6 PLEURAL EFFUSIONS 1 Aims of this subject
6 PLEURAL EFFUSIONS 1
Aims of this subject: § § § Define pleural effusion & discuss causes. Transudate Vs Exudate for diagnosis. Discuss the Important clinical clues that help in diagnosis. Investigations. Management.
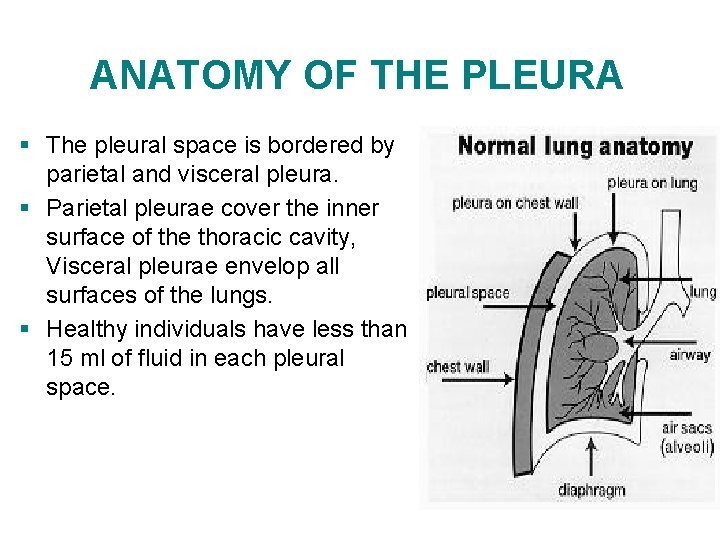
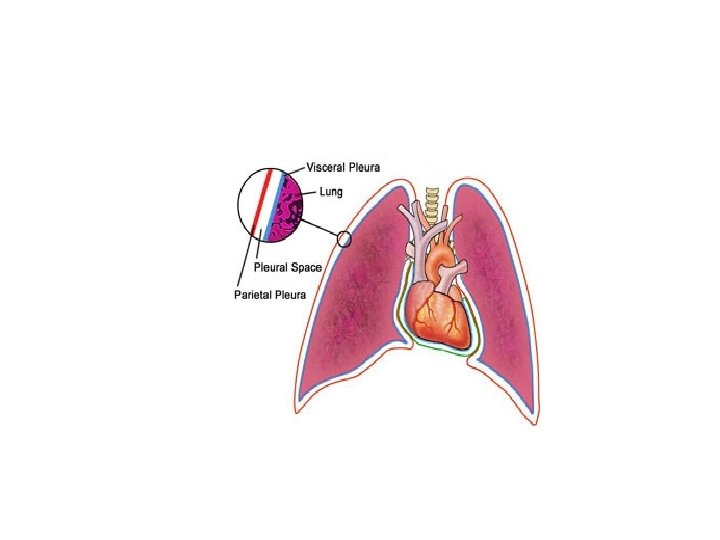
ANATOMY OF THE PLEURA § The pleural space is bordered by parietal and visceral pleura. § Parietal pleurae cover the inner surface of the thoracic cavity, Visceral pleurae envelop all surfaces of the lungs. § Healthy individuals have less than 15 ml of fluid in each pleural space.
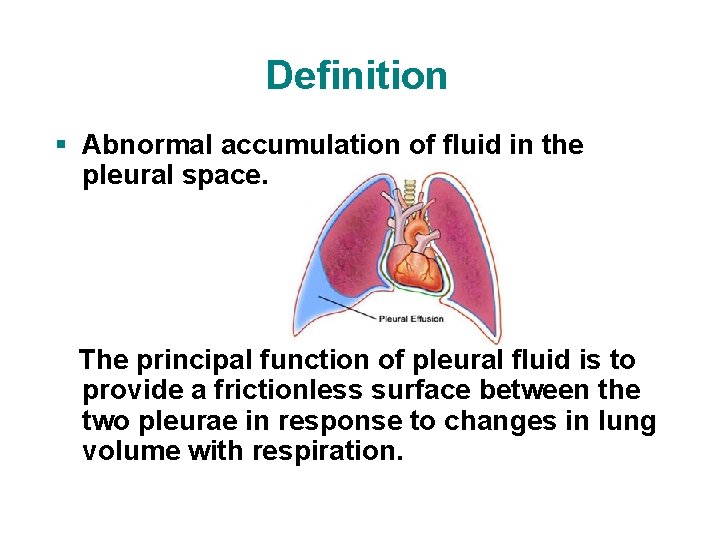
Definition § Abnormal accumulation of fluid in the pleural space. The principal function of pleural fluid is to provide a frictionless surface between the two pleurae in response to changes in lung volume with respiration.
Pathophysiology § Normally, fluid enters the pleural space from the : - Capillaries via parietal pleura. - Interstitial spaces of lung via visceral pleura. - Peritoneal cavity via holes in diaphragm • This fluid is normally removed by lymphatics in the visceral pleura, which have the capacity to absorb 20 times more fluid than is normally formed.
Mechanisms § Altered permeability (e. g. inflammation) § Reduction in intravascular oncotic pressure (e. g. hypoalbuminemia) § Increased capillary hydrostatic pressure (e. g. congestive heart failure) § Reduction of pressure in pleural space; lung unable to expand (e. g. extensive atelectasis) § Decreased lymphatic drainage.
Mechanisms (2) § Increased fluid in peritoneal cavity, with migration across the diaphragm via the lymphatics (e. g. hepatic cirrhosis, peritoneal dialysis) § Movement of fluid from pulmonary edema across the visceral pleura. § Iatrogenic causes (e. g. central line misplacement)
History usually with 1. Progressive dyspnea: Ø Most common presentation. Ø Indicates large effusion (usually not <500 ml). 2. Chest pain: Ø Sharp or stabbing, with deep inspiration. Ø Pain may be localized to the chest wall or referred to the ipsilateral shoulder or upper abdomen possible malignant mesothelioma Ø intensity as the pleural effusion in size.
History (2) Ø Pain is more suggestive of exudative effusion Chest pain signifies pleural irritation, which can aid in the diagnosis of the cause of the effusion, since most transudative effusions do not cause direct pleural irritation. 3. Non-productive cough Cough is usually related to the associated atelectasis, which to some degree accompanies all pleural effusions.
Physical Examination 1. Inspection: Ø Asymmetric expansion of thoracic cage, with lagging expansion on the affected side (i. e. , Hoover sign). Ø May be bulging on affected side.
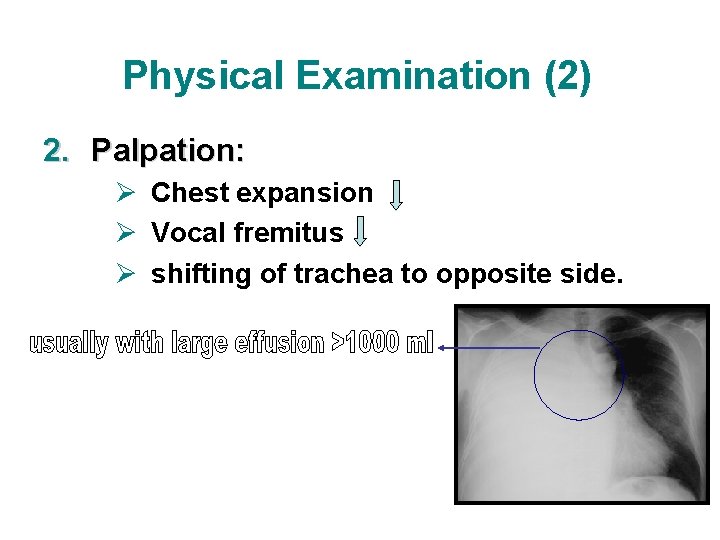
Physical Examination (2) 2. Palpation: Ø Chest expansion Ø Vocal fremitus Ø shifting of trachea to opposite side.
Physical Examination (3) 3. Percussion: Ø stony dullness Ø decreased tactile fremitus 4. Auscultation: Ø or absent breath sounds Ø vocal resonance Ø bronchial breathing & egophony above the fluid level Ø pleural friction rub
Thoracentesis and Pleural Fluid Analysis Ø To establish the etiology, a thoracentesis usually needs to be performed: 50 to 100 ml of fluid are usually removed and sent for analysis. Ø Not every effusion needs to be tapped, but when the patient has no obvious clinical cause for the effusion, is febrile, or has dyspnea, fluid should be removed. Ø The first step is to determine if the fluid is a transudate or an exudate
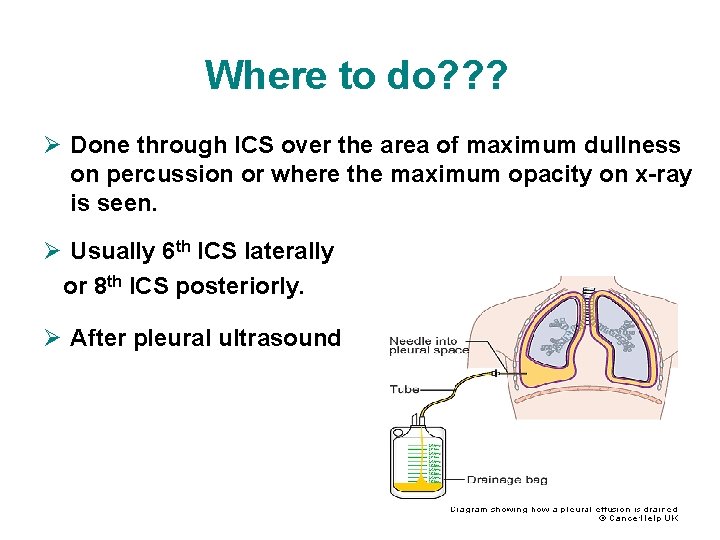
Where to do? ? ? Ø Done through ICS over the area of maximum dullness on percussion or where the maximum opacity on x-ray is seen. Ø Usually 6 th ICS laterally or 8 th ICS posteriorly. Ø After pleural ultrasound
Types • Hydrothorax • Hemothorax • Chylothorax • Pyothorax or Empyema
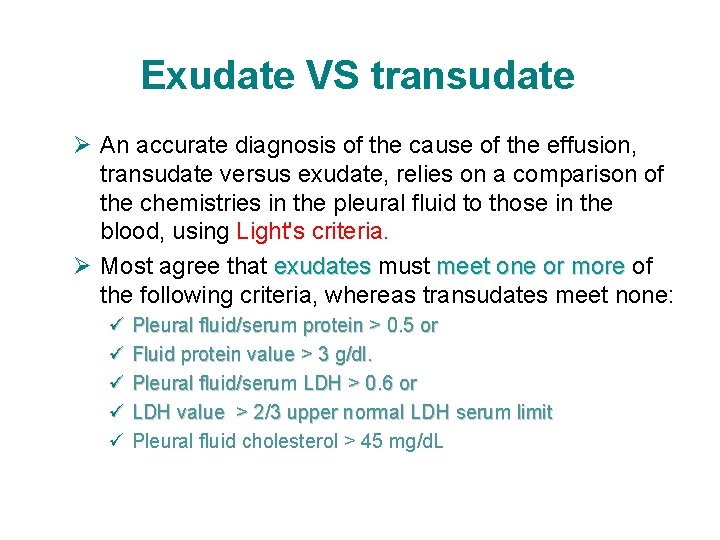
Exudate VS transudate Ø An accurate diagnosis of the cause of the effusion, transudate versus exudate, relies on a comparison of the chemistries in the pleural fluid to those in the blood, using Light's criteria. Ø Most agree that exudates must meet one or more of the following criteria, whereas transudates meet none: ü Pleural fluid/serum protein > 0. 5 or ü Fluid protein value > 3 g/dl. ü Pleural fluid/serum LDH > 0. 6 or ü LDH value > 2/3 upper normal LDH serum limit ü Pleural fluid cholesterol > 45 mg/d. L
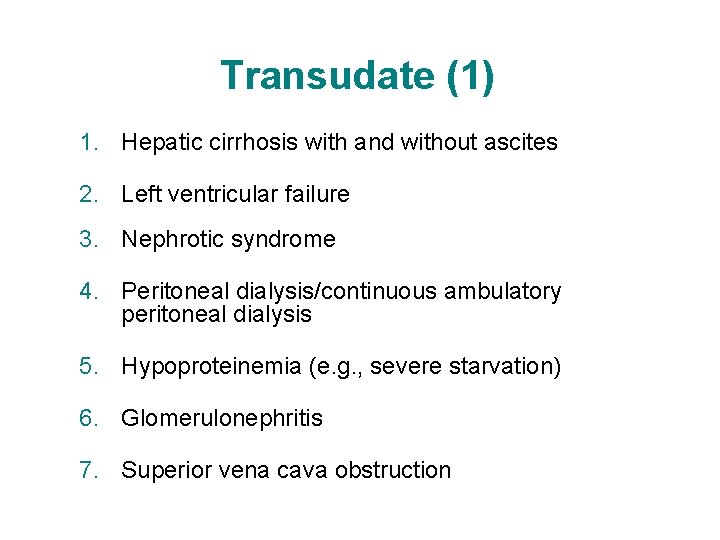
Transudate (1) 1. Hepatic cirrhosis with and without ascites 2. Left ventricular failure 3. Nephrotic syndrome 4. Peritoneal dialysis/continuous ambulatory peritoneal dialysis 5. Hypoproteinemia (e. g. , severe starvation) 6. Glomerulonephritis 7. Superior vena cava obstruction
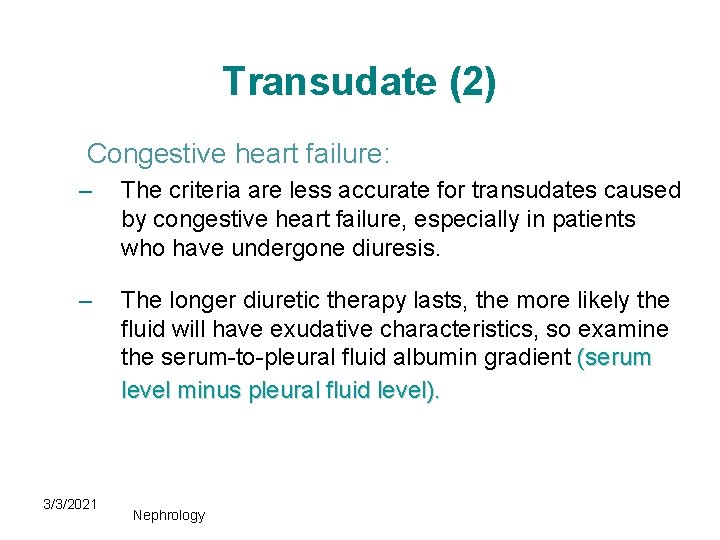
Transudate (2) Congestive heart failure: – The criteria are less accurate for transudates caused by congestive heart failure, especially in patients who have undergone diuresis. – The longer diuretic therapy lasts, the more likely the fluid will have exudative characteristics, so examine the serum-to-pleural fluid albumin gradient (serum level minus pleural fluid level). 3/3/2021 Nephrology
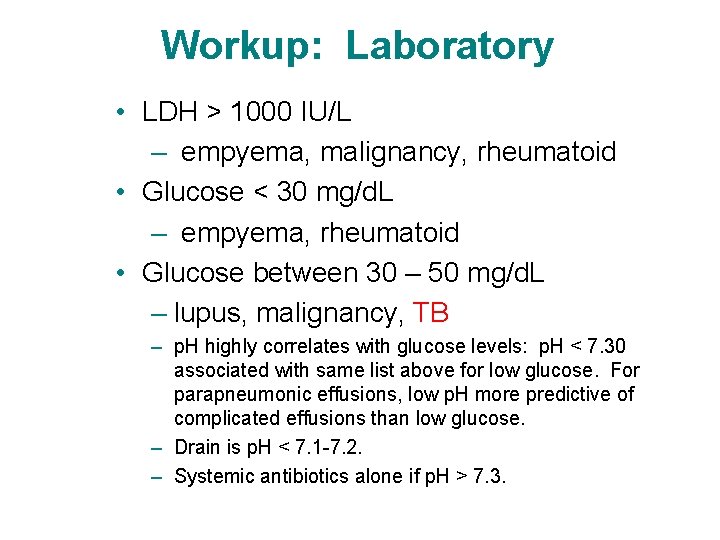
Workup: Laboratory • LDH > 1000 IU/L – empyema, malignancy, rheumatoid • Glucose < 30 mg/d. L – empyema, rheumatoid • Glucose between 30 – 50 mg/d. L – lupus, malignancy, TB – p. H highly correlates with glucose levels: p. H < 7. 30 associated with same list above for low glucose. For parapneumonic effusions, low p. H more predictive of complicated effusions than low glucose. – Drain is p. H < 7. 1 -7. 2. – Systemic antibiotics alone if p. H > 7. 3.
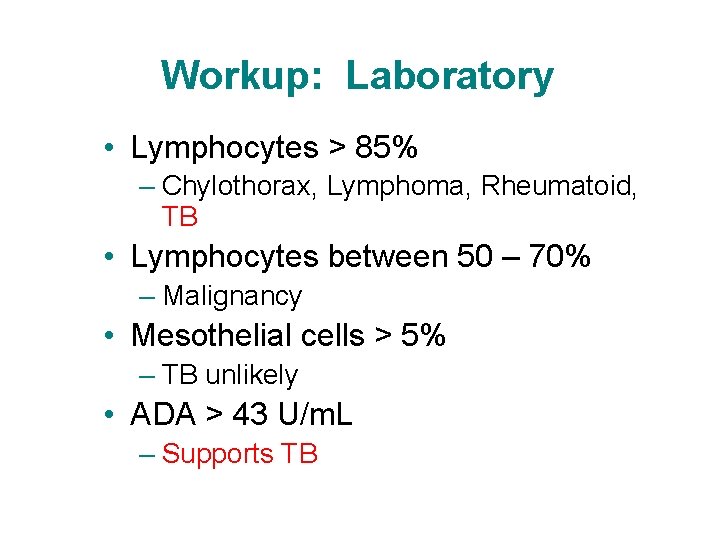
Workup: Laboratory • Lymphocytes > 85% – Chylothorax, Lymphoma, Rheumatoid, TB • Lymphocytes between 50 – 70% – Malignancy • Mesothelial cells > 5% – TB unlikely • ADA > 43 U/m. L – Supports TB
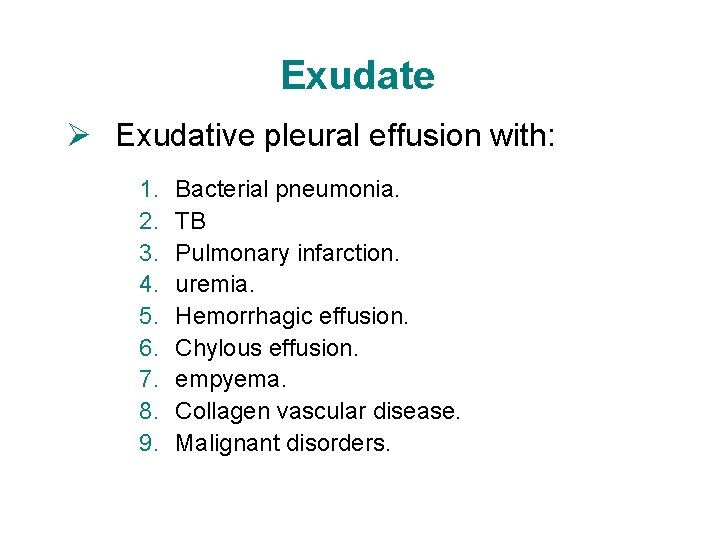
Exudate Ø Exudative pleural effusion with: 1. 2. 3. 4. 5. 6. 7. 8. 9. Bacterial pneumonia. TB Pulmonary infarction. uremia. Hemorrhagic effusion. Chylous effusion. empyema. Collagen vascular disease. Malignant disorders.

Exudate (2) Ø Conditions causing pleural fluid with exudative or transudative characteristics: 1. Pulmonary embolism. 2. Hypothyroidism. 3. Pericardial disease (inflammatory or constrictive) 4. Atelectasis. 5. Sarcoidosis (usually an exudate) 6. Amyloidosis
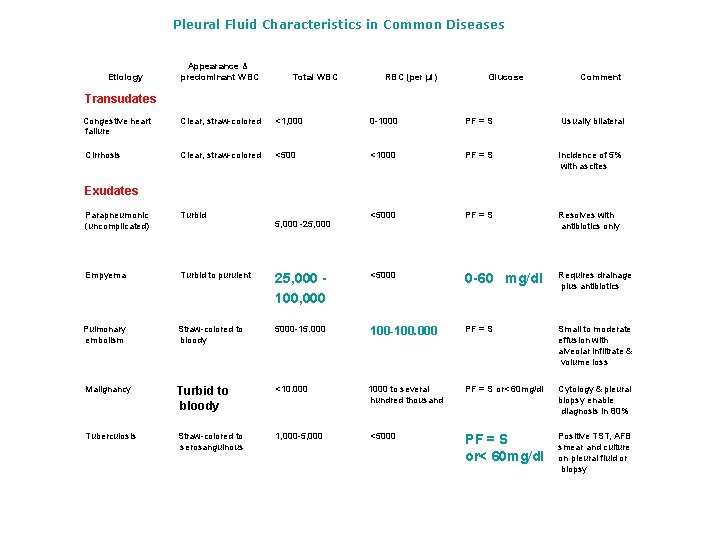
Pleural Fluid Characteristics in Common Diseases Etiology Appearance & predominant WBC Total WBC RBC (per µl) Glucose Comment Transudates Congestive heart failure Clear, straw-colored <1, 000 0 -1000 PF = S Usually bilateral Cirrhosis Clear, straw-colored <500 <1000 PF = S Incidence of 5% with ascites <5000 PF = S Resolves with antibiotics only Exudates Parapneumonic (uncomplicated) Turbid Empyema Turbid to purulent 25, 000 100, 000 <5000 0 -60 mg/dl Requires drainage plus antibiotics Pulmonary embolism Straw-colored to bloody 5000 -15. 000 100 -100. 000 PF = S Small to moderate effusion with alveolar infiltrate & volume loss Malignancy Turbid to bloody <10. 000 1000 to several hundred thousand PF = S or< 60 mg/dl Cytology & pleural biopsy enable diagnosis in 80% Tuberculosis Straw-colored to serosanguinous 1, 000 -5, 000 <5000 PF = S or< 60 mg/dl Positive TST, AFB smear and culture on pleural fluid or biopsy 5, 000 -25, 000
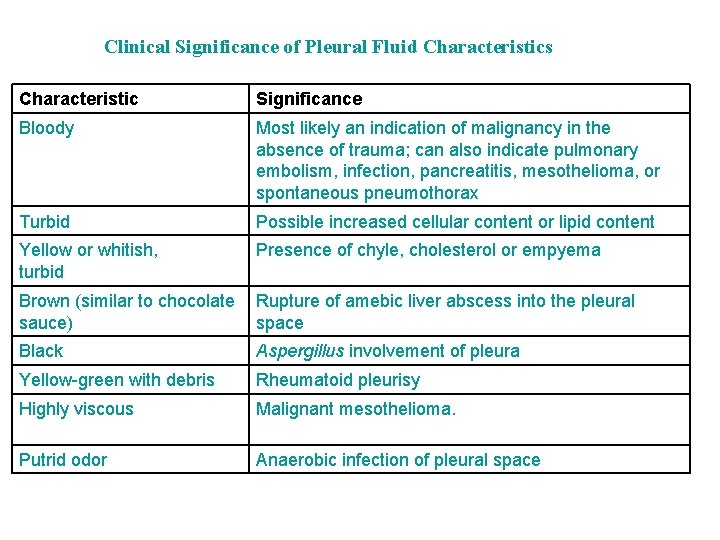
Clinical Significance of Pleural Fluid Characteristics Characteristic Significance Bloody Most likely an indication of malignancy in the absence of trauma; can also indicate pulmonary embolism, infection, pancreatitis, mesothelioma, or spontaneous pneumothorax Turbid Possible increased cellular content or lipid content Yellow or whitish, turbid Presence of chyle, cholesterol or empyema Brown (similar to chocolate sauce) Rupture of amebic liver abscess into the pleural space Black Aspergillus involvement of pleura Yellow-green with debris Rheumatoid pleurisy Highly viscous Malignant mesothelioma. Putrid odor Anaerobic infection of pleural space
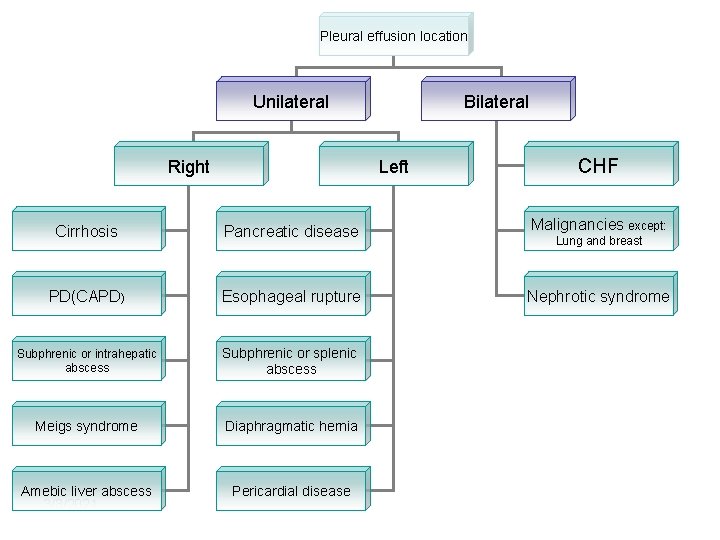
Pleural effusion location Unilateral Right Bilateral Left CHF Cirrhosis Pancreatic disease Malignancies except: PD(CAPD) Esophageal rupture Nephrotic syndrome Subphrenic or intrahepatic abscess Subphrenic or splenic abscess Meigs syndrome Diaphragmatic hernia Amebic liver abscess 3/3/2021 Pericardial disease Lung and breast
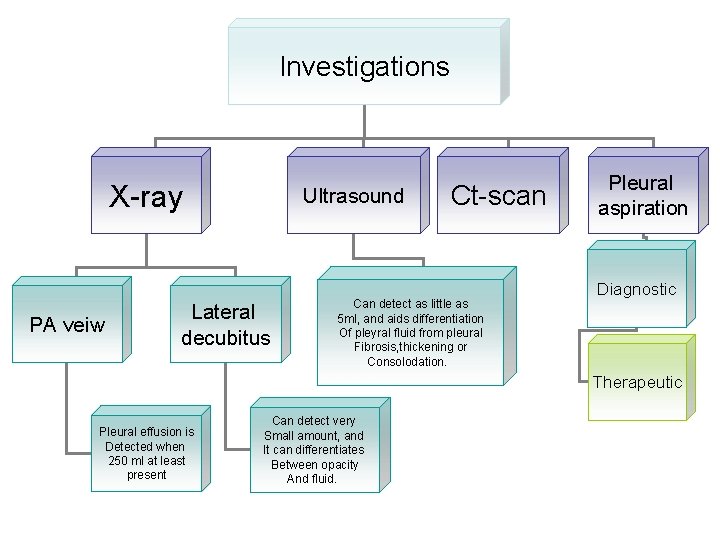
Investigations X-ray PA veiw Ultrasound Lateral decubitus Ct-scan Can detect as little as 5 ml, and aids differentiation Of pleyral fluid from pleural Fibrosis, thickening or Consolodation. Pleural aspiration Diagnostic Therapeutic Pleural effusion is Detected when 250 ml at least present Can detect very Small amount, and It can differentiates Between opacity And fluid.
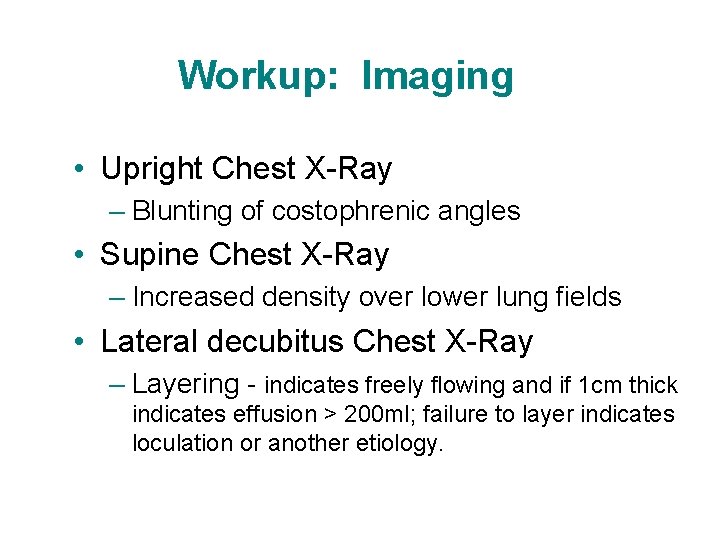
Workup: Imaging • Upright Chest X-Ray – Blunting of costophrenic angles • Supine Chest X-Ray – Increased density over lower lung fields • Lateral decubitus Chest X-Ray – Layering - indicates freely flowing and if 1 cm thick indicates effusion > 200 ml; failure to layer indicates loculation or another etiology.
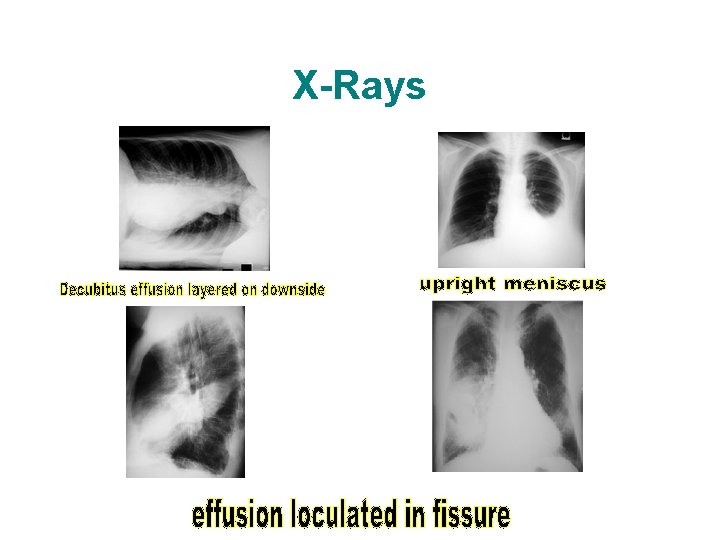
X-Rays
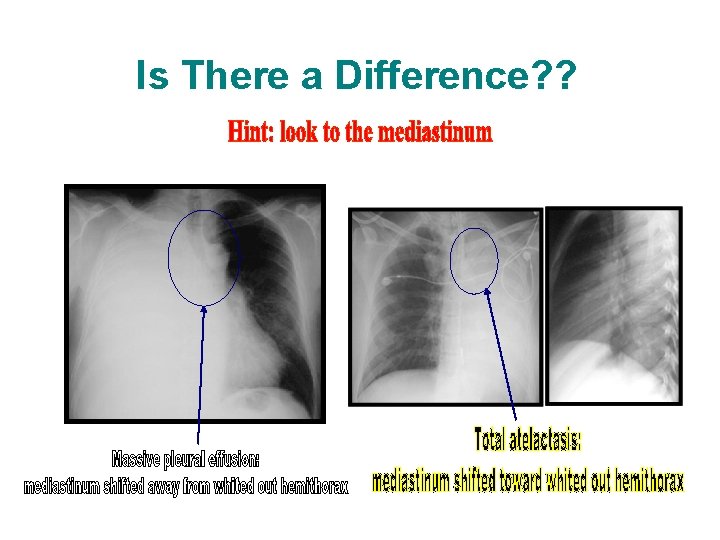
Is There a Difference? ?

Workup: Imaging • Pleural ultrasound – Helps in: v identification of loculated effusions v differentiation of fluid from fibrosis v identification of thoracentesis site – Available at bedside
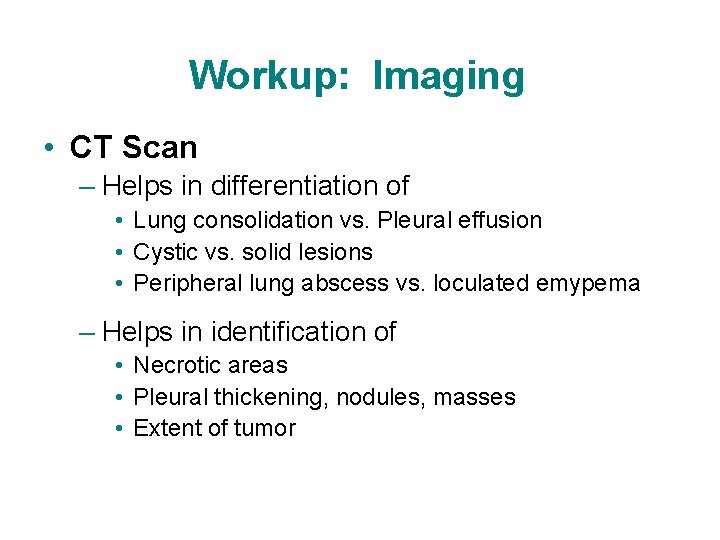
Workup: Imaging • CT Scan – Helps in differentiation of • Lung consolidation vs. Pleural effusion • Cystic vs. solid lesions • Peripheral lung abscess vs. loculated emypema – Helps in identification of • Necrotic areas • Pleural thickening, nodules, masses • Extent of tumor
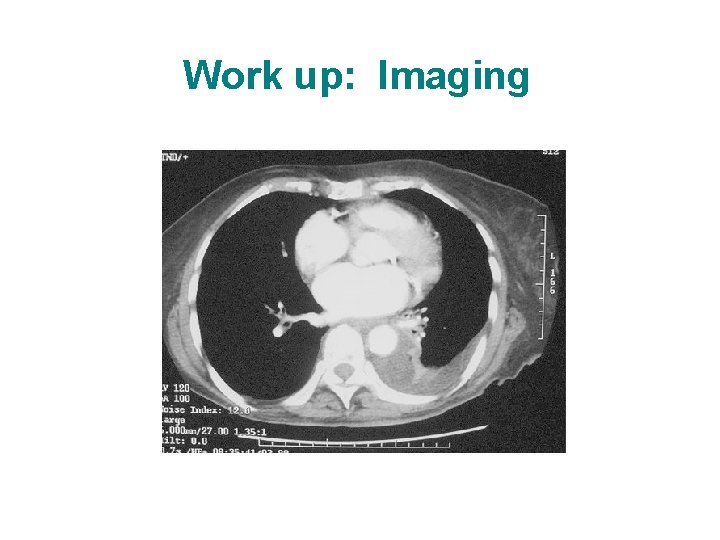
Work up: Imaging
Pleural histology • Proves the etiology of the pleural effusion • A pleural fragment can be obtained by: v needle pleural biopsy v thoracoscopy v thoracotomy 34
Management Ø It is usually directed to the treatment of the underlying cause. Ø Bed rest. Ø Therapeutics aspiration to relieve breathlessness, The recommended limit is about 1, 000 ml at a single thoracentesis but removal of smaller volumes of 400 -500 ml usually alleviates severe symptoms. Aspiration of larger amount may cause pulmonary edema.
Management (2) In cases of recurrent effusion such as in lung cancer, pleurodesis with tetracycline, bleomycin or talc can sclerose the pleural space and effectively prevent recurrence of the malignant pleural effusion.
Take a Message Large pleural effusions, whether transudates or exudates, should be drained if they are causing severe respiratory symptoms, regardless of whether the cause is understood and disease-specific treatment is available. Relief of symptoms in these patients is the goal of drainage therapy.
- Slides: 37