5 year Results from a Prospective Randomized Study

- Slides: 12
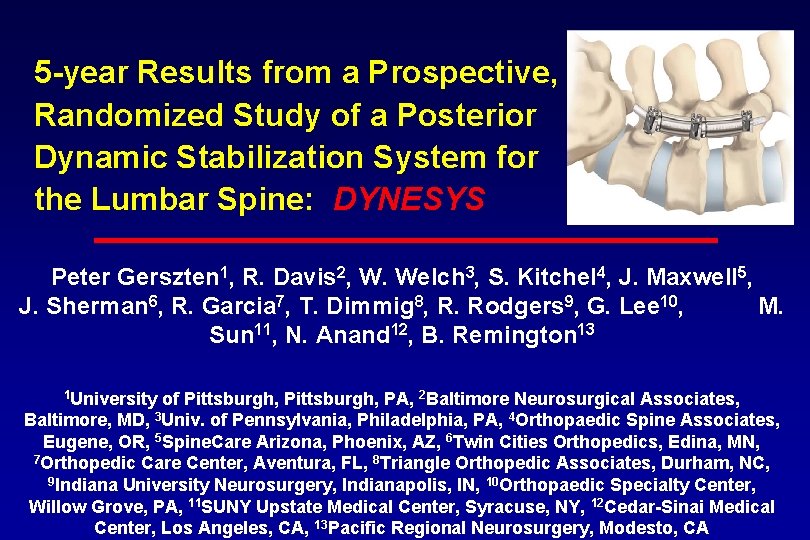
5 -year Results from a Prospective, Randomized Study of a Posterior Dynamic Stabilization System for the Lumbar Spine: DYNESYS Peter Gerszten 1, R. Davis 2, W. Welch 3, S. Kitchel 4, J. Maxwell 5, J. Sherman 6, R. Garcia 7, T. Dimmig 8, R. Rodgers 9, G. Lee 10, M. Sun 11, N. Anand 12, B. Remington 13 1 University of Pittsburgh, PA, 2 Baltimore Neurosurgical Associates, Baltimore, MD, 3 Univ. of Pennsylvania, Philadelphia, PA, 4 Orthopaedic Spine Associates, Eugene, OR, 5 Spine. Care Arizona, Phoenix, AZ, 6 Twin Cities Orthopedics, Edina, MN, 7 Orthopedic Care Center, Aventura, FL, 8 Triangle Orthopedic Associates, Durham, NC, 9 Indiana University Neurosurgery, Indianapolis, IN, 10 Orthopaedic Specialty Center, Willow Grove, PA, 11 SUNY Upstate Medical Center, Syracuse, NY, 12 Cedar-Sinai Medical Center, Los Angeles, CA, 13 Pacific Regional Neurosurgery, Modesto, CA
Introduction Surgical decompression with fusion is an accepted treatment for patients with symptomatic lumbar spondylolisthesis. A system designed for posterior lumbar stabilization without fusion was evaluated under a US FDA study. The results examining this dynamic system compared to rigid stabilization were evaluated. The purpose of this study was to evaluate outcomes following dynamic stabilization (DS) vs. instrumented posterolateral fusion (PLF) for patients with symptomatic lumbar spondylolisthesis.

Methods Study Design: Prospective, randomized, multi-center trial. Patient Sample: 253 patients (DS) and 114 patients (PLF) at 28 centers. Outcome Measures: The Oswestry Disability Index and 100 mm Visual Analog Scales for radicular and back pain were used. Quality of life was assessed with the SF-12 questionnaire. » Radiographs were independently analyzed. Inclusion Criteria: Symptomatic lumbar stenosis, spondylolisthesis (≤Grade I), and candidates for instrumented fusion at 1 -2 contiguous levels (L 1 -S 1). Participants randomly received treatment with DS or instrumented PLF (2: 1 ratio) and were evaluated at 3 -weeks, 3 -, 6 -, 12 -, and 24 -months, and annually thereafter.
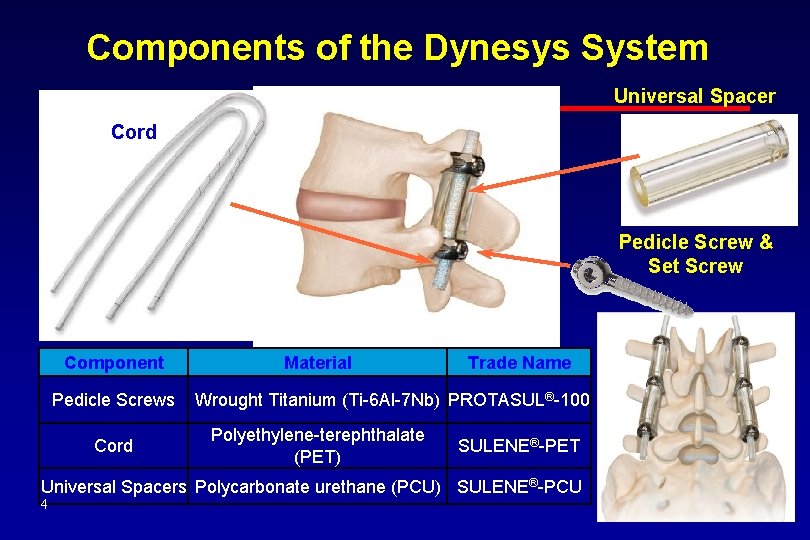
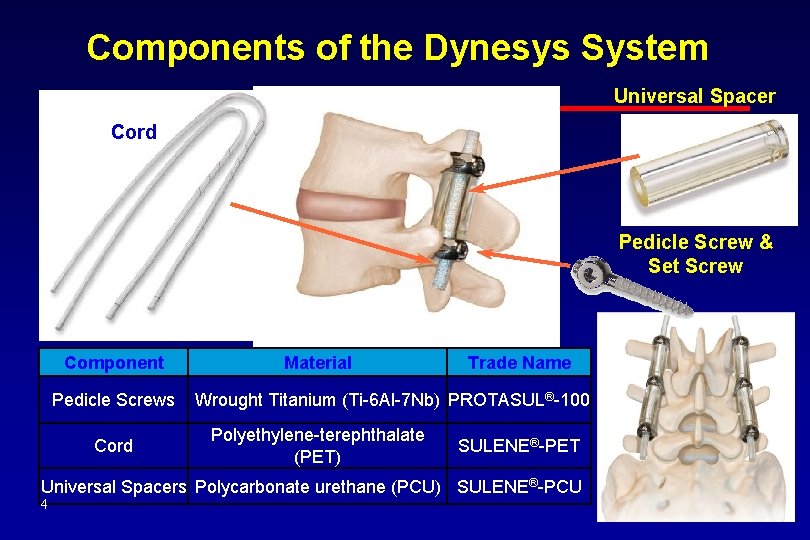
Components of the Dynesys System Universal Spacer Cord Pedicle Screw & Set Screw Component Pedicle Screws Cord Material Trade Name Wrought Titanium (Ti-6 Al-7 Nb) PROTASUL®-100 Polyethylene-terephthalate (PET) SULENE®-PET Universal Spacers Polycarbonate urethane (PCU) SULENE®-PCU 4
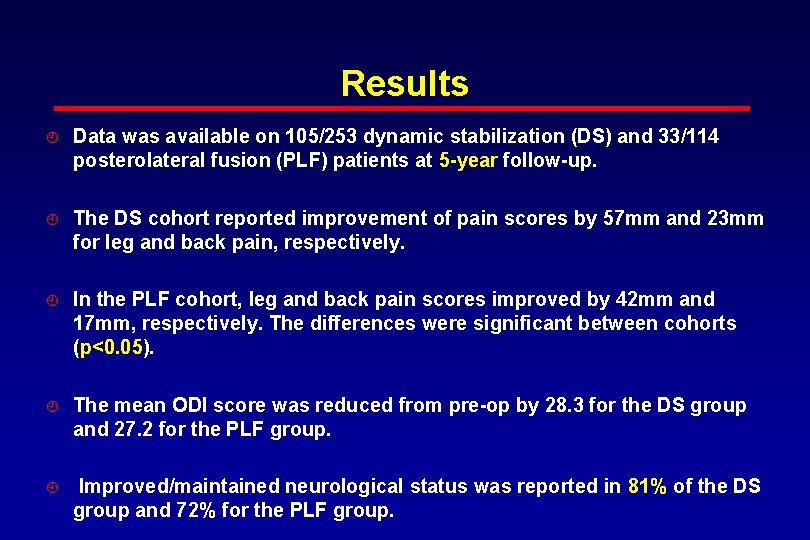
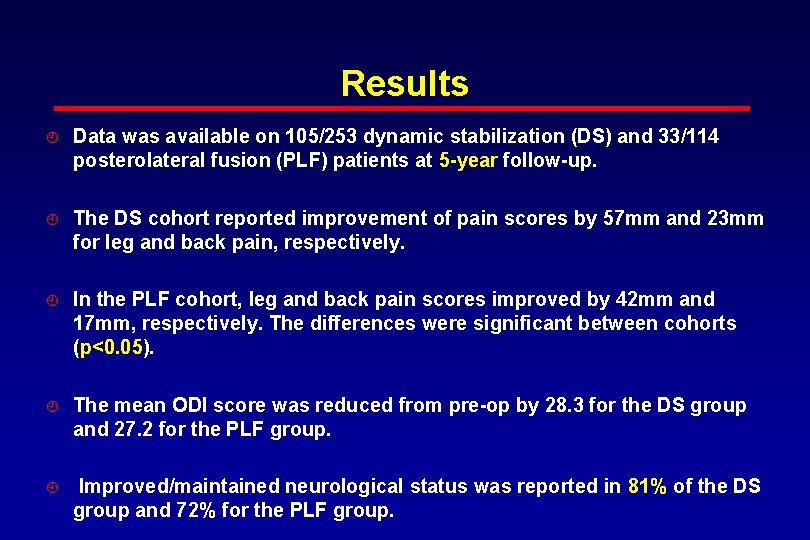
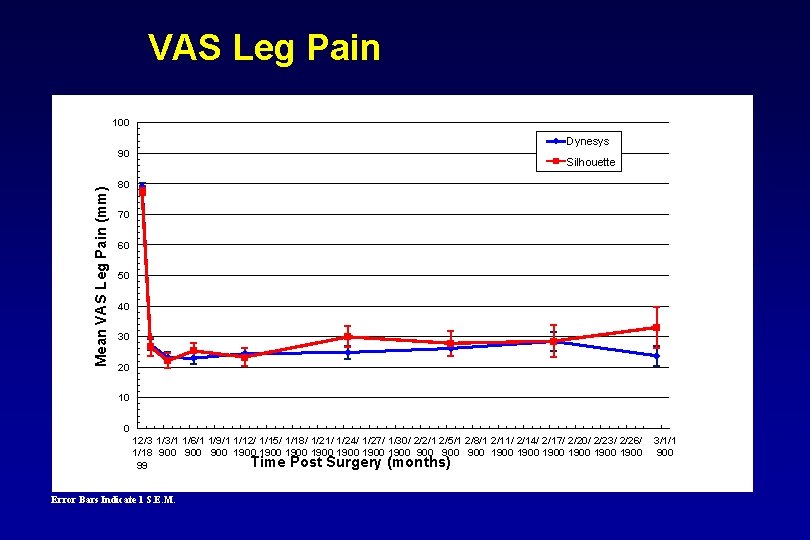
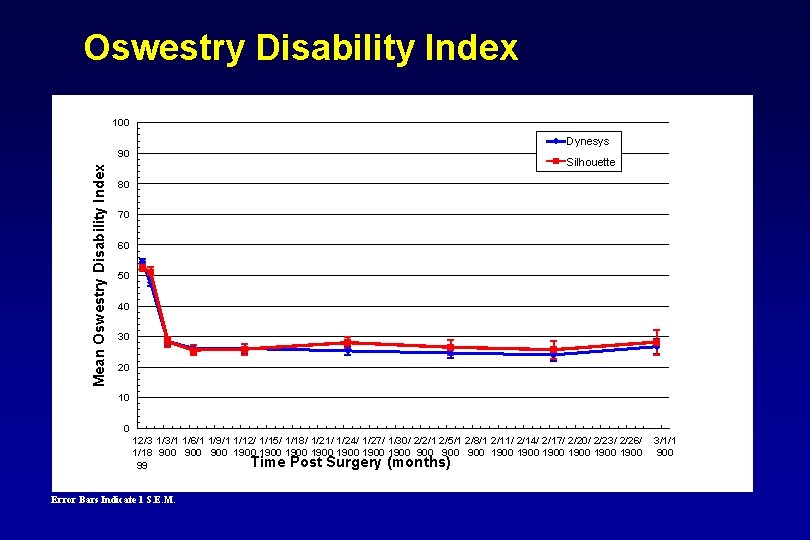
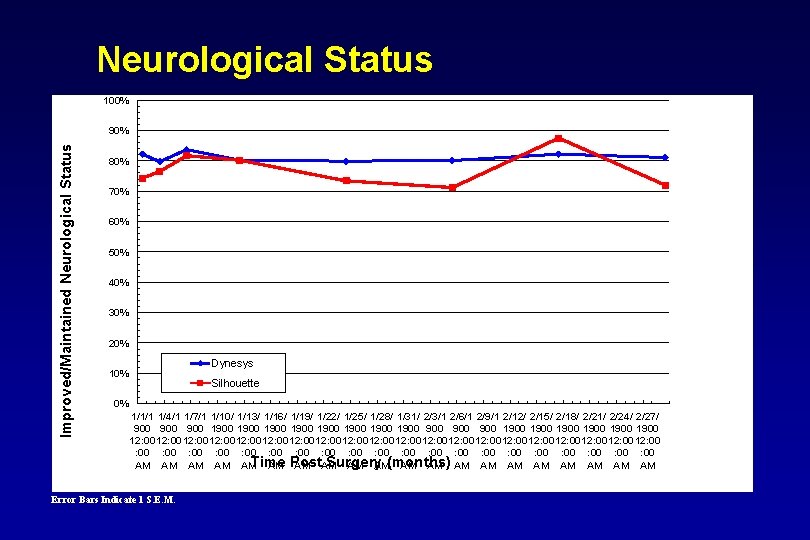
Results Data was available on 105/253 dynamic stabilization (DS) and 33/114 posterolateral fusion (PLF) patients at 5 -year follow-up. The DS cohort reported improvement of pain scores by 57 mm and 23 mm for leg and back pain, respectively. In the PLF cohort, leg and back pain scores improved by 42 mm and 17 mm, respectively. The differences were significant between cohorts (p<0. 05). The mean ODI score was reduced from pre-op by 28. 3 for the DS group and 27. 2 for the PLF group. Improved/maintained neurological status was reported in 81% of the DS group and 72% for the PLF group.
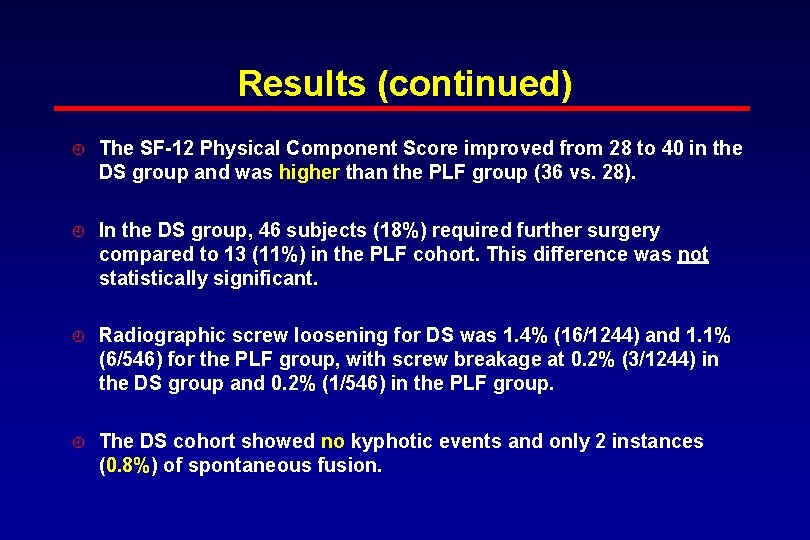
Results (continued) The SF-12 Physical Component Score improved from 28 to 40 in the DS group and was higher than the PLF group (36 vs. 28). In the DS group, 46 subjects (18%) required further surgery compared to 13 (11%) in the PLF cohort. This difference was not statistically significant. Radiographic screw loosening for DS was 1. 4% (16/1244) and 1. 1% (6/546) for the PLF group, with screw breakage at 0. 2% (3/1244) in the DS group and 0. 2% (1/546) in the PLF group. The DS cohort showed no kyphotic events and only 2 instances (0. 8%) of spontaneous fusion.
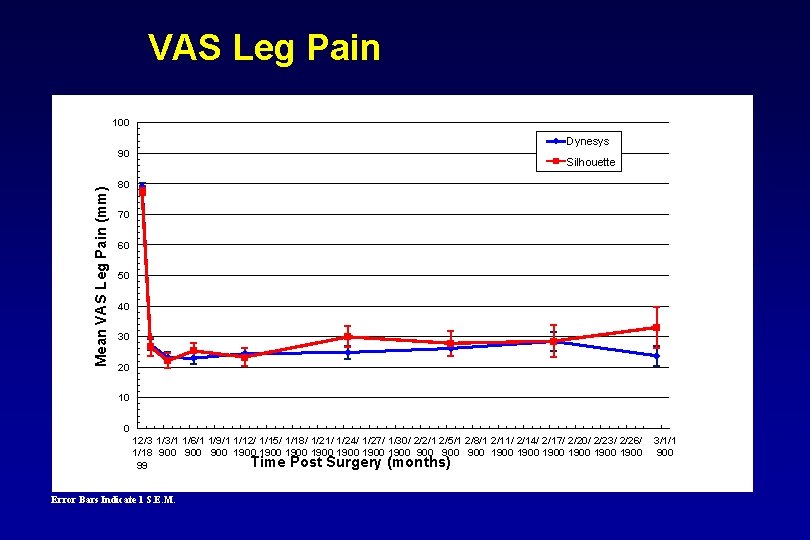
VAS Leg Pain 100 Dynesys Mean VAS Leg Pain (mm) 90 Silhouette 80 70 60 50 40 30 20 10 0 12/3 1/3/1 1/6/1 1/9/1 1/12/ 1/15/ 1/18/ 1/21/ 1/24/ 1/27/ 1/30/ 2/2/1 2/5/1 2/8/1 2/11/ 2/14/ 2/17/ 2/20/ 2/23/ 2/26/ 1/18 900 900 1900 1900 900 1900 1900 Time Post Surgery (months) 99 Error Bars Indicate 1 S. E. M. 3/1/1 900
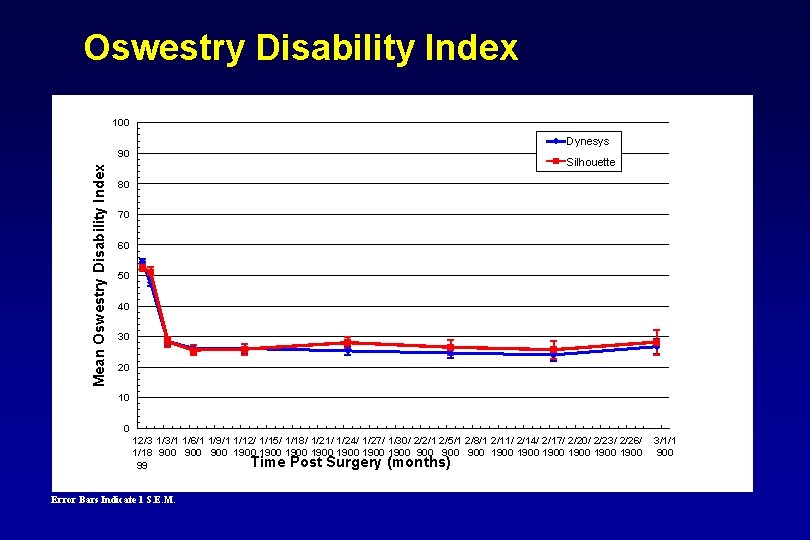
Oswestry Disability Index 100 Dynesys Mean Oswestry Disability Index 90 Silhouette 80 70 60 50 40 30 20 10 0 12/3 1/3/1 1/6/1 1/9/1 1/12/ 1/15/ 1/18/ 1/21/ 1/24/ 1/27/ 1/30/ 2/2/1 2/5/1 2/8/1 2/11/ 2/14/ 2/17/ 2/20/ 2/23/ 2/26/ 1/18 900 900 1900 1900 900 1900 1900 Time Post Surgery (months) 99 Error Bars Indicate 1 S. E. M. 3/1/1 900
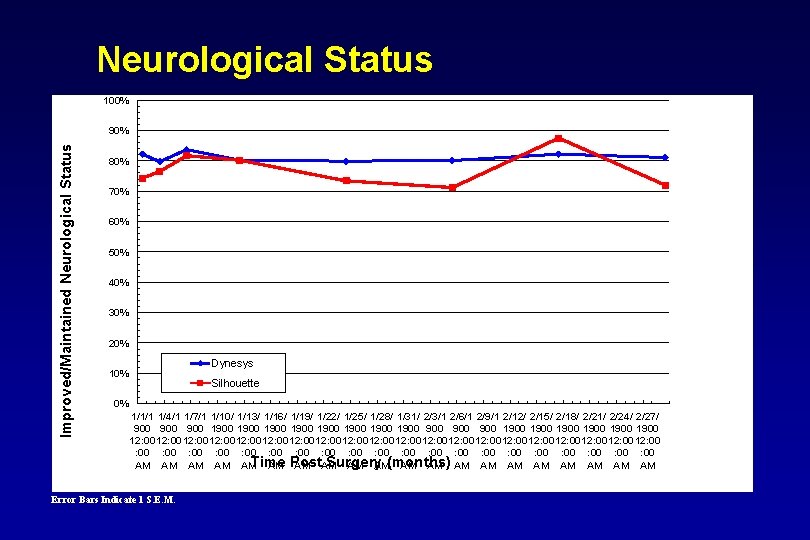
Neurological Status 100% Improved/Maintained Neurological Status 90% 80% 70% 60% 50% 40% 30% 20% Dynesys 10% Silhouette 0% 1/1/1 1/4/1 1/7/1 1/10/ 1/13/ 1/16/ 1/19/ 1/22/ 1/25/ 1/28/ 1/31/ 2/3/1 2/6/1 2/9/1 2/12/ 2/15/ 2/18/ 2/21/ 2/24/ 2/27/ 900 900 1900 1900 900 1900 1900 12: 00 12: 00 12: 00 12: 00 12: 00 : 00 : 00 : 00 : 00 : 00 Time Surgery AM AM AM Post AM AM(months) AM AM AM Error Bars Indicate 1 S. E. M.
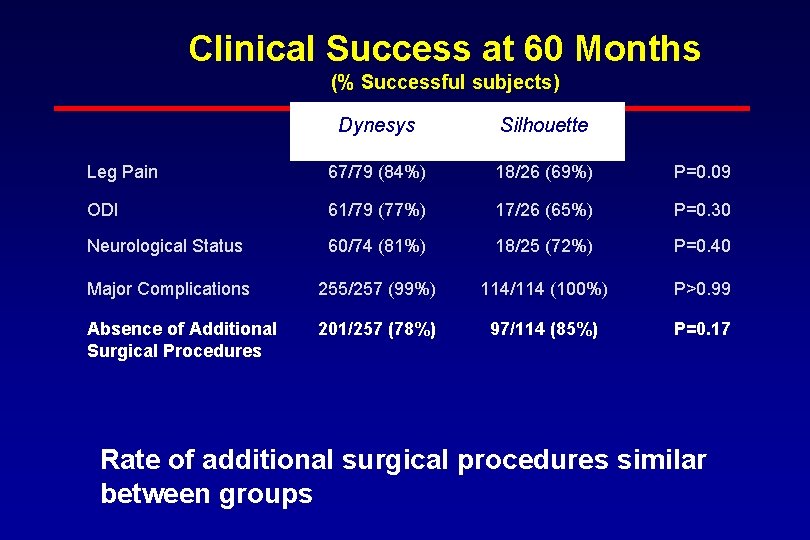
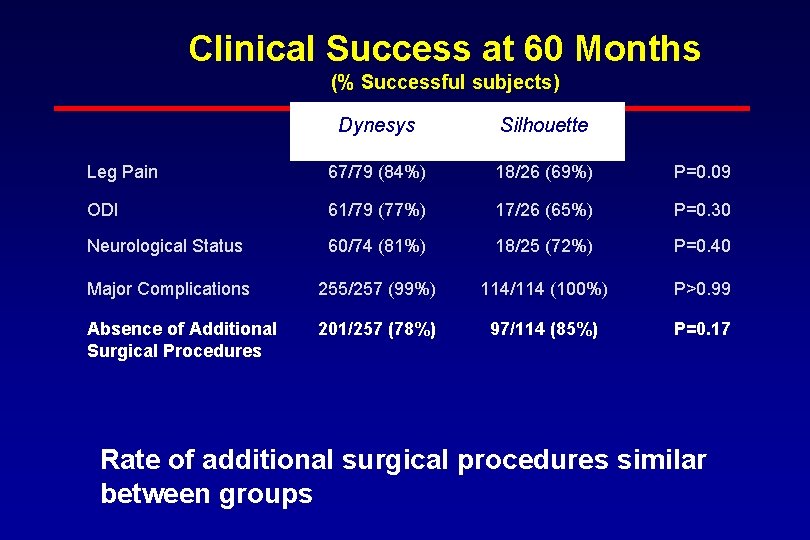
Clinical Success at 60 Months (% Successful subjects) Dynesys Silhouette Leg Pain 67/79 (84%) 18/26 (69%) P=0. 09 ODI 61/79 (77%) 17/26 (65%) P=0. 30 Neurological Status 60/74 (81%) 18/25 (72%) P=0. 40 Major Complications 255/257 (99%) 114/114 (100%) P>0. 99 Absence of Additional Surgical Procedures 201/257 (78%) 97/114 (85%) P=0. 17 Rate of additional surgical procedures similar between groups
Conclusions At 5 years, the subjects implanted with the Dynesys dynamic stabilization system continued to show a clinically significant improvement in… » leg, » back pain, and » SF-12 PCS …compared to the fusion subjects. Radiographic outcomes were also positive, with less than a 1. 5% rate of negative events reported.
Disclosures All authors participated in this United States Food and Drug Administration clinical trial under a consulting agreement with Zimmer.