3 YEAR CASE HISTORY EMERGENCY vedi pag 309





- Slides: 80
3° YEAR CASE HISTORY EMERGENCY vedi pag 309 PATIENT’S FILE PHYSICAL EXAMINATION TREATMENTS
MEDICAL/CASE/HEALTH HISTORY The patient's past and present which may contain relevant information on their health past, present, and future. It contains information gained by a physician by asking specific questions, either of the patient or of other people who know the person, with the aim of obtaining information useful in formulating a diagnosis and providing medical care to the patient.
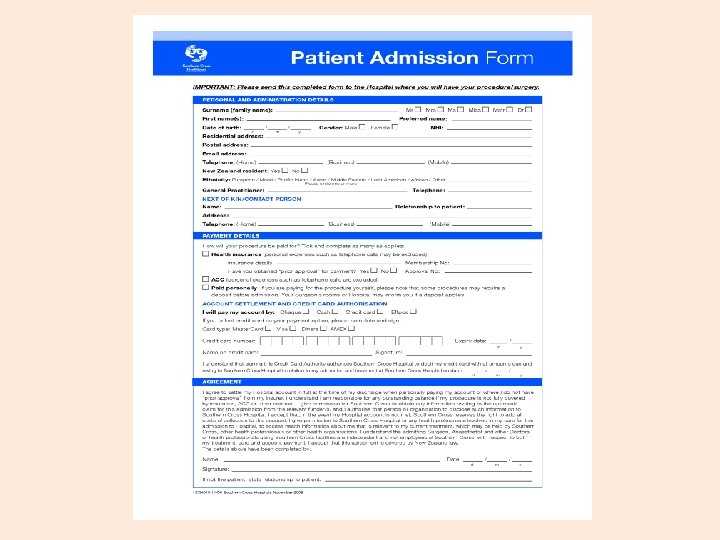
Nurses need to communicate so they can find out about the people in their care by taking a nursing history, give them information about their care and teach them about managing their illness. - ‘Hello [or good morning/good evening] Mrs Jones. I am Nurse [your last name/surname/family name]. ’ Do not use a person’s first name unless they ask you to do so. - Ask simple questions saying to Mrs Jones ‘I will be back to do your vital signs or obs’ will mean nothing to her; you will need to explain that you will be back to record her blood pressure, temperature, pulse and respiration. - Always check any prepared documents that arrive from the admissions office or the emergency department.
- You will need to start with the assessment sheet, finding out details about your patient such as their full name, where they live (address) and who with. ‘Mrs Jones can you tell me your full name and your address and telephone number. ’ - You will need to ask the patient if they work. ‘What do you do? ’ ‘What is your work? ’, ‘What job do you do’? - An assessment includes asking about the patient’s religion or spiritual needs. ‘What religion are you Mrs Jones? ’
Reason for admission : the patient’s understanding of reason for admission/treatment ‘What are your symptoms? ’ ‘What do you think is the matter with you? ’ ‘Tell me why you have come in today. ’ ‘Why do you come here today? ’E. g. ‘I’ve come in to get my cataract done [or operated on]. ’ ‘Have you been having some problems at home? ’E. g. ‘I’ve been having dizzy turns’. …
PATIENT’S FILE: social history – family history – allergies You will need to ask about past illnesses or operations. ‘Have you ever had any serious illnesses in the past? ’ ‘Have you ever had an operation? ’ ‘Have you ever been in hospital before? ’ ‘Have you ever had any accidents or injuries? ‘Is there anything else you’d like to tell me? As some illnesses, such as some types of heart disease and diabetes, may run in certain families (familial) you will also need to ask about the family medical history: ‘Are there any serious illnesses in your family? ’
Allergies: Always ask about any allergies, including foods, drugs and other substances such as washing powders, dust, grass family, pollen, nickel…: ‘Are you allergic to anything? ’ ‘Have you any allergies? ’ ‘Do you suffer from allergies? ’ It might be necessary to ask the family, for example, if the patient is a child, has dementia or is unconscious.
Drugs: It is necessary to ask all patients if they are taking any drugs, but it is worth remembering that some patients will associate the word ‘drugs’ with illegal substances and drug misuse, so you can ask: ‘Are you taking any medicines (or drugs)? ’ Always ask patients about all types of drugs, including those prescribed by a doctor or nurse, drugs they buy at the chemist (pharmacy) or supermarket (OTC, over-thecounter drugs) and if appropriate ask about recreational (illegal) drugs such as cannabis. It is vital to know about any drug allergies (e. g. penicillin) or adverse drug reactions.
Social history: Support networks are important particularly after discharge. You can ask questions such as: ‘Do your family live close by? ’ ‘Who will be at home to look after you when you are discharged? ’ ‘Do you see the nurse/doctor at home? ’ ‘What do the nurses do? ’ ‘Do they come in everyday? ’
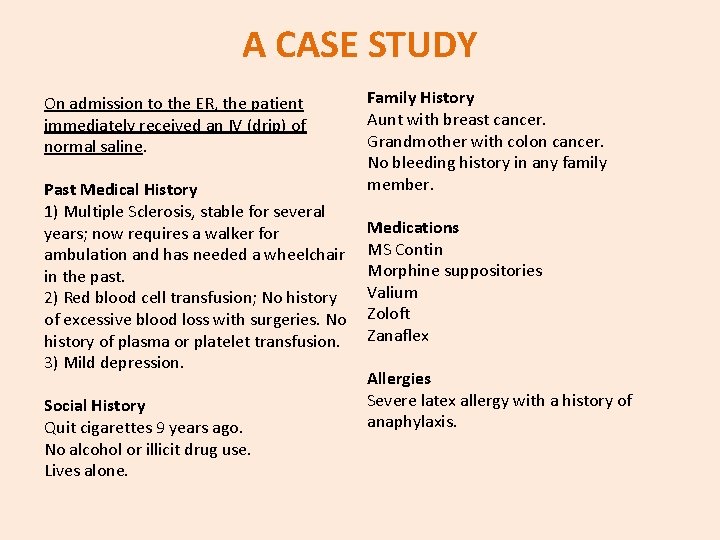
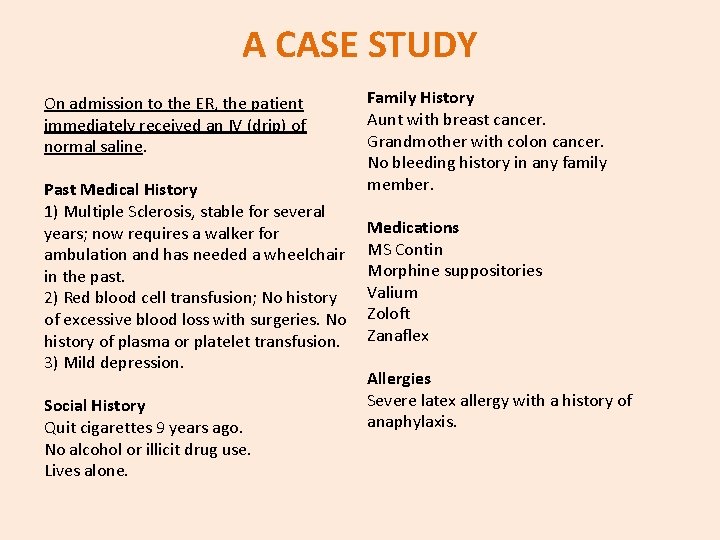
A CASE STUDY On admission to the ER, the patient immediately received an IV (drip) of normal saline. Past Medical History 1) Multiple Sclerosis, stable for several years; now requires a walker for ambulation and has needed a wheelchair in the past. 2) Red blood cell transfusion; No history of excessive blood loss with surgeries. No history of plasma or platelet transfusion. 3) Mild depression. Social History Quit cigarettes 9 years ago. No alcohol or illicit drug use. Lives alone. Family History Aunt with breast cancer. Grandmother with colon cancer. No bleeding history in any family member. Medications MS Contin Morphine suppositories Valium Zoloft Zanaflex Allergies Severe latex allergy with a history of anaphylaxis.
10 question every nurse should ask their patients What should I call you? Who is your family doctor? Who helps you at home? What makes you say that? Are you sexually active? Can you repeat, please? What is your opinion on that? Are you getting dental care? Why do you take this medication? Would you like to try doing it yourself?
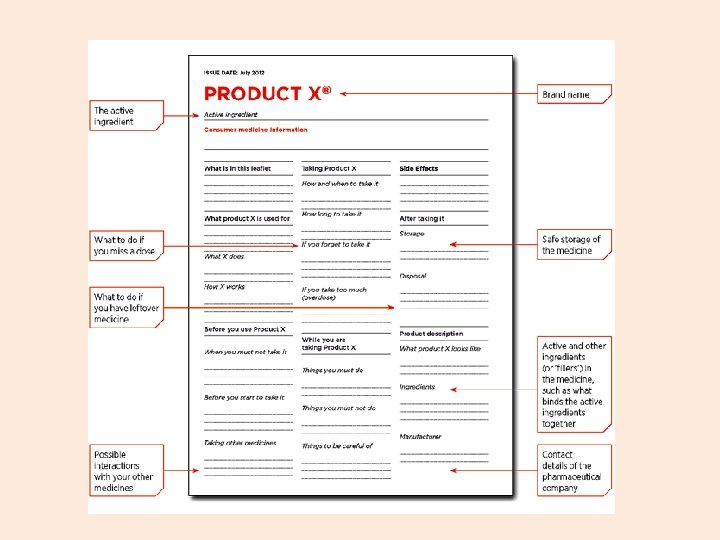
DRUGS Generic drug, content, prescription, active ingredient, excipient, drug label or leaflet (PIL – Patient Information Leaflet). VERBS: to prescribe, to dispense, to give, to administer, to suspend; to take, to swallow, to chew, to eat, to melt, to inhale, to relieve-to heal -to get better-to recover. FORM: tablet/pill/capsule/blister/syrup/inhaler(asthma)/ sachet/vial/applicator/soluble/ointment or cream/drops.
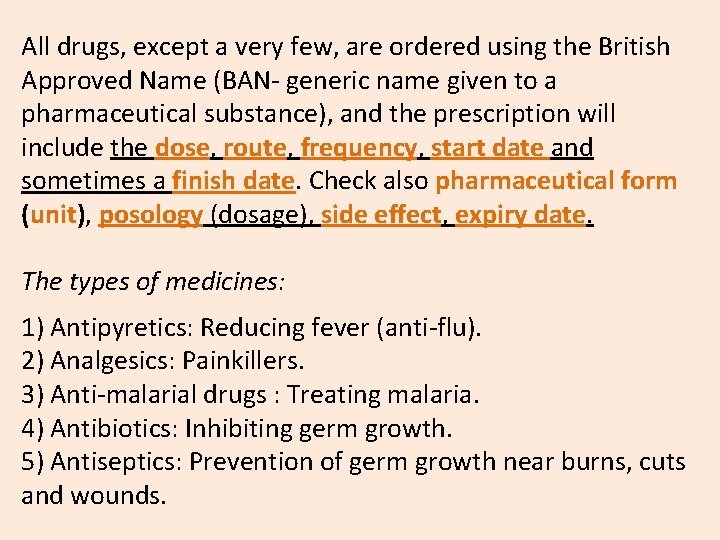
All drugs, except a very few, are ordered using the British Approved Name (BAN- generic name given to a pharmaceutical substance), and the prescription will include the dose, route, frequency, start date and sometimes a finish date. Check also pharmaceutical form (unit), posology (dosage), side effect, expiry date. The types of medicines: 1) Antipyretics: Reducing fever (anti-flu). 2) Analgesics: Painkillers. 3) Anti-malarial drugs : Treating malaria. 4) Antibiotics: Inhibiting germ growth. 5) Antiseptics: Prevention of germ growth near burns, cuts and wounds.
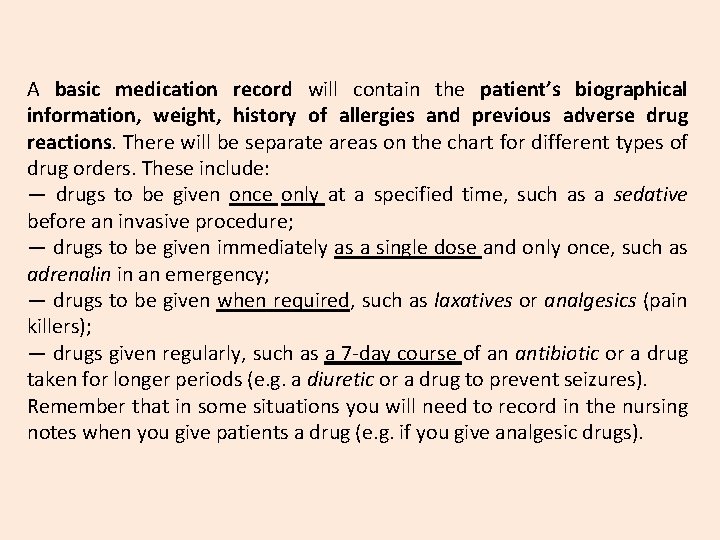
A basic medication record will contain the patient’s biographical information, weight, history of allergies and previous adverse drug reactions. There will be separate areas on the chart for different types of drug orders. These include: — drugs to be given once only at a specified time, such as a sedative before an invasive procedure; — drugs to be given immediately as a single dose and only once, such as adrenalin in an emergency; — drugs to be given when required, such as laxatives or analgesics (pain killers); — drugs given regularly, such as a 7 -day course of an antibiotic or a drug taken for longer periods (e. g. a diuretic or a drug to prevent seizures). Remember that in some situations you will need to record in the nursing notes when you give patients a drug (e. g. if you give analgesic drugs).
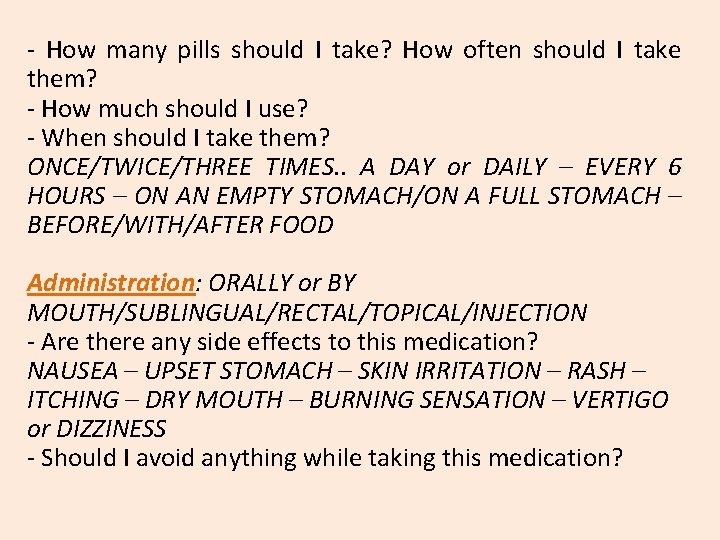
- How many pills should I take? How often should I take them? - How much should I use? - When should I take them? ONCE/TWICE/THREE TIMES. . A DAY or DAILY – EVERY 6 HOURS – ON AN EMPTY STOMACH/ON A FULL STOMACH – BEFORE/WITH/AFTER FOOD Administration: ORALLY or BY MOUTH/SUBLINGUAL/RECTAL/TOPICAL/INJECTION - Are there any side effects to this medication? NAUSEA – UPSET STOMACH – SKIN IRRITATION – RASH – ITCHING – DRY MOUTH – BURNING SENSATION – VERTIGO or DIZZINESS - Should I avoid anything while taking this medication?
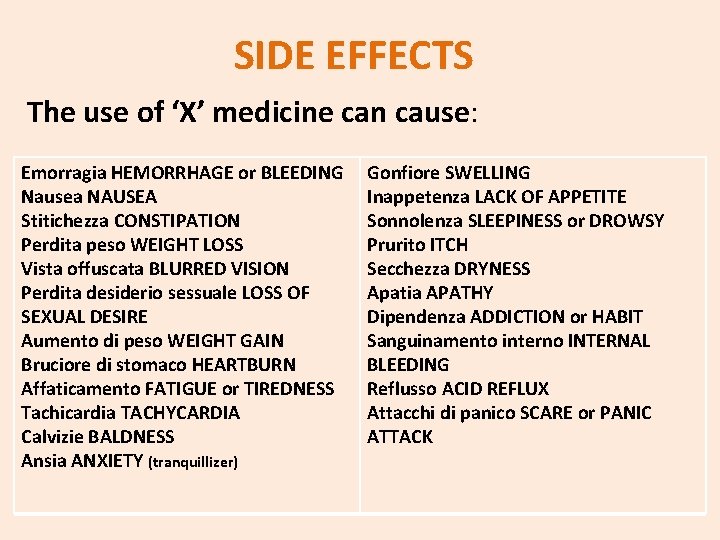
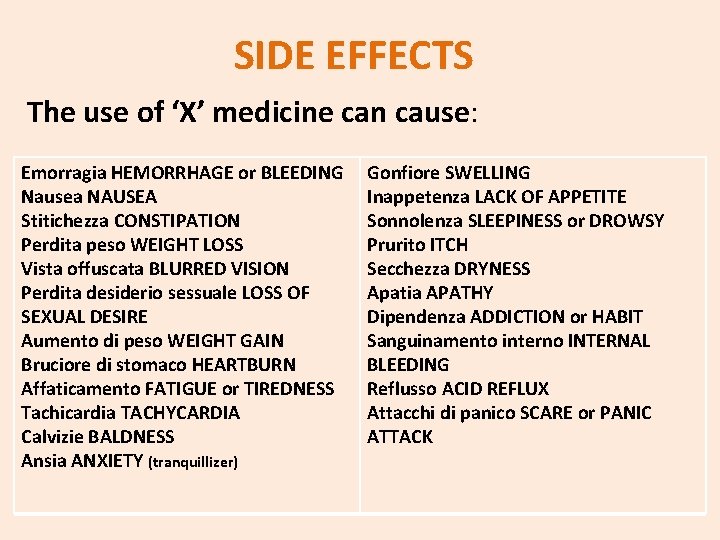
SIDE EFFECTS The use of ‘X’ medicine can cause: Emorragia HEMORRHAGE or BLEEDING Nausea NAUSEA Stitichezza CONSTIPATION Perdita peso WEIGHT LOSS Vista offuscata BLURRED VISION Perdita desiderio sessuale LOSS OF SEXUAL DESIRE Aumento di peso WEIGHT GAIN Bruciore di stomaco HEARTBURN Affaticamento FATIGUE or TIREDNESS Tachicardia TACHYCARDIA Calvizie BALDNESS Ansia ANXIETY (tranquillizer) Gonfiore SWELLING Inappetenza LACK OF APPETITE Sonnolenza SLEEPINESS or DROWSY Prurito ITCH Secchezza DRYNESS Apatia APATHY Dipendenza ADDICTION or HABIT Sanguinamento interno INTERNAL BLEEDING Reflusso ACID REFLUX Attacchi di panico SCARE or PANIC ATTACK
Medicine: a substance that you drink or swallow so as to cure an illness You look so pale. Haven’t you taken your medicine this morning? The doctor prescribed three kinds of medicine for me. Antibiotics: medicine that kills bacteria and cures infections My mum’s throat infection went away after she started the antibiotics. Hot tea won’t be enough to cure your flu, I think you also need antibiotics. Pain killer: kind of medicine that takes away some or all of the discomfort of an illness or injury I had such a horrible headache last night that I took two pain killers. She says she doesn’t think it’s a good idea to take pain killers too often.

(Hypertension treatment) Trade name: Verelan Generic name: verapamil HCl Dosage units: mg Administration units: cap Concentration: Each capsule is 120 mg.
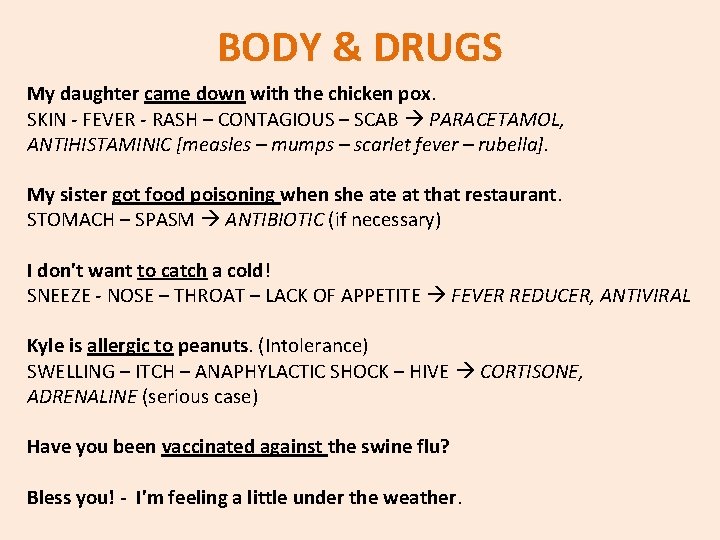
BODY & DRUGS My daughter came down with the chicken pox. SKIN - FEVER - RASH – CONTAGIOUS – SCAB PARACETAMOL, ANTIHISTAMINIC [measles – mumps – scarlet fever – rubella]. My sister got food poisoning when she at that restaurant. STOMACH – SPASM ANTIBIOTIC (if necessary) I don't want to catch a cold! SNEEZE - NOSE – THROAT – LACK OF APPETITE FEVER REDUCER, ANTIVIRAL Kyle is allergic to peanuts. (Intolerance) SWELLING – ITCH – ANAPHYLACTIC SHOCK – HIVE CORTISONE, ADRENALINE (serious case) Have you been vaccinated against the swine flu? Bless you! - I'm feeling a little under the weather.
BODY & DRUGS My THROAT infection went away after I started the antibiotics. The anti-depressants helped me get on with life after Lucy died. The biopsy ruled out a number of illnesses. We're going to remove the cysts just to be on the safe side. People with diabetes have to constantly check their blood sugar levels. INSULIN Your WRIST is fractured and needs a cast. The victim was shot in two places but the bullet wounds are not lifethreatening. I sprained my KNEE playing soccer. ANALGESIC You can see your husband now; he is in a stable condition. You need to take some time off work and relieve some of your stress. SUPPLEMENT, VITAMIN
CAUSES OF INJURY: WHERE IS THE PAIN? ADJECTIVES Pain may be described as being: L Acute - Agonising - Chronic - Constricting Convulsive - Deep-seated - Difficult to move – Diffuse - Excruciating - Intense - Intermittent – Obstinate - Persistent - Radiating - Severe - Sharp – Spasmodic - Spreading – Stupor - Stubborn Unbearable - Very severe – Violent J Ailment - Constant – Dull – Fleeting – Localised – Mild - Numb - Superficial - Tender
NURSE TO PATIENT: Questions Where is your pain? Is there more than one site? What makes your pain worse? Does it cause much pain? What makes your pain better? What previous treatment have you tried to relieve your pain? What words would you use to describe your pain? When did your pain start? When did the symptoms start? How often does it occur? Has its intensity changed? How long does it last? Is there anything you don’t or can’t eat? How intense is the pain, at rest and on movement? You seem to be down today, am I right? Can you describe how the experience made you feel? What kinds of things do you struggle with? What help do you need to deal with your pain? How did you manage that pain?
BEHAVIOURS Restless Angry Confused Depressed Dull Healthy Nervous Not eating Tired Not sleeping Withdrawn Noisy breathing Resistant to movement Unsettled, Agitated Coma: diabetic coma – alcohol intoxication (drunken stupor) – drug induced coma …
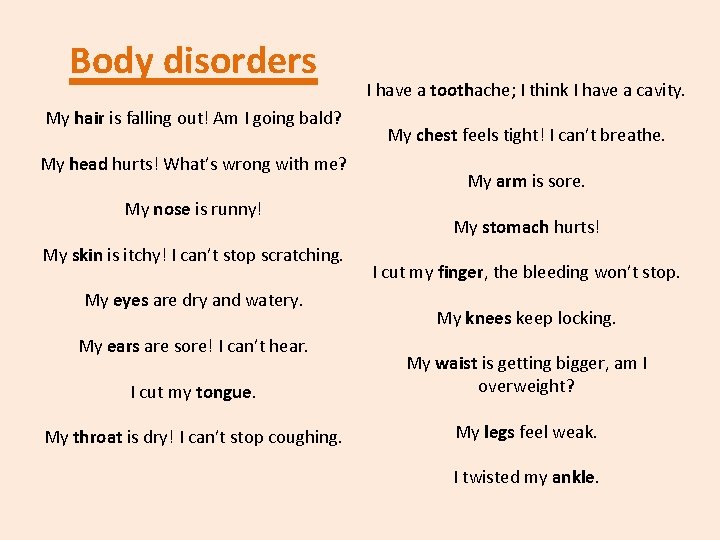
Body disorders My hair is falling out! Am I going bald? My head hurts! What’s wrong with me? My nose is runny! My skin is itchy! I can’t stop scratching. My eyes are dry and watery. My ears are sore! I can’t hear. I have a toothache; I think I have a cavity. My chest feels tight! I can’t breathe. My arm is sore. My stomach hurts! I cut my finger, the bleeding won’t stop. My knees keep locking. I cut my tongue. My waist is getting bigger, am I overweight? My throat is dry! I can’t stop coughing. My legs feel weak. I twisted my ankle.
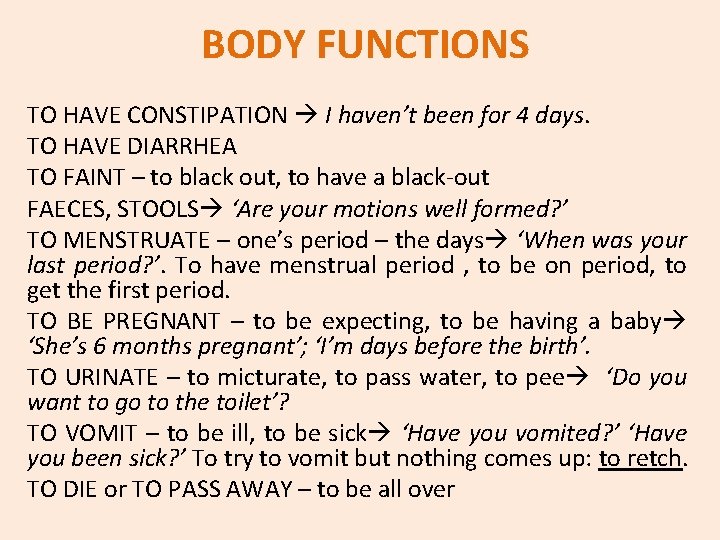
BODY FUNCTIONS TO HAVE CONSTIPATION I haven’t been for 4 days. TO HAVE DIARRHEA TO FAINT – to black out, to have a black-out FAECES, STOOLS ‘Are your motions well formed? ’ TO MENSTRUATE – one’s period – the days ‘When was your last period? ’. To have menstrual period , to be on period, to get the first period. TO BE PREGNANT – to be expecting, to be having a baby ‘She’s 6 months pregnant’; ‘I’m days before the birth’. TO URINATE – to micturate, to pass water, to pee ‘Do you want to go to the toilet’? TO VOMIT – to be ill, to be sick ‘Have you vomited? ’ ‘Have you been sick? ’ To try to vomit but nothing comes up: to retch. TO DIE or TO PASS AWAY – to be all over
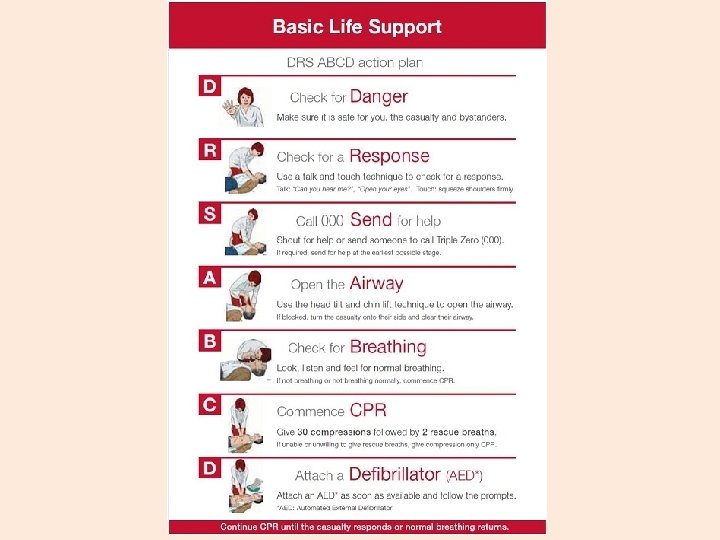
EMERGENCY & FIRST AID Basically, taking care of somebody during an emergency if some bad thing happened, like anything bad that happened when you got injured or wounded, you're going to be receiving first aid before they get you to the hospital where they're going to take care of you. So first aid is the first thing they do when the emergency happened. Somebody will call 911 (112), the emergency medical services. Basically these are the people that send the ambulance and come in the ambulance. They're also called first responders (emergency medic). The people who drive the ambulance are called paramedics. They're going to assess the situation. They're going to look around, see what kind of injury's involved, what kind of action they need to take, for example.
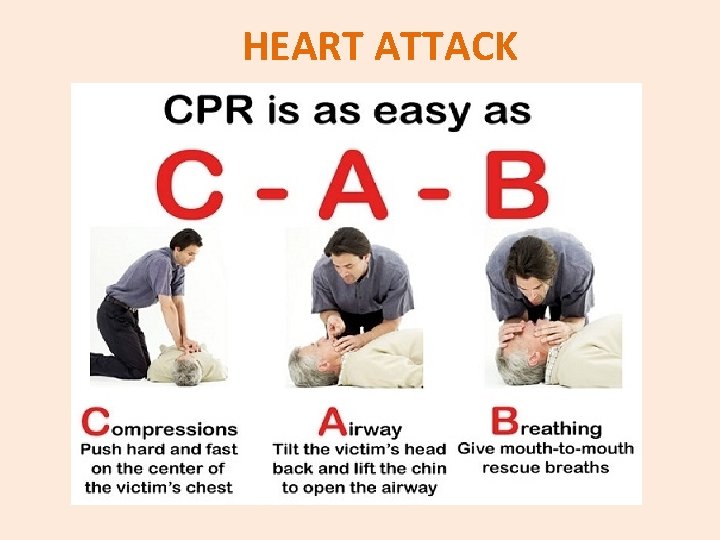
In some cases they're going to have to defibrillate. They're going to use a defibrillator. This is a machine that sends an electric shock into the body. So if someone's having a heart attack, for example, and their heart just stops beating, they're going to take the two paddles, they're going to charge the machine with electricity, going to put them two paddles, and send electricity into the body, get that heart pumping again. Something else they might have to do is give CPR, cardiopulmonary resuscitation. To resuscitate basically means to bring back to life. So CPR, if somebody stops breathing, if the lungs stop pumping air in and out of the body, then they're going to have to give CPR, administer CPR.
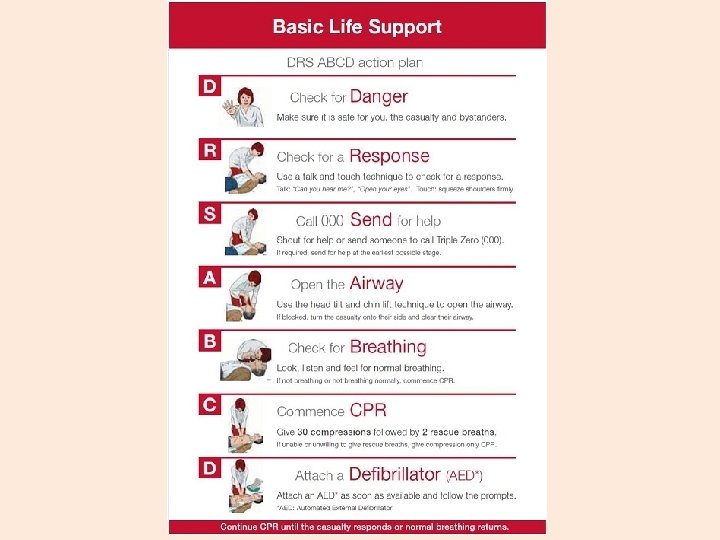
Remember the ABCDs in giving first aid: Check the victim’s Airway, Breathing, perform CPR (if necessary)/ Control major bleeding and Defibrillate, if available (and if necessary). The three P‘s must also be kept in mind when giving first aid: to Preserve life and give initial emergency care and treatment to people who are sick or injured; to Protect unresponsive/ unconscious people; to Prevent the condition of the victim to worsen and to Promote the victim’s recovery.
FIRST AID KIT Thermometer Pain medication and gauze Low grade disinfectant Alcohol rub (hand sanitizer) or antiseptic hand wipes Scissors Adhesive bandages, sticking plasters Tweezers EQUIPMENT USED IN EMERGENCY MEDICINE: Bag valve mask Chest tube Defibrillator Electrocardiogram Intraosseous transfusion Intubation
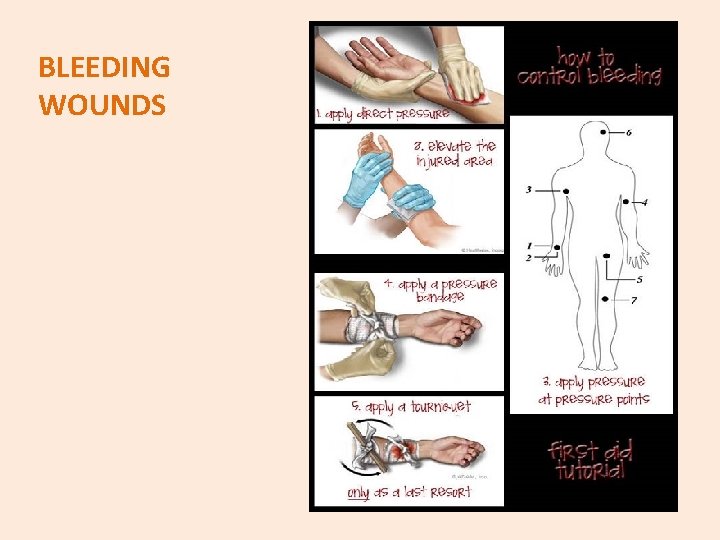
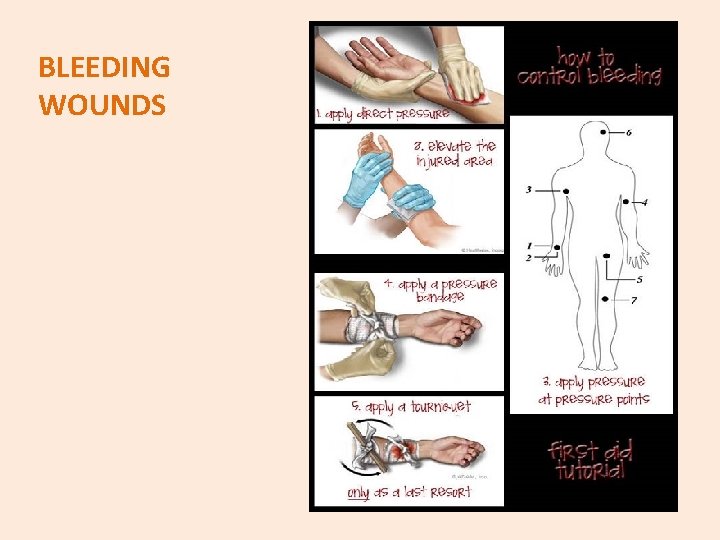
BLEEDING WOUNDS
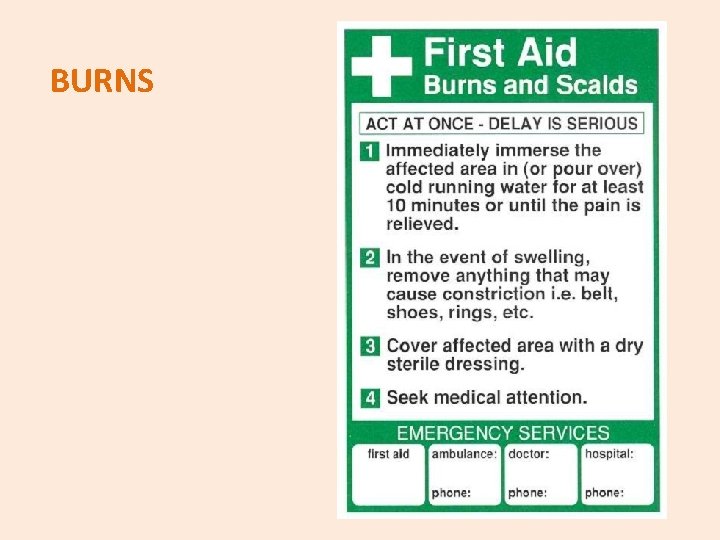
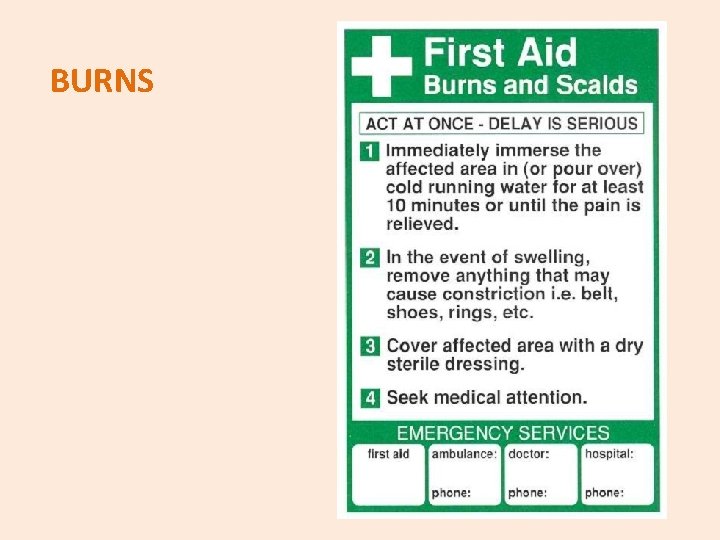
BURNS
SIGNS AND SYMPTOMS The most serious burns are painless and involve all layers of the skin. Fat, muscle and even bone may be affected. Areas may be charred black or appear dry and white.
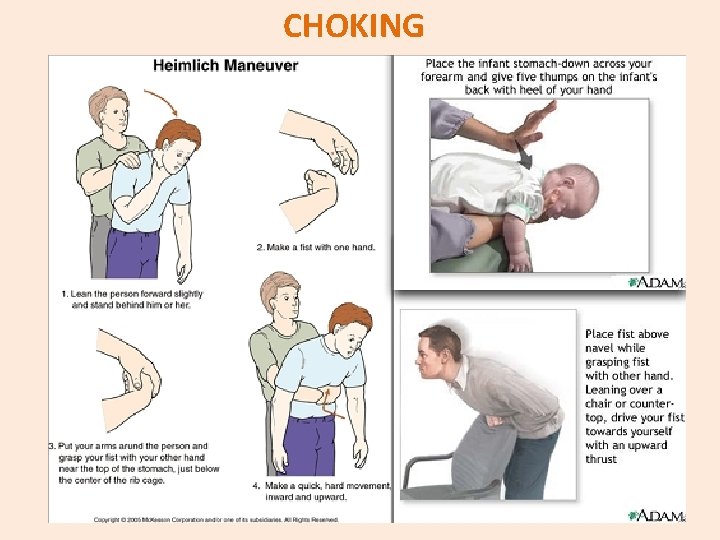
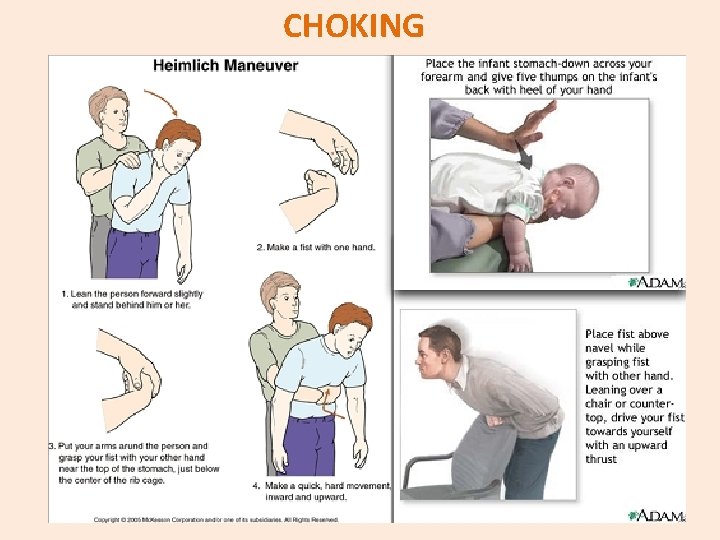
CHOKING
SIGNS AND SYMPTOMS Inability to talk, difficulty in breathing, inability to cough forcefully, skin, lips and nails turning blue, loss of consciousness.
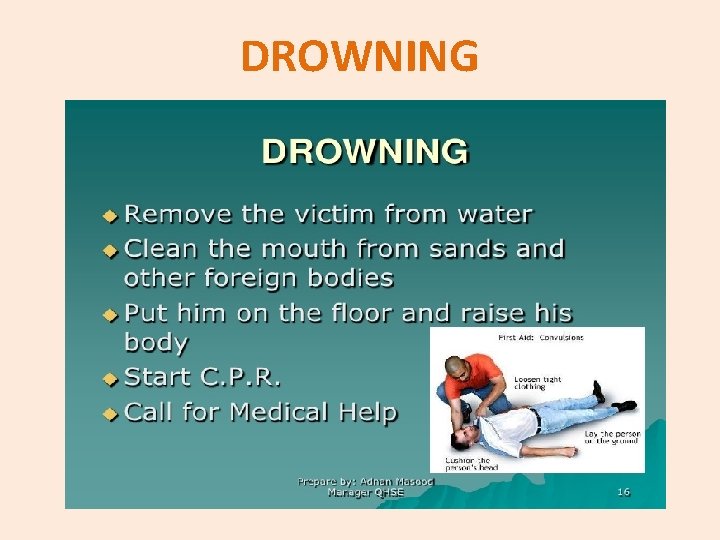
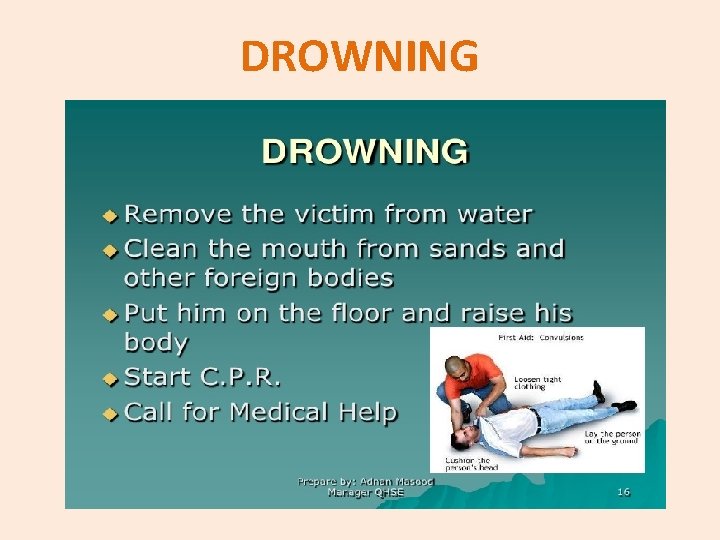
DROWNING
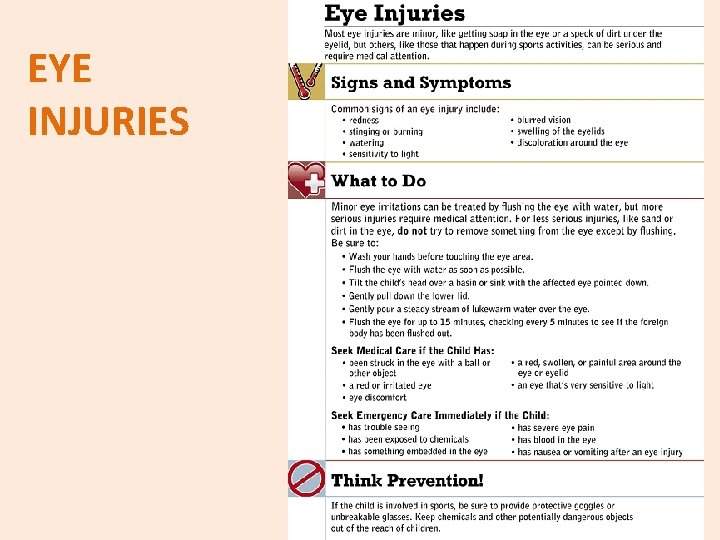
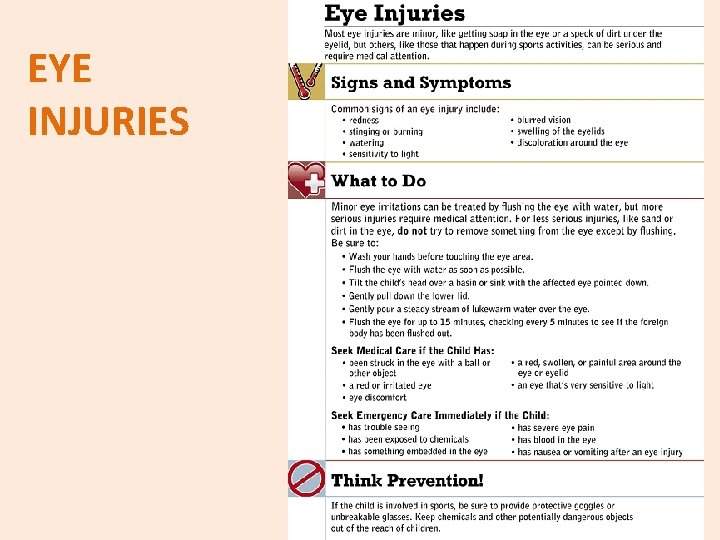
EYE INJURIES
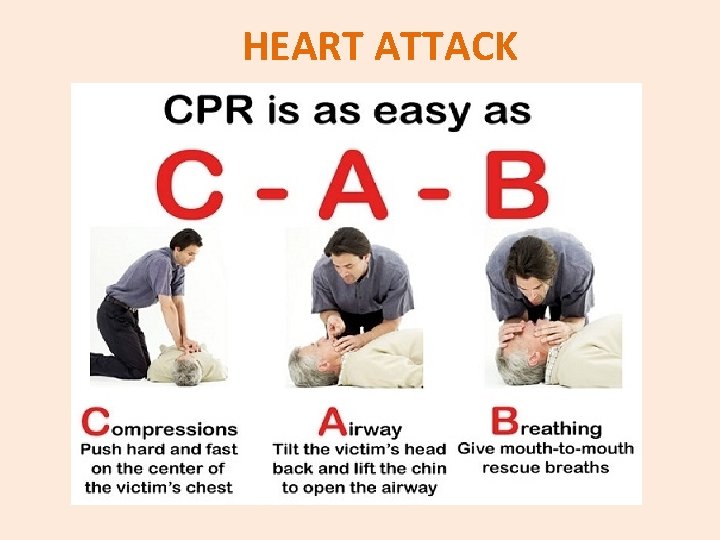
HEART ATTACK
SIGNS AND SYMPTOMS Uncomfortable pressure, fullness pain in the centre of the chest. It may be triggered by exertion and relieved by rest. Prolonged pain in the upper abdomen. Pain spreading beyond the chest to the shoulders, neck, jaw, teeth, one or both arms. Shortness of breath.
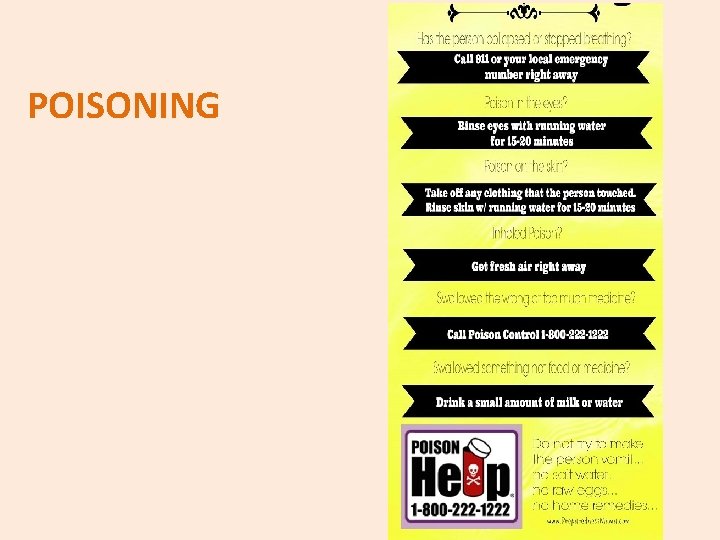
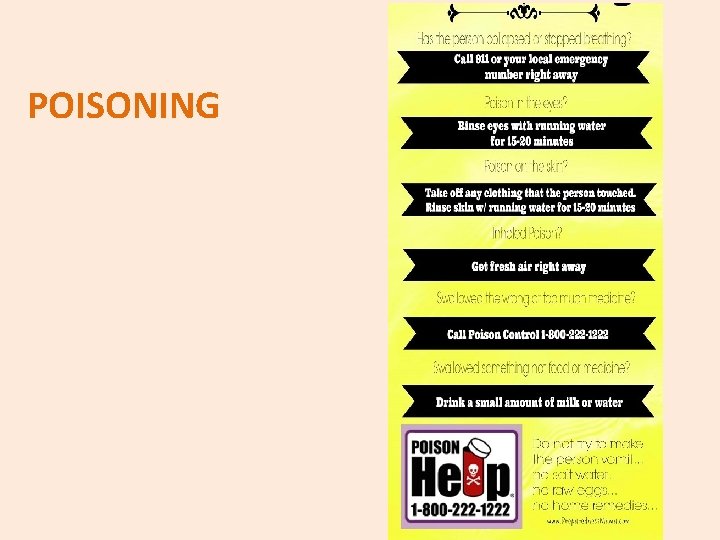
POISONING
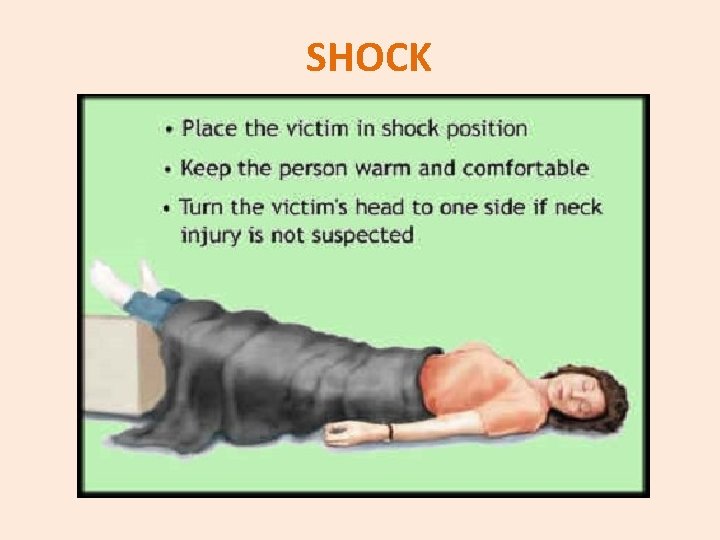
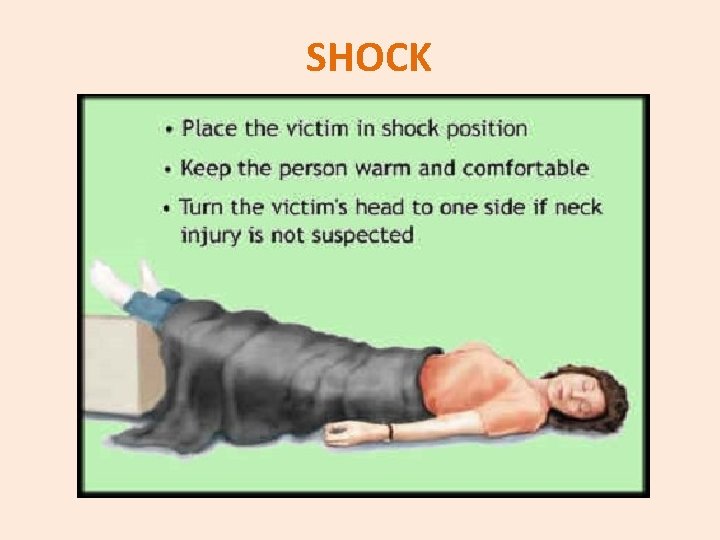
SHOCK
SIGNS AND SYMPTOMS Cool and clammy skin. The pulse is weak and rapid. Breathing may be slow or hyperventilation may occur. Blood pressure is below normal. The eyes may seem to stare. Sometimes the pupils are dilated. The person may be conscious or unconscious. If conscious the person may feel like fainting or be very weak or confused.
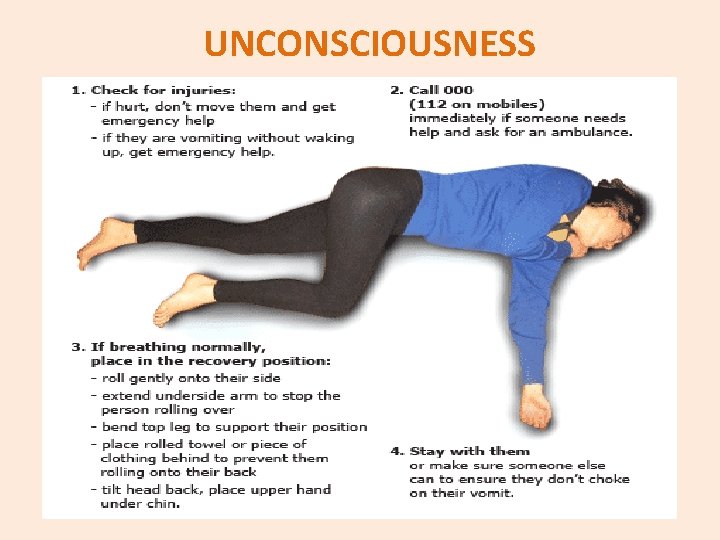
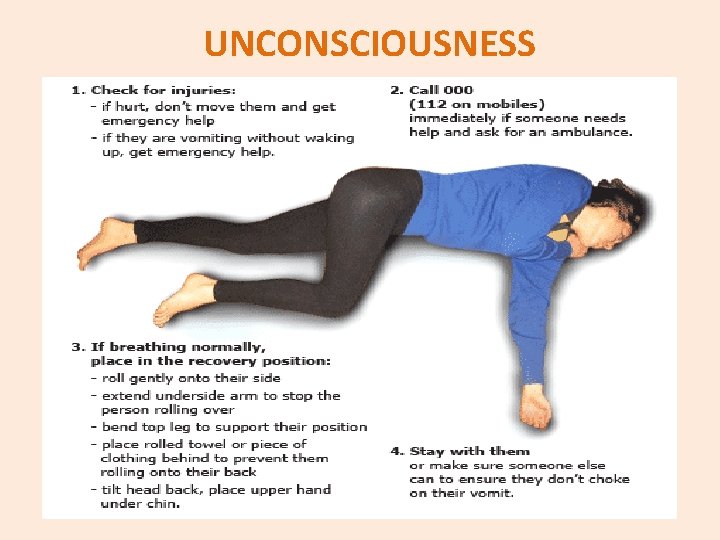
UNCONSCIOUSNESS
SIGNS AND SYMPTOMS Fainting occurs when the blood supply to the brain is momentarily inadequate, causing loss of consciousness.
GIVING INSTRUCTIONS TO PATIENT Can you tilt back your head, please? Can you open your mouth, please? Can you put out your tongue, please? Can you say “ah”, please? Can you look up, please? Can you roll your sleeve up, please? Can you hold out your wrist, please? Can you raise your leg, please? Can you lift your arm, please? Can you bend your arm, please? Can you lower your hand, please? Can you move your fingers, please? Can you lie down, please? Can you sit down, please? Can you undress, please? Can you take your shirt off, please? Can you change into your pyjamas, please?
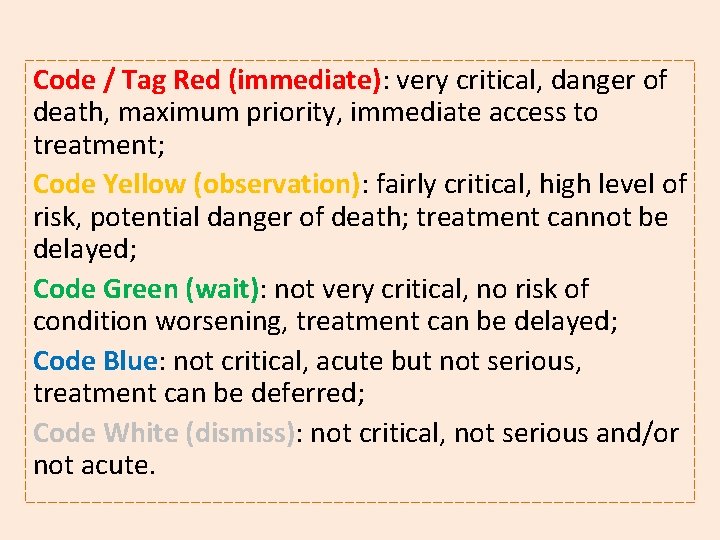
TRIAGE When arriving at the Accident and Emergency department, the patient’s level of urgency will be evaluated by trained nurses. A "colour code" will be given to establish the priority of access to treatment on the basis of the seriousness of the case. This does not depend on the arrival time at the hospital. This approach is called “Triage” and it is aimed at avoiding delays for truly urgent cases. Triage does not guarantee any reduction in waiting times, as its goal is to ensure that patients in extremely serious condition do not have to waste precious time. If more than one person has the same colour code, priority is given to the following: children, pregnant women, people with disabilities, people who have suffered violence, the elderly over 80 and other special categories of patients.
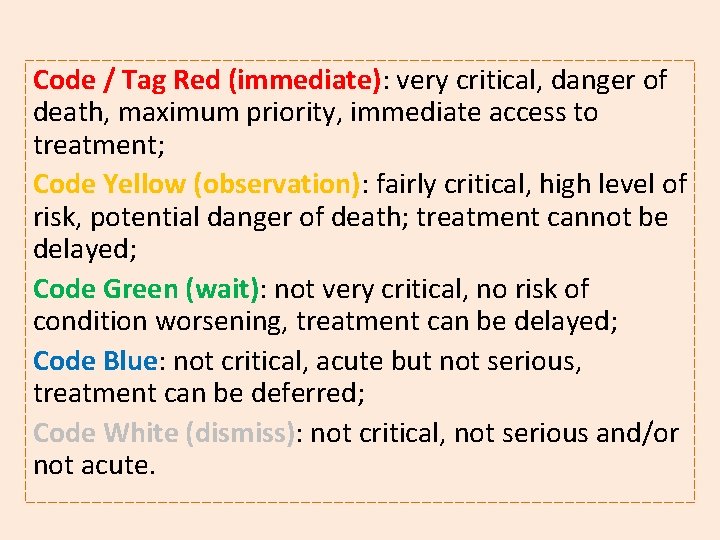
Code / Tag Red (immediate): very critical, danger of death, maximum priority, immediate access to treatment; Code Yellow (observation): fairly critical, high level of risk, potential danger of death; treatment cannot be delayed; Code Green (wait): not very critical, no risk of condition worsening, treatment can be delayed; Code Blue: not critical, acute but not serious, treatment can be deferred; Code White (dismiss): not critical, not serious and/or not acute.
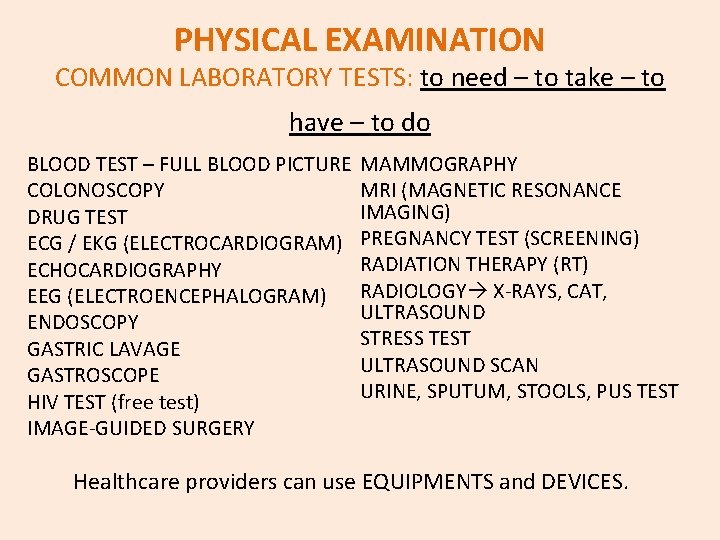
PHYSICAL EXAMINATION COMMON LABORATORY TESTS: to need – to take – to have – to do BLOOD TEST – FULL BLOOD PICTURE COLONOSCOPY DRUG TEST ECG / EKG (ELECTROCARDIOGRAM) ECHOCARDIOGRAPHY EEG (ELECTROENCEPHALOGRAM) ENDOSCOPY GASTRIC LAVAGE GASTROSCOPE HIV TEST (free test) IMAGE-GUIDED SURGERY MAMMOGRAPHY MRI (MAGNETIC RESONANCE IMAGING) PREGNANCY TEST (SCREENING) RADIATION THERAPY (RT) RADIOLOGY X-RAYS, CAT, ULTRASOUND STRESS TEST ULTRASOUND SCAN URINE, SPUTUM, STOOLS, PUS TEST Healthcare providers can use EQUIPMENTS and DEVICES.
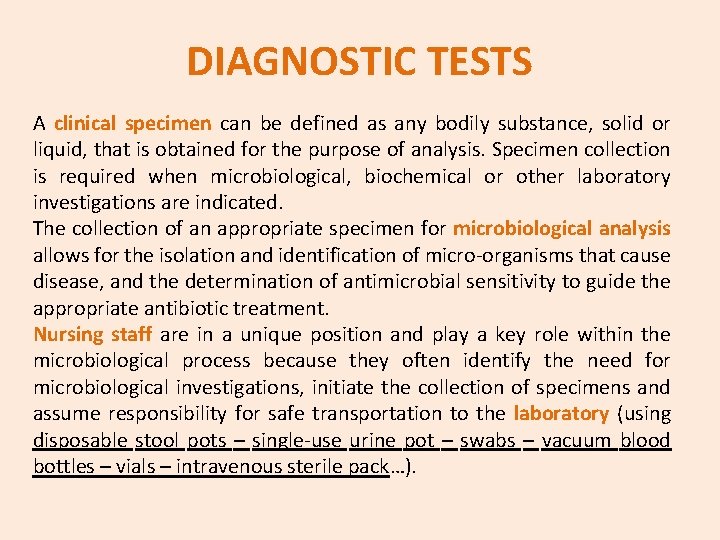
DIAGNOSTIC TESTS A clinical specimen can be defined as any bodily substance, solid or liquid, that is obtained for the purpose of analysis. Specimen collection is required when microbiological, biochemical or other laboratory investigations are indicated. The collection of an appropriate specimen for microbiological analysis allows for the isolation and identification of micro-organisms that cause disease, and the determination of antimicrobial sensitivity to guide the appropriate antibiotic treatment. Nursing staff are in a unique position and play a key role within the microbiological process because they often identify the need for microbiological investigations, initiate the collection of specimens and assume responsibility for safe transportation to the laboratory (using disposable stool pots – single-use urine pot – swabs – vacuum blood bottles – vials – intravenous sterile pack…).

TREATMENTS ACUPUNCTURE CHEMOTHERAPY ELECTRICAL STIMULATIONS HOMEOPATHY HYPNOSIS PALLIATIVE CARE PET THERAPY PHARMACOTHERAPY PHYSICAL THERAPY PSYCHOTHERAPY RADIOTHERAPY SPEECH THERAPY SURGICAL TREATMENT
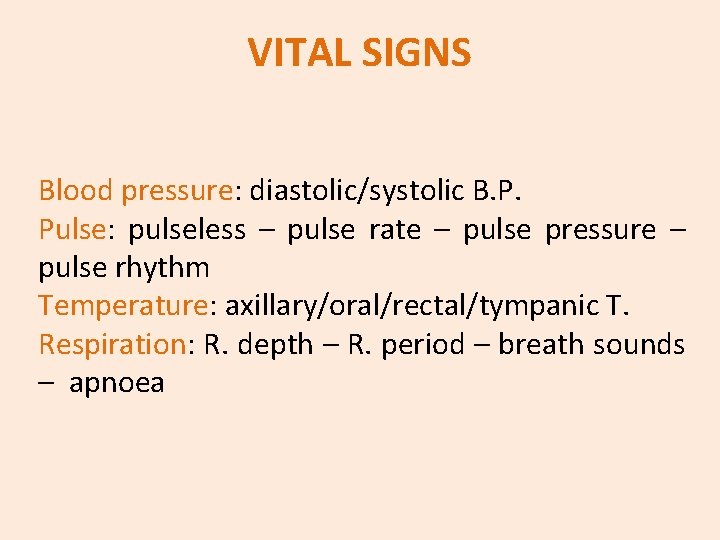
VITAL SIGNS Blood pressure: diastolic/systolic B. P. Pulse: pulseless – pulse rate – pulse pressure – pulse rhythm Temperature: axillary/oral/rectal/tympanic T. Respiration: R. depth – R. period – breath sounds – apnoea
COMPLICATIONS Infection Haemorrhage Herniation Headache Backache Leakage from puncture site High/low pain threshold Fever Bleeding Effusion Thrombosis Water retention Shiver/ Shake
THE MEDICAL HISTORY The history of the present illness begins with a statement of the patient’s: FULL NAME AGE RACE (White/Caucasian, Black, American Indian, Hispanic, Chinese. . ) SEX OCCUPATION CHIEF COMPLAINT (symptoms, location, intensity, duration, alleviation, social habits, family history, allergies. . )
Patient’s habits: smoking (if positive “how many cigarettes per day have you smoked for how many years? ” – alcohol – drugs – all medication at present being taken – contraceptive pill – over the-counter drugs (e. g. painkillers); Past medical history: major acute and chronic illnesses – operations; Family history: chronic illnesses of the immediate family; Social history: marital status – number of children – education – present occupation.
REVIEW OF SYSTEMS In this part of history the nurse/doctor asks: ANY RECENT WEIGHT CHANGE FEVER NIGHT SWEATS BLEEDING DIZZINESS …
BODY PARTS HEAD: loss of hearing – tinnitus – dental problems – sore throat – hoarse voice; BREAST: any lumps or discharge; RESPIRATORY SYSTEM: any cough – shortness of breath – chest pain; CARDIOVASCULAR SYSTEM: angina pectoris – palpitations – blood cots – hypertension; GASTROINTESTINAL S. : heartburn – indigestion – nausea – constipation; GENITOURINARY S. : incontinence – urinary tract infections – kydney stone (gallstone).
THE CASE DESCRIPTION Mr. James is a 57 year old gentleman admitted to room 224 A two days ago for dehydration secondary to nausea and vomiting for three days. His sclera is slightly yellowed and his abdomen is distended and tender to palpation especially in the upper right quadrant. After two days of IV lasix therapy, he has 2+ edema in his lower extremities to the mid calf. (At admission he had 4+ edema up to the knee. ) He complains of mild shortness of breath with moderate activity which he has experienced for several weeks. He has a history of alcohol abuse for 20 years, but denies any use for the past 6 months. He has no history of hepatitis or HIV. No history of drug abuse. At 7: 45 AM, Mr. James is complaining of increasing nausea. He has had no emesis for at least 5 hours, but feels (and fears) the need to vomit is becoming imminent. His last dose of anti-emetic (Tigan) was given at 4: 30 AM and he states “it only slightly relieved the nausea this time. ” It let him sleep for about two hours, but now he’s “wide awake and very uncomfortable. ” The orders for the Tigan are 200 milligrams (2 ml)IM QID (four times a day), and is scheduled every six hours. It has only been a little over three hours since the last dose and is not due again until 10: 30 AM. You tell him you will have to contact the MD (Doctor of Medicine) for orders for something else.
Mr. James is reluctant to have you do this and thinks that if he can wait about 30 minutes, the MD is likely to be making his morning rounds. Mr. James wants to try to wait. He thinks he “can control the urge to vomit more it if he can get more comfortable in the bed. ” A quick assessment of vital signs and his body systems reveals no change in condition. In assessing Mr. James, you determine that measures which usually help him to reduce his nausea include using a cold cloth on his forehead and one on the back of his neck. He is usually more comfortable lying on his left side, but is on his right side now because he’s trying to comply with the need to alternate the pressure on his skin. It has been about an hour that he’s been on his right side. Turning can increase his nausea, but doing so slowly may be OK. You assist him to slowly turn and find a more comfortable position. You place the cold cloths on his forehead and the back of his neck, and he reports feeling “much better already. ” Slow deep breaths also help him to relax, as well as minimizing distractions such as the TV, lights and closing the door to the room. Pulling the curtains around his bed further isolate him and allow him to relax and concentrate on his slow breathing. In a few minutes he is sleeping.
How do you document your assessment and intervention? The Who: Mr. James in 224 A The What: the increased nausea and fear of imminent emesis The When: began with the fact that the last dose of Tigan did not completely relieve the nausea The Where: Mr. James lying in his bed on his right side (to alternate the pressure on his skin) The Why: the nausea is presumed to be due to an exacerbation of his cirrhosis but it’s unclear why the Tigan was ineffective this time. The patient states he thinks “lying on my right side is so uncomfortable that I can’t relax and let the medication work. ” [Use patient quotes for subjective details].
The How - the intervention: No apparent significant change in condition noted. At this time, patient requests to try other measures and to wait for MD assessment before requesting additional medications. Assisted patient to turn slowly to his left side without incident. Placed cold cloths on his forehead and back of his neck as requested. Patient reports feeling immediately “much better. ” Reduced outside stimuli including turning off the TV, turning off the lights, closing the door and drawing the curtain around the bed. Patient performed deep breathing and relaxation techniques as instructed. Patent able to fall asleep within 5 minutes without further c/o nausea and no vomiting. Expect MD to make rounds within the hour.
NARCOTICS - ADDICTIVE SUBSTANCES (natural or chemicals) - DRUG ADDICT / ADDICT - STRONG CRAVINGS FOR DRUGS - TO BE HIGH - WITHDRAWAL, ABSTINENCE (going through ~; ~ from. . . ) - DETOXIFICATION
AMPHETAMINES It is also a diet pills prescribed by doctors; Stimulants accellerate brain functions TAKING, USE: smoked – swallowed – snorted (sniffed) – injected WHAT IT DOES: fast high – powerful – alert – energized SYMPTOMS: sweating – headaches – no sleep – shaking – blurred vision – hallucinations – paranoia AFTER: aggression – anxiety CALLED: speed – uppers – truck drivers
GAMMA HYDROXYBUTYRATE It is a clear liquid; no odour, no colours. The “drug of rave parties” like ecstasy, mixed with alcohol has a depressant effect. Takers can go into coma. USE: swallowed in liquid – powder form or tablets EFFECTS: hallucinations – euphoric – high – dizziness – vomiting – vision changes – nausea – drowsiness – no breathing. CALLED: liquid ecstasy – G - georgia
METHAMPHETAMINES Stimulants give ability to stay awake and active. FORMS: pills – powders – crystals USE: swallowed – inhaled – smoked – injected into a vein WHAT IT DOES: intense high – rush and flash – full energy damage to brain SIDE EFFECTS: high blood pressure – sweating – hot flashes – dizziness – dry mouth – headaches – blurred vision – no appetite – mood swings – violent behaviour – convulsions CALLED: ice – speed – xmas tree – chalk - crystalmeth
COCAINE - CRACK FORMS: COCAINE white powder from dried leaves of coca plant / CRACK obtained by cooking coca powder with baking soda USE: inhaled – snorted through the nose – injected crack is smoked in a pipe EFFECTS: stimulant for energy and intense power – fast heart beat – high blood pressure (possible strokes and death) AFTER USE: depressed – nervous – craves of drugs to feel good again CALLED: rock – snow – blow – candy – smack – powder
MARIJUANA Illegal drug from chopped leaves or seeds and flowers of cannabis. USE: smoked in hand-rolled cigarettes – in a pipe or water pipe (bong) EFFECTS: difficulty with memory – raising of blood pressure and heart rate- red eyes – dry mouth – sleepy – paranoid – cough – respiratory infections – colds – pupil enlargement CALLED: grass – joint – herb – cannabis – hashish – maryjane - pot
HEROIN It comes from a flower called opium poppy. Codeine and Morphine are legal and prescribed for pain relief. It is an illegal narcotic. USE: injected with needles – smoked – inhaled EFFECTS: users feel high and relaxed – nausea – drowsiness – needle marks or tracks – needle sharing germs like hepatitis B or C, HIV WITHDRAWAL SYMPTOMS: feeling of panic – sleeplessness – bad chills – sweats – muscle pain – cramps – vomiting – diarrhea – overdose – death CALLED: shock – glut - overkill
FOOD AND DIET A healthy diet should: • emphasise fruits, vegetables, whole grain, fat free or low fat milk and milk products; • include lean meats, poultry, fish, beans, eggs and nuts; • be low in saturated fats, cholesterol, salt (sodium), added sugars. COMPONENTS OF A BALANCED DIET (healthy diet pyramid): carbohydrates – fats – grains – minerals – oils – proteins – roughage – starch – sugars – vitamins.
KINDS OF DIET Absolute diet – fasting Adequate diet Balanced diet High-caloric diet Low salt diet Low fat diet Mediterranean diet
EATING DISORDERS Anaemia Anorexia Binge eating Bulimia Cirrhosis Dehydration Gout Indigestion Nutritional deficiencies Obesity Overweight
PREGNANCY It lasts 40 weeks, starting from the first day of the last menstrual period. Some women choose to have amniocentesis, a test that is diagnostic for genetic disorders. DIFFERENT KIND OF PREGNANCY: bigeminal pregnancy – extrauterine – false – high-risk – hysteric – post-term

COMMON WORDS Amniotic fluid Amniotic sac Artificial insemination Blood show Embryo Fertilisation Foetus Gestation Ovum Placenta Stretch marks Umbilical cord Uterus Zygote
ROUTINE TESTS - DISORDERS Pregnancy test – blood tests – scans – manual palpation of abdomen – double-test – glycaemia. Anxiety – backache – dizziness – constipation – fainting – irritability – fatigue – frequent urination – morning sickness – painful joints and bones – stretch marks – swollen ankles – varicose veins PREGNANCY INTERRUPTION abortion – foetal death – miscarriage / spontaneous abortion.
CHILDBIRTH DISORDERS: burps – colic – cradle cap – nappy rash – reflux – breast milk jaundice – cleft lip – hydrocephalus – Down’s syndrome – squint – sudden infant death syndrome (SIDS) / cot death – umbilical hernia EQUIPMENT: breast-pump – bottle – changing table – cleaning brush – cot – cradle – dummy – napkin/nappy – pram – steriliser - teat

COMMON DISEASES ALCOHOLISM ALLERGY ANAEMIA APPENDICITIS ARTHRITIS ASTHMA BRONCHITIS CANCER CATARACT CONJUNCTIVITIS CONSTIPATION CYSTITIS DENTAL CARIES DEPRESSION DERMATITIS DIABETES
EPILEPSY GALLSTONE HEART ATTACK HERNIA HYPERTENSION INDIGESTION LEUKEMIA MIGRAINE MULTIPLE SCLEROSIS OTITIS RHEUMATISM RHINITIS SCIATICA SINUSITIS STROKE TONSILLITIS TUMOUR ULCER

SIGNS & SYMPTOMS BLISTER BOIL BRUISE CUT INJURY ITCH LACERATION LESION SCAB SCRATCH STING WOUND