6 1 Functions of the Skeletal System Components
- Slides: 31
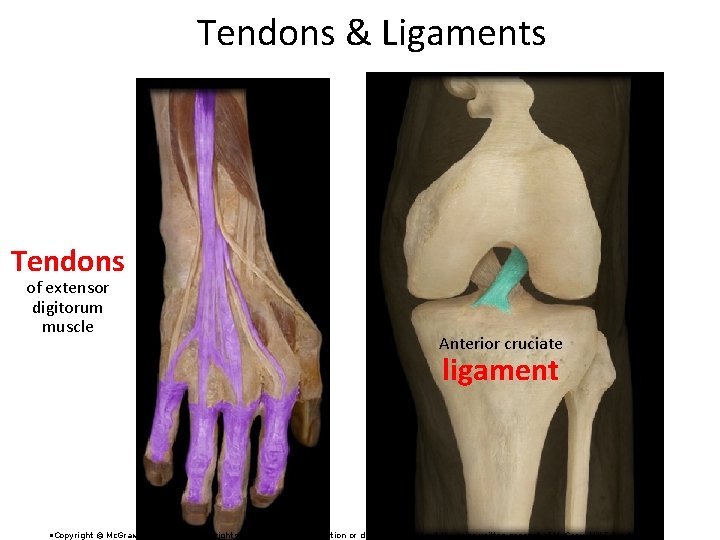
6. 1 Functions of the Skeletal System • Components of Skeletal System: – Bone – Cartilage: three types • Hyaline • Fibrocartilage • Elastic – Tendons and ligaments 6 -1
Three Types of Cartilage –Cartilage: three types • Hyaline • Fibrocartilage • Elastic Which one is more closely associated with bone? 6 -2
Three Types of Cartilage –Cartilage: three types • Hyaline • Fibrocartilage • Elastic Is more closely associated with bone. 6 -3
6. 1 Functions of the Skeletal System (2) 1. 2. 3. 4. Support. Protection. Movement. Storage. Calcium and Phosphorus. Stored then released as needed. Adipose tissue stored in marrow cavities 5. Blood cell production. Bone marrow that gives rise to blood cells and platelets 6 -4
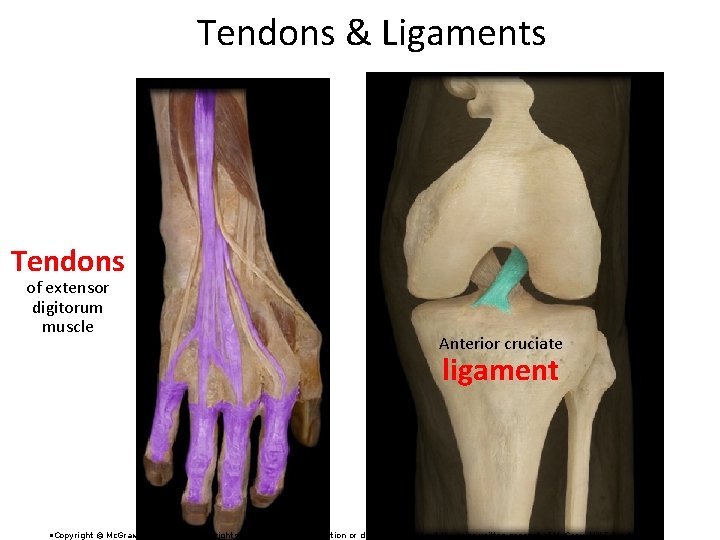
Tendons & Ligaments Tendons of extensor digitorum muscle Anterior cruciate ligament • Copyright © Mc. Graw-Hill Education. All rights reserved. No reproduction or distribution without the prior written consent of Mc. Graw-Hill Education.
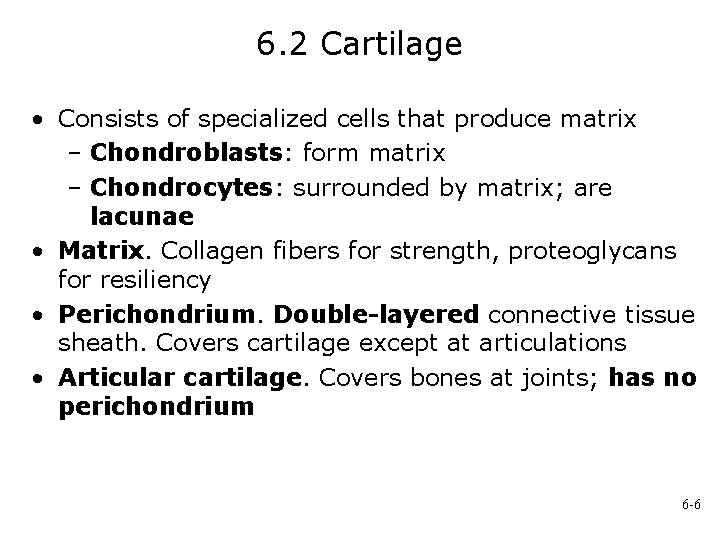
6. 2 Cartilage • Consists of specialized cells that produce matrix – Chondroblasts: form matrix – Chondrocytes: surrounded by matrix; are lacunae • Matrix. Collagen fibers for strength, proteoglycans for resiliency • Perichondrium. Double-layered connective tissue sheath. Covers cartilage except at articulations • Articular cartilage. Covers bones at joints; has no perichondrium 6 -6
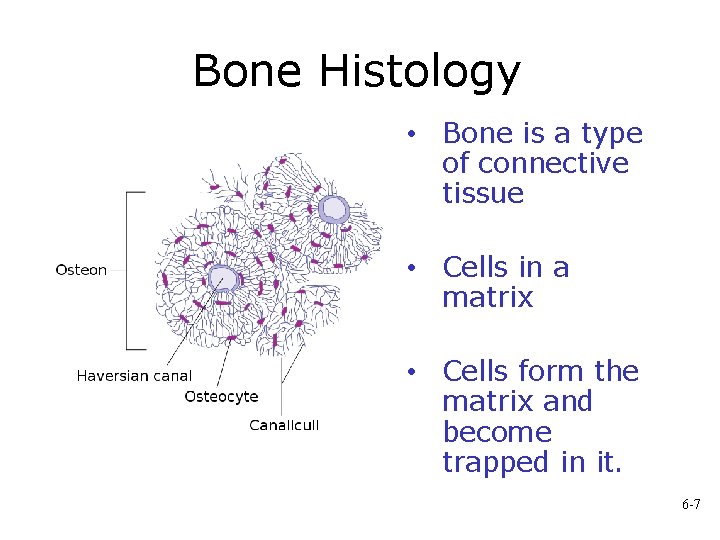
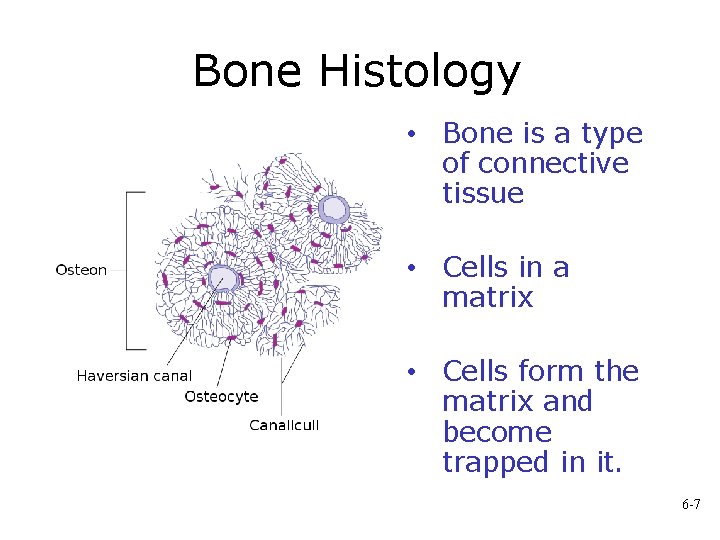
Bone Histology • Bone is a type of connective tissue • Cells in a matrix • Cells form the matrix and become trapped in it. 6 -7
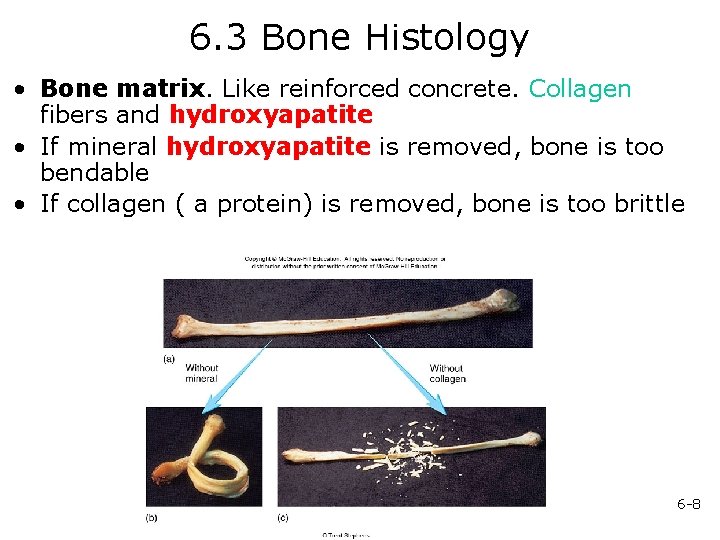
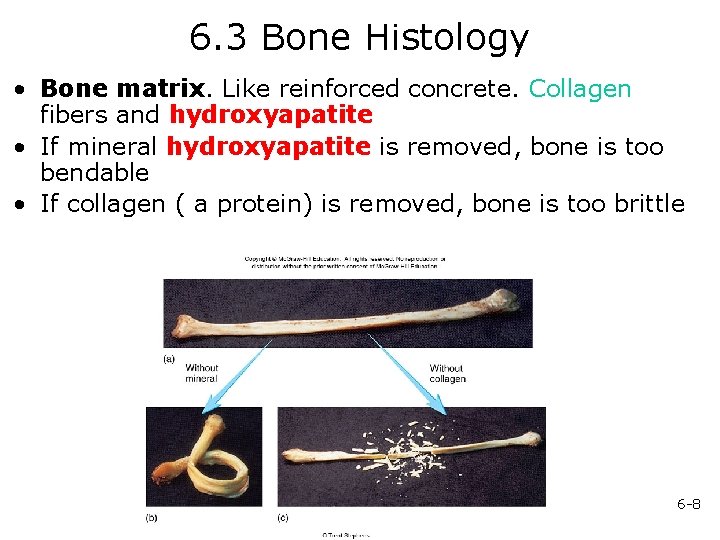
6. 3 Bone Histology • Bone matrix. Like reinforced concrete. Collagen fibers and hydroxyapatite • If mineral hydroxyapatite is removed, bone is too bendable • If collagen ( a protein) is removed, bone is too brittle 6 -8
Hydroxyapatite Calcium and Phosphorus Forms a crystal Bone matrix is like reinforced concrete The collagen lends some flexibility Hydroxyapatite makes it strong 6 -9
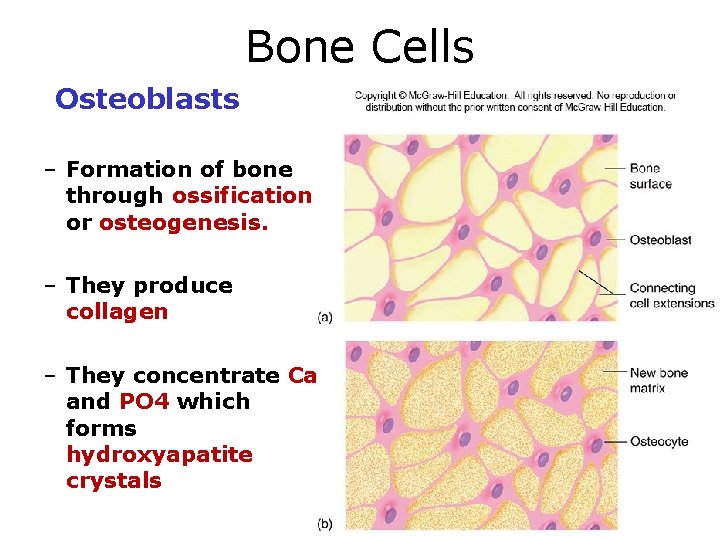
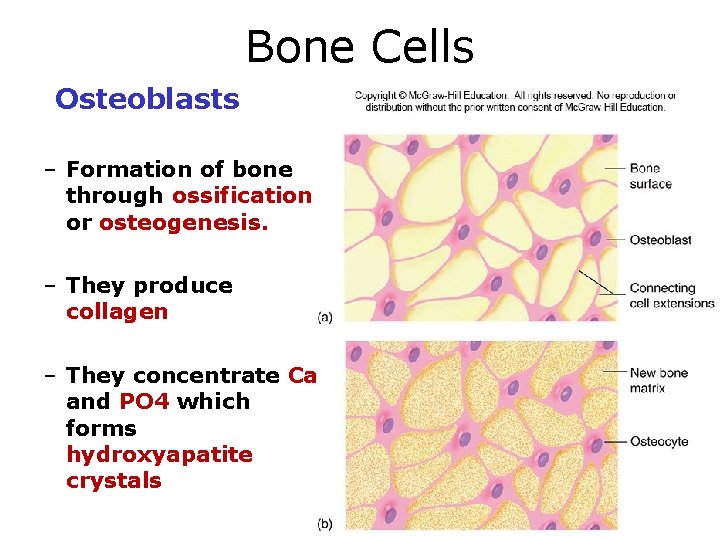
Bone Cells Osteoblasts – Formation of bone through ossification or osteogenesis. – They produce collagen – They concentrate Ca and PO 4 which forms hydroxyapatite crystals 6 -10
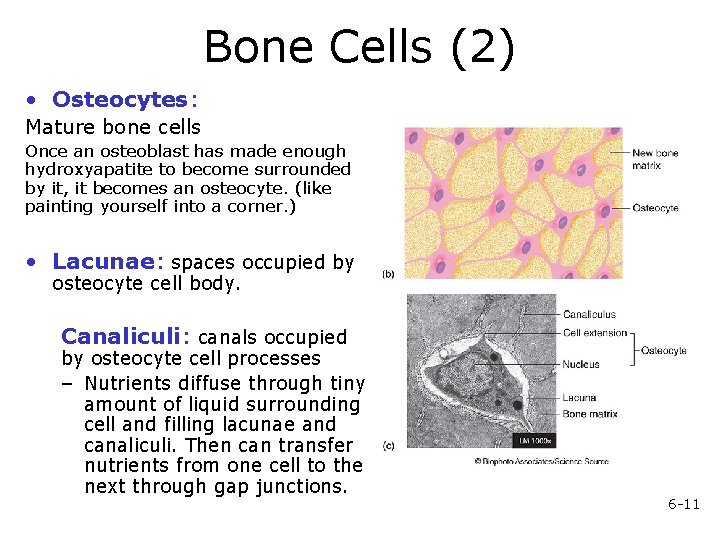
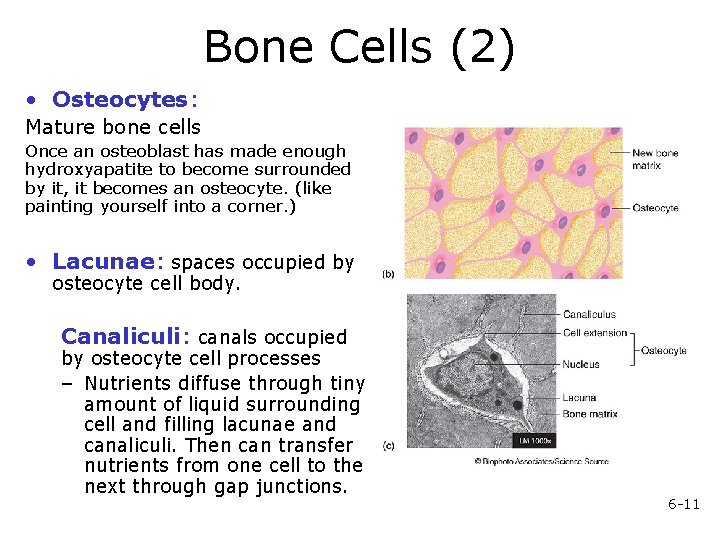
Bone Cells (2) • Osteocytes: Mature bone cells Once an osteoblast has made enough hydroxyapatite to become surrounded by it, it becomes an osteocyte. (like painting yourself into a corner. ) • Lacunae: spaces occupied by osteocyte cell body. Canaliculi: canals occupied by osteocyte cell processes – Nutrients diffuse through tiny amount of liquid surrounding cell and filling lacunae and canaliculi. Then can transfer nutrients from one cell to the next through gap junctions. 6 -11
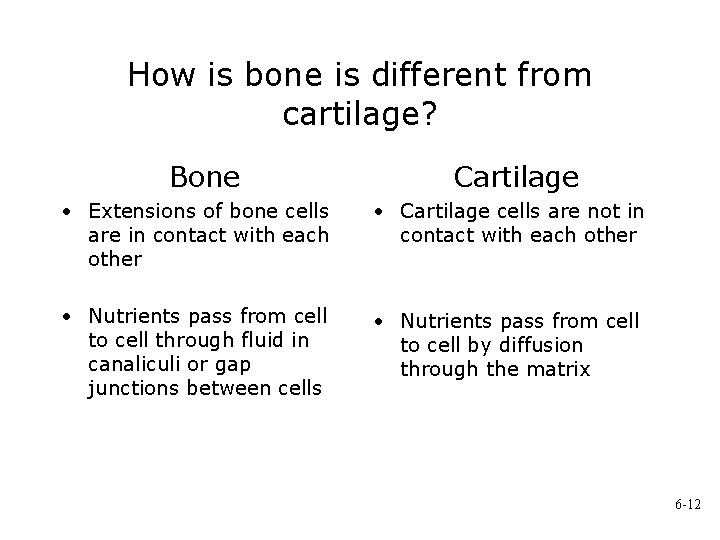
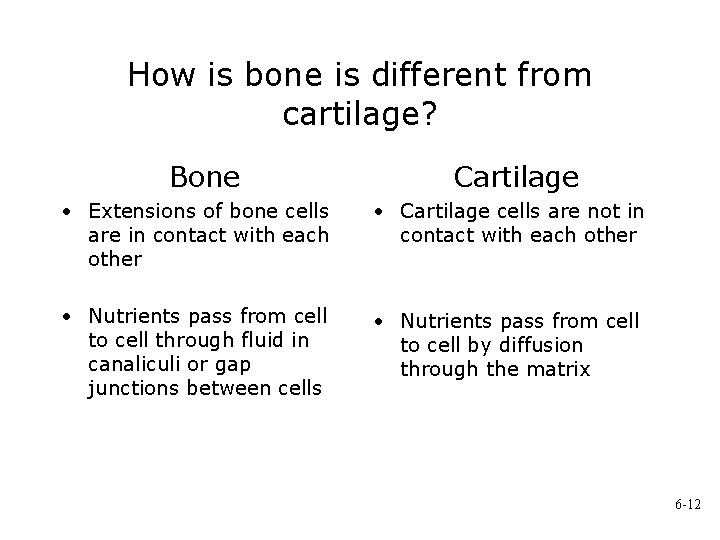
How is bone is different from cartilage? Bone Cartilage • Extensions of bone cells are in contact with each other • Cartilage cells are not in contact with each other • Nutrients pass from cell to cell through fluid in canaliculi or gap junctions between cells • Nutrients pass from cell to cell by diffusion through the matrix 6 -12
Bone Cells (3) • Osteoclasts. Resorption of bone – Ruffled border: where cell membrane borders bone and resorption is taking place. – H ions pumped across membrane, acid forms, eats away bone. – Release enzymes that digest the bone. – Derived from monocytes (which are formed from stem cells in red bone marrow) – Multinucleated and probably arise from fusion of a number of cells 6 -13
Origin of Bone Cells In Embryo • Connective tissue derives from mesenchymal cells • Some of these cells become stem cells. • Osteochondral progenitor cells are stem cells that become chondroblasts or osteoblasts. 6 -14
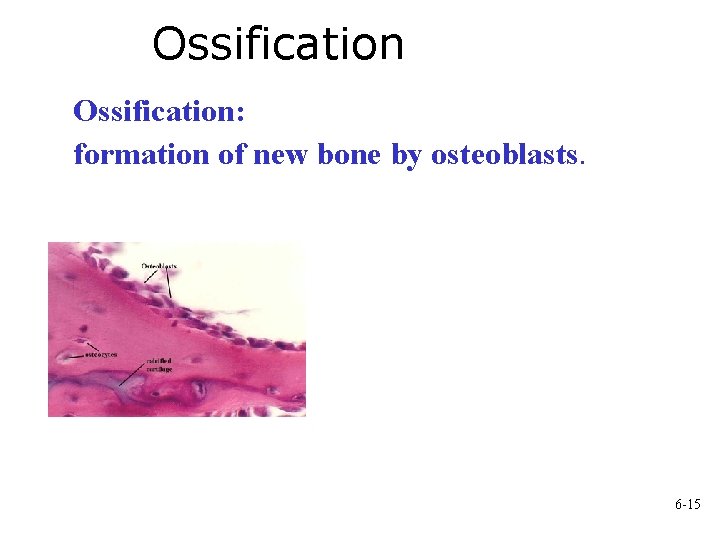
Ossification: formation of new bone by osteoblasts. 6 -15
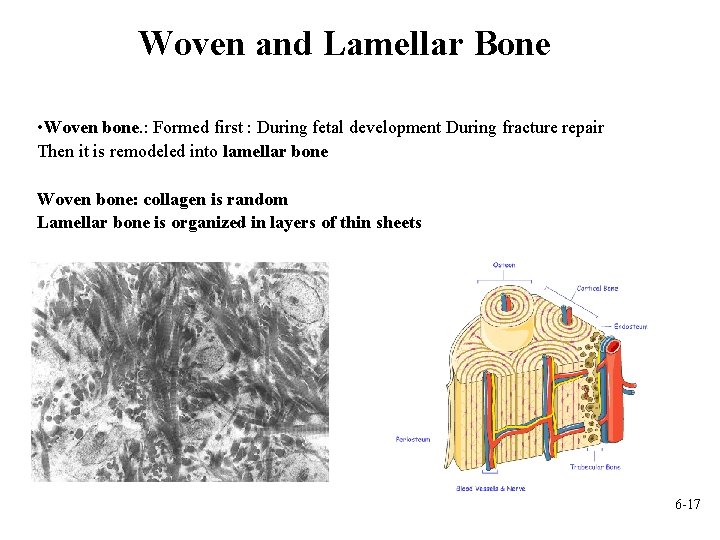
Ossification and Remodelling • Bone formation (ossification) proceeds in stages. • Ossification occurs at certain times: 1. As a fetus 2. As a growing child 3. When someone breaks a bone • Bone remodeling – replacing old bone with new bone continues throughout a lifetime. • Bone is classified as either woven or lamellar according to the organization of collagen fibers in the bone matrix. 6 -16
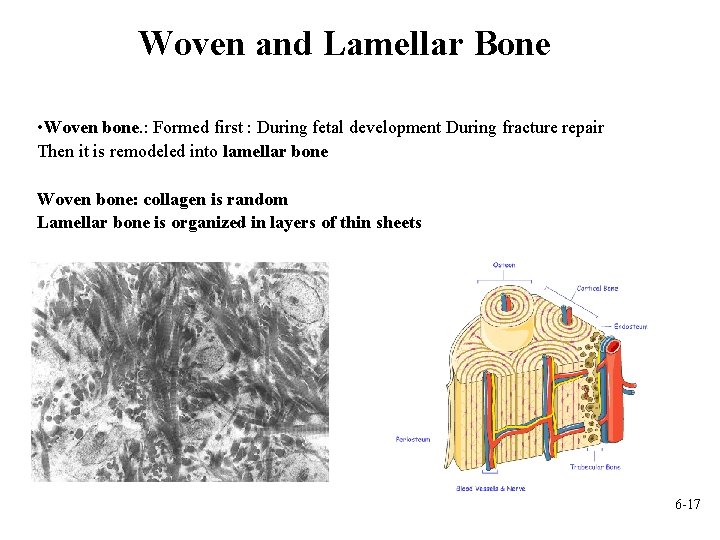
Woven and Lamellar Bone • Woven bone. : Formed first : During fetal development During fracture repair Then it is remodeled into lamellar bone Woven bone: collagen is random Lamellar bone is organized in layers of thin sheets 6 -17
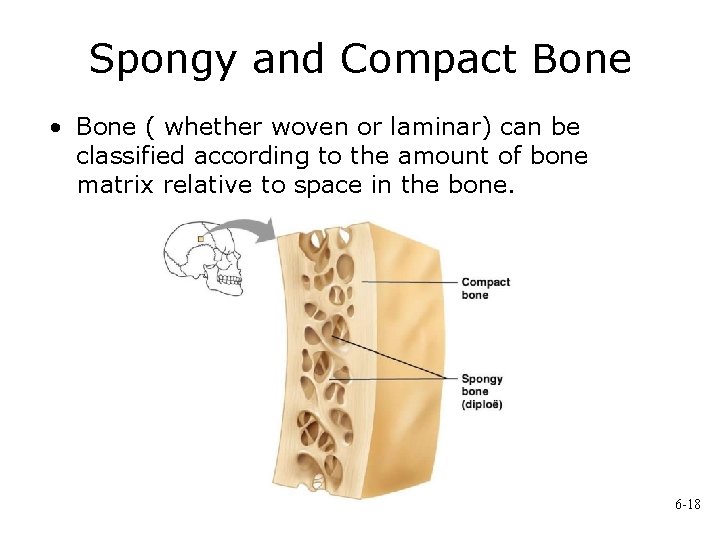
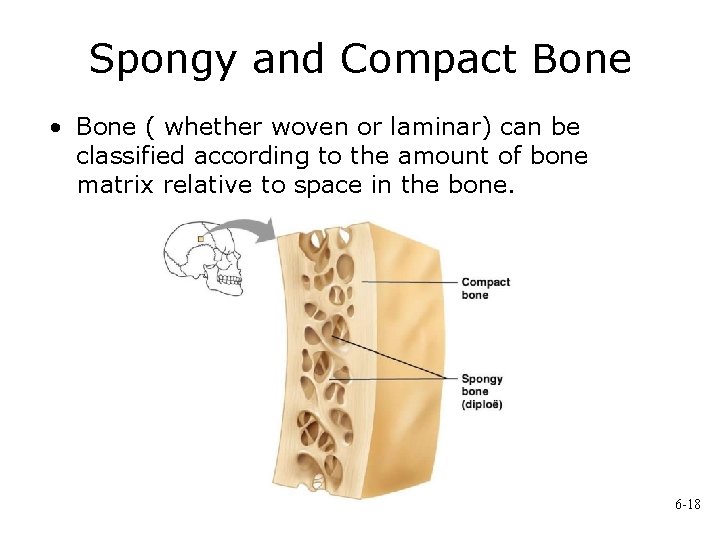
Spongy and Compact Bone • Bone ( whether woven or laminar) can be classified according to the amount of bone matrix relative to space in the bone. 6 -18
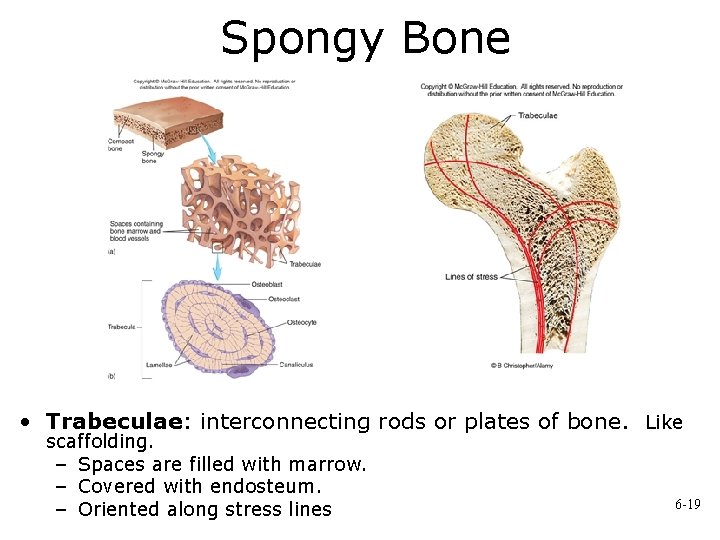
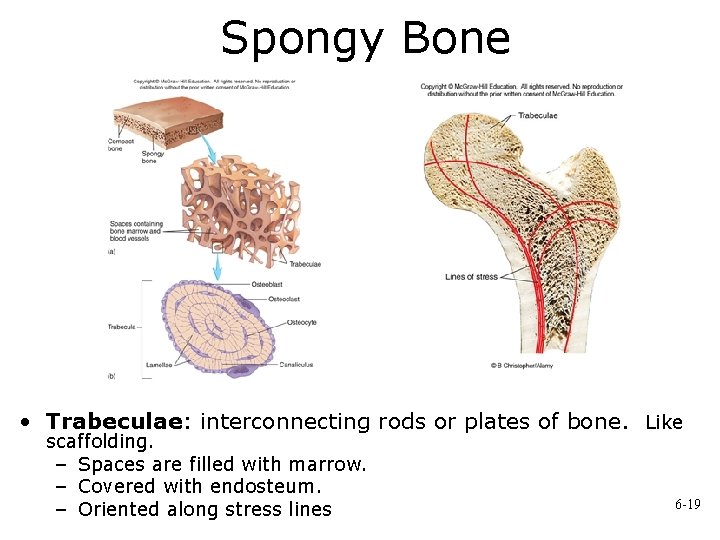
Spongy Bone • Trabeculae: interconnecting rods or plates of bone. Like scaffolding. – Spaces are filled with marrow. – Covered with endosteum. – Oriented along stress lines 6 -19
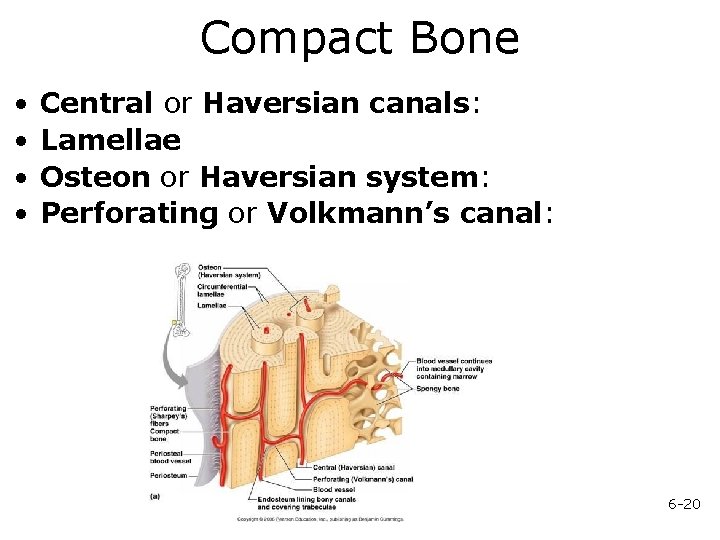
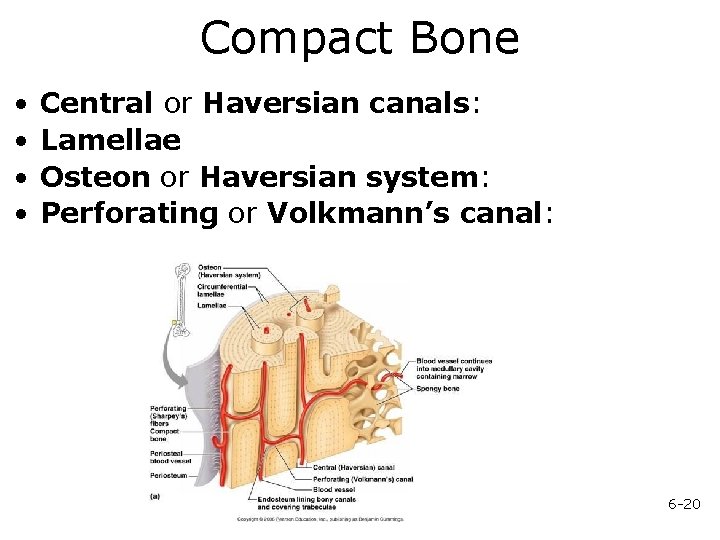
Compact Bone • • Central or Haversian canals: Lamellae Osteon or Haversian system: Perforating or Volkmann’s canal: 6 -20
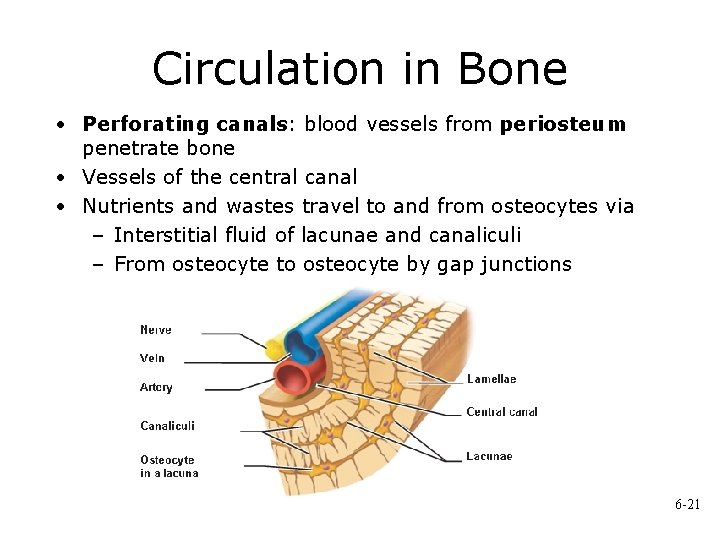
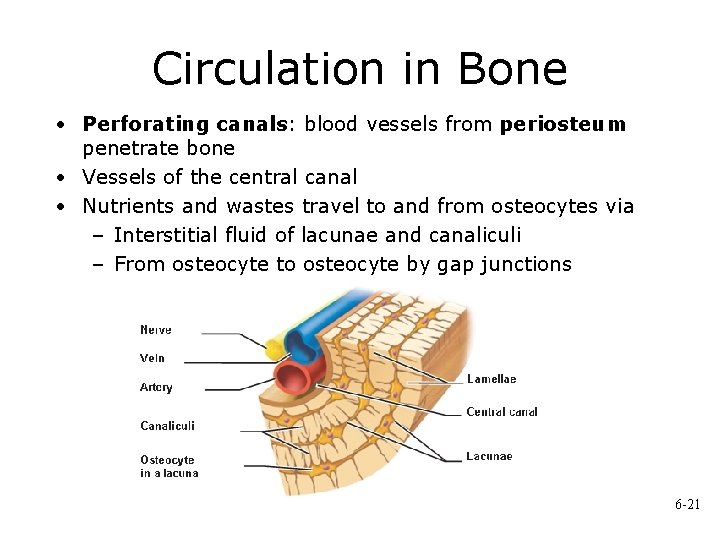
Circulation in Bone • Perforating canals: blood vessels from periosteum penetrate bone • Vessels of the central canal • Nutrients and wastes travel to and from osteocytes via – Interstitial fluid of lacunae and canaliculi – From osteocyte to osteocyte by gap junctions 6 -21
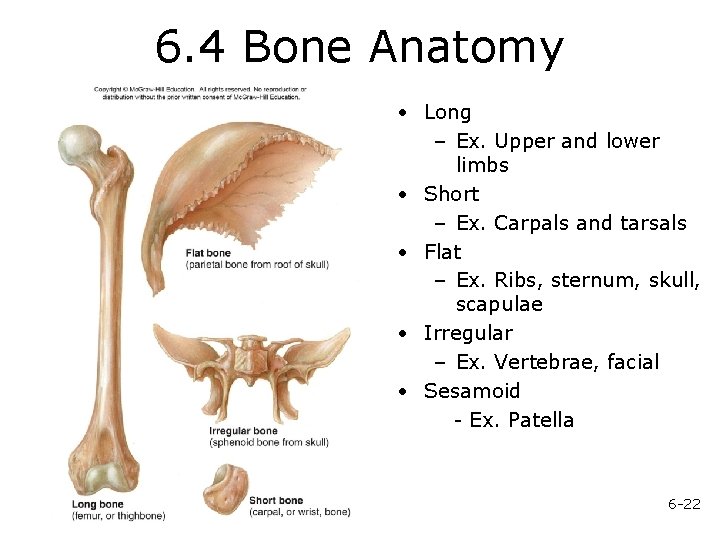
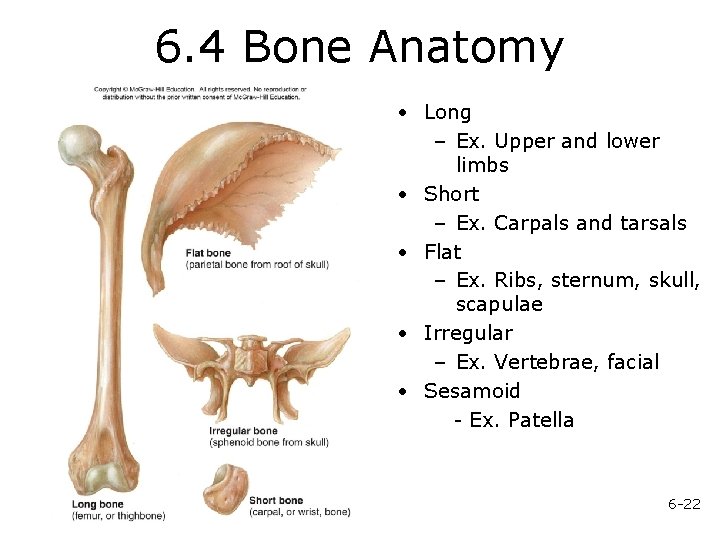
6. 4 Bone Anatomy • Long – Ex. Upper and lower limbs • Short – Ex. Carpals and tarsals • Flat – Ex. Ribs, sternum, skull, scapulae • Irregular – Ex. Vertebrae, facial • Sesamoid - Ex. Patella 6 -22
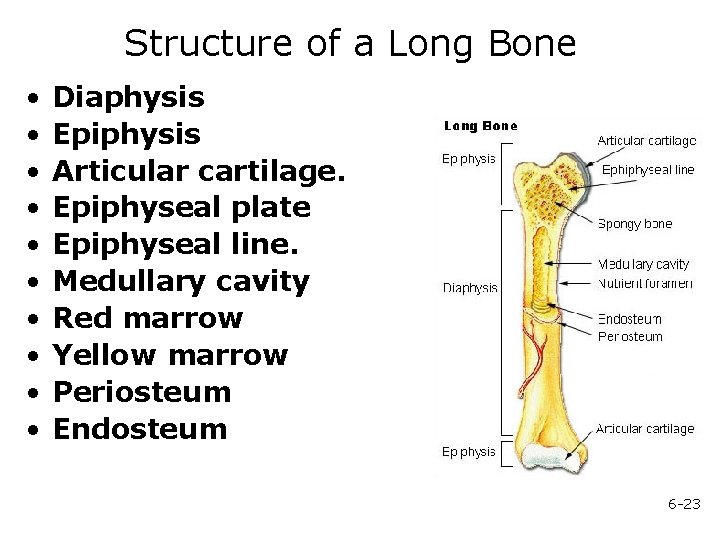
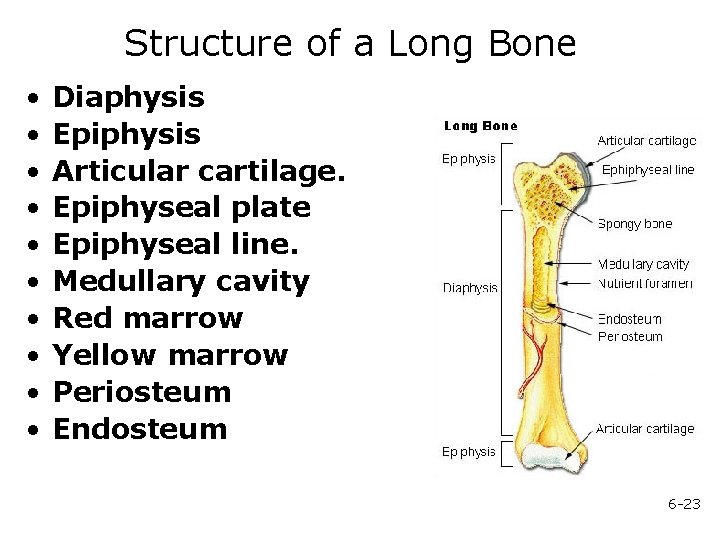
Structure of a Long Bone • • • Diaphysis Epiphysis Articular cartilage. Epiphyseal plate Epiphyseal line. Medullary cavity Red marrow Yellow marrow Periosteum Endosteum 6 -23
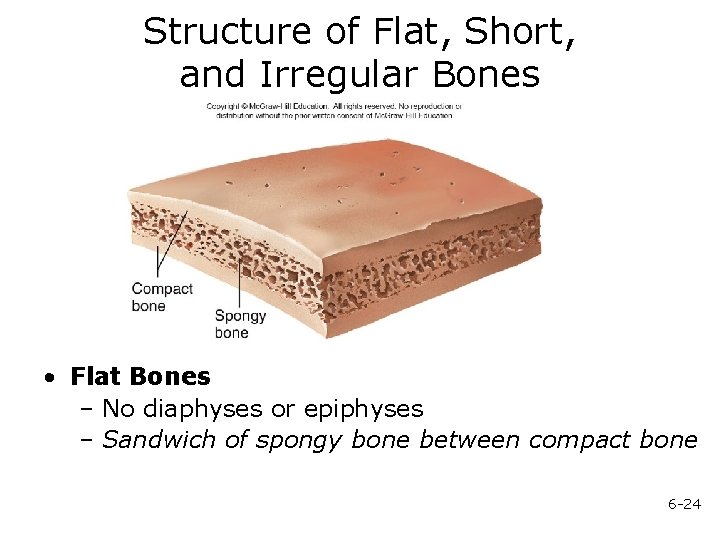
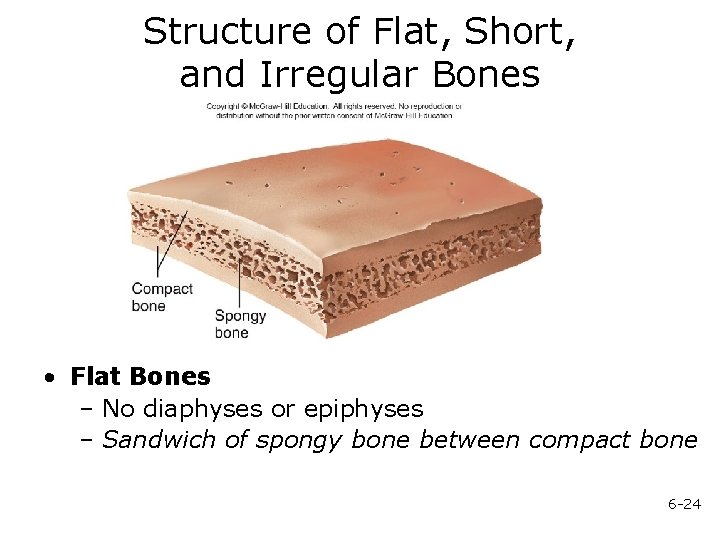
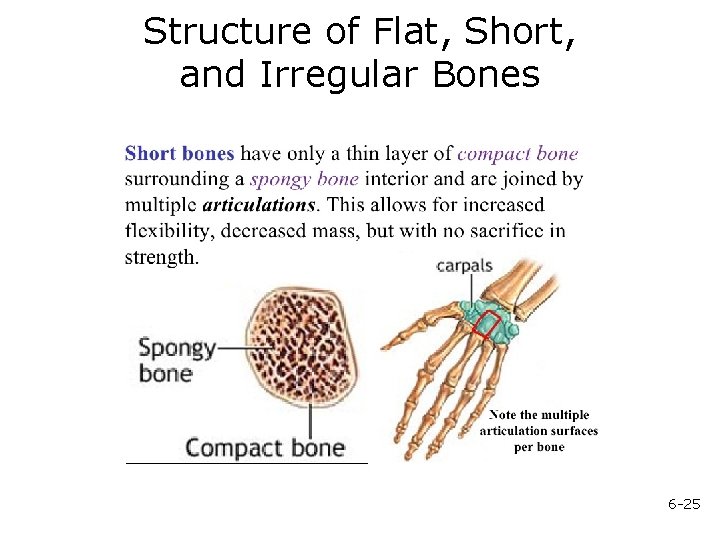
Structure of Flat, Short, and Irregular Bones • Flat Bones – No diaphyses or epiphyses – Sandwich of spongy bone between compact bone 6 -24
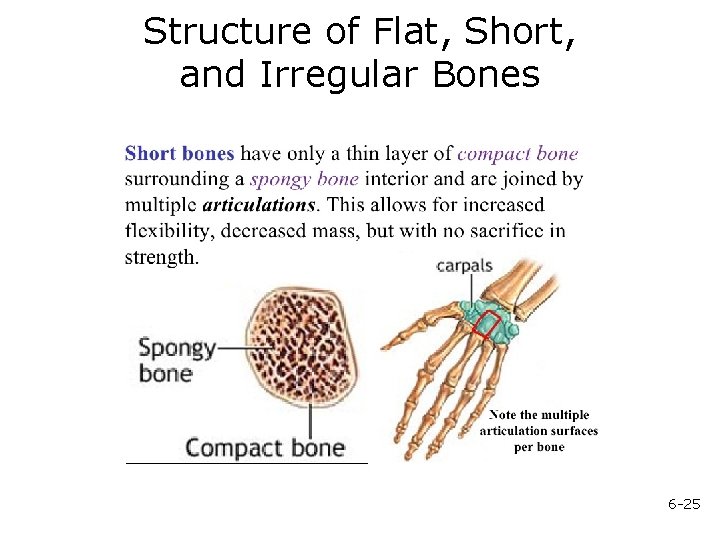
Structure of Flat, Short, and Irregular Bones 6 -25
6. 5 Bone Development • During fetal development, bone forms in two patterns: 1) Intramembranous ossification 2) Endochondral ossification • Both methods of ossification – Produce woven bone that is then remodeled – After remodeling, formation cannot be distinguished as one or other 6 -26
6. 6 Bone Growth • Growth in length occurs at the epiphyseal plate • Closure of epiphyseal plate: epiphyseal plate is ossified becoming the epiphyseal line. Between 12 and 25 years of age • Articular cartilage: does not ossify, and persists through life 6 -27
Factors Affecting Bone Growth • Nutrition Calcium: Vitamin D Rickets: lack of vitamin D during childhood Osteomalacia: lack of vitamin D during adulthood leading to softening of bones Vitamin C Necessary for collagen synthesis by osteoblasts Scurvy: deficiency of vitamin C Lack of vitamin C also causes wounds not to heal, teeth to fall out Hormones Mechanical stress 6 -28
6. 7 Bone Remodeling • Converts woven bone into lamellar bone • Caused by migration of Basic Multicellular Units – Groups of osteoclasts and osteoblasts that remodel bones • Involved in bone growth, changes in bone shape, adjustments in bone due to stress, bone repair, and Ca ion regulation 6 -29
6. 8 Bone Repair 1. Hematoma formation. 2. Callus formation. Callus 3. Callus ossification. Callus replaced by woven, spongy bone 4. Bone remodeling. Replacement of spongy bone and damaged material by compact bone. Sculpting of site by osteoclasts 6 -30
6. 9 Calcium Homeostasis • Bone is major storage site for calcium • The level of calcium in the blood depends upon movement of calcium into or out of bone. – Calcium enters bone when osteoblasts create new bone; calcium leaves bone when osteoclasts break down bone – Two hormones control blood calcium levels- parathyroid hormone and calcitonin. 6 -31