7 EKG Adaptations and Troubleshooting 7 REMEMBER The

7 EKG Adaptations and Troubleshooting
7 REMEMBER: The key responsibility of an EKG technician is to generate a correct and readable EKG tracing. This Learning Objective is an overview of situations that might require changes to the usual EKG procedures in order to achieve that goal. 2 EKG Adaptations and Troubleshooting 1. Define artifact and identify situations in which adjustments or adaptations may be required during EKG testing
7 EKG Adaptations and Troubleshooting 1. Discuss artifact and identify situations in which adjustments or adaptations may be required during EKG testing Artifact – interference or distortion that appears on an EKG tracing – may be caused by • Environmental factors • Defective equipment • Patient conditions 3
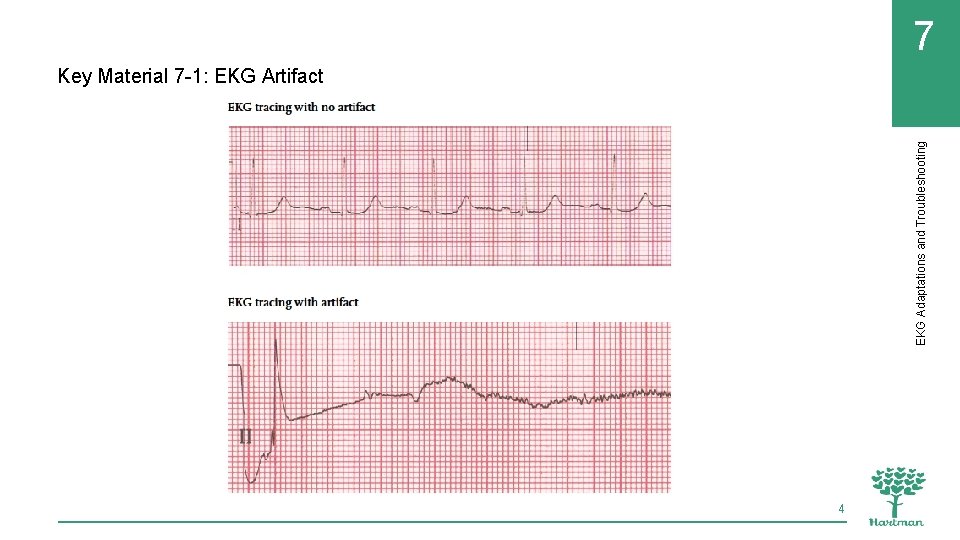
EKG Adaptations and Troubleshooting 7 Key Material 7 -1: EKG Artifact 4
7 These patient conditions/situations may require changes to standard EKG testing: • Pregnancy beyond the sixth month • Limb amputation or injury • Presence of scar tissue/broken skin • Situations in which the patient’s age or health condition affects the position of the heart 5 EKG Adaptations and Troubleshooting 1. Discuss artifact and identify situations in which adjustments or adaptations may be required during EKG testing
7 EKG Adaptations and Troubleshooting 1. Discuss artifact and identify situations in which adjustments or adaptations may be required during EKG testing EKG procedures may also have to be adapted for patients under Transmission-Based Precautions: • Disposable lead wires may be used • Testing may take place in a specially ventilated room • There may be different or additional procedures required for disinfection of EKG equipment after testing • EKG technicians should always follow any special infection prevention measures noted in the patient’s record or required by the facility 6
7 2. Demonstrate solutions to different types of EKG artifact EKG Adaptations and Troubleshooting Define the following terms: somatic tremor EKG artifact usually caused by patient tremors or shivering. wandering baseline EKG artifact in which the normally flat baseline moves up and down across the tracing. abrade in electrocardiography, to lightly scrub the outer layer of the skin to remove debris that can interfere with electrode contact. 7
7 2. Demonstrate solutions to different types of EKG artifact EKG Adaptations and Troubleshooting Define the following terms: electrical interference in electrocardiography, a type of artifact caused by the presence of other appliances or equipment in the area surrounding the EKG machine. broken recording EKG artifact that occurs when the signal is compromised by frayed or faulty lead wires. 8
7 REMEMBER: Although many modern EKG machines can detect and correct for artifact, recognizing the possible causes of artifact and knowing how to correct artifact are still essential skills for EKG technicians. 9 EKG Adaptations and Troubleshooting 2. Demonstrate solutions to different types of EKG artifact
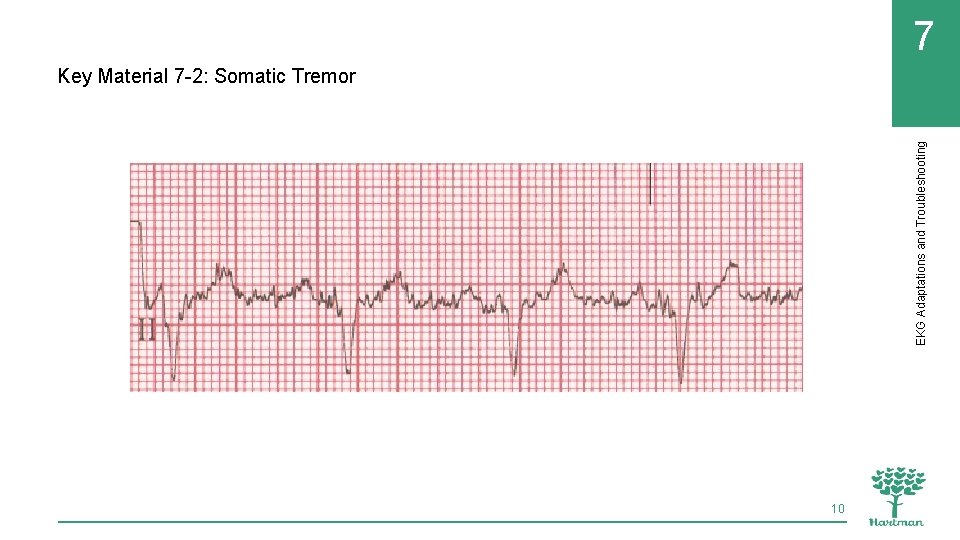
7 EKG Adaptations and Troubleshooting Key Material 7 -2: Somatic Tremor 10
7 Remember these points about addressing somatic tremor artifact: • Patients with Parkinson’s disease or other medical problems may need to be positioned with their hands palms-up under their buttocks to reduce tremors • Placing limb electrodes on the torso may reduce artifact in patients with tremors • Blankets can help stop tremors in patients who are cold, as can increasing the room temperature • Pillows may be used to make a patient more comfortable and less likely to tremble or move • Anxious or nervous patients should be reassured and given time to relax 11 EKG Adaptations and Troubleshooting 2. Demonstrate solutions to different types of EKG artifact
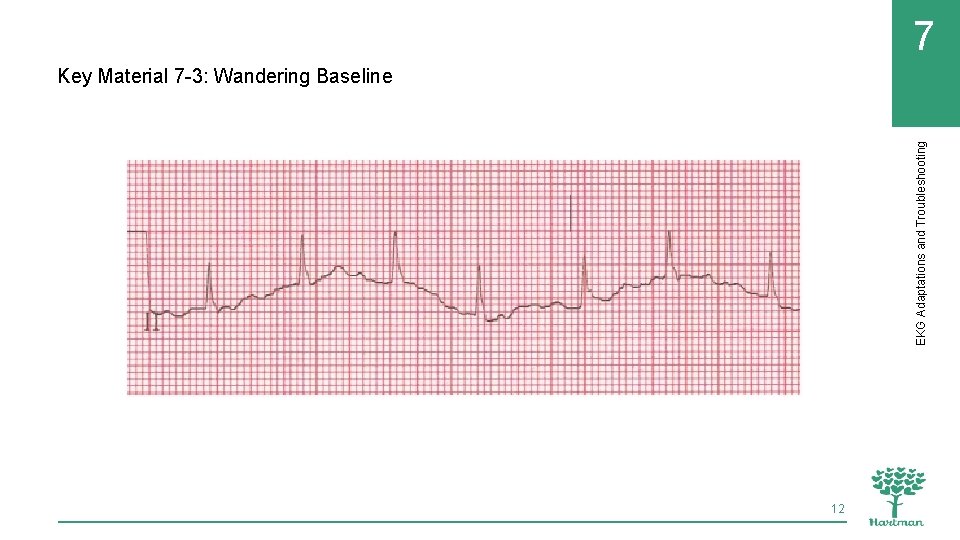
7 EKG Adaptations and Troubleshooting Key Material 7 -3: Wandering Baseline 12
7 Remember these points about addressing wandering baseline artifact: • Movement of muscle groups like those used for breathing can cause wandering baseline, so it can be helpful to remind patients to remain still and breathe normally • Placing the electrodes for the limb leads on the wrists and ankles can help eliminate wandering baseline caused by breathing irregularities • Loose electrodes or poor electrode contact are common causes of wandering baseline. The following skin preparation techniques can improve electrode contact: • Remove sweat or moisture with towel, paper towel, or gauze pads. • Remove skin oil or substances like lotion with soap and water. • Gently abrade the skin using dry gauze or a special skin abrading product. • Remove body hair as needed to increase contact between skin and electrodes (use only medical clippers) 13 EKG Adaptations and Troubleshooting 2. Demonstrate solutions to different types of EKG artifact
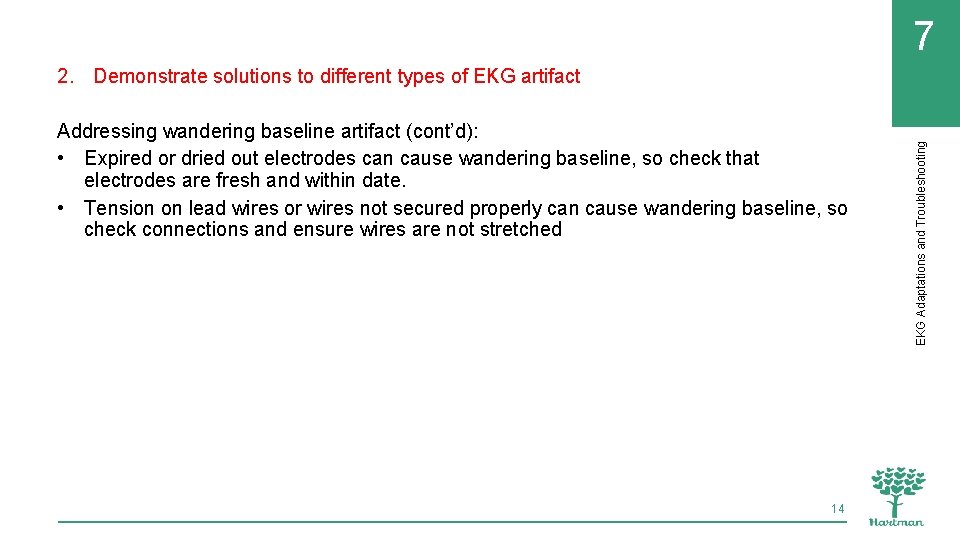
7 Addressing wandering baseline artifact (cont’d): • Expired or dried out electrodes can cause wandering baseline, so check that electrodes are fresh and within date. • Tension on lead wires or wires not secured properly can cause wandering baseline, so check connections and ensure wires are not stretched 14 EKG Adaptations and Troubleshooting 2. Demonstrate solutions to different types of EKG artifact
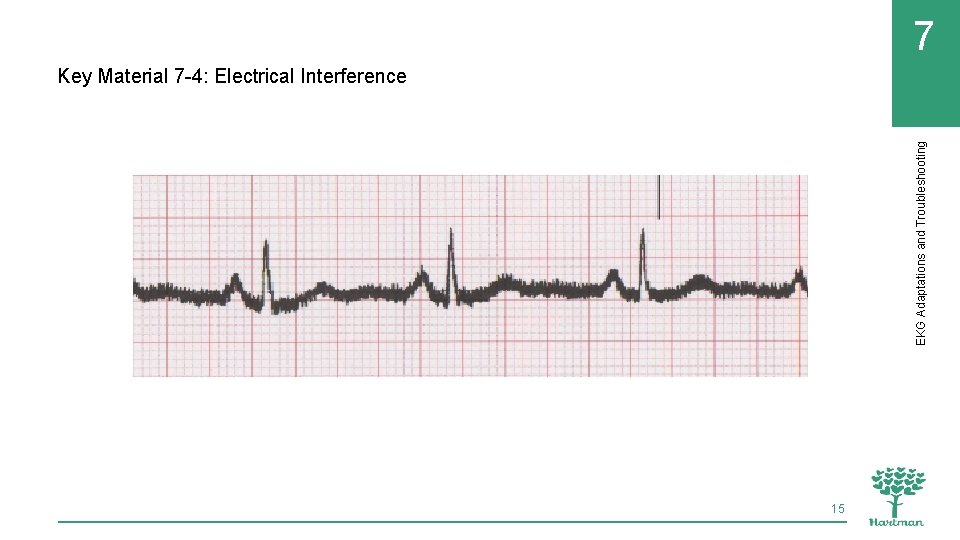
7 EKG Adaptations and Troubleshooting Key Material 7 -4: Electrical Interference 15
7 Remember these points about addressing electrical interference artifact: • Turn off other electrical appliances in the area • Plug the EKG machine in to a different outlet • If an extension cord is being used, discontinue use of extension cord • Make sure the machine is properly grounded (three prongs on the cord, plugged in to a three-prong outlet) • Turn off fluorescent lights • Mobile phones can cause electrical interference, so any phones in the room should be removed from the immediate testing area 16 EKG Adaptations and Troubleshooting 2. Demonstrate solutions to different types of EKG artifact
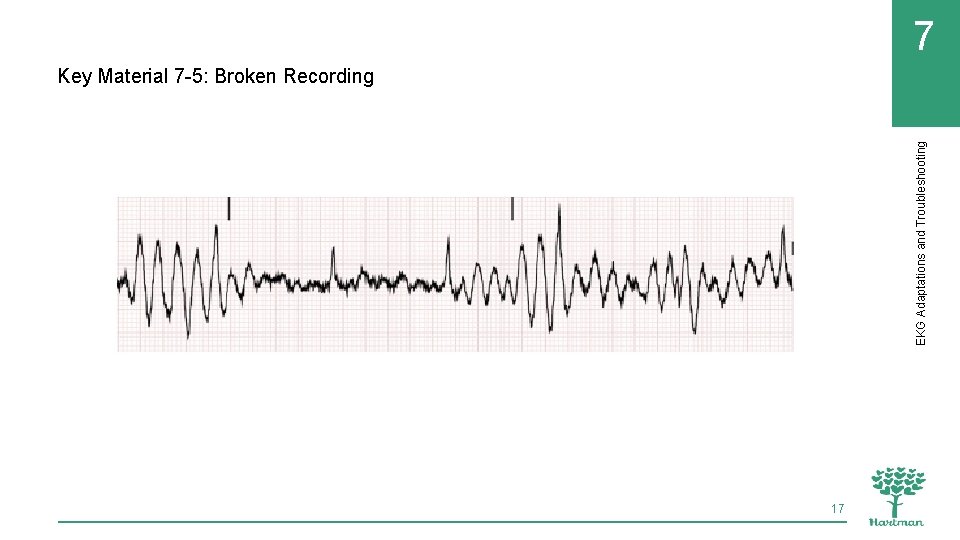
7 EKG Adaptations and Troubleshooting Key Material 7 -5: Broken Recording 17
7 2. Demonstrate solutions to different types of EKG artifact EKG Adaptations and Troubleshooting Making a habit of double-checking all of the following will help ensure accurate, artifactfree EKG tracings: • Fresh, in-date electrodes adhering properly to the patient’s skin • Electrodes in the correct locations and attached to the correct lead wires • Lead wires properly connected to the electrodes and to the machine • Lead wires not frayed or damaged in any way 18
7 Define the following term: dextrocardia a rare heart condition that causes the heart to develop pointing to the right side of the chest instead of the left side. 19 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
7 REMEMBER: Most resting EKGs are performed with the patient in supine position, using standard electrode placement. Any change to this situation should be documented in the patient’s medical record. 20 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
7 Remember these points about dextrocardia: • It is a rare heart condition that causes the heart to develop pointing to the right side of the chest rather than to the left side • The patient is usually aware of this condition or it is noted in the chart • If the electrodes are placed in the standard, left-sided positions, the EKG will not be accurate 21 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
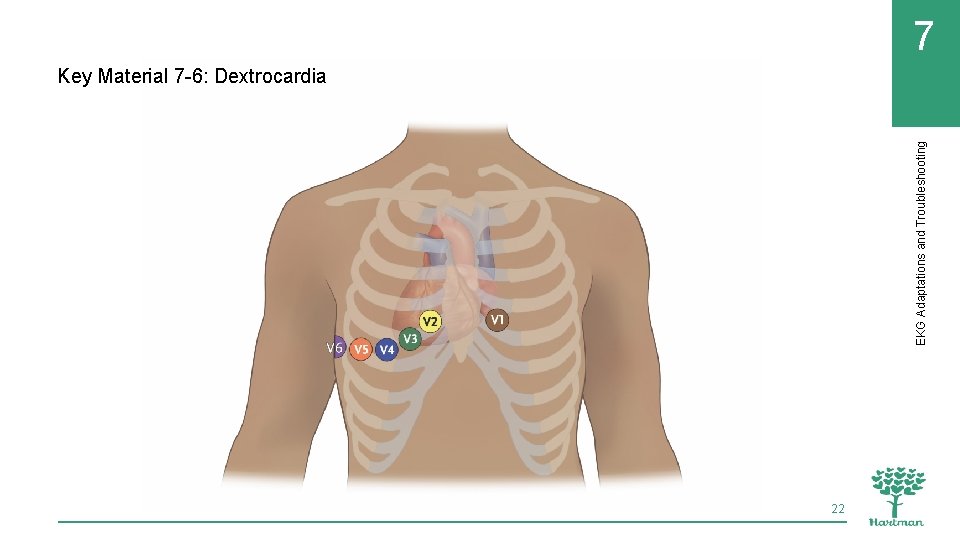
EKG Adaptations and Troubleshooting 7 Key Material 7 -6: Dextrocardia 22
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients Remember these points about electrode placement for patients with limb amputation or injury: • A patient who has had a limb amputation or who has an injury that limits access to a limb requires adapted electrode placement • The key for adaptations is that the electrode for the corresponding, unaffected limb should be placed in a mirror position 23
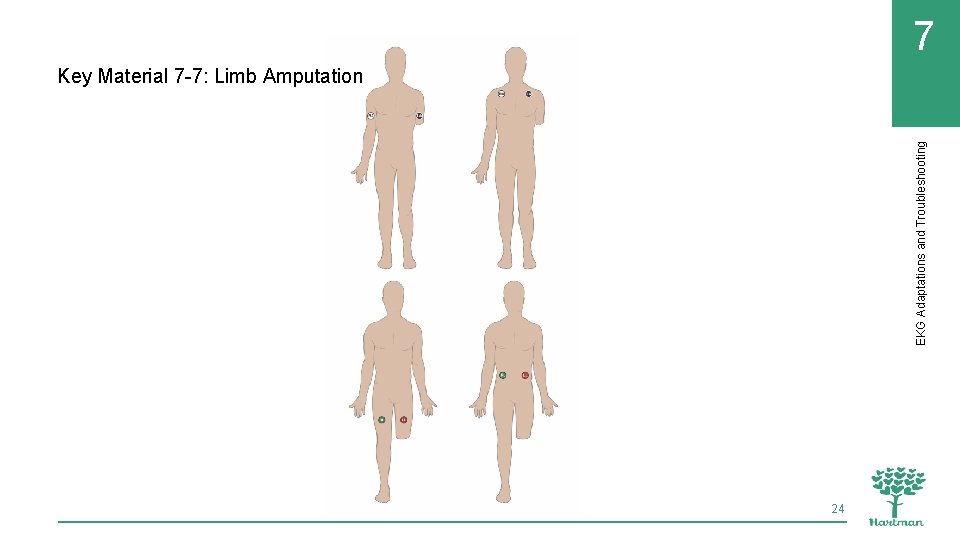
7 EKG Adaptations and Troubleshooting Key Material 7 -7: Limb Amputation 24
7 Remember these points about electrode placement for patients who have undergone mastectomy or who have scars on/injury to the chest wall: • Avoid placing electrodes on scar tissue, which can be fragile and may be injured when the electrode is removed • Electrodes should be placed as close as possible to the standard locations 25 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
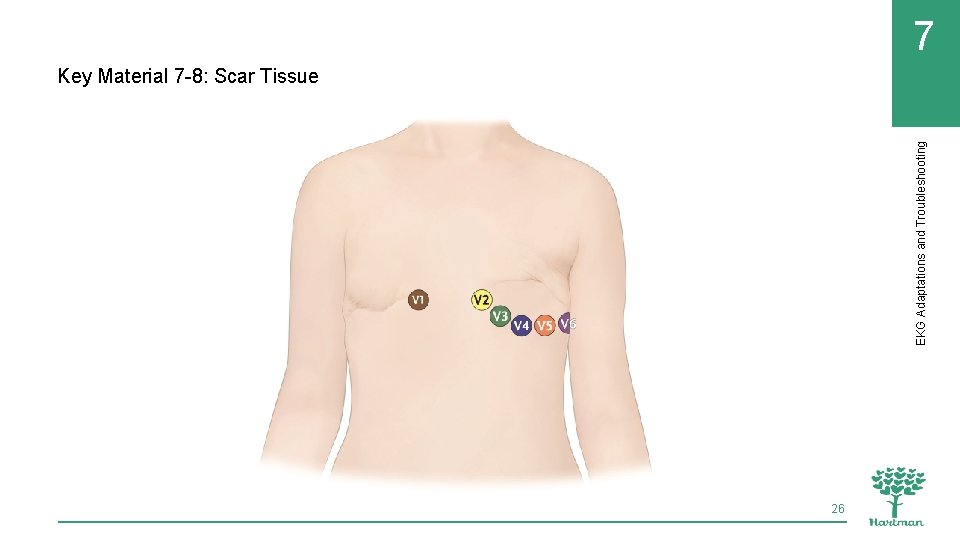
EKG Adaptations and Troubleshooting 7 Key Material 7 -8: Scar Tissue 26
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients REMEMBER: Electrodes should not be placed over medical implants (such as pacemakers) or over breast implants, but should be placed as close as possible to the standard positions. 27
7 Remember these points about electrode placement for patients with large breasts: • Move breast tissue away from the electrode site as much as possible so the electrodes are placed on the chest wall • Explain the process to the patient and get the patient’s consent before making any contact • The patient can lift her own breast tissue or the technician can use the back of a hand to move the tissue • Electrodes should be placed as closely as possible to the standard position and should not be placed on top of breast tissue 28 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients Electrode placement for pediatric patients differs from placement for adult patients: • Children under two years of age require right-sided placement • Children between two and twelve require adapted placement as shown in the next slide 29
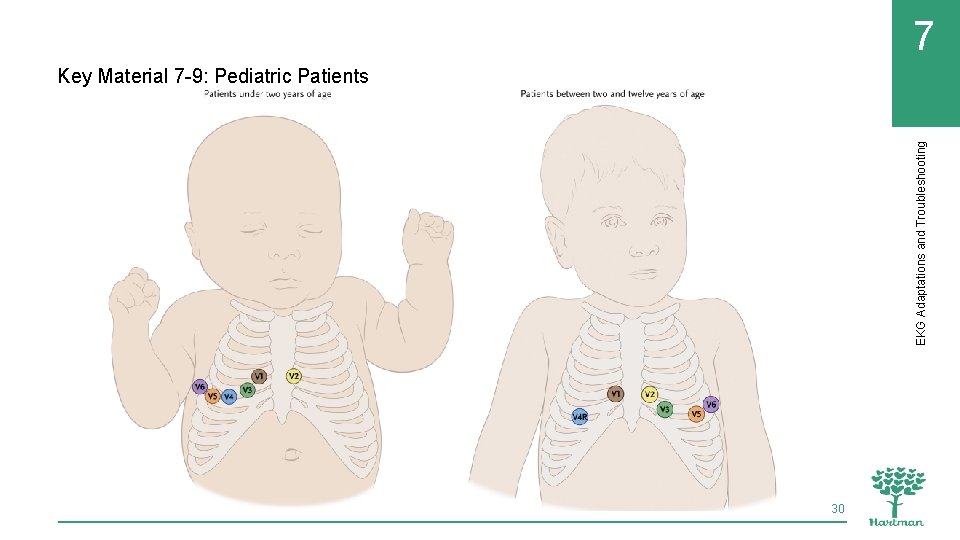
7 EKG Adaptations and Troubleshooting Key Material 7 -9: Pediatric Patients 30
7 REMEMBER: In addition to adapting electrode placement for pediatric patients, it is important to use appropriate language and to answer their questions and put them at ease. Small children may be calmer in a parent’s or guardian’s arms during the EKG. 31 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients Remember these points about posterior EKGs: • Sometimes a doctor will ask to have an EKG repeated using posterior leads • This can help to diagnose a particular type of heart attack (inferior wall myocardial infarction) 32
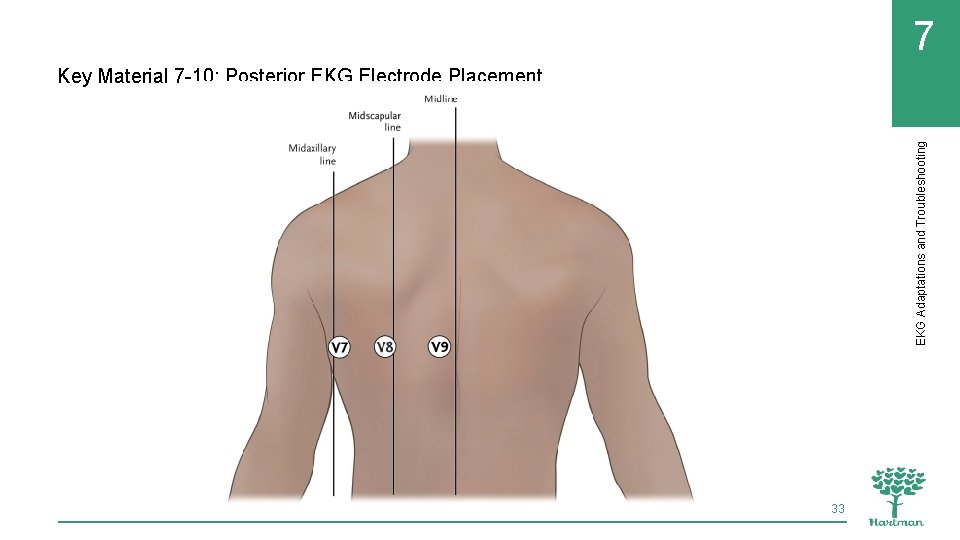
7 EKG Adaptations and Troubleshooting Key Material 7 -10: Posterior EKG Electrode Placement 33
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients REMEMBER: It is crucial for the EKG technician to mark as posterior EKG to reflect the change in electrode placement. 34
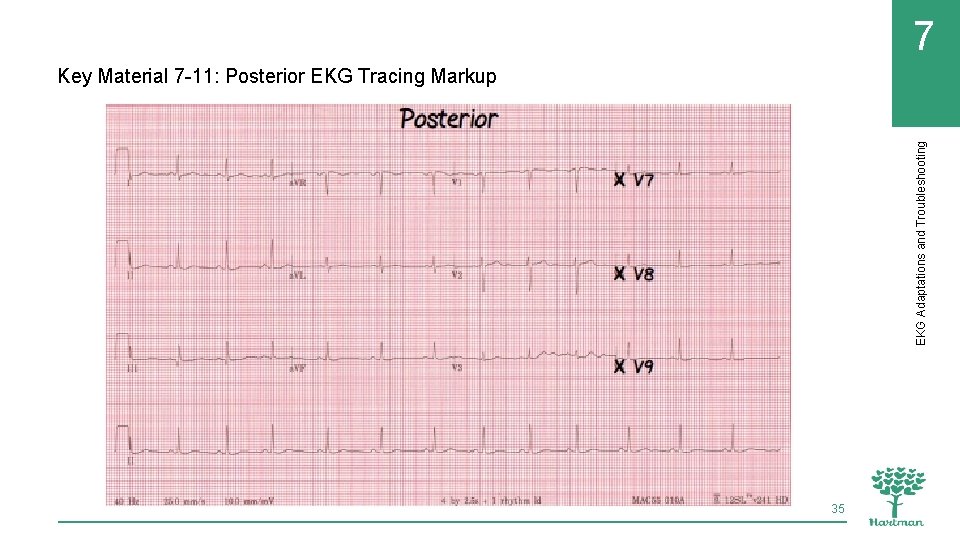
7 EKG Adaptations and Troubleshooting Key Material 7 -11: Posterior EKG Tracing Markup 35
7 EKG Adaptations and Troubleshooting 3. Demonstrate adaptations to electrode placement and patient positioning in special situations and pediatric patients Patient health conditions or circumstances might require changes to positioning: • Respiratory or heart problems might make it difficult for patients to tolerate supine position. Semi-Folwer’s position will likely be more comfortable for these patients. • Patients who are six months or more pregnant should not be placed in the supine position. Pillows can be used to tilt these patients to the left, taking pressure off the vena cava. 36
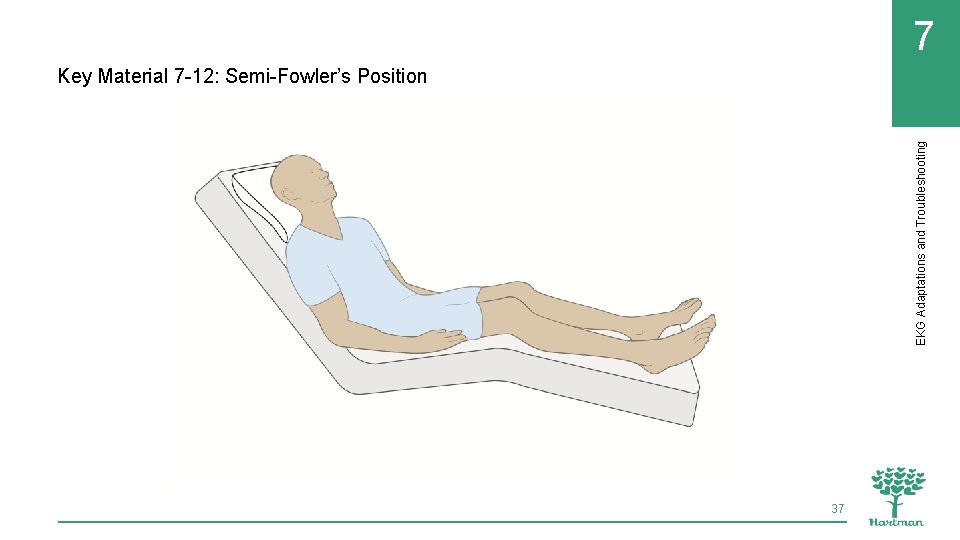
7 EKG Adaptations and Troubleshooting Key Material 7 -12: Semi-Fowler’s Position 37
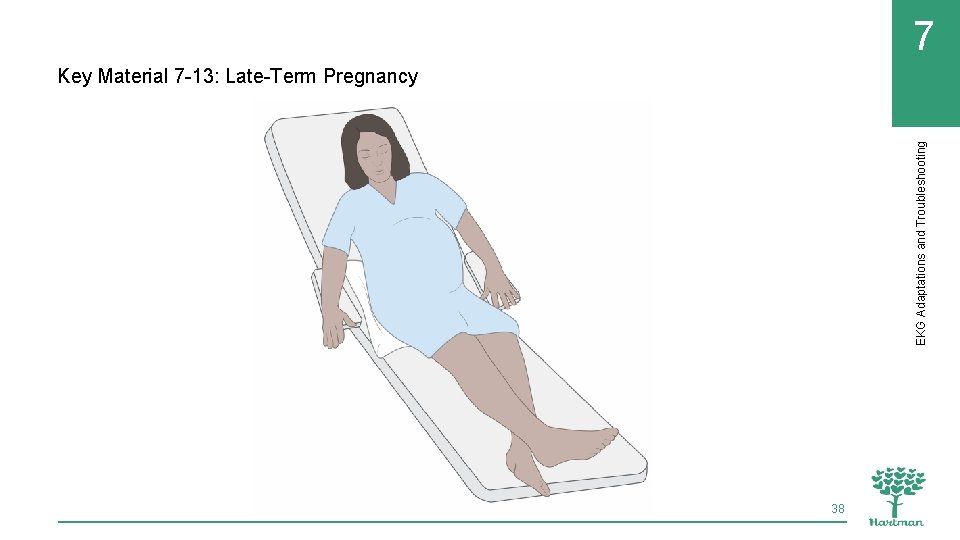
7 EKG Adaptations and Troubleshooting Key Material 7 -13: Late-Term Pregnancy 38
7 REMEMBER: EKG machines should always be operated according to manufacturer’s instructions and facility policy. 39 EKG Adaptations and Troubleshooting 4. Identify sources of information for EKG machine troubleshooting and maintenance
7 4. Identify sources of information for EKG machine troubleshooting and maintenance EKG Adaptations and Troubleshooting Remember these basic troubleshooting steps to follow if an EKG machine is not functioning properly: • Check the battery/power supply • Check the paper supply • Make sure supplies have not expired • Consult the basic troubleshooting information available in the manual 40
7 4. Identify sources of information for EKG machine troubleshooting and maintenance EKG Adaptations and Troubleshooting If the measures listed on the previous slide do not solve the problem, take these steps: • Follow facility policy for reporting the machine’s malfunction • Acquire a backup machine if one is available • If a backup is not available, notify the person responsible for scheduling so appointments can be rescheduled 41
7 4. Identify sources of information for EKG machine troubleshooting and maintenance EKG Adaptations and Troubleshooting REMEMBER: EKG machines should only be serviced and repaired by manufacturer-approved companies. 42
7 Chapter Review EKG Adaptations and Troubleshooting 1. What is artifact and what can cause artifact? 2. List three situations in which the condition of the patient’s skin can interfere with electrode contact. 3. Why should the EKG technician avoid placing electrodes on surgical scars or open wounds? 4. Why should patients who are in the last trimester of pregnancy never be placed flat on their backs? Describe the proper position for these patients. 5. Why are precordial leads placed differently for a patient with dextrocardia? 43
7 Chapter Review EKG Adaptations and Troubleshooting 6. List two ways to reduce somatic tremor on the EKG. 7. What type of baseline interference is caused by electrodes that have dried out? 8. Where would you find basic troubleshooting information for the EKG machine? 9. What should the EKG technician do if he has attempted the suggested troubleshooting actions and the EKG machine will not work? 44
7 Chapter Review EKG Adaptations and Troubleshooting Critical Thinking: Quick Case Studies How would you handle these situations? A patient arrives for an EKG appointment visibly anxious and upset. Her hands are trembling and her breathing uneven. She says she has just received bad news about a family member’s health. She does not wish to reschedule her appointment. A patient with a cast from his left foot up to the middle of his left thigh needs an EKG. A preschool child is scheduled for an EKG but insists on staying curled into a ball on his mother’s lap. Any attempt to get him to move or let go results in screaming and crying. 45
7 Critical Thinking: Quick Case Studies (cont’d) A 7 -year-old girl is scheduled for an EKG but is extremely scared and does not want to lie down. Her father suggests that she might be distracted enough to get the test done if she is allowed to play a game on his mobile phone during the EKG. An EKG technician sees what she thinks might be MRSA skin lesions on a patient’s body. There is nothing noted in the patient’s record about MRSA. 46 EKG Adaptations and Troubleshooting Chapter Review

- Slides: 47