9 Skeletal Muscle Tissue Power Point Lecture Presentations
- Slides: 129
9 Skeletal Muscle Tissue Power. Point® Lecture Presentations prepared by Alexander G. Cheroske Mesa Community College at Red Mountain © 2011 Pearson Education, Inc.
Section 1: Functional Anatomy of Skeletal Muscle Tissue • Learning Outcomes • 9. 1 Describe the organization of skeletal muscle at the tissue level. • 9. 2 Identify the structural components of a sarcomere. • 9. 3 Describe the structural components of a thin filament and a thick filament. • 9. 4 Identify the components of the neuromuscular junction, and summarize the events involved in the neural control of skeletal muscles. • 9. 5 Describe the role of ATP in a muscle contraction, and explain the steps involved in the contraction of a skeletal muscle fiber. © 2011 Pearson Education, Inc.
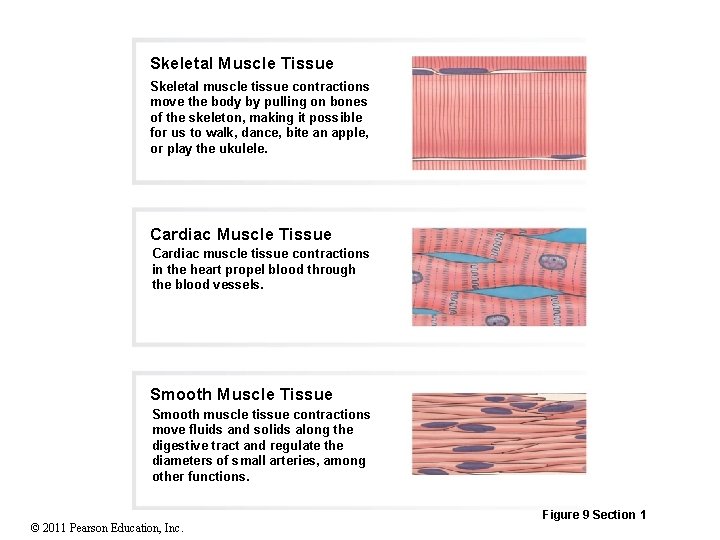
Section 1: Functional Anatomy of Skeletal Muscle Tissue • Muscle tissue • One of the four primary tissue types • Consists chiefly of muscle cells specialized for contraction • Three types 1. Cardiac • In heart propelling blood through blood vessels 2. Smooth • Move fluids and solids along digestive tract • Regulate diameters of small arteries • Other functions © 2011 Pearson Education, Inc.
Section 1: Functional Anatomy of Skeletal Muscle Tissue • Muscle tissue (continued) • Three types (continued) 3. Skeletal • Move body by pulling on bones • Each cell is a single muscle fiber • Each muscle is an organ • © 2011 Pearson Education, Inc. Primarily muscle cells plus connective tissues, nerves, and blood vessels
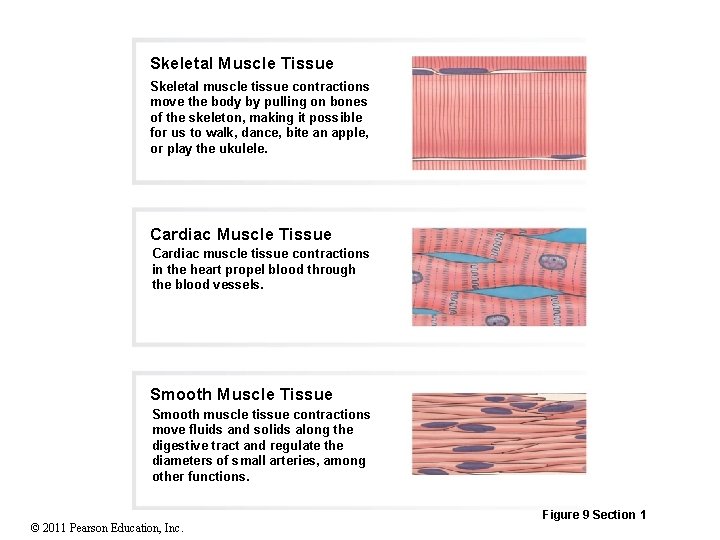
Skeletal Muscle Tissue Skeletal muscle tissue contractions move the body by pulling on bones of the skeleton, making it possible for us to walk, dance, bite an apple, or play the ukulele. Cardiac Muscle Tissue Cardiac muscle tissue contractions in the heart propel blood through the blood vessels. Smooth Muscle Tissue Smooth muscle tissue contractions move fluids and solids along the digestive tract and regulate the diameters of small arteries, among other functions. © 2011 Pearson Education, Inc. Figure 9 Section 1
Section 1: Functional Anatomy of Skeletal Muscle Tissue • Skeletal muscle tissue functions • Produce skeletal movements • Pull tendons and move bones • Maintain posture and body position • Skeletal muscle tension maintains body posture • Support soft tissues • Support weight of visceral organs and shield internal tissues from injury © 2011 Pearson Education, Inc.
Section 1: Functional Anatomy of Skeletal Muscle Tissue • Skeletal muscle tissue functions (continued) • Guard entrances and exits • Openings of digestive and urinary tracts encircled by skeletal muscle (sphincters) • Provide voluntary control of swallowing, defecation, and urination • Maintain body temperature • Some energy used for muscle contraction is released as heat • Provide nutrient reserves • Amino acids from muscle fibers can be released into circulation and used to produce glucose and energy © 2011 Pearson Education, Inc.
Module 9. 1: Skeletal muscle anatomy • Skeletal muscle • Complex organ containing: • Skeletal muscle fibers (contraction) • Connective tissues (harness contractile forces) • Blood vessels (nourish muscle fibers) • Nerves (control contractions) © 2011 Pearson Education, Inc.
Module 9. 1: Skeletal muscle anatomy • Skeletal muscle connective tissues • Tendon • Bundle of collagen fibers that attach muscle to bone • Collagen fibers extend into bone matrix providing firm attachment • Also occurs as a sheet (= aponeurosis) • Epimysium (epi-, on + mys, muscle) • Dense layer of collagen fibers surrounding entire muscle • Separates muscle from surrounding tissues and organs • Connected to deep fascia © 2011 Pearson Education, Inc.
Module 9. 1: Skeletal muscle anatomy • Skeletal muscle connective tissues (continued) • Perimysium (peri-, around) • Fibrous layer that divides muscle into compartments or bundles of cells (= fascicles) • Contains collagen and elastin fibers, blood vessels, and nerves • Endomysium (endo-, inside) • Surrounds individual muscle cells or fibers • Loosely interconnects adjacent muscle fibers • Contains capillaries, myosatellite (stem) cells, and axons of neurons that control muscle fibers © 2011 Pearson Education, Inc.
Module 9. 1: Skeletal muscle anatomy Animation: Muscle Physiology: Muscle Layers Animation: Anatomy of Skeletal Muscles © 2011 Pearson Education, Inc.
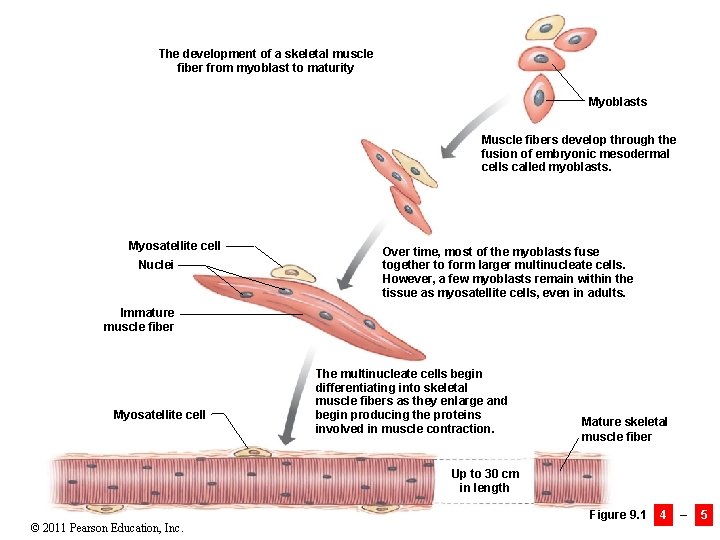
Module 9. 1: Skeletal muscle anatomy • Skeletal muscle cell development • Myoblasts (myo-, muscle + blastos, formative cell) fuse, forming multinucleate cells • Develop into skeletal muscle fibers • Each skeletal muscle fiber nucleus represents a myoblast • Not all myoblasts fuse into developing muscle fibers • Some remain in endomysium and help muscle repair © 2011 Pearson Education, Inc.
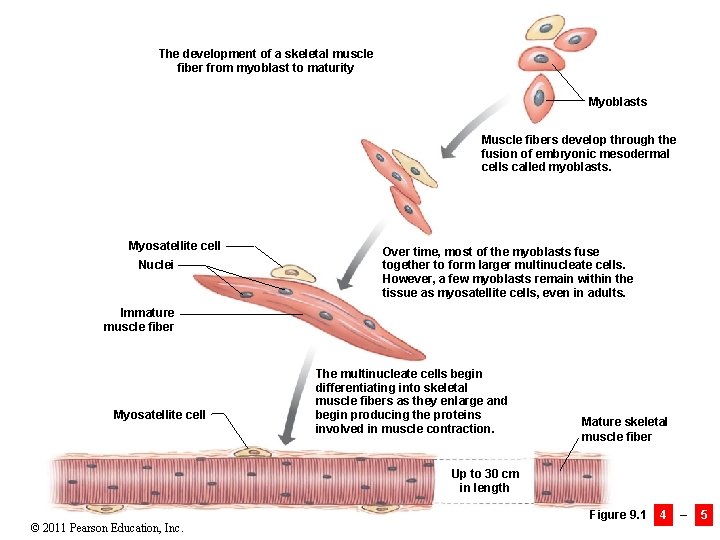
The development of a skeletal muscle fiber from myoblast to maturity Myoblasts Muscle fibers develop through the fusion of embryonic mesodermal cells called myoblasts. Myosatellite cell Nuclei Over time, most of the myoblasts fuse together to form larger multinucleate cells. However, a few myoblasts remain within the tissue as myosatellite cells, even in adults. Immature muscle fiber Myosatellite cell The multinucleate cells begin differentiating into skeletal muscle fibers as they enlarge and begin producing the proteins involved in muscle contraction. Mature skeletal muscle fiber Up to 30 cm in length © 2011 Pearson Education, Inc. Figure 9. 1 4 – 5
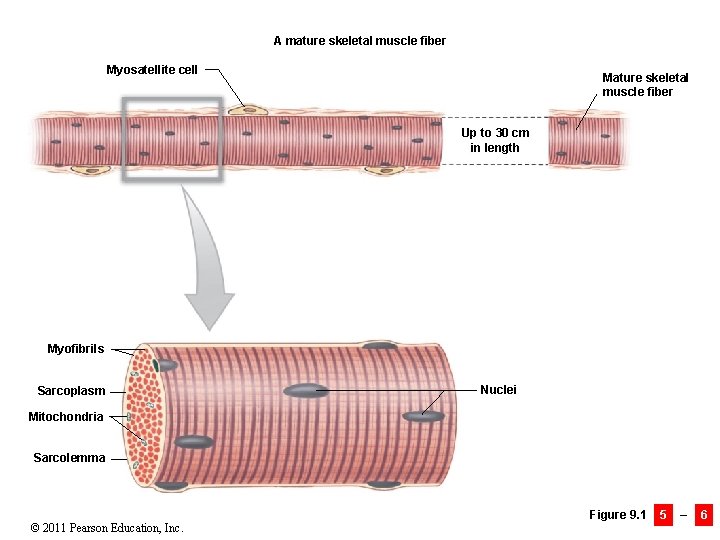
Module 9. 1: Skeletal muscle anatomy • Mature muscle cell characteristics • Very large cells • Can have diameter of 100 µm and length of 30 cm (12 in. ) • Each contains hundreds of nuclei just internal to plasma membrane (sarcolemma) (sarkos, flesh + lemma, husk) • Genes in nuclei control production of enzymes and structural proteins for contraction • Many nuclei = many genes = faster production • Cytoplasm = sarcoplasm © 2011 Pearson Education, Inc.
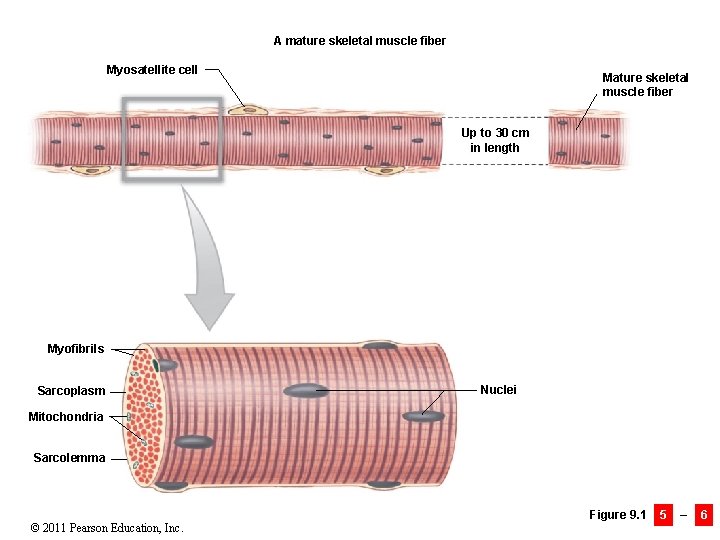
A mature skeletal muscle fiber Myosatellite cell Mature skeletal muscle fiber Up to 30 cm in length Myofibrils Sarcoplasm Nuclei Mitochondria Sarcolemma © 2011 Pearson Education, Inc. Figure 9. 1 5 – 6
Module 9. 1 Review a. Define tendon and aponeurosis. b. Describe the connective tissue layers associated with skeletal muscle tissue. c. How would severing the tendon attached to a muscle affect the muscle’s ability to move a body part? © 2011 Pearson Education, Inc.
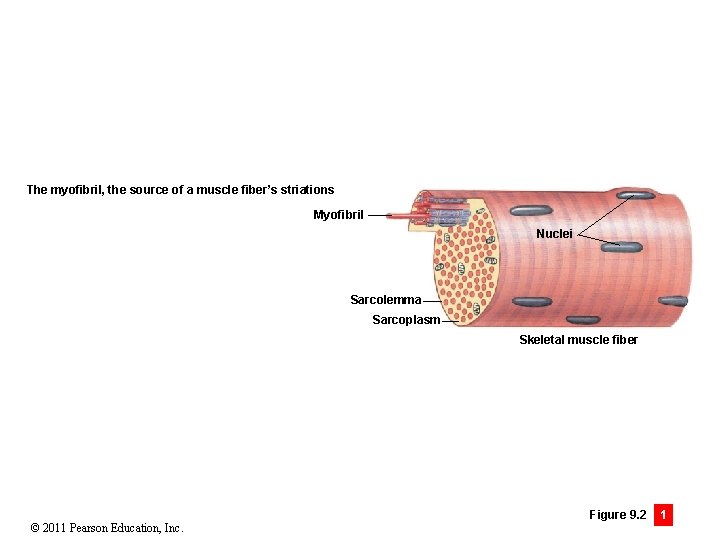
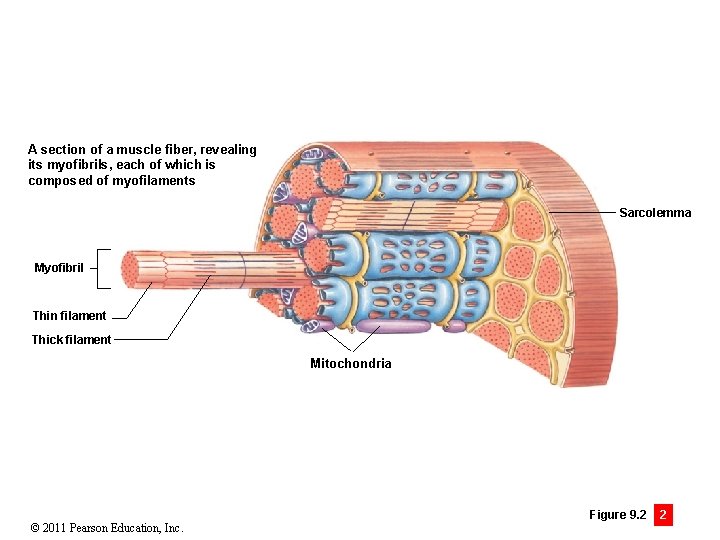
Module 9. 2: Skeletal muscle fiber anatomy • Myofibrils • Cylindrical structures 1– 2 µm in diameter and as long as muscle fiber • Hundreds to thousands comprise an individual muscle cell • Each is banded and gives the skeletal muscle cells their banded appearance • Made of protein filaments (= myofilaments) • Thin filaments (primarily actin) • Thick filaments (primarily myosin) © 2011 Pearson Education, Inc.
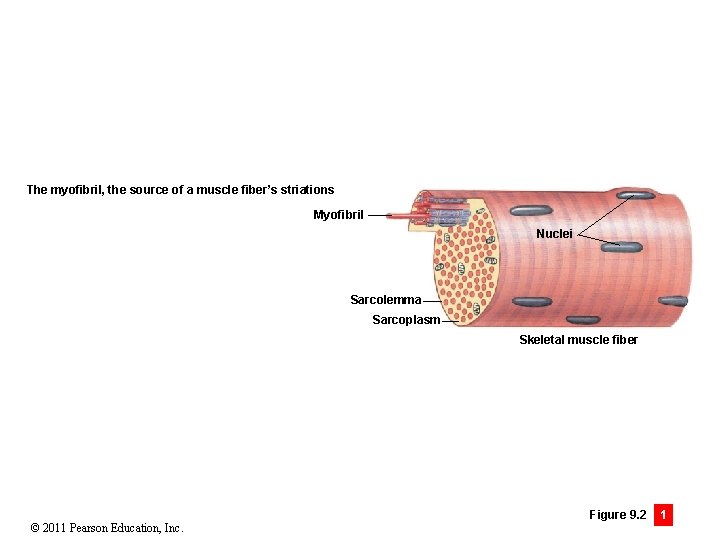
The myofibril, the source of a muscle fiber’s striations Myofibril Nuclei Sarcolemma Sarcoplasm Skeletal muscle fiber © 2011 Pearson Education, Inc. Figure 9. 2 1
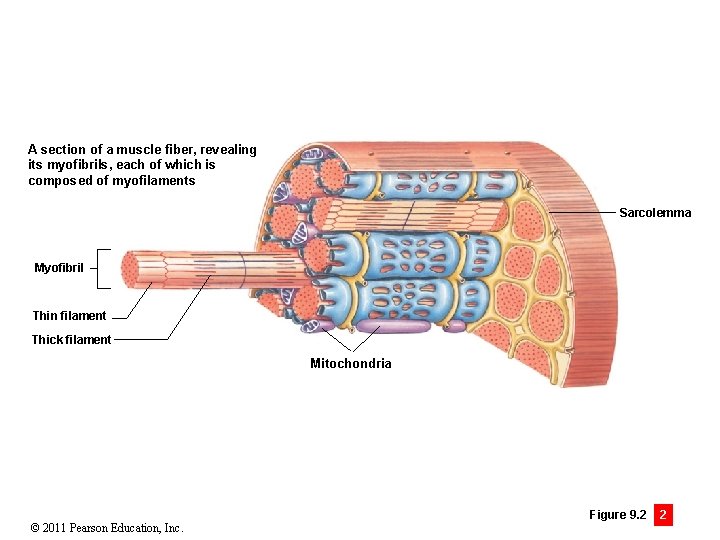
A section of a muscle fiber, revealing its myofibrils, each of which is composed of myofilaments Sarcolemma Myofibril Thin filament Thick filament Mitochondria © 2011 Pearson Education, Inc. Figure 9. 2 2
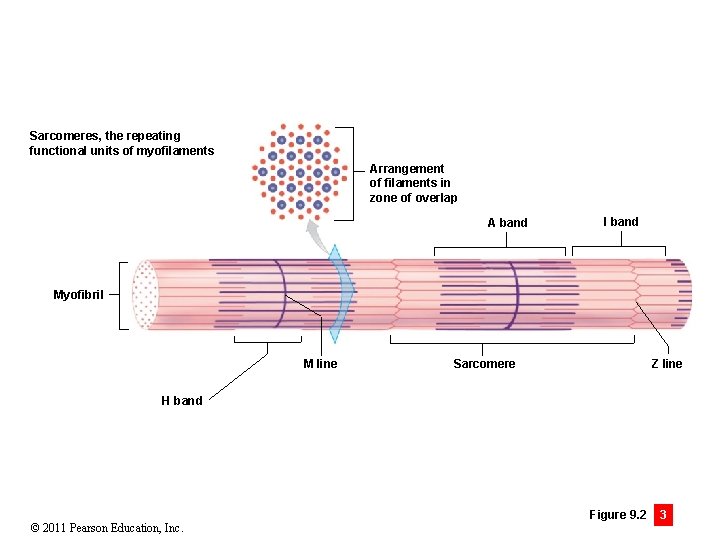
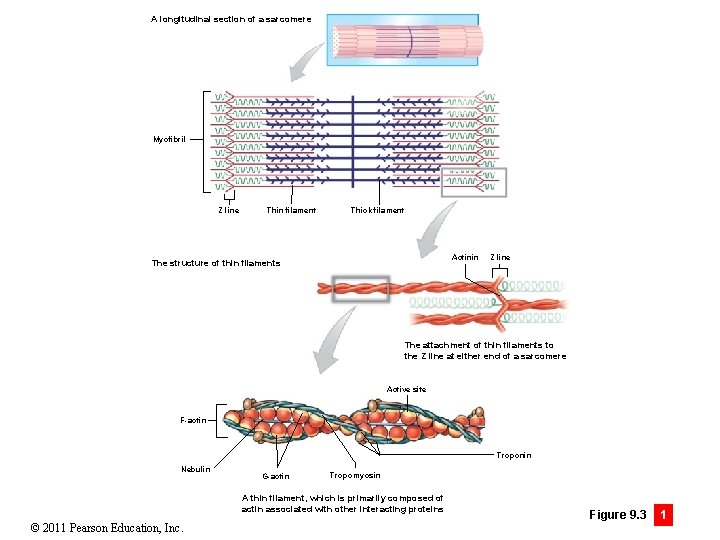
Module 9. 2: Skeletal muscle fiber anatomy • Myofilament structure • Have repeating functional units called sarcomeres (sarkos, flesh + meros, part) • Approximately 10, 000 sarcomeres/myofibril • Each sarcomere has a 2 -µm resting length • Zone of overlap • • Thin and thick filaments interspersed Z lines • Boundary of adjacent sarcomeres • Interconnect thin filaments from adjacent sarcomeres • Consist of proteins (actinins) © 2011 Pearson Education, Inc.
Module 9. 2: Skeletal muscle fiber anatomy • Myofilament structure (continued) • A band • • Dense sarcomere region containing thick filaments I band • Contains thin filaments (no thick) • Extends from A band of one sarcomere to the next A band • M line • • Connects central portion of each thick filament H band • Lighter region around M line • Contains only thick filaments (no thin) © 2011 Pearson Education, Inc.
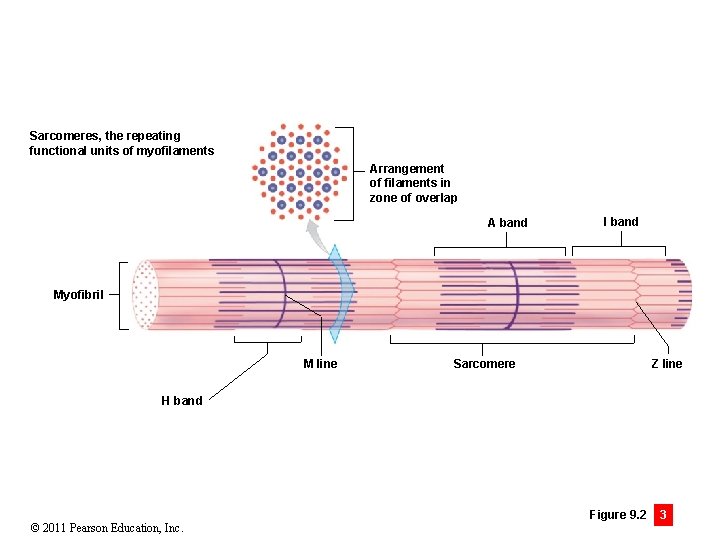
Sarcomeres, the repeating functional units of myofilaments Arrangement of filaments in zone of overlap A band I band Myofibril M line Z line Sarcomere H band © 2011 Pearson Education, Inc. Figure 9. 2 3
Module 9. 2: Skeletal muscle fiber anatomy • Specialized parts of skeletal muscle cells • Sarcolemma • Separates sarcoplasm from interstitial fluid • Maintains distribution of positive and negative charges on either side • = Transmembrane potential • All cells have a characteristic transmembrane potential • Large changes in skeletal muscle transmembrane potential lead to contraction • © 2011 Pearson Education, Inc. Are transmitted along entire muscle cell surface
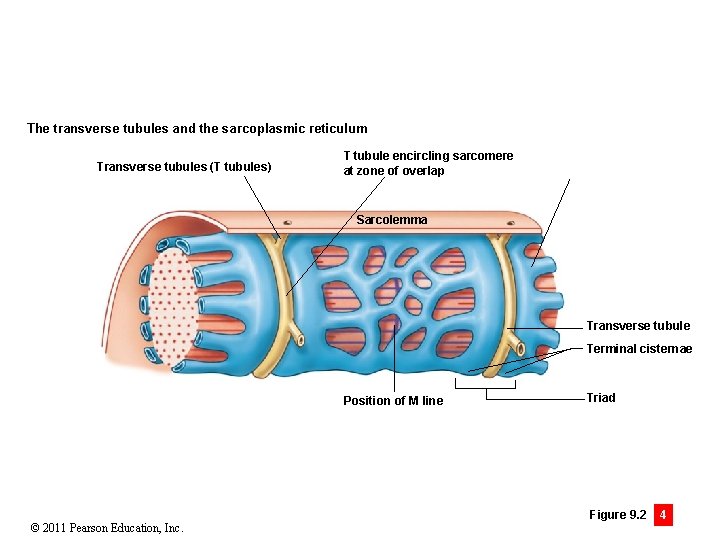
Module 9. 2: Skeletal muscle fiber anatomy • Specialized parts of skeletal muscle cells (continued) • Transverse tubules (T tubules) • Narrow tubes from sarcolemma extending into sarcoplasm • Transmembrane potential changes travel along T tubules to cell interior • Encircle each sarcomere © 2011 Pearson Education, Inc.
Module 9. 2: Skeletal muscle fiber anatomy • Specialized parts of skeletal muscle cells (continued) • Sarcoplasmic reticulum (SR) • Similar to smooth endoplasmic reticulum of other cells • Forms tubular network around each myofibril • On either side of T tubule, forms expanded chambers (terminal cisternae) • T tubule + terminal cisternae = triad © 2011 Pearson Education, Inc.
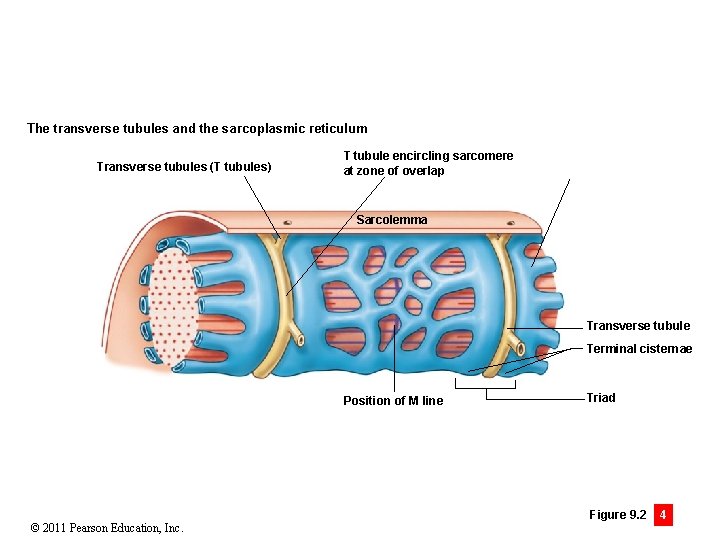
The transverse tubules and the sarcoplasmic reticulum Transverse tubules (T tubules) T tubule encircling sarcomere at zone of overlap Sarcolemma Transverse tubule Terminal cisternae Position of M line © 2011 Pearson Education, Inc. Triad Figure 9. 2 4
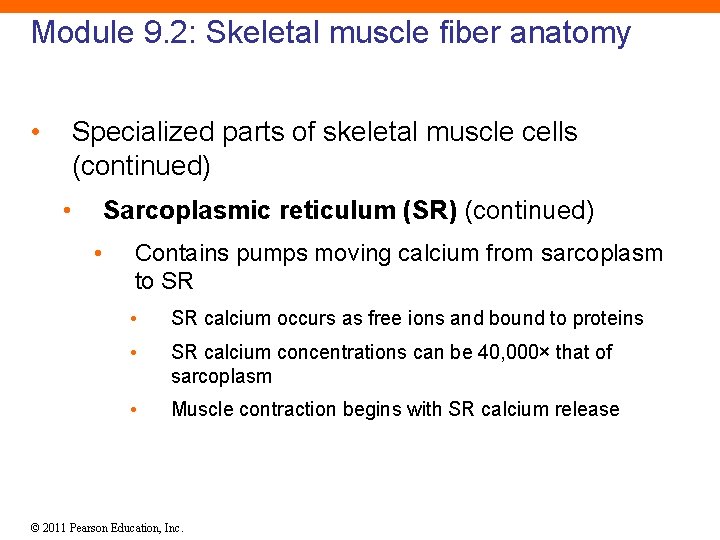
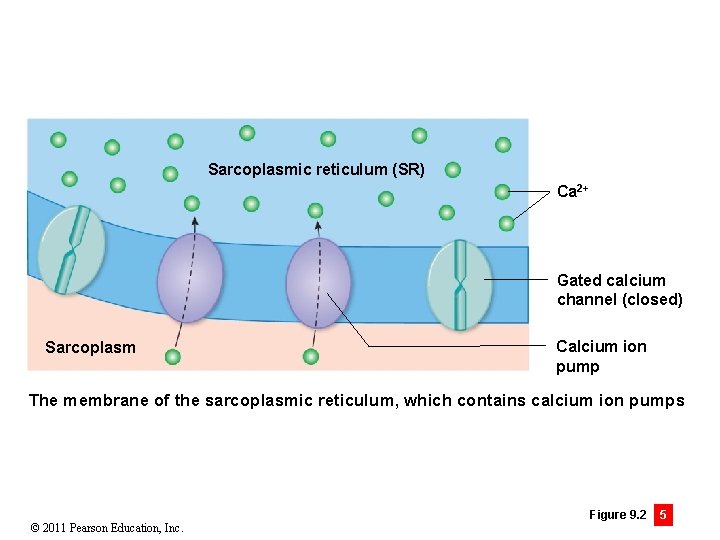
Module 9. 2: Skeletal muscle fiber anatomy • Specialized parts of skeletal muscle cells (continued) • Sarcoplasmic reticulum (SR) (continued) • Contains pumps moving calcium from sarcoplasm to SR • SR calcium occurs as free ions and bound to proteins • SR calcium concentrations can be 40, 000× that of sarcoplasm • Muscle contraction begins with SR calcium release © 2011 Pearson Education, Inc.
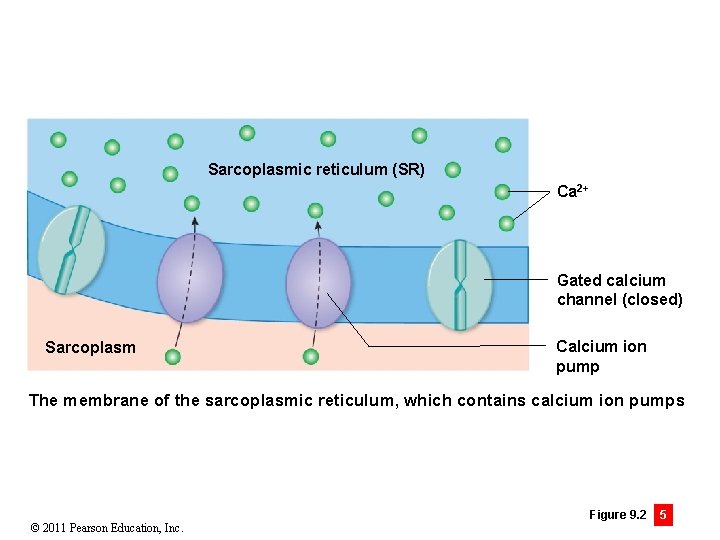
Sarcoplasmic reticulum (SR) Ca 2+ Gated calcium channel (closed) Sarcoplasm Calcium ion pump The membrane of the sarcoplasmic reticulum, which contains calcium ion pumps © 2011 Pearson Education, Inc. Figure 9. 2 5
Module 9. 2 Review a. Define transverse tubules. b. Describe the structural components of a sarcomere. c. Where would you expect the greatest concentration of Ca 2+ to be in a resting skeletal muscle? © 2011 Pearson Education, Inc.
Module 9. 3: Thick and thin filaments • Thin filaments • Attached to Z lines with actinin • 5– 6 µm in diameter, 1 µm in length • Primarily actin • Individual G-actin molecules (with active site for binding myosin) link together to form F-actin (filamentous) • F-actin strand held together with nebulin © 2011 Pearson Education, Inc.
Module 9. 3: Thick and thin filaments • Thin filaments (continued) • Also contain two regulatory proteins 1. 2. Tropomyosin • Covers G-actin active sites and prevents actin–myosin interaction • Attached to troponin Troponin • Consists of three subunits 1. Binds to tropomyosin (forms complex) 2. Binds to G-actin (maintains position on actin) 3. Binds two calcium ions (for activation during contraction) Animation: Muscle Physiology: Troponin © 2011 Pearson Education, Inc.
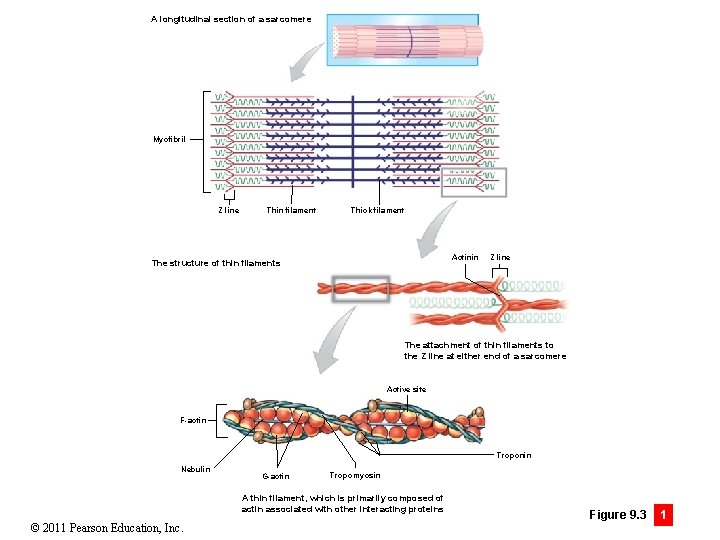
A longitudinal section of a sarcomere Myofibril Z line Thin filament Thick filament Actinin The structure of thin filaments Z line The attachment of thin filaments to the Z line at either end of a sarcomere Active site F-actin Troponin Nebulin G-actin Tropomyosin A thin filament, which is primarily composed of actin associated with other interacting proteins © 2011 Pearson Education, Inc. Figure 9. 3 1
Module 9. 3: Thick and thin filaments • Thick filaments • 10– 12 nm in diameter and 1. 6 µm long • Have core of titin • • Connect to Z lines • Are elastic and recoil after stretching Contain ~300 myosin molecules © 2011 Pearson Education, Inc.
Module 9. 3: Thick and thin filaments • Thick filaments (continued) • Myosin molecule • Has long tail bound to other myosin molecules • Has two globular subunits (= free head) • • Forms cross-bridges with actin during contraction Connection between head and tail allows a hinge-like (pivot) motion Animation: Muscle Physiology: Myosin Parts Animation: Muscle Physiology: Muscle Proteins © 2011 Pearson Education, Inc.
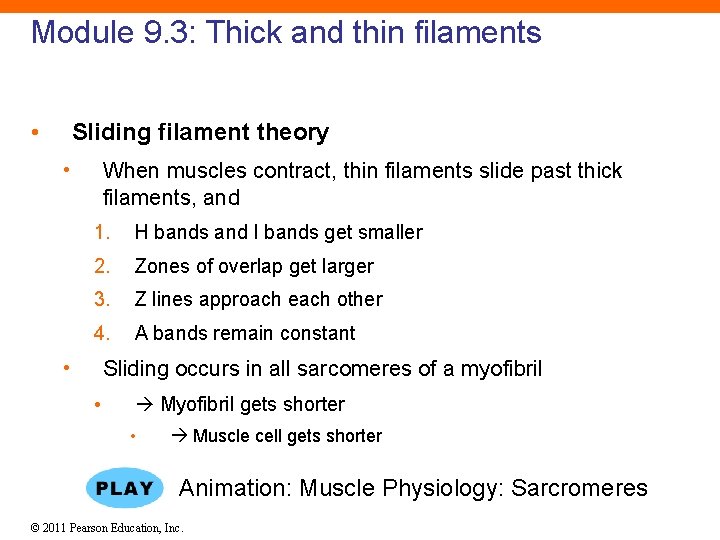
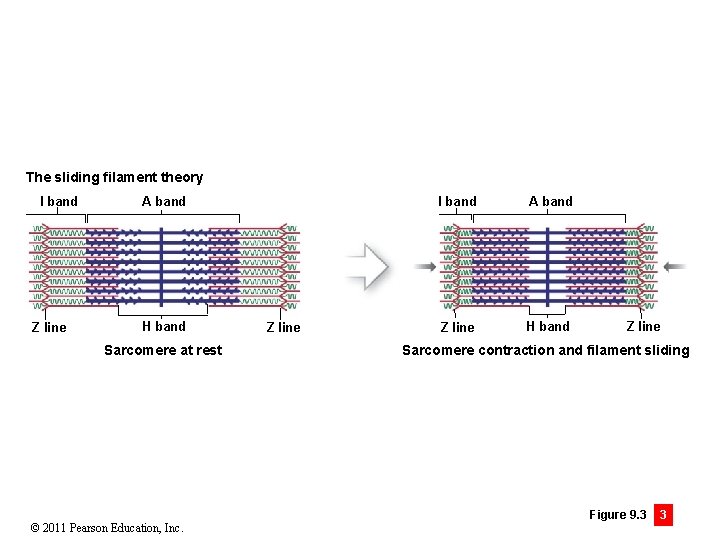
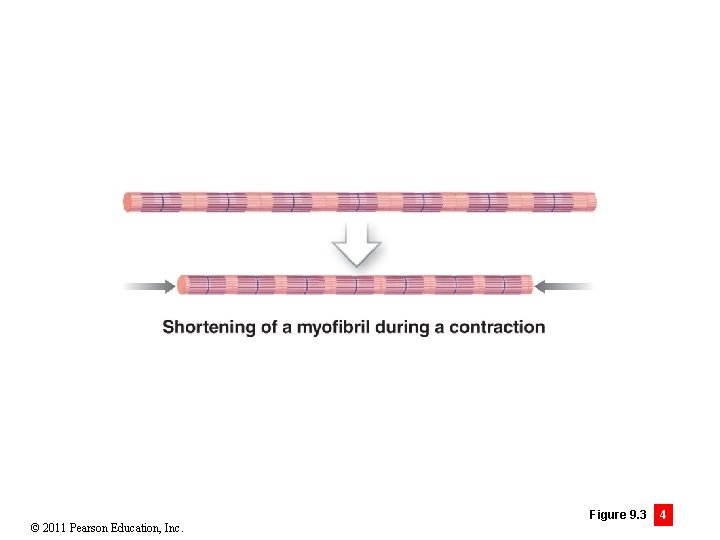
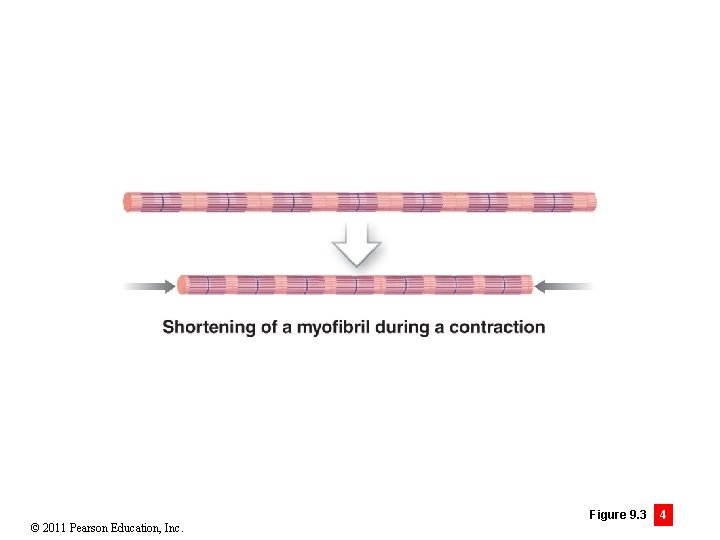
Module 9. 3: Thick and thin filaments • Sliding filament theory • When muscles contract, thin filaments slide past thick filaments, and 1. H bands and I bands get smaller 2. Zones of overlap get larger 3. Z lines approach each other 4. A bands remain constant • Sliding occurs in all sarcomeres of a myofibril • Myofibril gets shorter • Muscle cell gets shorter Animation: Muscle Physiology: Sarcromeres © 2011 Pearson Education, Inc.
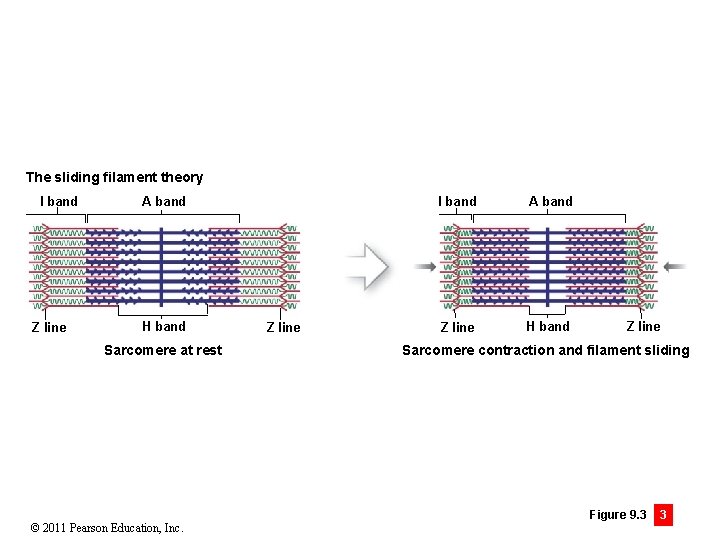
The sliding filament theory I band Z line A band H band Sarcomere at rest © 2011 Pearson Education, Inc. Z line I band A band Z line H band Z line Sarcomere contraction and filament sliding Figure 9. 3 3
© 2011 Pearson Education, Inc. Figure 9. 3 4
Module 9. 3 Review a. Describe the components of thin filaments and thick filaments. b. What gives skeletal muscle its striated appearance? c. Briefly describe the sliding filament theory. © 2011 Pearson Education, Inc.
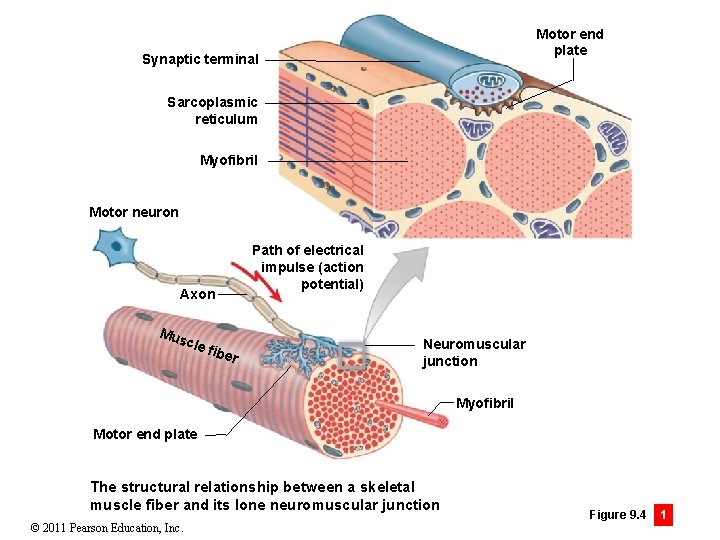
Module 9. 4: Neuromuscular junction • Neuromuscular junction (NMJ) • Intercellular connection between motor neuron and skeletal muscle fiber • Muscle fiber contracts only under control from the NMJ • Only one NMJ per muscle fiber • Although one motor neuron axon may branch to control multiple muscle cells A&P Flix: Events at the Neuromuscular Junction © 2011 Pearson Education, Inc.
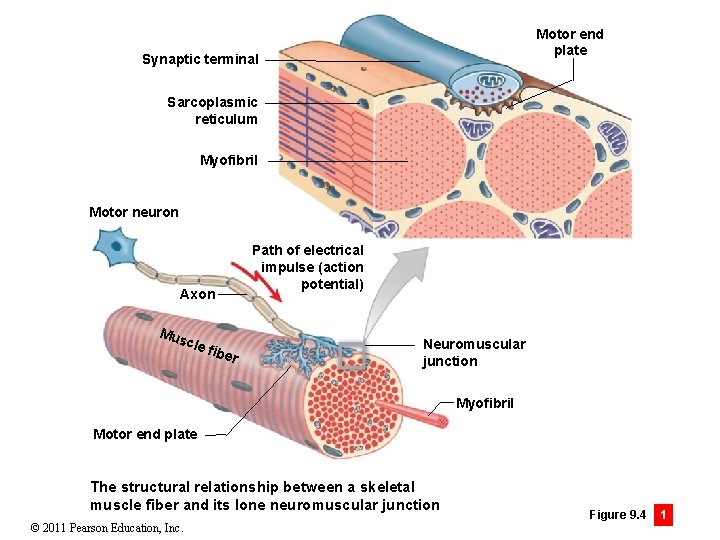
Motor end plate Synaptic terminal Sarcoplasmic reticulum Myofibril Motor neuron Path of electrical impulse (action potential) Axon Mus cle fibe r Neuromuscular junction Myofibril Motor end plate The structural relationship between a skeletal muscle fiber and its lone neuromuscular junction © 2011 Pearson Education, Inc. Figure 9. 4 1
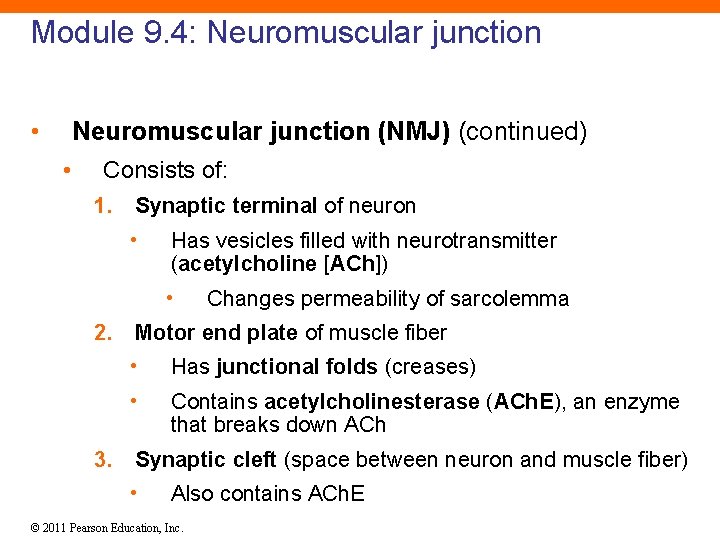
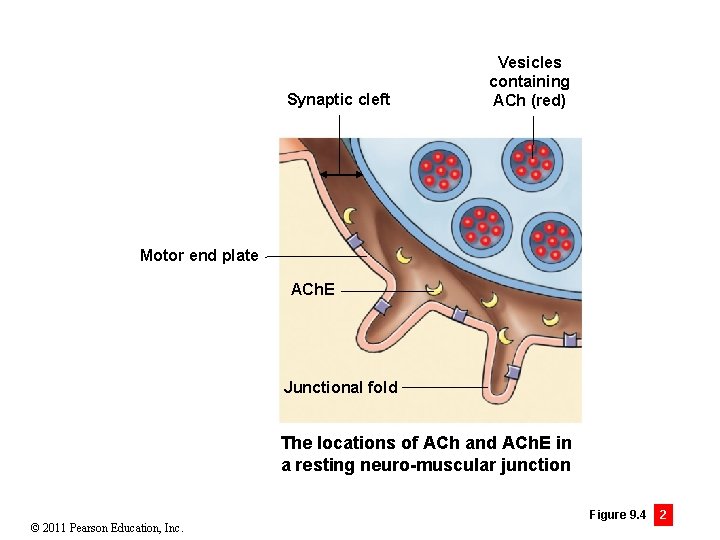
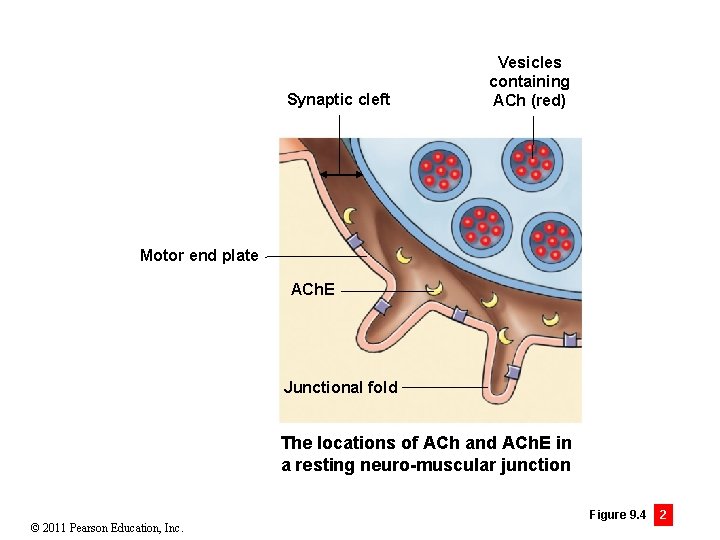
Module 9. 4: Neuromuscular junction • Neuromuscular junction (NMJ) (continued) • Consists of: 1. Synaptic terminal of neuron • Has vesicles filled with neurotransmitter (acetylcholine [ACh]) • Changes permeability of sarcolemma 2. Motor end plate of muscle fiber • Has junctional folds (creases) • Contains acetylcholinesterase (ACh. E), an enzyme that breaks down ACh 3. Synaptic cleft (space between neuron and muscle fiber) • Also contains ACh. E © 2011 Pearson Education, Inc.
Synaptic cleft Vesicles containing ACh (red) Motor end plate ACh. E Junctional fold The locations of ACh and ACh. E in a resting neuro-muscular junction © 2011 Pearson Education, Inc. Figure 9. 4 2
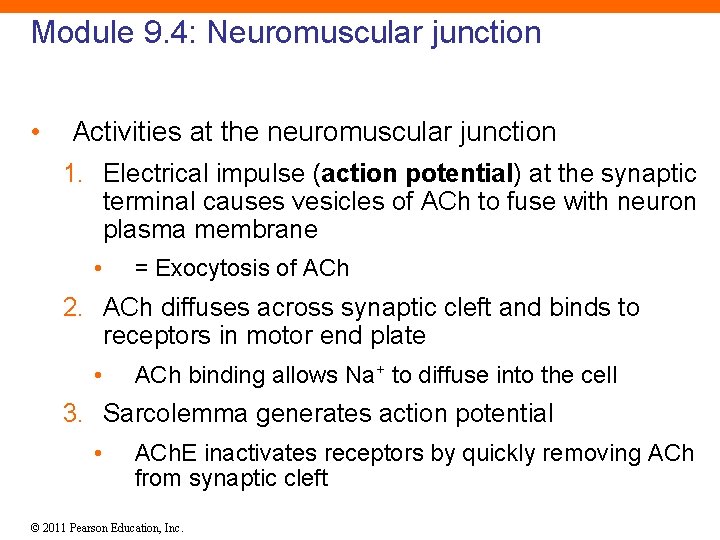
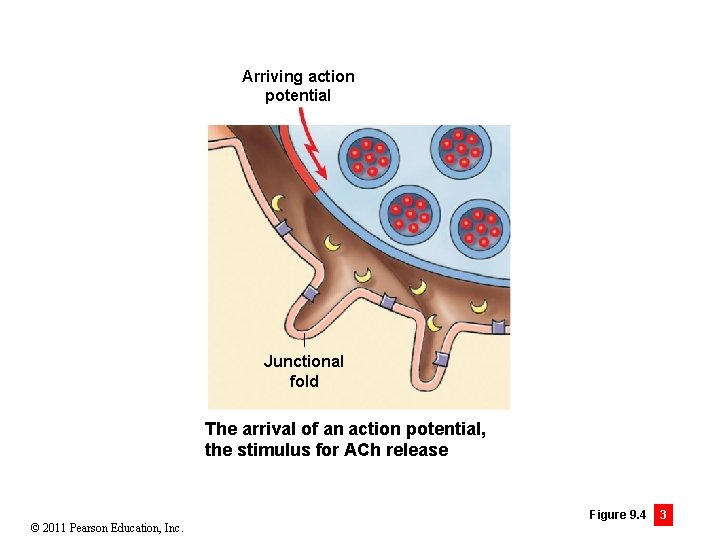
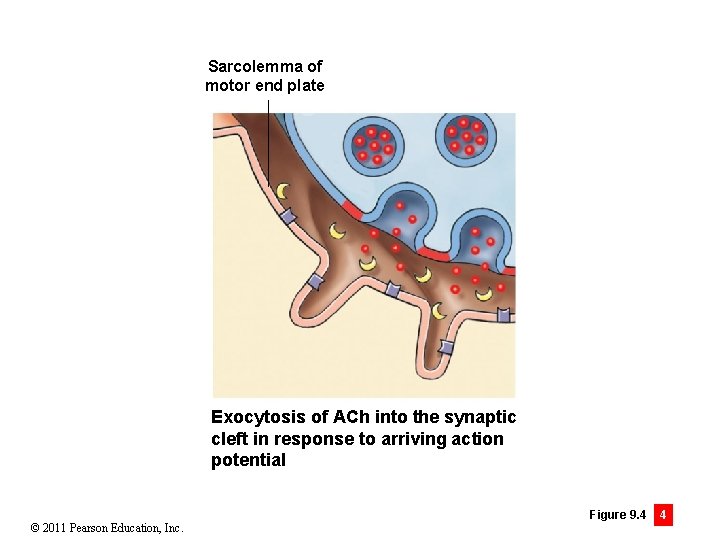
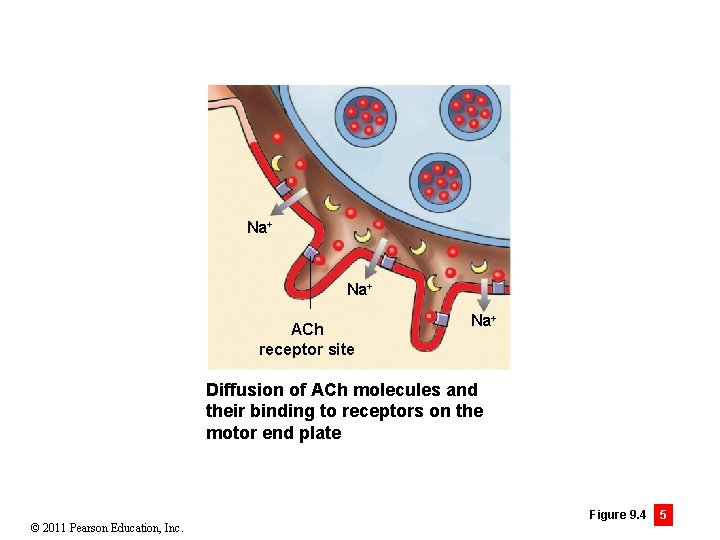
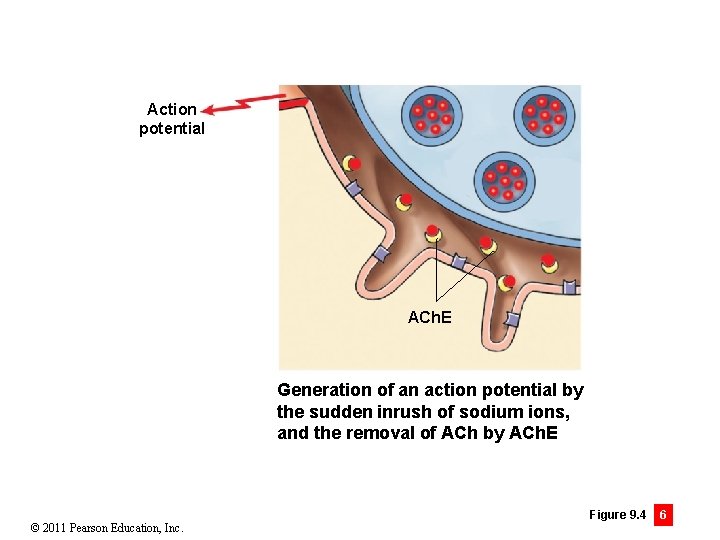
Module 9. 4: Neuromuscular junction • Activities at the neuromuscular junction 1. Electrical impulse (action potential) at the synaptic terminal causes vesicles of ACh to fuse with neuron plasma membrane • = Exocytosis of ACh 2. ACh diffuses across synaptic cleft and binds to receptors in motor end plate • ACh binding allows Na+ to diffuse into the cell 3. Sarcolemma generates action potential • ACh. E inactivates receptors by quickly removing ACh from synaptic cleft © 2011 Pearson Education, Inc.
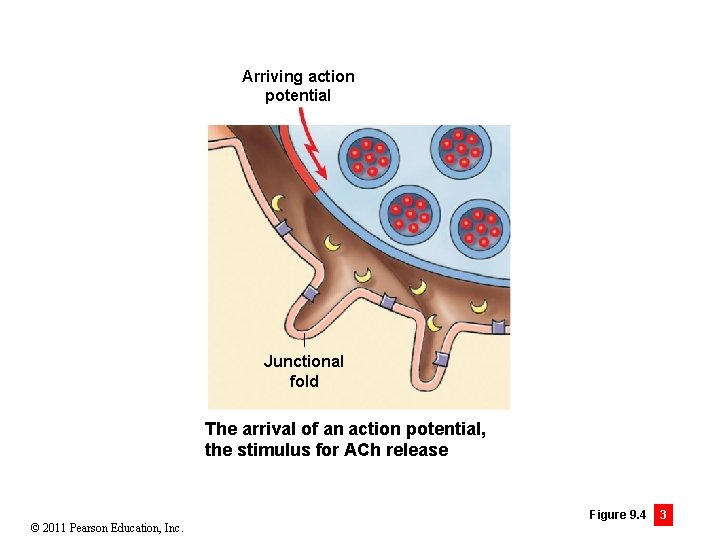
Arriving action potential Junctional fold The arrival of an action potential, the stimulus for ACh release © 2011 Pearson Education, Inc. Figure 9. 4 3
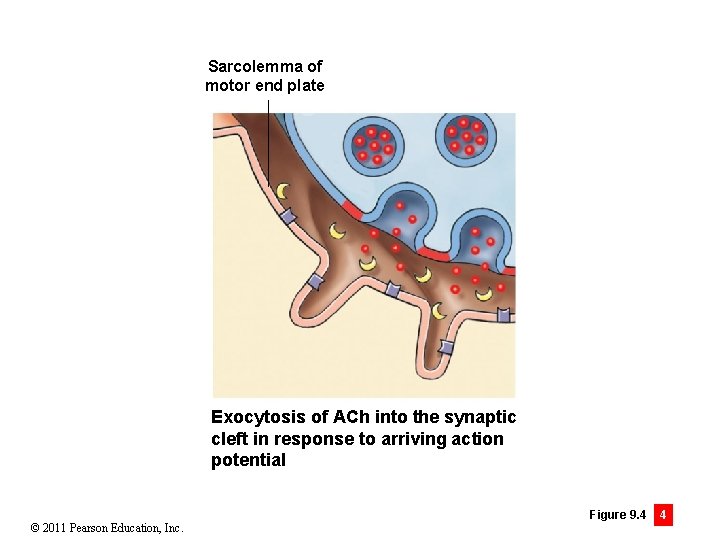
Sarcolemma of motor end plate Exocytosis of ACh into the synaptic cleft in response to arriving action potential © 2011 Pearson Education, Inc. Figure 9. 4 4
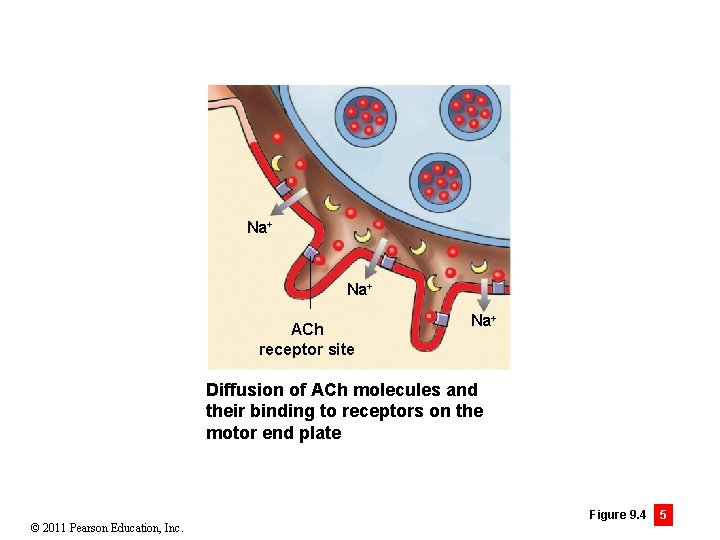
Na+ ACh receptor site Na+ Diffusion of ACh molecules and their binding to receptors on the motor end plate © 2011 Pearson Education, Inc. Figure 9. 4 5
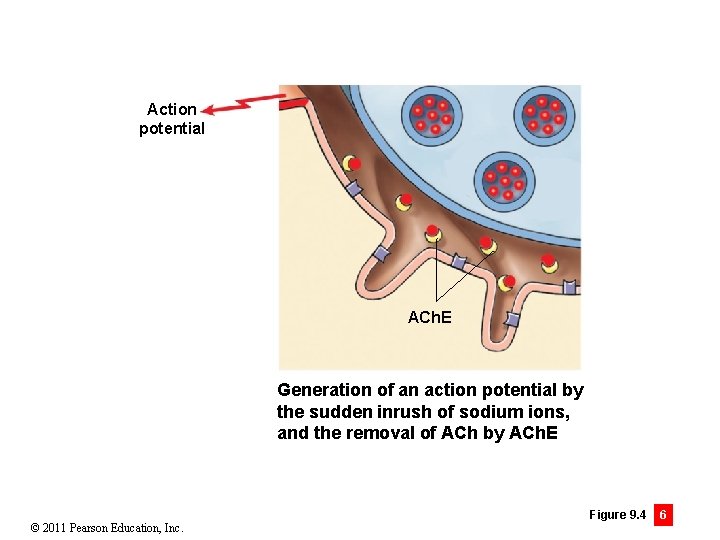
Action potential ACh. E Generation of an action potential by the sudden inrush of sodium ions, and the removal of ACh by ACh. E © 2011 Pearson Education, Inc. Figure 9. 4 6
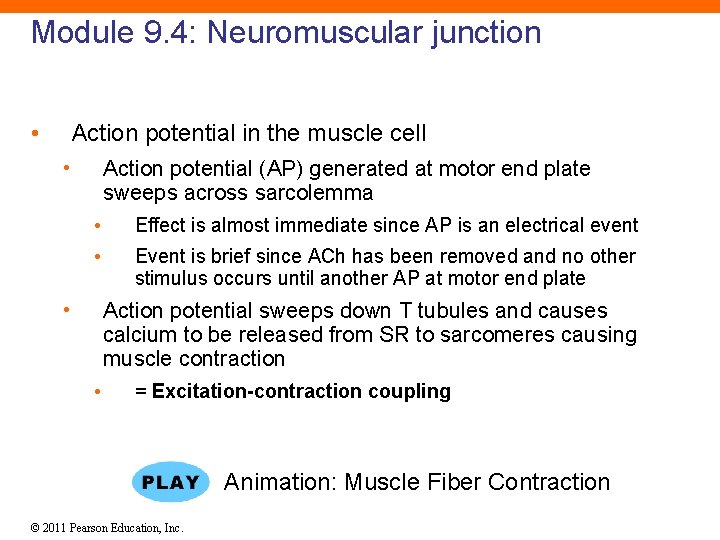
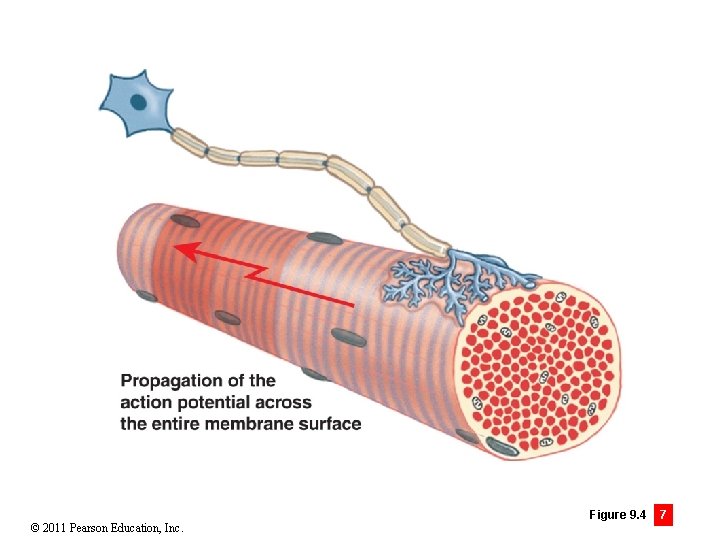
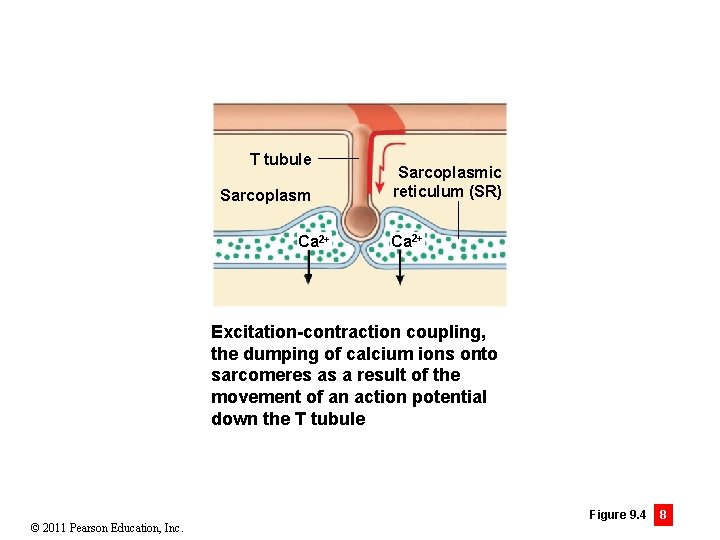
Module 9. 4: Neuromuscular junction • Action potential in the muscle cell • Action potential (AP) generated at motor end plate sweeps across sarcolemma • Effect is almost immediate since AP is an electrical event • Event is brief since ACh has been removed and no other stimulus occurs until another AP at motor end plate • Action potential sweeps down T tubules and causes calcium to be released from SR to sarcomeres causing muscle contraction • = Excitation-contraction coupling Animation: Muscle Fiber Contraction © 2011 Pearson Education, Inc.
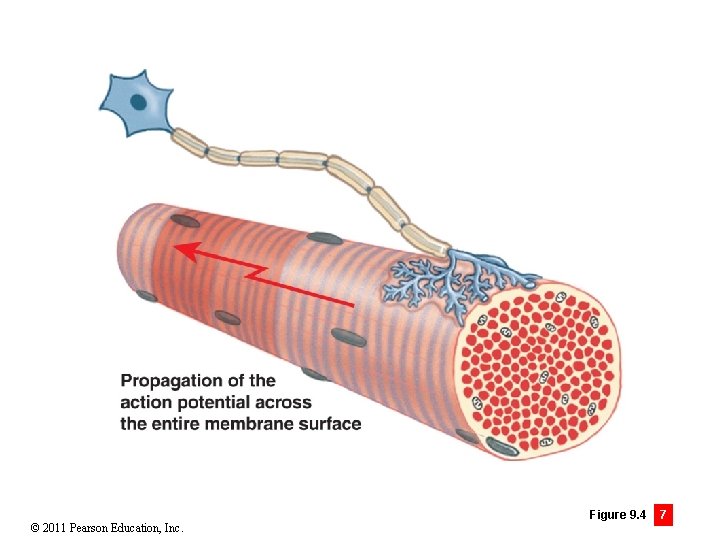
© 2011 Pearson Education, Inc. Figure 9. 4 7
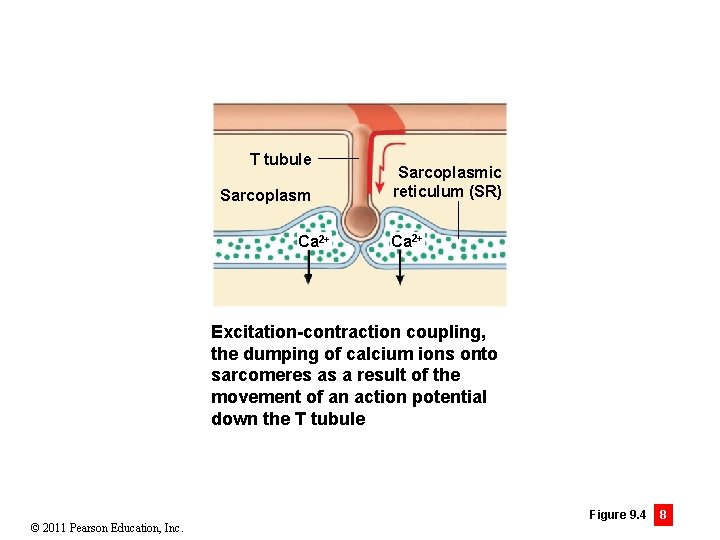
T tubule Sarcoplasm Ca 2+ Sarcoplasmic reticulum (SR) Ca 2+ Excitation-contraction coupling, the dumping of calcium ions onto sarcomeres as a result of the movement of an action potential down the T tubule © 2011 Pearson Education, Inc. Figure 9. 4 8
Module 9. 4 Review a. Describe the neuromuscular junction. b. How would a drug that blocks acetylcholine release affect muscle contraction? c. Predict what would happen if there were no ACh. E in the synaptic cleft. © 2011 Pearson Education, Inc.
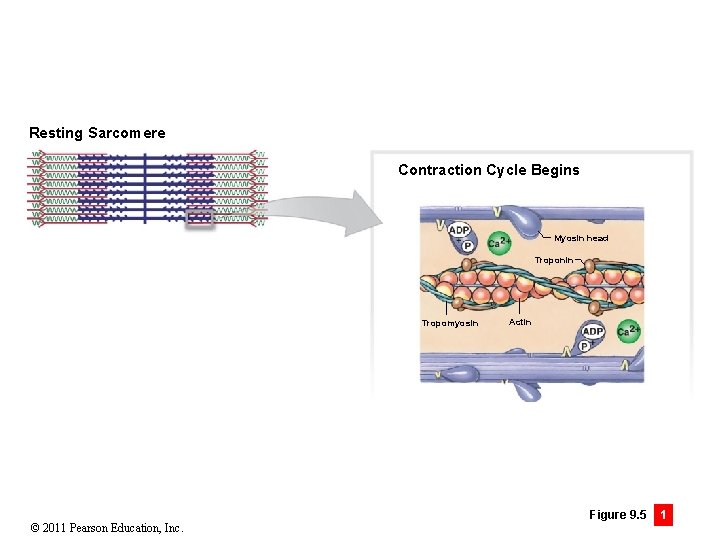
Module 9. 5: Muscle fiber contraction cycle • Resting sarcomere • Each myosin head is already “energized” and “cocked” (heads pointing away from M line) • Energy supplied by breakdown of ATP by myosin • Myosin acting as an ATPase • Breakdown products (ADP and P) still attached to myosin head © 2011 Pearson Education, Inc.
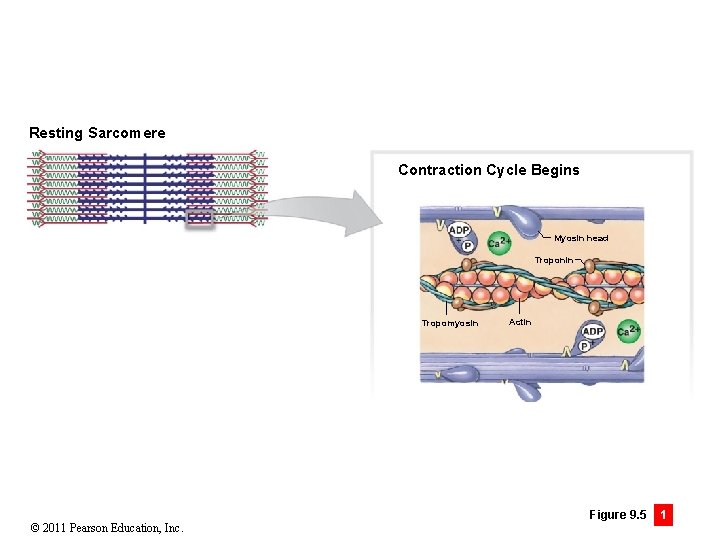
Resting Sarcomere Contraction Cycle Begins Myosin head Troponin Tropomyosin © 2011 Pearson Education, Inc. Actin Figure 9. 5 1
Module 9. 5: Muscle fiber contraction cycle • Steps of muscle fiber contraction cycle 1. Contraction cycle begins • Arrival of calcium ions at zone of overlap 2. Active-site exposure • Calcium binds to troponin • • Weakens bond between actin and troponin– tropomyosin complex Troponin changes position, exposing active sites on actin 3. Cross-bridge formation • Myosin heads bind to exposed active sites on actin forming cross-bridges © 2011 Pearson Education, Inc.
Module 9. 5: Muscle fiber contraction cycle • Steps of muscle fiber contraction cycle (continued) 4. Myosin head pivoting • Stored energy within myosin head releases and head pivots toward M line • • = Power stroke ADP and P are released from myosin head 5. Cross-bridge detachment • Attachment of new ATP causes release of myosin from actin • Exposes active site again formation of another cross-bridge 6. Myosin reactivation • New ATP broken down and head “recocks” © 2011 Pearson Education, Inc.
Module 9. 5: Muscle fiber contraction cycle A&P Flix: The Cross Bridge Cycle Animation: Muscle Physiology: Intracellular Calcium Proteins © 2011 Pearson Education, Inc.
Module 9. 5: Muscle fiber contraction cycle • Contracted sarcomere • Entire cycle repeated as long as Ca 2+ concentrations remain high and ATP is available • • Calcium levels remain high as long as action potentials continue down T tubules Once stimulus is removed • SR calcium channels close • Calcium pumps move Ca 2+ from sarcoplasm into terminal cisternae • Troponin–tropomyosin complex moves to cover active sites, preventing further cross-bridge formation Animation: Muscle Physiology: Muscle Cycles of Attachment and Detachment © 2011 Pearson Education, Inc.
Module 9. 5 Review a. What molecule supplies the energy for a muscle contraction? b. List the interrelated steps that occur once the contraction cycle has begun. c. What triggers myosin reactivation? © 2011 Pearson Education, Inc.
Section 2: Functional Properties of Skeletal Muscle Tissue • Learning Outcomes • 9. 6 Describe the mechanism responsible for tension production in a muscle fiber, and discuss the factors that determine the peak tension developed during a contraction. • 9. 7 Discuss the factors that affect peak tension production during the contraction of an entire skeletal muscle, and explain the significance of the motor unit in this process. • 9. 8 Compare the different types of muscle contractions. © 2011 Pearson Education, Inc.
Section 2: Functional Properties of Skeletal Muscle Tissue • Learning Outcomes • 9. 9 Describe the mechanisms by which muscle fibers obtain the energy to power contractions. • 9. 10 Describe the factors that contribute to muscle fatigue, and discuss the stages and mechanisms involved in the muscle’s subsequent recovery. • 9. 11 Relate the types of muscle fibers to muscle performance. • 9. 12 CLINICAL MODULE Explain the physiological factors responsible for muscle hypertrophy, and paralysis. © 2011 Pearson Education, Inc.
Section 2: Functional Properties of Skeletal Muscle Tissue • Review • Neural control • Skeletal muscle fibers contract when stimulated by motor neuron at neuromuscular junction • Stimulus is an action potential (AP) at synaptic terminal • Excitation-contraction coupling • AP causes release of ACh into synaptic cleft • ACh binds to motor end plate receptors opening Na+ channels • Leads to AP in sarcolemma • AP travels along T tubules causing release of Ca 2+ from terminal cisternae of SR © 2011 Pearson Education, Inc.
Section 2: Functional Properties of Skeletal Muscle Tissue • Review (continued) • Excitation-contraction coupling (continued) • Contraction cycle begins and continues as long as ATP is available and APs are still produced at motor end plate • Thick and thin filaments interact, shortening sarcomeres/muscle fibers/muscle • Contraction of entire muscle produces a pull or tension © 2011 Pearson Education, Inc.
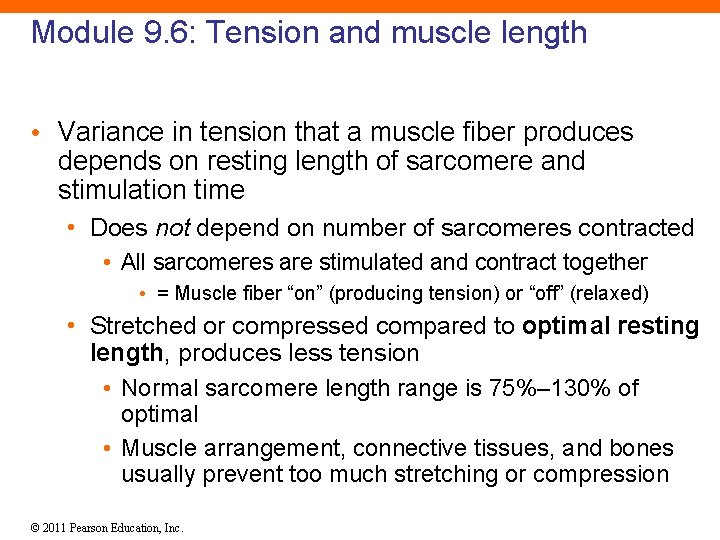
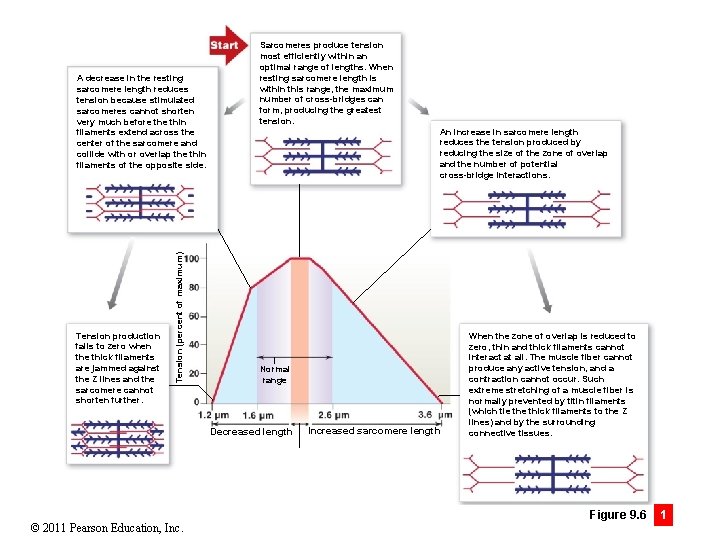
Module 9. 6: Tension and muscle length • Variance in tension that a muscle fiber produces depends on resting length of sarcomere and stimulation time • Does not depend on number of sarcomeres contracted • All sarcomeres are stimulated and contract together • = Muscle fiber “on” (producing tension) or “off” (relaxed) • Stretched or compressed compared to optimal resting length, produces less tension • Normal sarcomere length range is 75%– 130% of optimal • Muscle arrangement, connective tissues, and bones usually prevent too much stretching or compression © 2011 Pearson Education, Inc.
Module 9. 6: Tension and muscle length • Tension within optimal sarcomere lengths • Maximum number of cross-bridges can form • Produces greatest tension • Tension at increased (stretched) sarcomere lengths • Reduction in tension due to reduction in size of zone of overlap and number of cross-bridges • At extreme lengths, no zone of overlap exists and no tension can be generated • Normally prevented by titin filaments (tie thick filaments to Z lines) and connective tissues © 2011 Pearson Education, Inc.
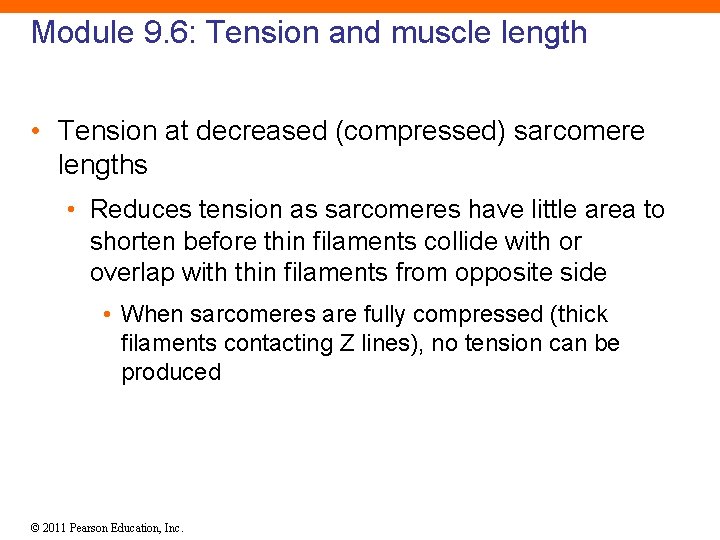
Module 9. 6: Tension and muscle length • Tension at decreased (compressed) sarcomere lengths • Reduces tension as sarcomeres have little area to shorten before thin filaments collide with or overlap with thin filaments from opposite side • When sarcomeres are fully compressed (thick filaments contacting Z lines), no tension can be produced © 2011 Pearson Education, Inc.
Tension production falls to zero when the thick filaments are jammed against the Z lines and the sarcomere cannot shorten further. Tension (percent of maximum) A decrease in the resting sarcomere length reduces tension because stimulated sarcomeres cannot shorten very much before thin filaments extend across the center of the sarcomere and collide with or overlap the thin filaments of the opposite side. Sarcomeres produce tension most efficiently within an optimal range of lengths. When resting sarcomere length is within this range, the maximum number of cross-bridges can form, producing the greatest tension. An increase in sarcomere length reduces the tension produced by reducing the size of the zone of overlap and the number of potential cross-bridge interactions. Normal range Decreased length © 2011 Pearson Education, Increased sarcomere length When the zone of overlap is reduced to zero, thin and thick filaments cannot interact at all. The muscle fiber cannot produce any active tension, and a contraction cannot occur. Such extreme stretching of a muscle fiber is normally prevented by titin filaments (which tie thick filaments to the Z lines) and by the surrounding connective tissues. Figure 9. 6 1
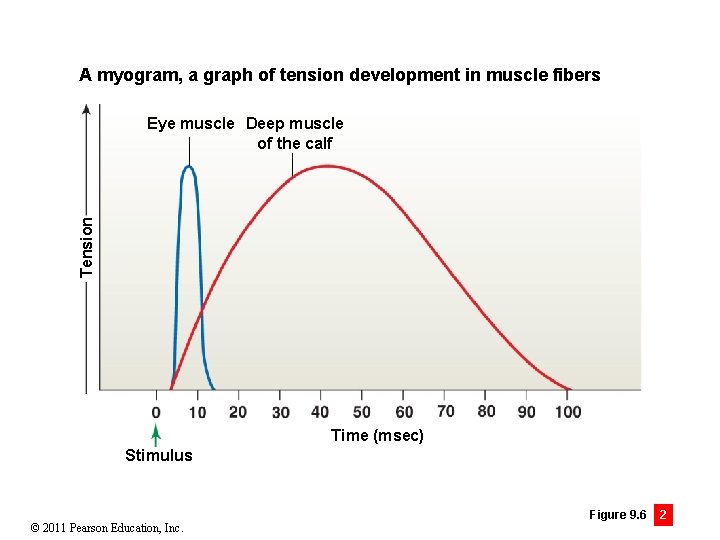
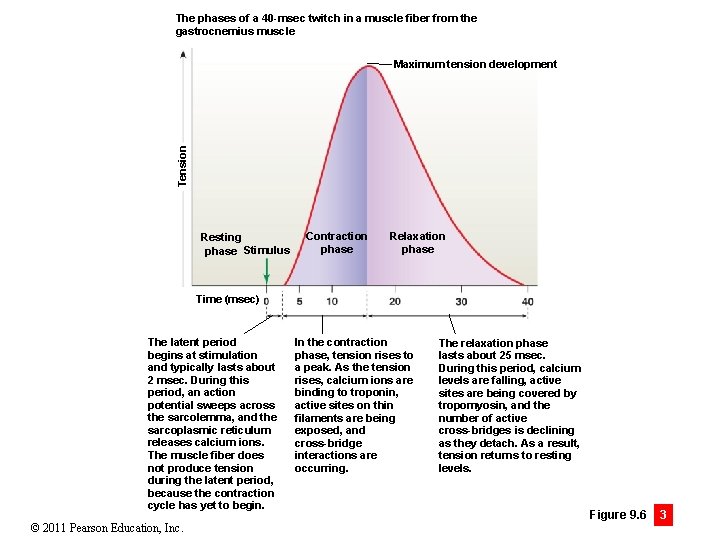
Module 9. 6: Tension and muscle length • Muscle twitch • Single stimulus-contraction-relaxation sequence in a muscle fiber • Vary in duration depending on: • Muscle type • Muscle location • Internal and external conditions • Other factors • Can be viewed on myograms (graph of tension development in muscle fibers) © 2011 Pearson Education, Inc.
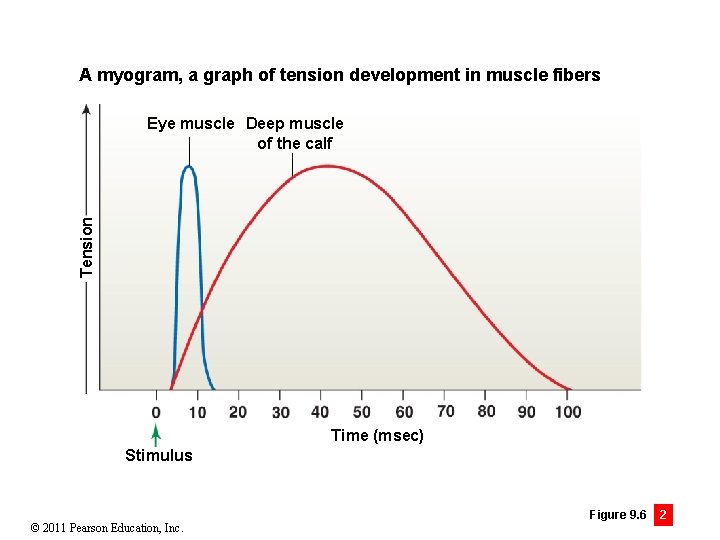
A myogram, a graph of tension development in muscle fibers Tension Eye muscle Deep muscle of the calf Time (msec) Stimulus © 2011 Pearson Education, Inc. Figure 9. 6 2
Module 9. 6: Tension and muscle length • Twitch phases • Latent period • Action potential sweeps across sarcolemma • SR releases calcium ions • Contraction cycle has not begun (= no tension) • Contraction phase • Tension rises to peak • Calcium binds to troponin allowing cross-bridge formation between myosin head and active site on actin © 2011 Pearson Education, Inc.
Module 9. 6: Tension and muscle length • Twitch phases (continued) • Relaxation phase • Calcium levels fall • Active sites covered by tropomyosin • Number of cross-bridges decline with detachment © 2011 Pearson Education, Inc.
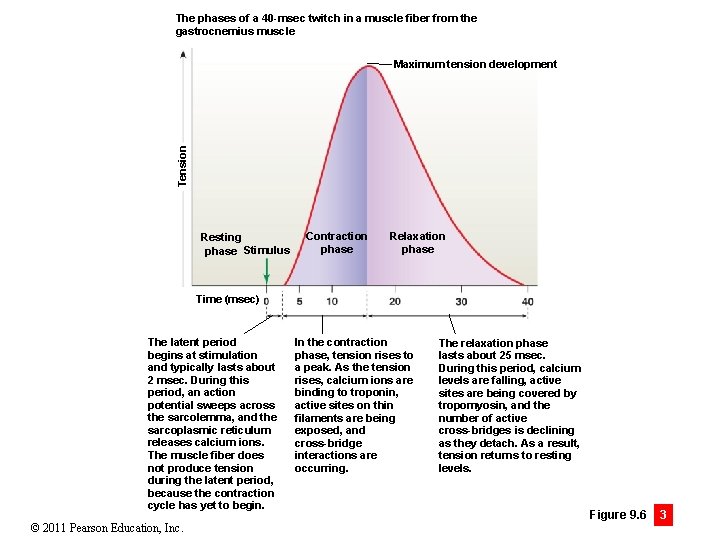
The phases of a 40 -msec twitch in a muscle fiber from the gastrocnemius muscle Tension Maximum tension development Resting phase Stimulus Contraction phase Relaxation phase Time (msec) The latent period begins at stimulation and typically lasts about 2 msec. During this period, an action potential sweeps across the sarcolemma, and the sarcoplasmic reticulum releases calcium ions. The muscle fiber does not produce tension during the latent period, because the contraction cycle has yet to begin. © 2011 Pearson Education, Inc. In the contraction phase, tension rises to a peak. As the tension rises, calcium ions are binding to troponin, active sites on thin filaments are being exposed, and cross-bridge interactions are occurring. The relaxation phase lasts about 25 msec. During this period, calcium levels are falling, active sites are being covered by tropomyosin, and the number of active cross-bridges is declining as they detach. As a result, tension returns to resting levels. Figure 9. 6 3
Module 9. 6 Review a. Name a factor that affects the amount of tension produced when a skeletal muscle contracts. b. Explain two key concepts of the length–tension relationship. c. For each portion of a myogram tracing a twitch in a stimulated gastrocnemius (calf) muscle fiber, describe the events that occur within the muscle. © 2011 Pearson Education, Inc.
Module 9. 7: Developing peak tension • Two factors determine amount of tension produced by a skeletal muscle 1. Amount of tension produced by each muscle fiber • Dependent on stimulation frequency 2. Total number of muscle fibers stimulated © 2011 Pearson Education, Inc.
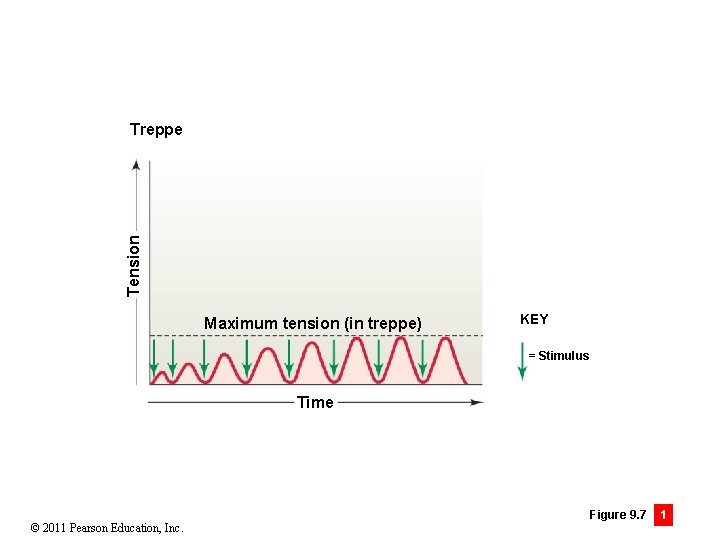
Module 9. 7: Developing peak tension • Effects of stimulation frequency on tension • Treppe (German for staircase) • Stimulation of skeletal muscle fiber immediately after relaxation phase produces increasing maximum tension • Continues for first 30– 50 stimulations • Most skeletal muscles do not demonstrate treppe © 2011 Pearson Education, Inc.
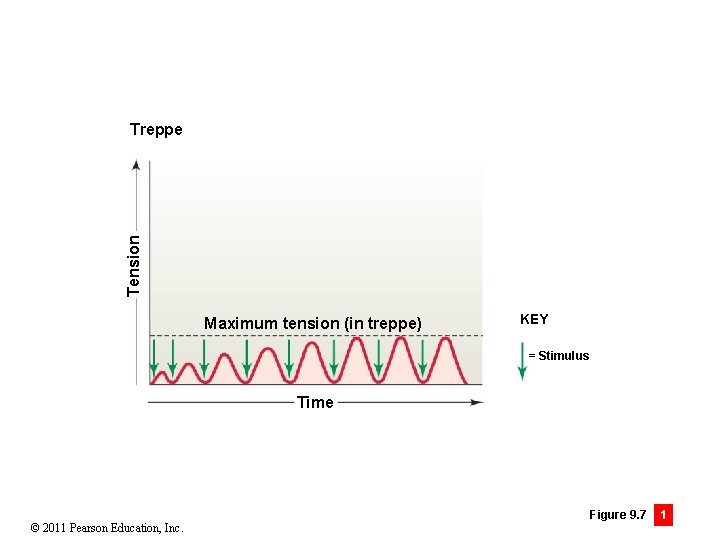
Tension Treppe Maximum tension (in treppe) KEY = Stimulus Time © 2011 Pearson Education, Inc. Figure 9. 7 1
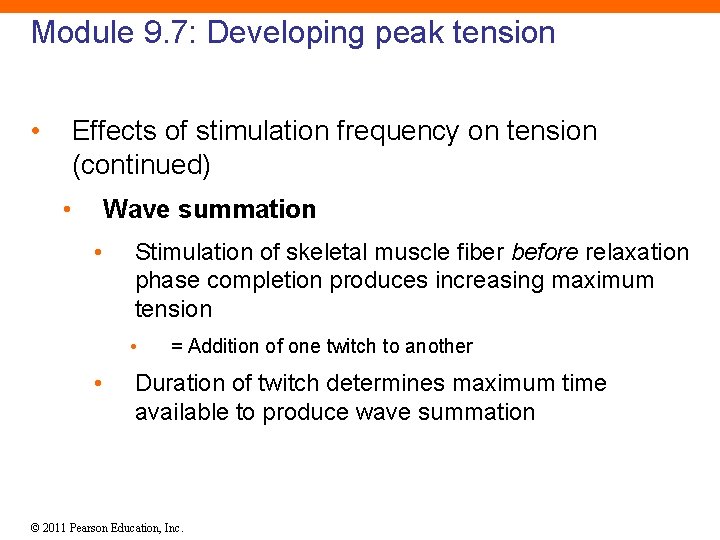
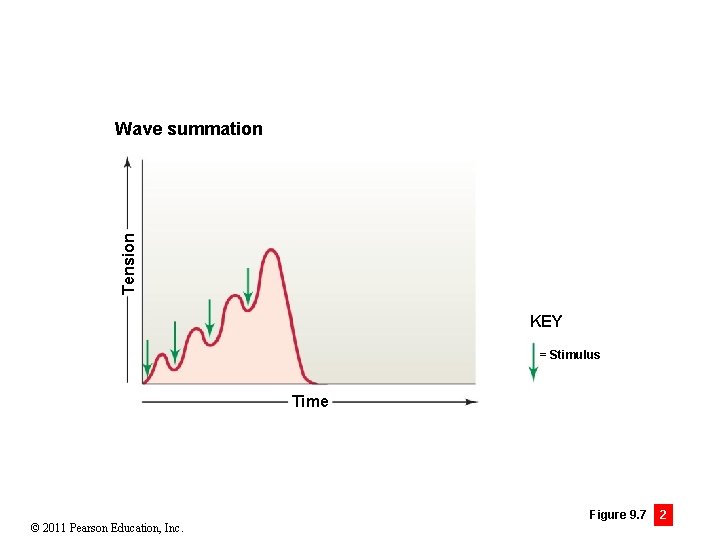
Module 9. 7: Developing peak tension • Effects of stimulation frequency on tension (continued) • Wave summation • Stimulation of skeletal muscle fiber before relaxation phase completion produces increasing maximum tension • • = Addition of one twitch to another Duration of twitch determines maximum time available to produce wave summation © 2011 Pearson Education, Inc.
Tension Wave summation KEY = Stimulus Time © 2011 Pearson Education, Inc. Figure 9. 7 2
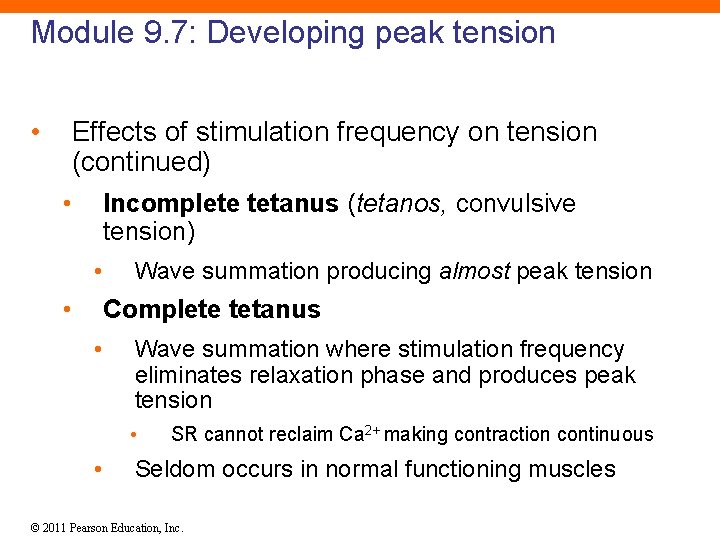
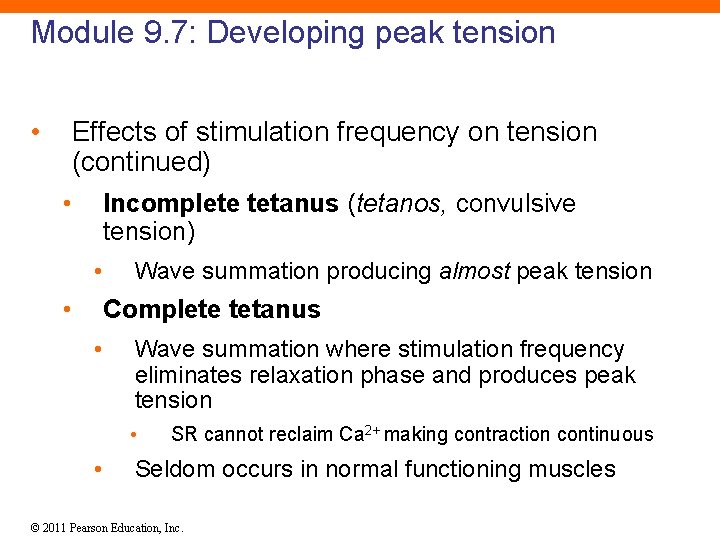
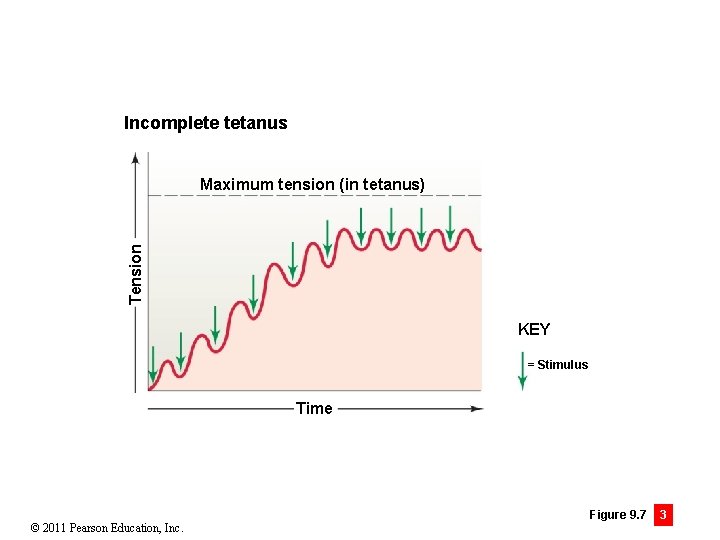
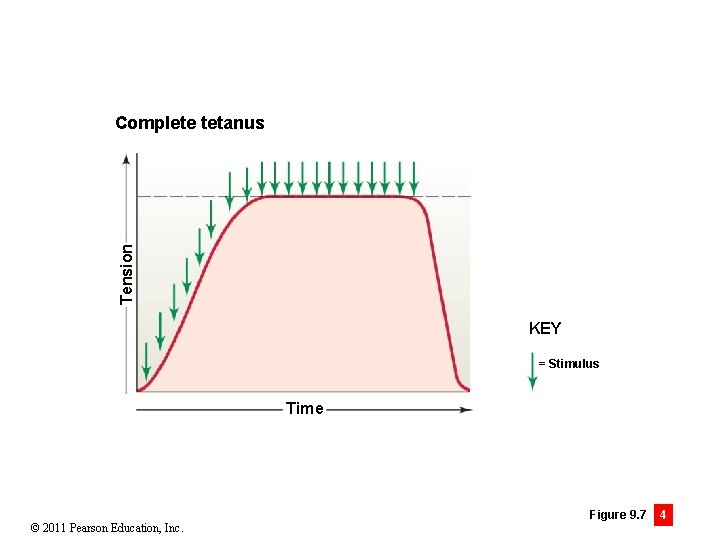
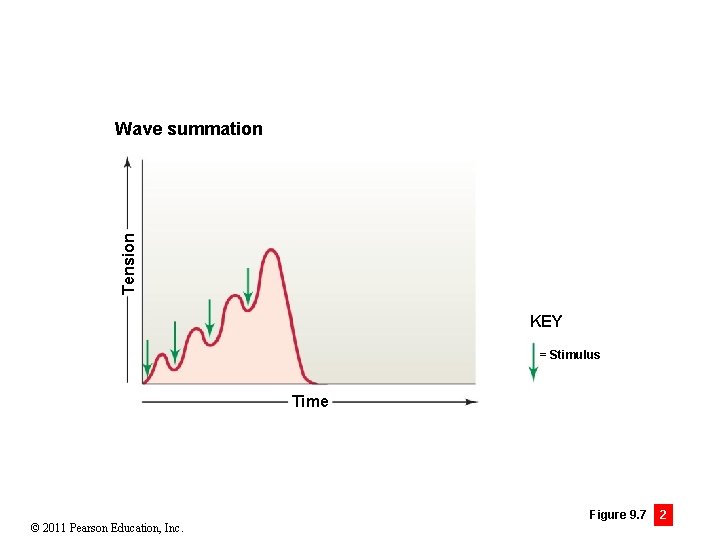
Module 9. 7: Developing peak tension • Effects of stimulation frequency on tension (continued) • Incomplete tetanus (tetanos, convulsive tension) • • Wave summation producing almost peak tension Complete tetanus • Wave summation where stimulation frequency eliminates relaxation phase and produces peak tension • • SR cannot reclaim Ca 2+ making contraction continuous Seldom occurs in normal functioning muscles © 2011 Pearson Education, Inc.
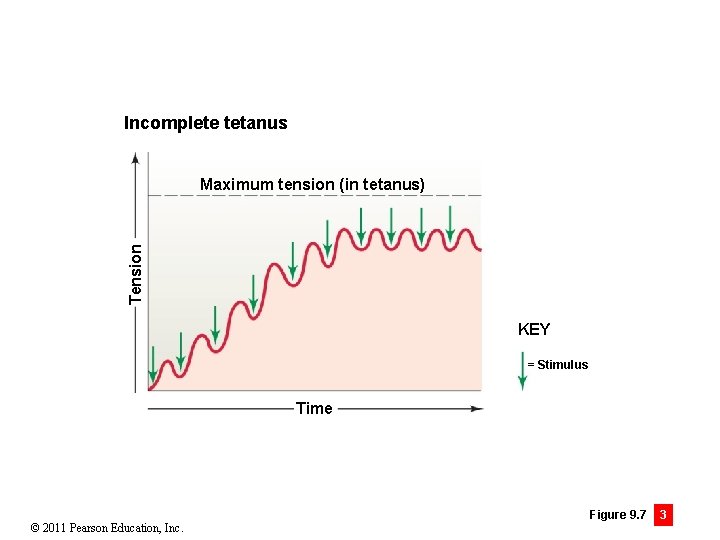
Incomplete tetanus Tension Maximum tension (in tetanus) KEY = Stimulus Time © 2011 Pearson Education, Inc. Figure 9. 7 3
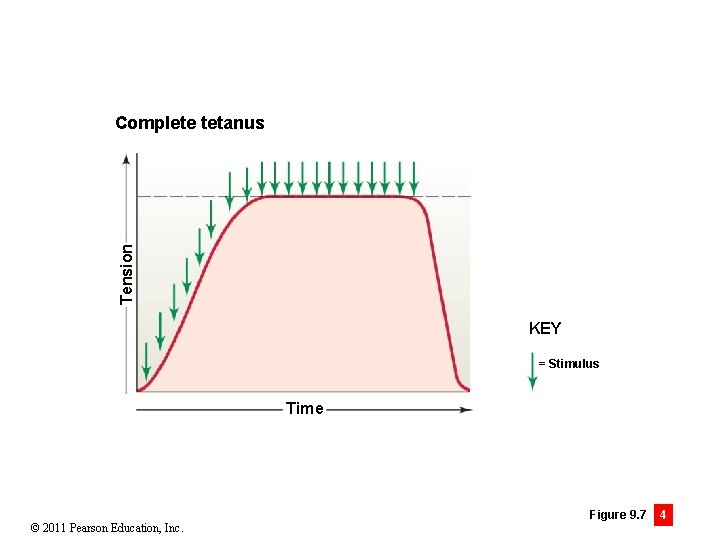
Tension Complete tetanus KEY = Stimulus Time © 2011 Pearson Education, Inc. Figure 9. 7 4
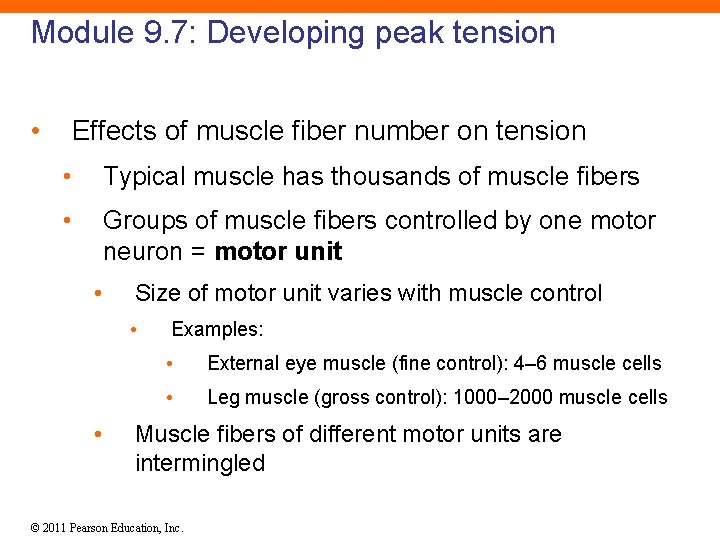
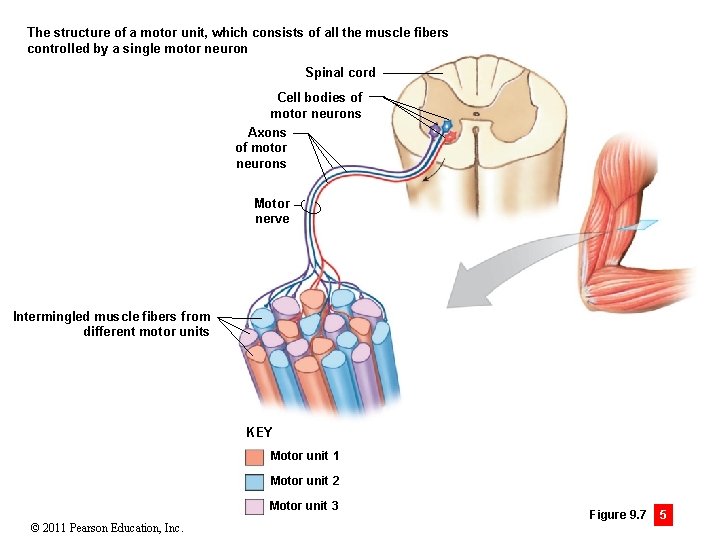
Module 9. 7: Developing peak tension • Effects of muscle fiber number on tension • Typical muscle has thousands of muscle fibers • Groups of muscle fibers controlled by one motor neuron = motor unit • Size of motor unit varies with muscle control • • Examples: • External eye muscle (fine control): 4– 6 muscle cells • Leg muscle (gross control): 1000– 2000 muscle cells Muscle fibers of different motor units are intermingled © 2011 Pearson Education, Inc.
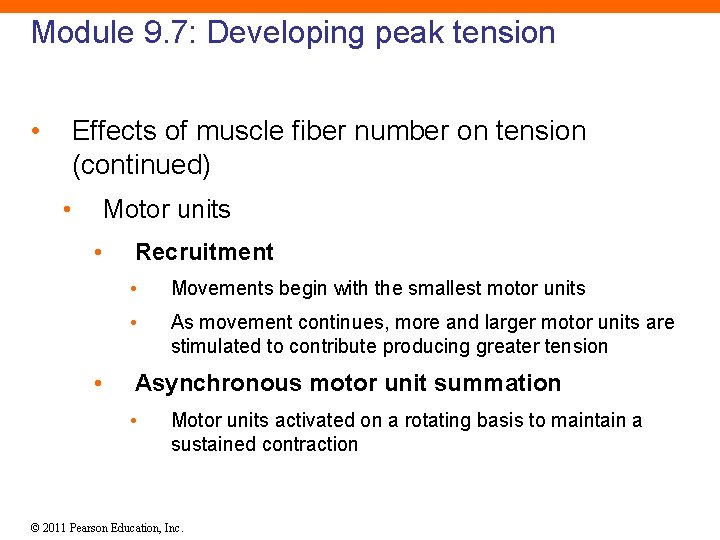
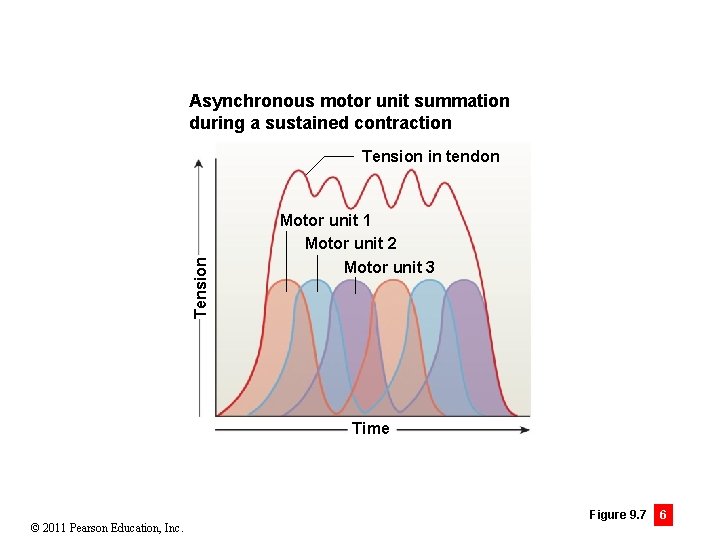
Module 9. 7: Developing peak tension • Effects of muscle fiber number on tension (continued) • Motor units • • Recruitment • Movements begin with the smallest motor units • As movement continues, more and larger motor units are stimulated to contribute producing greater tension Asynchronous motor unit summation • Motor units activated on a rotating basis to maintain a sustained contraction © 2011 Pearson Education, Inc.
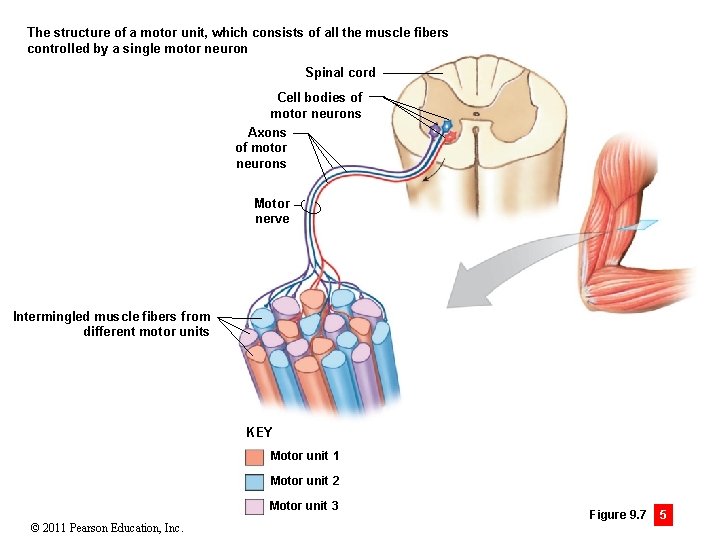
The structure of a motor unit, which consists of all the muscle fibers controlled by a single motor neuron Spinal cord Cell bodies of motor neurons Axons of motor neurons Motor nerve Intermingled muscle fibers from different motor units KEY Motor unit 1 Motor unit 2 Motor unit 3 © 2011 Pearson Education, Inc. Figure 9. 7 5
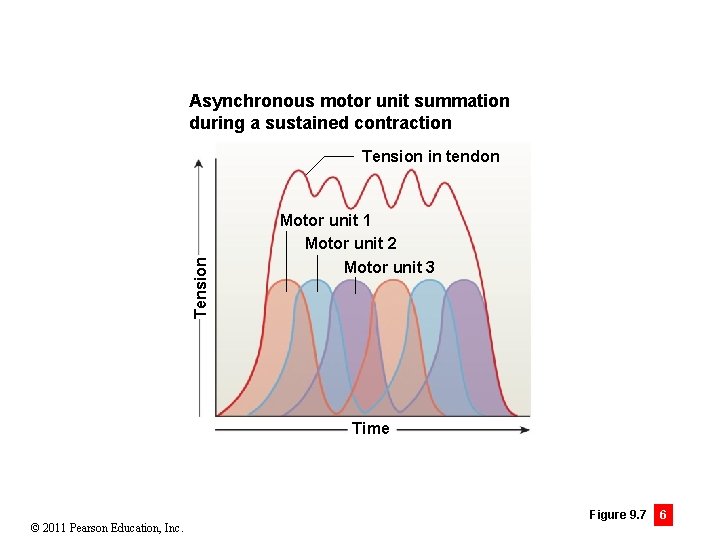
Asynchronous motor unit summation during a sustained contraction Tension in tendon Motor unit 1 Motor unit 2 Motor unit 3 Time © 2011 Pearson Education, Inc. Figure 9. 7 6
Module 9. 7: Developing peak tension • Effects of muscle fiber number on tension (continued) • Motor units (continued) • Muscle tone • Variable number of motor units always active to produce low level tension (not enough to produce movement) • Regulated at subconscious level • Activated muscle fibers use energy and therefore can affect metabolism by a small amount © 2011 Pearson Education, Inc.
Module 9. 7 Review a. Define motor unit. b. Describe the relationship between the number of fibers in a motor unit and the precision of body movements. c. Compare incomplete tetanus with wave summation. © 2011 Pearson Education, Inc.
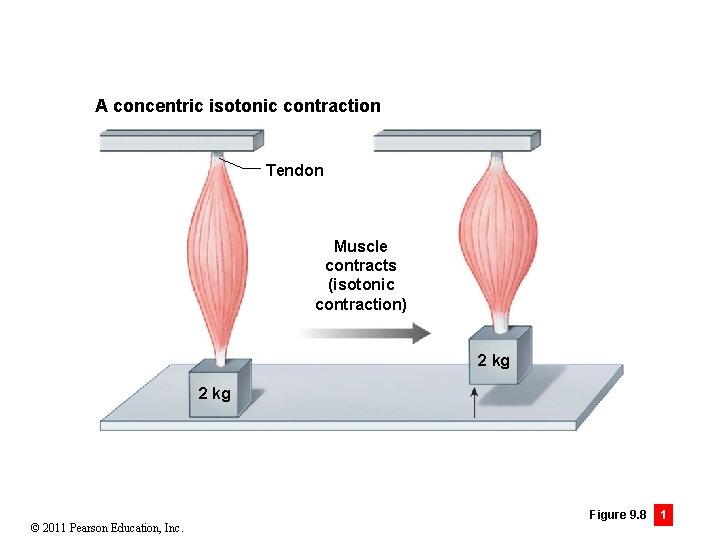
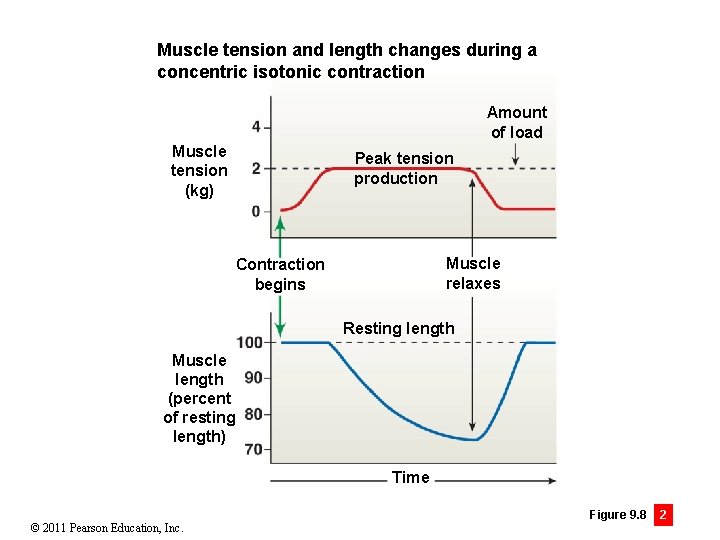
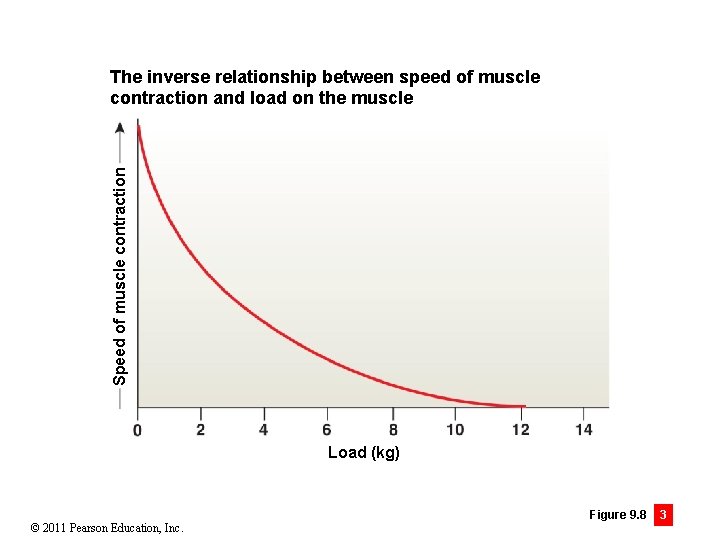
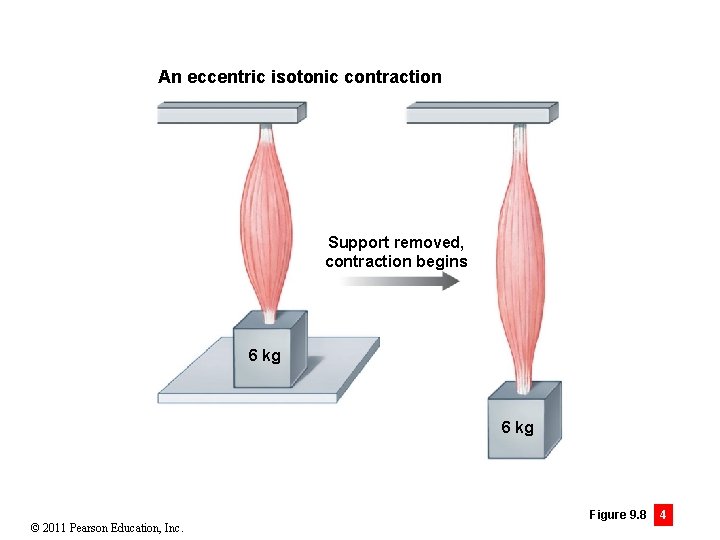
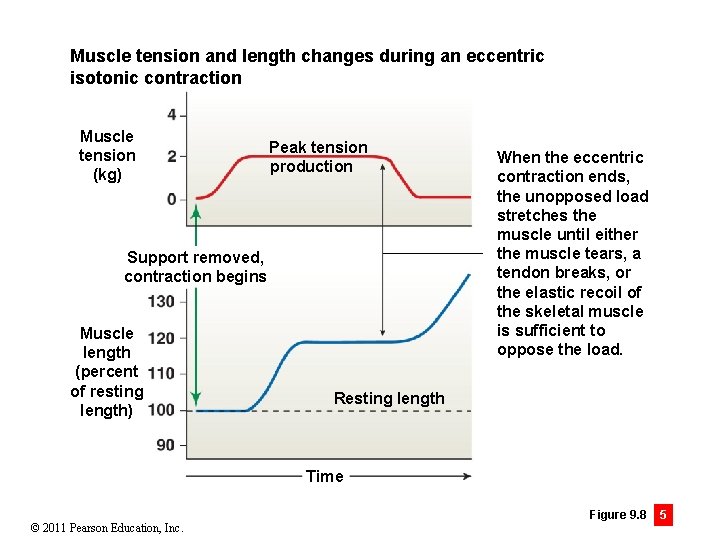
Module 9. 8: Isotonic and isometric contractions • Isotonic contraction (iso-, equal + tonos, tension) • Tension rises, until muscle length changes, then remains constant • Examples: lifting an object, walking, running • Concentric contraction • Muscle tension overcomes load and muscle shortens • Speed of contraction inversely related to load • Eccentric contraction • When load is more than peak tension produced, muscle lengthens • Rate of elongation varies with difference in load/tension © 2011 Pearson Education, Inc.
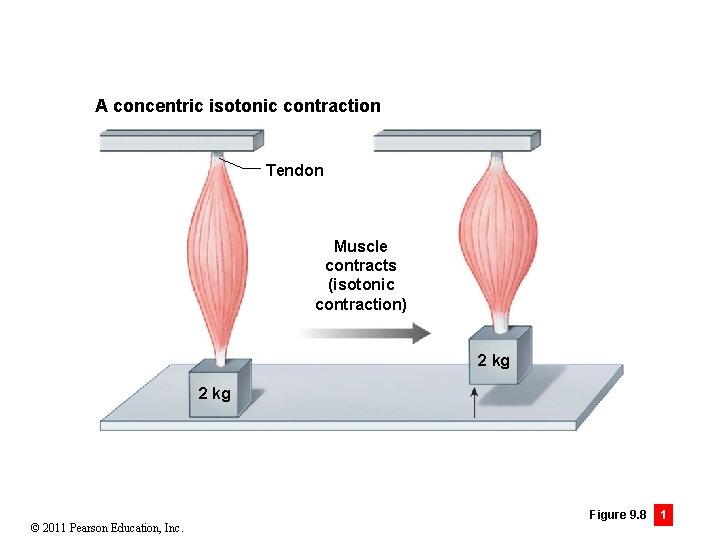
A concentric isotonic contraction Tendon Muscle contracts (isotonic contraction) 2 kg © 2011 Pearson Education, Inc. Figure 9. 8 1
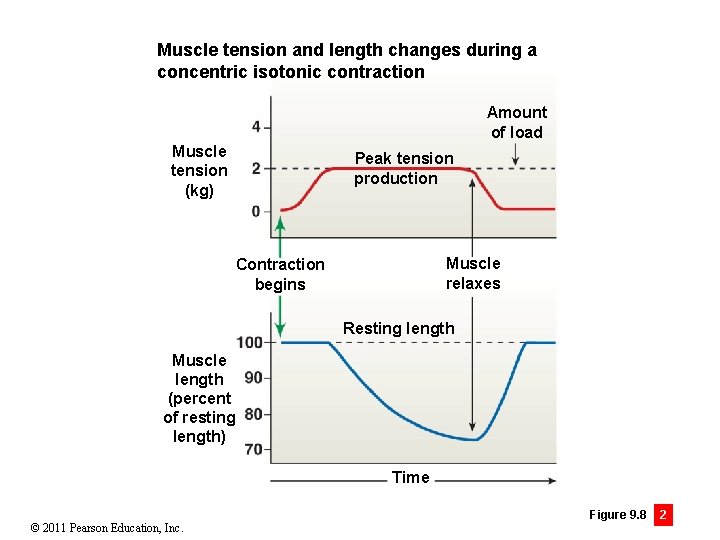
Muscle tension and length changes during a concentric isotonic contraction Amount of load Muscle tension (kg) Peak tension production Muscle relaxes Contraction begins Resting length Muscle length (percent of resting length) Time © 2011 Pearson Education, Inc. Figure 9. 8 2
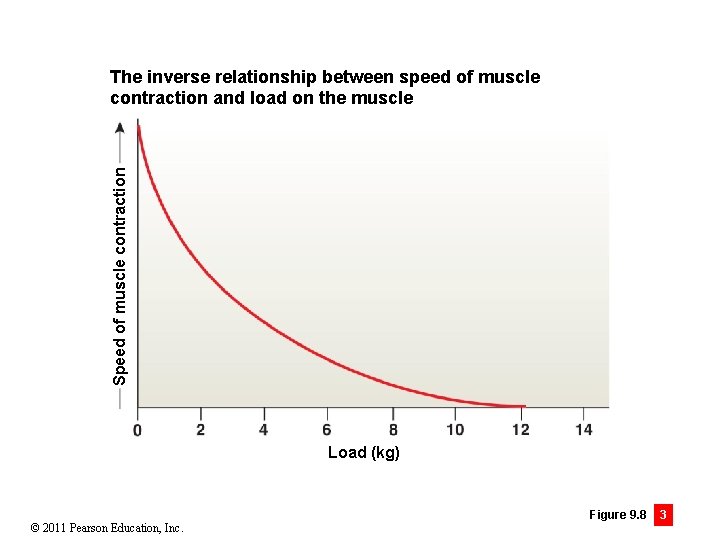
Speed of muscle contraction The inverse relationship between speed of muscle contraction and load on the muscle Load (kg) © 2011 Pearson Education, Inc. Figure 9. 8 3
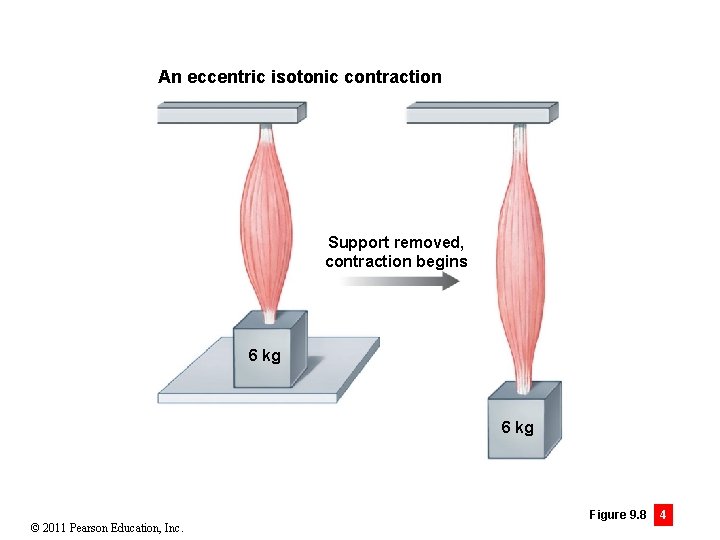
An eccentric isotonic contraction Support removed, contraction begins 6 kg © 2011 Pearson Education, Inc. Figure 9. 8 4
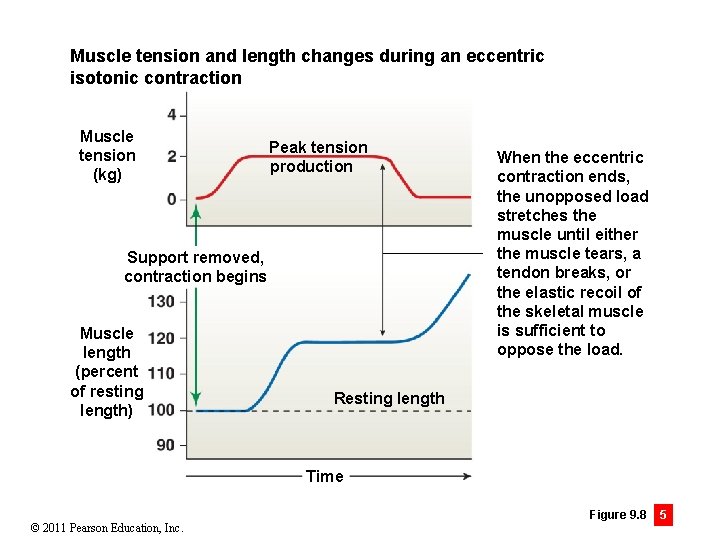
Muscle tension and length changes during an eccentric isotonic contraction Muscle tension (kg) Peak tension production Support removed, contraction begins Muscle length (percent of resting length) When the eccentric contraction ends, the unopposed load stretches the muscle until either the muscle tears, a tendon breaks, or the elastic recoil of the skeletal muscle is sufficient to oppose the load. Resting length Time © 2011 Pearson Education, Inc. Figure 9. 8 5
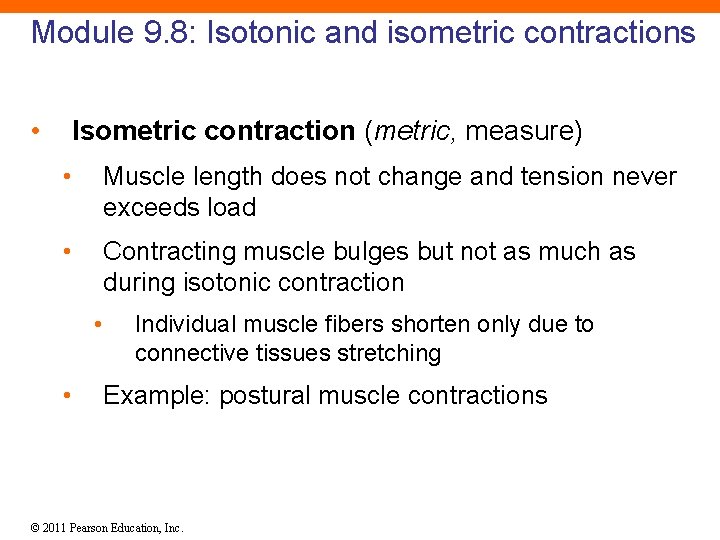
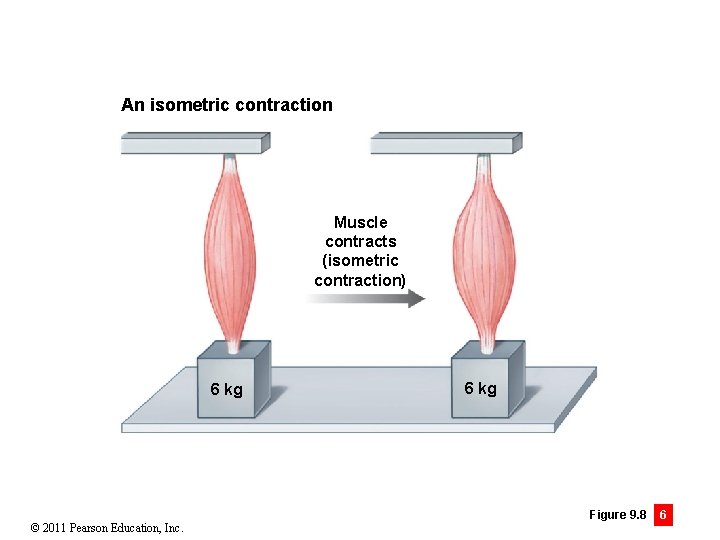
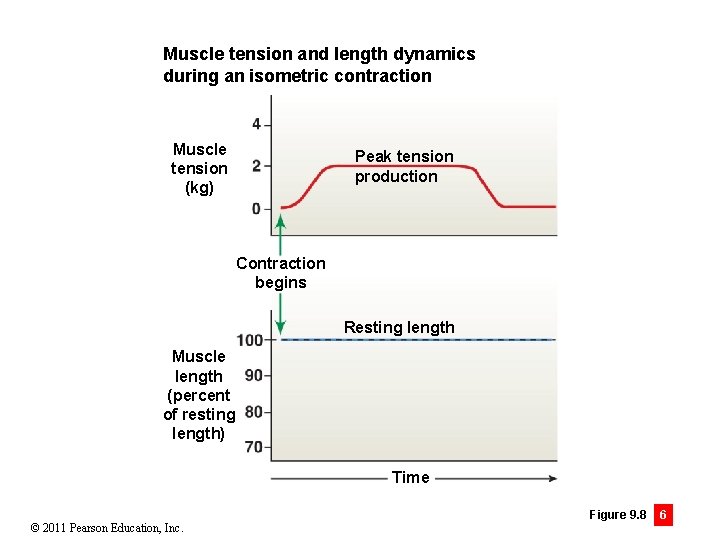
Module 9. 8: Isotonic and isometric contractions • Isometric contraction (metric, measure) • Muscle length does not change and tension never exceeds load • Contracting muscle bulges but not as much as during isotonic contraction • • Individual muscle fibers shorten only due to connective tissues stretching Example: postural muscle contractions © 2011 Pearson Education, Inc.
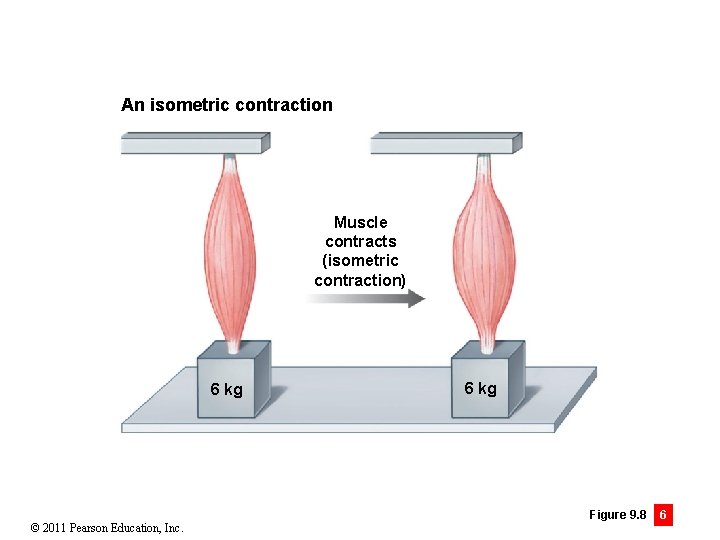
An isometric contraction Muscle contracts (isometric contraction) 6 kg © 2011 Pearson Education, Inc. 6 kg Figure 9. 8 6
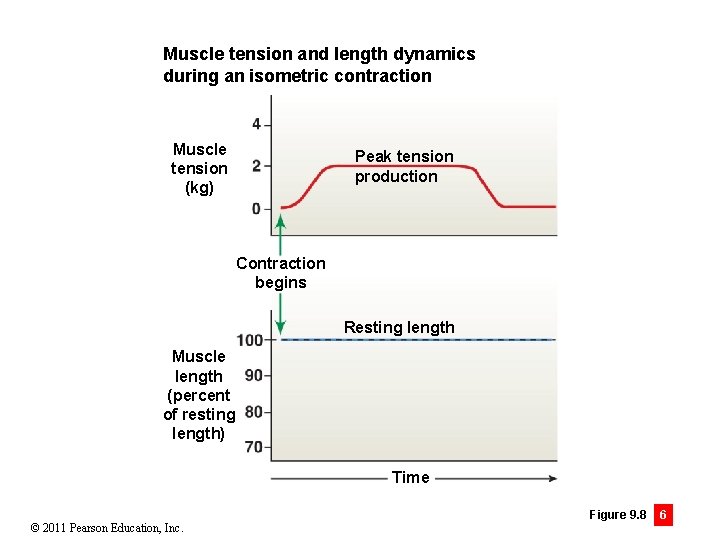
Muscle tension and length dynamics during an isometric contraction Muscle tension (kg) Peak tension production Contraction begins Resting length Muscle length (percent of resting length) Time © 2011 Pearson Education, Inc. Figure 9. 8 6
Module 9. 8 Review a. Define isotonic contraction and isometric contraction. b. Can a skeletal muscle contract without shortening? Why or why not? c. Explain the relationship between load and speed of muscle contraction. © 2011 Pearson Education, Inc.
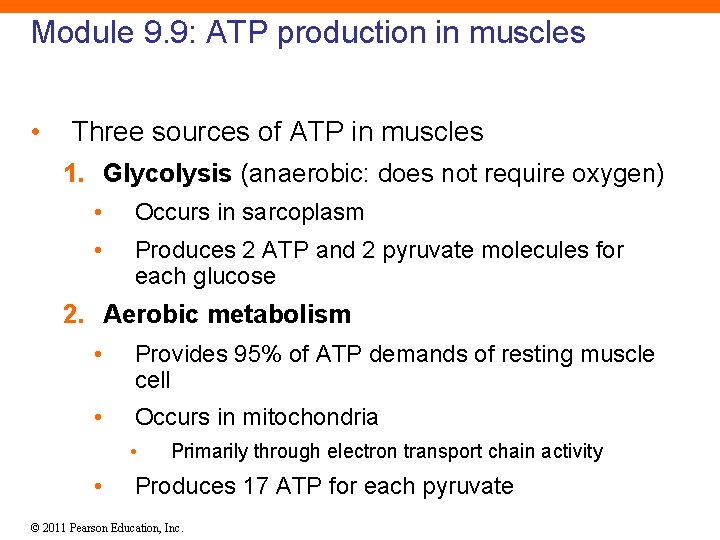
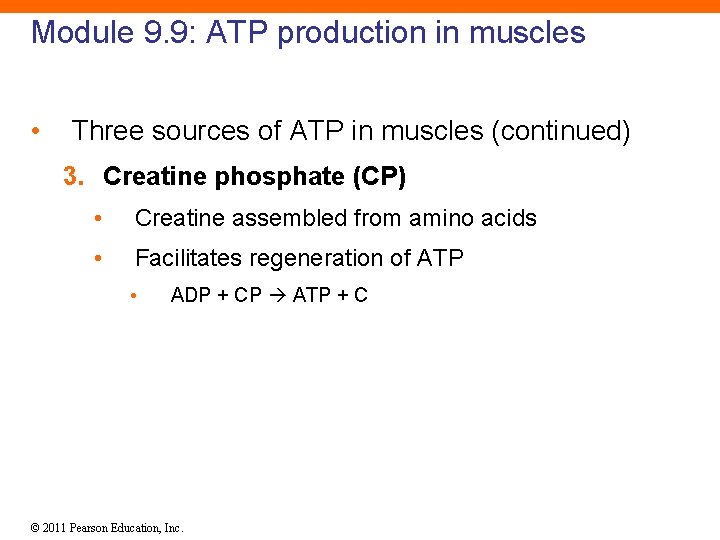
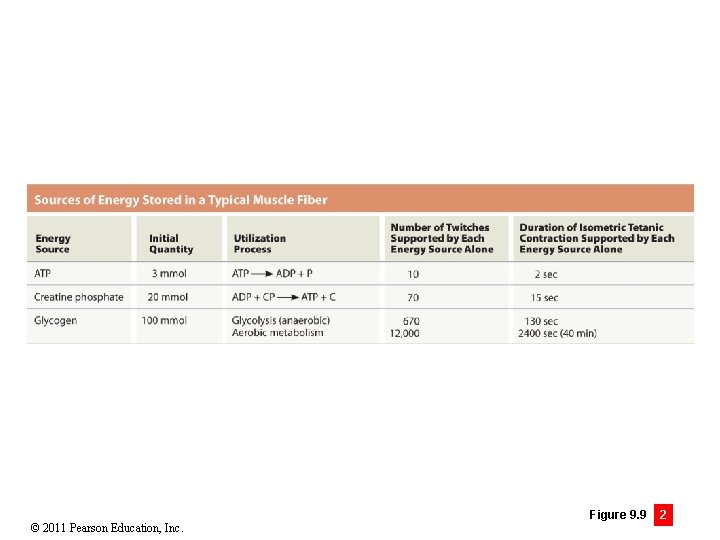
Module 9. 9: ATP production in muscles • Three sources of ATP in muscles 1. Glycolysis (anaerobic: does not require oxygen) • Occurs in sarcoplasm • Produces 2 ATP and 2 pyruvate molecules for each glucose 2. Aerobic metabolism • Provides 95% of ATP demands of resting muscle cell • Occurs in mitochondria • • Primarily through electron transport chain activity Produces 17 ATP for each pyruvate © 2011 Pearson Education, Inc.
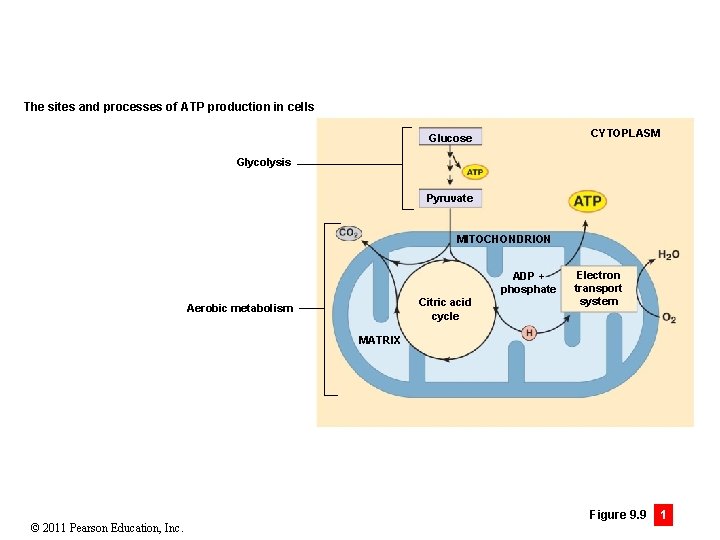
The sites and processes of ATP production in cells CYTOPLASM Glucose Glycolysis Pyruvate MITOCHONDRION ADP + phosphate Citric acid cycle Aerobic metabolism Electron transport system MATRIX © 2011 Pearson Education, Inc. Figure 9. 9 1
Module 9. 9: ATP production in muscles • Three sources of ATP in muscles (continued) 3. Creatine phosphate (CP) • Creatine assembled from amino acids • Facilitates regeneration of ATP • ADP + CP ATP + C © 2011 Pearson Education, Inc.
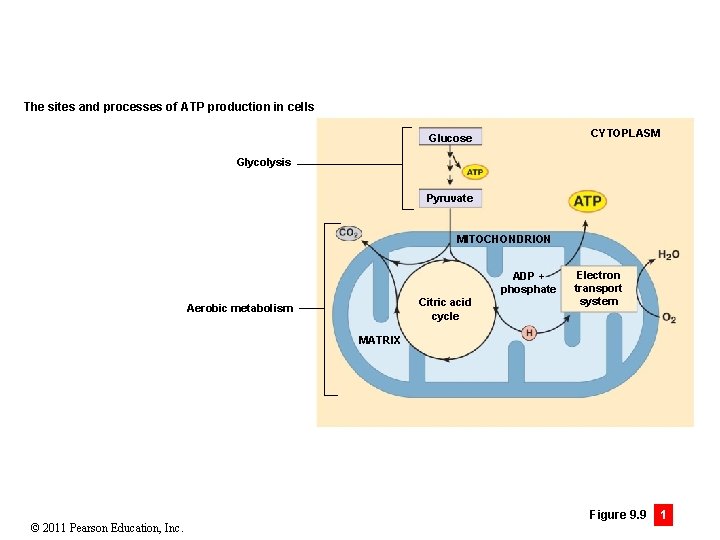
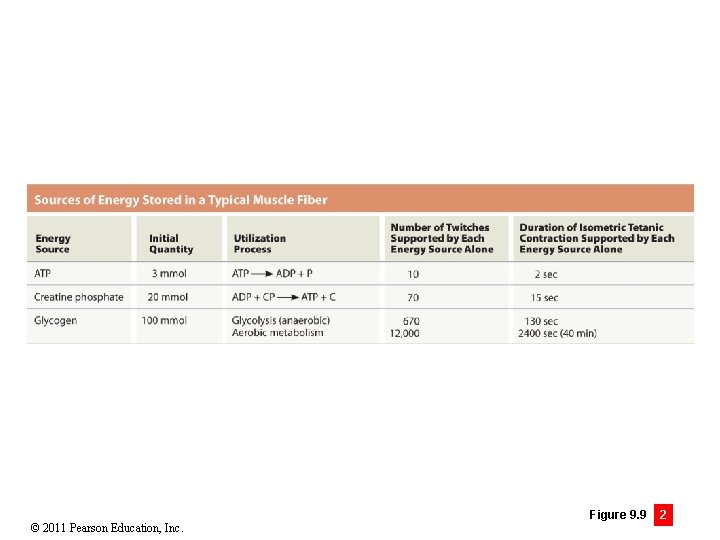
© 2011 Pearson Education, Inc. Figure 9. 9 2
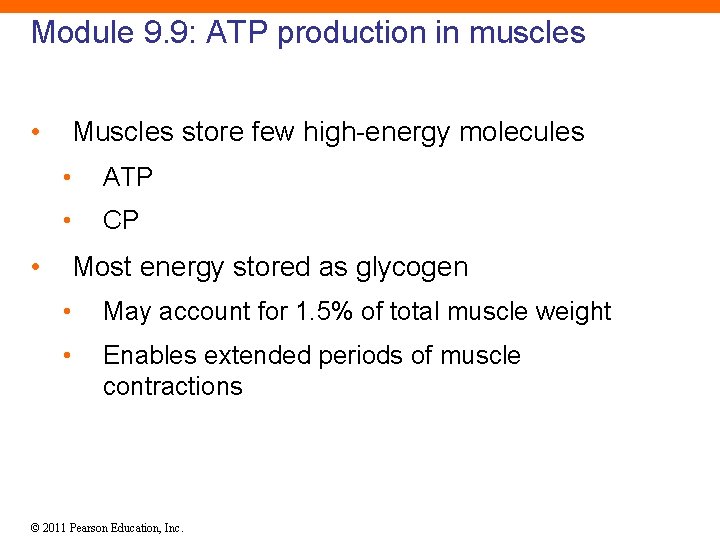
Module 9. 9: ATP production in muscles • • Muscles store few high-energy molecules • ATP • CP Most energy stored as glycogen • May account for 1. 5% of total muscle weight • Enables extended periods of muscle contractions © 2011 Pearson Education, Inc.
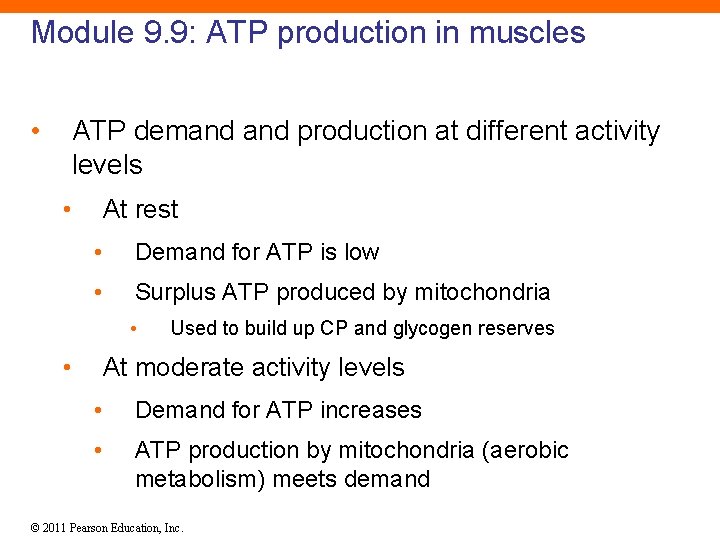
Module 9. 9: ATP production in muscles • ATP demand production at different activity levels • At rest • Demand for ATP is low • Surplus ATP produced by mitochondria • • Used to build up CP and glycogen reserves At moderate activity levels • Demand for ATP increases • ATP production by mitochondria (aerobic metabolism) meets demand © 2011 Pearson Education, Inc.
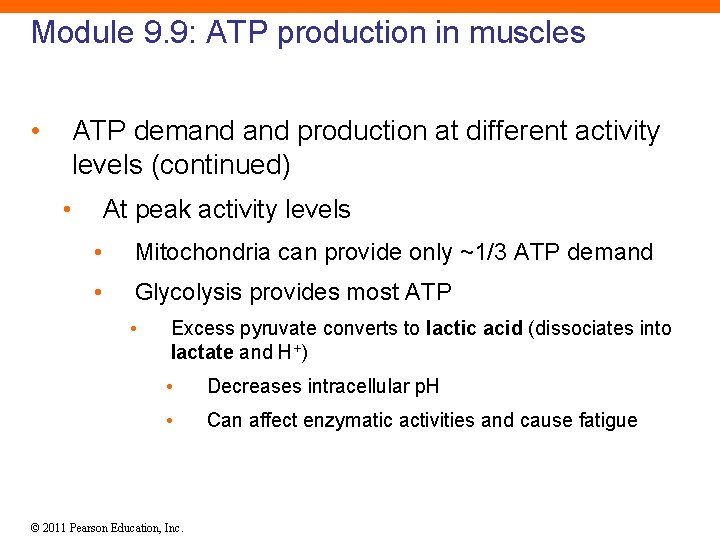
Module 9. 9: ATP production in muscles • ATP demand production at different activity levels (continued) • At peak activity levels • Mitochondria can provide only ~1/3 ATP demand • Glycolysis provides most ATP • Excess pyruvate converts to lactic acid (dissociates into lactate and H+) • Decreases intracellular p. H • Can affect enzymatic activities and cause fatigue © 2011 Pearson Education, Inc.
Module 9. 9 Review a. Identify three sources of energy utilized by muscle fibers. b. How do muscle cells continuously synthesize ATP? c. Under what conditions do muscle fibers produce lactic acid? © 2011 Pearson Education, Inc.
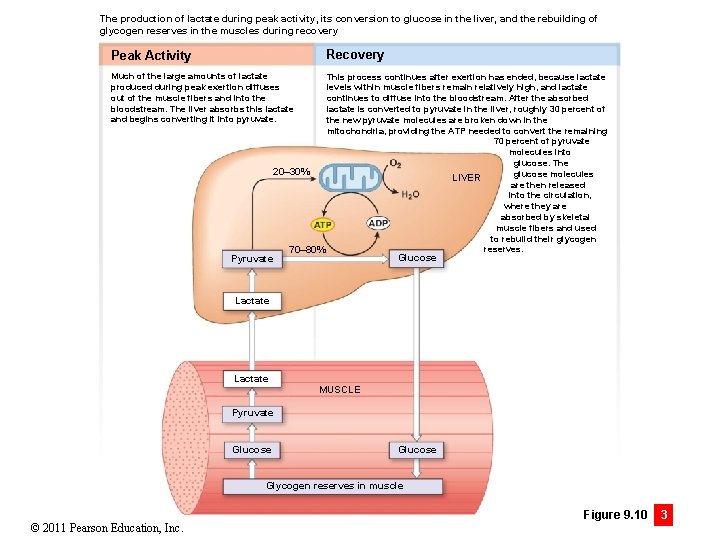
Module 9. 10: Muscle fatigue and recovery • Fatigue • When a muscle can no longer perform at the required activity level • Decline in p. H is a major factor • Decreases calcium/troponin binding • Alters enzyme activities © 2011 Pearson Education, Inc.
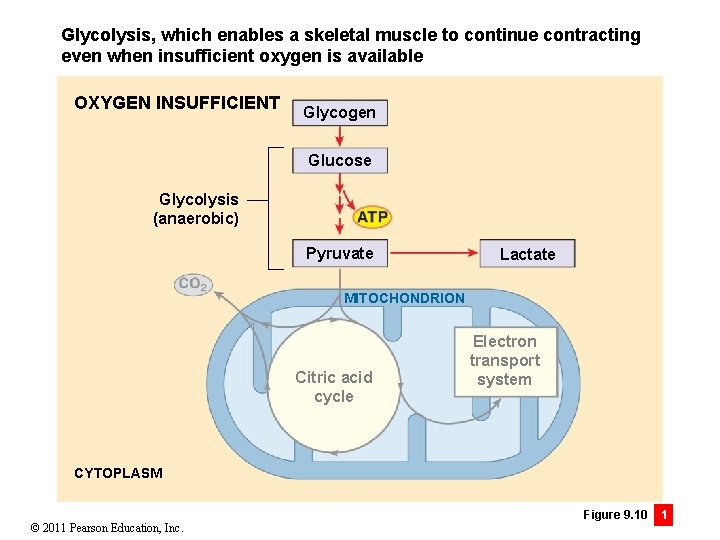
Module 9. 10: Muscle fatigue and recovery • Under conditions of insufficient oxygen • Glycolysis quickly produces ATP • Lowers p. H due to lactic acid buildup • Faster ATP production than aerobic metabolism • • Less efficient than aerobic metabolism • • Only until glycogen reserves are depleted (1– 2 min) Only 4%– 6% of energy captured from conversion of glucose to pyruvate Elevates body temperature • Triggers increased sweating © 2011 Pearson Education, Inc.
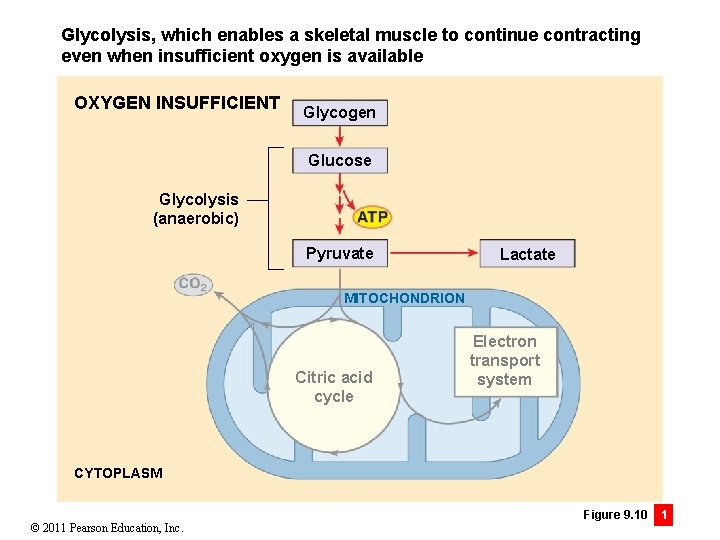
Glycolysis, which enables a skeletal muscle to continue contracting even when insufficient oxygen is available OXYGEN INSUFFICIENT Glycogen Glucose Glycolysis (anaerobic) Pyruvate Lactate MITOCHONDRION Citric acid cycle Electron transport system CYTOPLASM © 2011 Pearson Education, Inc. Figure 9. 10 1
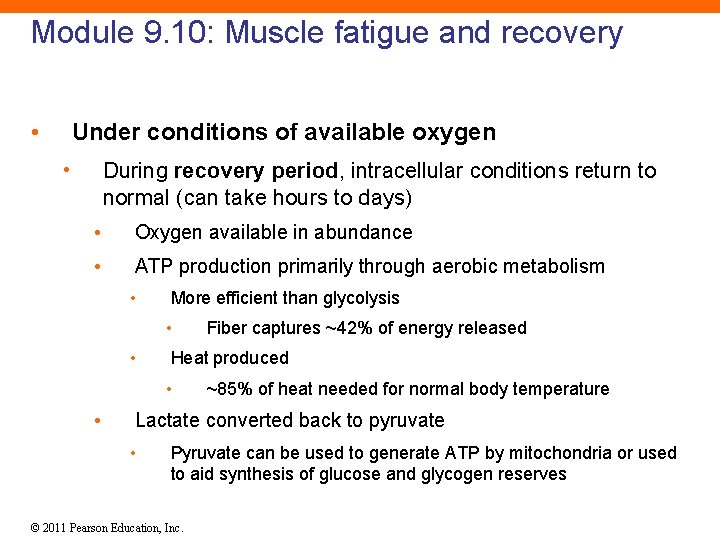
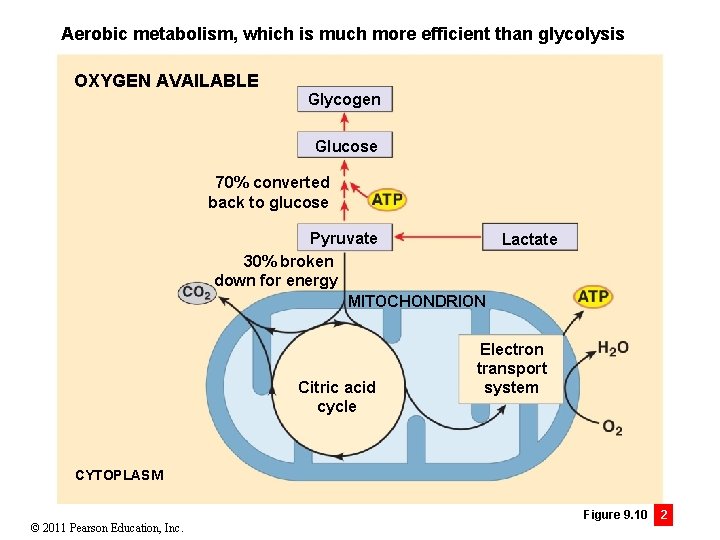
Module 9. 10: Muscle fatigue and recovery • Under conditions of available oxygen • During recovery period, intracellular conditions return to normal (can take hours to days) • Oxygen available in abundance • ATP production primarily through aerobic metabolism • More efficient than glycolysis • • Heat produced • • Fiber captures ~42% of energy released ~85% of heat needed for normal body temperature Lactate converted back to pyruvate • Pyruvate can be used to generate ATP by mitochondria or used to aid synthesis of glucose and glycogen reserves © 2011 Pearson Education, Inc.
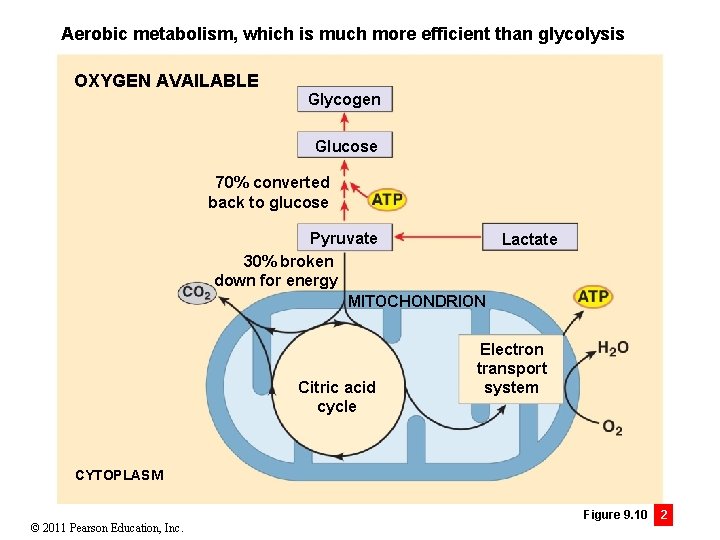
Aerobic metabolism, which is much more efficient than glycolysis OXYGEN AVAILABLE Glycogen Glucose 70% converted back to glucose Pyruvate Lactate 30% broken down for energy MITOCHONDRION Citric acid cycle Electron transport system CYTOPLASM © 2011 Pearson Education, Inc. Figure 9. 10 2
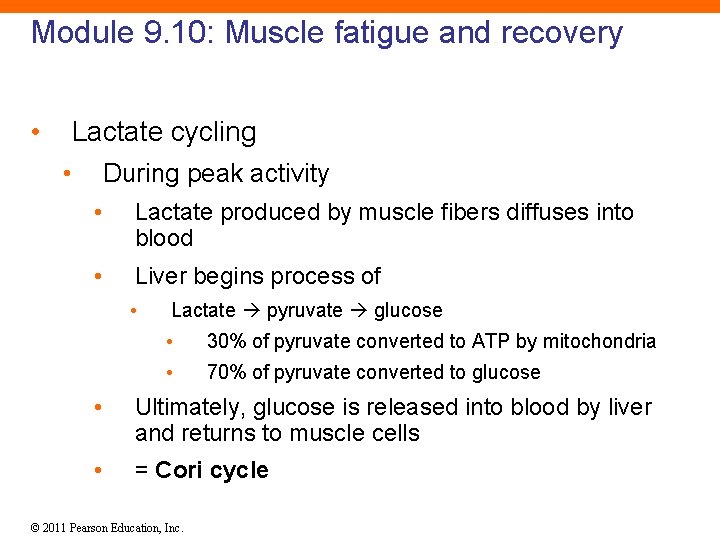
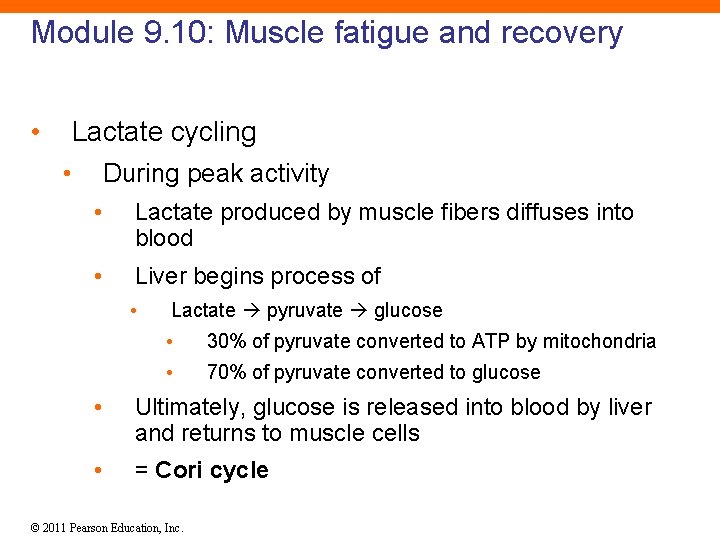
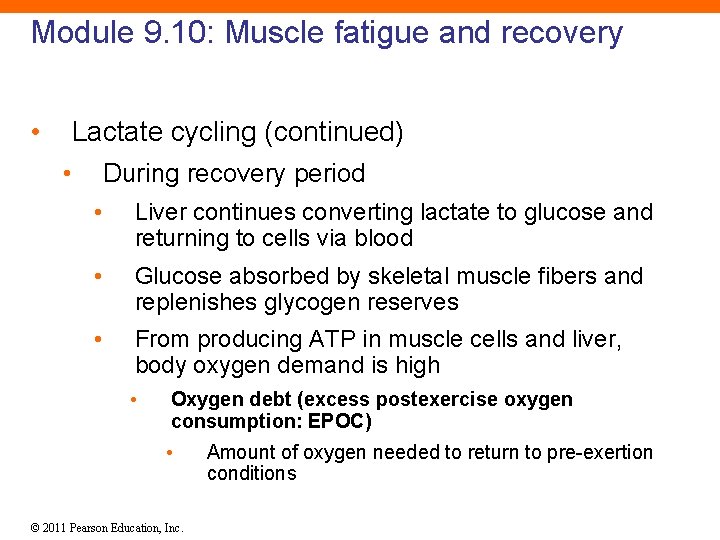
Module 9. 10: Muscle fatigue and recovery • Lactate cycling • During peak activity • Lactate produced by muscle fibers diffuses into blood • Liver begins process of • Lactate pyruvate glucose • 30% of pyruvate converted to ATP by mitochondria • 70% of pyruvate converted to glucose • Ultimately, glucose is released into blood by liver and returns to muscle cells • = Cori cycle © 2011 Pearson Education, Inc.
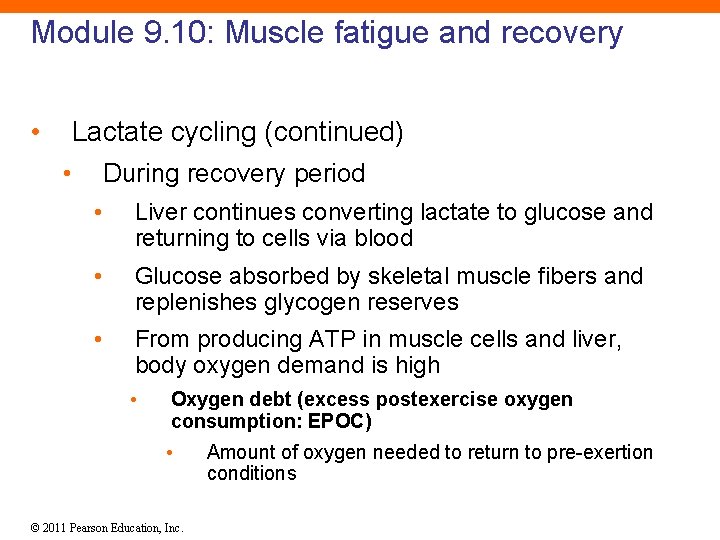
Module 9. 10: Muscle fatigue and recovery • Lactate cycling (continued) • During recovery period • Liver continues converting lactate to glucose and returning to cells via blood • Glucose absorbed by skeletal muscle fibers and replenishes glycogen reserves • From producing ATP in muscle cells and liver, body oxygen demand is high • Oxygen debt (excess postexercise oxygen consumption: EPOC) • © 2011 Pearson Education, Inc. Amount of oxygen needed to return to pre-exertion conditions
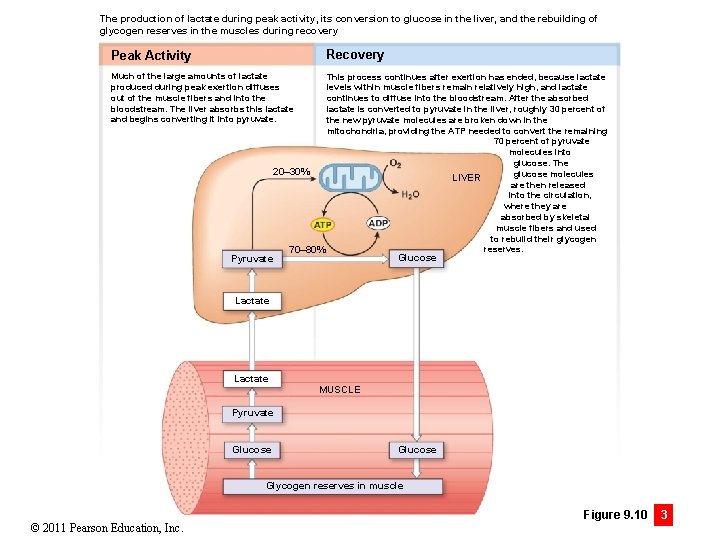
The production of lactate during peak activity, its conversion to glucose in the liver, and the rebuilding of glycogen reserves in the muscles during recovery Recovery Peak Activity Much of the large amounts of lactate produced during peak exertion diffuses out of the muscle fibers and into the bloodstream. The liver absorbs this lactate and begins converting it into pyruvate. Pyruvate This process continues after exertion has ended, because lactate levels within muscle fibers remain relatively high, and lactate continues to diffuse into the bloodstream. After the absorbed lactate is converted to pyruvate in the liver, roughly 30 percent of the new pyruvate molecules are broken down in the mitochondria, providing the ATP needed to convert the remaining 70 percent of pyruvate molecules into glucose. The 20– 30% glucose molecules LIVER are then released into the circulation, where they are absorbed by skeletal muscle fibers and used to rebuild their glycogen reserves. 70– 80% Glucose Lactate MUSCLE Pyruvate Glucose Glycogen reserves in muscle © 2011 Pearson Education, Inc. Figure 9. 10 3
Module 9. 10 Review a. Define oxygen debt (excess postexercise oxygen consumption). b. What two processes are crucial in repaying a muscle’s oxygen debt during the recovery period? c. After strenuous exercise, what causes the “burning” sensation in skeletal muscles? © 2011 Pearson Education, Inc.
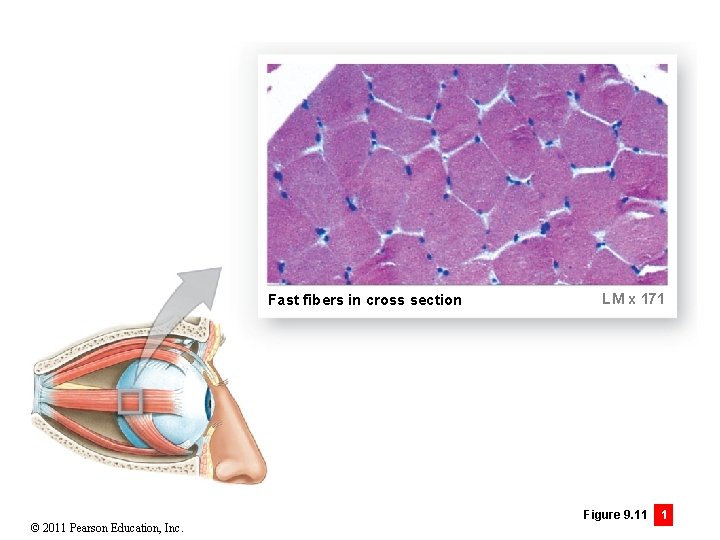
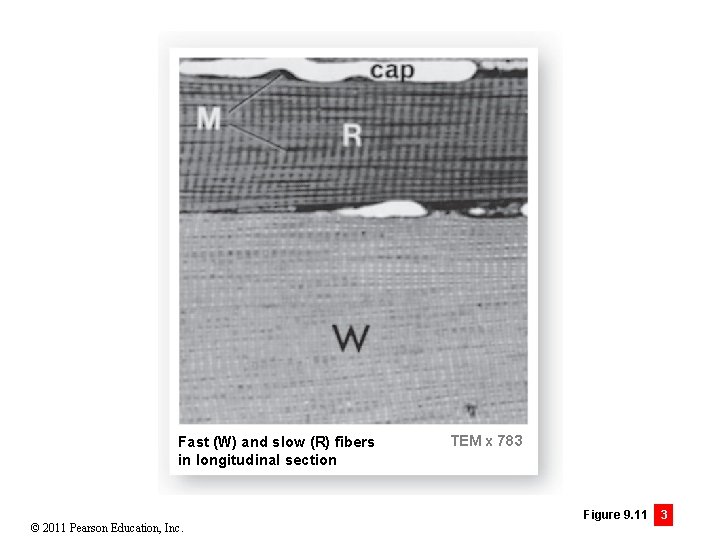
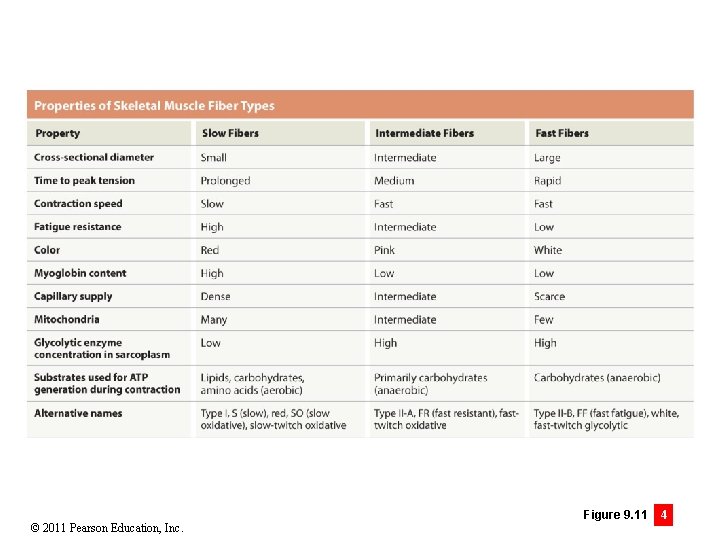
Module 9. 11: Skeletal muscle fiber types • Three major types of skeletal muscle fibers 1. Fast fibers • Reach peak tensions in <0. 01 sec • Large in diameter • Have densely packed myofibrils, large glycogen reserves, few mitochondria • Powerful • Fatigue rapidly since most ATP produced anaerobically © 2011 Pearson Education, Inc.
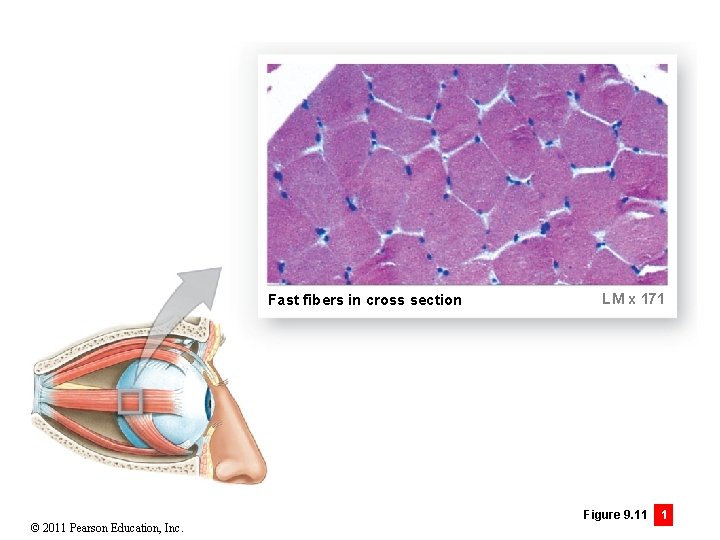
Fast fibers in cross section © 2011 Pearson Education, Inc. LM x 171 Figure 9. 11 1
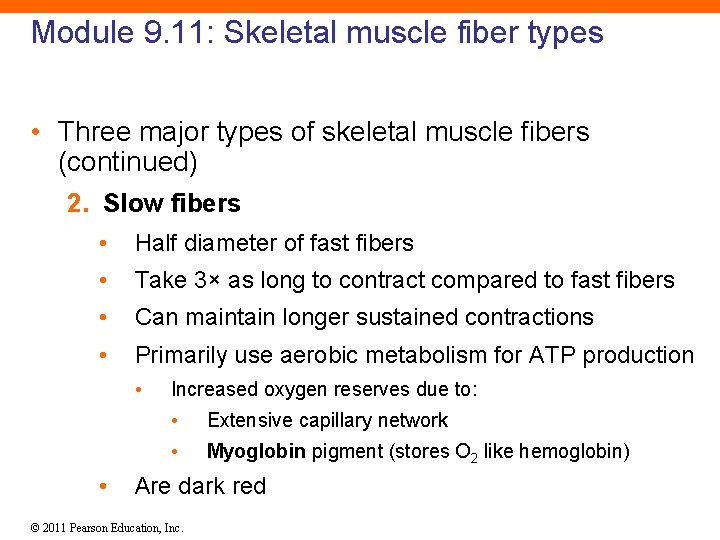
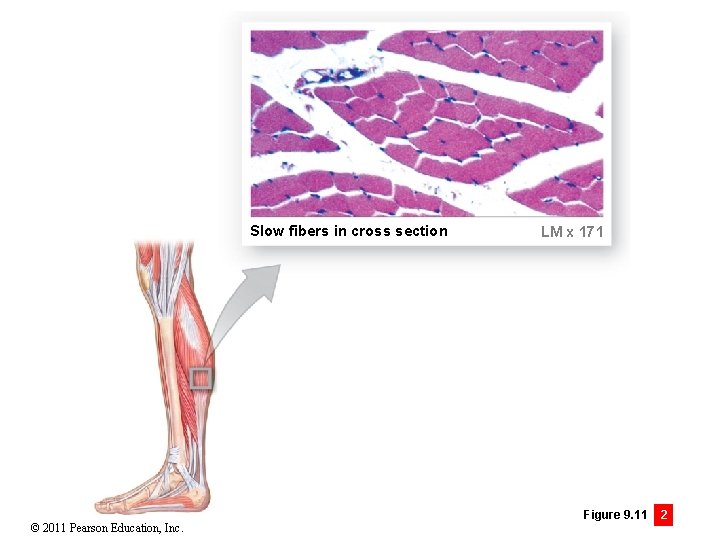
Module 9. 11: Skeletal muscle fiber types • Three major types of skeletal muscle fibers (continued) 2. Slow fibers • Half diameter of fast fibers • Take 3× as long to contract compared to fast fibers • Can maintain longer sustained contractions • Primarily use aerobic metabolism for ATP production • • Increased oxygen reserves due to: • Extensive capillary network • Myoglobin pigment (stores O 2 like hemoglobin) Are dark red © 2011 Pearson Education, Inc.
Slow fibers in cross section © 2011 Pearson Education, Inc. LM x 171 Figure 9. 11 2
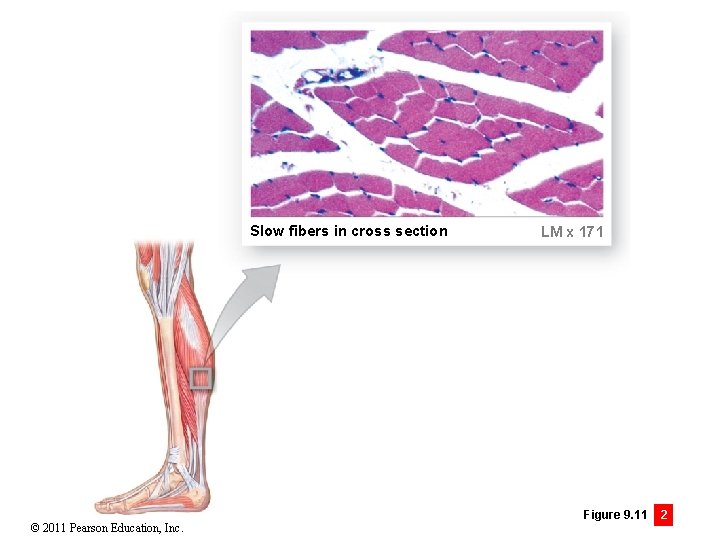
Module 9. 11: Skeletal muscle fiber types • Three major types of skeletal muscle fibers (continued) 3. Intermediate fibers • More closely resemble fast fibers • Contain little myoglobin • Relatively pale • But more capillaries and more fatigue resistant © 2011 Pearson Education, Inc.
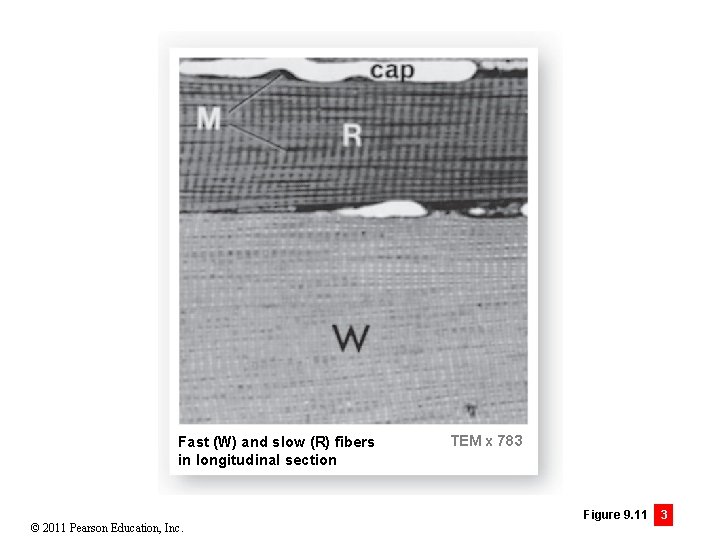
Fast (W) and slow (R) fibers in longitudinal section © 2011 Pearson Education, Inc. TEM x 783 Figure 9. 11 3
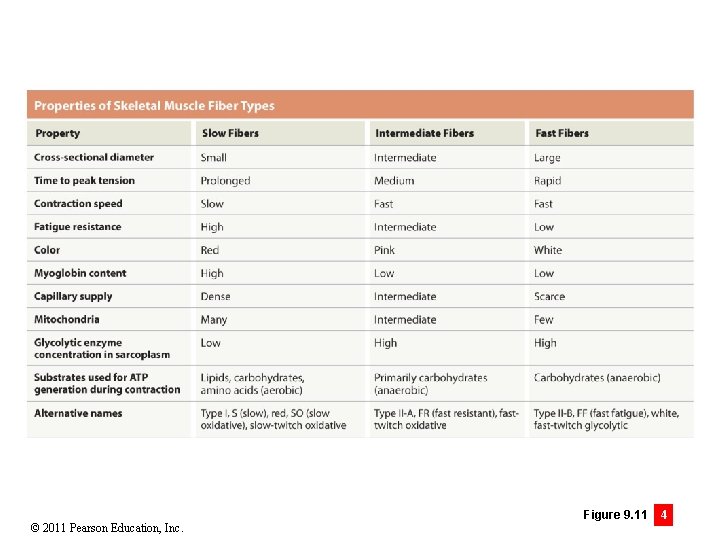
© 2011 Pearson Education, Inc. Figure 9. 11 4
Module 9. 11: Skeletal muscle fiber types • Most muscles have a mixture of fiber types • Percentages of each type vary • According to muscle function • Back and calf muscles dominated by slow fibers • Eye or hand may have no slow fibers • According to genetics • Percentage of fast to slow inherited • According to physical training • Percentage of intermediate to fast can be modified with athletic training © 2011 Pearson Education, Inc.
Module 9. 11 Review a. Identify the three types of skeletal muscle fibers. b. Why would a sprinter experience muscle fatigue before a marathon runner would? c. Which type of muscle fiber would you expect to predominate in the large leg muscles of someone who excels at endurance activities, such as cycling or long-distance running? © 2011 Pearson Education, Inc.
CLINICAL MODULE 9. 12: Factors and clinical conditions affecting muscles • Hypertrophy • Increase in muscle size due to: • Increase in myofilaments • Increase in myofibril size • Increase in mitochondria • More glycogen and glycolytic enzymes • As a result of repeated exhaustive stimulation • Can be promoted by administration of steroid hormones © 2011 Pearson Education, Inc.
CLINICAL MODULE 9. 12: Factors and clinical conditions affecting muscles • Atrophy • Decrease in muscle size, tone, and power • As a result of decreased stimulation such as during: • Paralysis by spinal injury • Damage to nervous system • Having body part in cast after bone fracture • Initially reversible, but after prolonged disuse, muscle fibers can die and not be replaced © 2011 Pearson Education, Inc.
CLINICAL MODULE 9. 12: Factors and clinical conditions affecting muscles • Clinical conditions • Polio • Virus attacks motor neurons of brain and spinal cord causing paralysis (lost of voluntary movement) • Tetanus • Toxin from bacteria (Clostridium tetani) that suppresses the mechanism inhibiting motor neuron activity • Thrives in low-oxygen areas like deep punctured tissues • Results in sustained, powerful contractions of affected muscles • Severe tetanus can have 40%– 60% mortality • Deaths rare due to immunization in U. S. © 2011 Pearson Education, Inc.
CLINICAL MODULE 9. 12: Factors and clinical conditions affecting muscles • Clinical conditions (continued) • Botulism • Toxin from bacteria (Clostridium botulinum) that blocks ACh release at neuromuscular junctions • Acquired through bacteria-contaminated food • Myasthenia gravis • Loss of ACh receptors at neuromuscular junctions • Results in progressive weakness © 2011 Pearson Education, Inc.
CLINICAL MODULE 9. 12: Factors and clinical conditions affecting muscles • Clinical conditions (continued) • Rigor mortis • Generalized muscle contraction shortly after death (2– 7 hours) • Begins with small muscles of face, neck, and arms • Due to depletion of ATP, leaving myosin crossbridges attached to actin • Ends 1– 6 days later as muscular tissue decomposes © 2011 Pearson Education, Inc.
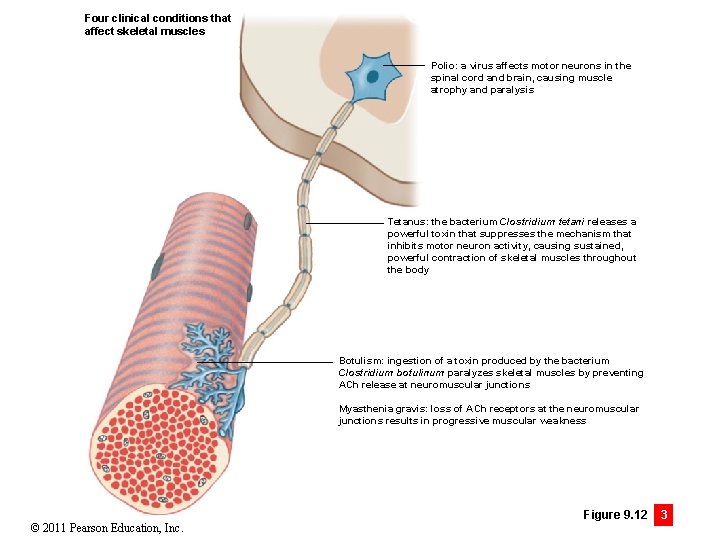
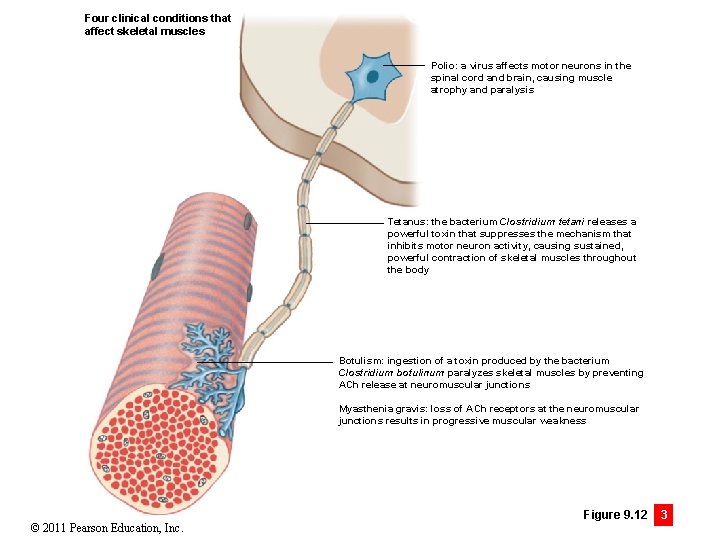
Four clinical conditions that affect skeletal muscles Polio: a virus affects motor neurons in the spinal cord and brain, causing muscle atrophy and paralysis Tetanus: the bacterium Clostridium tetani releases a powerful toxin that suppresses the mechanism that inhibits motor neuron activity, causing sustained, powerful contraction of skeletal muscles throughout the body Botulism: ingestion of a toxin produced by the bacterium Clostridium botulinum paralyzes skeletal muscles by preventing ACh release at neuromuscular junctions Myasthenia gravis: loss of ACh receptors at the neuromuscular junctions results in progressive muscular weakness © 2011 Pearson Education, Inc. Figure 9. 12 3
CLINICAL MODULE 9. 12 Review a. Define muscle hypertrophy and muscle atrophy. b. Six weeks after Fred broke his leg the cast is removed, and as he steps down from the exam table, his leg gives way and he falls. Propose a logical explanation. c. Explain how the flexibility or rigidity of a dead body can provide a clue about a murder victim’s time of death. © 2011 Pearson Education, Inc.