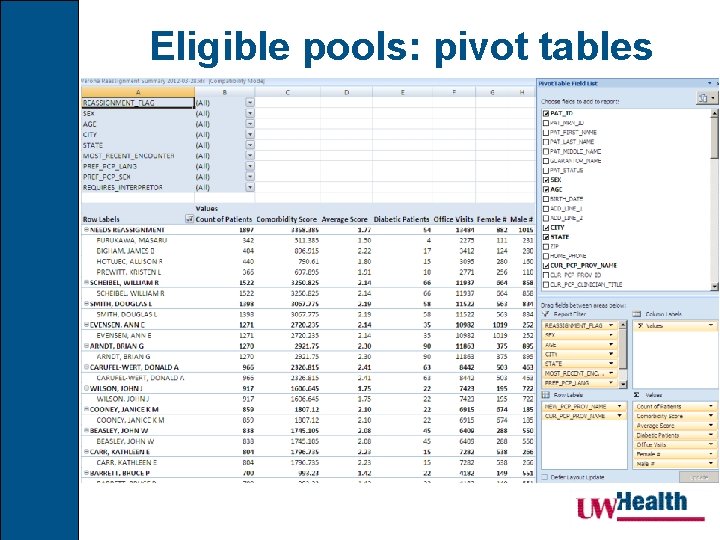
Eligible pools: pivot tables
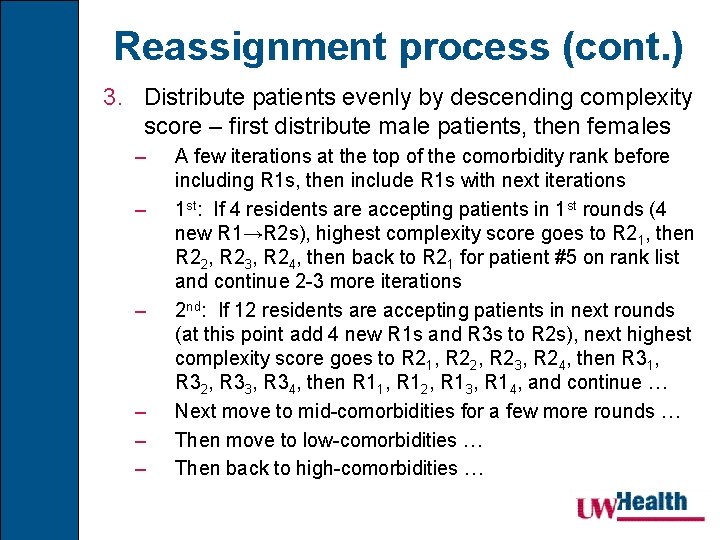
Reassignment process (cont. ) 3. Distribute patients evenly by descending complexity score – first distribute male patients, then females – – – A few iterations at the top of the comorbidity rank before including R 1 s, then include R 1 s with next iterations 1 st: If 4 residents are accepting patients in 1 st rounds (4 new R 1→R 2 s), highest complexity score goes to R 21, then R 22, R 23, R 24, then back to R 21 for patient #5 on rank list and continue 2 -3 more iterations 2 nd: If 12 residents are accepting patients in next rounds (at this point add 4 new R 1 s and R 3 s to R 2 s), next highest complexity score goes to R 21, R 22, R 23, R 24, then R 31, R 32, R 33, R 34, then R 11, R 12, R 13, R 14, and continue … Next move to mid-comorbidities for a few more rounds … Then move to low-comorbidities … Then back to high-comorbidities …

Comorbidity Ranking
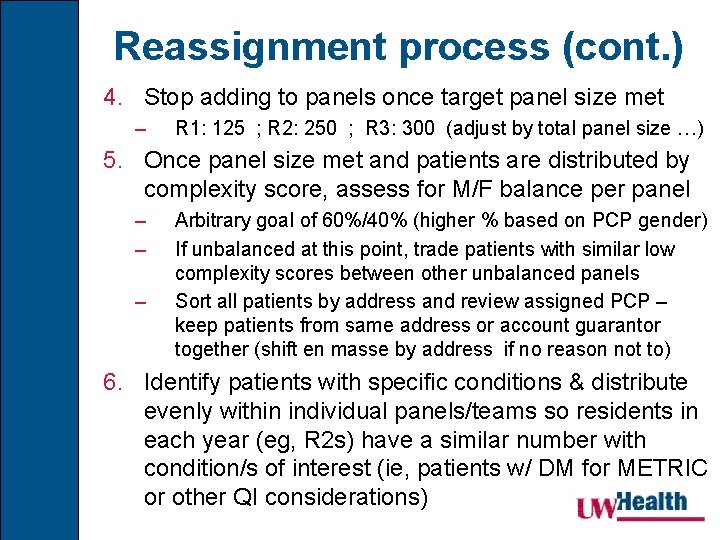
Reassignment process (cont. ) 4. Stop adding to panels once target panel size met – R 1: 125 ; R 2: 250 ; R 3: 300 (adjust by total panel size …) 5. Once panel size met and patients are distributed by complexity score, assess for M/F balance per panel – – – Arbitrary goal of 60%/40% (higher % based on PCP gender) If unbalanced at this point, trade patients with similar low complexity scores between other unbalanced panels Sort all patients by address and review assigned PCP – keep patients from same address or account guarantor together (shift en masse by address if no reason not to) 6. Identify patients with specific conditions & distribute evenly within individual panels/teams so residents in each year (eg, R 2 s) have a similar number with condition/s of interest (ie, patients w/ DM for METRIC or other QI considerations)
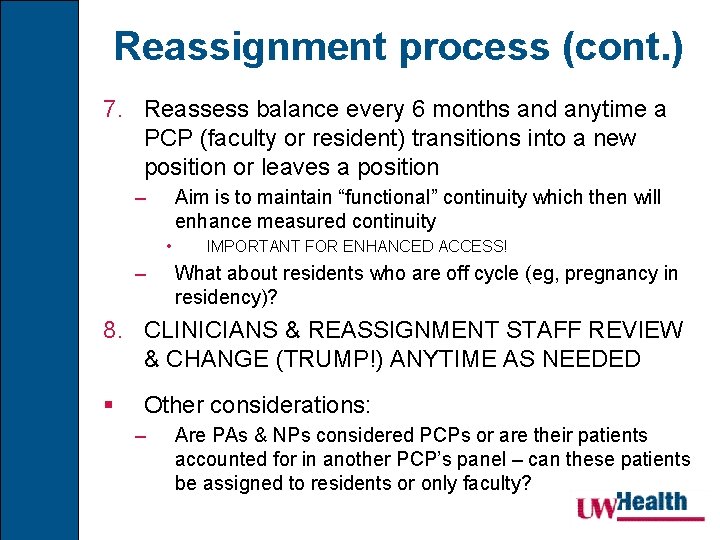
Reassignment process (cont. ) 7. Reassess balance every 6 months and anytime a PCP (faculty or resident) transitions into a new position or leaves a position – Aim is to maintain “functional” continuity which then will enhance measured continuity • – IMPORTANT FOR ENHANCED ACCESS! What about residents who are off cycle (eg, pregnancy in residency)? 8. CLINICIANS & REASSIGNMENT STAFF REVIEW & CHANGE (TRUMP!) ANYTIME AS NEEDED § Other considerations: – Are PAs & NPs considered PCPs or are their patients accounted for in another PCP’s panel – can these patients be assigned to residents or only faculty?
Outpatient Handoff Challenges § Minimal training devoted to transitions (Reiss & Gibson, 2002) § Transfers can trigger emotions of grief, guilt, anger, anxiety, & fear for patients (De. Witt & Roberts, 1995) § Patients anticipating transitions may avoid closeness with the physician (Serwint & Johnson, 1995) § Clinicians are unable to accurately identify the patients who will have a difficult time with transfers (De. Witt & Roberts, 1995)
Handoff Curriculum? (mainly inpatient focus …) Wohlauer MV, Arora VM, Horwitz LI, Bass EJ, Mahar SE, Philibert I, for the Handoff Education and Assessment for Residents (HEAR) Computer Supported Cooperative Workgroup. The Patient Handoff: A Comprehensive Curricular Blueprint for Resident Education to Improve Continuity of Care. Acad Med. 2012 Apr; 87(4): 411 -418.
Handoff best practices to transfer relationships! § Face-to-face dialogue is best! § Identify the patient and discuss: – Pertinent background information including necessary psychosocial information – Major clinical problems & status of each • Relevant & up-to-date data • Anticipated problems (ie, history of non-adherence, frequently cancels follow ups) § Allow for interactive questioning § Ask for verification – summarize & read back § Minimize disruptions
Outpatient Panel Handoffs § Outgoing residents need training on how to: – Identify patients who need additional case management &/or priority scheduling • Improves patient & clinician satisfaction along with enhancing patient safety – Educate patients about the transfer, – Address the loss (changing clinician) & its meaning, – Plan for any anticipated problems, & – Introduce (sell? ) patients to their new clinician
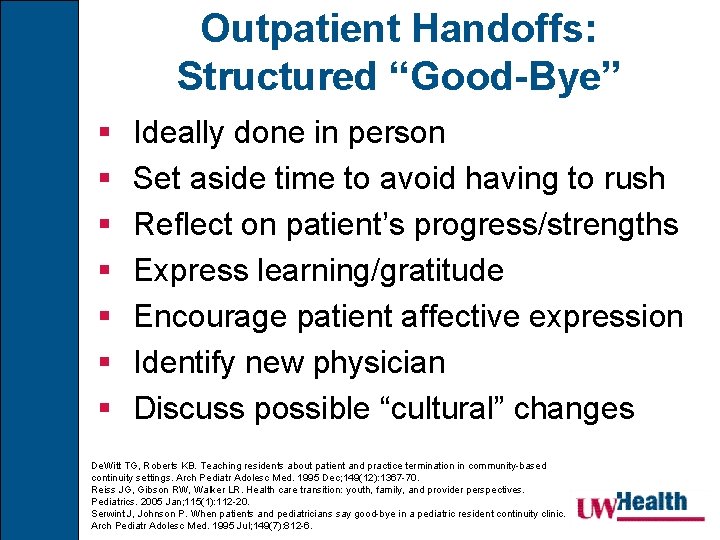
Outpatient Handoffs: Structured “Good-Bye” § § § § Ideally done in person Set aside time to avoid having to rush Reflect on patient’s progress/strengths Express learning/gratitude Encourage patient affective expression Identify new physician Discuss possible “cultural” changes De. Witt TG, Roberts KB. Teaching residents about patient and practice termination in community-based continuity settings. Arch Pediatr Adolesc Med. 1995 Dec; 149(12): 1367 -70. Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005 Jan; 115(1): 112 -20. Serwint J, Johnson P. When patients and pediatricians say good-bye in a pediatric resident continuity clinic. Arch Pediatr Adolesc Med. 1995 Jul; 149(7): 812 -6.
Outpatient Panel Handoffs § Incoming residents need training on how to: – Establish new therapeutic relationships including how to address the patient’s relationship with previous PCP (eg, what did/did not work well), & • Elicit expectations for new relationship, • Establish goals, – How can the whole care team be informed once new goals are established?
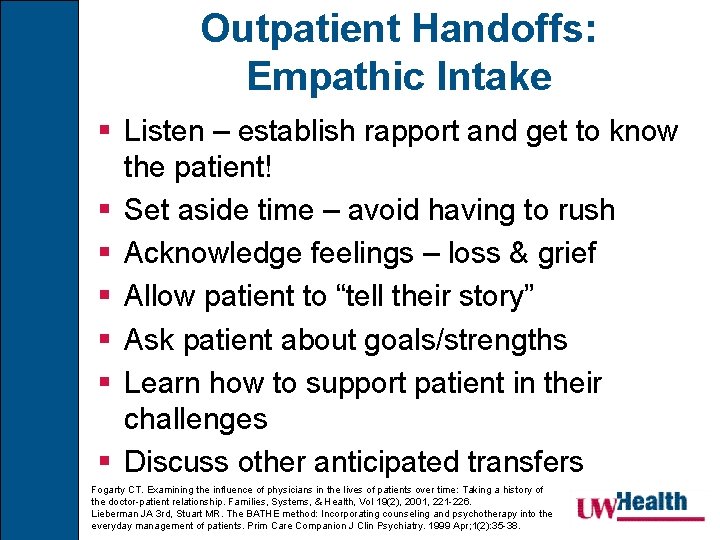
Outpatient Handoffs: Empathic Intake § Listen – establish rapport and get to know the patient! § Set aside time – avoid having to rush § Acknowledge feelings – loss & grief § Allow patient to “tell their story” § Ask patient about goals/strengths § Learn how to support patient in their challenges § Discuss other anticipated transfers Fogarty CT. Examining the influence of physicians in the lives of patients over time: Taking a history of the doctor-patient relationship. Families, Systems, & Health, Vol 19(2), 2001, 221 -226. Lieberman JA 3 rd, Stuart MR. The BATHE method: Incorporating counseling and psychotherapy into the everyday management of patients. Prim Care Companion J Clin Psychiatry. 1999 Apr; 1(2): 35 -38.

Thank you for your attention! On Wisconsin! Any questions? brian. arndt@fammed. wisc. edu
- Slides: 52