4 Small and Large Intestines DIARRHEAL MALABSORPTIVE DISEASE

4. Small and Large Intestines DIARRHEAL & MALABSORPTIVE DISEASE Ghadeer Hayel, MD
Diarrhea Ø Diarrhea: an increase in stool mass, frequency, or fluidity, typically to amounts greater than 200 grams per day. Ø Dysentery: Painful, bloody, small-volume diarrhea. Ø Diarrhea is a symptom of many intestinal diseases: +Infection. +Inflammation. +Ischemia. +Malabsorption. +Nutritional deficiency. 2
Diarrhea is classified into four major categories: Ø Secretory diarrhea: isotonic stool persists during fasting. Ø Osmotic diarrhea: due to osmotic forces exerted by unabsorbed luminal solutes. (diarrhea in lactase deficiency) fluid is at least 50 m. Osm more concentrated than plasma abates with fasting. Ø Malabsorptive diarrhea: due to inadequate nutrient absorption is ass with steatorrhea relieved by fasting. Ø Exudative diarrhea: due to inflammatory disease, characterized by purulent, bloody stools continue during fasting. 3
Malabsorptive Diarrhea Ø Malabsorption: A defective absorption of fats, fat- and water-soluble vitamins, proteins, carbohydrates, electrolytes, minerals, & water. Ø Manifests most commonly as chronic diarrhea. Ø Causes: weight loss, anorexia, abdominal distention, borborygmi, and muscle wasting. Ø A hallmark is steatorrhea: excessive fecal fat & bulky, frothy, greasy, yellow, or clay-colored stools. 4
Malabsorptive Diarrhea results from disturbance in at least one of the four phases of nutrient absorption: • Intraluminal digestion: proteins, carbohydrates, & fats are broken down into absorbable forms • Terminal digestion: hydrolysis of carbohydrates & peptides by disaccharidases and peptidases, respectively, in the brush borders of small-intestinal mucosa. • Transepithelial transport: nutrients, fluid, & electrolytes are transported across & processed in small-intestinal epithelium. • Lymphatic transport of absorbed lipids. 5
Celiac Disease Celiac disease: (celiac sprue or glutensensitive enteropathy) is an immune-mediated enteropathy triggered by the ingestion of gluten-containing cereals, such as wheat, rye, or barley, in genetically predisposed individuals. ‐ An intestinal immune reaction togluten (major storage protein) ‐ Celiac patients have higher rate of these malignancies; T cell lymphoma, & Small-intestinal adenocarcinoma ‐ 6
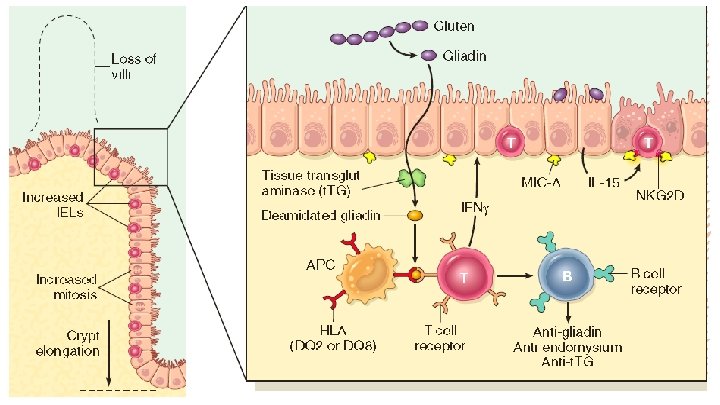
Celiac Disease 7
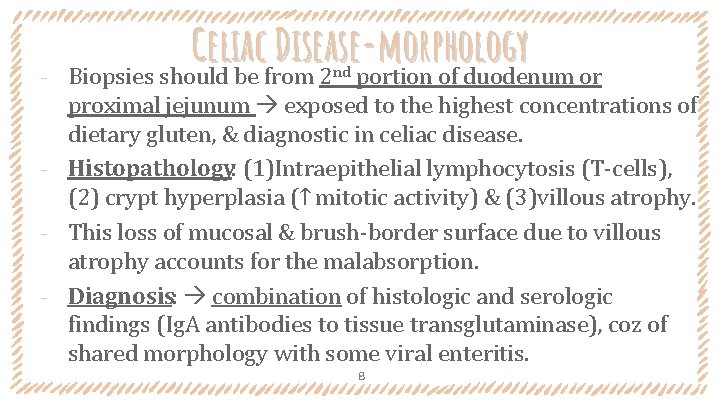
‐ Celiac Disease-morphology Biopsies should be from 2 portion of duodenum or nd proximal jejunum exposed to the highest concentrations of dietary gluten, & diagnostic in celiac disease. ‐ Histopathology: (1)Intraepithelial lymphocytosis (T-cells), (2) crypt hyperplasia (↑ mitotic activity) & (3)villous atrophy. ‐ This loss of mucosal & brush-border surface due to villous atrophy accounts for the malabsorption. ‐ Diagnosis: combination of histologic and serologic findings (Ig. A antibodies to tissue transglutaminase), coz of shared morphology with some viral enteritis. 8
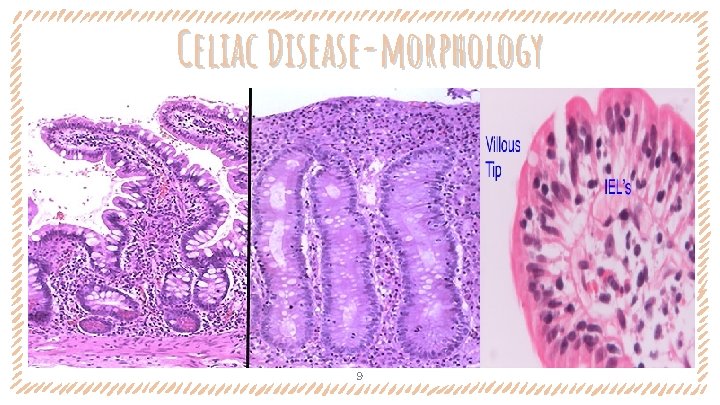
Celiac Disease-morphology 9
Celiac Disease-CLINICAL ‐ Pediatric celiac: 6 -24 months +After introduction of gluten to diet. +Symptoms: Irritability, abdominal distention, anorexia, diarrhea, failure to grow, weight loss, or muscle wasting. ‐ Adults celiac: 30 and 60 years of age. + atypical presentations or anemia-IDA, diarrhea, bloating, & fatigue. +silent disease: positive serology & villous atrophy without symptoms. +Latent disease: positive serology, no villous atrophy, no symptoms. 10
environmental enteric dysfunction Ø A syndrome of stunted growth & impairedintestinal function that iscommon in developing countries. Ø Neither supplementary feeding nor vitamin & mineral supplementation are able to fully reverse the syndrome. Ø Repeated bouts of diarrhea suffered within the first 2 or 3 years of life but no single infectious agent has been established as causal in these diarrheal episodes. Ø Intestinal biopsy overlap with severe celiac disease & infectious enteritis. 11
Lactase (Disaccharidase) Deficiency Ø Lead to osmotic diarrhea osmotically active lactose remains in the lumen & draw fluid. Ø The defect is biochemical biopsies are unremarkable. • Congenital lactase deficiency : Rare. AR disorder; mutations in the gene encoding lactase. Sx: Explosive diarrhea with watery, frothy stools & distention after milk ingestion. Symptoms abate when exposure to milk products is terminated. • Acquired lactase deficiency: Common. Downregulation of lactase gene expression. Onset is sometimes associated with 12 enteric viral or bacterial infections.
Infectious Enterocolitis Signs & symptoms: diarrhea, abdominal pain, urgency, perianal discomfort, incontinence, & hemorrhage. ‐ The most common pathogens vary with age, nutrition, host immune status, & environment. ‐ Escherichia coliare gram-negative bacilli that colonize the healthy gastrointestinal tract most are nonpathogenic, but a subset cause a disease & produce a bloody diarrhea. ‐ E. coli is the most common cause of traveler’s diarrhea. ‐ 13
‐ ‐ ‐ Cholera Vibrio cholerae are comma-shaped, gram –ve bacteria. An endemic disease in which V. cholerae is transmitted primarily by contaminated drinking water. Causes disease by producinga toxin that interferes with the absorptive functionof enterocytes. Mostly aymptomatic Severe disease: abrupt onset of watery diarrhea & vomiting. The volume of diarrhea (1 L /hour) dehydration hypotension, anuria, shock, loss of consciousness, and death. 14
Campylobacter Enterocolitis Campylobacter jejuni is the most commonbacterial enteric pathogen in developed countries& a cause of traveler’s diarrhea. ‐ Most infections are ass with ingestion of improperly cooked chicken. ‐ Outbreaks can be caused by unpasteurized milk or contaminated water. ‐ Campylobacter infection can result in reactive arthritis, erythema nodosum and Guillain-Barré syndrome (0. 1% or less). 15 ‐
Campylobacter Enterocolitis Clinical Features: ‐ Watery diarrhea, either acute or after an influenza like prodrome. ‐ Dysentery develops in up to 50% of patients. ‐ Patients may shed bacteria for 1 month or more after clinical resolution. ‐ The disease is self-limited, and antibiotic therapy generally is not required ‐ Specific diagnosis is primarily by stool culture. 16
‐ ‐ ‐ Shigellosis Shigella are gram-negativebacilli. One of the most common causes of bloodydiarrhea. Highly transmissible by the fecal-oral route or contaminated water and food Shigella causes self-limited disease characterized by 6 days of diarrhea, fever, and abdominal pain. Watery diarrhea progresses to a dysenteric phase in 50% of patients. Most prominent in the leftcolon. 17
Salmonellosis Salmonella species are gram-negative bacilli. ‐ Divided into Salmonella typhi , & nontyphoid Salmonella strains that cause gastroenteritis. ‐ Nontyphoid Salmonella infection usually is due to Salmonella enteritidis ; +most common in young children and older adults. +Transmission usually is through contaminated food, (raw or undercooked meat, poultry, eggs, and milk) ‐ 18
Typhoid Fever - enteric fever Caused by Salmonella typhi & Salmonella paratyphi. ‐ S. typhi is more common in endemic areas (children & adolescents) ‐ S. paratyphi predominates in travelers and those living in developed countries. ‐ Humans are the sole reservoir for S. typhi and S. paratyphi, transmission occurs person to person or via contaminated food or water. ‐ 19
Typhoid Fever - enteric fever Acute infection is associated with anorexia, abdominal pain, bloating, nausea, vomiting, and bloody diarrhea a short asymptomatic phase during which bacteremia occur & fever with flulike symptoms then 2 weeks of sustained high fevers with abdominal tenderness. ‐ Cultures are positive in 90% of cases during the febrile phase ‐ Rose spots, spots small erythematous maculopapular lesions, are seen on the chest and abdomen. ‐ 20

morphology Ø Campylobacter, Shigella, Salmonella, and E. coli, all induce a similar microscopic picture acute self-limited colitis. Ø So. . Specific diagnosis is primarily by stool culture. Ø Histology: prominent lamina propria & intraepithelial neutrophil infiltrates, cryptitis & crypt abscesses Ø preservation of crypt architecture in most cases of acute selflimited colitis distinguishing these infections inflammatory bowel disease 21
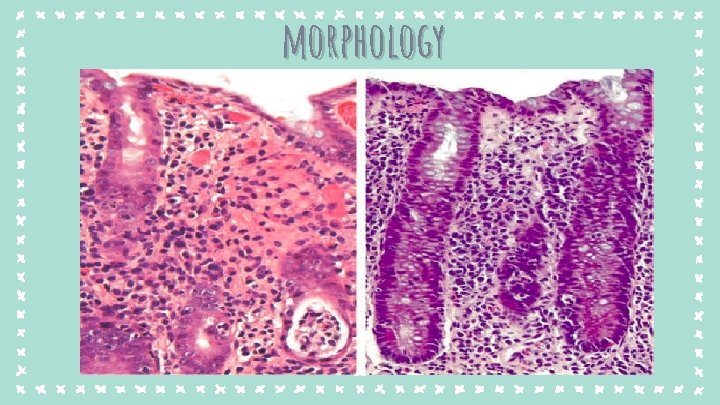
morphology 22
Pseudomembranous Colitis Generally caused by Clostridium difficile ‐ Referred to as antibiotic-associated colitis or antibioticassociated diarrhea. (any antibiotic may be responsible) ‐ Disruption of the normal colonic microbiota by antibiotics allows C. difficile overgrowth. ‐ Toxins released by C. difficile lead to disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release, and apoptosis. ‐ 23
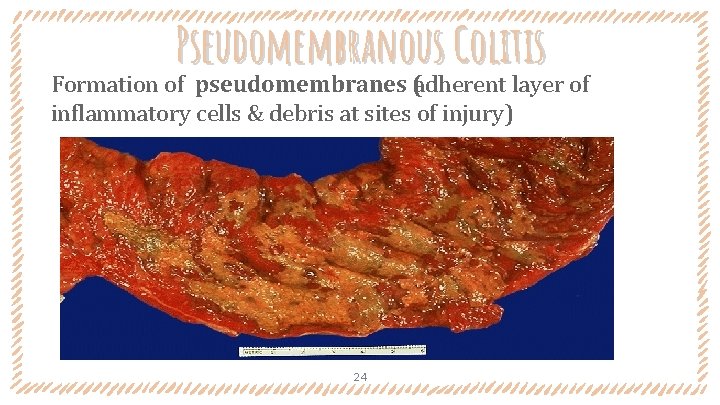
Pseudomembranous Colitis Formation of pseudomembranes (adherent layer of inflammatory cells & debris at sites of injury) 24
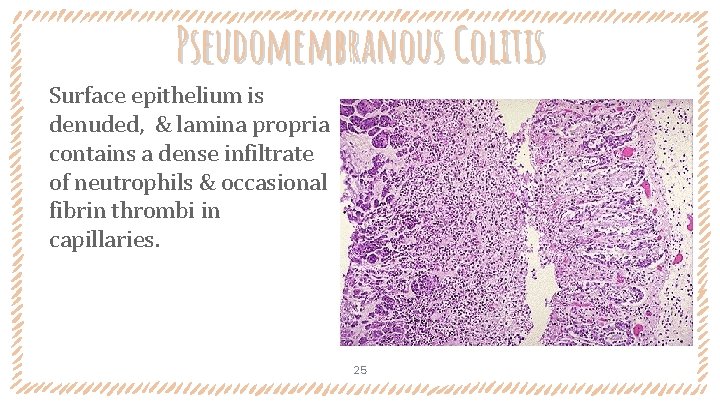
Pseudomembranous Colitis Surface epithelium is denuded, & lamina propria contains a dense infiltrate of neutrophils & occasional fibrin thrombi in capillaries. 25
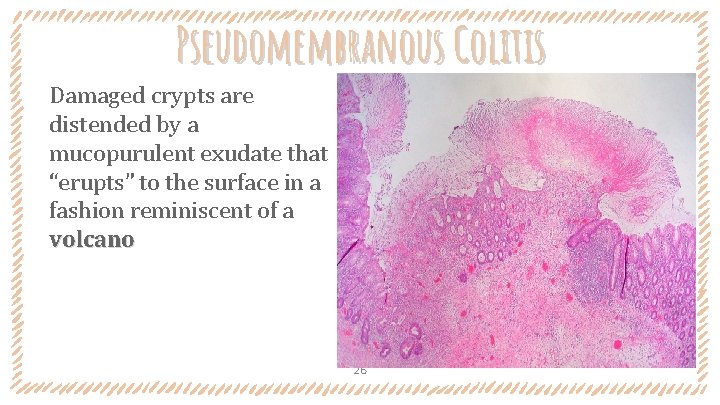
Pseudomembranous Colitis Damaged crypts are distended by a mucopurulent exudate that “erupts” to the surface in a fashion reminiscent of a volcano 26
Pseudomembranous Colitis Clinically: ‐ Risk factors: In addition to antibiotic exposure; advanced age, hospitalization & immunosuppression. ‐ Symptoms: watery diarrhea & cramping. Dehydration, fever, and leukocytosis may be seen in more severe cases. ‐ Diagnosis of C. difficile –associated colitis usually is by detection of C. difficile toxin, rather than culture, supporeted by the characteristic histopathology. 27
Rotavirus Ø The most common cause of severe childhood diarrhea & diarrhea Ø Ø -related deaths worldwide. Children most vulnaravle are between 6 & 24 months Spreads easily; the estimated minimal infective inoculum is only 10 viral particles. Rotavirus infects & destroys mature (absorptive) enterocytes in the small intestine villus surface is repopulated by immature secretory cells loss of absorptive function secretion of water and electrolytes osmotic diarrhea from incompletely absorbed nutrients. After a short incubation period several days of vomiting & watery diarrhea. 28
Irritable bowel syndrome (IBS) Ø Characterized by chronic, relapsing abdominal pain, bloating, & changes in bowel habits. Ø The gross and microscopic evaluation is normal in most IBS patients diagnosis depends on clinical symptoms Ø Pathogenesis: (psychologic stressors, diet, perturbation of microbiome, & abnormal GI motility) Ø Clinical criteria: Abdominal pain or discomfort at least 3 days per month over 3 months with improvement after defecation and a change in stool frequency or form. Other causes, such as enteric infection or inflammatory bowel disease, must be excluded 29
30
- Slides: 30