7 Mediastinal Syndromes 1 Mediastinum Division Superior Inferior
















- Slides: 66

7 Mediastinal Syndromes 1
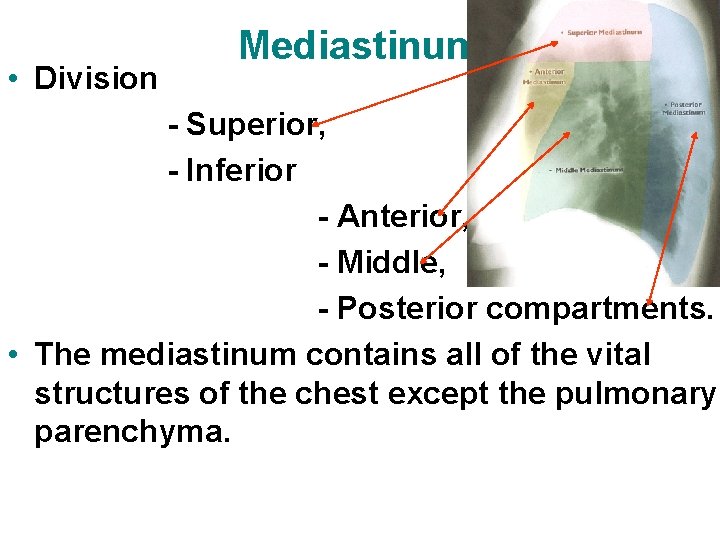
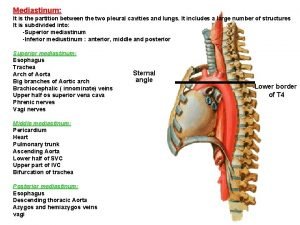
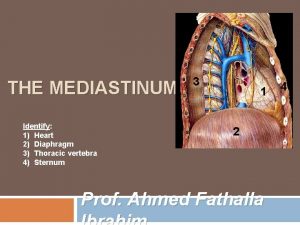
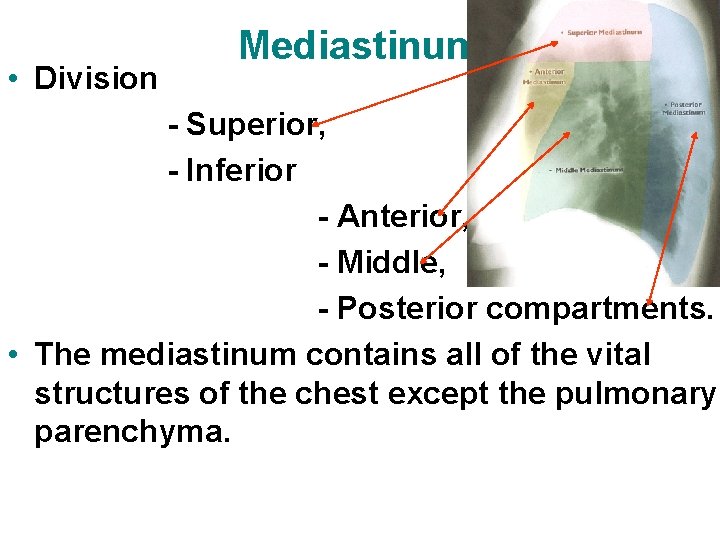
Mediastinum • Division - Superior, - Inferior - Anterior, - Middle, - Posterior compartments. • The mediastinum contains all of the vital structures of the chest except the pulmonary parenchyma.
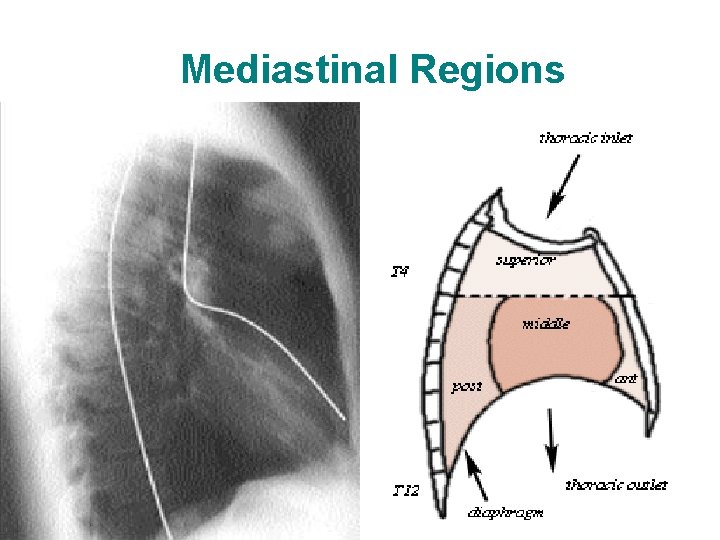
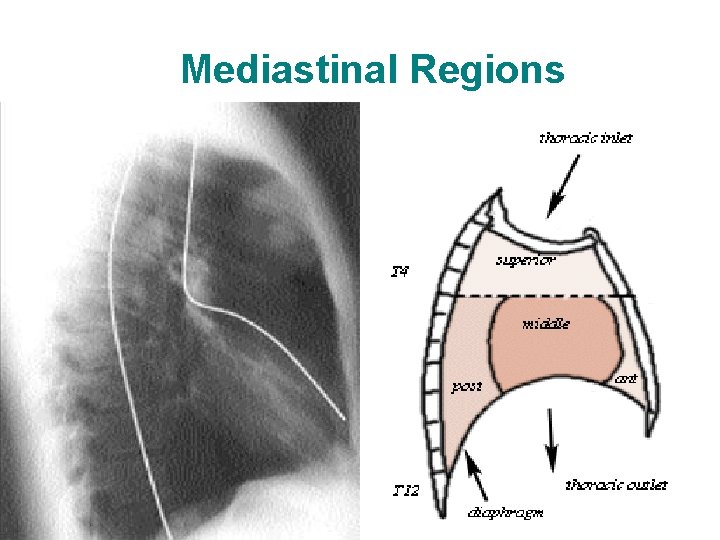
Mediastinal Regions
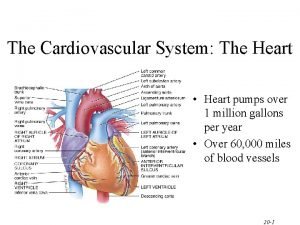
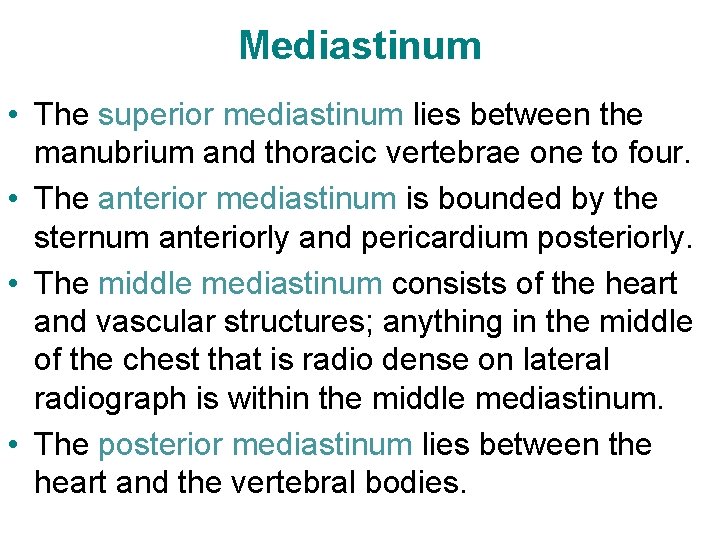
Mediastinum • The superior mediastinum lies between the manubrium and thoracic vertebrae one to four. • The anterior mediastinum is bounded by the sternum anteriorly and pericardium posteriorly. • The middle mediastinum consists of the heart and vascular structures; anything in the middle of the chest that is radio dense on lateral radiograph is within the middle mediastinum. • The posterior mediastinum lies between the heart and the vertebral bodies.

Subdivision of mediastinum • anterior mediastinum • middle mediastinum • posterior mediastinum
Mediastinal Lesions • Any lesion that occurs in the mediastinum – can be focal or diffuse. • CT scan or MRI with contrast is usually indicated for further evaluation.

Mediastinal Lesions Focal vs Diffuse Anthrax Thymoma
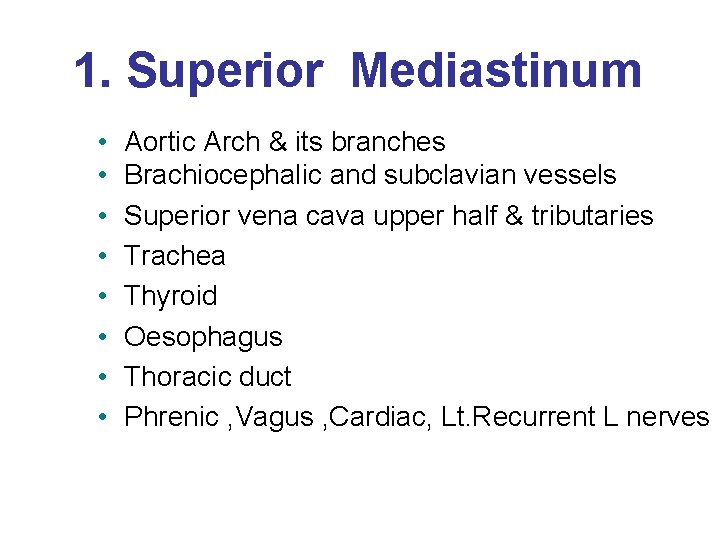
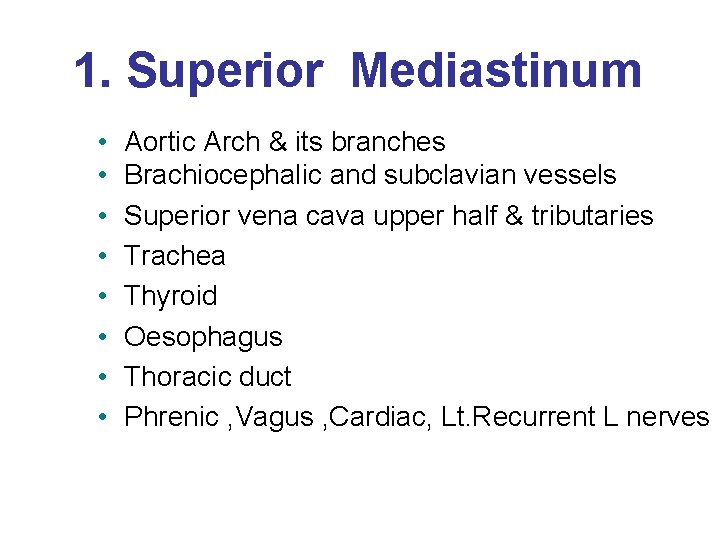
1. Superior Mediastinum • • Aortic Arch & its branches Brachiocephalic and subclavian vessels Superior vena cava upper half & tributaries Trachea Thyroid Oesophagus Thoracic duct Phrenic , Vagus , Cardiac, Lt. Recurrent L nerves

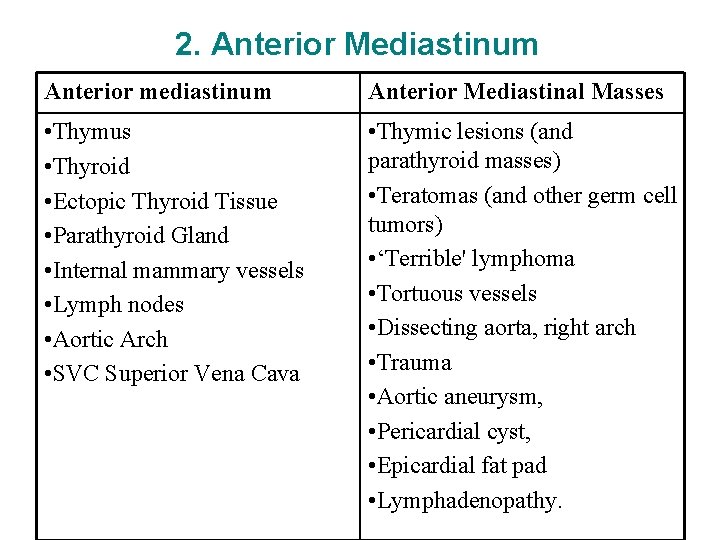
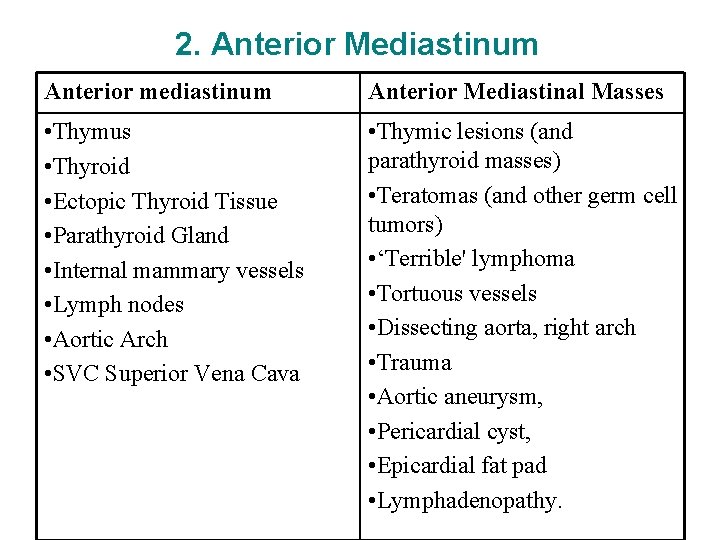
2. Anterior Mediastinum Anterior mediastinum Anterior Mediastinal Masses • Thymus • Thyroid • Ectopic Thyroid Tissue • Parathyroid Gland • Internal mammary vessels • Lymph nodes • Aortic Arch • SVC Superior Vena Cava • Thymic lesions (and parathyroid masses) • Teratomas (and other germ cell tumors) • ‘Terrible' lymphoma • Tortuous vessels • Dissecting aorta, right arch • Trauma • Aortic aneurysm, • Pericardial cyst, • Epicardial fat pad • Lymphadenopathy.

Anterior mediastinal mass
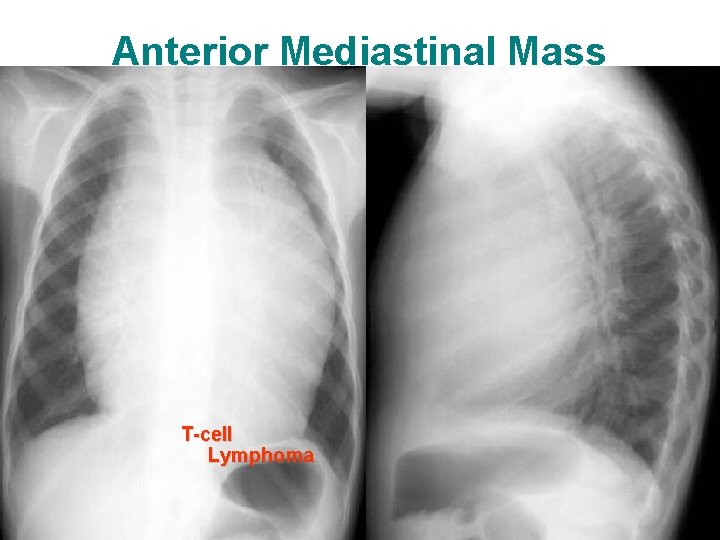
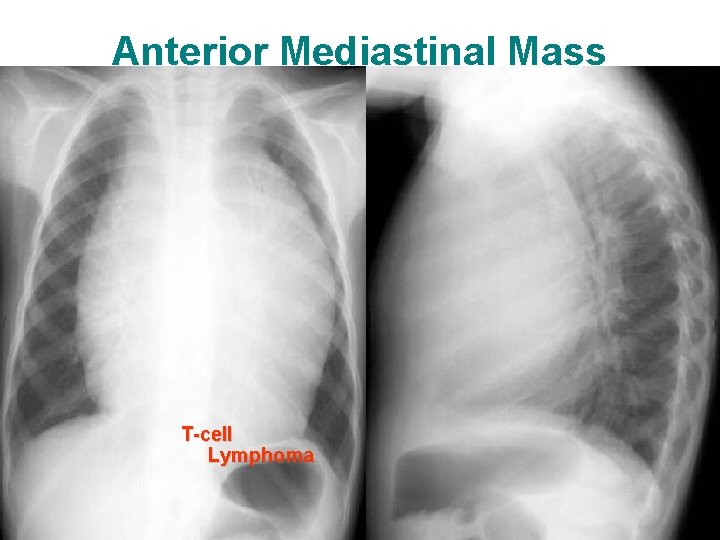
Anterior Mediastinal Mass T-cell Lymphoma
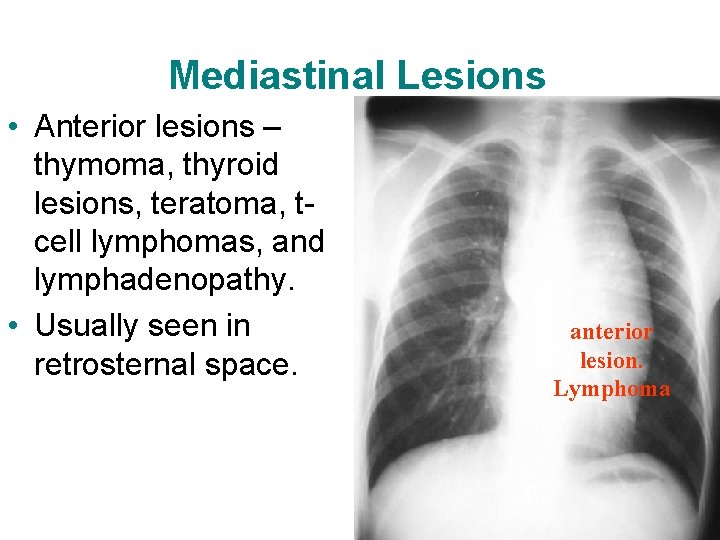
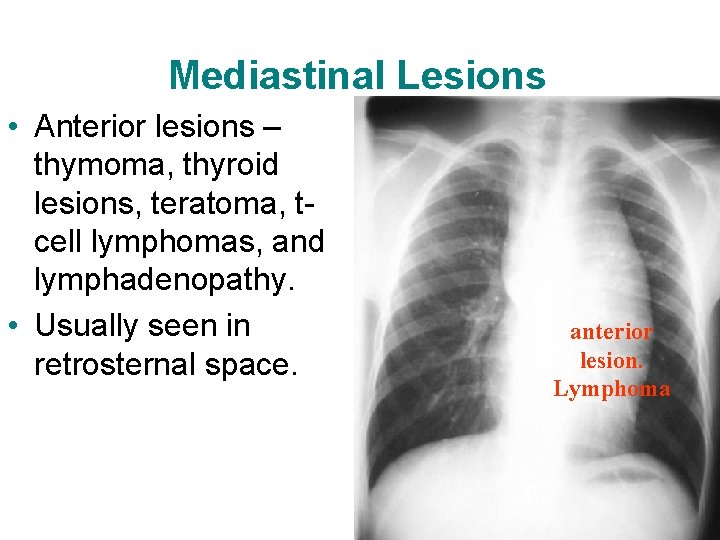
Mediastinal Lesions • Anterior lesions – thymoma, thyroid lesions, teratoma, tcell lymphomas, and lymphadenopathy. • Usually seen in retrosternal space. anterior lesion. Lymphoma
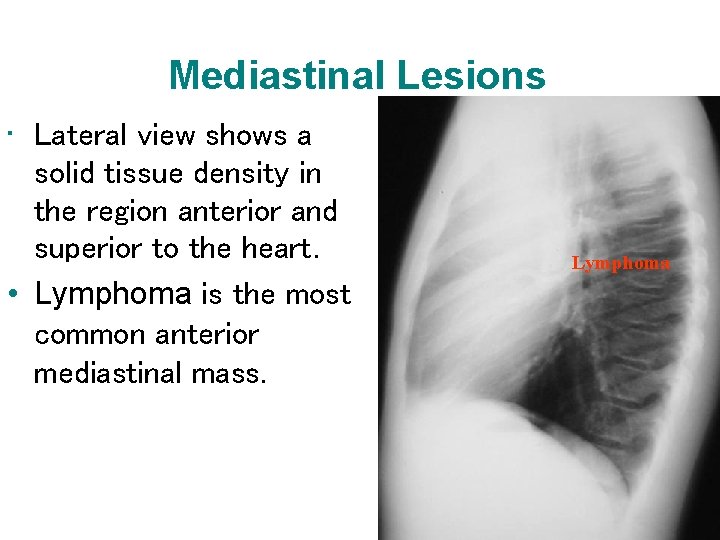
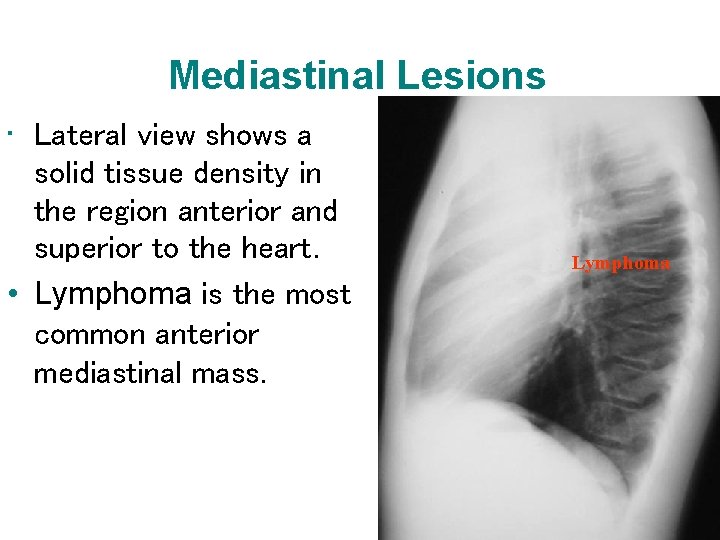
Mediastinal Lesions • Lateral view shows a solid tissue density in the region anterior and superior to the heart. • Lymphoma is the most common anterior mediastinal mass. Lymphoma
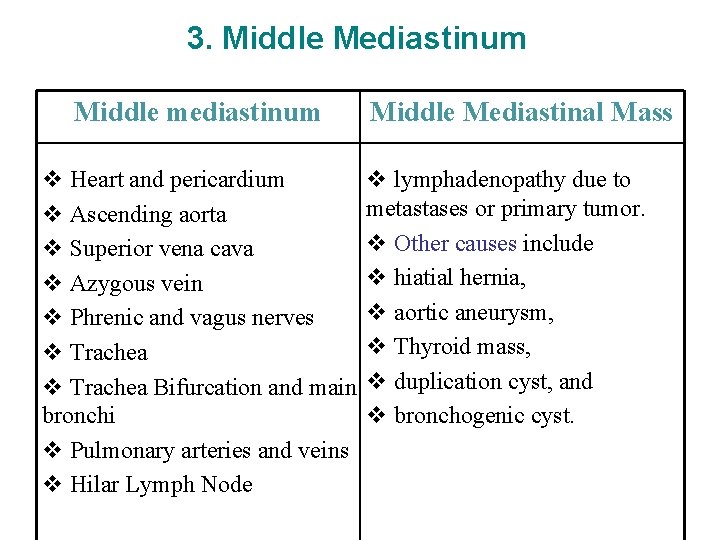
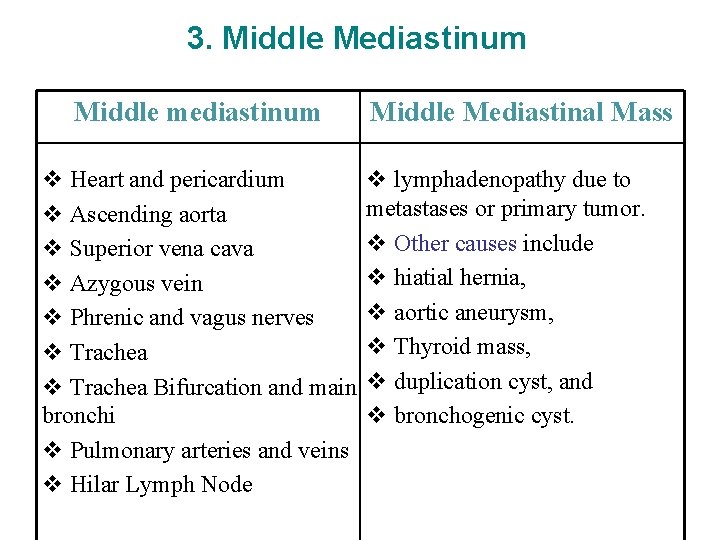
3. Middle Mediastinum Middle mediastinum Middle Mediastinal Mass v Heart and pericardium v lymphadenopathy due to metastases or primary tumor. v Ascending aorta v Other causes include v Superior vena cava v hiatial hernia, v Azygous vein v aortic aneurysm, v Phrenic and vagus nerves v Thyroid mass, v Trachea Bifurcation and main v duplication cyst, and bronchi v bronchogenic cyst. v Pulmonary arteries and veins v Hilar Lymph Node

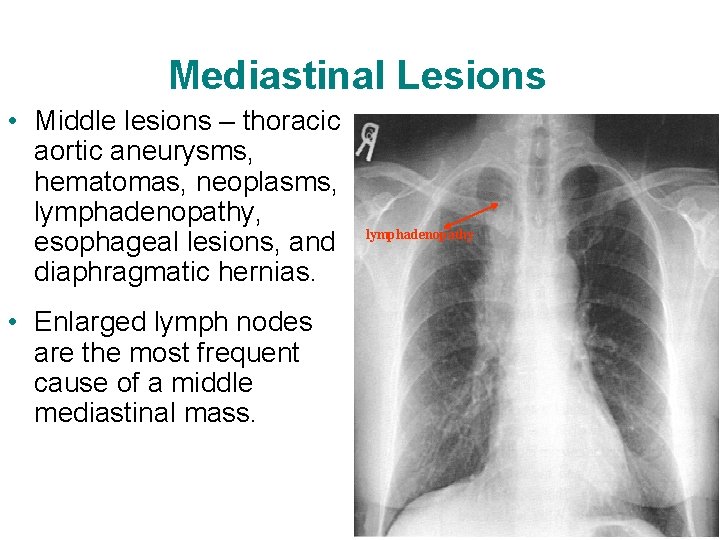
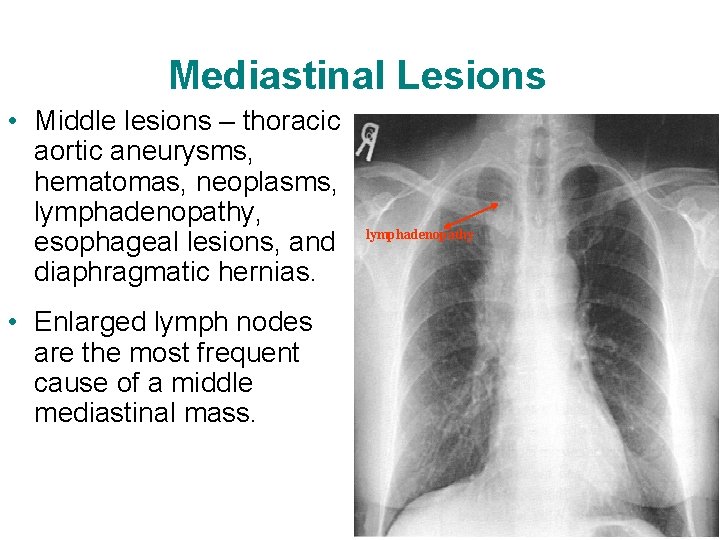
Mediastinal Lesions • Middle lesions – thoracic aortic aneurysms, hematomas, neoplasms, lymphadenopathy, esophageal lesions, and diaphragmatic hernias. • Enlarged lymph nodes are the most frequent cause of a middle mediastinal mass. lymphadenopathy
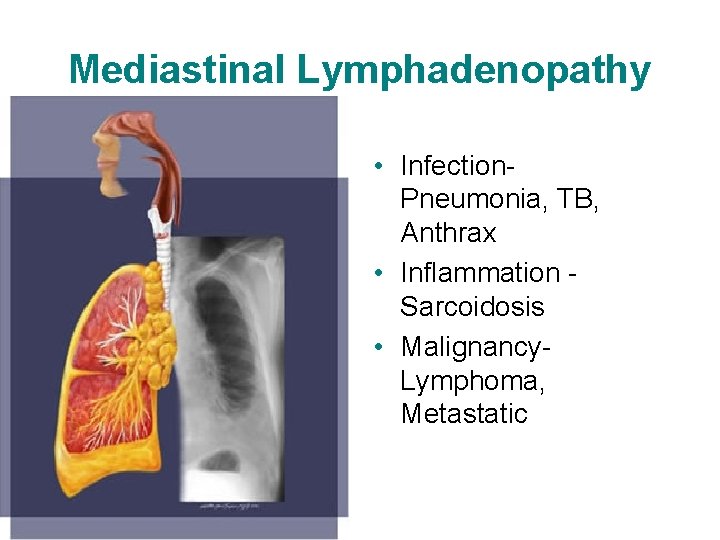
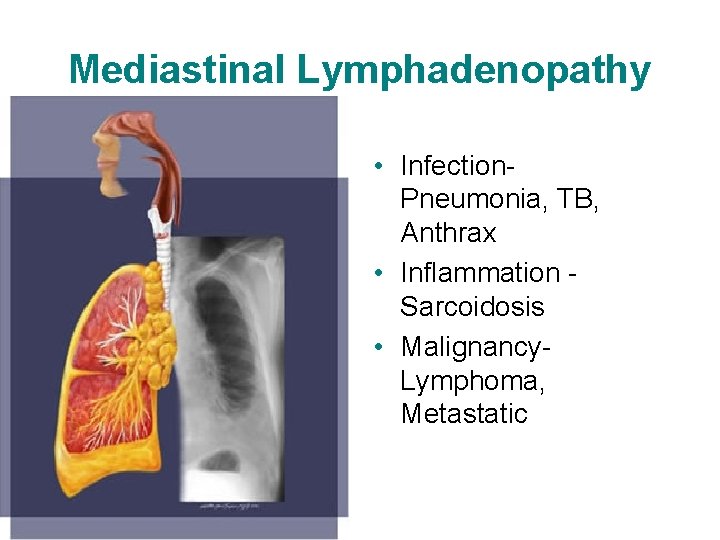
Mediastinal Lymphadenopathy • Infection. Pneumonia, TB, Anthrax • Inflammation Sarcoidosis • Malignancy. Lymphoma, Metastatic
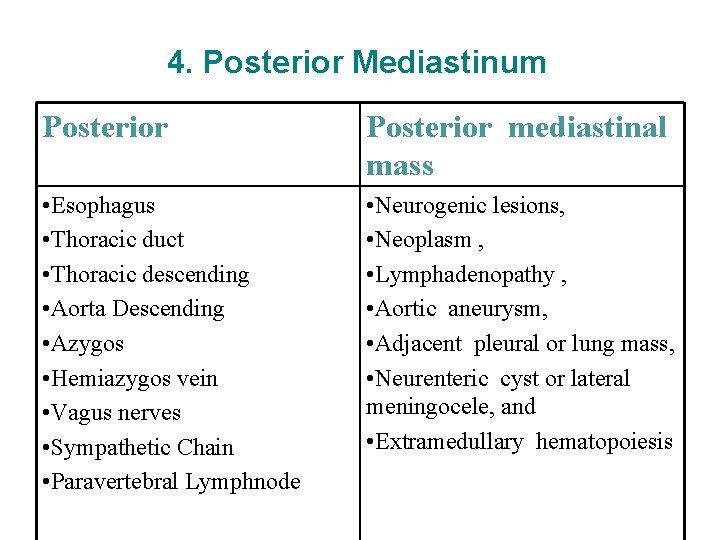
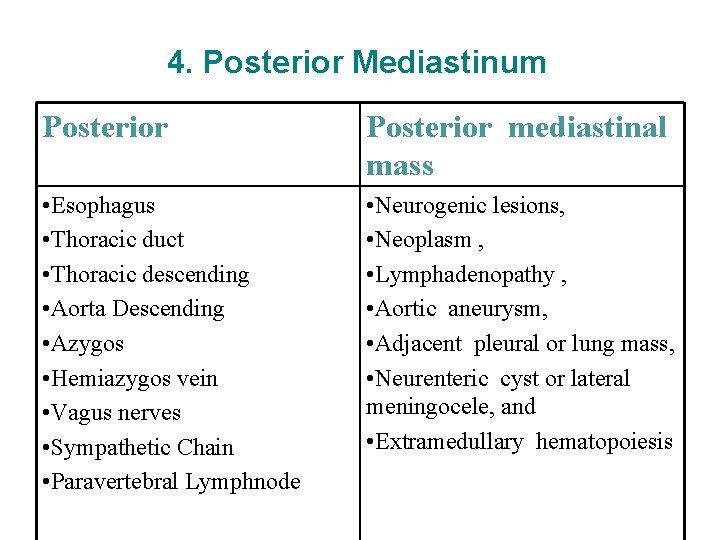
4. Posterior Mediastinum Posterior mediastinal mass • Esophagus • Thoracic duct • Thoracic descending • Aorta Descending • Azygos • Hemiazygos vein • Vagus nerves • Sympathetic Chain • Paravertebral Lymphnode • Neurogenic lesions, • Neoplasm , • Lymphadenopathy , • Aortic aneurysm, • Adjacent pleural or lung mass, • Neurenteric cyst or lateral meningocele, and • Extramedullary hematopoiesis
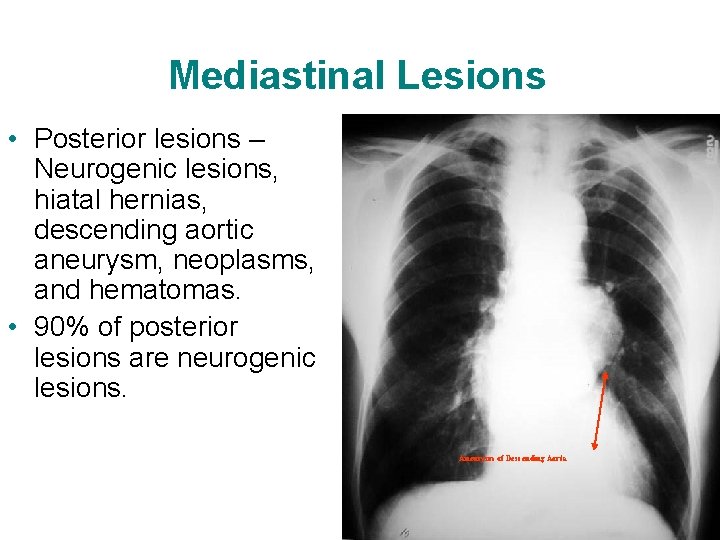
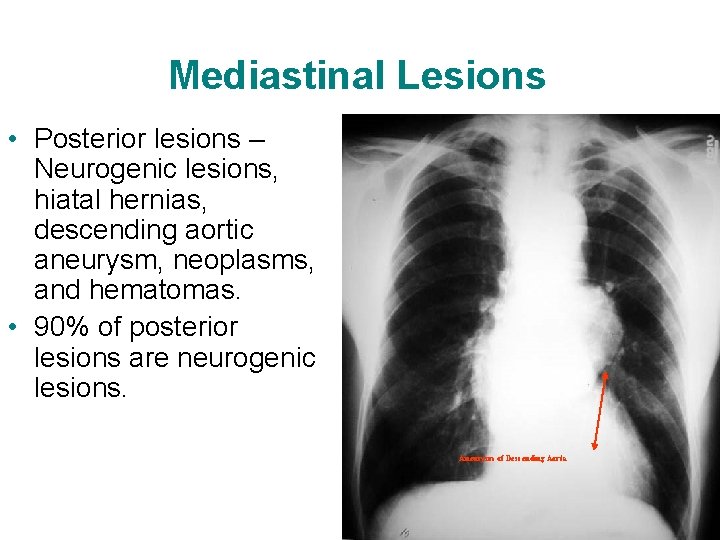
Mediastinal Lesions • Posterior lesions – Neurogenic lesions, hiatal hernias, descending aortic aneurysm, neoplasms, and hematomas. • 90% of posterior lesions are neurogenic lesions. Aneurysm of Descending Aorta

Posterior mediastinal masses will give double density over left side of heart.
Origins of Mediastinal Mass • • • Developmental Neoplastic Infectious Traumatic Cardiovascular disorders

Mediastinologists • • • Thoracic Surgeon Pulmonologist ENT Cardiologist Endoscopist Radiologist
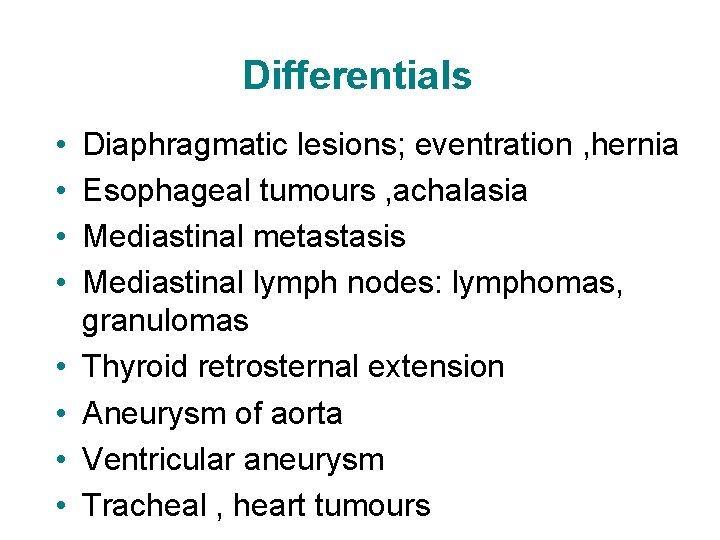
Differentials • • Diaphragmatic lesions; eventration , hernia Esophageal tumours , achalasia Mediastinal metastasis Mediastinal lymph nodes: lymphomas, granulomas Thyroid retrosternal extension Aneurysm of aorta Ventricular aneurysm Tracheal , heart tumours
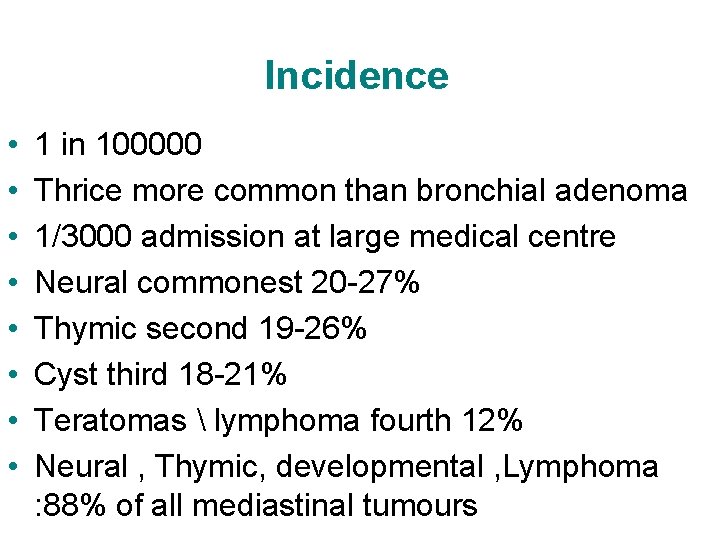
Incidence • • 1 in 100000 Thrice more common than bronchial adenoma 1/3000 admission at large medical centre Neural commonest 20 -27% Thymic second 19 -26% Cyst third 18 -21% Teratomas lymphoma fourth 12% Neural , Thymic, developmental , Lymphoma : 88% of all mediastinal tumours
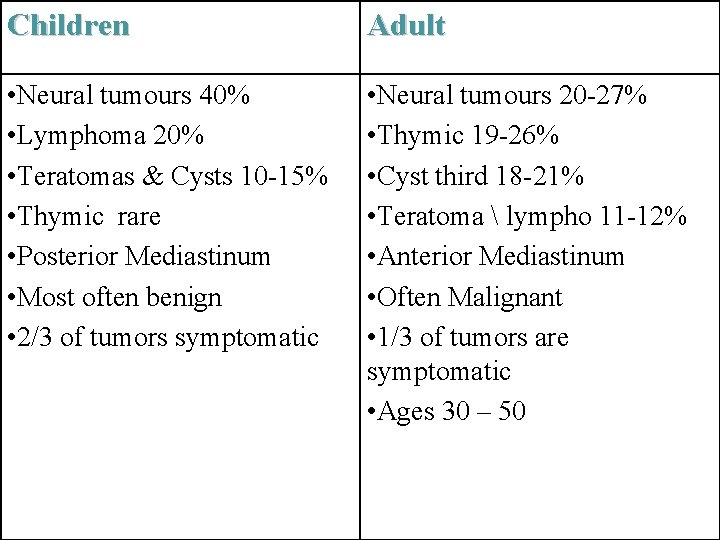
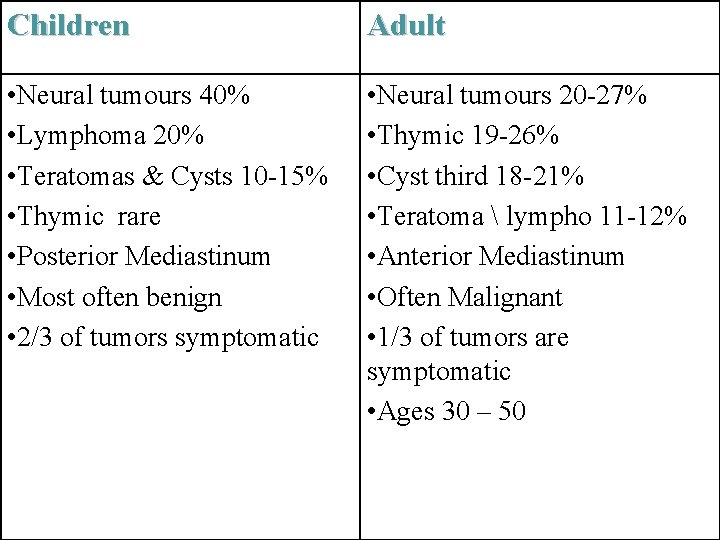
Children Adult • Neural tumours 40% • Lymphoma 20% • Teratomas & Cysts 10 -15% • Thymic rare • Posterior Mediastinum • Most often benign • 2/3 of tumors symptomatic • Neural tumours 20 -27% • Thymic 19 -26% • Cyst third 18 -21% • Teratoma lympho 11 -12% • Anterior Mediastinum • Often Malignant • 1/3 of tumors are symptomatic • Ages 30 – 50
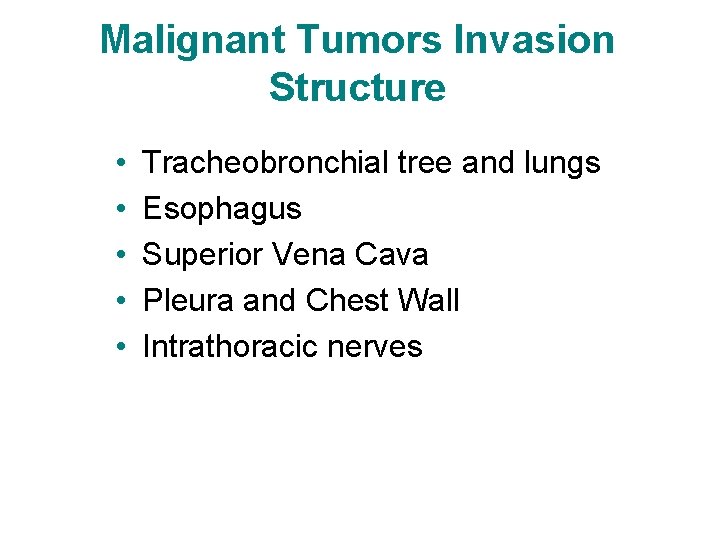
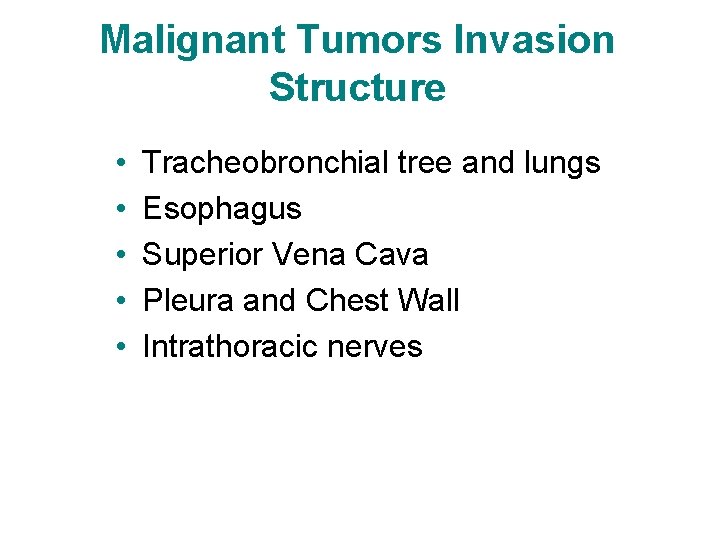
Malignant Tumors Invasion Structure • • • Tracheobronchial tree and lungs Esophagus Superior Vena Cava Pleura and Chest Wall Intrathoracic nerves
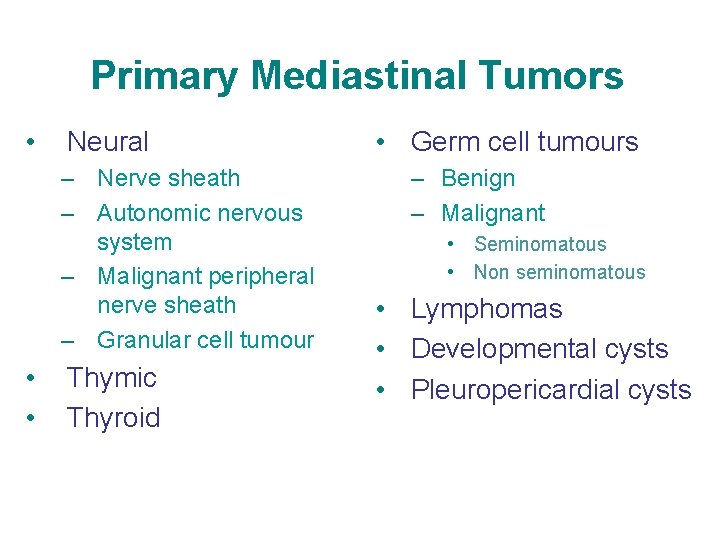
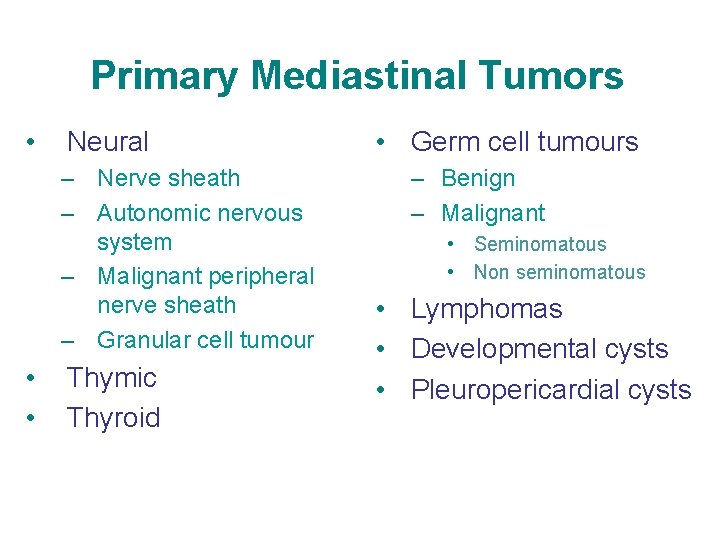
Primary Mediastinal Tumors • Neural – Nerve sheath – Autonomic nervous system – Malignant peripheral nerve sheath – Granular cell tumour • • Thymic Thyroid • Germ cell tumours – Benign – Malignant • Seminomatous • Non seminomatous • Lymphomas • Developmental cysts • Pleuropericardial cysts
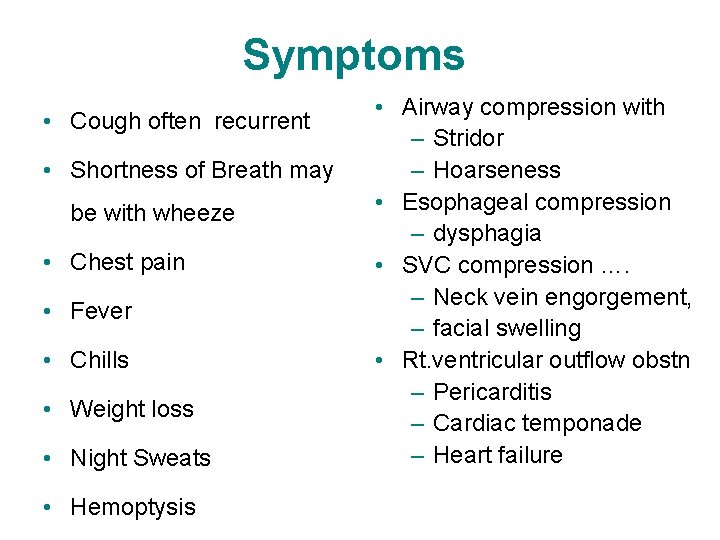
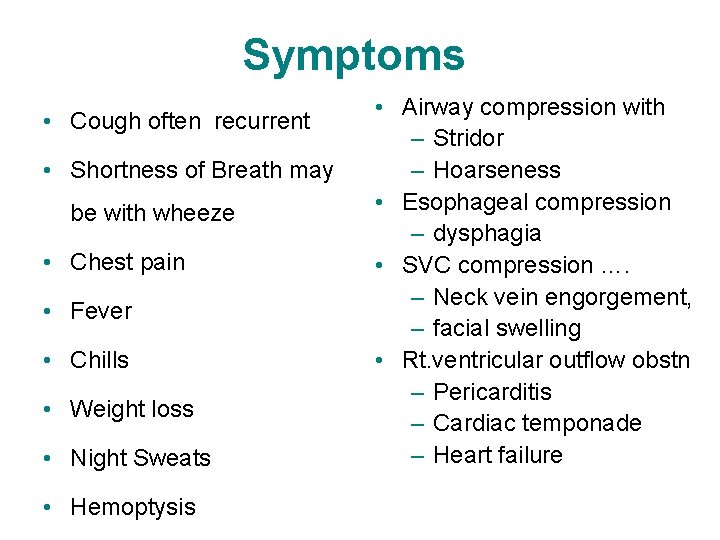
Symptoms • Cough often recurrent • Shortness of Breath may be with wheeze • Chest pain • Fever • Chills • Weight loss • Night Sweats • Hemoptysis • Airway compression with – Stridor – Hoarseness • Esophageal compression – dysphagia • SVC compression …. – Neck vein engorgement, – facial swelling • Rt. ventricular outflow obstn – Pericarditis – Cardiac temponade – Heart failure

Mediastinal Neural tumours Nerve sheath t 0 • Benign (neurolemmoma) – Schwannoma – Neurofibroma • Malignant peripheral nerve sheath t 0 – – – Neurosarcoma Neurofibrosarcoma Neurogenic sarcoma Malignant schwannoma Malignant neurinoma • Granular cell tumour Granular cell myoblastoma – Autonomic nervous system (neurocyte) • • Ganglioneuroma Ganglioneuroblastoma Neuroblastoma Paraganglioma – Aorticopulmonary – Aorticosympathetic
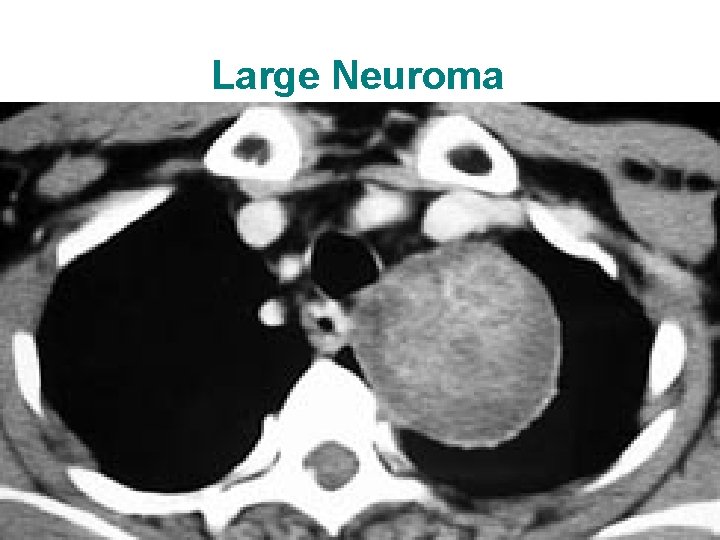
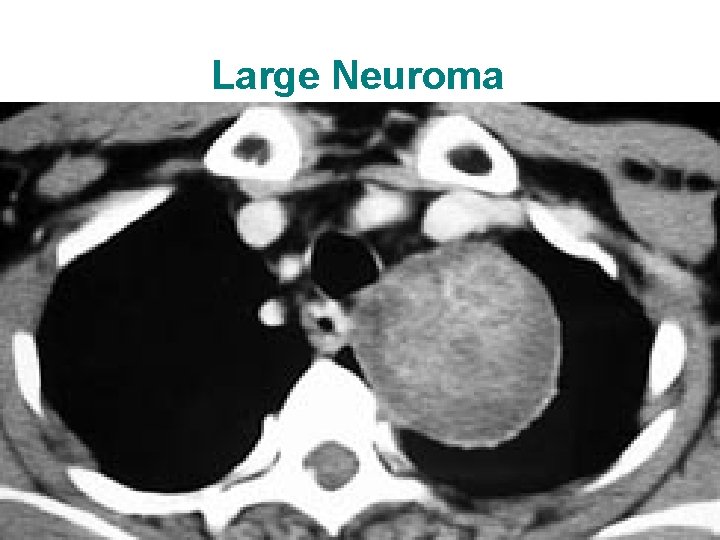
Large Neuroma
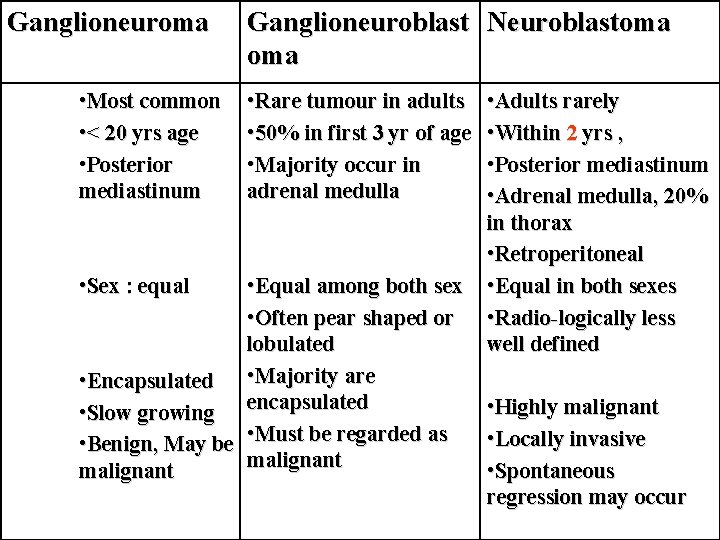
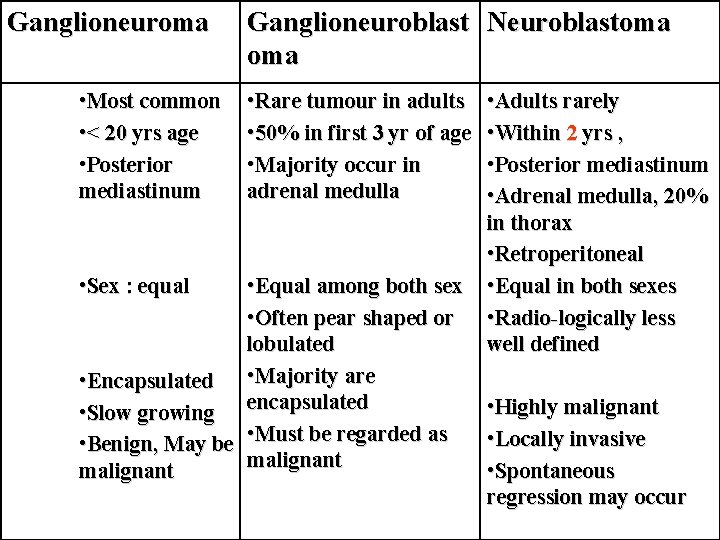
Ganglioneuroma • Most common • < 20 yrs age • Posterior mediastinum • Sex : equal Ganglioneuroblast Neuroblastoma • Rare tumour in adults • 50% in first 3 yr of age • Majority occur in adrenal medulla • Equal among both sex • Often pear shaped or lobulated • Encapsulated • Majority are • Slow growing encapsulated • Benign, May be • Must be regarded as malignant • Adults rarely • Within 2 yrs , • Posterior mediastinum • Adrenal medulla, 20% in thorax • Retroperitoneal • Equal in both sexes • Radio-logically less well defined • Highly malignant • Locally invasive • Spontaneous regression may occur

Intrathoracic Meningocele
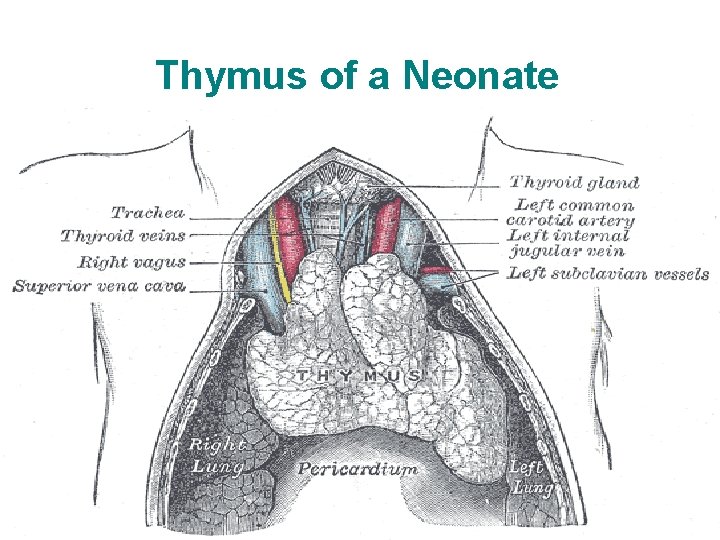
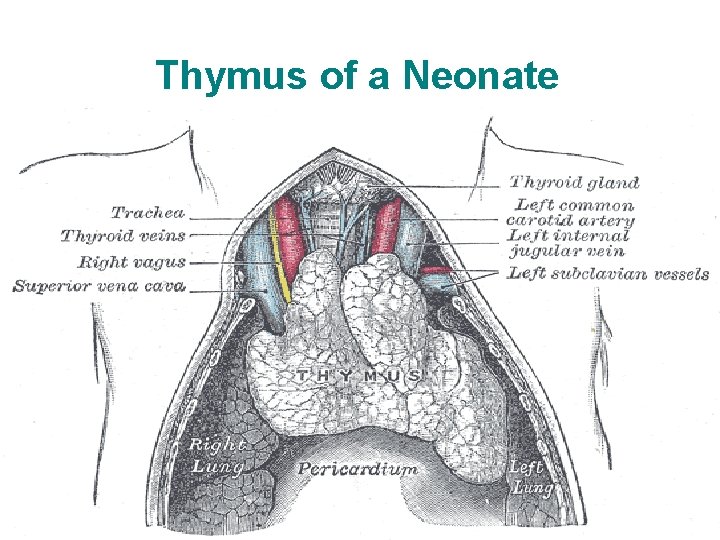
Thymus of a Neonate
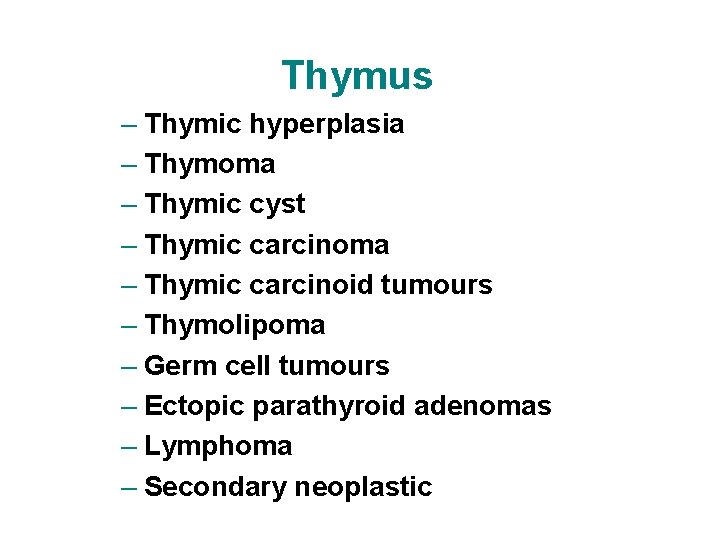
Thymus – Thymic hyperplasia – Thymoma – Thymic cyst – Thymic carcinoma – Thymic carcinoid tumours – Thymolipoma – Germ cell tumours – Ectopic parathyroid adenomas – Lymphoma – Secondary neoplastic
Thymic hyperplasia • • Nearly always infantile or childhood Usually asymptomatic Pronounced in HIV, SLE, Thyrotoxicosis Indistinct from other thymic t 0 on Radio or CT • Steroids may reduce • Subtotal surgery
Thymoma • Epithelial neoplasms • most common primary neoplasms of the anterior superior mediastinum • Any age , rare <20, nearly all middle-aged adults. • Male predominance • ½ of the patients are asymptomatic • 25 -30% of patients have symptoms related to compression of adjacent mediastinal structures including cough, chest pain, and shortness of breath
Thymoma • • • may have myasthenia gravis (30 -40%), pure red cell aplasia, hypogammoglobulinemia, endocrine disorders can be completely encapsulated (benign) or locally invasive without a fibrous capsule • classified by predominant cell types: – epithelial, – lymphoid, or – Biphasic , mixed or lymphoepithelial type • one- third of thymomas are invasive and may grow into the surrounding mediastinal structures,
Thymoma • This is determined at surgery and is not a histologic diagnosis, • local invasion of the pleura occurs frequently, • distant metastases are infrequent • Surgical removal enmass with capsule intact – Median sterotomy – Thoracotomy – Transcervical approach • Radiotherapy usually reserved for incomplete excission • Chemo-sensitive (May be) : cis, doxo, vin, c-phos
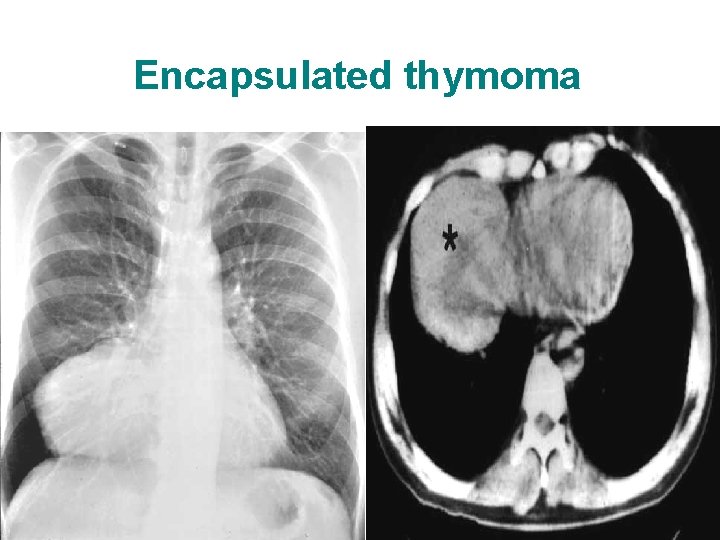
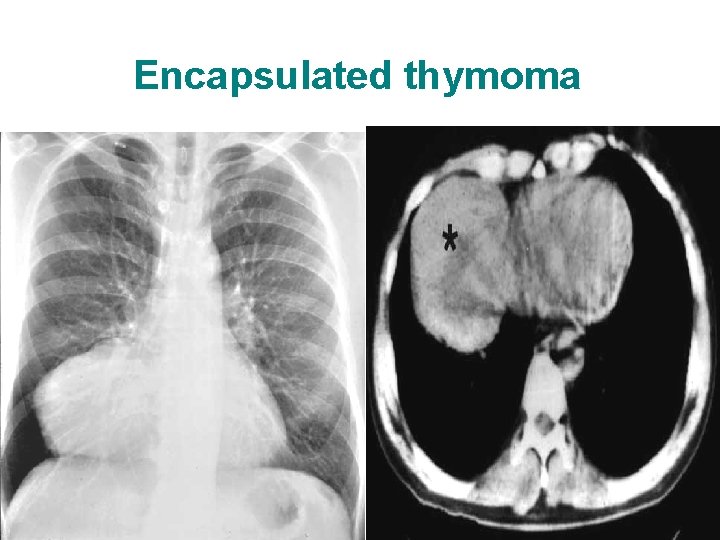
Encapsulated thymoma
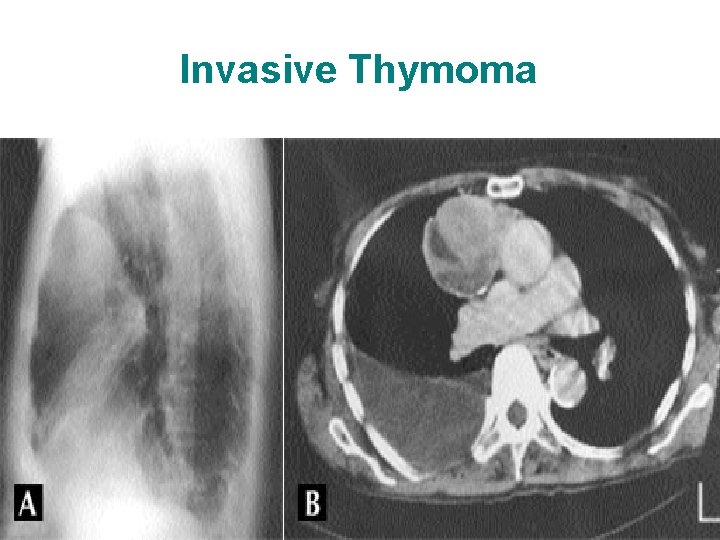
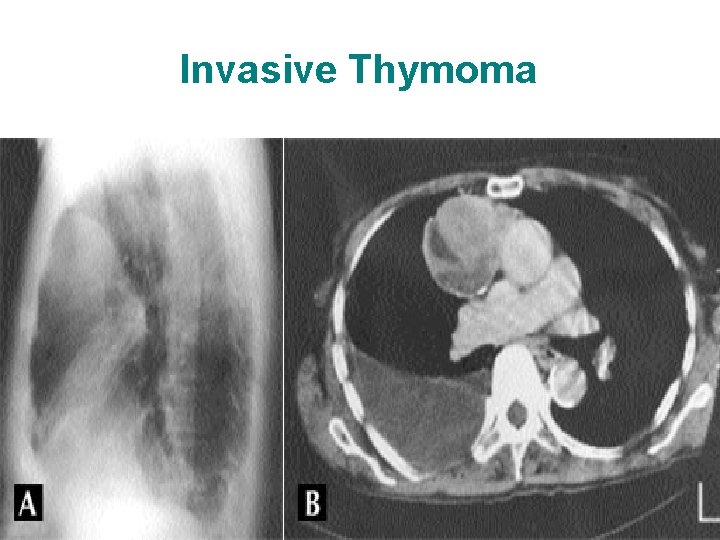
Invasive Thymoma
Germ cell tumours • As a result of the proliferation of the primary extragonadal germ cell • Mostly found near the midline – Adults : anterior mediastinum – Child : sacrococcygeal area
Germ cell tumours • Benign – Mature cystic teratoma • Malignant – Seminomatous* : – Non Seminomatous*
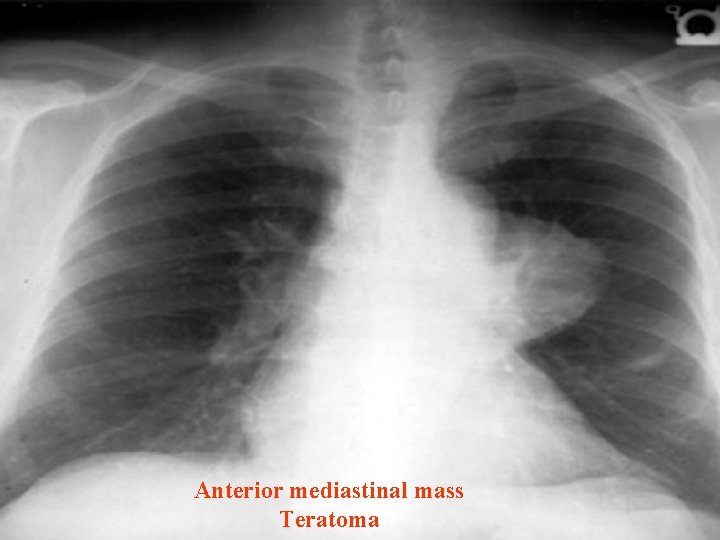
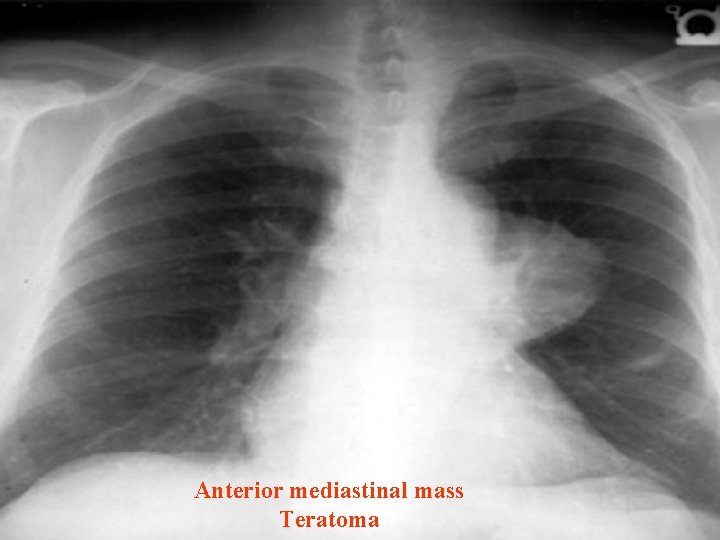
Anterior mediastinal mass Teratoma
Malignant Germ cell tumours • Seminomatous* : Seminoma – Exclusively young male 20 -40 yrs – 1/3 asymptomatic , – Chest pain, dysponea, SVC obstruction – Radio ; lobulated , non cacified , anterior mediastinal – Normal serum AFP – USG testicle discrete hypoecoic masses, with microcalcifictions – Treatment ; chemotherapy* , Radio or combi • Et +cis *4 cycle or Et +cis +bleo * 3 cycles • Highly radiosensitive radio reserved for bulky

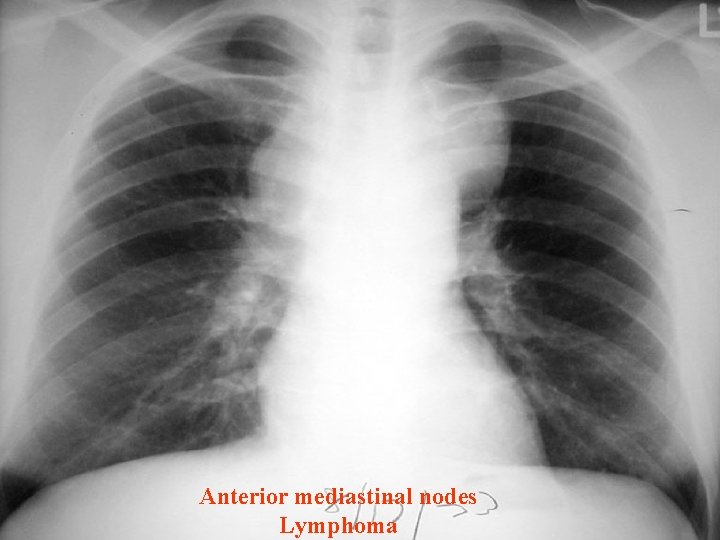
Mediastinal Lymphoma • Mediastinum is involved in 50% Hodgkin’s diseases • Most cases are of nodular sclerosing type • Treatable and many are curable too • Intensive chemotherapy or radiotherapy or both • Radio alone relapse 50 -74% • Chemo alone relapse 33 -50% • “MOPP” or “DBVD” followed by radio preferred
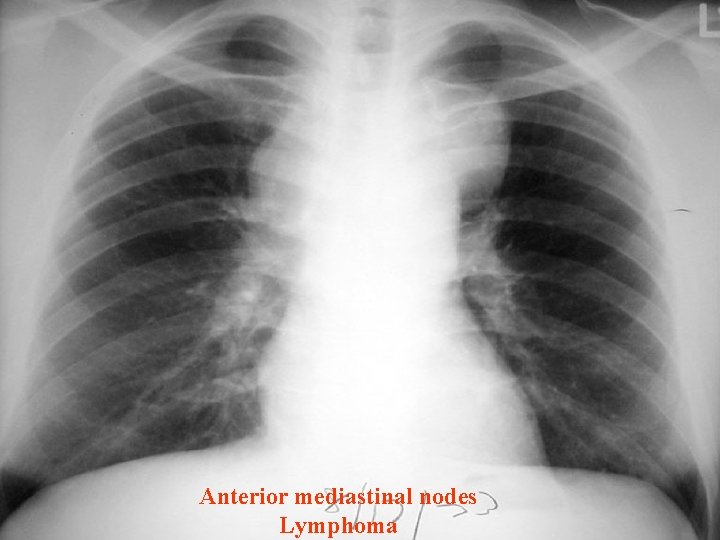
Anterior mediastinal nodes Lymphoma

Anterior mediastinal nodes Lymphoma
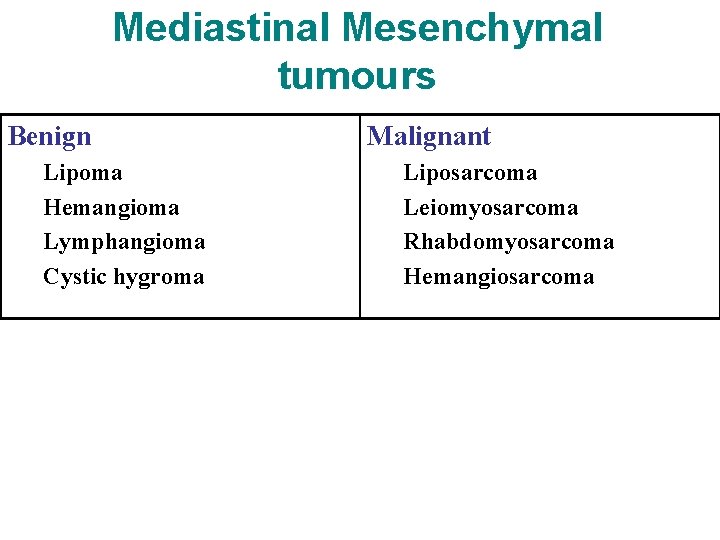
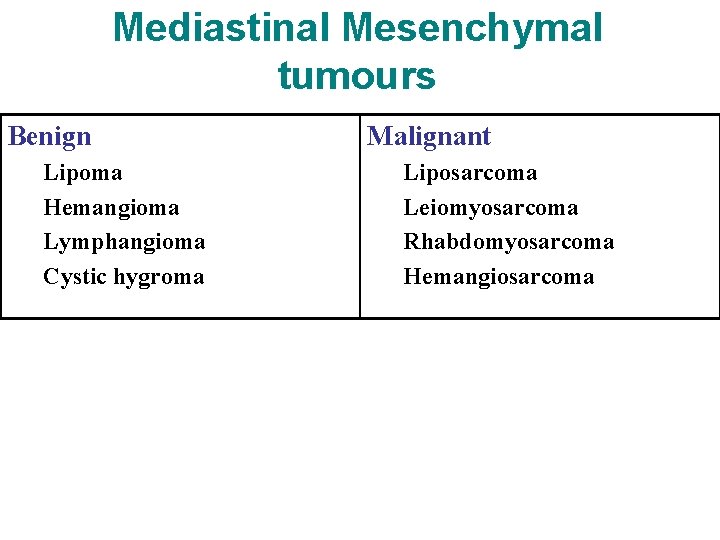
Mediastinal Mesenchymal tumours Benign Lipoma Hemangioma Lymphangioma Cystic hygroma Malignant Liposarcoma Leiomyosarcoma Rhabdomyosarcoma Hemangiosarcoma

Angiolipoma
Developmental Mediastinal cysts • Congenital ; 16% of all mediastinal cyst 16% • Foregut duplication largest group • Pleuropericardial next to it
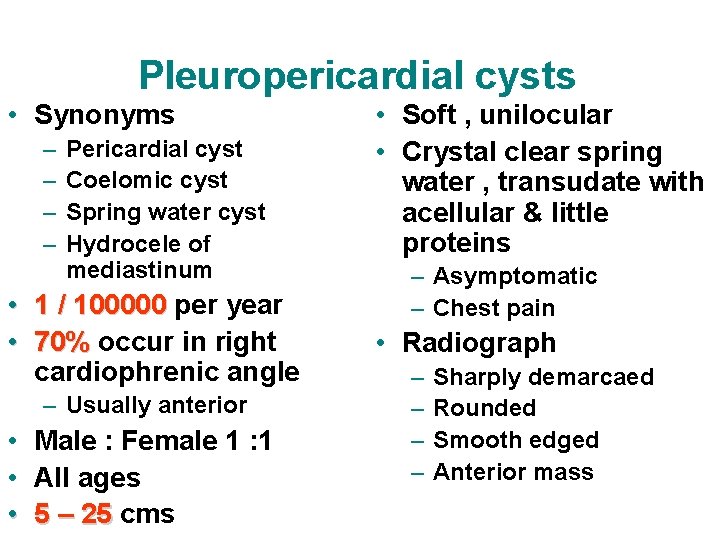
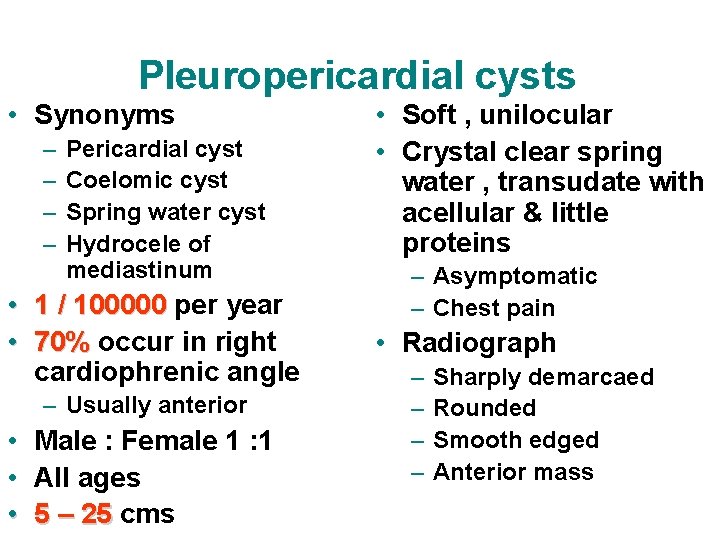
Pleuropericardial cysts • Synonyms – – Pericardial cyst Coelomic cyst Spring water cyst Hydrocele of mediastinum • 1 / 100000 per year 1 / 100000 • 70% occur in right 70% cardiophrenic angle – Usually anterior • • • Male : Female 1 : 1 All ages 5 – 25 cms 5 – 25 • Soft , unilocular • Crystal clear spring water , transudate with acellular & little proteins – Asymptomatic – Chest pain • Radiograph – – Sharply demarcaed Rounded Smooth edged Anterior mass
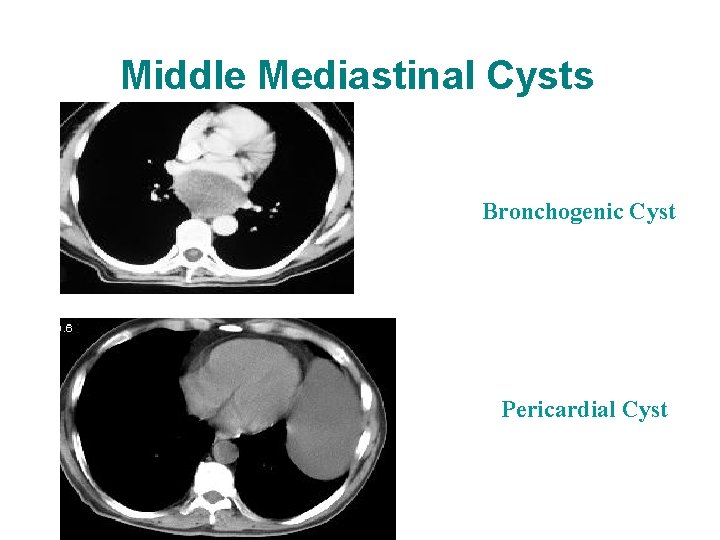
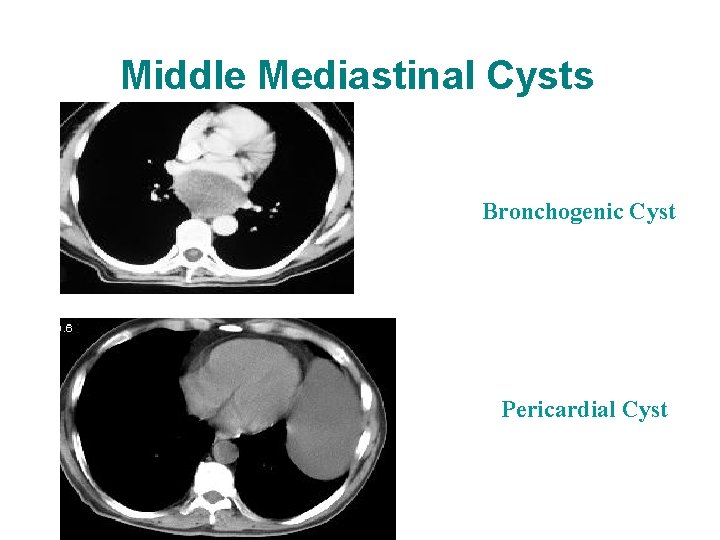
Middle Mediastinal Cysts Bronchogenic Cyst Pericardial Cyst
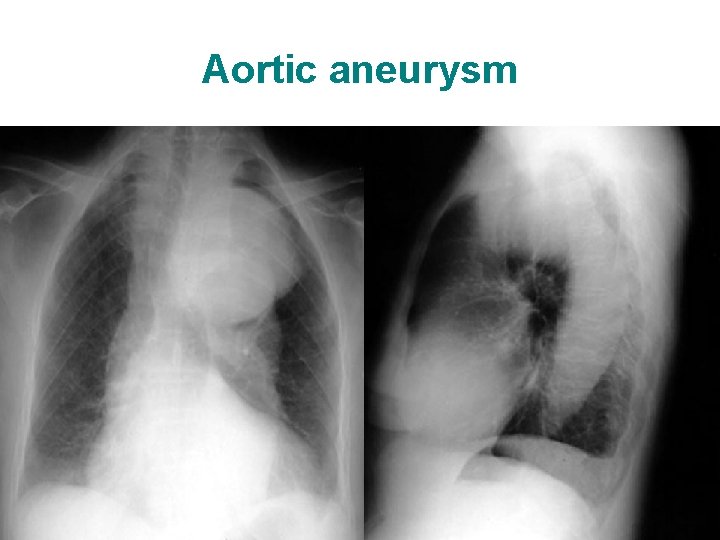
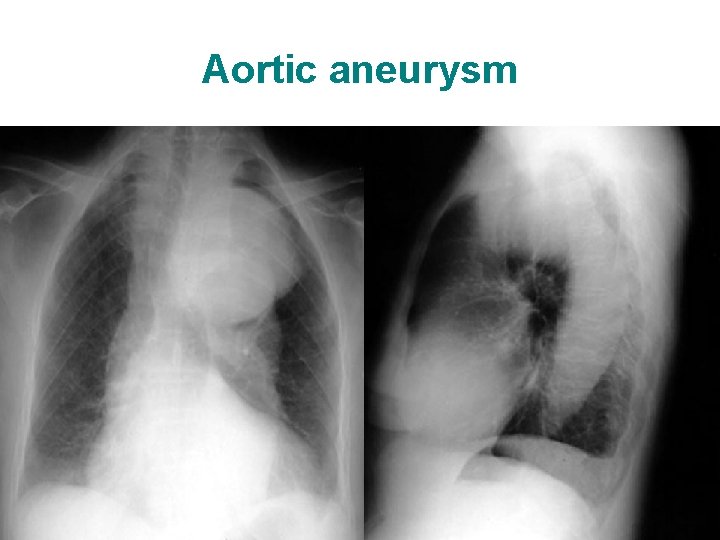
Aortic aneurysm
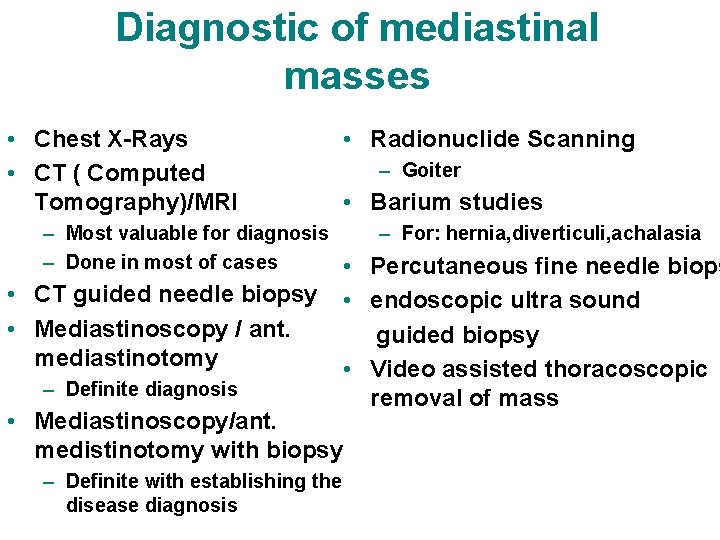
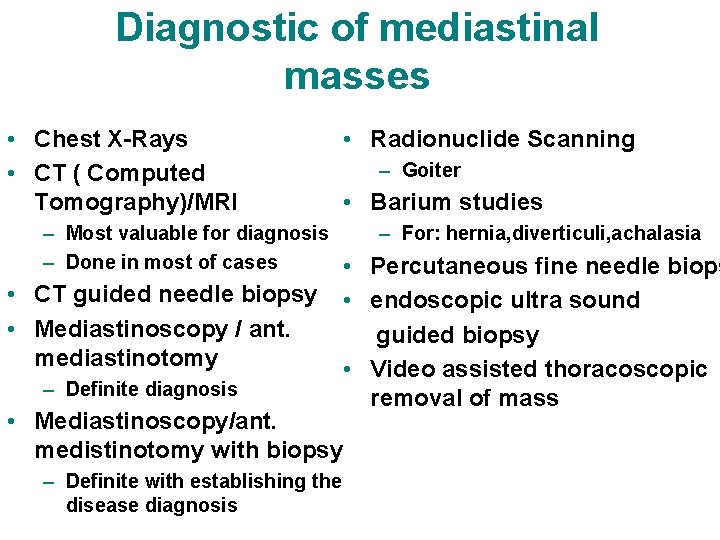
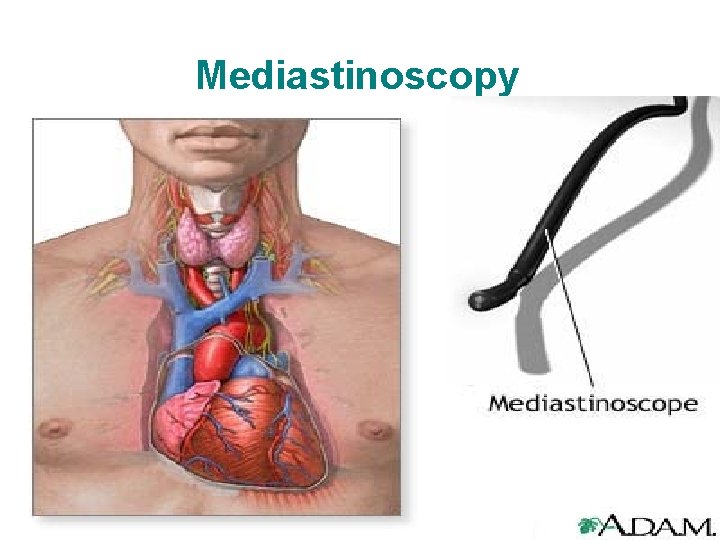
Diagnostic of mediastinal masses • Chest X-Rays • CT ( Computed Tomography)/MRI • Radionuclide Scanning – Goiter • Barium studies – For: hernia, diverticuli, achalasia – Most valuable for diagnosis – Done in most of cases • Percutaneous fine needle biops • CT guided needle biopsy • Mediastinoscopy / ant. mediastinotomy – Definite diagnosis • endoscopic ultra sound guided biopsy • Video assisted thoracoscopic removal of mass • Mediastinoscopy/ant. medistinotomy with biopsy – Definite with establishing the disease diagnosis
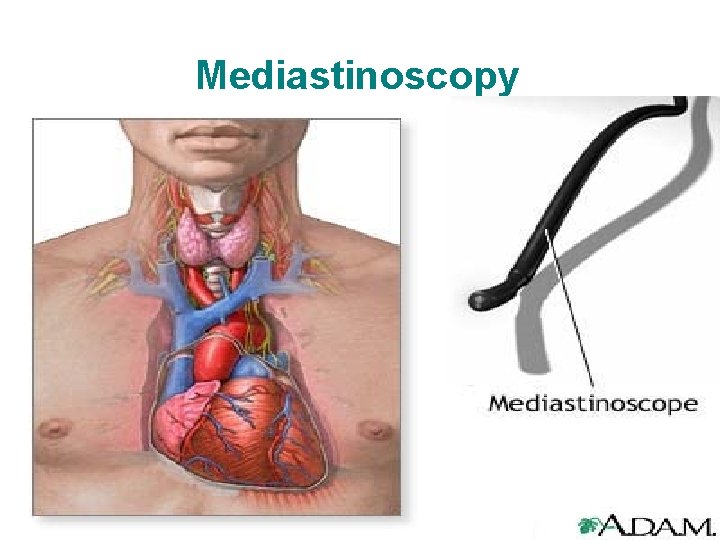
Mediastinoscopy

Mediastinoscopy: Overused, Invasive, Limited Applications
• Mediastinoscopy: Invasive, requires general anesthesia. Subcarinal and subaortic (a-p window) nodes inaccessible.
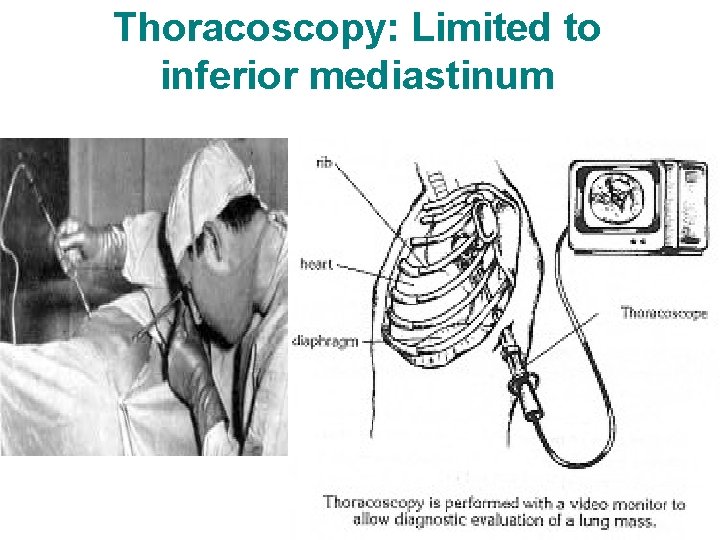
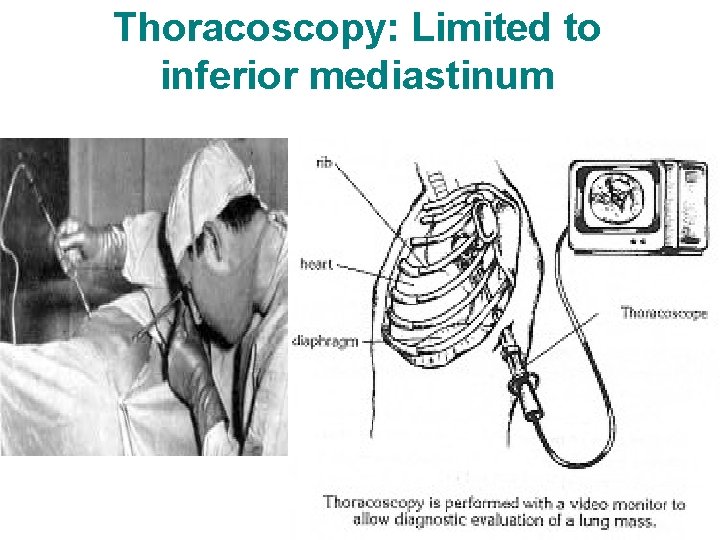
Thoracoscopy: Limited to inferior mediastinum
• Thoracoscopic biopsy (video-assisted thoracoscopy) Limited to inferior mediastinum.
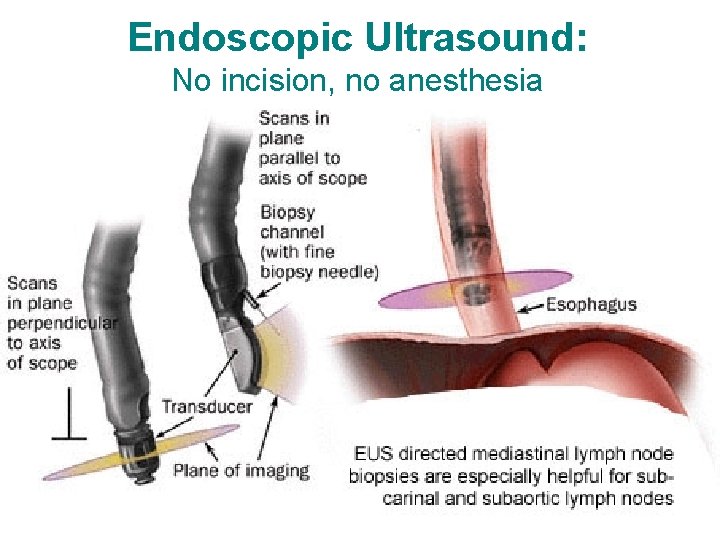
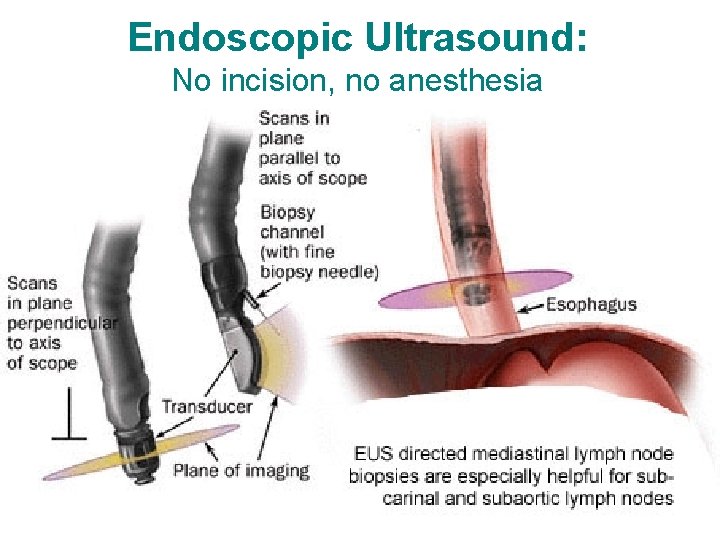
Endoscopic Ultrasound: No incision, no anesthesia
Endoscopic ultrasound guided biopsy of mediastinal lesions has a major impact on patient management. • It is a safe and sensitive minimally invasive method for evaluating patients with a solid lesion of the mediastinum suspected by CT scanning. • It has a significant impact on patient management and should be considered for diagnosing the spread of cancer to the mediastinum in patients with lung cancer considered for surgery, as well as for the primary diagnosis of solid lesions located in the mediastinum adjacent to the oesophagus. Thorax 2002 Feb; 57(2): 98 -103

• “Endoscopic ultrasonography also provides information helpful for clinical staging of lung cancer and is the procedure of choice for performing fineneedle aspiration biopsy of posterior mediastinal and subcarinal lymph nodes. ” AJCC manual 2007
CT scan or MRI • CT scan or MRI with contrast is always indicated for further evaluation. • MRI is preferred for neurogenic lesions but obtaining a CT scan is never wrong with a mediastinal mass. • CT-guided transthoracic fine needle aspiration (FNA): Limited by surrounding vascular structures, size of the targeted lesion. – Pneumothorax risk.

Prognosis • Varies depending on type of tumors and resection. • Benign tumors – excellent prognosis • Malignant tumors – depends on the type
 Inferior vena cava mediastinum
Inferior vena cava mediastinum Epicardium
Epicardium Posterior mediastinum
Posterior mediastinum Middle mediastinum: contents mnemonic
Middle mediastinum: contents mnemonic Superior mediastinum contents
Superior mediastinum contents Definition of mediastinum
Definition of mediastinum Bracnhes of aorta
Bracnhes of aorta Subdivision of mediastinum
Subdivision of mediastinum What is geriatric syndromes
What is geriatric syndromes Cerebellar syndromes
Cerebellar syndromes Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology Best language nih
Best language nih Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Glomerulus cerebellaris
Glomerulus cerebellaris Poosterior
Poosterior Axillary lymph nodes drainage
Axillary lymph nodes drainage Mediastinal flatter
Mediastinal flatter Composition of lymphatic system
Composition of lymphatic system Root of lung anatomy
Root of lung anatomy Costodiaphragmatic recess
Costodiaphragmatic recess Pleural recesses
Pleural recesses Costal pleura
Costal pleura Achalasia cardia
Achalasia cardia Superior vs inferior mirage
Superior vs inferior mirage Flexion adduction internal rotation
Flexion adduction internal rotation Inferior vena cava tributaries
Inferior vena cava tributaries Solera superior
Solera superior Sindrome de neurona motora superior
Sindrome de neurona motora superior Via piramidal y via extrapiramidal
Via piramidal y via extrapiramidal Reproductive structure of a plant
Reproductive structure of a plant Pinza radial inferior y superior
Pinza radial inferior y superior Anterior/ventral
Anterior/ventral Superior and inferior colliculi
Superior and inferior colliculi Manto inferior y superior
Manto inferior y superior Foramen epiploicum arka duvarı
Foramen epiploicum arka duvarı Area nuda foie
Area nuda foie Trigonum linguale
Trigonum linguale Superior and inferior colliculi
Superior and inferior colliculi Poder calorifico superior
Poder calorifico superior Neurona motora superior e inferior
Neurona motora superior e inferior Ala ossis ilii fraktur
Ala ossis ilii fraktur Canino inferior anatomia
Canino inferior anatomia What does erect mean in anatomy
What does erect mean in anatomy Musculo semitendinoso
Musculo semitendinoso Distal and proximal
Distal and proximal Gemellus superior and inferior
Gemellus superior and inferior Brachium of superior colliculus
Brachium of superior colliculus Sistema eixo base
Sistema eixo base Impressiones gyrorum nedir
Impressiones gyrorum nedir Canalis pterygopalatina
Canalis pterygopalatina Tabla de distribucion de frecuencia
Tabla de distribucion de frecuencia Synthetic dicision
Synthetic dicision Long division vocabulary
Long division vocabulary Synthetic.division
Synthetic.division 369 times 2
369 times 2 Lethenic
Lethenic Regio thorax posterior
Regio thorax posterior Mediastinum heart
Mediastinum heart Mediastinum ehk
Mediastinum ehk Mediastinum
Mediastinum Contents of the middle mediastinum
Contents of the middle mediastinum Heart orientation
Heart orientation Spermatic cord function
Spermatic cord function Aortaruptur
Aortaruptur Mediastinum superius sınırları
Mediastinum superius sınırları Cadaver blood vessels
Cadaver blood vessels Middle mediastinum: contents mnemonic
Middle mediastinum: contents mnemonic