5 3 102 studies 171 756 children Africa
























- Slides: 61





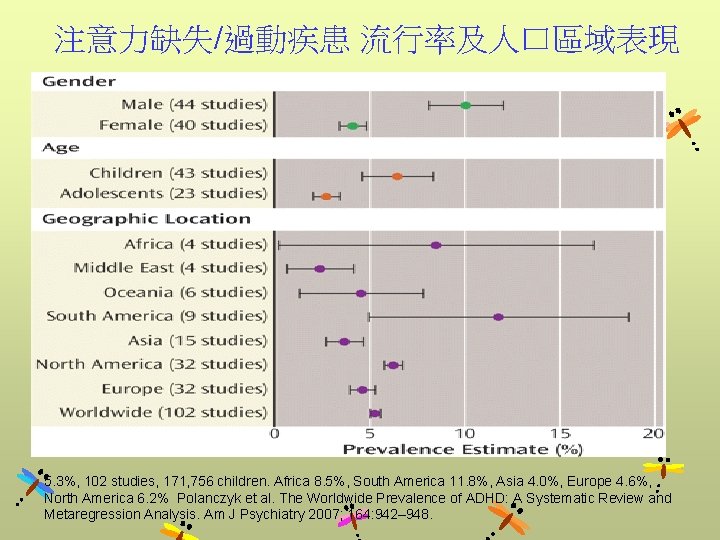
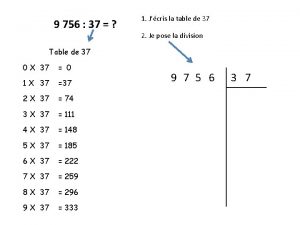
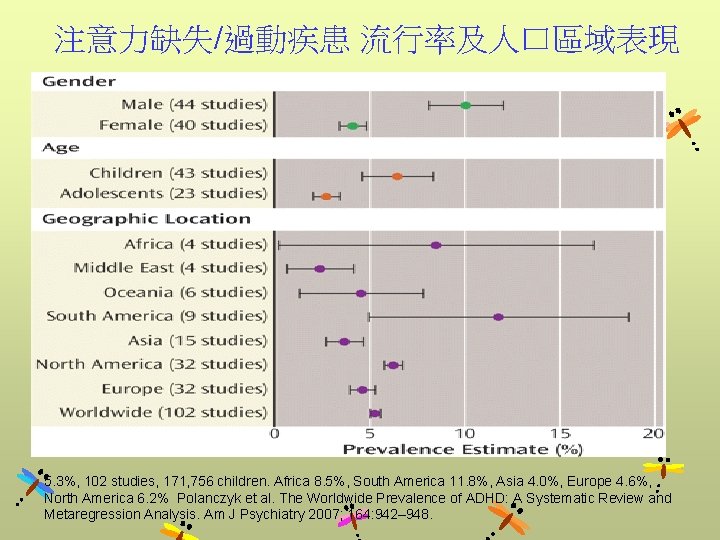
注意力缺失/過動疾患 流行率及人口區域表現 5. 3%, 102 studies, 171, 756 children. Africa 8. 5%, South America 11. 8%, Asia 4. 0%, Europe 4. 6%, North America 6. 2% Polanczyk et al. The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis. Am J Psychiatry 2007; 164: 942– 948.
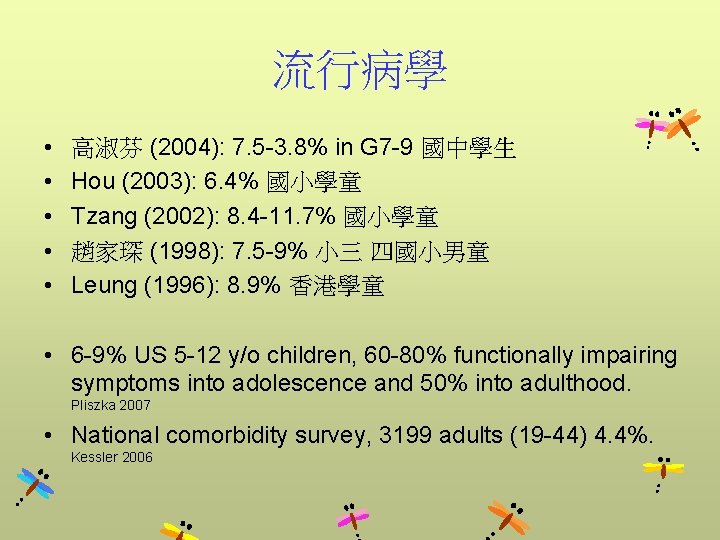
流行病學 • • • 高淑芬 (2004): 7. 5 -3. 8% in G 7 -9 國中學生 Hou (2003): 6. 4% 國小學童 Tzang (2002): 8. 4 -11. 7% 國小學童 趙家琛 (1998): 7. 5 -9% 小三 四國小男童 Leung (1996): 8. 9% 香港學童 • 6 -9% US 5 -12 y/o children, 60 -80% functionally impairing symptoms into adolescence and 50% into adulthood. Pliszka 2007 • National comorbidity survey, 3199 adults (19 -44) 4. 4%. Kessler 2006

FIGURE 1 Age-specific incidence rates of MR, ADHD, and autism in childhood, according to birth year, in Taiwan Chen, C. -Y. et al. Pediatrics 2007; 119: e 435 -e 443 Copyright © 2007 American Academy of Pediatrics

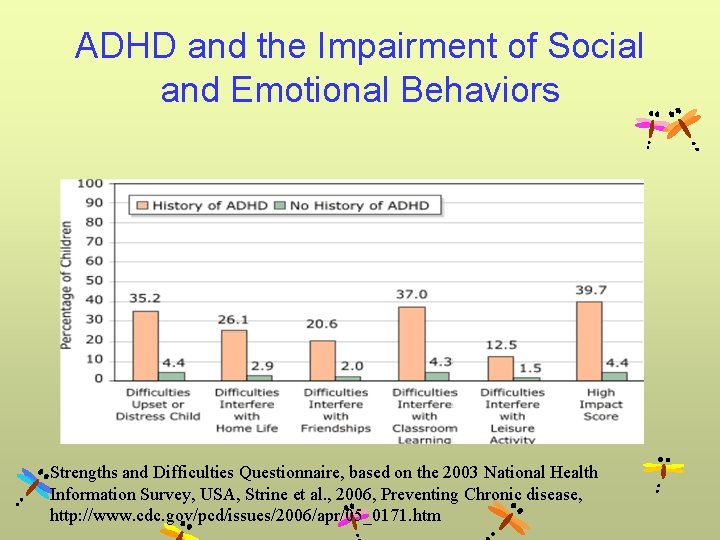
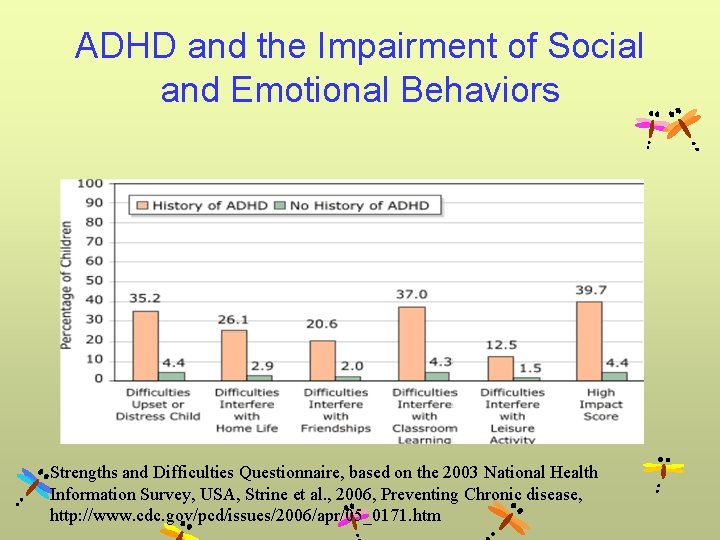
ADHD and the Impairment of Social and Emotional Behaviors Strengths and Difficulties Questionnaire, based on the 2003 National Health Information Survey, USA, Strine et al. , 2006, Preventing Chronic disease, http: //www. cdc. gov/pcd/issues/2006/apr/05_0171. htm

Social and Emotional Behavioral Problems in Children with ADHD European survey of parents of children with ADHD (n=910) and without ADHD (N=995). *† p<. 0001 , (Coghill et al. , Child and adolescent psychiatry and mental health, 2: 31, 2008)
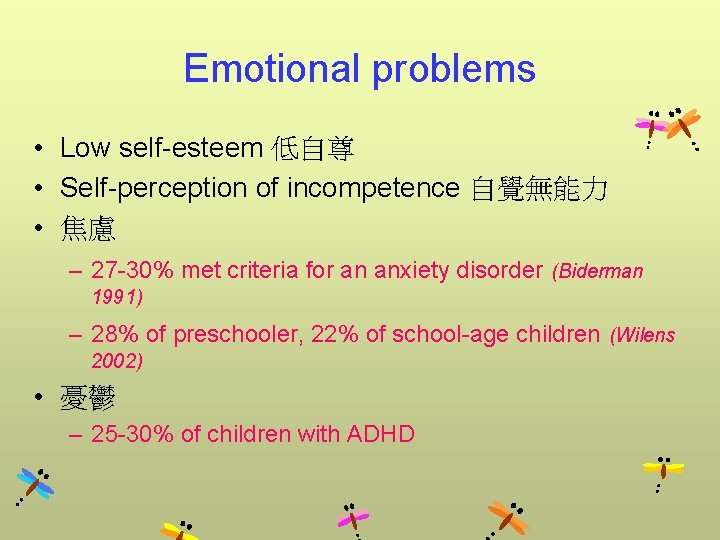
Emotional problems • Low self-esteem 低自尊 • Self-perception of incompetence 自覺無能力 • 焦慮 – 27 -30% met criteria for an anxiety disorder (Biderman 1991) – 28% of preschooler, 22% of school-age children (Wilens 2002) • 憂鬱 – 25 -30% of children with ADHD

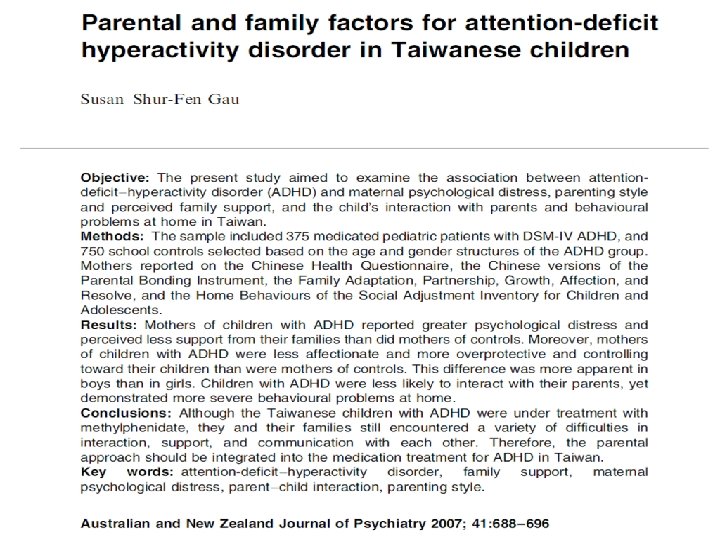
Relationship of attention-deficit-hyperactivity disorder symptoms, depressive/anxiety symptoms, and life quality in young men • 929 draftees into the Taiwanese army – – – Adult ADHD Self-Report Scale (ASRS), WHO: Quality of Life-Brief Version, Epworth Sleepiness Scale, Beck Depression Inventory-II, Beck Anxiety Scale. • 328 adults (35. 3%) identified as having ADHD: – 65 (7. 0%) with definite ADHD and – 263 (28. 3%) with probable ADHD • More severe depressive, anxiety symptoms and daytime sleepiness, and had poorer quality of life than the 601 controls (all P < 0. 05). Chao CY, Psychiatry Clin Neurosci. 2008 Aug; 62(4): 421 -6

ADHD, Internet addiction, Sleep disturbance and Depression in colleges students • • • 426 college students ASRS: inattention 5. 2%; impulsivity 2. 8%; CIAS-R: 2. 8% internet addiction; Sleep influence test 10. 3% sleep disturbance; BDI-II: 4. 5% depression • The depression group had significantly higher scores in inattention (P < 0. 01), and impulsivity (P < 0. 01) than the non-depression group.

Predictive values of psychiatric symptoms for internet addiction in adolescents • 2293 (1179 boys and 1114 girls) • Predicting the occurrence of Internet addiction in the 2 -year F/U – – Depression, Attention-deficit/hyperactivity disorder, (female) Social phobia, and Hostility (male) Yen CF Arch Pediatr Adolesc Med. 2009 Oct; 163(10): 937 -43.
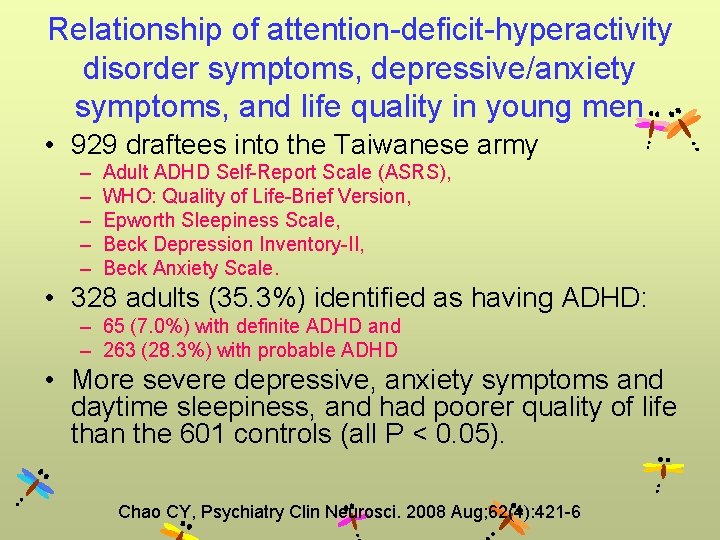
Peer relation • More than 50% of children with ADHD have significant problems in peer relationship (Pelham 1982) • Less knowledge about – social skills, appropriate behavior with others (Grenell 1987) • More likely to be engage in – Bullying, Victimized in bullying episode (Unnever 2003) • Children with ADHD are stigmatized by their behavior – – Troublemaking Excessive talking Breaking rules Impulsive aggression (Barkley 1991)
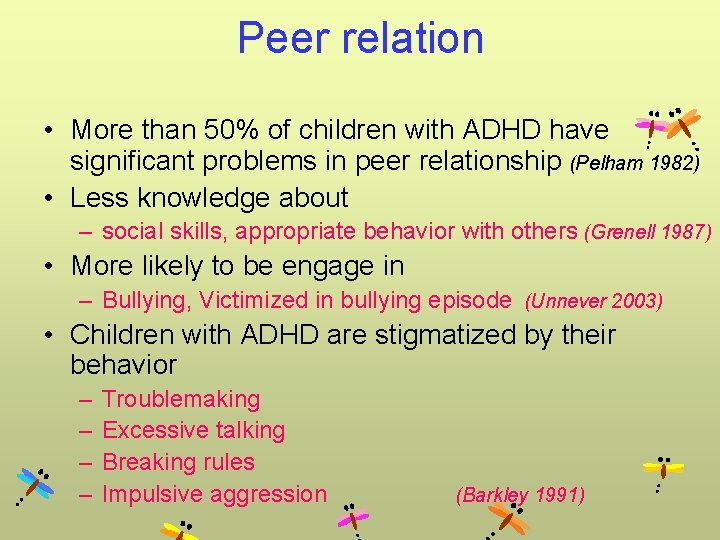
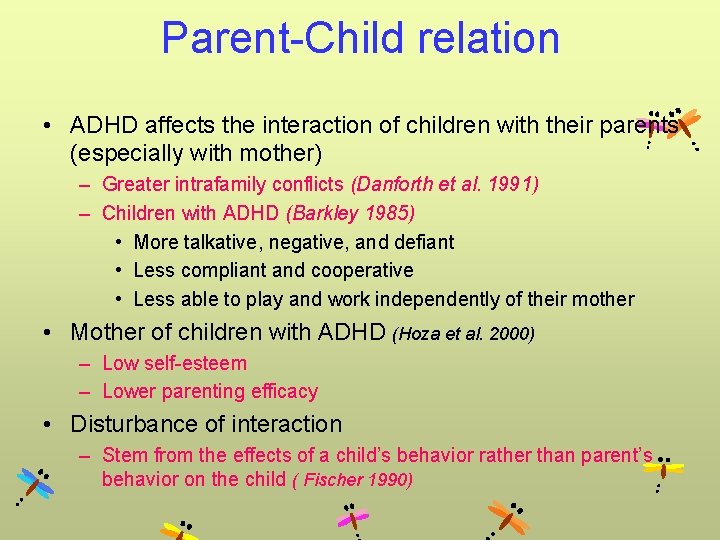
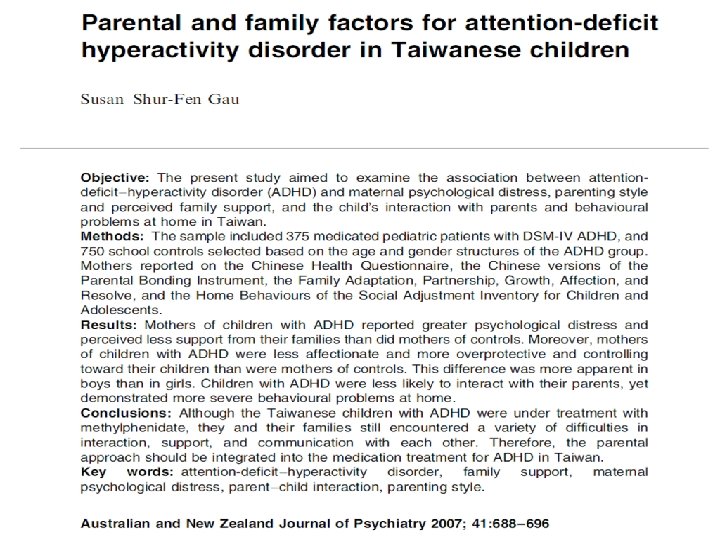
Parent-Child relation • ADHD affects the interaction of children with their parents (especially with mother) – Greater intrafamily conflicts (Danforth et al. 1991) – Children with ADHD (Barkley 1985) • More talkative, negative, and defiant • Less compliant and cooperative • Less able to play and work independently of their mother • Mother of children with ADHD (Hoza et al. 2000) – Low self-esteem – Lower parenting efficacy • Disturbance of interaction – Stem from the effects of a child’s behavior rather than parent’s behavior on the child ( Fischer 1990)
Academic & School performance • Lower academic performance than their classmates – By 10 -30 points on standardized achievement test – Including reading, spelling, math, and reading comprehension • Disruptive classroom behavior • Underperforming in school relative to ability – Repetition of a grade (30% or more) – Be placed in one or more special education programs (30 -40%) – Suspended from school (up to 46%) (Barkely et al. 1990)
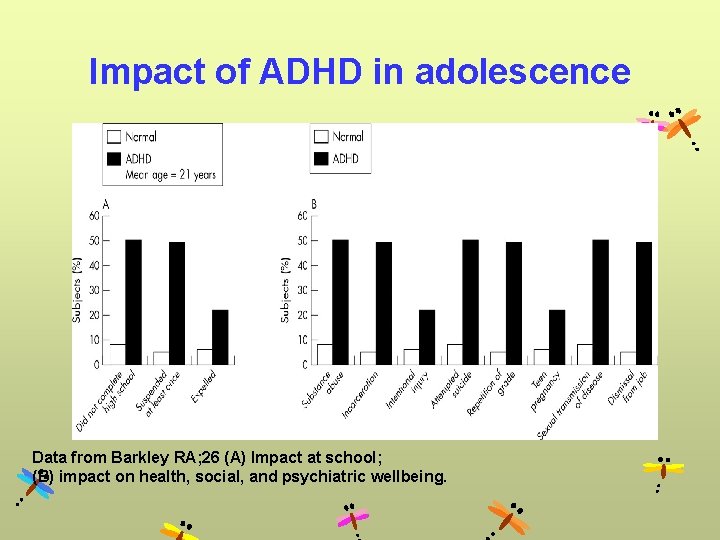
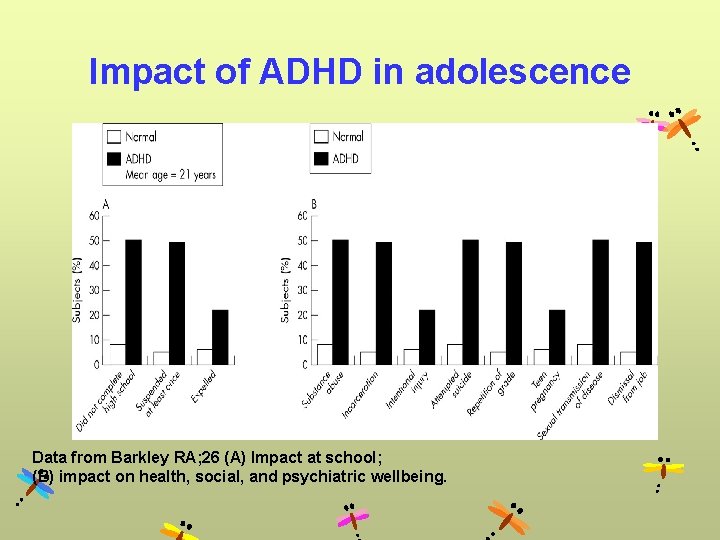
Impact of ADHD in adolescence Data from Barkley RA; 26 (A) Impact at school; (B) impact on health, social, and psychiatric wellbeing.
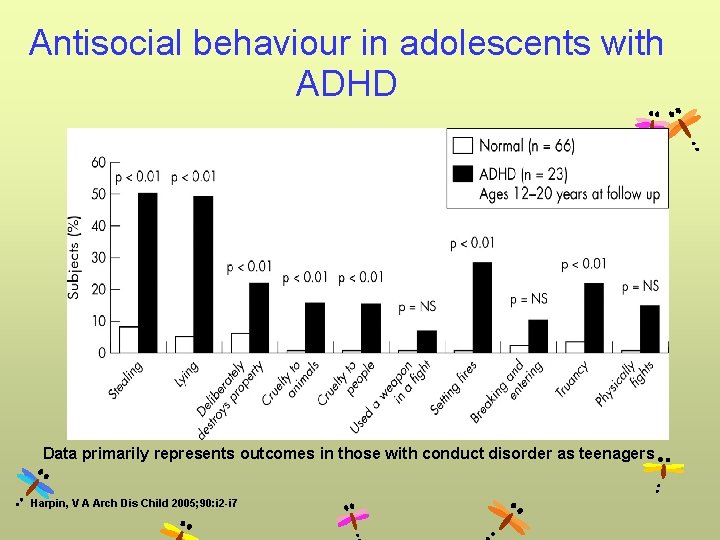
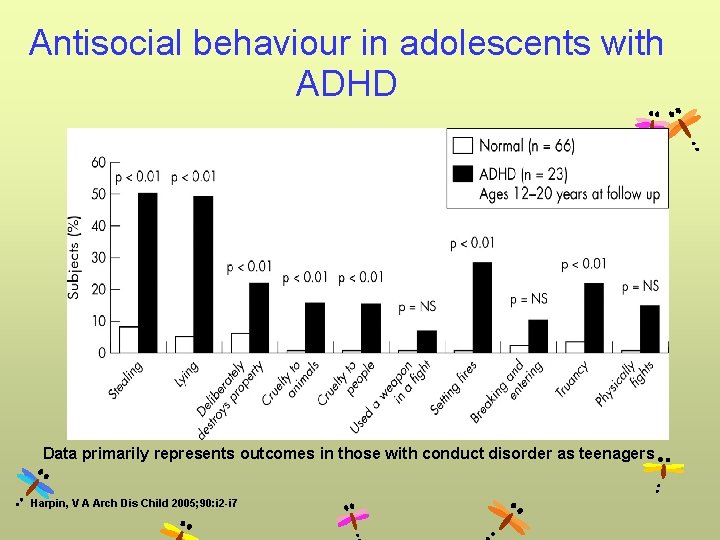
Antisocial behaviour in adolescents with ADHD Data primarily represents outcomes in those with conduct disorder as teenagers Harpin, V A Arch Dis Child 2005; 90: i 2 -i 7
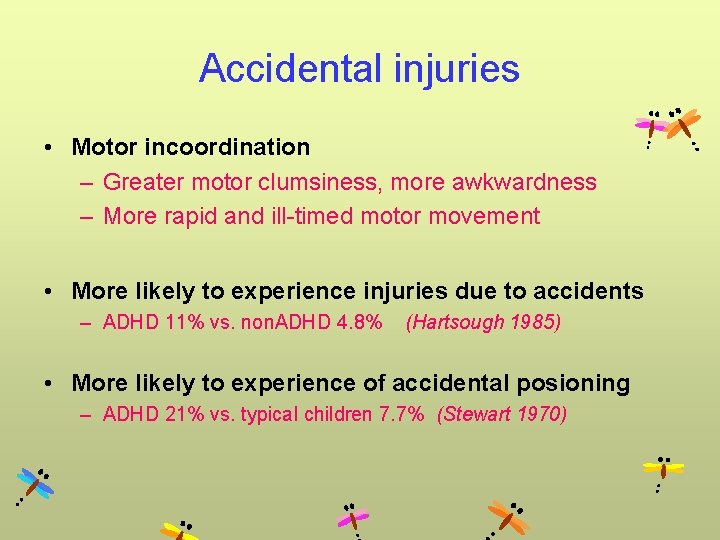
Accidental injuries • Motor incoordination – Greater motor clumsiness, more awkwardness – More rapid and ill-timed motor movement • More likely to experience injuries due to accidents – ADHD 11% vs. non. ADHD 4. 8% (Hartsough 1985) • More likely to experience of accidental posioning – ADHD 21% vs. typical children 7. 7% (Stewart 1970)
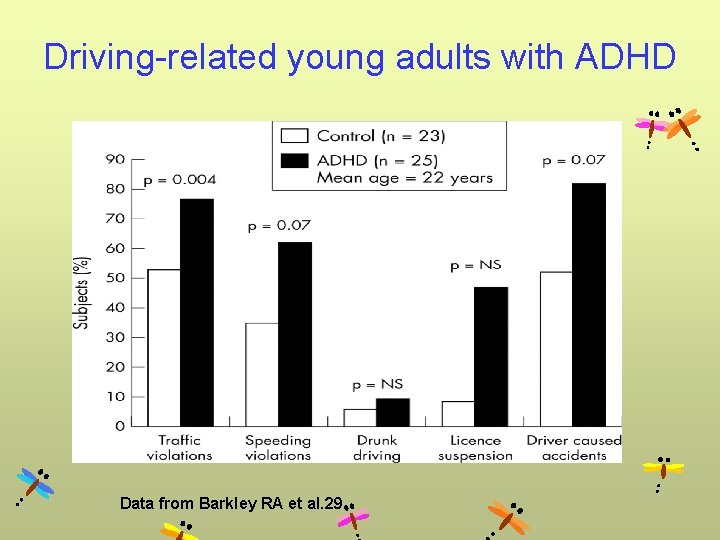
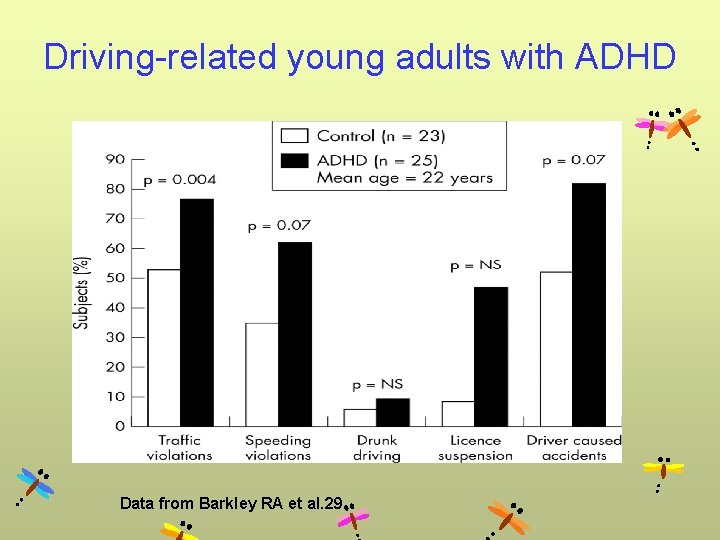
Driving-related young adults with ADHD Data from Barkley RA et al. 29
Neurobiology and Etiology
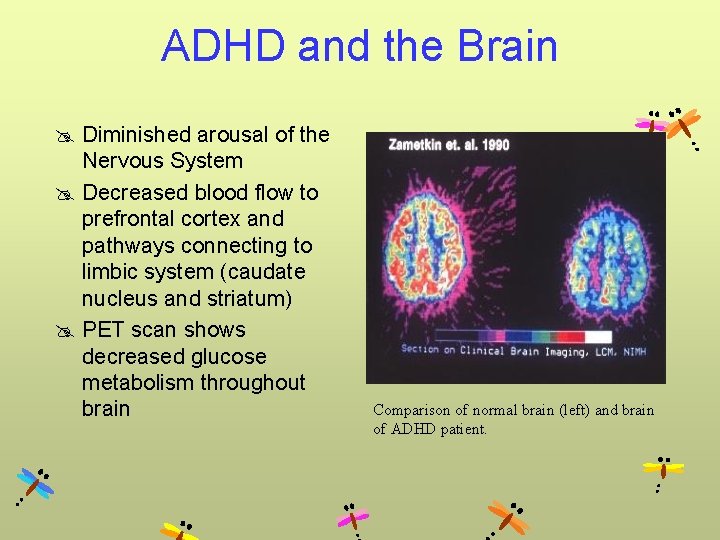
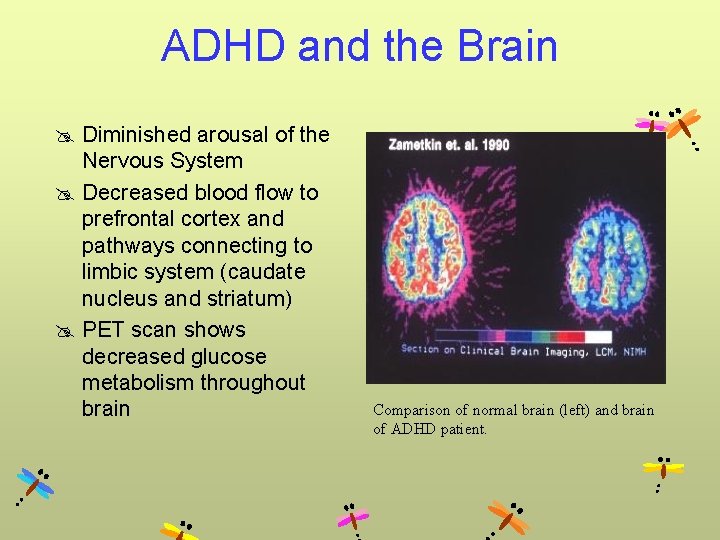
ADHD and the Brain @ Diminished arousal of the Nervous System @ Decreased blood flow to prefrontal cortex and pathways connecting to limbic system (caudate nucleus and striatum) @ PET scan shows decreased glucose metabolism throughout brain Comparison of normal brain (left) and brain of ADHD patient.
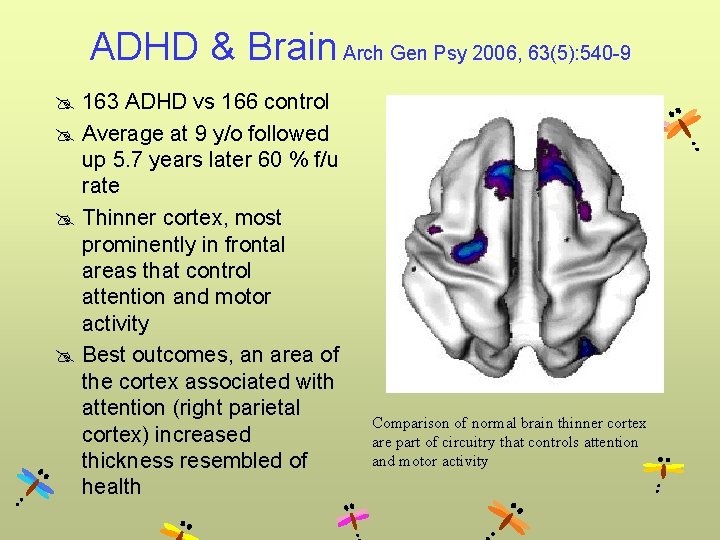
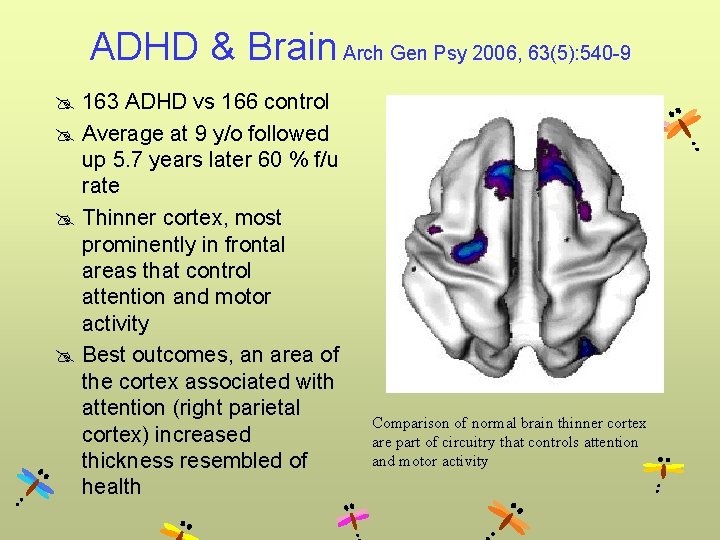
ADHD & Brain Arch Gen Psy 2006, 63(5): 540 -9 @ 163 ADHD vs 166 control @ Average at 9 y/o followed up 5. 7 years later 60 % f/u rate @ Thinner cortex, most prominently in frontal areas that control attention and motor activity @ Best outcomes, an area of the cortex associated with attention (right parietal cortex) increased thickness resembled of health Comparison of normal brain thinner cortex are part of circuitry that controls attention and motor activity
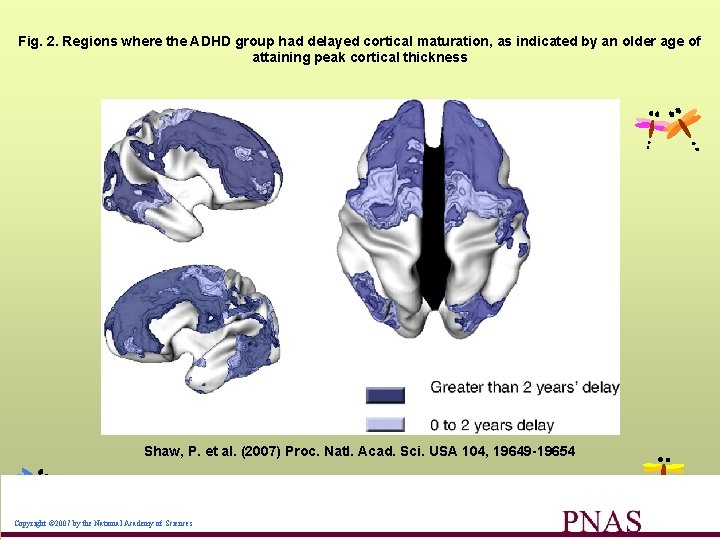
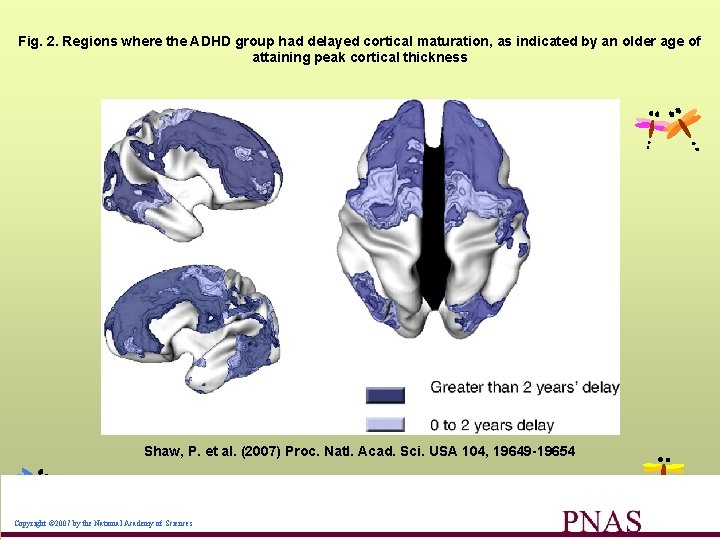
Fig. 2. Regions where the ADHD group had delayed cortical maturation, as indicated by an older age of attaining peak cortical thickness Shaw, P. et al. (2007) Proc. Natl. Acad. Sci. USA 104, 19649 -19654 Copyright © 2007 by the National Academy of Sciences
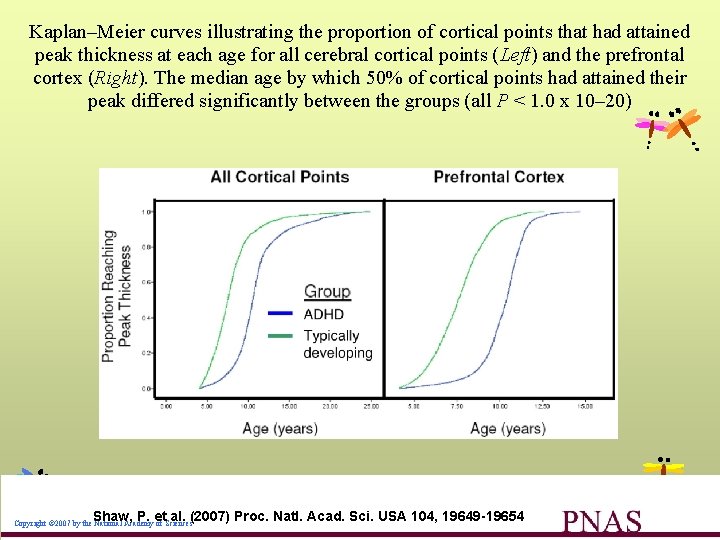
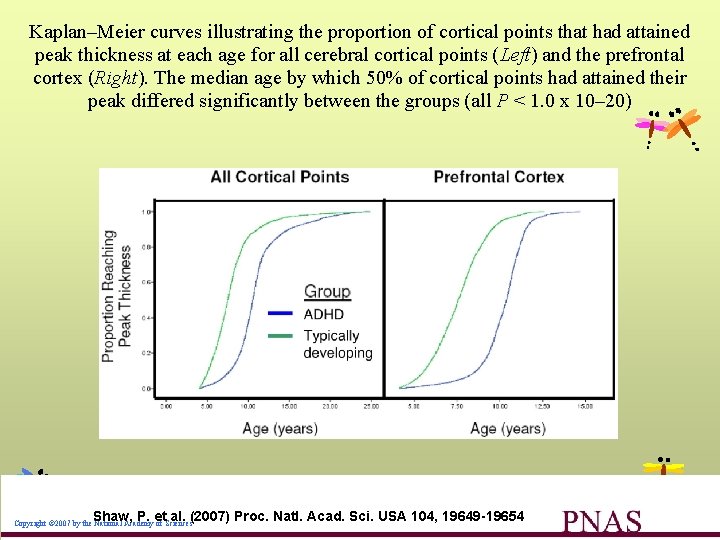
Kaplan–Meier curves illustrating the proportion of cortical points that had attained peak thickness at each age for all cerebral cortical points (Left) and the prefrontal cortex (Right). The median age by which 50% of cortical points had attained their peak differed significantly between the groups (all P < 1. 0 x 10– 20) Shaw, P. et al. (2007) Proc. Natl. Acad. Sci. USA 104, 19649 -19654 Copyright © 2007 by the National Academy of Sciences
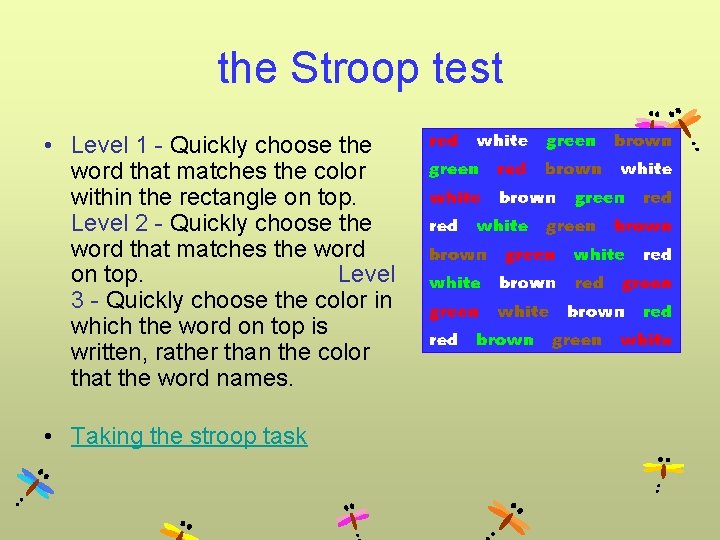
the Stroop test • Level 1 - Quickly choose the word that matches the color within the rectangle on top. Level 2 - Quickly choose the word that matches the word on top. Level 3 - Quickly choose the color in which the word on top is written, rather than the color that the word names. • Taking the stroop task
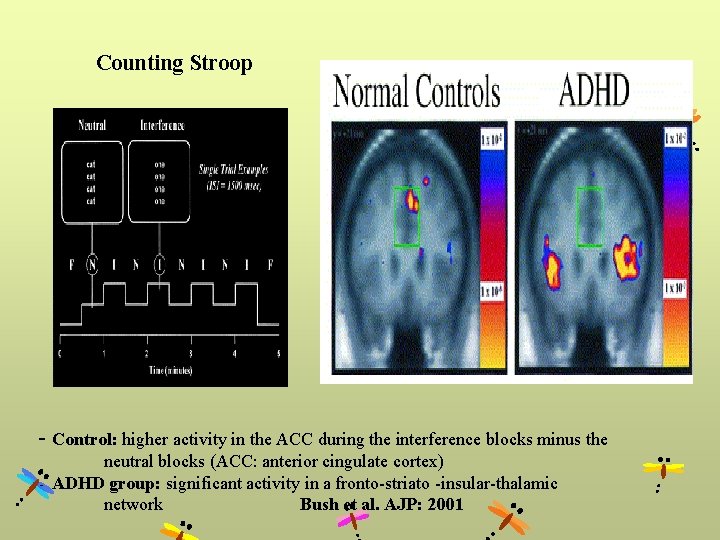
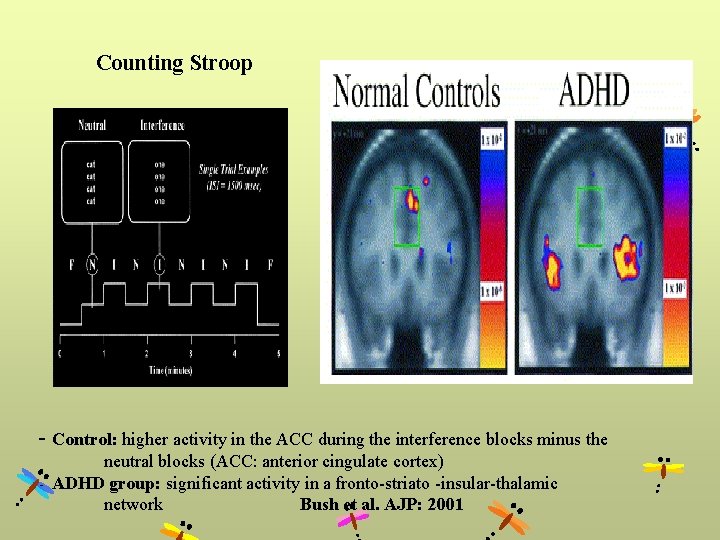
Counting Stroop - Control: higher activity in the ACC during the interference blocks minus the neutral blocks (ACC: anterior cingulate cortex) - ADHD group: significant activity in a fronto-striato -insular-thalamic network Bush et al. AJP: 2001
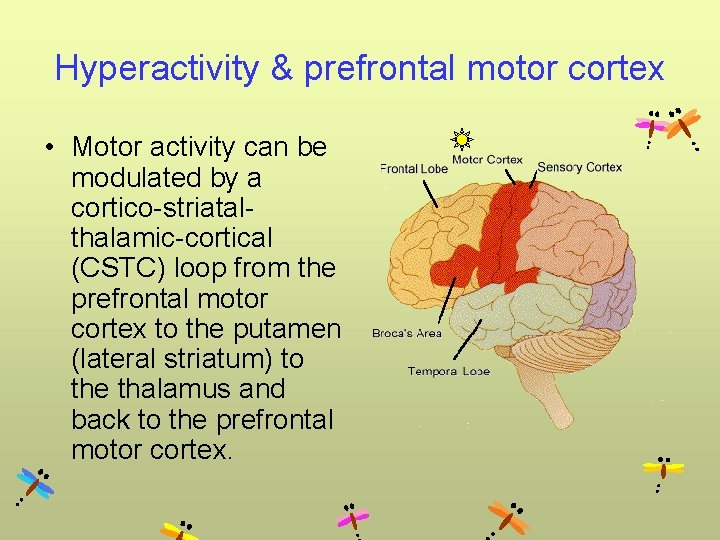
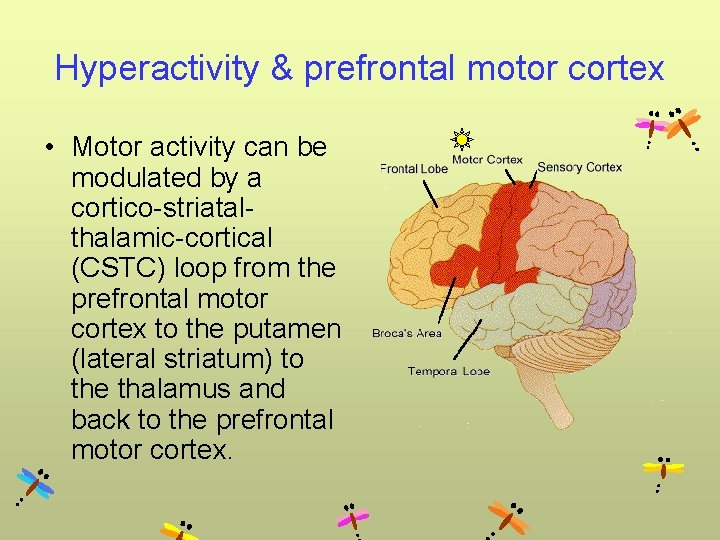
Hyperactivity & prefrontal motor cortex • Motor activity can be modulated by a cortico-striatalthalamic-cortical (CSTC) loop from the prefrontal motor cortex to the putamen (lateral striatum) to the thalamus and back to the prefrontal motor cortex.

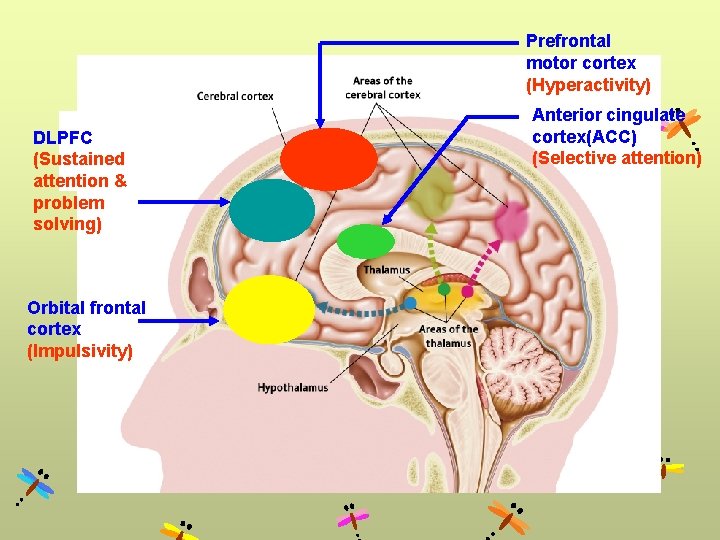
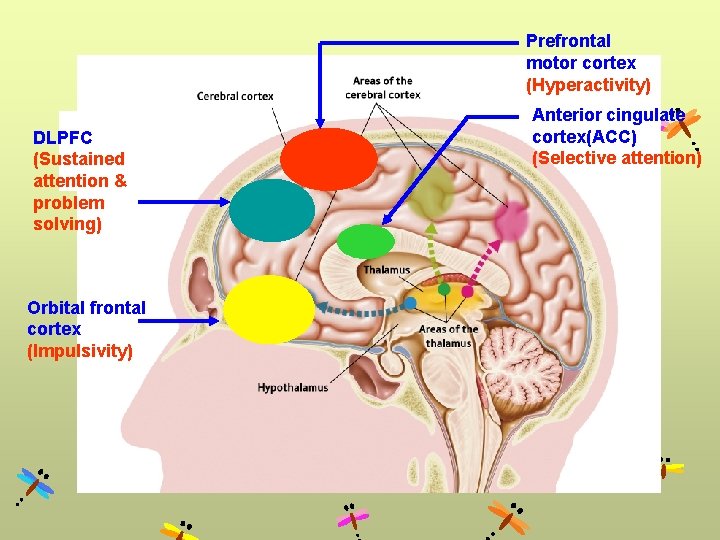
Prefrontal motor cortex (Hyperactivity) DLPFC (Sustained attention & problem solving) Orbital frontal cortex (Impulsivity) Anterior cingulate cortex(ACC) (Selective attention)
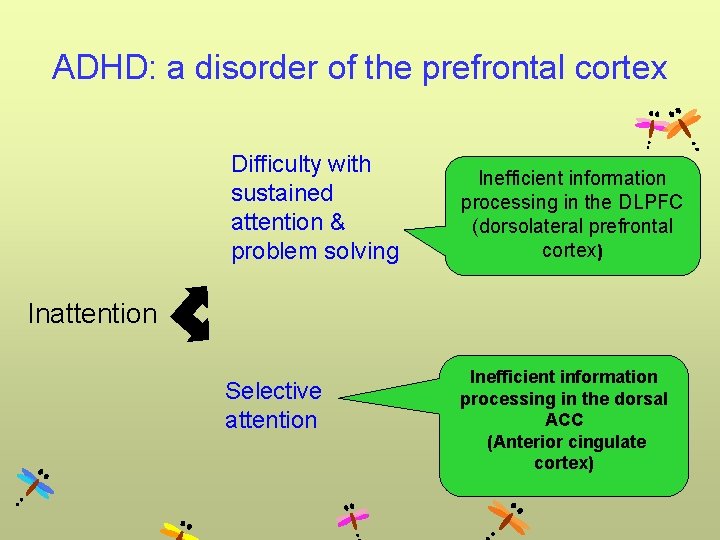
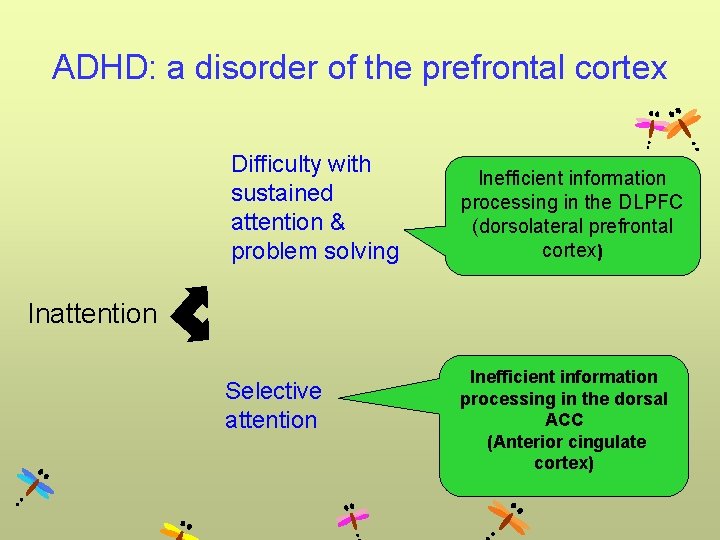
ADHD: a disorder of the prefrontal cortex Difficulty with sustained attention & problem solving Inefficient information processing in the DLPFC (dorsolateral prefrontal cortex) Inattention Selective attention Inefficient information processing in the dorsal ACC (Anterior cingulate cortex)
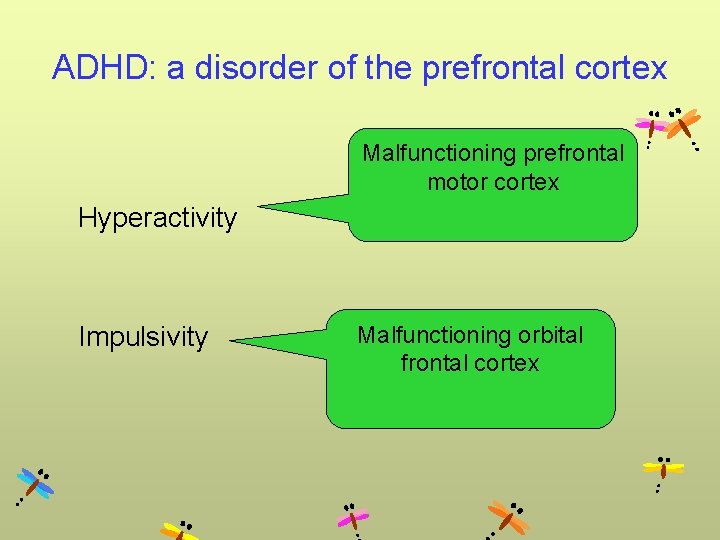
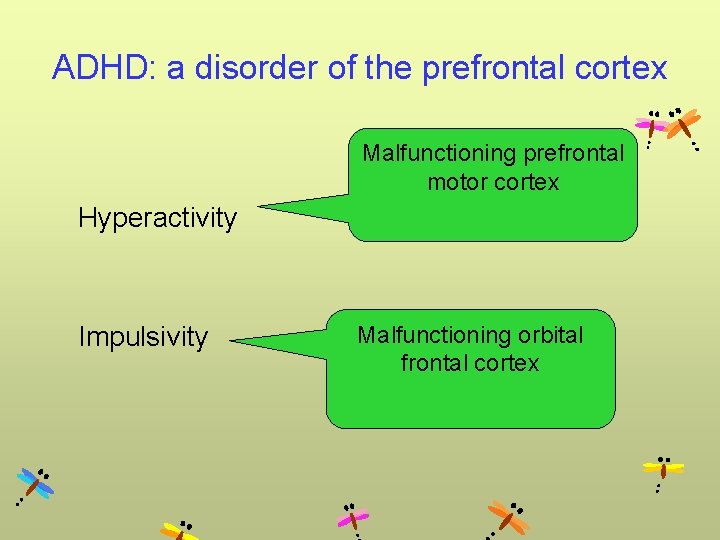
ADHD: a disorder of the prefrontal cortex Malfunctioning prefrontal motor cortex Hyperactivity Impulsivity Malfunctioning orbital frontal cortex
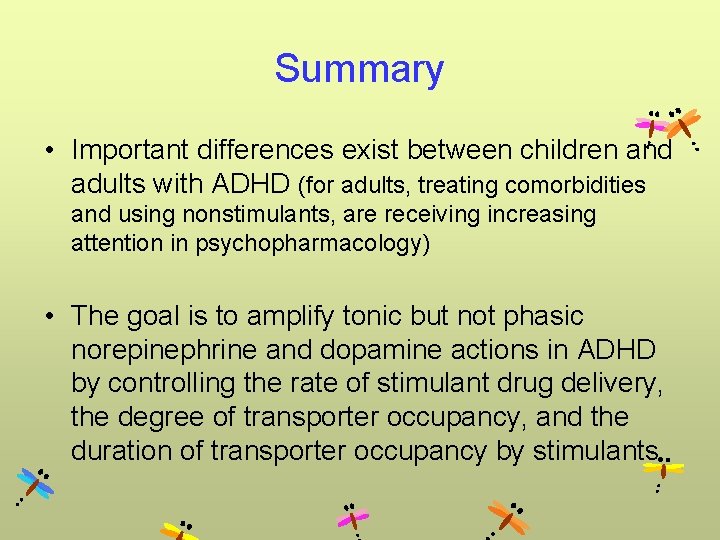
Summary • Important differences exist between children and adults with ADHD (for adults, treating comorbidities and using nonstimulants, are receiving increasing attention in psychopharmacology) • The goal is to amplify tonic but not phasic norepinephrine and dopamine actions in ADHD by controlling the rate of stimulant drug delivery, the degree of transporter occupancy, and the duration of transporter occupancy by stimulants
Neurocognition in ADHD (Neuropsychological Functioning)

Pharmacotherapy for ADHD

Stimulant treatment of ADHD
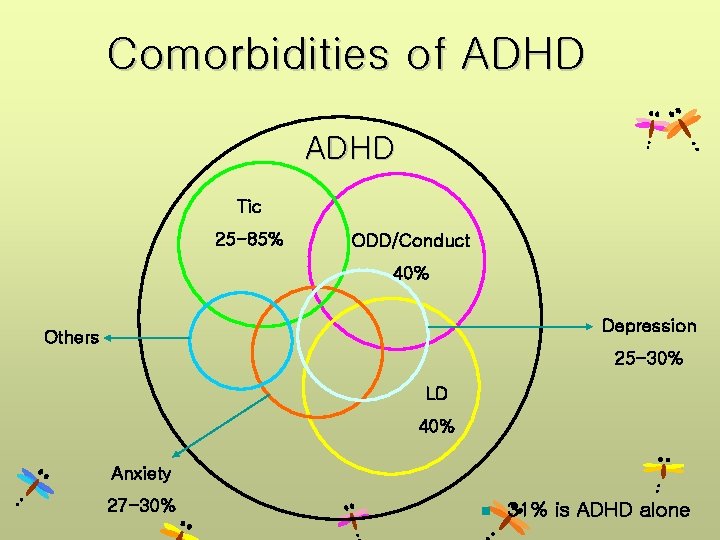
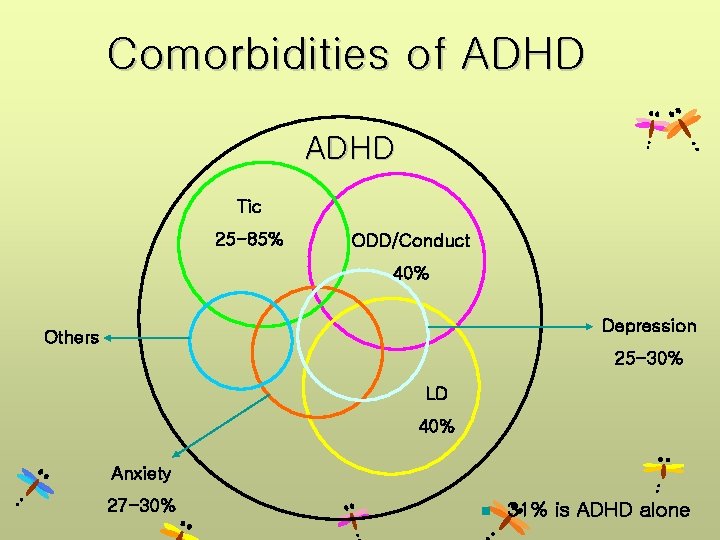
Comorbidities of ADHD Tic 25 -85% ODD/Conduct 40% Depression Others 25 -30% LD 40% Anxiety 27 -30% n 31% is ADHD alone
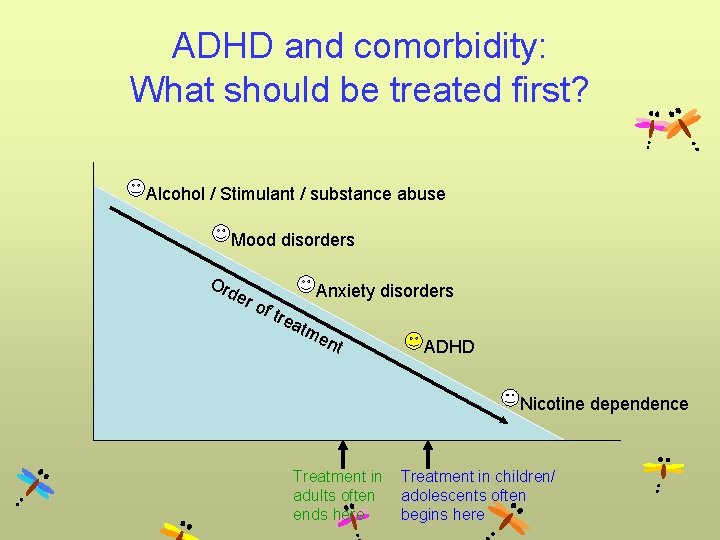
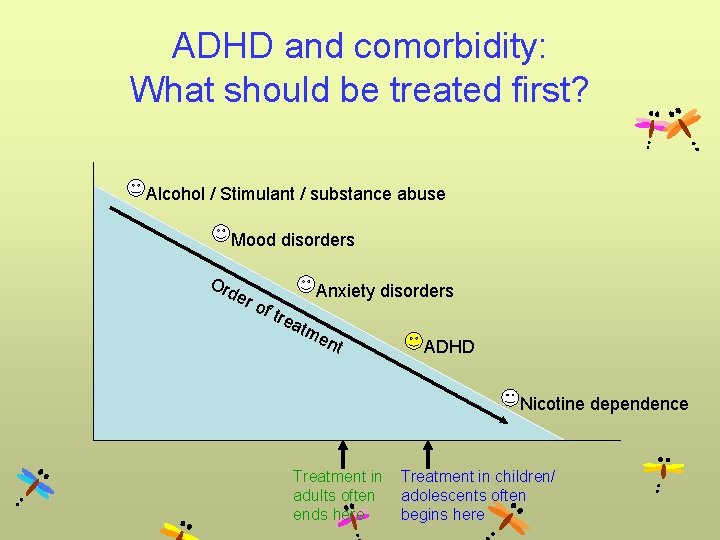
ADHD and comorbidity: What should be treated first? Alcohol / Stimulant / substance abuse Mood disorders Or de r o f tr Anxiety disorders ea tm en t ADHD Nicotine dependence Treatment in children/ adults often adolescents often ends here begins here

Pharmacological agents used in ADHD treatment • First-line: Stimulants – – Methylphenidate Amphetamine compounds Dextroamphetamine Magnesium pemoline • Second line: Antidepressants – Tricyclics, bupropion, atomoxetien • Third line: Alpha 2 Agonist – Clonidine, Guanfacine • Antipsychotics • Research: Cholinergic agents – Unlicensed for treatment of ADHD, only licensed in USA
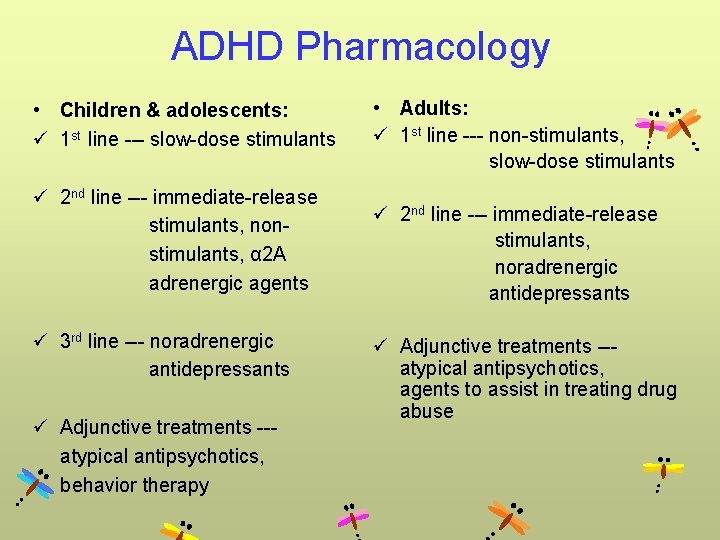
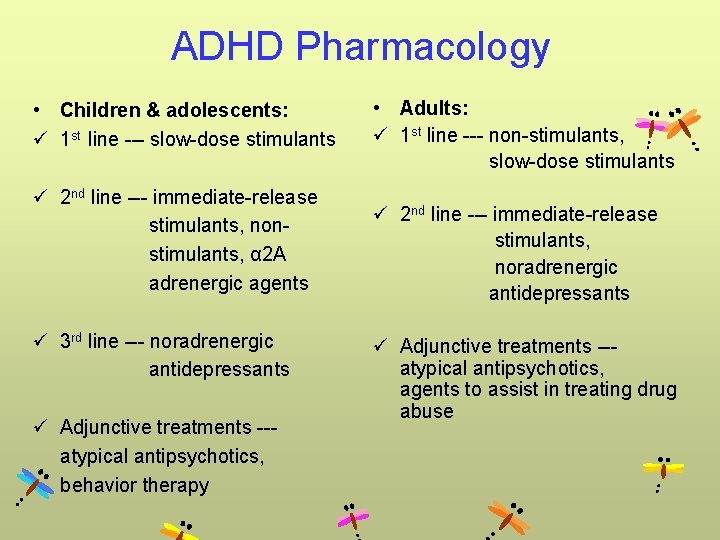
ADHD Pharmacology • Children & adolescents: ü 1 st line --- slow-dose stimulants ü 2 nd line --- immediate-release stimulants, non stimulants, α 2 A adrenergic agents ü 3 rd line --- noradrenergic antidepressants ü Adjunctive treatments --- atypical antipsychotics, behavior therapy • Adults: ü 1 st line --- non-stimulants, slow-dose stimulants ü 2 nd line --- immediate-release stimulants, noradrenergic antidepressants ü Adjunctive treatments --- atypical antipsychotics, agents to assist in treating drug abuse

Methylphenidate
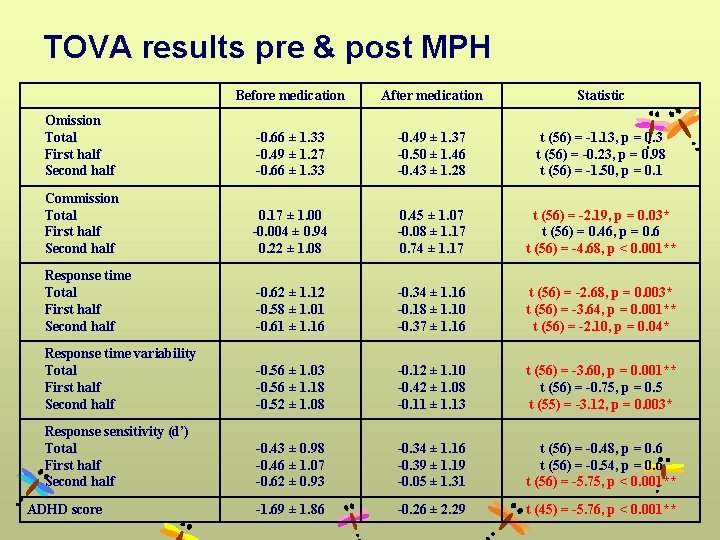
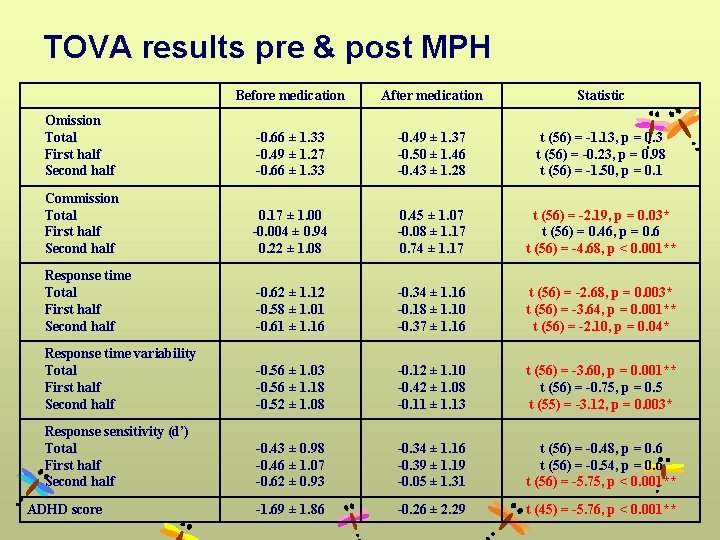
TOVA results pre & post MPH Before medication After medication Statistic Omission Total First half Second half -0. 66 ± 1. 33 -0. 49 ± 1. 27 -0. 66 ± 1. 33 -0. 49 ± 1. 37 -0. 50 ± 1. 46 -0. 43 ± 1. 28 t (56) = -1. 13, p = 0. 3 t (56) = -0. 23, p = 0. 98 t (56) = -1. 50, p = 0. 1 Commission Total First half Second half 0. 17 ± 1. 00 -0. 004 ± 0. 94 0. 22 ± 1. 08 0. 45 ± 1. 07 -0. 08 ± 1. 17 0. 74 ± 1. 17 t (56) = -2. 19, p = 0. 03* t (56) = 0. 46, p = 0. 6 t (56) = -4. 68, p < 0. 001** Response time Total First half Second half -0. 62 ± 1. 12 -0. 58 ± 1. 01 -0. 61 ± 1. 16 -0. 34 ± 1. 16 -0. 18 ± 1. 10 -0. 37 ± 1. 16 t (56) = -2. 68, p = 0. 003* t (56) = -3. 64, p = 0. 001** t (56) = -2. 10, p = 0. 04* Response time variability Total First half Second half -0. 56 ± 1. 03 -0. 56 ± 1. 18 -0. 52 ± 1. 08 -0. 12 ± 1. 10 -0. 42 ± 1. 08 -0. 11 ± 1. 13 t (56) = -3. 60, p = 0. 001** t (56) = -0. 75, p = 0. 5 t (55) = -3. 12, p = 0. 003* Response sensitivity (d’) Total First half Second half -0. 43 ± 0. 98 -0. 46 ± 1. 07 -0. 62 ± 0. 93 -0. 34 ± 1. 16 -0. 39 ± 1. 19 -0. 05 ± 1. 31 t (56) = -0. 48, p = 0. 6 t (56) = -0. 54, p = 0. 6 t (56) = -5. 75, p < 0. 001** -1. 69 ± 1. 86 -0. 26 ± 2. 29 t (45) = -5. 76, p < 0. 001** ADHD score

Atomoxetine


Conclusion • Methylphenidate and atomoxetine were associated with improvement in a variety of neuropsychological functions in ADHD.

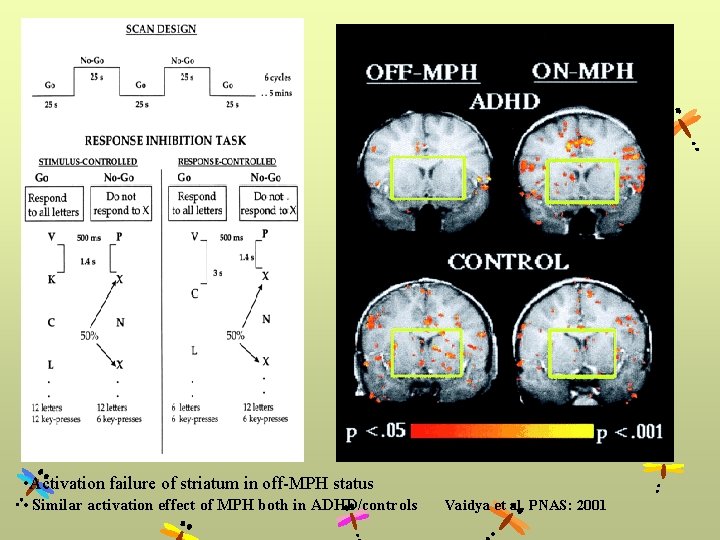
Medication on Neuroimaging
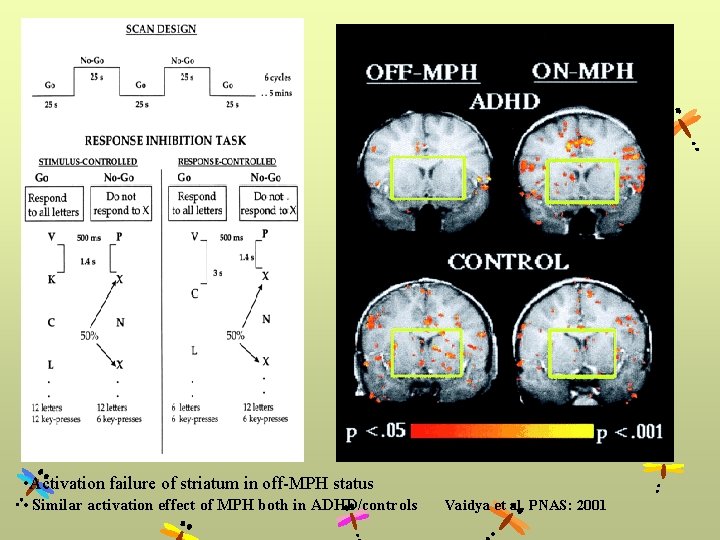
• Activation failure of striatum in off-MPH status • Similar activation effect of MPH both in ADHD/controls Vaidya et al. PNAS: 2001
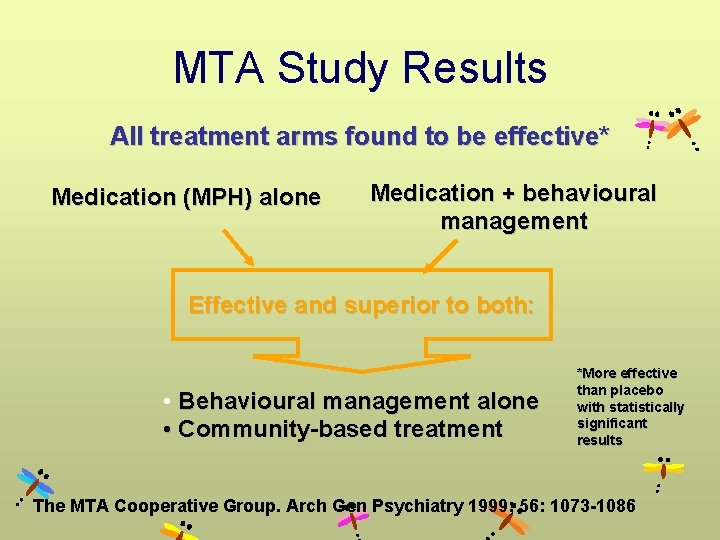
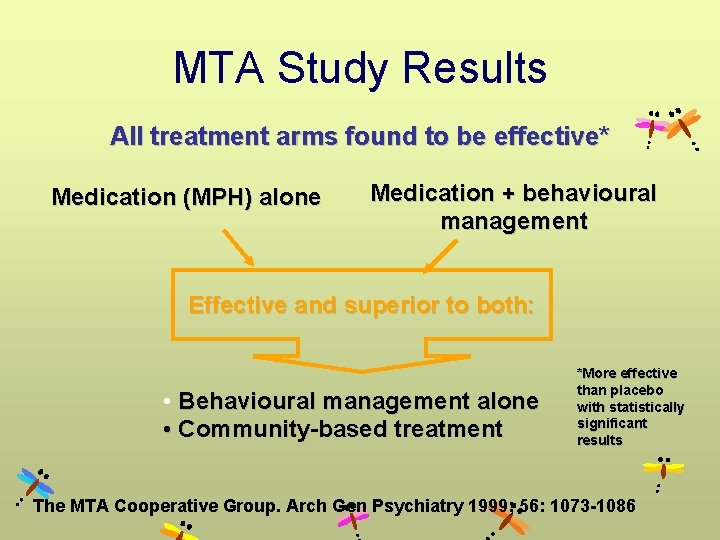
MTA Study Results All treatment arms found to be effective* Medication (MPH) alone Medication + behavioural management Effective and superior to both: • Behavioural management alone • Community-based treatment *More effective than placebo with statistically significant results The MTA Cooperative Group. Arch Gen Psychiatry 1999; 56: 1073 -1086


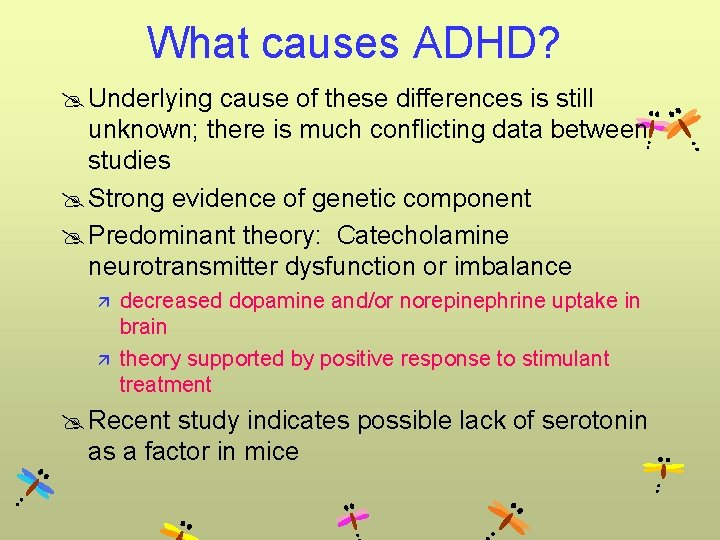
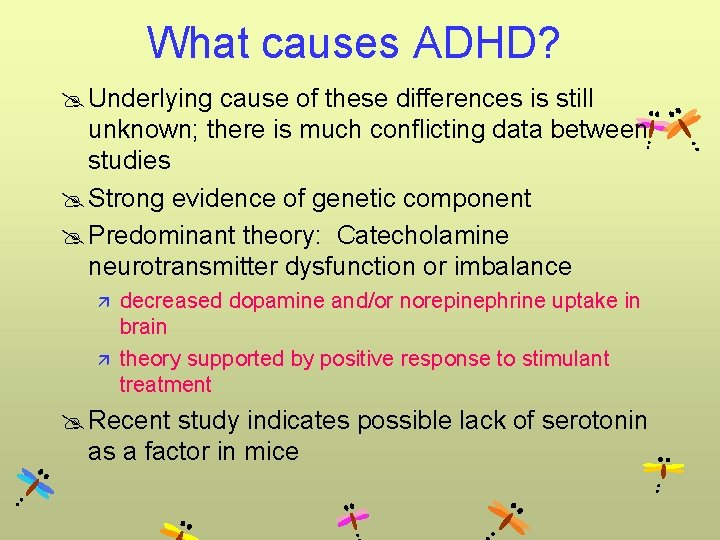
What causes ADHD? @ Underlying cause of these differences is still unknown; there is much conflicting data between studies @ Strong evidence of genetic component @ Predominant theory: Catecholamine neurotransmitter dysfunction or imbalance ä ä decreased dopamine and/or norepinephrine uptake in brain theory supported by positive response to stimulant treatment @ Recent study indicates possible lack of serotonin as a factor in mice
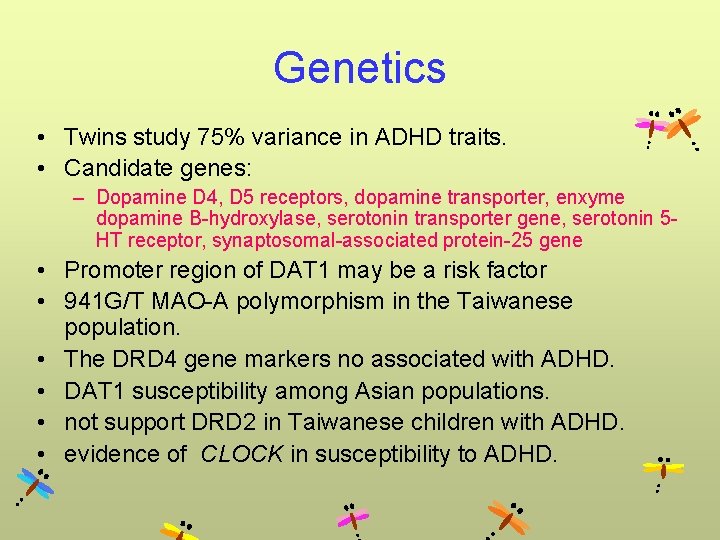
Genetics • Twins study 75% variance in ADHD traits. • Candidate genes: – Dopamine D 4, D 5 receptors, dopamine transporter, enxyme dopamine B-hydroxylase, serotonin transporter gene, serotonin 5 HT receptor, synaptosomal-associated protein-25 gene • Promoter region of DAT 1 may be a risk factor • 941 G/T MAO-A polymorphism in the Taiwanese population. • The DRD 4 gene markers no associated with ADHD. • DAT 1 susceptibility among Asian populations. • not support DRD 2 in Taiwanese children with ADHD. • evidence of CLOCK in susceptibility to ADHD.
Environmental factors • Perinatal stress, low birth weight, severe traumatic brain injury, maternal smoking, exposure to lead, severe early social deprivation • Psychosocial adversity (maternal mental disorder, paternal criminality, chaotic home) • Carrying the dopamine transporter gene, D 4 receptor, nicotinic acetylcholine receptor


Thank you for your attention!
 Emirato dependiente de damasco
Emirato dependiente de damasco 171 nomreli mekteb
171 nomreli mekteb 171 nomreli mekteb
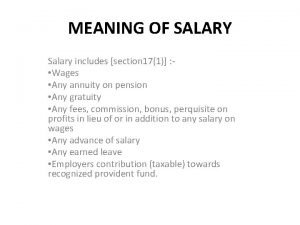
171 nomreli mekteb Tax allowance meaning
Tax allowance meaning Hazardous material table
Hazardous material table 171
171 171 nomreli mekteb
171 nomreli mekteb Pg 171
Pg 171 Cs 171 uci
Cs 171 uci Ai 171
Ai 171 171 nomreli mekteb
171 nomreli mekteb Lei 171 de 2007
Lei 171 de 2007 171 in binary
171 in binary Ai 171
Ai 171 Decret 171/2015
Decret 171/2015 The verbs salir decir and venir p.155
The verbs salir decir and venir p.155 Flynn effect psychology
Flynn effect psychology Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Iho s-102
Iho s-102 Opord format
Opord format 102 graphic
102 graphic Sinak s102
Sinak s102 Gauss law statement
Gauss law statement Pulser
Pulser 109 prime number
109 prime number Ka 102
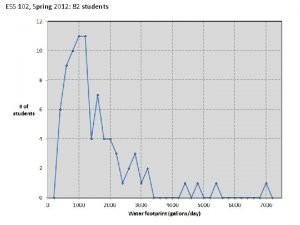
Ka 102 Ess 102 uw
Ess 102 uw Tc 7-102
Tc 7-102 Ni 23-102
Ni 23-102 102 capacitor
102 capacitor Physics 102
Physics 102 Cse 102
Cse 102 48 elmanın çeyreği kaç elma eder
48 elmanın çeyreği kaç elma eder Uiuc physics 102
Uiuc physics 102 Lisa weaver
Lisa weaver Emil ruder
Emil ruder Im 102 portable tank
Im 102 portable tank Iat 102
Iat 102 Dom 102
Dom 102 ?3305501049 0000 28|.|091 27|.|071 98|.|553 102|.|311 13`
?3305501049 0000 28|.|091 27|.|071 98|.|553 102|.|311 13` Find x
Find x Bct 102
Bct 102 Eng 102 bilkent
Eng 102 bilkent Introduction to business notes
Introduction to business notes Ess 102
Ess 102 Hum 102
Hum 102 Psalms 102 niv
Psalms 102 niv Comp 102
Comp 102 Bisc 102 sfu
Bisc 102 sfu Info 102
Info 102 George carlin philosophy
George carlin philosophy 35 usc 102e
35 usc 102e 102 cube
102 cube Cse 102
Cse 102 Hum 102
Hum 102 Ds-102
Ds-102 Asp 102
Asp 102 Csc 102 pdf
Csc 102 pdf 101 102 103
101 102 103 Nur 102
Nur 102 Physics 102
Physics 102 Cs 102 midterm
Cs 102 midterm