5 Intro to EM Airway Management RSI Pharmacology
- Slides: 9
#5 Intro to EM Airway Management. RSI Pharmacology Andrew Brainard 1
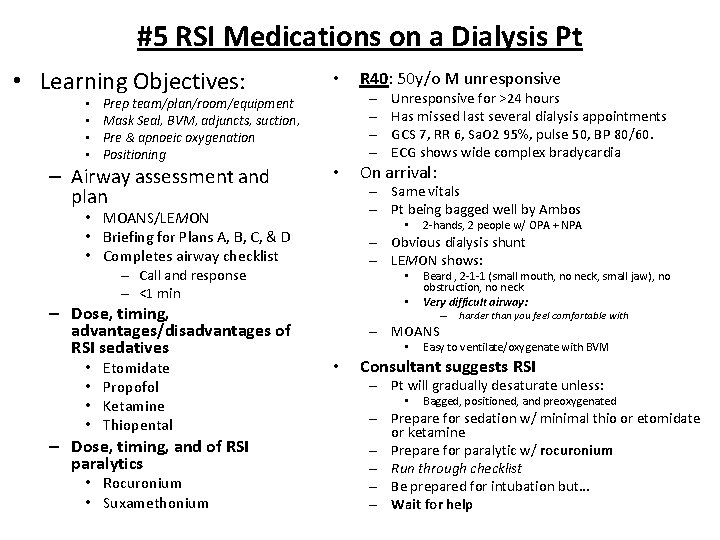
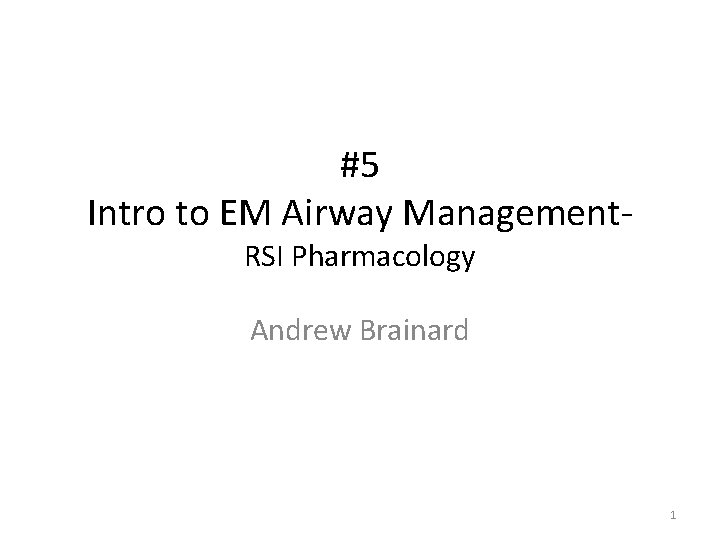
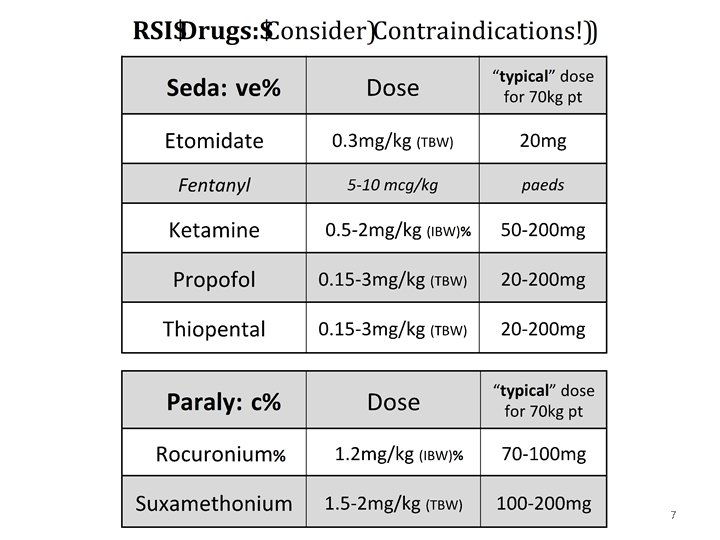
#5 RSI Medications on a Dialysis Pt • Learning Objectives: • • Prep team/plan/room/equipment Mask Seal, BVM, adjuncts, suction, Pre & apnoeic oxygenation Positioning – Airway assessment and plan • – – • Etomidate Propofol Ketamine Thiopental – Dose, timing, and of RSI paralytics • Rocuronium • Suxamethonium On arrival: • 2 -hands, 2 people w/ OPA + NPA – Obvious dialysis shunt – LEMON shows: – Call and response – <1 min • • Unresponsive for >24 hours Has missed last several dialysis appointments GCS 7, RR 6, Sa. O 2 95%, pulse 50, BP 80/60. ECG shows wide complex bradycardia – Same vitals – Pt being bagged well by Ambos • MOANS/LEMON • Briefing for Plans A, B, C, & D • Completes airway checklist – Dose, timing, advantages/disadvantages of RSI sedatives R 40: 50 y/o M unresponsive • • Beard , 2 -1 -1 (small mouth, no neck, small jaw), no obstruction, no neck Very difficult airway: – harder than you feel comfortable with – MOANS • • Easy to ventilate/oxygenate with BVM Consultant suggests RSI – Pt will gradually desaturate unless: • Bagged, positioned, and preoxygenated – Prepare for sedation w/ minimal thio or etomidate or ketamine – Prepare for paralytic w/ rocuronium – Run through checklist – Be prepared for intubation but… – Wait for help
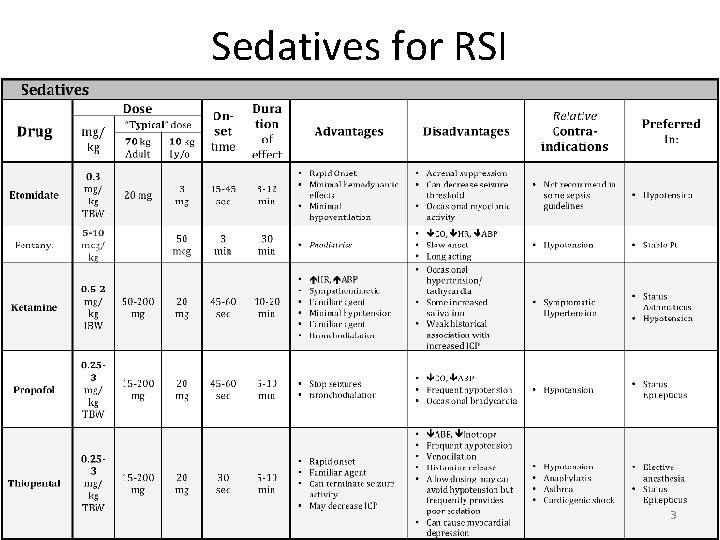
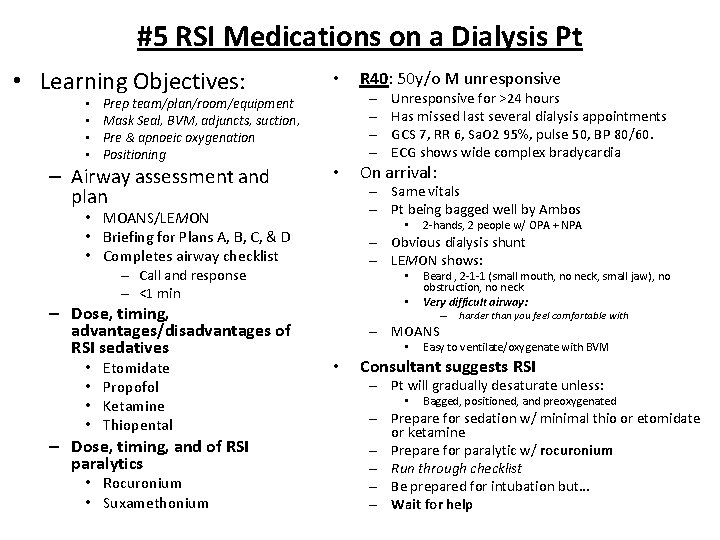
Sedatives for RSI 3
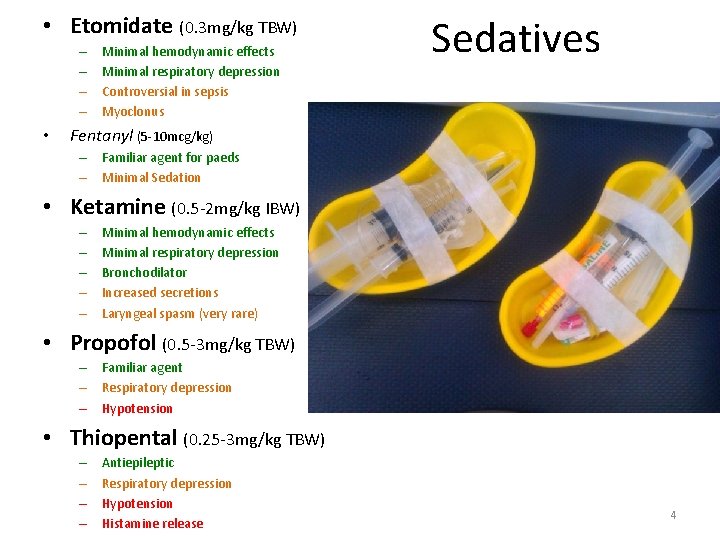
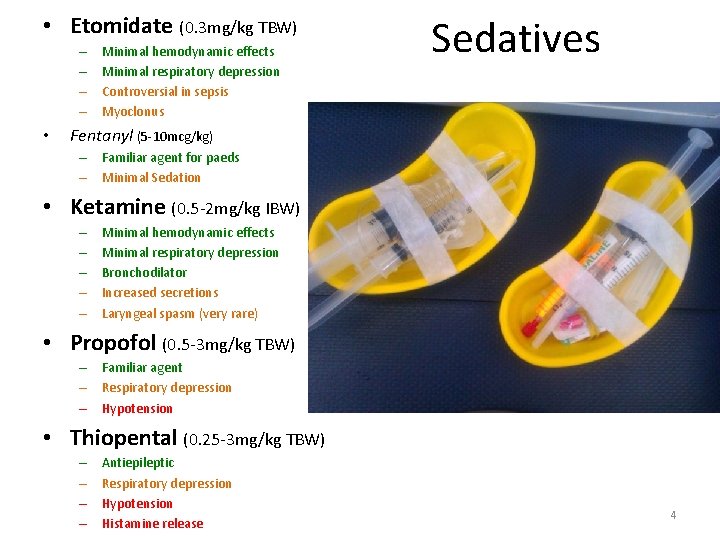
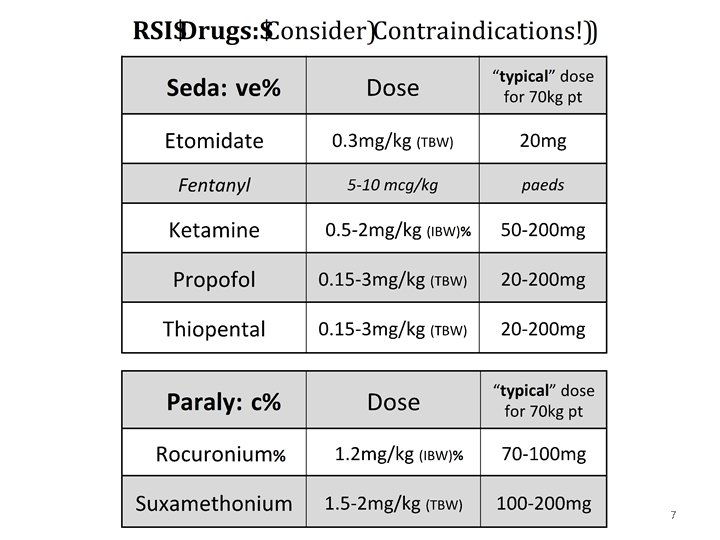
• Etomidate (0. 3 mg/kg TBW) – – • Minimal hemodynamic effects Minimal respiratory depression Controversial in sepsis Myoclonus Sedatives Fentanyl (5 -10 mcg/kg) – Familiar agent for paeds – Minimal Sedation • Ketamine (0. 5 -2 mg/kg IBW) – – – Minimal hemodynamic effects Minimal respiratory depression Bronchodilator Increased secretions Laryngeal spasm (very rare) • Propofol (0. 5 -3 mg/kg TBW) – Familiar agent – Respiratory depression – Hypotension • Thiopental (0. 25 -3 mg/kg TBW) – – Antiepileptic Respiratory depression Hypotension Histamine release 4
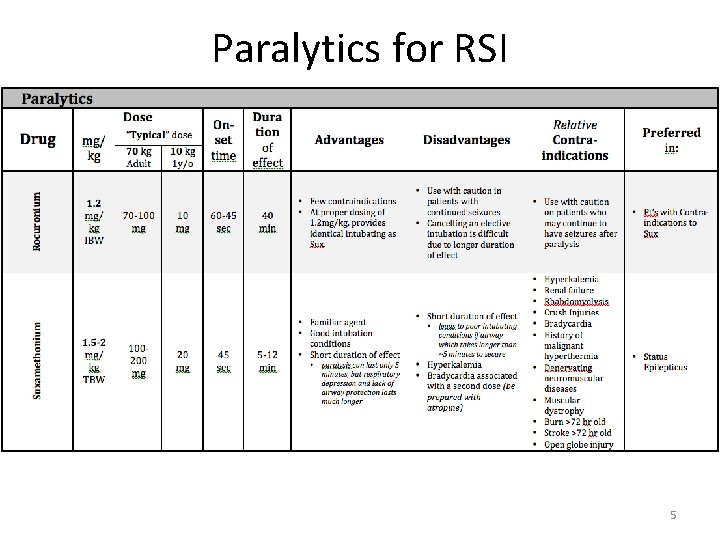
Paralytics for RSI 5
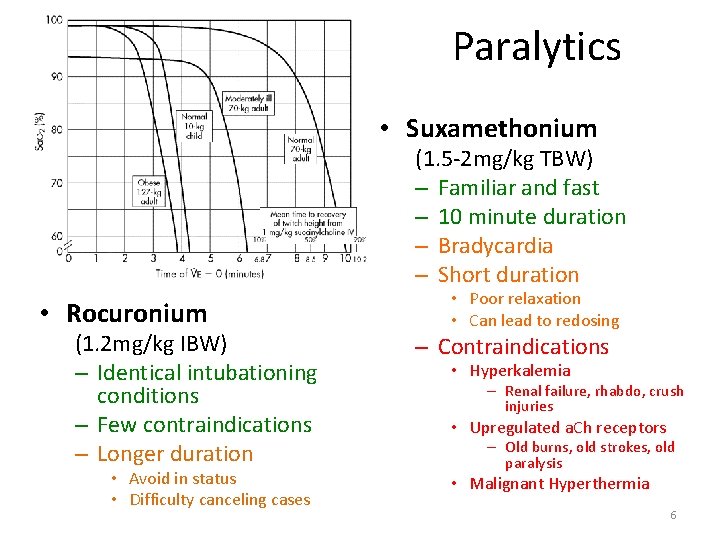
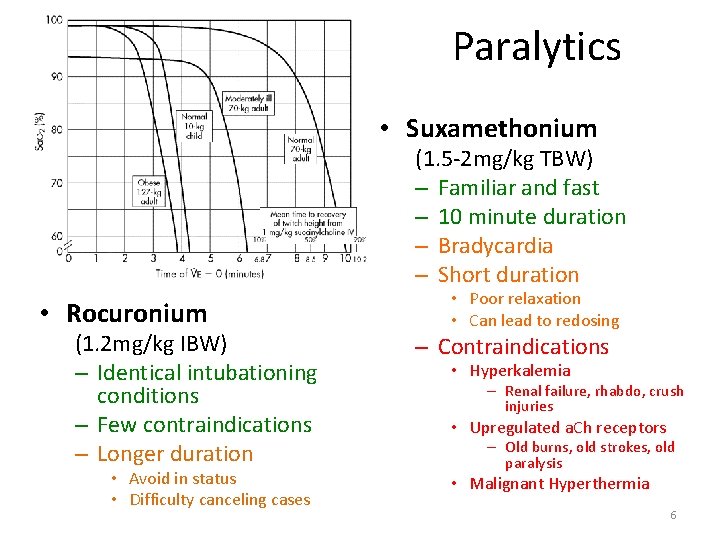
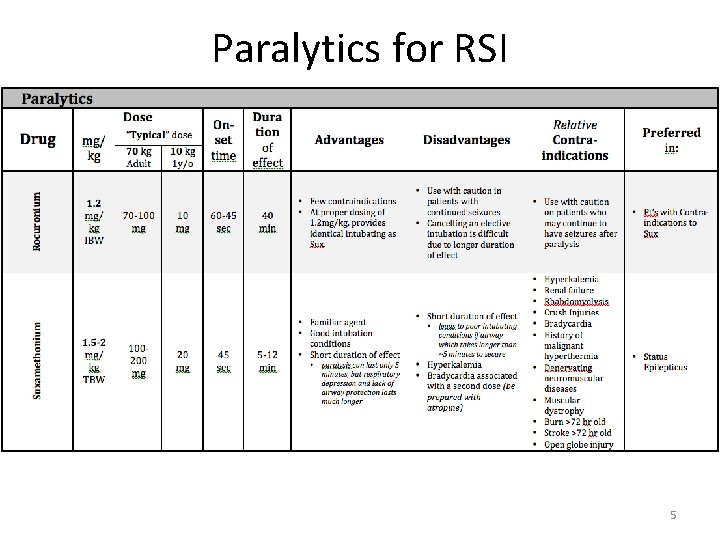
Paralytics • Suxamethonium (1. 5 -2 mg/kg TBW) – Familiar and fast – 10 minute duration – Bradycardia – Short duration • Rocuronium (1. 2 mg/kg IBW) – Identical intubationing conditions – Few contraindications – Longer duration • Avoid in status • Difficulty canceling cases • Poor relaxation • Can lead to redosing – Contraindications • Hyperkalemia – Renal failure, rhabdo, crush injuries • Upregulated a. Ch receptors – Old burns, old strokes, old paralysis • Malignant Hyperthermia 6
7
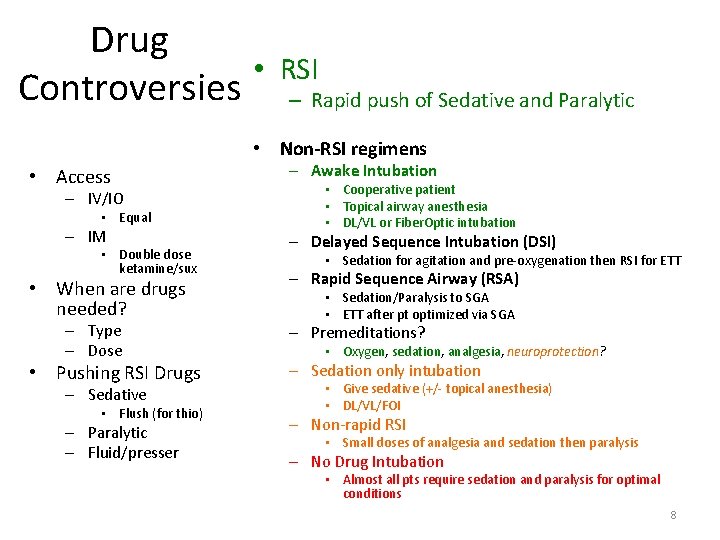
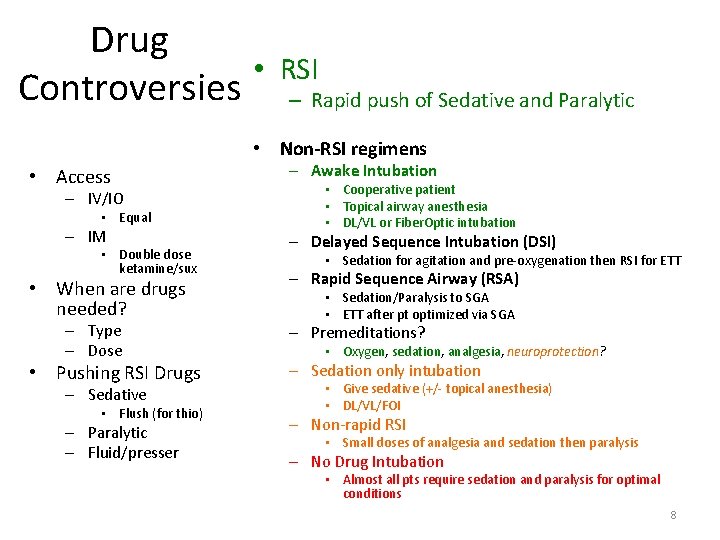
Drug • Controversies RSI – Rapid push of Sedative and Paralytic • Non-RSI regimens • Access – IV/IO • Equal – IM • Double dose ketamine/sux • When are drugs needed? – Type – Dose • Pushing RSI Drugs – Sedative • Flush (for thio) – Paralytic – Fluid/presser – Awake Intubation • Cooperative patient • Topical airway anesthesia • DL/VL or Fiber. Optic intubation – Delayed Sequence Intubation (DSI) • Sedation for agitation and pre-oxygenation then RSI for ETT – Rapid Sequence Airway (RSA) • Sedation/Paralysis to SGA • ETT after pt optimized via SGA – Premeditations? • Oxygen, sedation, analgesia, neuroprotection? – Sedation only intubation • Give sedative (+/- topical anesthesia) • DL/VL/FOI – Non-rapid RSI • Small doses of analgesia and sedation then paralysis – No Drug Intubation • Almost all pts require sedation and paralysis for optimal conditions 8
• ACEP Practice Management- Focus on Rapid Sequent Intubation: http: //www. acep. org/Clinical---Practice. Management/Focus-On--Rapid-Sequence-Intubation. Pharmacology/ (Accessed 21/03/2013) • Walls RM. Manual of Emergency Airway Management, 4 th, Walls RM, Murphy MF. (Eds), Lippincott Williams and Wilkins, Philadelphia 2012 • Morris et al Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia. 2009 May; 64(5): 532 -9.