4 Small and Large Intestines Obstructive and vascular
4. Small and Large Intestines Obstructive and vascular disease Ghadeer Hayel, MD
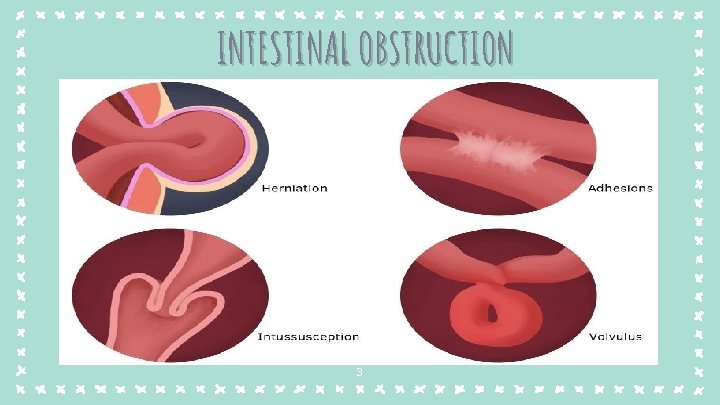
INTESTINAL OBSTRUCTION Ø Most often in small intestine narrow lumen. Ø Symptoms: abdominal pain, distention, vomiting, & constipation. Ø 80% of mechanical obstructions are caused by: + Hernia. + Adhesion: Surgical procedures & inflammation scars can cause adhesions between bowel segments or operation sites. +Volvulus: twisting of a loop of bowel around its mesenteric point. +Intussusception: a segment of the intestine, constricted by a wave of peristalsis, telescopes into the immediately distal segment. Ø Tumors & infarction account for most of the remainder 2
INTESTINAL OBSTRUCTION 3
Abdominal Hernia Ø Hernia sac: weakness or defect in the peritoneal cavity wall that may permit protrusion of pouch of peritoneum. Ø Most commonly occur anteriorly; 1) inguinal & 2) femoral canals or 3) umbilicus, or 4) sites of surgical scars. Ø Can cause visceral protrusion (external herniation). Ø Complications: entrapped viscera pressure at the neck of the pouch impair venous drainage stasis & edema increase the bulk of the herniated loop permanent entrapment (incarceration) arterial & venous compromise (strangulation) infarction. 4
Functional Obstruction Hirschsprung. Disease: a congenital defect in colonic innervation, where the patient has an aganglionic segment no peristaltic contractions functional obstruction. Pathogenesis: Neural cells migration from cecum to rectum is arrested distal intestinal segment lacks both Meissner submucosal & Auerbach myenteric plexi (aganglionosis) Clinical: Failure to pass meconium in immediate postnatal period, followed by obstruction or constipation 5

Morphology: Usually limited to the rectum & sigmoid colon. The aganglionic region may be normal or contracted, while the normally innervated proximal colon undergo progressive dilation as a result of functional distal obstruction 6
Ischemic Bowel Disease Largest portion GIT is supplied by celiac, superior mesenteric, & inferior mesenteric arteries. As they approach intestinal wall, superior & inferior mesenteric arteries fan out to form arcades. ‐ Interconnections between arcades & collateral supplies small intestine & colon can tolerate slowly progressive loss of the blood supply from one artery. ‐ But acute compromise of any major vessel can lead to infarction of several meters of intestine. ‐ 7
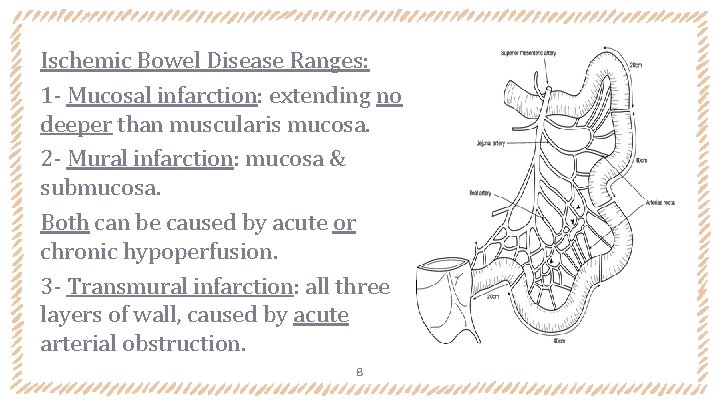
Ischemic Bowel Disease Ranges: 1 - Mucosal infarction: extending no deeper than muscularis mucosa. 2 - Mural infarction: mucosa & submucosa. Both can be caused by acute or chronic hypoperfusion. 3 - Transmural infarction: all three layers of wall, caused by acute arterial obstruction. 8
Pathogenesis: Pathogenesis ‐ Important causes of acute arterial obstruction: severe atherosclerosis, aortic aneurysm, hypercoagulable states, oral contraceptive use & embolization. ‐ Important causes of Intestinal hypoperfusion: Cardiac failure, shock, dehydration, or vasoconstrictive drugs. ‐ Intestinal responses to ischemia occur in twophases: Initial hypoxic injury: at onset of vascular compromise mild damage but epithelial cells are relatively resistant to transient hypoxia. Reperfusion injury: on restoration of blood supply greatest damage free radical production, neutrophil infiltration & inflammatory mediators (complement & cytokines) 9
Morphology - Gross +Involvement is frequently segmental and patchy +Mucosal hemorrhages and often ulceration. +Bowel wall is thickening by edema. +Blood tinged mucus or blood within the lumen. Morphology - Microscopic +Atrophy/sloughing of surface epithelium, butcrypts may be hyperproliferative. +Inflammatory infiltrates (neutrophils) recruited within hours of reperfusion. +Chronic ischemia is ass/w fibrous scarring of lamina propria. 10

11
Clinically: ‐ Older adults with coexisting cardiac or vascular disease. Acute transmural infarction: Symptoms: sudden, severe abdominal pain & tenderness, nausea, vomiting, bloody diarrhea, or dark melanotic stool. May progress to shock & vascular collapse in hours. Signs: +Peristaltic sounds diminish or disappear. +muscular spasm boardlike rigidity of abdominal wall. ‐ As the mucosal barrier breaks down, bacteria enter the circulation & sepsis can develop; the mortality rate exceed 50%. 12
Hemorrhoids Ø Hemorrhoids are dilated anal and perianal collateral vessels connect the portal and caval venous systems. Ø Less serious than esophageal varices, but similar pathogenesis. Ø Common, 5% of the general population. Ø predisposing factors: + constipation & straining increase intraabdominal & venous pressures. + venous stasis of pregnancy + Portal hypertension. 13
Hemorrhoids Ø External hemorrhoidsdilation of collateral vessels within the inferior hemorrhoidal plexus below the anorectal line. Ø Internal hemorrhoids: dilation of the superior hemorrhoidal plexus within the distal rectum. Ø Hemorrhoids often manifest with pain and rectal mildmoderate bleeding, particularly bright red blood seen on toilet tissue. Ø Tx: sclerotherapy, rubber band ligation, & infrared coagulation. In severe cases removed surgically by hemorrhoidectomy. 14
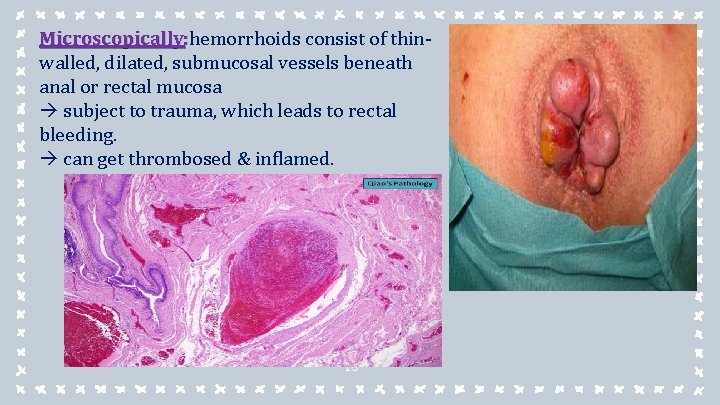
Microscopically: hemorrhoids consist of thinwalled, dilated, submucosal vessels beneath anal or rectal mucosa subject to trauma, which leads to rectal bleeding. can get thrombosed & inflamed. 15

4. Small and Large Intestines INFLAMMATORY DISEASE
Sigmoid Diverticulitis • Diverticulum : an outpouching (pocket) of the colonic mucosa and submucosa multiple diverticulosis. (Diverticula) • More common in adults older than 60 years in developed countries. • Pathogenesis: (1) High luminal pressures exaggerated peristaltic contractions. • (2) spasmodic sequestration of bowel segments exacerbated by low fiber diets (reduce stool bulk). • Mostly asymptomatic, 20% has intermittent cramping, lower abdominal discomfort, constipation, & diarrhea. 17
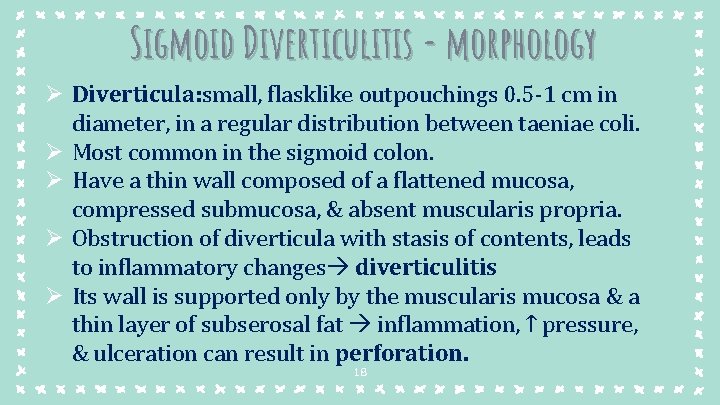
Sigmoid Diverticulitis - morphology Ø Diverticula: small, flasklike outpouchings 0. 5 -1 cm in diameter, in a regular distribution between taeniae coli. Ø Most common in the sigmoid colon. Ø Have a thin wall composed of a flattened mucosa, compressed submucosa, & absent muscularis propria. Ø Obstruction of diverticula with stasis of contents, leads to inflammatory changes diverticulitis Ø Its wall is supported only by the muscularis mucosa & a thin layer of subserosal fat inflammation, ↑ pressure, & ulceration can result in perforation. 18

Sigmoid Diverticulitis 19
Inflammatory Bowel Disease (IBD) A chronic condition resulting from inappropriate mucosal immune activation. ‐ Frequently present during adolescence or in young adults. ‐ IBD encompasses two entities, differentiated mainly based on affected sites & the morphologic features of the disease. +Crohn disease(CD) may involve any area in GIT/frequently transmural. +ulcerative colitis(UC) limited to the colon & rectum/ extends only to mucosa & submucosa. ‐ 20
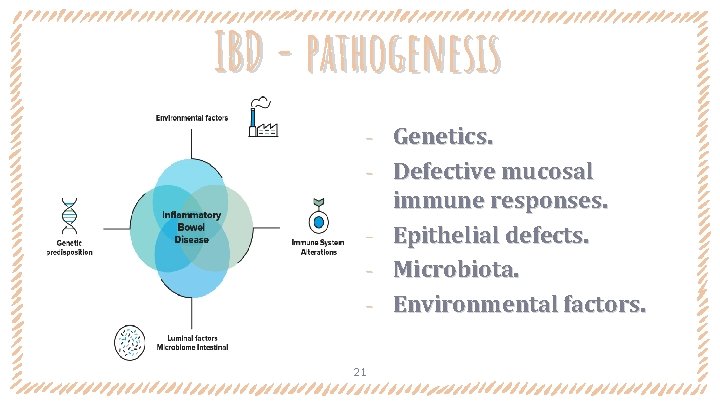
IBD - pathogenesis ‐ ‐ ‐ 21 Genetics. Defective mucosal immune responses. Epithelial defects. Microbiota. Environmental factors.
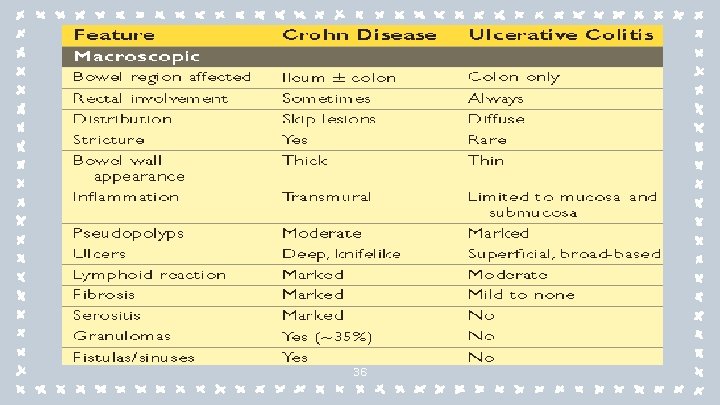
IBD -Morphology
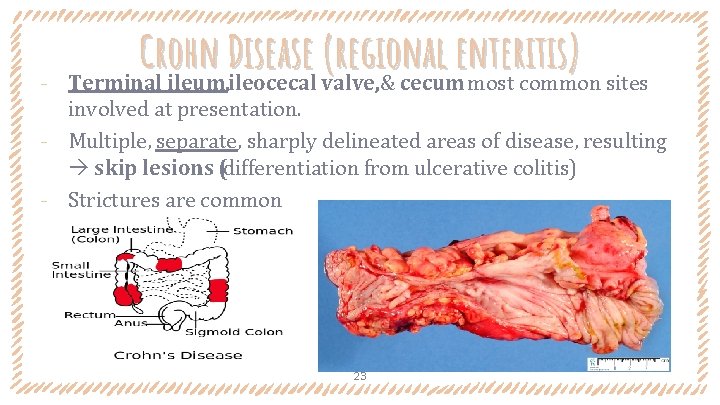
‐ Crohn Disease (regional enteritis) Terminal ileum, ileocecal valve, & cecum most common sites involved at presentation. ‐ Multiple, separate, sharply delineated areas of disease, resulting skip lesions (differentiation from ulcerative colitis) ‐ Strictures are common 23
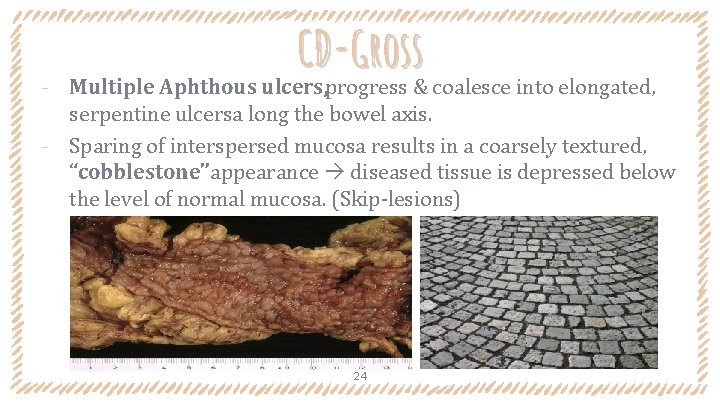
CD-Gross ‐ Multiple Aphthous ulcers, progress & coalesce into elongated, serpentine ulcersa long the bowel axis. ‐ Sparing of interspersed mucosa results in a coarsely textured, “cobblestone”appearance diseased tissue is depressed below the level of normal mucosa. (Skip-lesions) 24

CD-Gross Extensive transmural disease mesenteric fat frequently extends around the serosal surface (creeping fat). 25
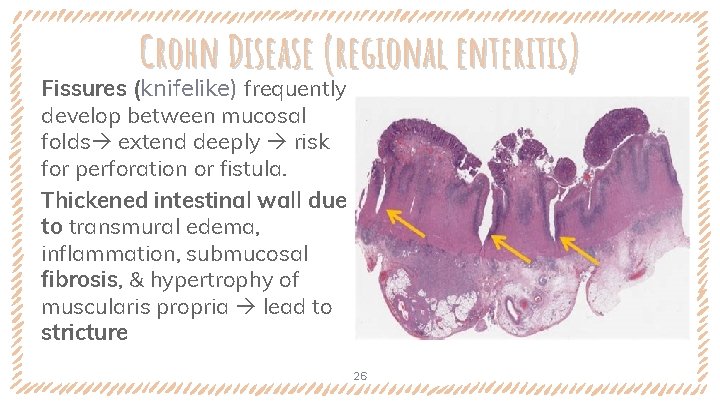
Crohn Disease (regional enteritis) Fissures (knifelike) frequently develop between mucosal folds extend deeply risk for perforation or fistula. Thickened intestinal wall due to transmural edema, inflammation, submucosal fibrosis, & hypertrophy of muscularis propria lead to stricture 26
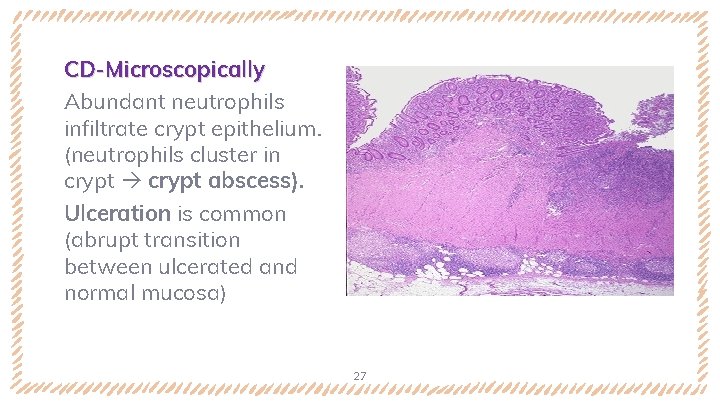
CD-Microscopically Abundant neutrophils infiltrate crypt epithelium. (neutrophils cluster in crypt abscess). Ulceration is common (abrupt transition between ulcerated and normal mucosa) 27

CD-Microscopically Cycles of crypt destruction & regeneration distortion of normal mucosal architecture (normal straight & parallel crypts take on bizarre branching shapes and unusual orientations. 28
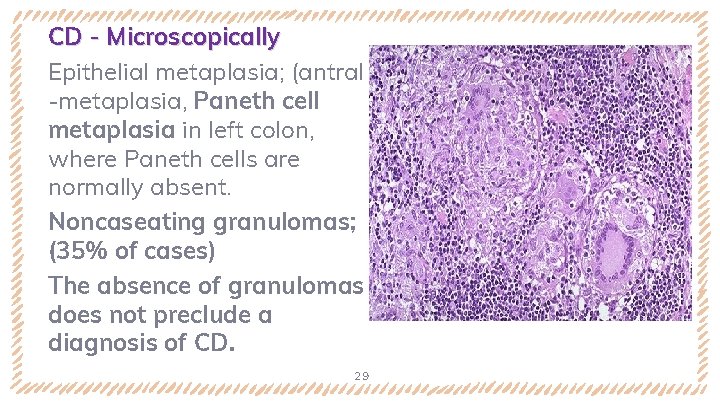
CD - Microscopically Epithelial metaplasia; (antral -metaplasia, Paneth cell metaplasia in left colon, where Paneth cells are normally absent. Noncaseating granulomas; (35% of cases) The absence of granulomas does not preclude a diagnosis of CD. 29
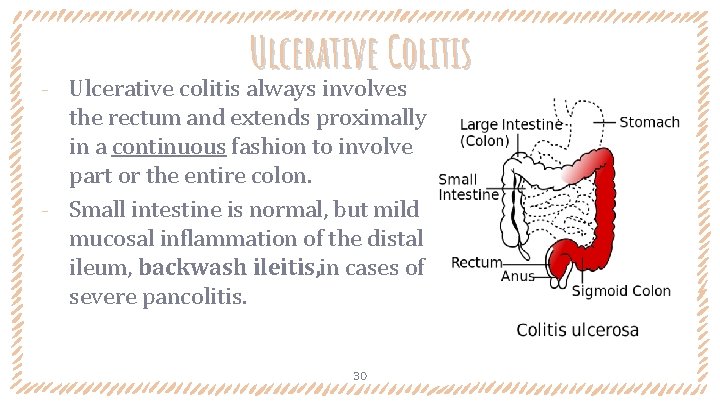
Ulcerative Colitis Ulcerative colitis always involves the rectum and extends proximally in a continuous fashion to involve part or the entire colon. ‐ Small intestine is normal, but mild mucosal inflammation of the distal ileum, backwash ileitis, in cases of severe pancolitis. ‐ 30
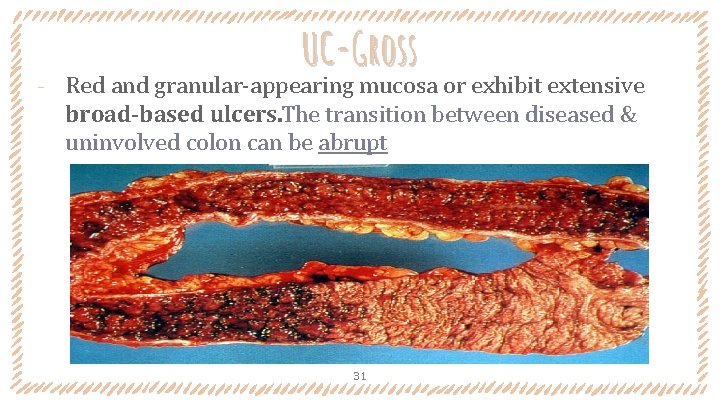
‐ UC-Gross Red and granular-appearing mucosa or exhibit extensive broad-based ulcers. The transition between diseased & uninvolved colon can be abrupt 31
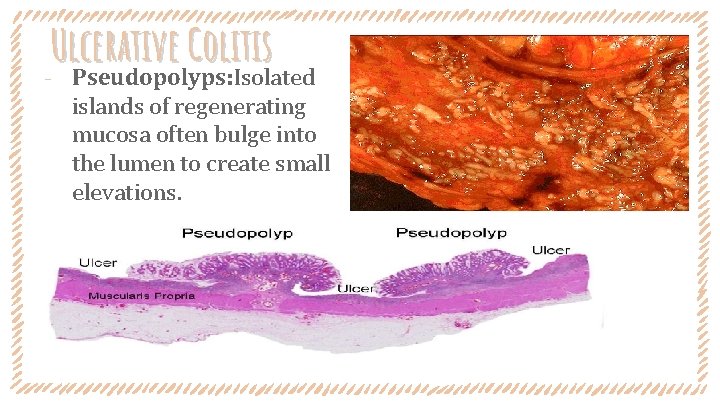
Ulcerative Colitis ‐ Pseudopolyps: Isolated islands of regenerating mucosa often bulge into the lumen to create small elevations. 32
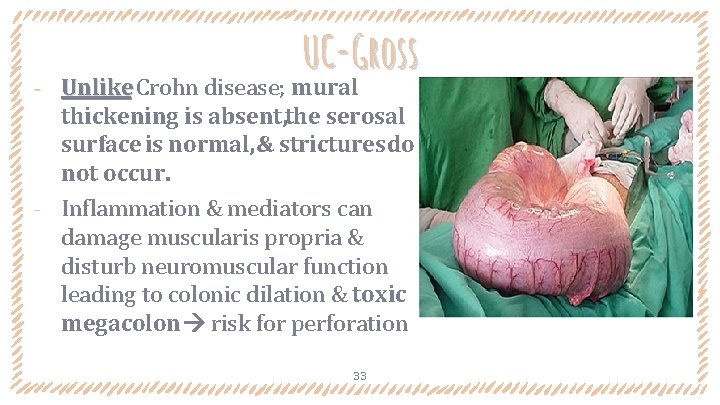
UC-Gross Unlike Crohn disease; mural thickening is absent, the serosal surface is normal, & strictures do not occur. ‐ Inflammation & mediators can damage muscularis propria & disturb neuromuscular function leading to colonic dilation & toxic megacolon risk for perforation ‐ 33
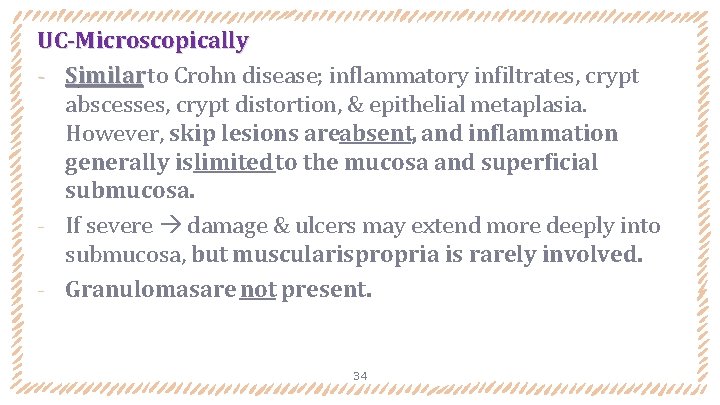
UC-Microscopically ‐ Similar to Crohn disease; inflammatory infiltrates, crypt abscesses, crypt distortion, & epithelial metaplasia. However, skip lesions areabsent, and inflammation generally islimited to the mucosa and superficial submucosa. ‐ If severe damage & ulcers may extend more deeply into submucosa, but muscularispropria is rarely involved. ‐ Granulomasare not present. 34
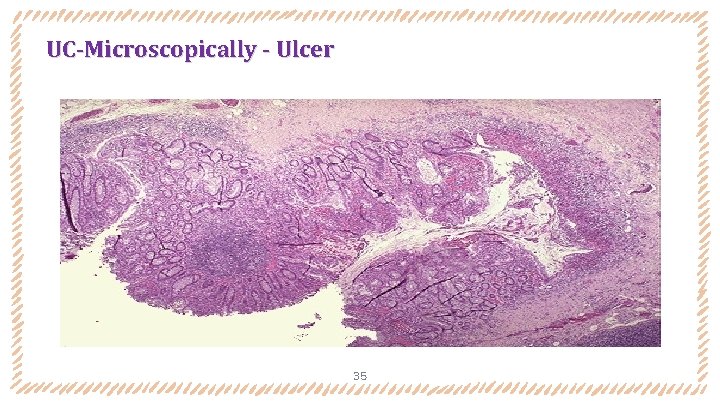
UC-Microscopically - Ulcer 35
36
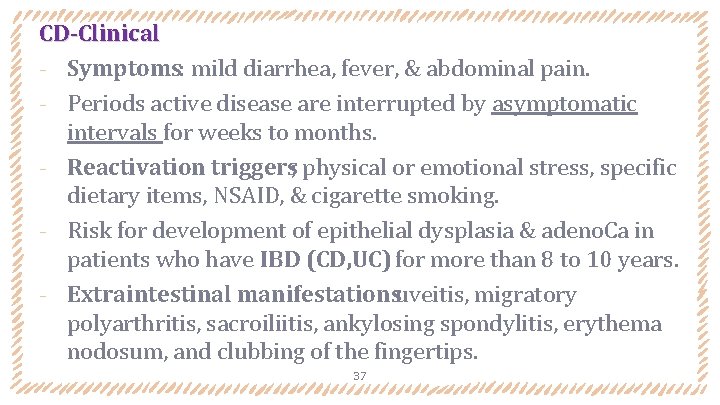
CD-Clinical ‐ Symptoms: mild diarrhea, fever, & abdominal pain. ‐ Periods active disease are interrupted by asymptomatic intervals for weeks to months. ‐ Reactivation triggers; physical or emotional stress, specific dietary items, NSAID, & cigarette smoking. ‐ Risk for development of epithelial dysplasia & adeno. Ca in patients who have IBD (CD, UC) for more than 8 to 10 years. ‐ Extraintestinal manifestationsuveitis, migratory polyarthritis, sacroiliitis, ankylosing spondylitis, erythema nodosum, and clubbing of the fingertips. 37

UC-Clinical ‐ Symptoms: bloody diarrhea with expulsion of stringy, mucoid material & lower abdominal pain & cramps relieved temporarily by defecation. ‐ Patients w mild disease, mostly relapse during 10 -years. ‐ Colectomy cures intestinal disease, but extraintestinal manifestations may persist. ‐ Triggers: symptoms can occur shortly after smoking cessation in some patients & smoking may partially relieve symptoms. ‐ Extraintestinal manifestationsoverlap with CD; but pericholangitis, & primary sclerosing Cholangitis are more common in UC. 38

39
- Slides: 39