428207110 Patient developed acute and chronic renal failure







- Slides: 39

#428207110 • Patient developed acute and chronic renal failure in 1999 associated with a renal stone. History, and a diagnosis of chronic pyelonephritis. She was started on peritoneal dialysis. • Laparoscopic left nephrectomy was performed in June 2000 for retained stones.
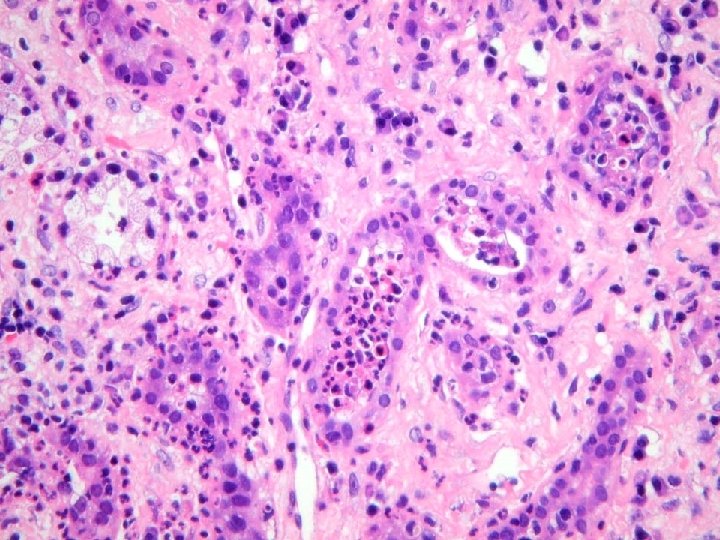
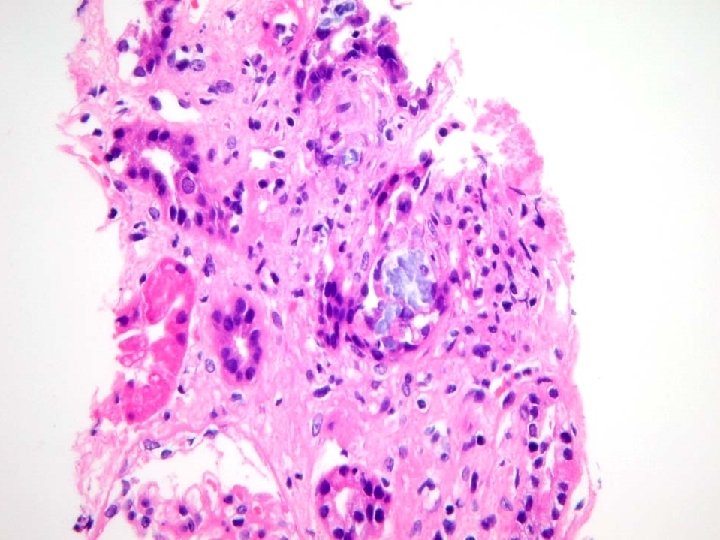
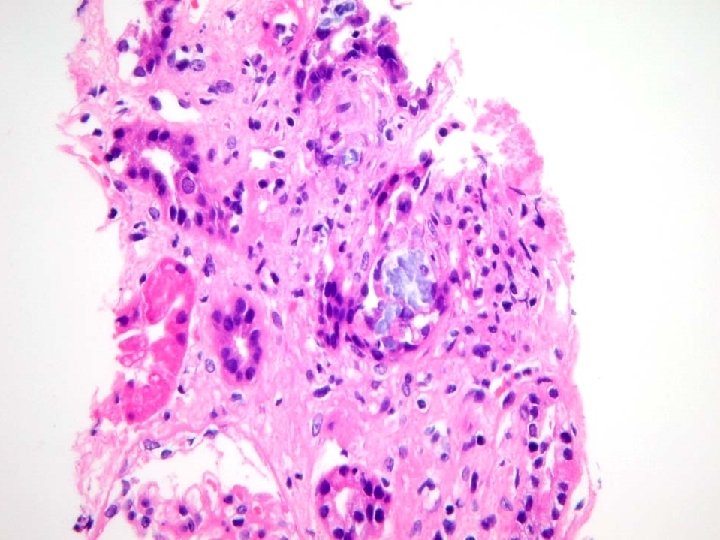
S 00 -45788 Left kidney, fragmentary removal: • End-stage kidney – Chronic tubulointerstitial inflammation and scarring, consistent with obstruction and/or pyelonephritis. – Marked parenchymal crystal deposits, probably secondary oxalate deposition.
« The findings here are probably secondary oxalosis on the basis of chronic renal failure, although I concede that the degree of crystal deposition is exceptional. I should add that there are congenital metabolic errors which usually lead to massive levels of oxalate retention in tissues, but these usually lead to end-stage renal disease before the age of 20. »
• LRD kidney transplant was performed October 25, 2000. • Rising creatinine about 2 months later lead to transplant biopsy • Demonstration of crystals which lead to investigations resulting in diagnosis of primary oxaluria (type I) • Creatinine continue to rise.
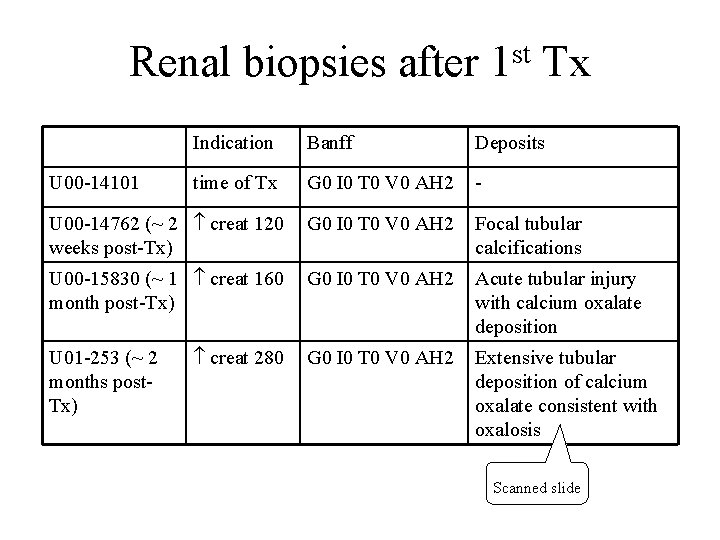
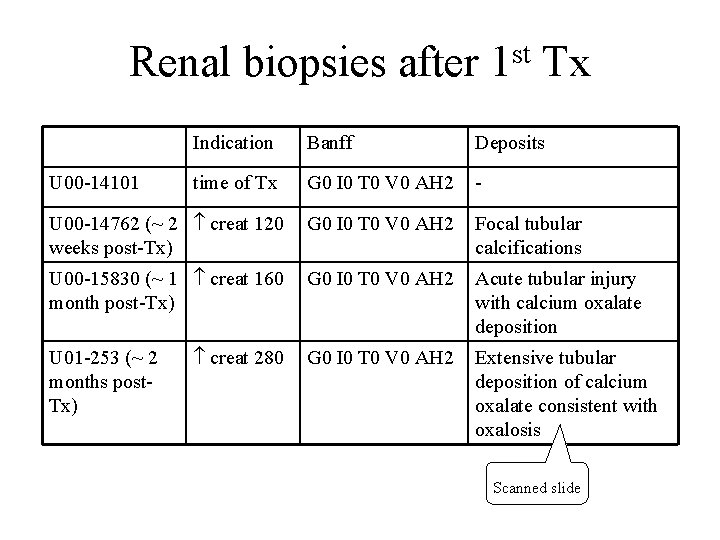
st Renal biopsies after 1 Tx Indication Banff Deposits time of Tx G 0 I 0 T 0 V 0 AH 2 - U 00 -14762 (~ 2 creat 120 weeks post-Tx) G 0 I 0 T 0 V 0 AH 2 Focal tubular calcifications U 00 -15830 (~ 1 creat 160 month post-Tx) G 0 I 0 T 0 V 0 AH 2 Acute tubular injury with calcium oxalate deposition creat 280 G 0 I 0 T 0 V 0 AH 2 Extensive tubular deposition of calcium oxalate consistent with oxalosis U 00 -14101 U 01 -253 (~ 2 months post. Tx) Scanned slide
• Combined liver/kidney transplant June 21, 2003 with initial serum creatinine of 80 µmol/L. • First post transplant biopsy done when creatinine rose to 120 µmol/L
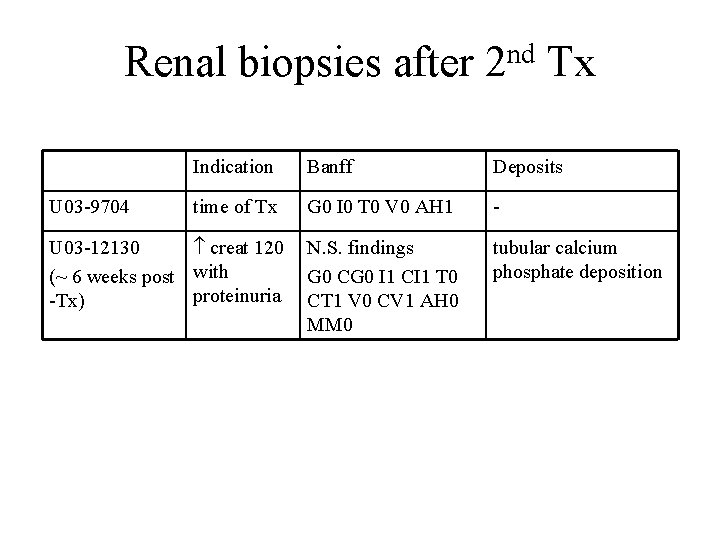
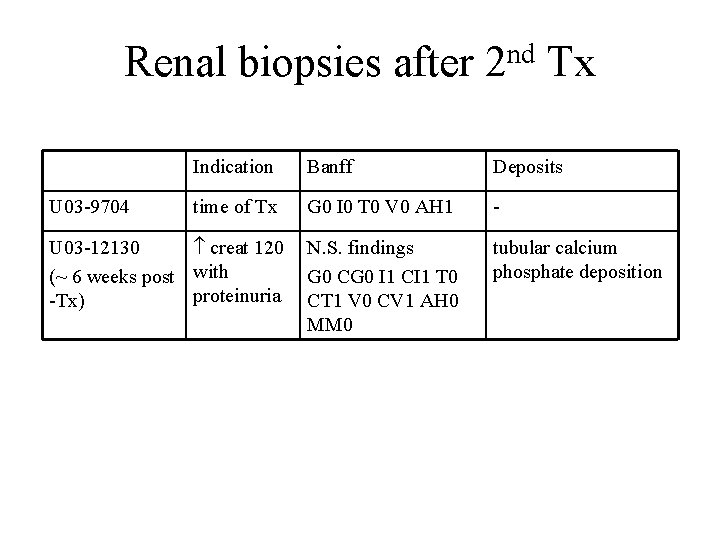
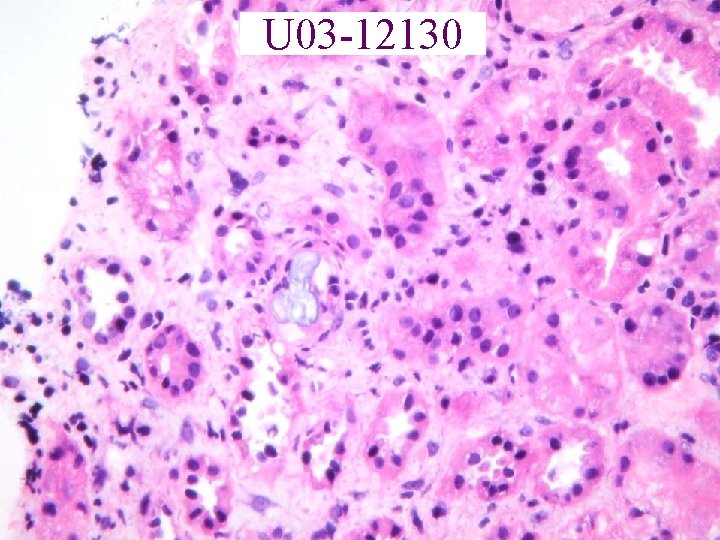
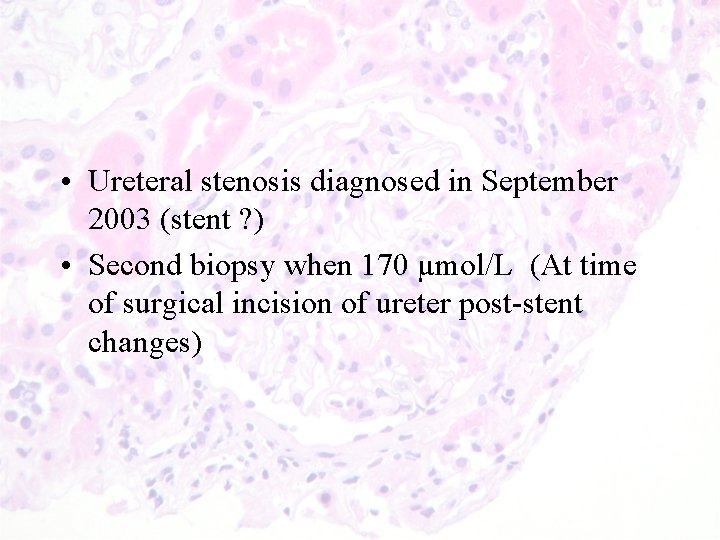
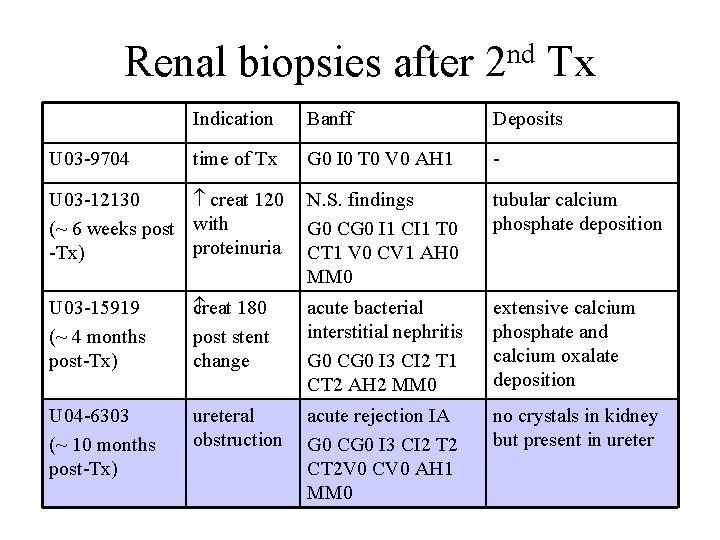
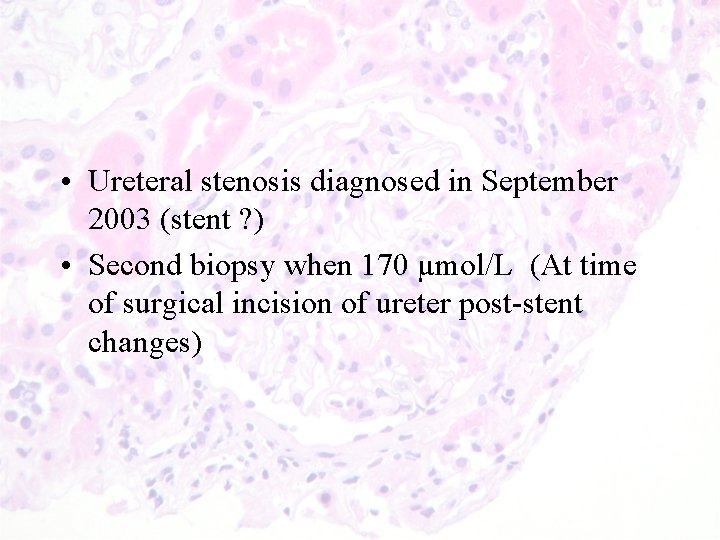
nd Renal biopsies after 2 Tx U 03 -9704 Indication Banff Deposits time of Tx G 0 I 0 T 0 V 0 AH 1 - U 03 -12130 creat 120 N. S. findings (~ 6 weeks post with G 0 CG 0 I 1 CI 1 T 0 proteinuria CT 1 V 0 CV 1 AH 0 -Tx) MM 0 tubular calcium phosphate deposition
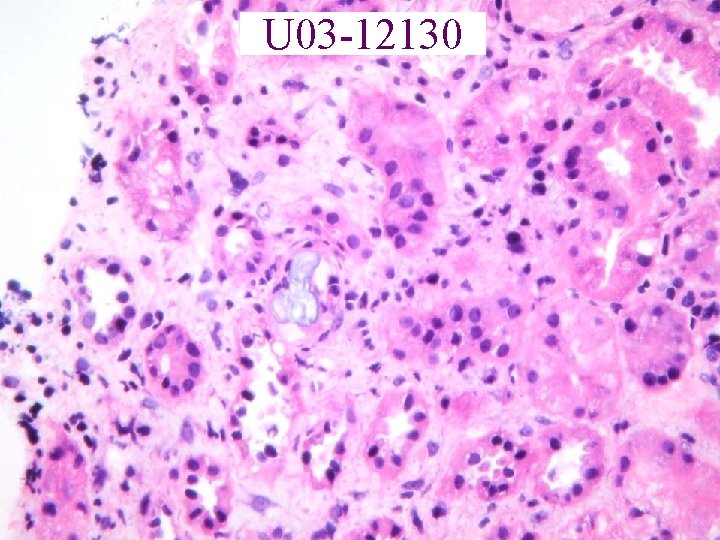
U 03 -12130
• Ureteral stenosis diagnosed in September 2003 (stent ? ) • Second biopsy when 170 µmol/L (At time of surgical incision of ureter post-stent changes)
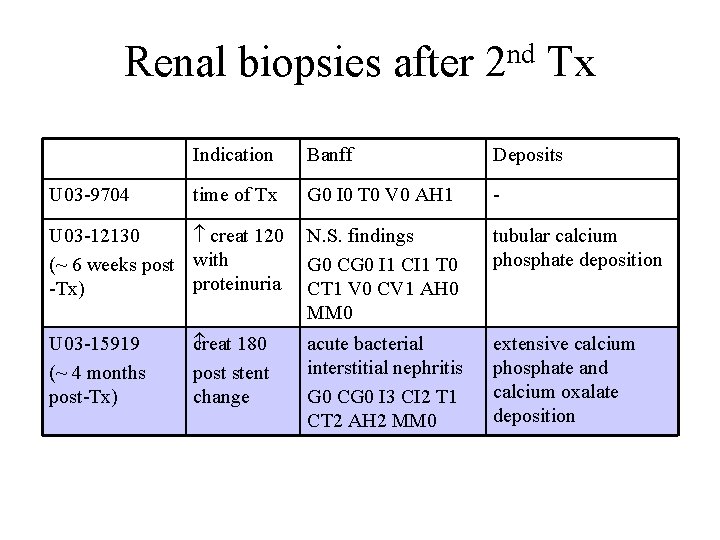
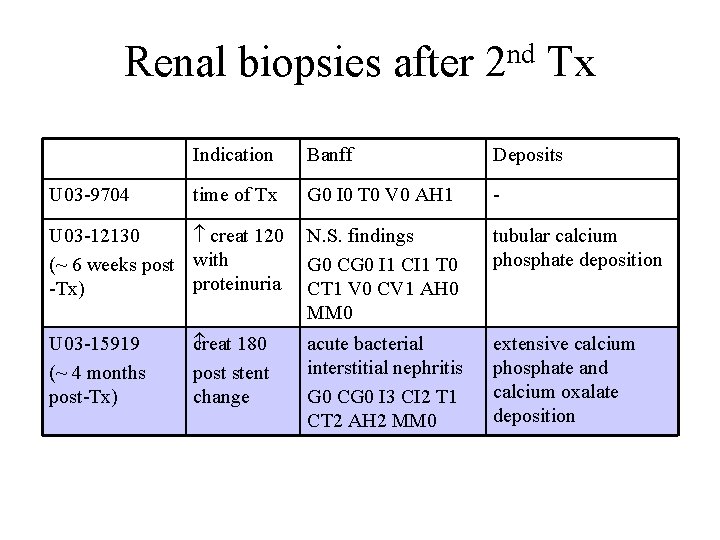
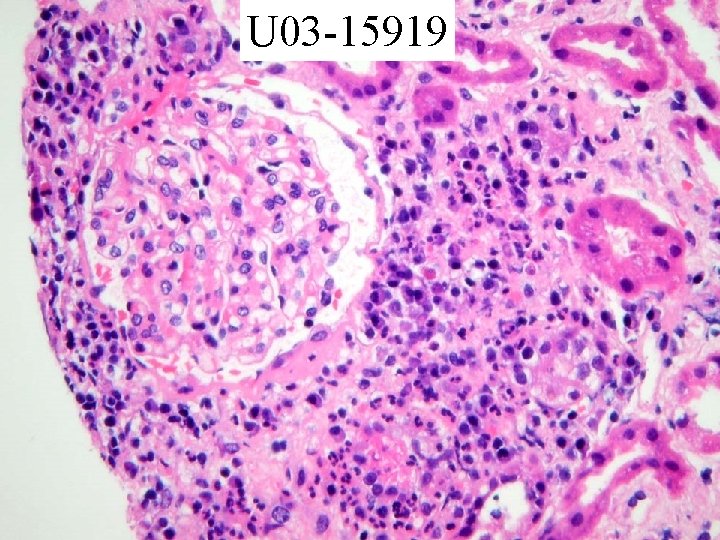
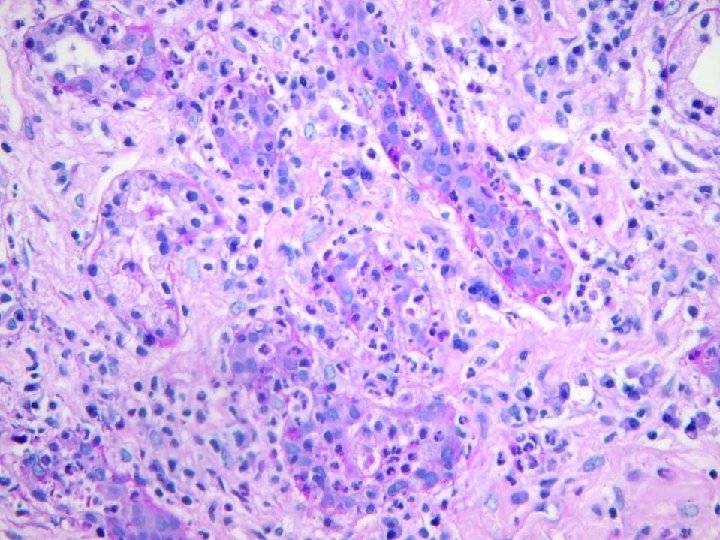
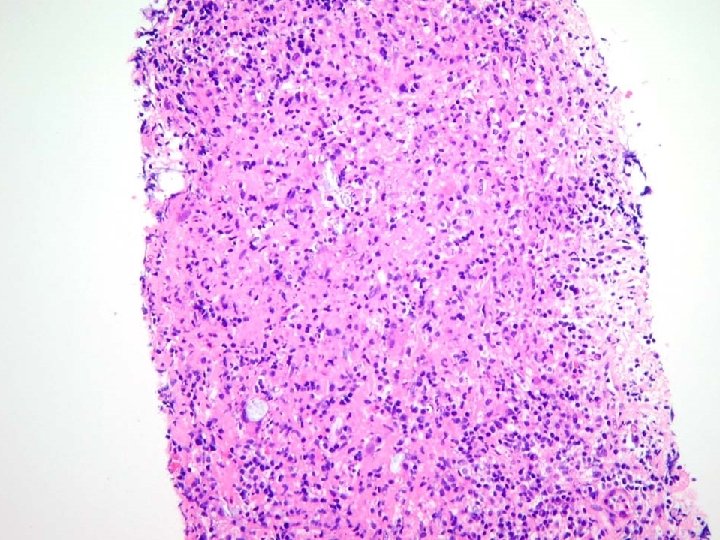
nd Renal biopsies after 2 Tx U 03 -9704 Indication Banff Deposits time of Tx G 0 I 0 T 0 V 0 AH 1 - U 03 -12130 creat 120 N. S. findings (~ 6 weeks post with G 0 CG 0 I 1 CI 1 T 0 proteinuria CT 1 V 0 CV 1 AH 0 -Tx) MM 0 U 03 -15919 (~ 4 months post-Tx) c reat 180 post stent change acute bacterial interstitial nephritis G 0 CG 0 I 3 CI 2 T 1 CT 2 AH 2 MM 0 tubular calcium phosphate deposition extensive calcium phosphate and calcium oxalate deposition
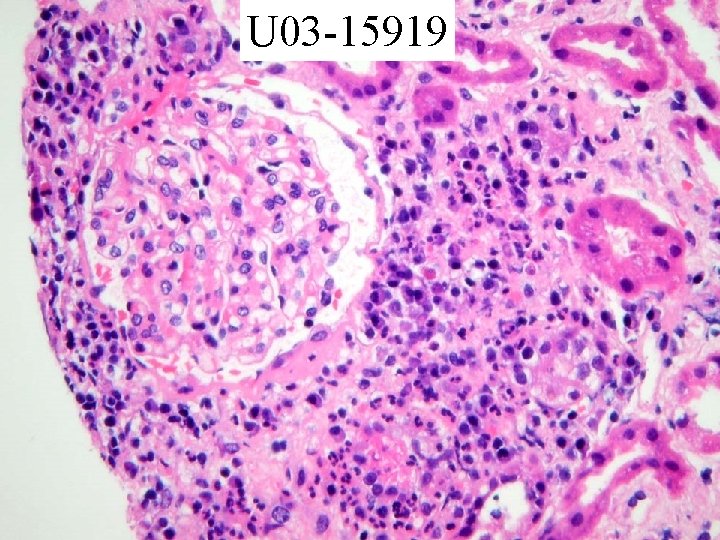
U 03 -15919
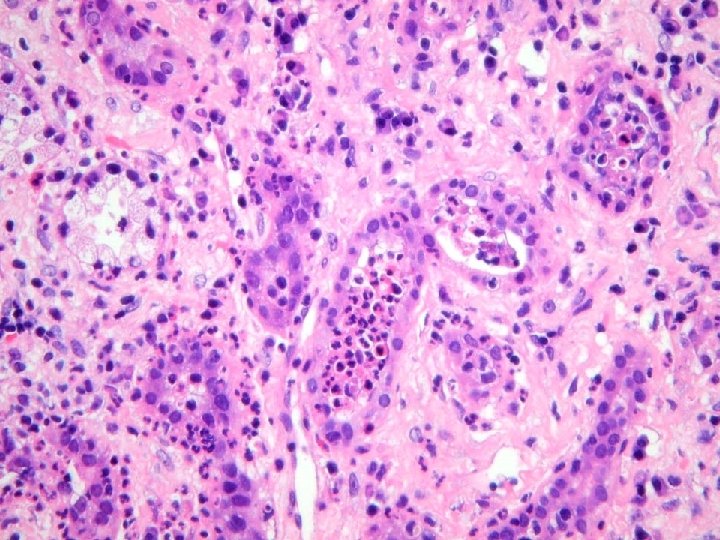
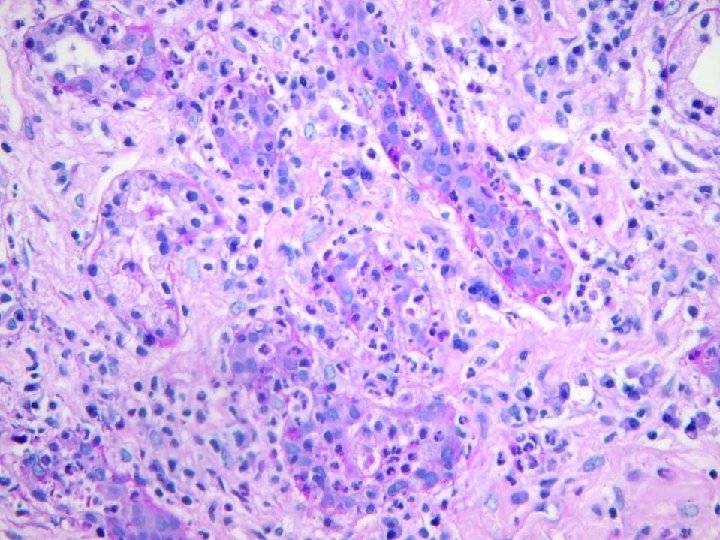


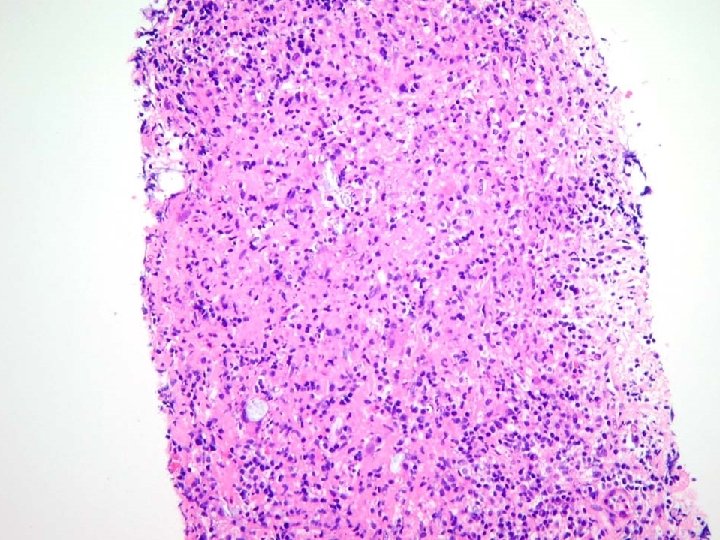
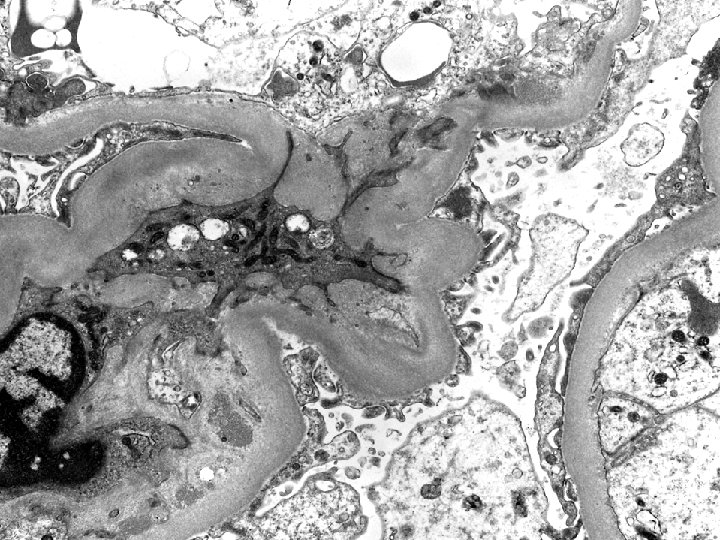
IF • Cytoplasmic staining of plasma cells for Ig. G, kappa, lambda
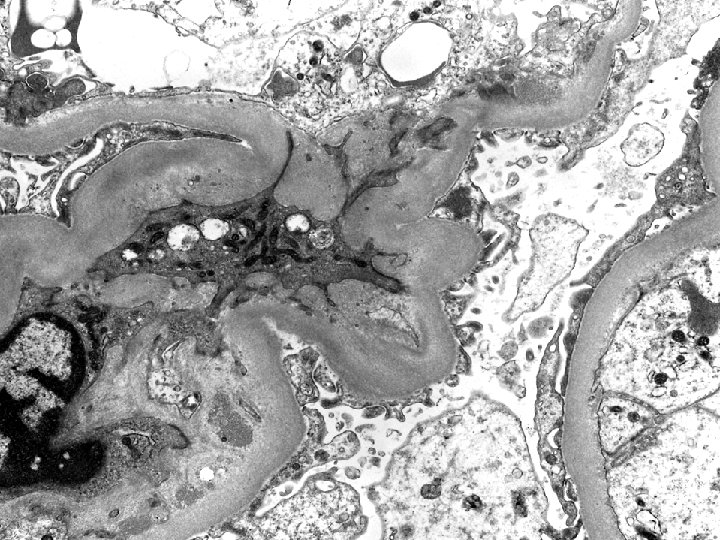
Diagnosis Renal Biopsy: • Acute bacterial interstitial nephritis with pus casts probably on the basis of partial ureteral obstruction by calcium oxalate debris. • Tubular deposition of calcific debris, both calcium phosphate and calcium oxalate. • Possible subclinical immune complex glomerulonephritis. • No evidence of rejection. • (G 0 CG 0 I 3 CI 2 T 1 CT 2 V- CV- AH 2 MM 0)
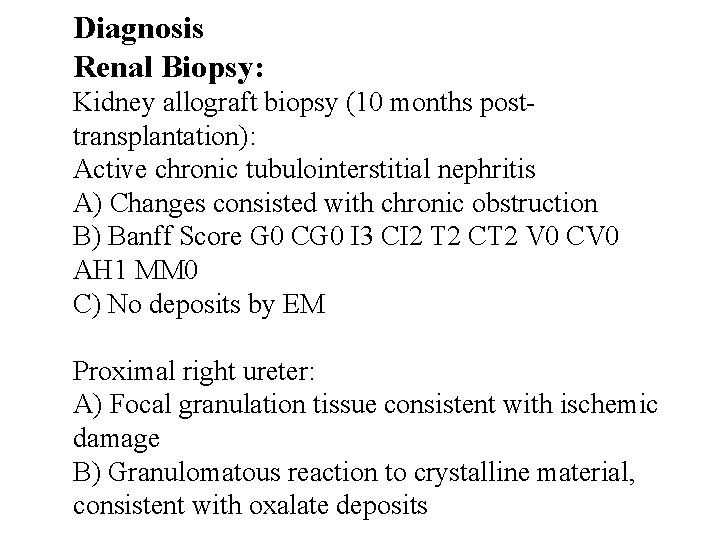
April 2004 • Obstructed renal transplant secondary to ischemic ureter ? • Portions of transplant ureter (proximal ureter) surgically removed + transplant biopsy.
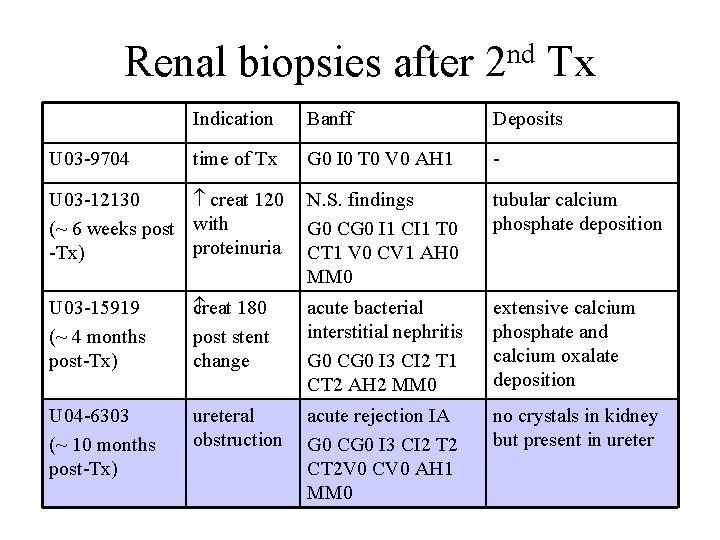
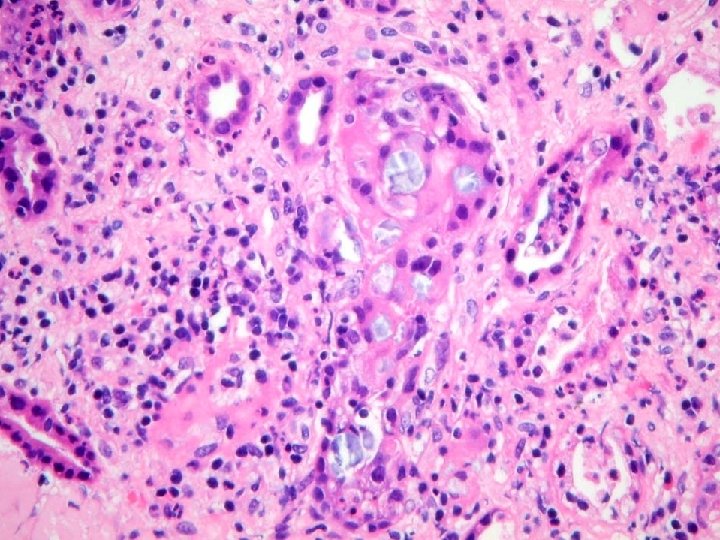
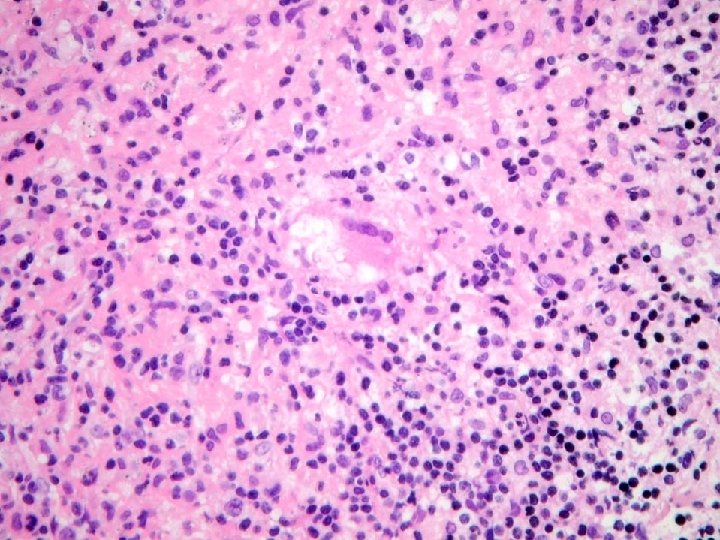
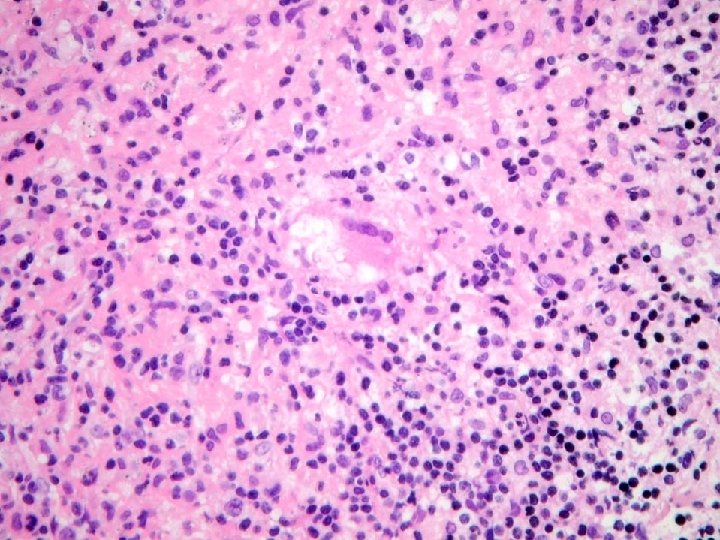
nd Renal biopsies after 2 Tx U 03 -9704 Indication Banff Deposits time of Tx G 0 I 0 T 0 V 0 AH 1 - U 03 -12130 creat 120 N. S. findings (~ 6 weeks post with G 0 CG 0 I 1 CI 1 T 0 proteinuria CT 1 V 0 CV 1 AH 0 -Tx) MM 0 tubular calcium phosphate deposition U 03 -15919 (~ 4 months post-Tx) c reat 180 post stent change acute bacterial interstitial nephritis G 0 CG 0 I 3 CI 2 T 1 CT 2 AH 2 MM 0 extensive calcium phosphate and calcium oxalate deposition U 04 -6303 (~ 10 months post-Tx) ureteral obstruction acute rejection IA G 0 CG 0 I 3 CI 2 T 2 CT 2 V 0 CV 0 AH 1 MM 0 no crystals in kidney but present in ureter




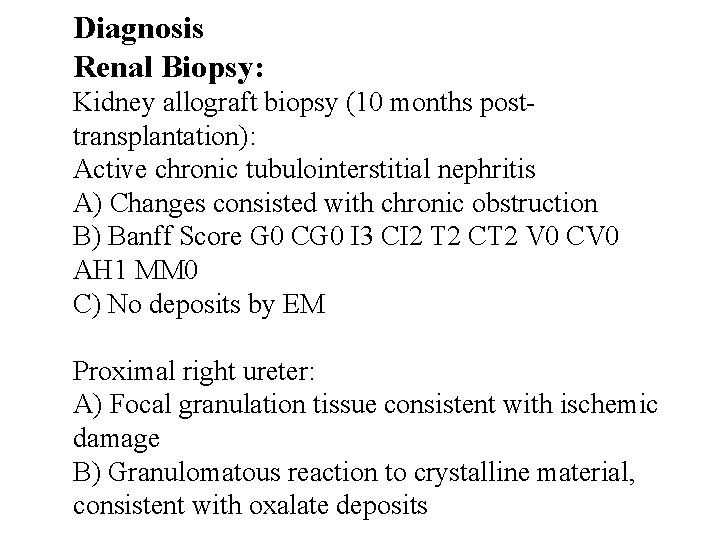
Diagnosis Renal Biopsy: Kidney allograft biopsy (10 months posttransplantation): Active chronic tubulointerstitial nephritis A) Changes consisted with chronic obstruction B) Banff Score G 0 CG 0 I 3 CI 2 T 2 CT 2 V 0 CV 0 AH 1 MM 0 C) No deposits by EM Proximal right ureter: A) Focal granulation tissue consistent with ischemic damage B) Granulomatous reaction to crystalline material, consistent with oxalate deposits
• Following her biopsy in April 2004 (with imaging studies documenting ureteral obstruction despite stent) at the time of surgical ureteral repair, she returned home and serum creatinine settled to the 130 -140 mol/L range. • On prednisone 5 mg daily, cellcept 500 mg bid, tacrolimus 3 mg bid, and other meds.
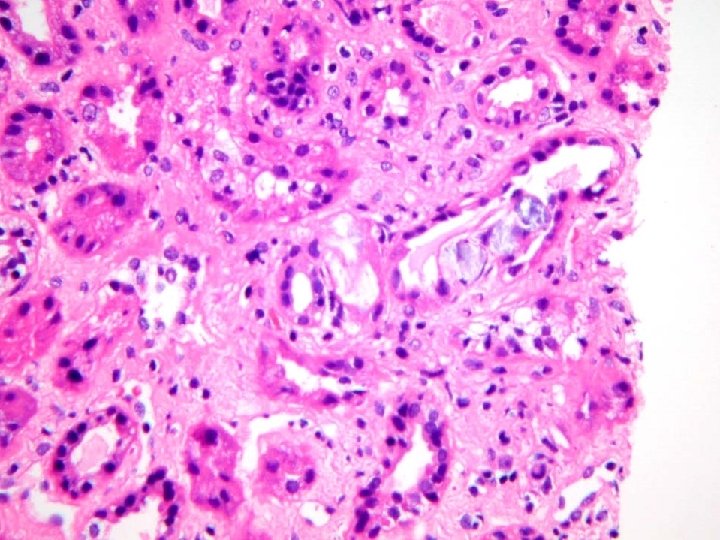
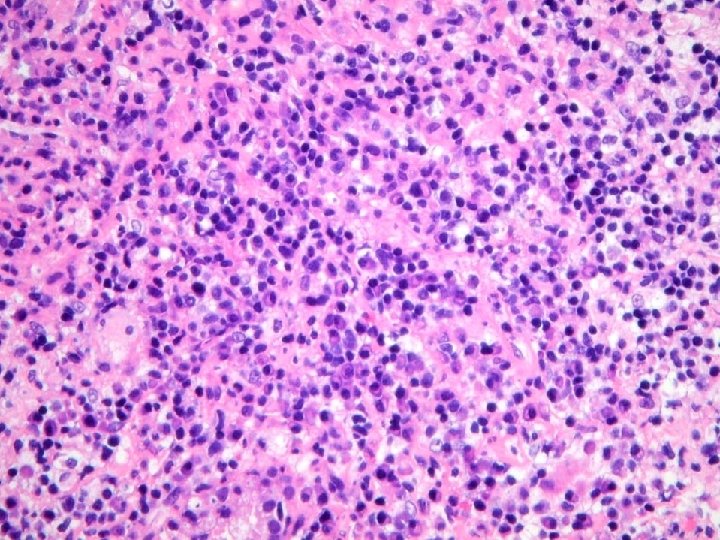
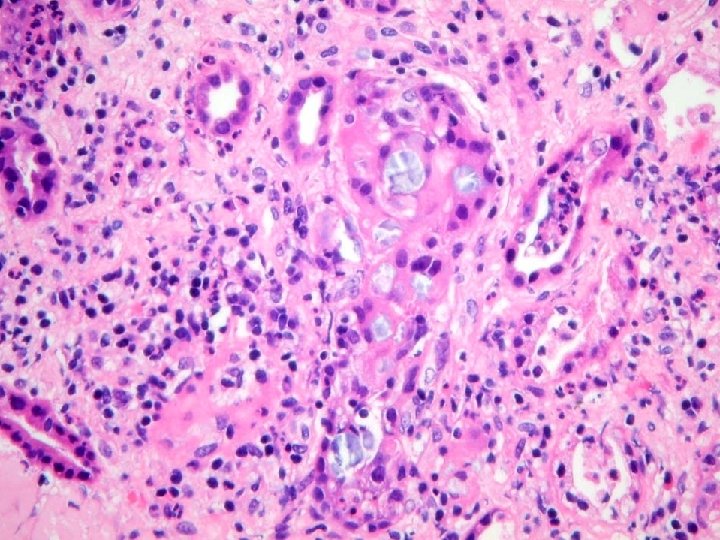
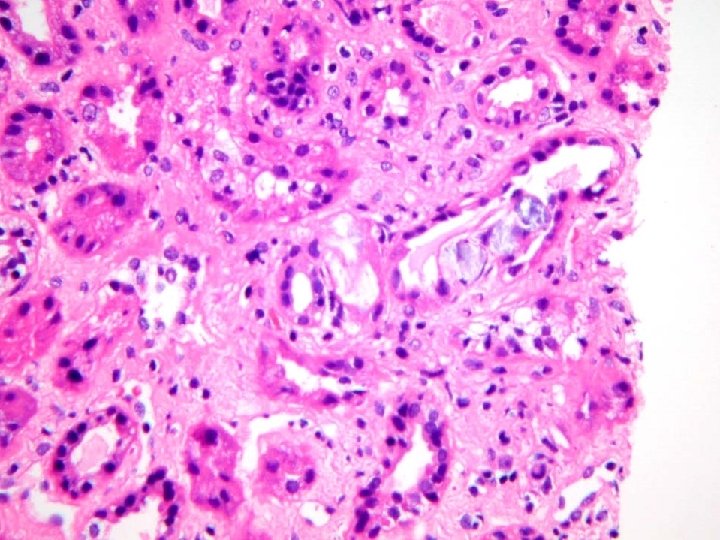
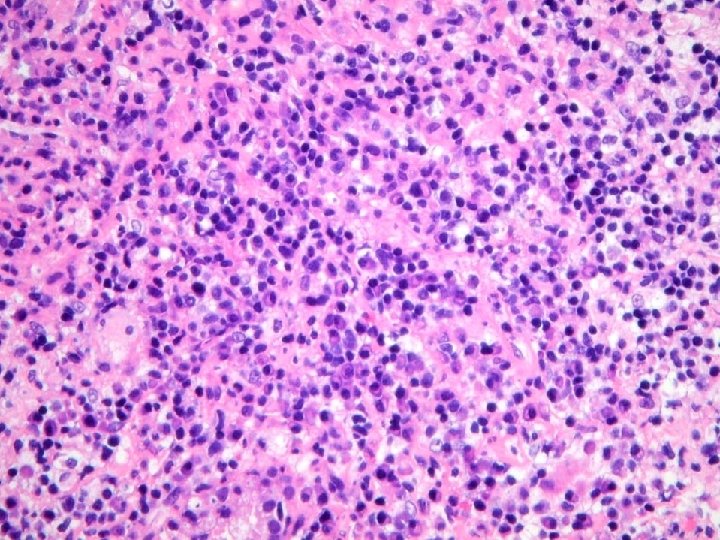
• When serum creatinine rose to 160 -170 in late September 2006 and 200 in early October 2006 with no change in medications or acute medical illness, concern lead to imaging studies (generally normal) and renal transplant biopsy (November 6). • Subsequently serum creatinine seems to have fallen 190 155.
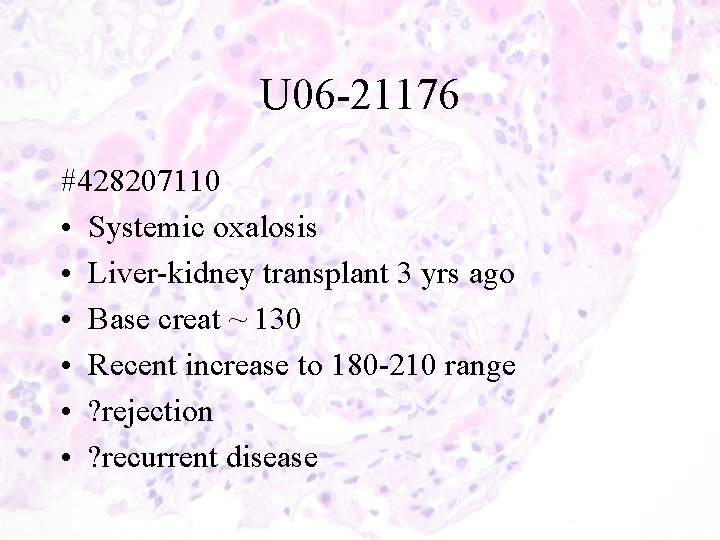
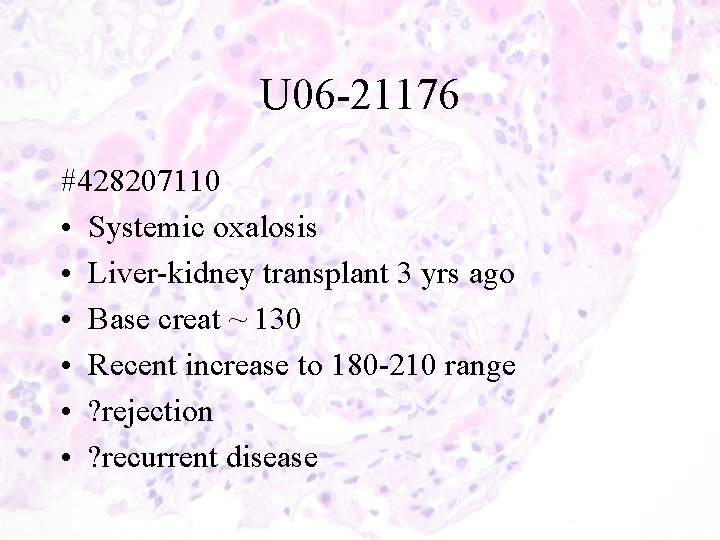
U 06 -21176 #428207110 • Systemic oxalosis • Liver-kidney transplant 3 yrs ago • Base creat ~ 130 • Recent increase to 180 -210 range • ? rejection • ? recurrent disease
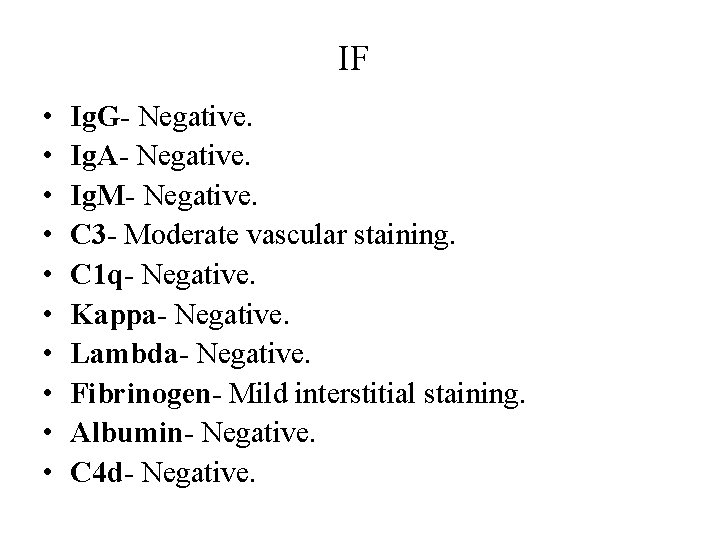
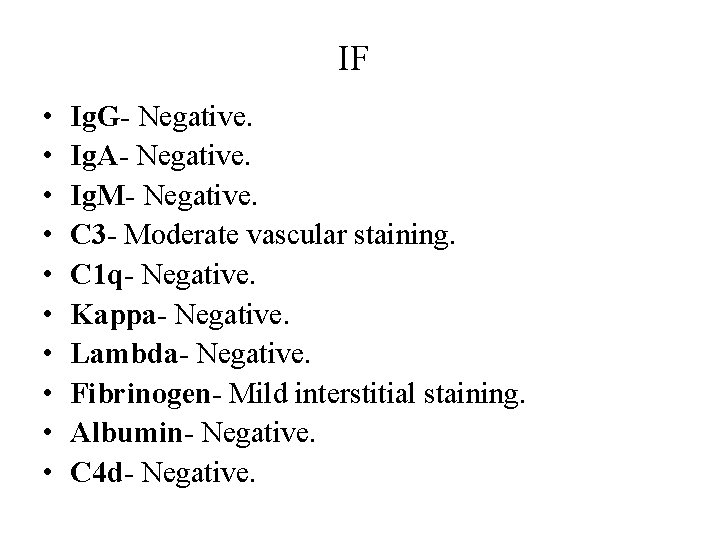
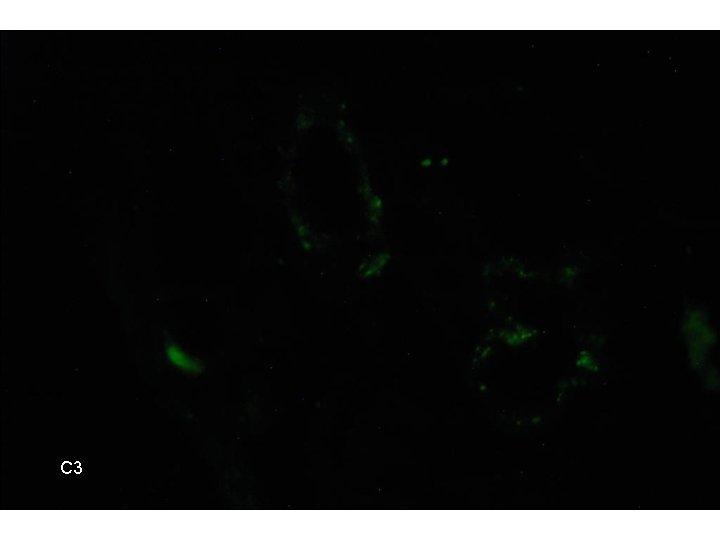
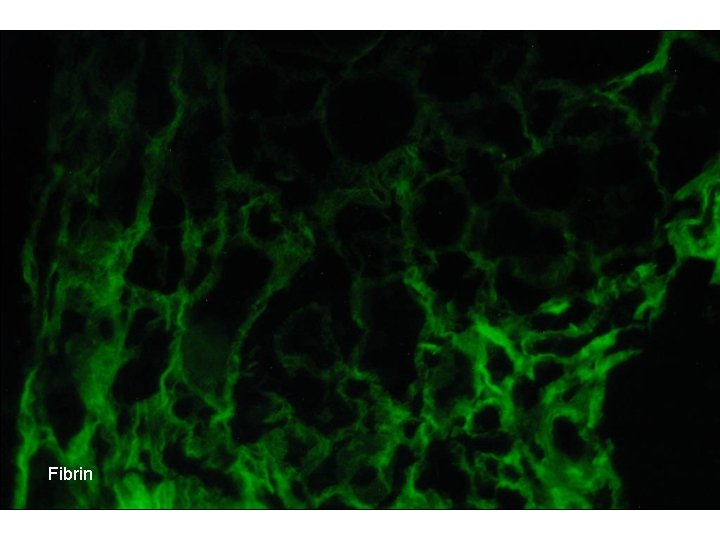
IF • • • Ig. G- Negative. Ig. A- Negative. Ig. M- Negative. C 3 - Moderate vascular staining. C 1 q- Negative. Kappa- Negative. Lambda- Negative. Fibrinogen- Mild interstitial staining. Albumin- Negative. C 4 d- Negative.
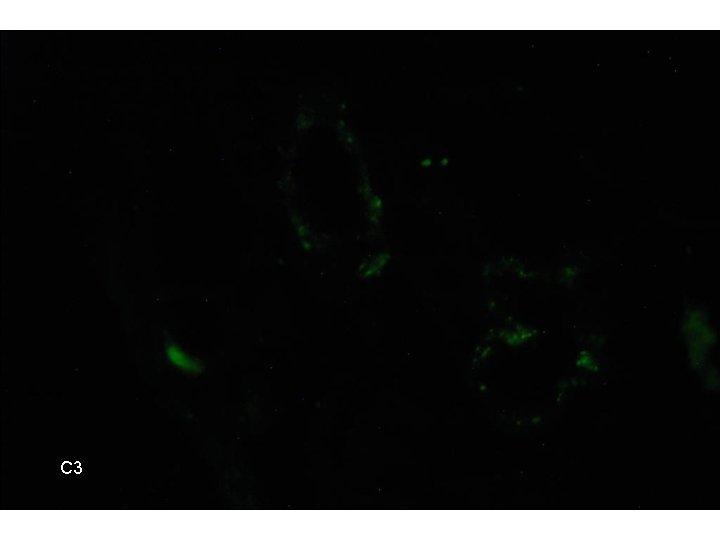
C 3
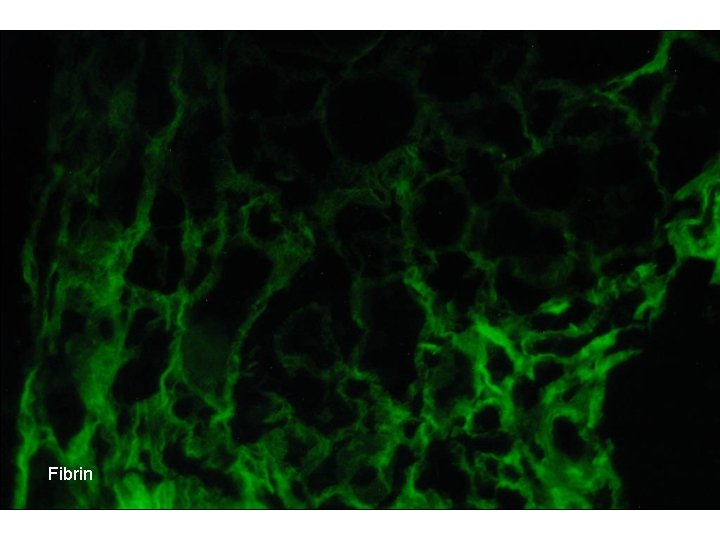
Fibrin
EM • Will be ready in the coming weeks
Diagnosis Renal Biopsy: • Chronic pyelonephritis with medullary calcium oxalate deposition related to systemic oxalosis • No evidence of rejection • Banff scores: – G 0 CG 1 I 1 CI 1 T 0 CT 1 V 0 CV 1 AH 0 MM 0
 Res extra commercium
Res extra commercium Teoria do nefron intacto
Teoria do nefron intacto Earthy look in chronic renal failure
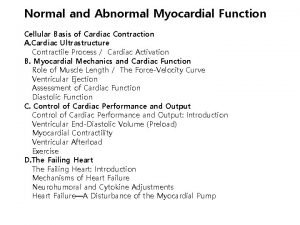
Earthy look in chronic renal failure Acute vs chronic heart failure
Acute vs chronic heart failure Treatments for acute renal failure
Treatments for acute renal failure Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries 5 cardinal signs of inflammation
5 cardinal signs of inflammation Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Morphological forms of inflammation
Morphological forms of inflammation How common is leukemia in adults
How common is leukemia in adults Cyst granuloma abscess
Cyst granuloma abscess Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Gallbladder histology drawing
Gallbladder histology drawing Developed by ed
Developed by ed Azotemia
Azotemia Renal failure
Renal failure Acute liver failure criteria
Acute liver failure criteria Cushings triad
Cushings triad Acute liver failure criteria
Acute liver failure criteria Acute brain failure
Acute brain failure Ventricular escape rhythm
Ventricular escape rhythm Failure to sense pacemaker
Failure to sense pacemaker Ductile break
Ductile break Patient 2 patient
Patient 2 patient What is renal lobule
What is renal lobule Dose adjustment in renal and hepatic disease
Dose adjustment in renal and hepatic disease Uti symptoms
Uti symptoms Function of nephron slideshare
Function of nephron slideshare Difference between renal and cardiac edema
Difference between renal and cardiac edema 4-1 classifying triangles
4-1 classifying triangles Cellular events of acute inflammation
Cellular events of acute inflammation Difference between acute and subacute rehab
Difference between acute and subacute rehab Failure of supporting utilities and structural collapse
Failure of supporting utilities and structural collapse Forrester classification heart failure
Forrester classification heart failure Stigma associated with failure and repetition is removed
Stigma associated with failure and repetition is removed Failure mode and effect analysis
Failure mode and effect analysis Ddmin
Ddmin Factors of project success and failure
Factors of project success and failure Cycle of failure mediocrity and success
Cycle of failure mediocrity and success