A and V Patterns and Other Types of
- Slides: 45
A and V Patterns and Other Types of Strabismus Paviglianiti / January 21, 2010
A and V Patterns ® ® ® ® Horizontal deviations that change in magnitude in upgaze and downgaze A or V patterns reportedly in 15 -25% of all horizontal strabismus IOOA assoc with V patterns SOOA assoc with A patterns Sometimes, if vertical muscles underacting (eg SR) then their tertiary adducting effect in upgaze will decrease, giving a V pattern; underacting IR will decrease its tertiary adduction in downgaze, giving an A pattern (both SR and IR are tertiary adductors) Pts with Aperts/Crouzons have V patterns since their orbits are excyclotorted Technically, need a difference between upgaze vs downgaze of at least 10 d in A pattern; 15 d in V pattern (I use 15 for both) If obliques are overacting, weaken them; if not, do MALE horizontal transposition by ½ tendon width…rules apply regardless of whether you are weakening or tightening or whether surgery on 2 eyes or R/R on 1.
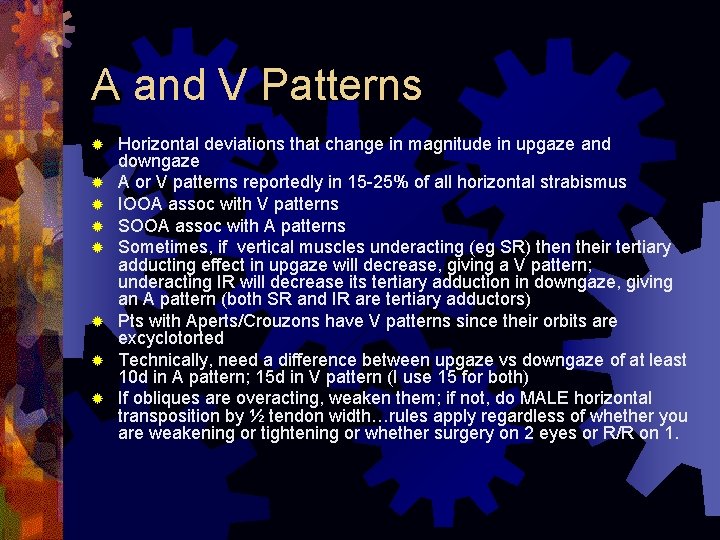
Special Forms of Strabismus ® Duanes Syndrome ® Möbius Syndrome ® Brown’s Syndrome ® Thyroid Eye Disease ® Congenital Fibrosis Syndrome ® Progressive External Ophthalmoplegia (PEO) ® Myasthenia ® Internuclear Ophthalmoplegia (INO) ® Congenital Oculomotor Apraxia ® Congenital / Acquired 3 rd, 4 th, 6 th palsies
Concomitant vs Incomitant ® Concomitant Strabismus: ® The measurements are the same in all fields of gaze (numbers on the tictactoe board are the same in all the boxes) AND the range of mvt of the eyes is full ® Incomitant Strabismus ® Measurements gaze different in different fields of
Duane’s Syndrome ® Type I =>reduced abduction ® Type II => reduced adduction ® Type III => reduced abd and add ® Clinically, little use this classification scheme is of
Duane’s Syndrome/Type I ® Can’t abduct, so usually esotropic in primary position, sometimes with compensatory head turn for fusion ® Usually girls ® More often left eye, but bilateral 20% ® On attempted abduction, involved lids widen ® Involved lids widen on attempted mvt toward deficit ® On adduction, involved lids narrow and globe retracts into orbit, and there are upshoots and downshoots ® Involved lids narrow on attempted mvt away from deficit; upshoots/downshoots on involved eye with attempted mvt away from deficit
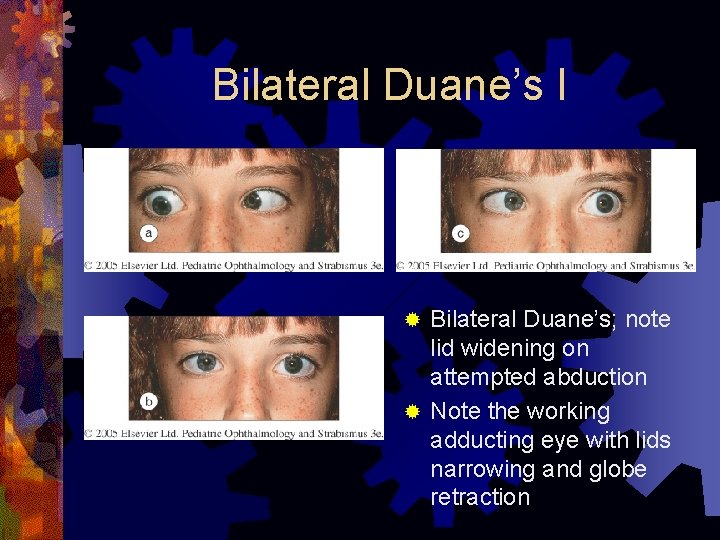
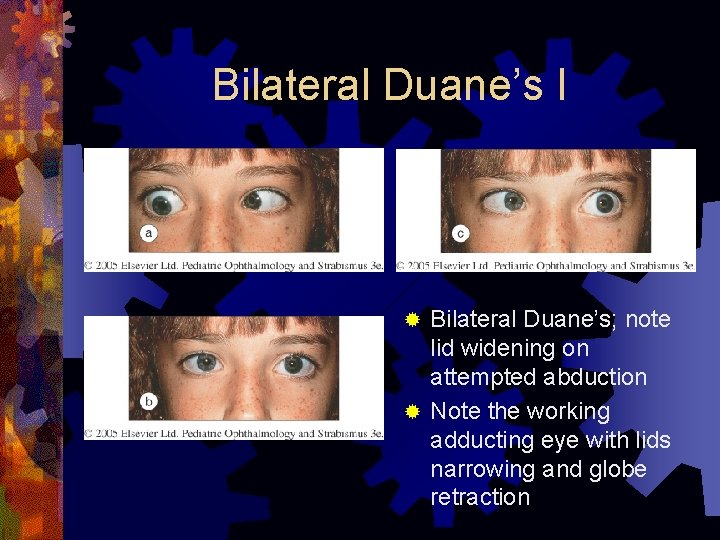
Bilateral Duane’s I Bilateral Duane’s; note lid widening on attempted abduction ® Note the working adducting eye with lids narrowing and globe retraction ®
Duane’s Syndrome Type II ® Limited adduction, so XT in primary ® Ddx includes INO, but INO has no lid fissure widening on attempted movement toward the deficit
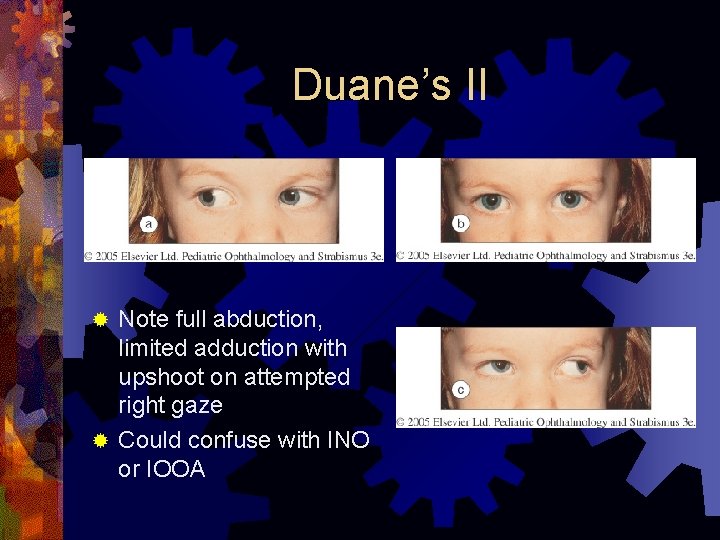
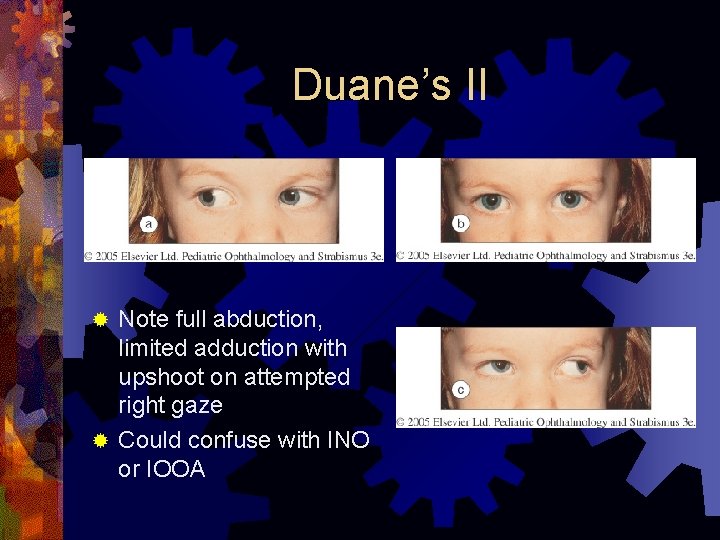
Duane’s II Note full abduction, limited adduction with upshoot on attempted right gaze ® Could confuse with INO or IOOA ®
Duane’s Syndrome Type III ® Limited abduction and adduction, so usually ortho in primary
Duane’s Syndrome ® Usually NOT inherited (sporadic), but 10% there is auto dominant inheritance ® Since bilateral 20%, ddx includes congenital esotropia with tight medial recti, which don’t allow full abduction ® Used to be thought it was caused by hypoplasia of 6 th nerve nucleus, with the 3 rd nerve taking over innervation of the LR in an abnormal way; this isn’t proven and exact cause of Duane’s still mysterious ® Ocular associations: ptosis of involved side; cataracts, iris heterochromia, iris/retina coloboma
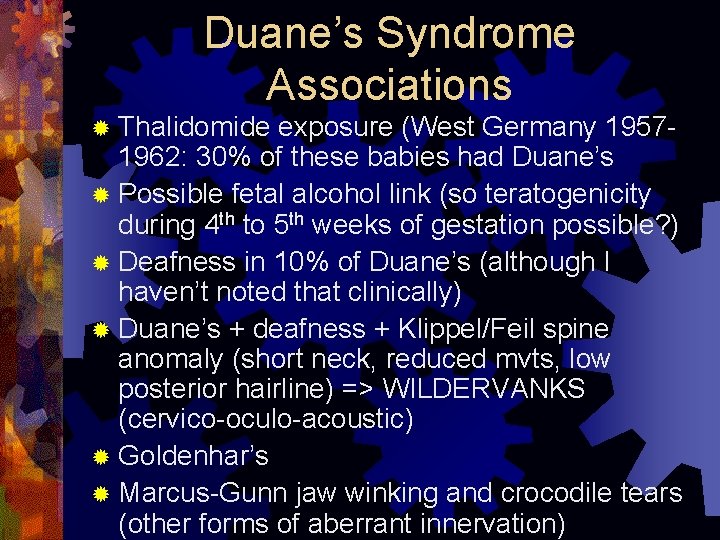
Duane’s Syndrome Associations ® Thalidomide exposure (West Germany 19571962: 30% of these babies had Duane’s ® Possible fetal alcohol link (so teratogenicity during 4 th to 5 th weeks of gestation possible? ) ® Deafness in 10% of Duane’s (although I haven’t noted that clinically) ® Duane’s + deafness + Klippel/Feil spine anomaly (short neck, reduced mvts, low posterior hairline) => WILDERVANKS (cervico-oculo-acoustic) ® Goldenhar’s ® Marcus-Gunn jaw winking and crocodile tears (other forms of aberrant innervation)
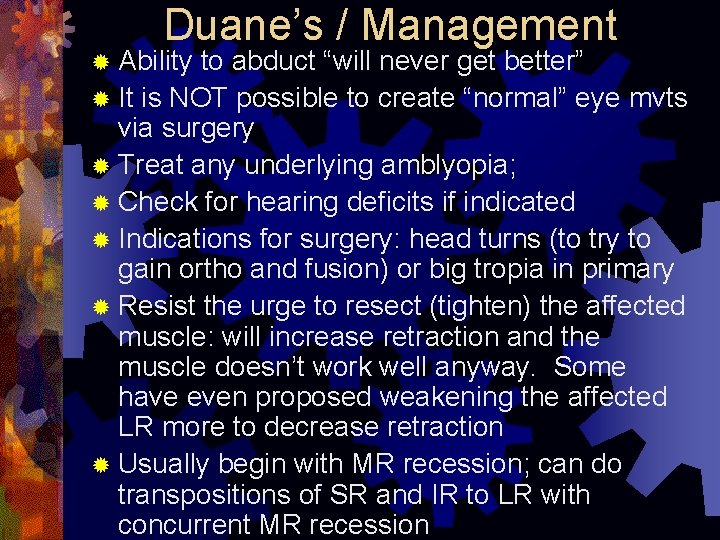
Duane’s / Management ® Ability to abduct “will never get better” ® It is NOT possible to create “normal” eye mvts via surgery ® Treat any underlying amblyopia; ® Check for hearing deficits if indicated ® Indications for surgery: head turns (to try to gain ortho and fusion) or big tropia in primary ® Resist the urge to resect (tighten) the affected muscle: will increase retraction and the muscle doesn’t work well anyway. Some have even proposed weakening the affected LR more to decrease retraction ® Usually begin with MR recession; can do transpositions of SR and IR to LR with concurrent MR recession
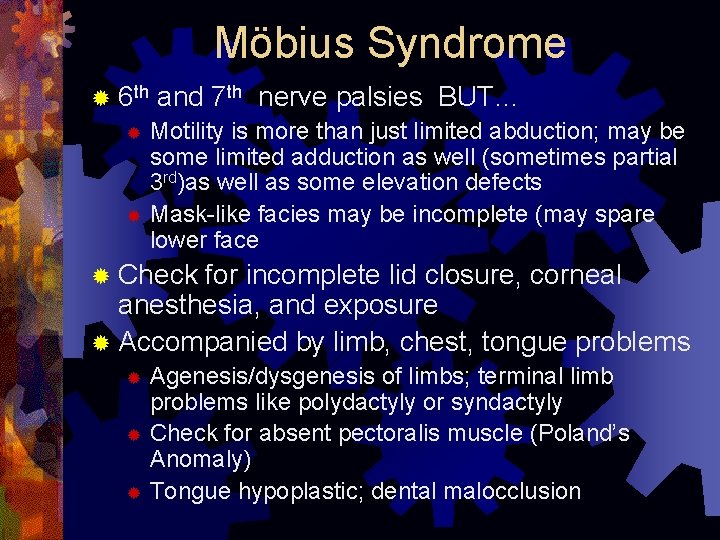
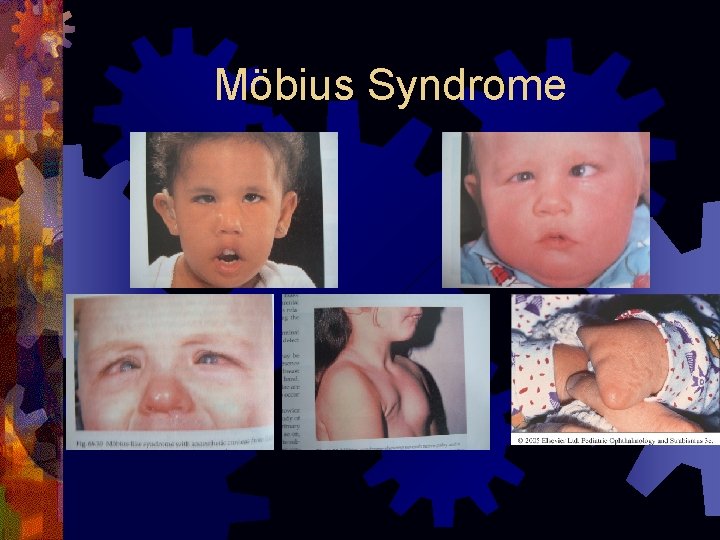
Möbius Syndrome ® 6 th and 7 th nerve palsies BUT… Motility is more than just limited abduction; may be some limited adduction as well (sometimes partial 3 rd)as well as some elevation defects ® Mask-like facies may be incomplete (may spare lower face ® ® Check for incomplete lid closure, corneal anesthesia, and exposure ® Accompanied by limb, chest, tongue problems Agenesis/dysgenesis of limbs; terminal limb problems like polydactyly or syndactyly ® Check for absent pectoralis muscle (Poland’s Anomaly) ® Tongue hypoplastic; dental malocclusion ®
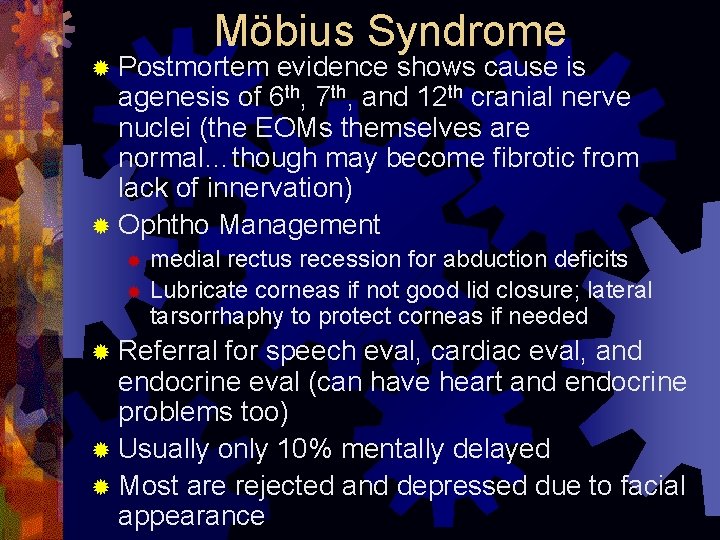
Möbius Syndrome ® Postmortem evidence shows cause is agenesis of 6 th, 7 th, and 12 th cranial nerve nuclei (the EOMs themselves are normal…though may become fibrotic from lack of innervation) ® Ophtho Management medial rectus recession for abduction deficits ® Lubricate corneas if not good lid closure; lateral tarsorrhaphy to protect corneas if needed ® ® Referral for speech eval, cardiac eval, and endocrine eval (can have heart and endocrine problems too) ® Usually only 10% mentally delayed ® Most are rejected and depressed due to facial appearance
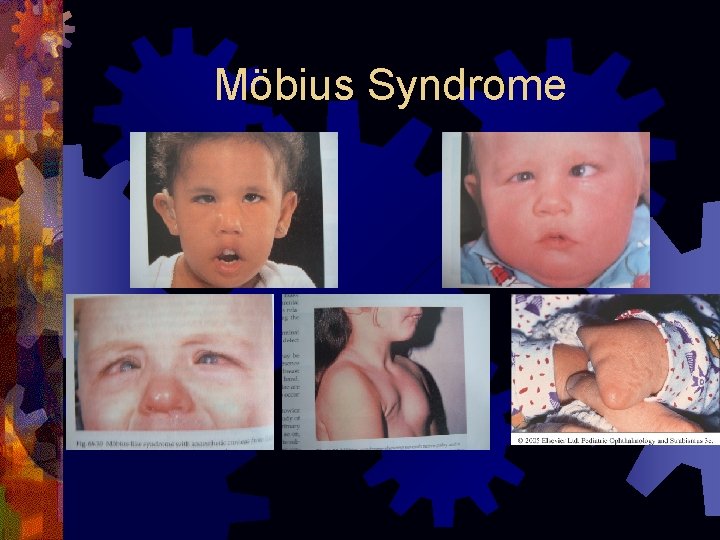
Möbius Syndrome
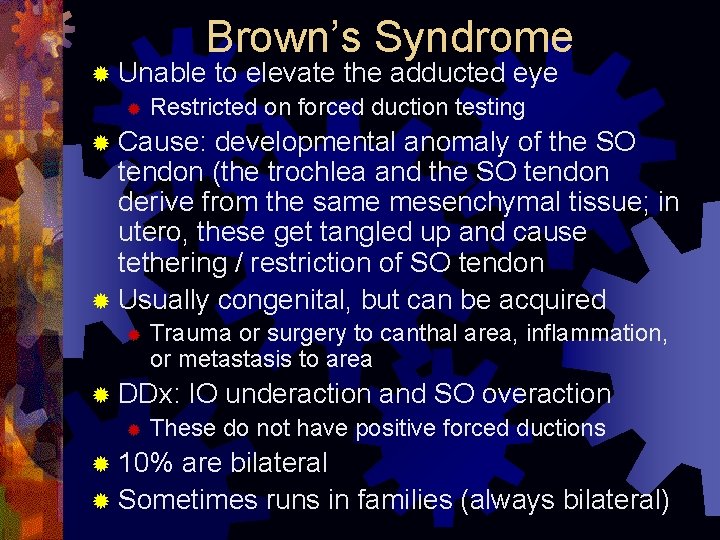
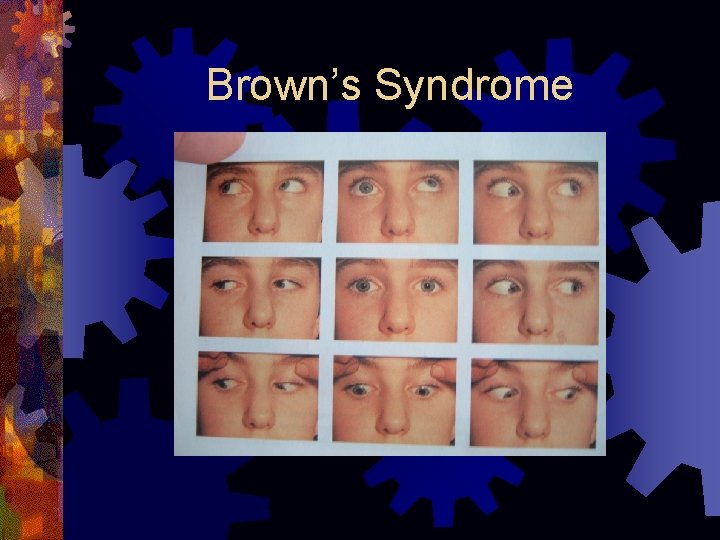
Brown’s Syndrome ® Unable to elevate the adducted eye ® Restricted on forced duction testing ® Cause: developmental anomaly of the SO tendon (the trochlea and the SO tendon derive from the same mesenchymal tissue; in utero, these get tangled up and cause tethering / restriction of SO tendon ® Usually congenital, but can be acquired ® Trauma or surgery to canthal area, inflammation, or metastasis to area ® DDx: IO underaction and SO overaction ® These do not have positive forced ductions ® 10% are bilateral ® Sometimes runs in families (always bilateral)
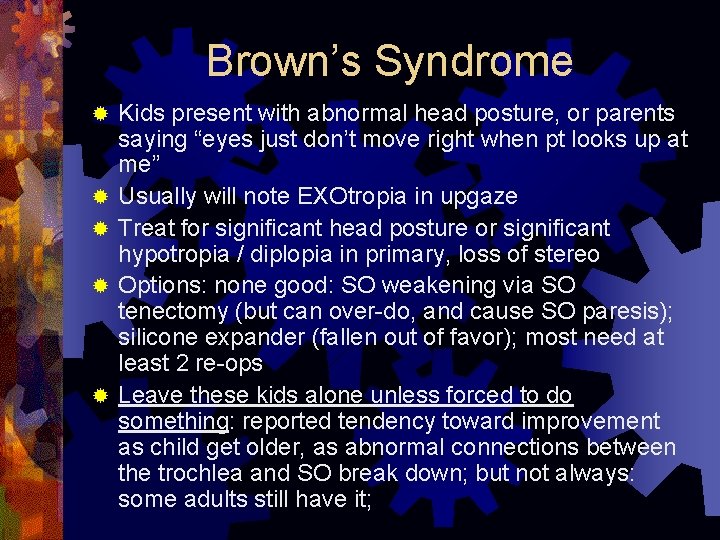
Brown’s Syndrome ® ® ® Kids present with abnormal head posture, or parents saying “eyes just don’t move right when pt looks up at me” Usually will note EXOtropia in upgaze Treat for significant head posture or significant hypotropia / diplopia in primary, loss of stereo Options: none good: SO weakening via SO tenectomy (but can over-do, and cause SO paresis); silicone expander (fallen out of favor); most need at least 2 re-ops Leave these kids alone unless forced to do something: reported tendency toward improvement as child get older, as abnormal connections between the trochlea and SO break down; but not always: some adults still have it;
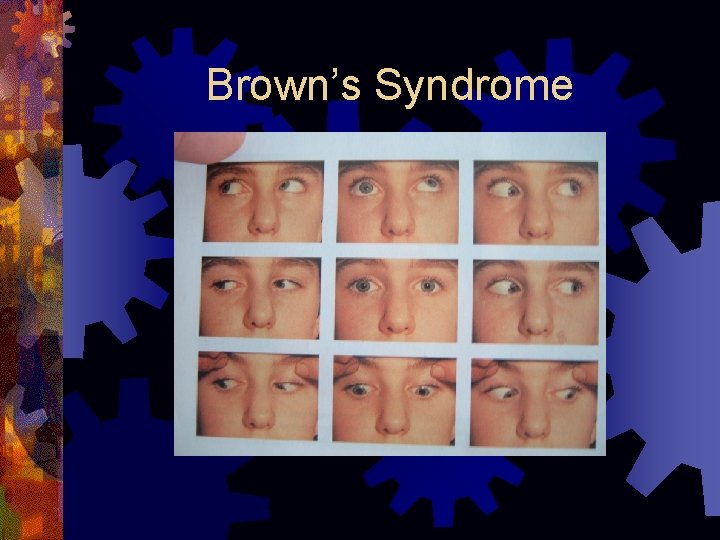
Brown’s Syndrome
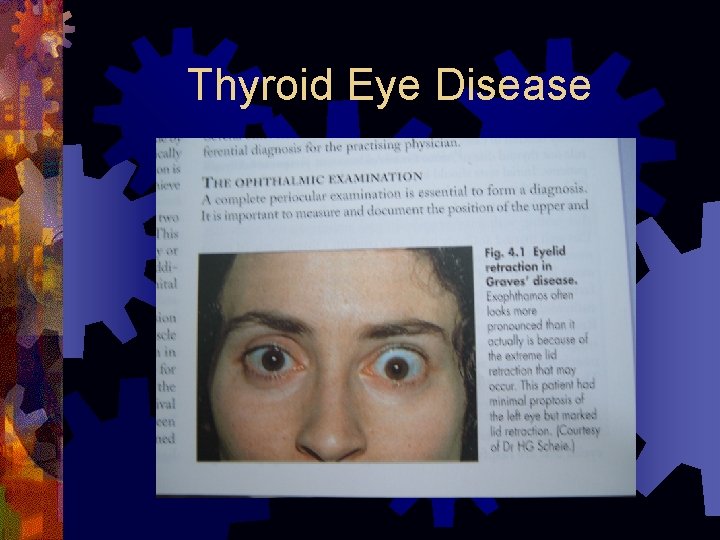
Thyroid Eye Disease ® Restrictive myopathy with lymphocytic infiltration of EOMs ® Usual order for boards IMSLow (IR affected most>MR>SR>LR; from recent lecture by Dr. Gearity, the 3 muscles are affected about the same. ® Usual misalignment is proptosis, hypotropia, and esotropia (from scarred/fibrosed IR pulling eye down; fibrosed MR pulling eye in); forced ductions are usually positive ® Present with diplopia that does not follow any pattern, therefore prisms usually don’t work
Thyroid Eye Disease ® Most are hyperthyroid at dx, but can be euthyroid or hypothyroid ® Get TSI, TSH, and T 4 (per Dr. Gearity) ® CT orbits can be helpful to see degree of EOM involvement ® Thyroid eye disease often co-exists with myasthenia so eval for this also ® If optic nerve involved, may need orbital decompression prior to strabismus surgery ® Surgery: optional oral prednisone for 2 weeks (“to soften things up”); then surgery (ie inferior rectus recession: aim to undercorrect
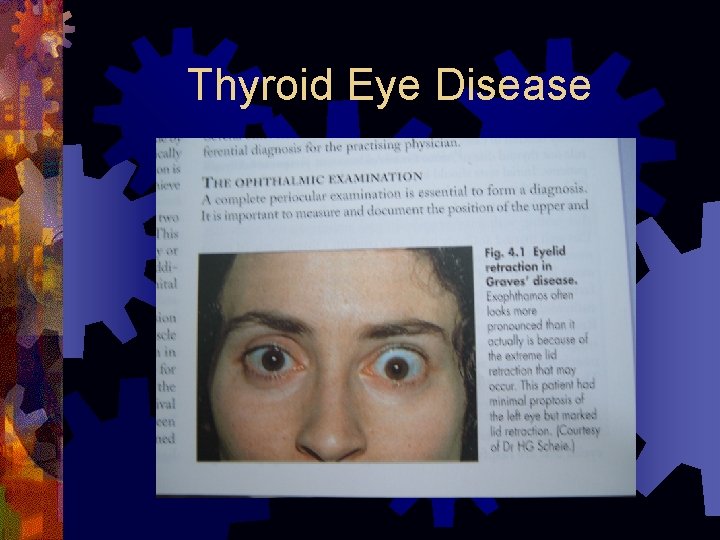
Thyroid Eye Disease
Congenital Fibrosis Syndromes ® Group of congenital anomalies with variable amts of restriction of EOMs via replacement of muscle tissue with fibrous tissue ® Can be single muscle on one eye to all muscles on both eyes ® Often levator involved=>ptosis=>chin up head posture ® DDx is PEO (frozen eyes and ptosis) ® Many types inherited (auto dominant usually) though can be sporadic ® Etiology unknown ® Goal: get ortho in primary
Congenital Fibrosis Syndromes ® General fibrosis of all the EOMs (mostly auto dominant inheritance) ® Congenital fibrosis of the IR=>cannot look up; can mimic double elevator palsy ® Congenital fibrosis of the MR/LR (strabismus fixus) ® Can present with congenital esotropia appearance with both eyes pointing down and in toward nose ® Congenital down fibrosis of the SR=>pt cannot look
Congenital Fibrosis - familial
Chronic Progressive External Ophthalmoplegia (CPEO) ® Presents as ptosis, followed by progressive paresis of EOMs; pupils spared ® DDX is Congenital Fibrosis (frozen eye and ptosis) ® Triad of PEO, pigmentary retina changes and heart block/cardio problems is Kearns-Sayre, (usually before age 20) (many times a board question); mgmt: refer for sequential EKG Other signs of K-S: short stature, hearing loss, diabetes/endocrine problems ® Dx: EOM or limb muscle bx show “ragged red fibers” (actually are clumps of degenerated mitochondria) on trichrome stain ® ® May be mitochondrial dysfunction as cause
Myasthenia ® Look for variable strabismus throughout the day or on sequential exams ® Diplopia is often intermittent ® Can be “ocular “ only or systemic ® Look for fatigueability on extended upgaze ® Often reversed by a few minutes of cold ice in a rubber glove on the eyelids
Myasthenia ® Refer to Neuro for Tensilon test / EMG ® Test dose 0. 1 cc edrophonium (tensilon) ® If ok, then 0. 9 cc edrophonium ® Keep IV atropine on hand as antidote ® Can test for ® Acetylcholine receptor antibody ® ® Found in 90% of acquired MG (not found in congenital MG); only present 50% of time in “ocular” MG Antistriated muscle antibody ® Found in 90% of MG with thymoma and 30% of MG pts without thymoma ® Therefore, in typical diplopia pt with fatigueability, but no systemic sx, these tests will be negative often despite disease, so still refer to neuro for tensilon test if suspicious
Internuclear Ophthalmoplegia (INO) ® Looks like a “one-sided MR palsy” (ipsilateral to the lesion), with the other eye having horizontal nystagmus ® The limited adduction may be total or partial ® Both eyes adduct normally on convergence to a near target ® Is a problem in the MLF (medial longitudinal fasciculus) of the brain stem ® Interruption in signal from abducens relay signals from reaching the contralateral oculomotor nucleus, impairing adduction
INO Anatomy ® IF I WANT TO LOOK LEFT: ® Left PPRF stimulates the Left 6 th N nucleus=> (abduct left eye) ® Left 6 th N nucleus stimulates the MLF ® MLF crosses and ascends to the contralateral (right) 3 rd nucleus ® To give contralateral (right) MR contraction (adduct right eye)
INO ® In adults: Multiple Sclerosis is common cause and many times is bilateral INO ® In kids: posterior fossa tumors (eg brainstem glioma), Arnold-Chiari, head trauma, sickle cell ® In old folks: frontal lobe CVA or tumor
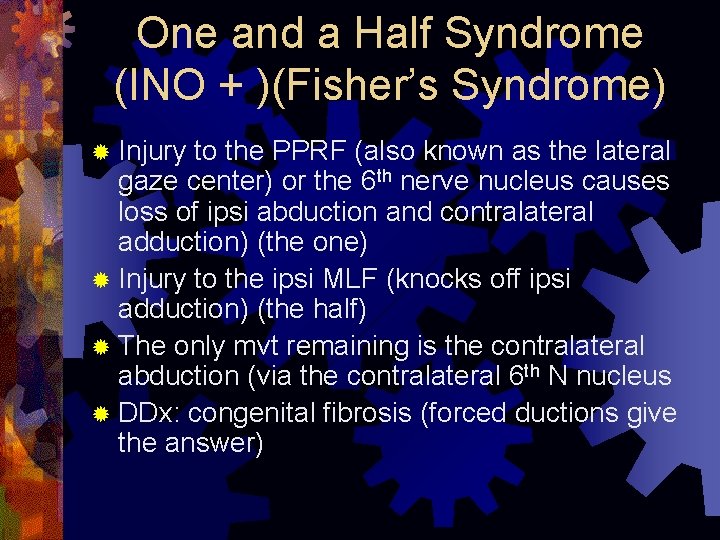
One and a Half Syndrome (INO + )(Fisher’s Syndrome) ® Injury to the PPRF (also known as the lateral gaze center) or the 6 th nerve nucleus causes loss of ipsi abduction and contralateral adduction) (the one) ® Injury to the ipsi MLF (knocks off ipsi adduction) (the half) ® The only mvt remaining is the contralateral abduction (via the contralateral 6 th N nucleus ® DDx: congenital fibrosis (forced ductions give the answer)
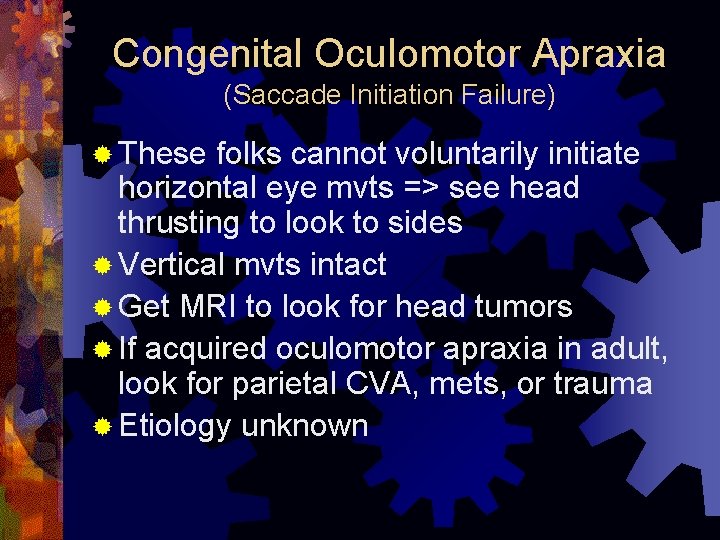
Congenital Oculomotor Apraxia (Saccade Initiation Failure) ® These folks cannot voluntarily initiate horizontal eye mvts => see head thrusting to look to sides ® Vertical mvts intact ® Get MRI to look for head tumors ® If acquired oculomotor apraxia in adult, look for parietal CVA, mets, or trauma ® Etiology unknown
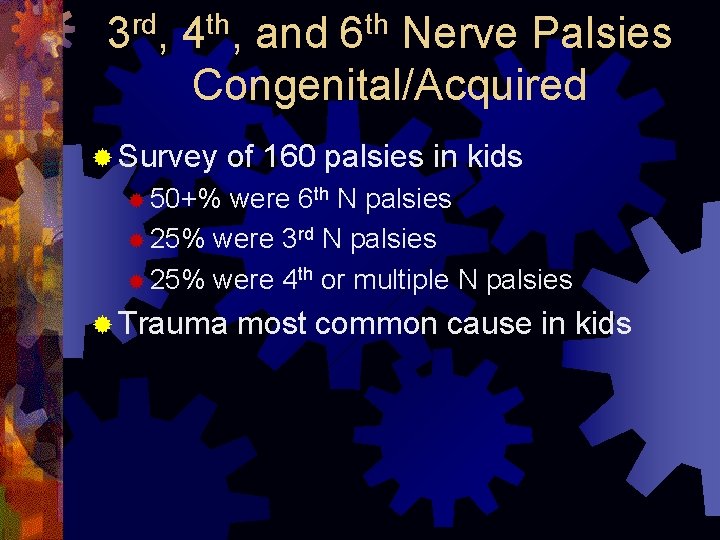
3 rd, 4 th, and 6 th Nerve Palsies Congenital/Acquired ® Survey of 160 palsies in kids ® 50+% were 6 th N palsies ® 25% were 3 rd N palsies ® 25% were 4 th or multiple N palsies ® Trauma most common cause in kids
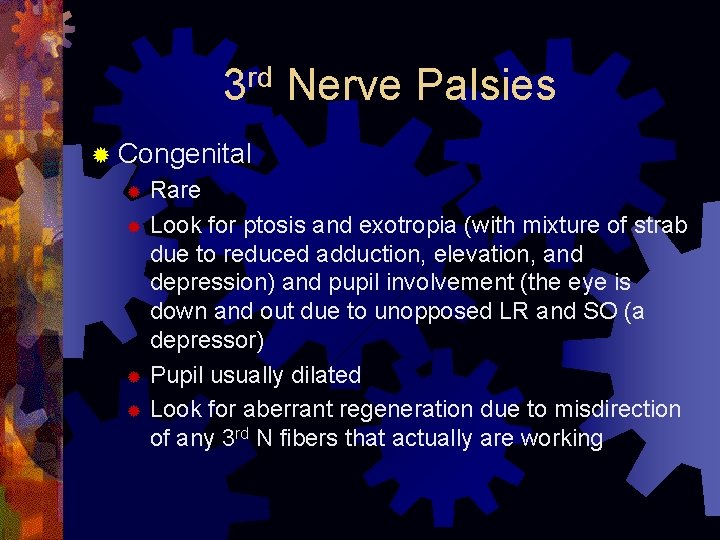
rd 3 Nerve Palsies ® Congenital Rare ® Look for ptosis and exotropia (with mixture of strab due to reduced adduction, elevation, and depression) and pupil involvement (the eye is down and out due to unopposed LR and SO (a depressor) ® Pupil usually dilated ® Look for aberrant regeneration due to misdirection of any 3 rd N fibers that actually are working ®
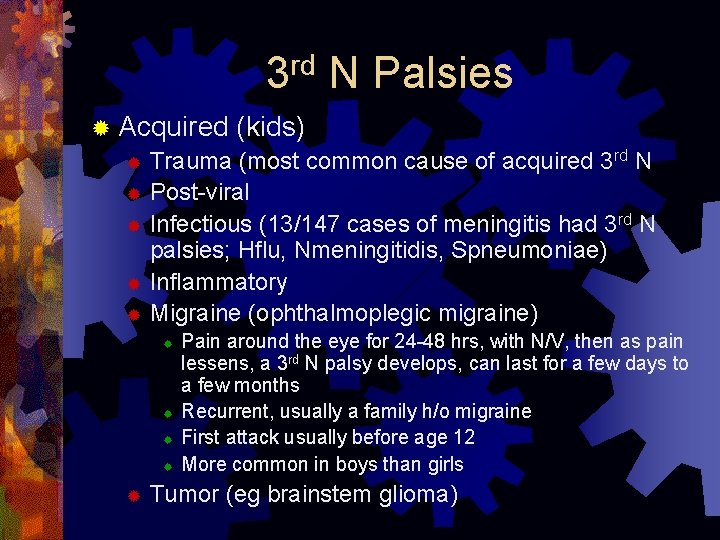
rd 3 N Palsies ® Acquired (kids) ® Trauma (most common cause of acquired 3 rd N ® Post-viral ® Infectious (13/147 cases of meningitis had 3 rd N palsies; Hflu, Nmeningitidis, Spneumoniae) ® Inflammatory ® Migraine (ophthalmoplegic migraine) ® ® ® Pain around the eye for 24 -48 hrs, with N/V, then as pain lessens, a 3 rd N palsy develops, can last for a few days to a few months Recurrent, usually a family h/o migraine First attack usually before age 12 More common in boys than girls Tumor (eg brainstem glioma)
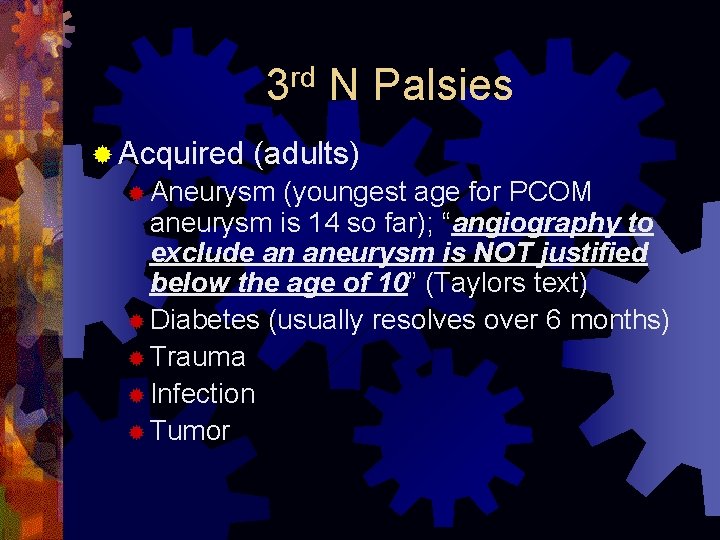
rd 3 ® Acquired N Palsies (adults) ® Aneurysm (youngest age for PCOM aneurysm is 14 so far); “angiography to exclude an aneurysm is NOT justified below the age of 10” (Taylors text) ® Diabetes (usually resolves over 6 months) ® Trauma ® Infection ® Tumor
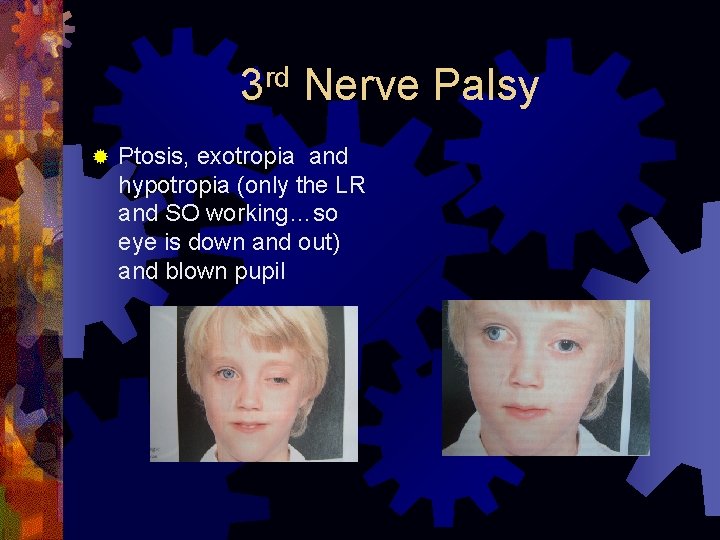
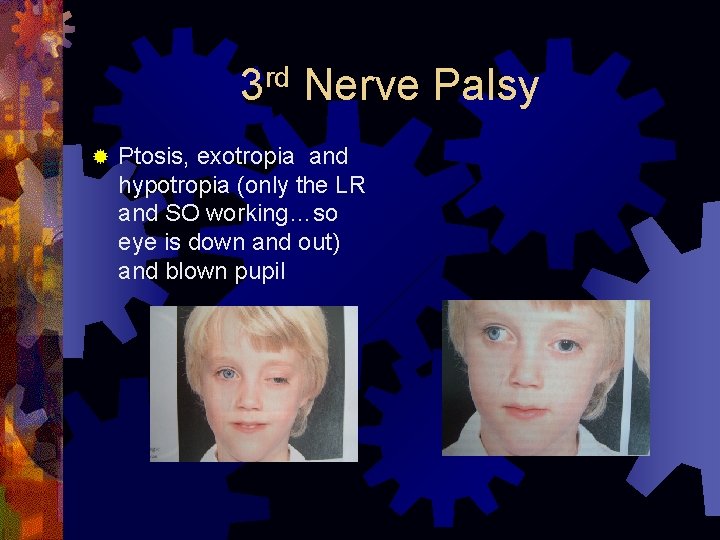
rd 3 ® Nerve Palsy Ptosis, exotropia and hypotropia (only the LR and SO working…so eye is down and out) and blown pupil
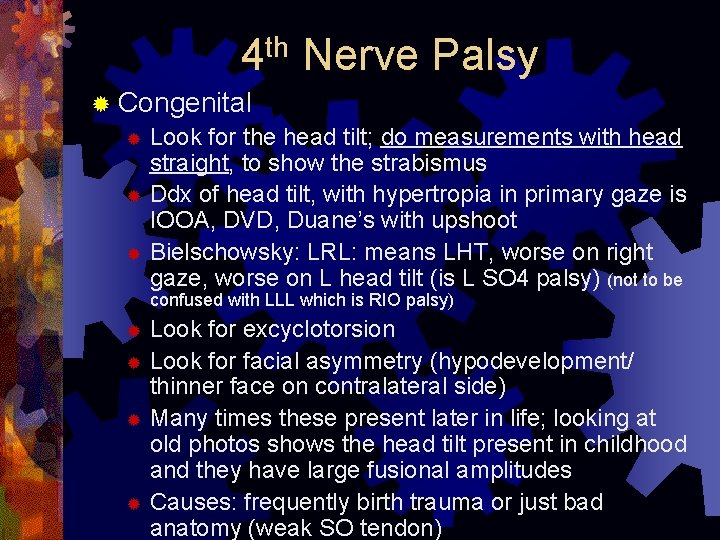
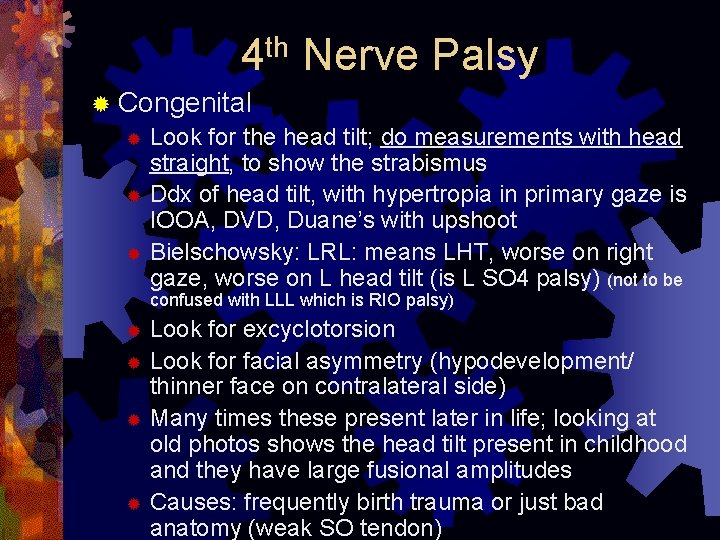
4 th Nerve Palsy ® Congenital ® Look for the head tilt; do measurements with head straight, to show the strabismus ® Ddx of head tilt, with hypertropia in primary gaze is IOOA, DVD, Duane’s with upshoot ® Bielschowsky: LRL: means LHT, worse on right gaze, worse on L head tilt (is L SO 4 palsy) (not to be confused with LLL which is RIO palsy) Look for excyclotorsion ® Look for facial asymmetry (hypodevelopment/ thinner face on contralateral side) ® Many times these present later in life; looking at old photos shows the head tilt present in childhood and they have large fusional amplitudes ® Causes: frequently birth trauma or just bad anatomy (weak SO tendon) ®
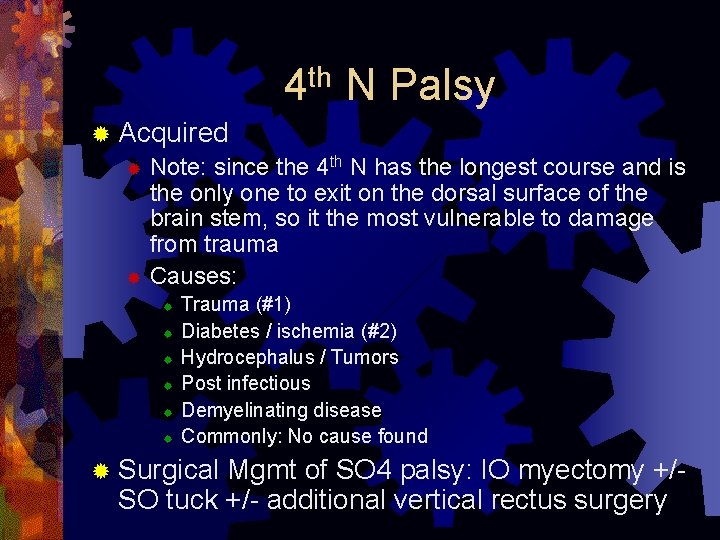
th 4 N Palsy ® Acquired ® Note: since the 4 th N has the longest course and is the only one to exit on the dorsal surface of the brain stem, so it the most vulnerable to damage from trauma ® Causes: ® ® ® Trauma (#1) Diabetes / ischemia (#2) Hydrocephalus / Tumors Post infectious Demyelinating disease Commonly: No cause found ® Surgical Mgmt of SO 4 palsy: IO myectomy +/SO tuck +/- additional vertical rectus surgery
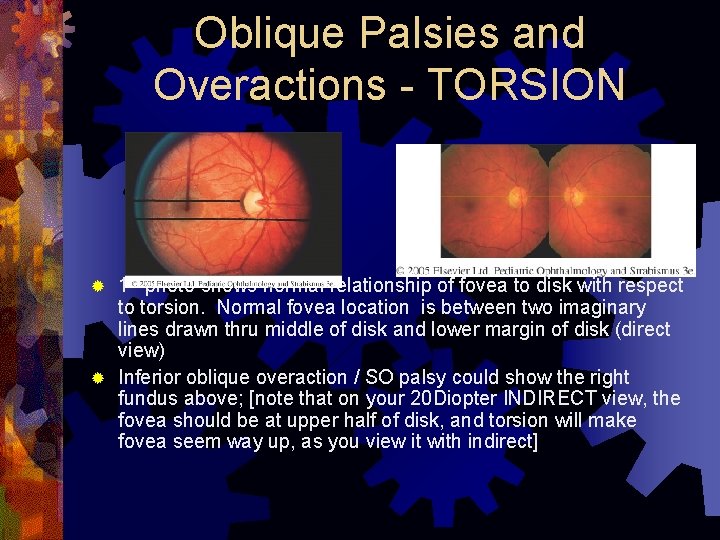
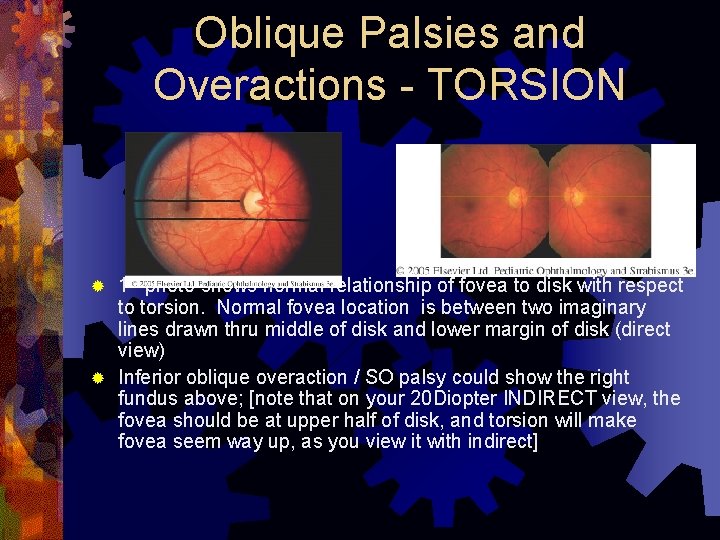
Oblique Palsies and Overactions - TORSION 1 st photo shows normal relationship of fovea to disk with respect to torsion. Normal fovea location is between two imaginary lines drawn thru middle of disk and lower margin of disk (direct view) ® Inferior oblique overaction / SO palsy could show the right fundus above; [note that on your 20 Diopter INDIRECT view, the fovea should be at upper half of disk, and torsion will make fovea seem way up, as you view it with indirect] ®
th 6 Nerve Palsy ® Congenital ® Duane’s ® Transient LR palsy of Newborns, usually goes away before it is even diagnosed (may be as common as 1/ 182 normal births); sometimes there is h/o birth trauma or forceps
th 6 N Palsy ® Acquired ® Trauma (40%) ® Neoplasms (16%) (pontine glioma) ® Intracranial Hypertension (Pseudotumor or hydrocephalus) ® Infection (meningitis, varicella, Lyme) and s/p vaccination (MMR) ® Acquired 6 th N palsy of unknown cause in children: isolated, painless 6 th N palsy that resolves in 8 -12 weeks; w/u negative (including MRI and CSF and neuro w/u); may recur
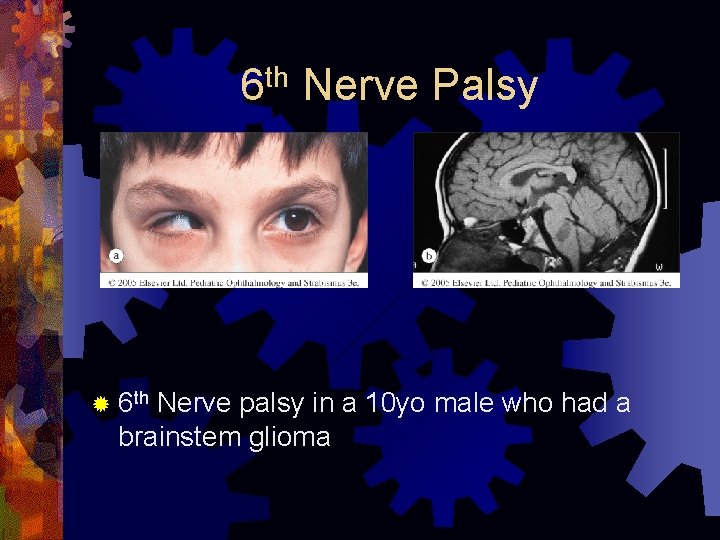
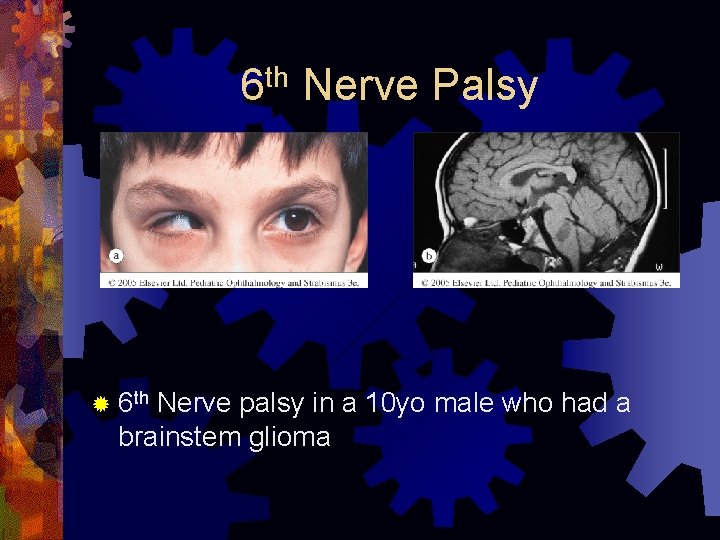
th 6 ® 6 th Nerve Palsy Nerve palsy in a 10 yo male who had a brainstem glioma
rd th thv 1 v 2 th 3 /4 /5 /6 ® Image combo palsy the cavernous sinus area ® If there is proptosis, consider an orbital apex syndrome