3 Steps to Successful Obesity Management Learning objectives

3 Steps to Successful Obesity Management
Learning objectives • Review recent findings about the biologic regulation of eating and weight control • Discuss the clinical recommendations and benefits of sustained weight loss in overweight and obese patients • Apply principles of motivational interviewing and shared decision-making to improve the clinical management of obesity and promote behavioral changes • Understand current guidelines for managing obesity, including the role of pharmacological therapy as an adjunct to lifestyle changes in reducing weight gain and promoting weight loss • Review reimbursement options for intensive behavioral therapy (IBT) in obesity management
Disclosures • Brought to you by a medical education collaboration between the Louisiana Association of Nurse Practitioners and the Endocrine Society • Developed by Knighten Health. • Supported by an unrestricted education grant from Novo Nordisk Inc. • Connie Hale, DNP, APRN, FNP-BC: No relevant financial relationships with any commercial interests
Weight First Initiative • The Endocrine Society engaged four health care practitioners -- an internist, a family practice physician, an osteopathic practitioner, and a nurse practitioner -- in a pilot program to collaborate with faculty on the Guidelines on Pharmacologic Management of Obesity to develop a curriculum for primary care practitioners in obesity medical management best practices. • The objective of the Weight First initiative 2016 pilot is to demonstrate that an obesity curriculum co-developed by endocrinologists and primary care practitioners overcomes barriers to the effective management of patients with obesity. • The goal was to encourage primary care practitioners to treat weight first, rather than treating co-morbidities without directly addressing weight as a factor in overall health.
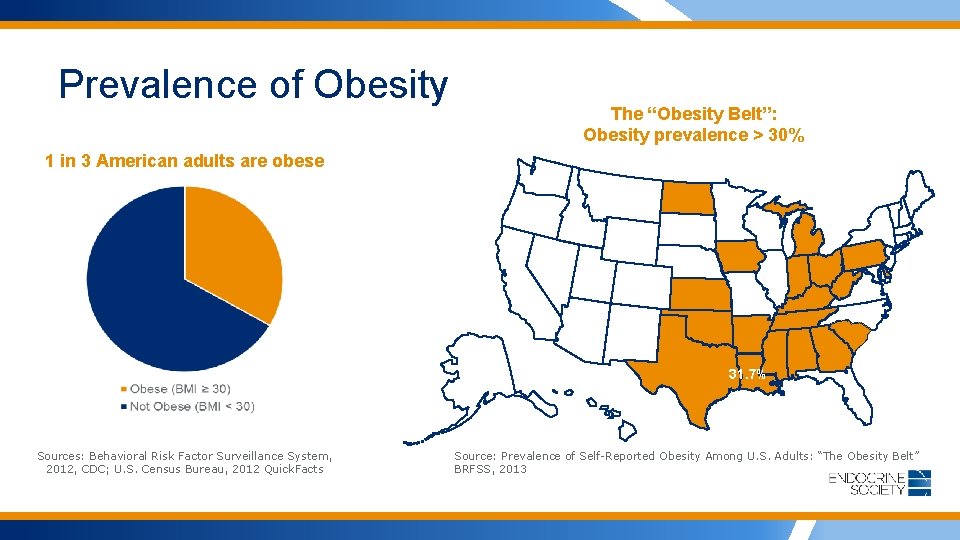
Prevalence of Obesity The “Obesity Belt”: Obesity prevalence > 30% 1 in 3 American adults are obese 31. 7% Sources: Behavioral Risk Factor Surveillance System, 2012, CDC; U. S. Census Bureau, 2012 Quick. Facts Source: Prevalence of Self-Reported Obesity Among U. S. Adults: “The Obesity Belt” BRFSS, 2013
What are the 3 Steps to Successful Obesity Management? Step 1: Motivational Interviewing Step 2: Therapeutic options Step 3: Reimbursement
The case for putting weight first
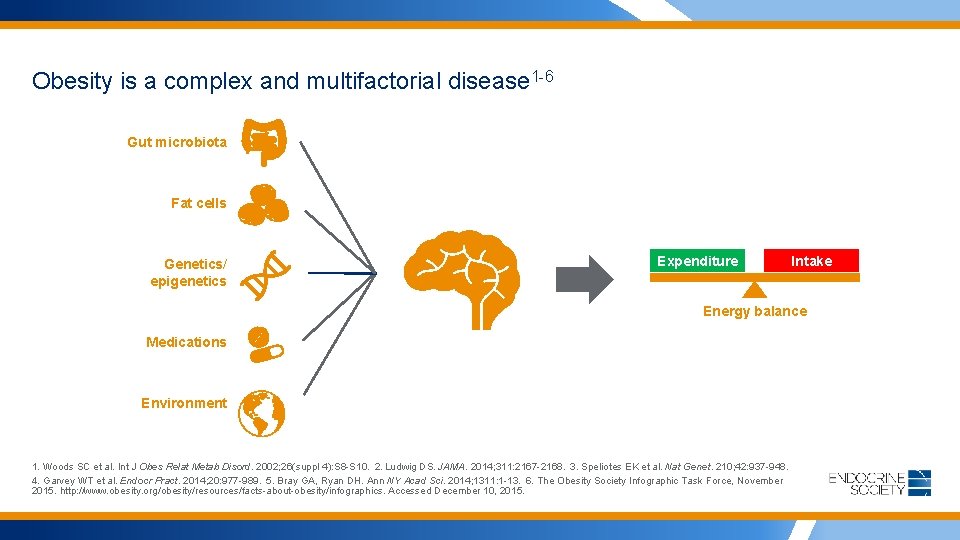
Obesity is a complex and multifactorial disease 1 -6 Gut microbiota Fat cells Genetics/ epigenetics Expenditure Intake Energy balance Medications Environment 1. Woods SC et al. Int J Obes Relat Metab Disord. 2002; 26(suppl 4): S 8 -S 10. 2. Ludwig DS. JAMA. 2014; 311: 2167 -2168. 3. Speliotes EK et al. Nat Genet. 210; 42: 937 -948. 4. Garvey WT et al. Endocr Pract. 2014; 20: 977 -989. 5. Bray GA, Ryan DH. Ann NY Acad Sci. 2014; 1311: 1 -13. 6. The Obesity Society Infographic Task Force, November 2015. http: //www. obesity. org/obesity/resources/facts-about-obesity/infographics. Accessed December 10, 2015.
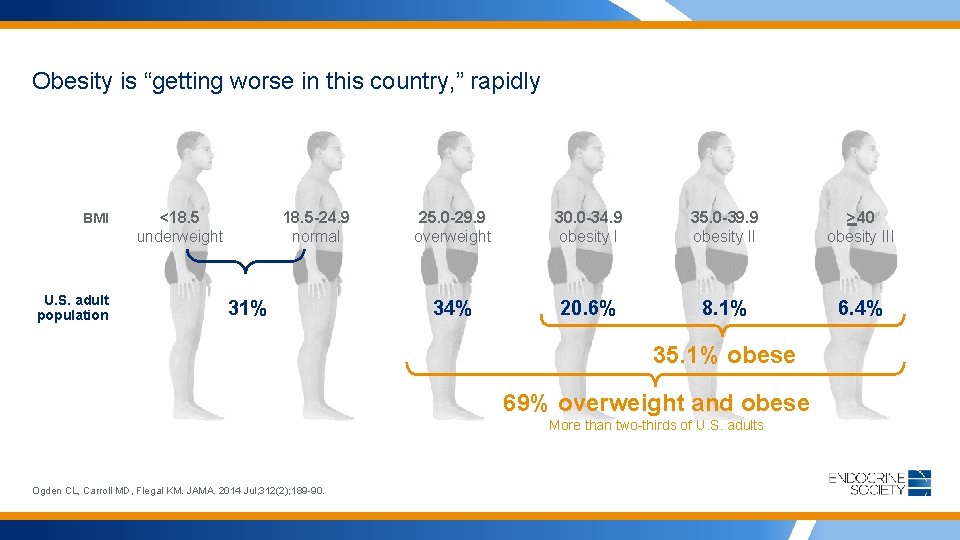
Obesity is “getting worse in this country, ” rapidly BMI U. S. adult population <18. 5 underweight 18. 5 -24. 9 normal 31% 25. 0 -29. 9 overweight 30. 0 -34. 9 obesity I 35. 0 -39. 9 obesity II >40 obesity III 34% 20. 6% 8. 1% 6. 4% 35. 1% obese 69% overweight and obese More than two-thirds of U. S. adults Ogden CL, Carroll MD, Flegal KM. JAMA. 2014 Jul; 312(2); 189 -90.
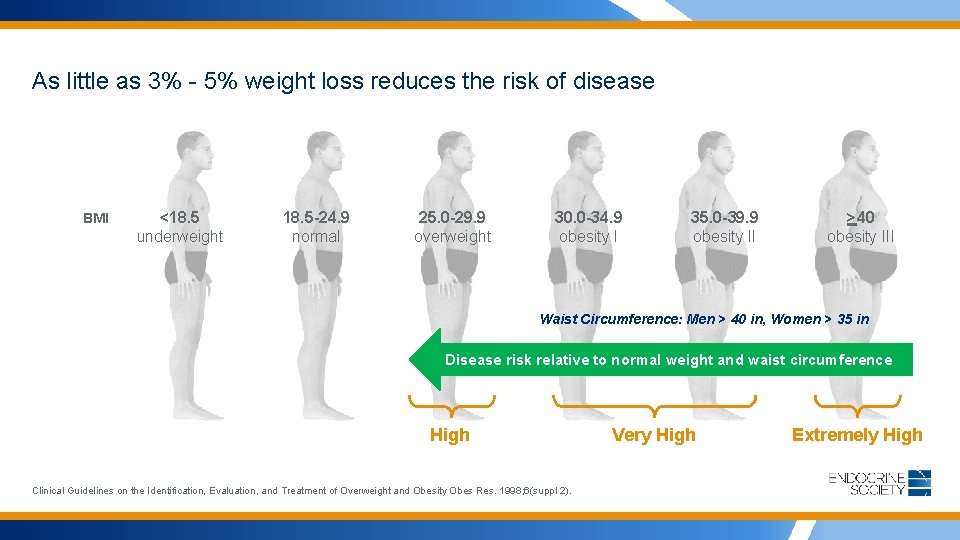
As little as 3% - 5% weight loss reduces the risk of disease BMI <18. 5 underweight 18. 5 -24. 9 normal 25. 0 -29. 9 overweight 30. 0 -34. 9 obesity I 35. 0 -39. 9 obesity II >40 obesity III Waist Circumference: Men > 40 in, Women > 35 in Disease risk relative to normal weight and waist circumference High Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity Obes Res. 1998; 6(suppl 2). Very High Extremely High
Why is losing weight and keeping it off so difficult?
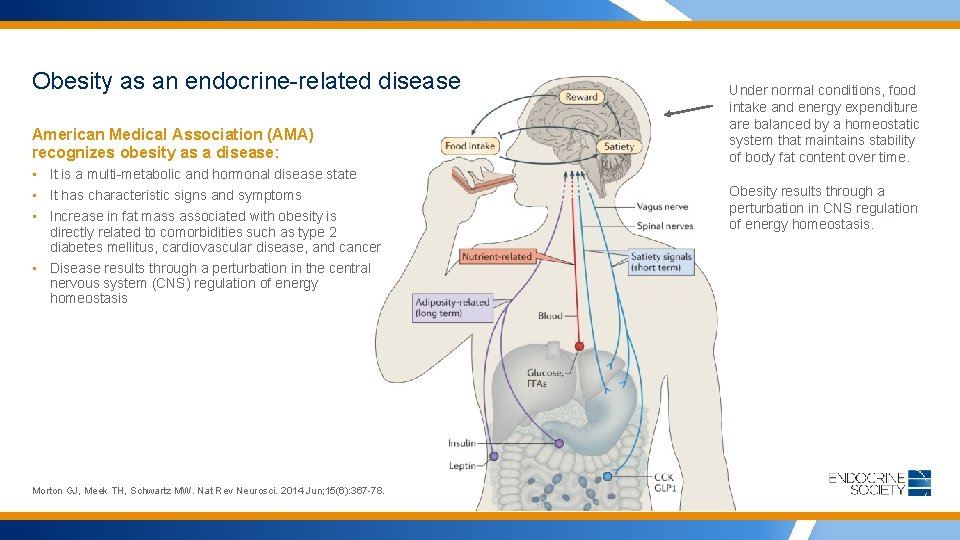
Obesity as an endocrine-related disease American Medical Association (AMA) recognizes obesity as a disease: • It is a multi-metabolic and hormonal disease state • It has characteristic signs and symptoms • Increase in fat mass associated with obesity is directly related to comorbidities such as type 2 diabetes mellitus, cardiovascular disease, and cancer • Disease results through a perturbation in the central nervous system (CNS) regulation of energy homeostasis Morton GJ, Meek TH, Schwartz MW. Nat Rev Neurosci. 2014 Jun; 15(6): 367 -78. Under normal conditions, food intake and energy expenditure are balanced by a homeostatic system that maintains stability of body fat content over time. Obesity results through a perturbation in CNS regulation of energy homeostasis.
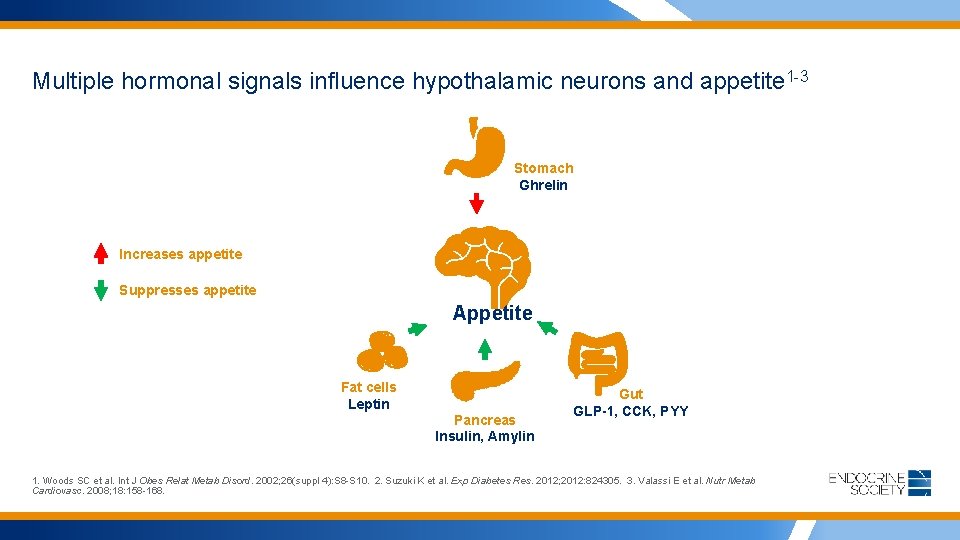
Multiple hormonal signals influence hypothalamic neurons and appetite 1 -3 Stomach Ghrelin Increases appetite Suppresses appetite Appetite Fat cells Leptin Pancreas Insulin, Amylin Gut GLP-1, CCK, PYY 1. Woods SC et al. Int J Obes Relat Metab Disord. 2002; 26(suppl 4): S 8 -S 10. 2. Suzuki K et al. Exp Diabetes Res. 2012; 2012: 824305. 3. Valassi E et al. Nutr Metab Cardiovasc. 2008; 18: 158 -168.
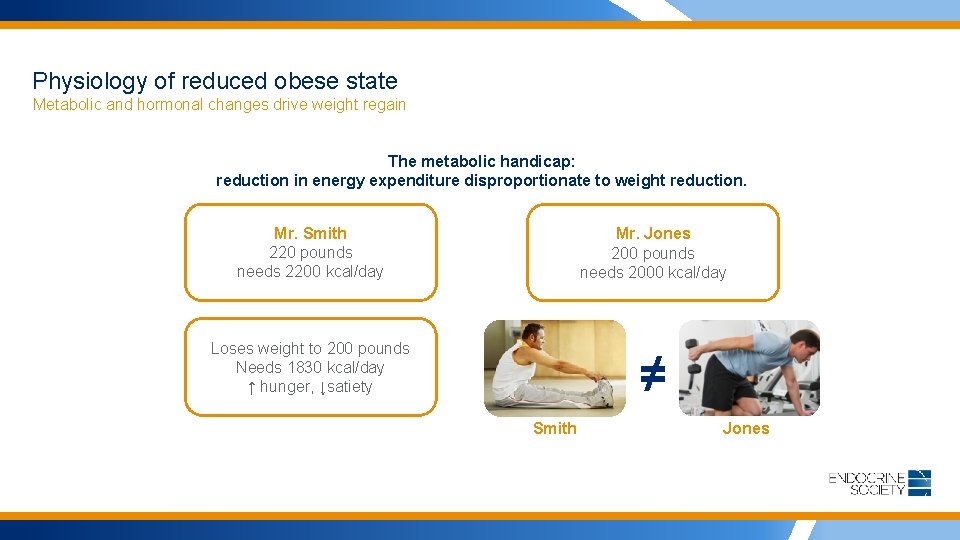
Physiology of reduced obese state Metabolic and hormonal changes drive weight regain The metabolic handicap: reduction in energy expenditure disproportionate to weight reduction. Mr. Smith 220 pounds needs 2200 kcal/day Mr. Jones 200 pounds needs 2000 kcal/day Loses weight to 200 pounds Needs 1830 kcal/day ↑ hunger, ↓satiety ≠ Smith Jones
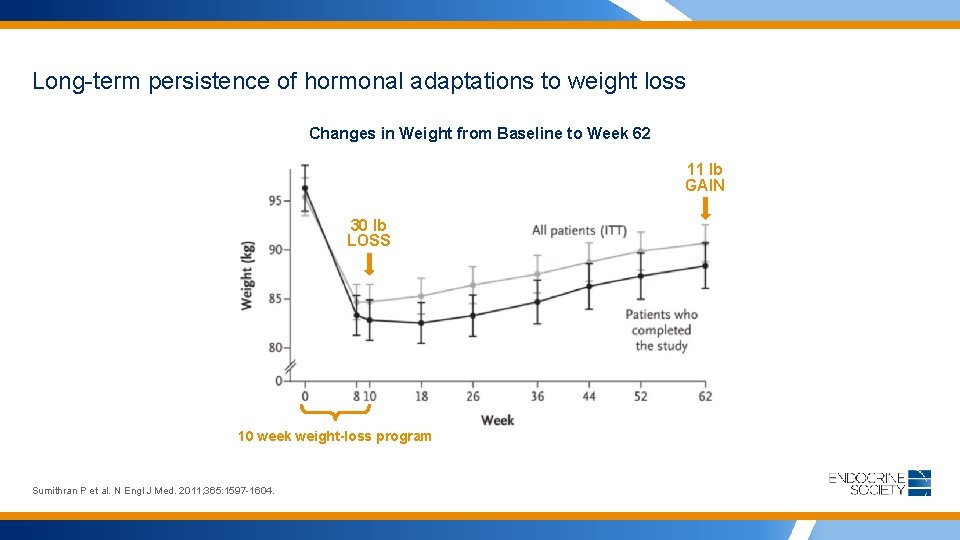
Long-term persistence of hormonal adaptations to weight loss Changes in Weight from Baseline to Week 62 11 lb GAIN 30 lb LOSS 10 week weight-loss program Sumithran P et al. N Engl J Med. 2011; 365: 1597 -1604.
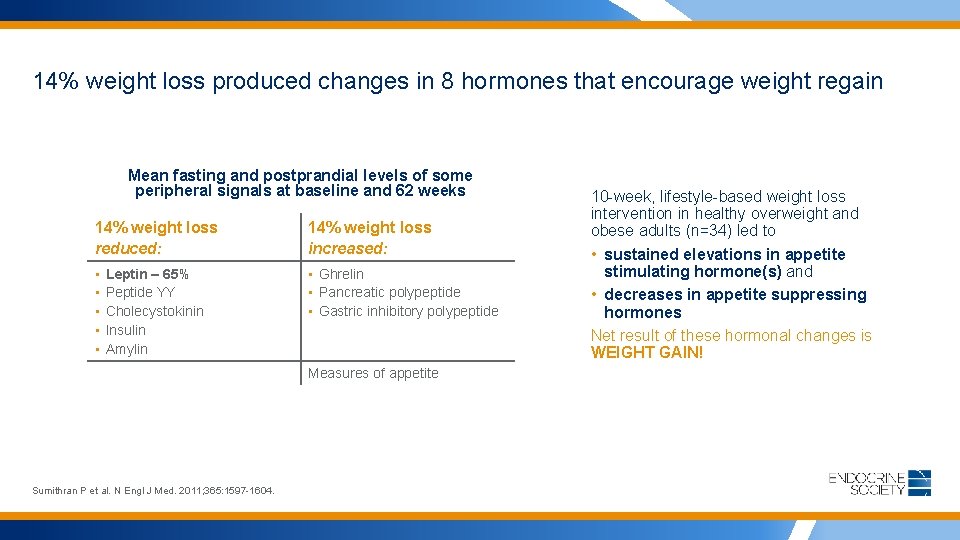
14% weight loss produced changes in 8 hormones that encourage weight regain Mean fasting and postprandial levels of some peripheral signals at baseline and 62 weeks 14% weight loss reduced: 14% weight loss increased: • • • Ghrelin • Pancreatic polypeptide • Gastric inhibitory polypeptide Leptin – 65% Peptide YY Cholecystokinin Insulin Amylin Measures of appetite Sumithran P et al. N Engl J Med. 2011; 365: 1597 -1604. 10 -week, lifestyle-based weight loss intervention in healthy overweight and obese adults (n=34) led to • sustained elevations in appetite stimulating hormone(s) and • decreases in appetite suppressing hormones Net result of these hormonal changes is WEIGHT GAIN!
What are the risks of overweight? How much weight loss is needed for health benefit?
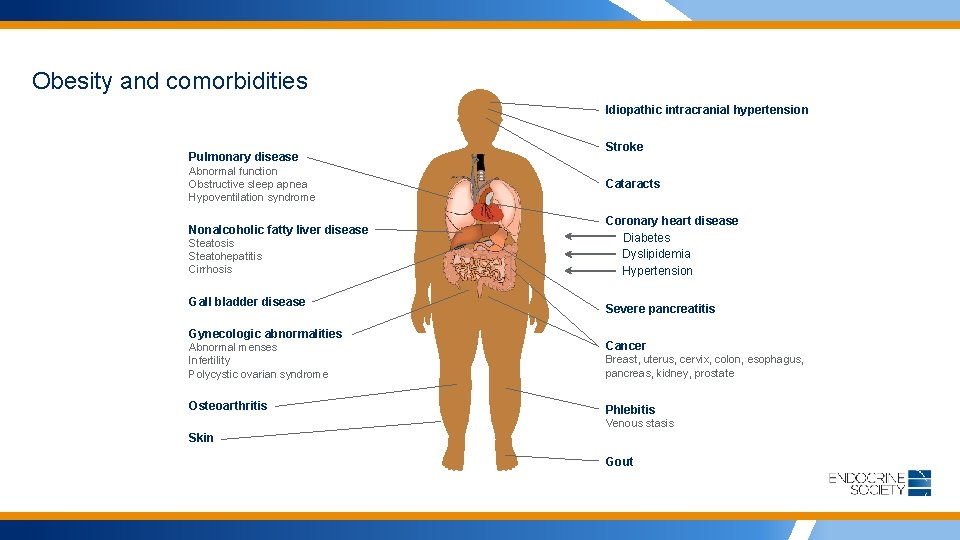
Obesity and comorbidities Idiopathic intracranial hypertension Pulmonary disease Abnormal function Obstructive sleep apnea Hypoventilation syndrome Nonalcoholic fatty liver disease Steatosis Steatohepatitis Cirrhosis Gall bladder disease Gynecologic abnormalities Stroke Cataracts Coronary heart disease Diabetes Dyslipidemia Hypertension Severe pancreatitis Abnormal menses Infertility Polycystic ovarian syndrome Cancer Osteoarthritis Phlebitis Breast, uterus, cervix, colon, esophagus, pancreas, kidney, prostate Venous stasis Skin Gout
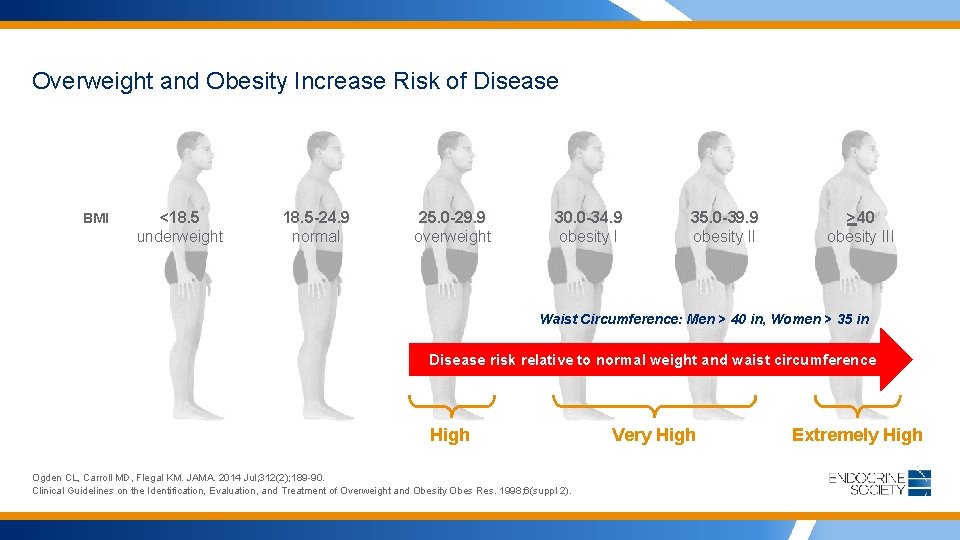
Overweight and Obesity Increase Risk of Disease BMI <18. 5 underweight 18. 5 -24. 9 normal 25. 0 -29. 9 overweight 30. 0 -34. 9 obesity I 35. 0 -39. 9 obesity II >40 obesity III Waist Circumference: Men > 40 in, Women > 35 in Disease risk relative to normal weight and waist circumference High Ogden CL, Carroll MD, Flegal KM. JAMA. 2014 Jul; 312(2); 189 -90. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity Obes Res. 1998; 6(suppl 2). Very High Extremely High
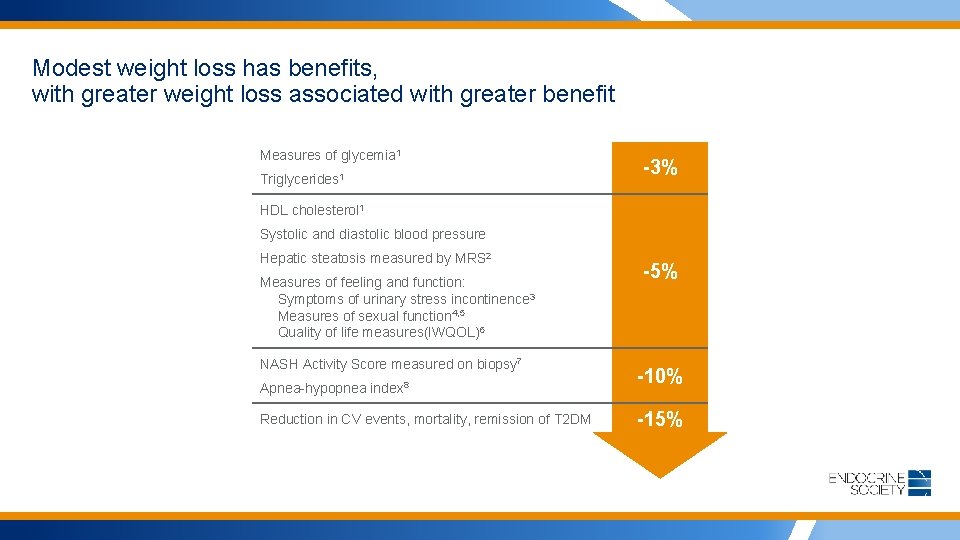
Modest weight loss has benefits, with greater weight loss associated with greater benefit Measures of glycemia 1 Triglycerides 1 -3% HDL cholesterol 1 Systolic and diastolic blood pressure Hepatic steatosis measured by MRS 2 Measures of feeling and function: Symptoms of urinary stress incontinence 3 Measures of sexual function 4, 5 Quality of life measures(IWQOL)6 NASH Activity Score measured on biopsy 7 Apnea-hypopnea index 8 Reduction in CV events, mortality, remission of T 2 DM -5% -10% -15%
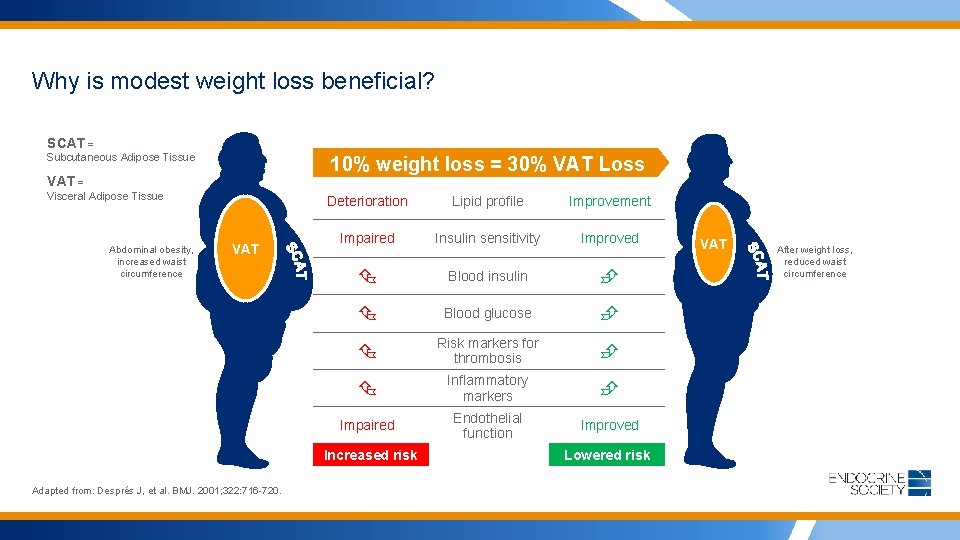
Why is modest weight loss beneficial? SCAT = Subcutaneous Adipose Tissue 10% weight loss = 30% VAT Loss VAT = Visceral Adipose Tissue Abdominal obesity, increased waist circumference VAT Deterioration Lipid profile Improvement Impaired Insulin sensitivity Improved Blood insulin Blood glucose Risk markers for thrombosis Inflammatory markers Impaired Endothelial function Improved Increased risk Adapted from: Després J, et al. BMJ. 2001; 322: 716 -720. Lowered risk VAT After weight loss, reduced waist circumference
Summary (Risks of overweight & obesity, Benefits of weight modest weight loss) • Obesity is associated with an increased risk for coronary heart disease, type 2 diabetes, various types of cancer, gallstones, and disability. • Obesity is associated with an increased risk for death, particularly in adults younger than 65 years. • The risk of disease increases with BMI and waist circumference. • Weight loss as little as 3% - 5% in obese individuals is associated with a lower incidence of health problems and death.
Obesity is a disease, but are we talking about it? USPSTF recommends screening all adults for obesity yet: • A third of patients with a BMI ≥ 30 were never told by their doctors that they have obesity • Rates of physician counseling appear to be decreasing, by as much as 25 percent. Those rates are worse for patients with obesity co-morbidities • Health care provider – patient conversations about nutrition last an average of 55 seconds • Intensive behavioral counseling can induce clinically meaningful weight loss, but there is little research on primary care practitioners providing such care Post RE et al. Arch Intern Med. 2011; 171(4): 316 -321 Kraschnewski JL et al. Med Care. 2013; 51: 186– 92. Eaton CB, Am J Prev Med. 2002 Oct; 23(3): 174 -9. Wadden TA et al. JAMA. 2014 Nov 5; 312(17): 1779 -91
STEP 1: Talk to patients about obesity Motivational interviewing and shared decision-making with patients
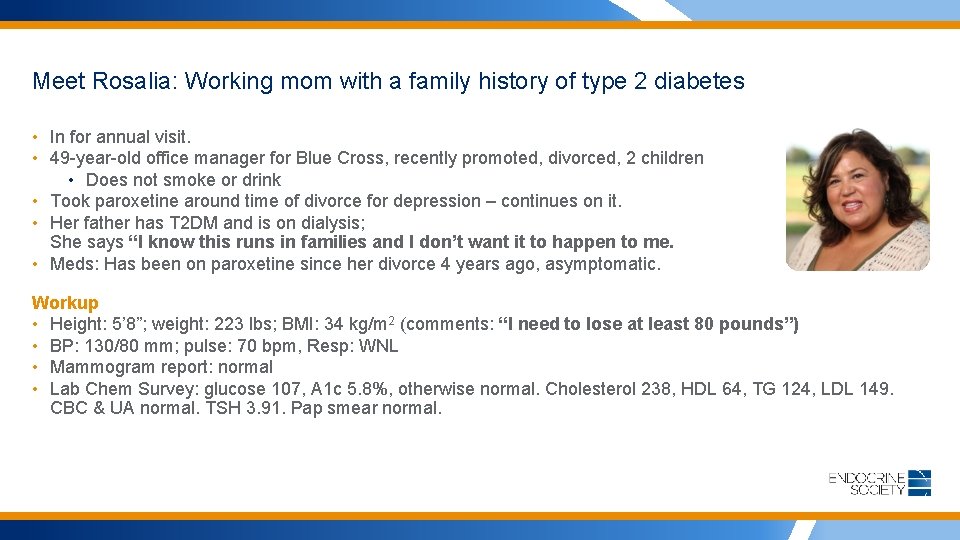
Meet Rosalia: Working mom with a family history of type 2 diabetes • In for annual visit. • 49 -year-old office manager for Blue Cross, recently promoted, divorced, 2 children • Does not smoke or drink • Took paroxetine around time of divorce for depression – continues on it. • Her father has T 2 DM and is on dialysis; She says “I know this runs in families and I don’t want it to happen to me. • Meds: Has been on paroxetine since her divorce 4 years ago, asymptomatic. Workup • Height: 5’ 8”; weight: 223 lbs; BMI: 34 kg/m 2 (comments: “I need to lose at least 80 pounds”) • BP: 130/80 mm; pulse: 70 bpm, Resp: WNL • Mammogram report: normal • Lab Chem Survey: glucose 107, A 1 c 5. 8%, otherwise normal. Cholesterol 238, HDL 64, TG 124, LDL 149. CBC & UA normal. TSH 3. 91. Pap smear normal.
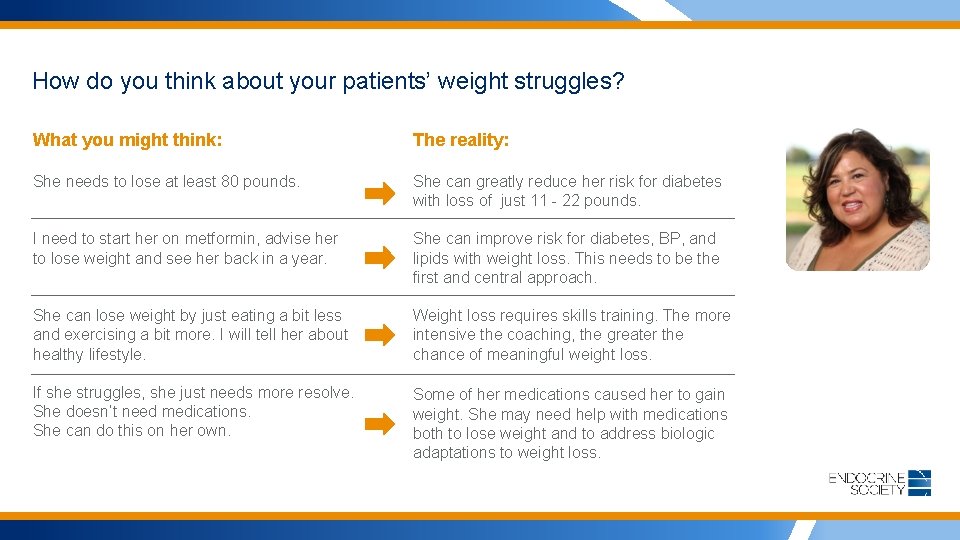
How do you think about your patients’ weight struggles? What you might think: The reality: She needs to lose at least 80 pounds. She can greatly reduce her risk for diabetes with loss of just 11 - 22 pounds. I need to start her on metformin, advise her to lose weight and see her back in a year. She can improve risk for diabetes, BP, and lipids with weight loss. This needs to be the first and central approach. She can lose weight by just eating a bit less and exercising a bit more. I will tell her about healthy lifestyle. Weight loss requires skills training. The more intensive the coaching, the greater the chance of meaningful weight loss. If she struggles, she just needs more resolve. She doesn’t need medications. She can do this on her own. Some of her medications caused her to gain weight. She may need help with medications both to lose weight and to address biologic adaptations to weight loss.
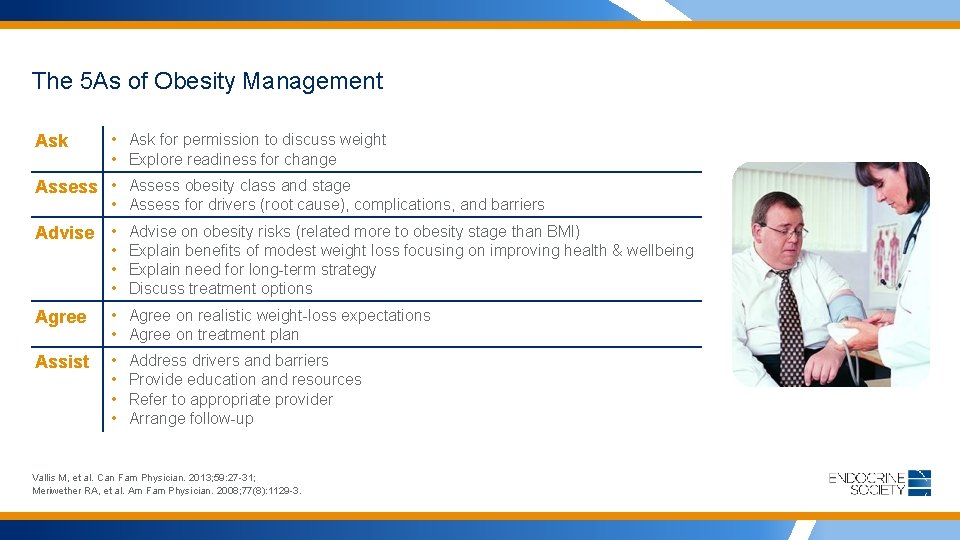
The 5 As of Obesity Management Ask • Ask for permission to discuss weight • Explore readiness for change Assess • Assess obesity class and stage • Assess for drivers (root cause), complications, and barriers Advise • Advise on obesity risks (related more to obesity stage than BMI) • Explain benefits of modest weight loss focusing on improving health & wellbeing • Explain need for long-term strategy • Discuss treatment options Agree • Agree on realistic weight-loss expectations • Agree on treatment plan Assist • • Address drivers and barriers Provide education and resources Refer to appropriate provider Arrange follow-up Vallis M, et al. Can Fam Physician. 2013; 59: 27 -31; Meriwether RA, et al. Am Fam Physician. 2008; 77(8): 1129 -3.

Talk to Rosalia using the 5 As of obesity management Ask: “Let’s talk about your exam. Your mammogram is normal and your exam and most of your tests are fine. But your blood sugar and A 1 c are higher than we like to see. This is prediabetes. The single best thing you could do for your health would be to make some lifestyle changes that produce some weight loss. Is today a good time to talk about your weight? ” Rosalia: “Yes, we can talk about it. I know I need to lose weight – at least 80 pounds. I don’t want to end up like my father. ” You: I’m glad to hear you are taking this seriously. We can talk about a goal later, but the good news is that you can improve your diabetes risk with 11 -22 pounds loss. Let me ask you a few questions to get started. ” What if she says, “No”? Assess: • Comorbidities (sleep apnea symptoms, depression symptoms) • Drivers of weight gain (medications including OTC; sleep deprivation, stress) • Complications and Barriers to weight loss success. • Current lifestyle. • What has worked in the past. • What hasn’t worked in the past.
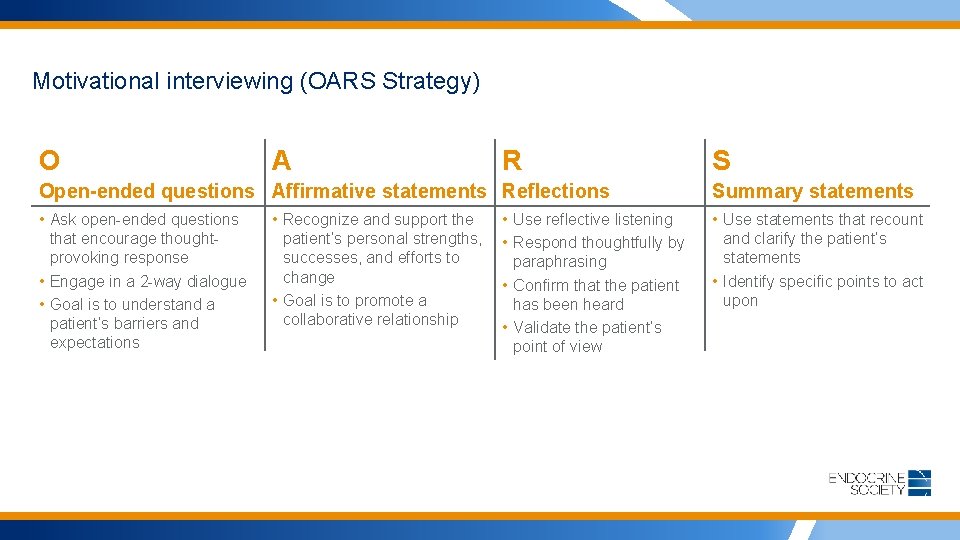
Motivational interviewing (OARS Strategy) O A R S Open-ended questions Affirmative statements Reflections Summary statements • Ask open-ended questions that encourage thoughtprovoking response • Engage in a 2 -way dialogue • Goal is to understand a patient’s barriers and expectations • Use statements that recount and clarify the patient’s statements • Identify specific points to act upon • Recognize and support the patient’s personal strengths, successes, and efforts to change • Goal is to promote a collaborative relationship • Use reflective listening • Respond thoughtfully by paraphrasing • Confirm that the patient has been heard • Validate the patient’s point of view
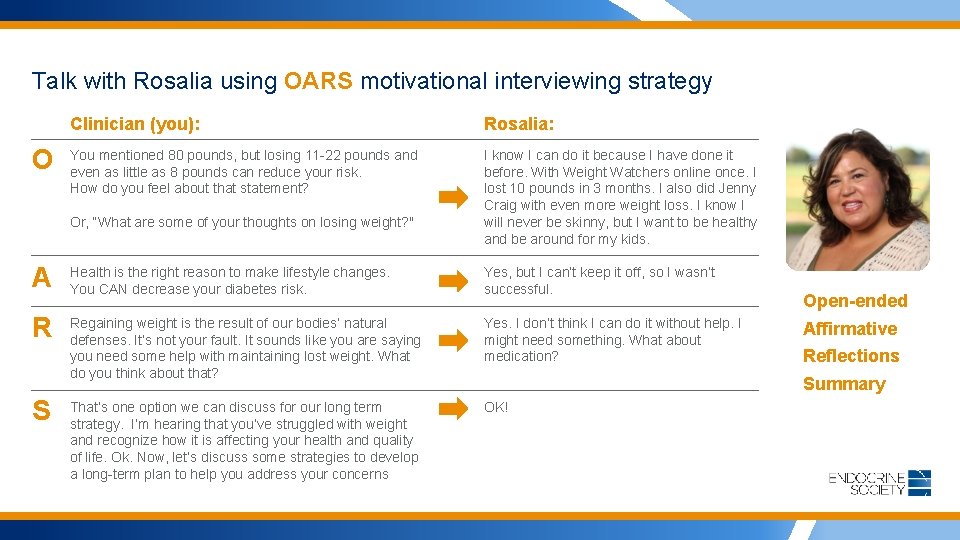
Talk with Rosalia using OARS motivational interviewing strategy O Clinician (you): Rosalia: You mentioned 80 pounds, but losing 11 -22 pounds and even as little as 8 pounds can reduce your risk. How do you feel about that statement? I know I can do it because I have done it before. With Weight Watchers online once. I lost 10 pounds in 3 months. I also did Jenny Craig with even more weight loss. I know I will never be skinny, but I want to be healthy and be around for my kids. Or, “What are some of your thoughts on losing weight? " A Health is the right reason to make lifestyle changes. You CAN decrease your diabetes risk. Yes, but I can’t keep it off, so I wasn’t successful. R Regaining weight is the result of our bodies’ natural defenses. It’s not your fault. It sounds like you are saying you need some help with maintaining lost weight. What do you think about that? Yes. I don’t think I can do it without help. I might need something. What about medication? That’s one option we can discuss for our long term strategy. I’m hearing that you’ve struggled with weight and recognize how it is affecting your health and quality of life. Ok. Now, let’s discuss some strategies to develop a long-term plan to help you address your concerns OK! S Open-ended Affirmative Reflections Summary
Talking to patients about weight: Patient-centered communication Keys to Successful Conversations • Choose words carefully: • “Healthy eating habits” not “diet” • “Physical activity routine” not “exercise” • “Weight” or “healthy weight” not “fat” or “fatness” • Other terms to avoid: “excess fat, ” “heaviness, ” “large size, ” “weight problem” • Listen actively, with empathy and encouragement • Be non-judgmental Preventing Weight Bias. Module 2: Helping Without Harming in Clinical Practice. The Rudd Center for Food Policy and Obesity. Yale University.
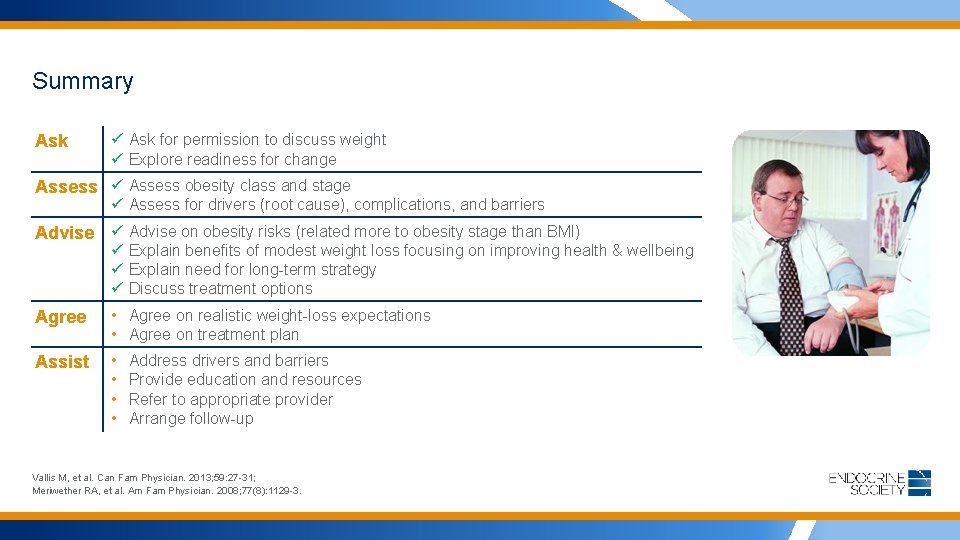
Summary Ask ü Ask for permission to discuss weight ü Explore readiness for change Assess ü Assess obesity class and stage ü Assess for drivers (root cause), complications, and barriers Advise ü Advise on obesity risks (related more to obesity stage than BMI) ü Explain benefits of modest weight loss focusing on improving health & wellbeing ü Explain need for long-term strategy ü Discuss treatment options Agree • Agree on realistic weight-loss expectations • Agree on treatment plan Assist • • Address drivers and barriers Provide education and resources Refer to appropriate provider Arrange follow-up Vallis M, et al. Can Fam Physician. 2013; 59: 27 -31; Meriwether RA, et al. Am Fam Physician. 2008; 77(8): 1129 -3.
STEP 2: Manage obesity with a toolbox of options Guidelines on Pharmacologic Management of Obesity
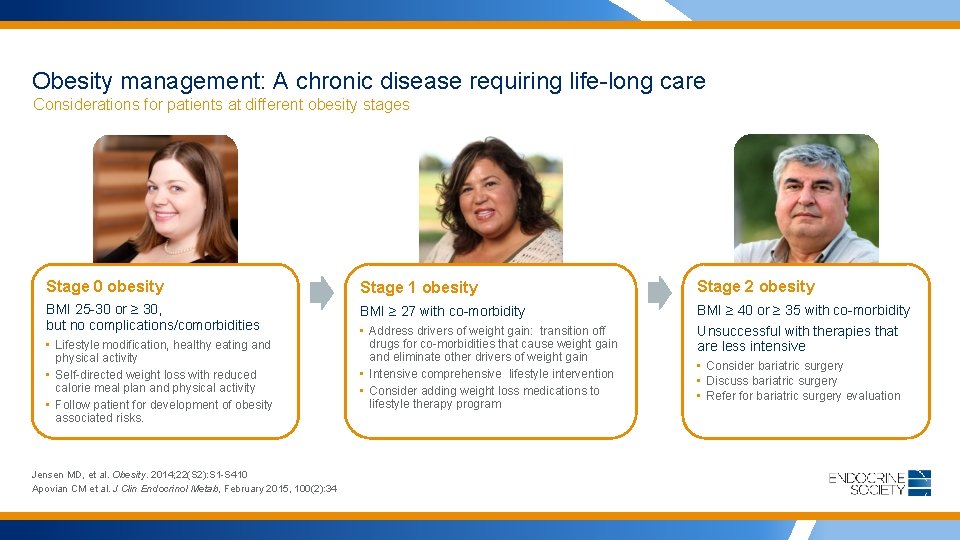
Obesity management: A chronic disease requiring life-long care Considerations for patients at different obesity stages Stage 0 obesity Stage 1 obesity Stage 2 obesity BMI 25 -30 or ≥ 30, but no complications/comorbidities BMI ≥ 27 with co-morbidity BMI ≥ 40 or ≥ 35 with co-morbidity • Address drivers of weight gain: transition off drugs for co-morbidities that cause weight gain and eliminate other drivers of weight gain • Intensive comprehensive lifestyle intervention • Consider adding weight loss medications to lifestyle therapy program Unsuccessful with therapies that are less intensive • Lifestyle modification, healthy eating and physical activity • Self-directed weight loss with reduced calorie meal plan and physical activity • Follow patient for development of obesity associated risks. Jensen MD, et al. Obesity. 2014; 22(S 2): S 1 -S 410 Apovian CM et al. J Clin Endocrinol Metab, February 2015, 100(2): 34 • Consider bariatric surgery • Discuss bariatric surgery • Refer for bariatric surgery evaluation

Weight management intensification options Patients with low risk should have lower intensity, less risk approaches. Higher risk approaches are justified when patients have more complicated obesity. Mean Weight Loss 0% 3% 8% Diet and Lifestyle 1 12% Lifestyle plus Obesity Medications 16% Gastric Band 2 32% Gastric Bypass or Sleeve 2 From LABS 3: Perioperative DVT, thromboembolism or death 1% for gastric band 5% for bypass 1. Jensen et al. Circulation 2014; 129(25 Suppl 2): S 102 -38; 2. Courcoulas et al. JAMA 2013; 310: 2416 -2425; 3. LABS consortium. N Engl J Med 2009; 361: 445 -54.
Best Diets to Support Weight Loss • Comparison of Weight Loss Among Named Diet Programs in Overweight and Obese Adults: A Meta-analysis • Over a 12 month period, low-Carbohydrate and low-fat diets were associated with more weight loss than no dietary intervention • Behavioral support and exercise enhanced weight loss • Weight loss differences between individual diets were small, and likely not significant to those seeking weight loss • Conclusion: The best diet is the one the patient will adhere to in order to lose weight Johnston, B, Kanters, S, Bandayrel, K, Wu, P, Naji, F, Siemieniuk, R, Ball, G, Busse, J, Thorlund, K, Guyatt, G, Jansen, J, Mills, E. (2014). Comparison of weight loss among named diet programs in overweight and obese adults: A meta-analysis. JAMA, 312(9): 923 -933. doi: 10. 1001/jama. 2014. 10397.
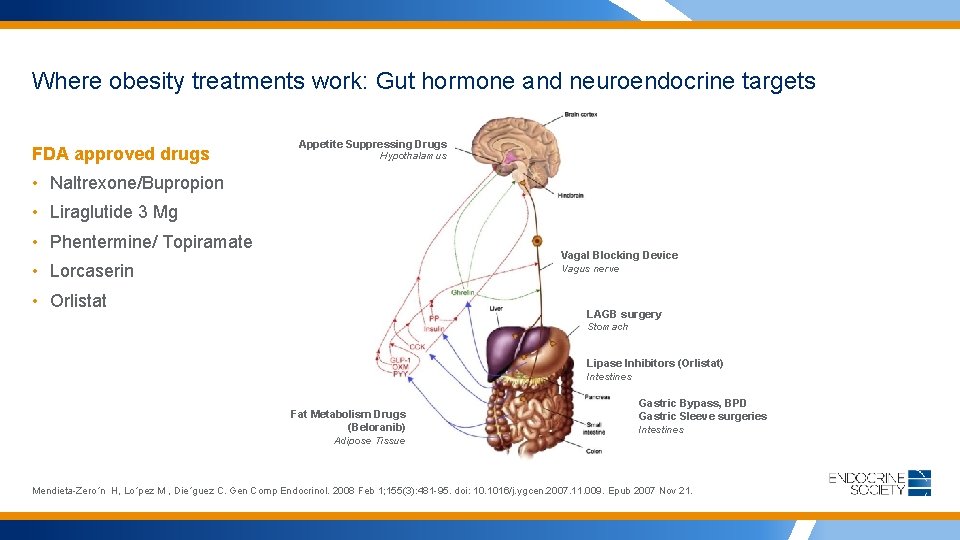
Where obesity treatments work: Gut hormone and neuroendocrine targets FDA approved drugs Appetite Suppressing Drugs Hypothalamus • Naltrexone/Bupropion • Liraglutide 3 Mg • Phentermine/ Topiramate Vagal Blocking Device Vagus nerve • Lorcaserin • Orlistat LAGB surgery Stomach Lipase Inhibitors (Orlistat) Intestines Fat Metabolism Drugs (Beloranib) Adipose Tissue Gastric Bypass, BPD Gastric Sleeve surgeries Intestines Mendieta-Zero´n H, Lo´pez M , Die´guez C. Gen Comp Endocrinol. 2008 Feb 1; 155(3): 481 -95. doi: 10. 1016/j. ygcen. 2007. 11. 009. Epub 2007 Nov 21.
Pharmacological Management Of Obesity: An Endocrine Society Clinical Practice Guideline January 15, 2015 Apovian C, Aronne LJ, et al. J Clin Endocrinol Metab. 2015 Feb; 100(2): 342 -62.
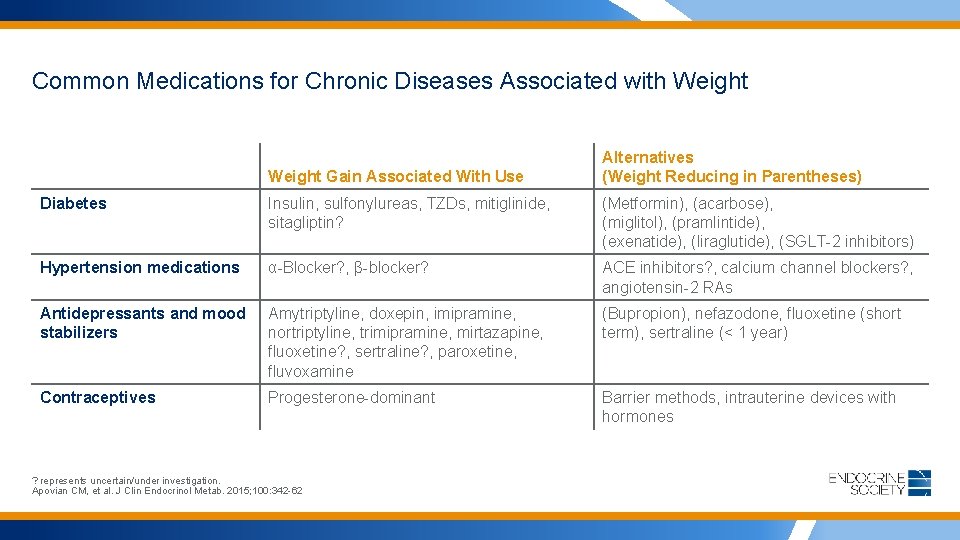
Common Medications for Chronic Diseases Associated with Weight Gain Associated With Use Alternatives (Weight Reducing in Parentheses) Diabetes Insulin, sulfonylureas, TZDs, mitiglinide, sitagliptin? (Metformin), (acarbose), (miglitol), (pramlintide), (exenatide), (liraglutide), (SGLT-2 inhibitors) Hypertension medications α-Blocker? , β-blocker? ACE inhibitors? , calcium channel blockers? , angiotensin-2 RAs Antidepressants and mood stabilizers Amytriptyline, doxepin, imipramine, nortriptyline, trimipramine, mirtazapine, fluoxetine? , sertraline? , paroxetine, fluvoxamine (Bupropion), nefazodone, fluoxetine (short term), sertraline (< 1 year) Contraceptives Progesterone-dominant Barrier methods, intrauterine devices with hormones ? represents uncertain/under investigation. Apovian CM, et al. J Clin Endocrinol Metab. 2015; 100: 342 -62

Who Qualifies for Obesity Medications? We need obesity medications to: • help patients better adhere to their dietary plan • help more patients achieve meaningful weight loss • produce more weight loss so that health benefits will be greater • help patients sustain lost weight Recommendation: Prescribe as an adjunct to diet, exercise and behavior modification for individuals: • with BMI 30+; or 27+ with comorbidity; • who are unable to lose and successfully maintain weight; and • who meet label indications. • 1 * • Strong recommendation based on High quality evidence Apovian CM et al. J Clin Endocrinol Metab, February 2015, 100(2): 34
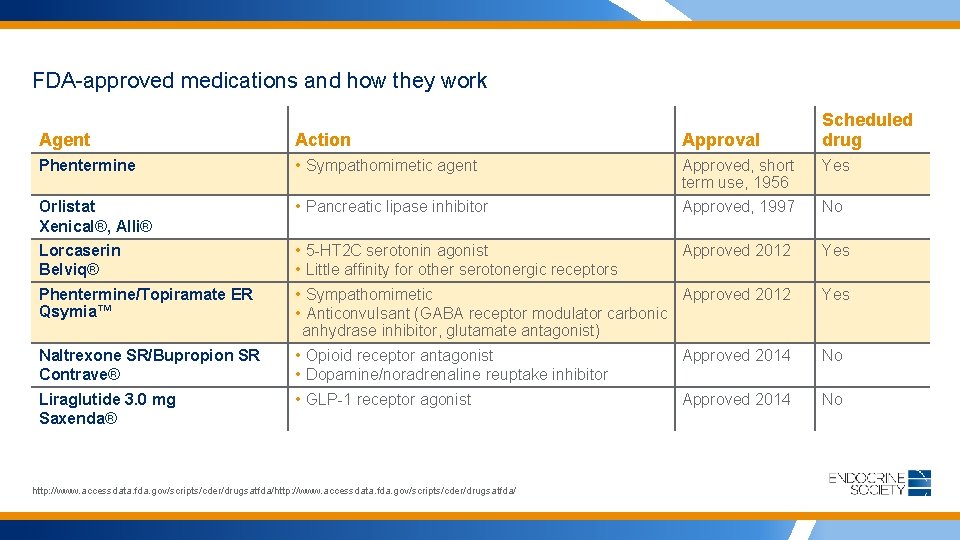
FDA-approved medications and how they work Scheduled drug Agent Action Approval Phentermine • Sympathomimetic agent Approved, short term use, 1956 Yes Orlistat Xenical®, Alli® • Pancreatic lipase inhibitor Approved, 1997 No Lorcaserin Belviq® • • Approved 2012 Yes Sympathomimetic Approved 2012 Anticonvulsant (GABA receptor modulator carbonic anhydrase inhibitor, glutamate antagonist) Yes Phentermine/Topiramate ER Qsymia™ Naltrexone SR/Bupropion SR Contrave® Liraglutide 3. 0 mg Saxenda® 5 -HT 2 C serotonin agonist Little affinity for other serotonergic receptors • Opioid receptor antagonist • Dopamine/noradrenaline reuptake inhibitor • GLP-1 receptor agonist http: //www. accessdata. fda. gov/scripts/cder/drugsatfda/ Approved 2014 No
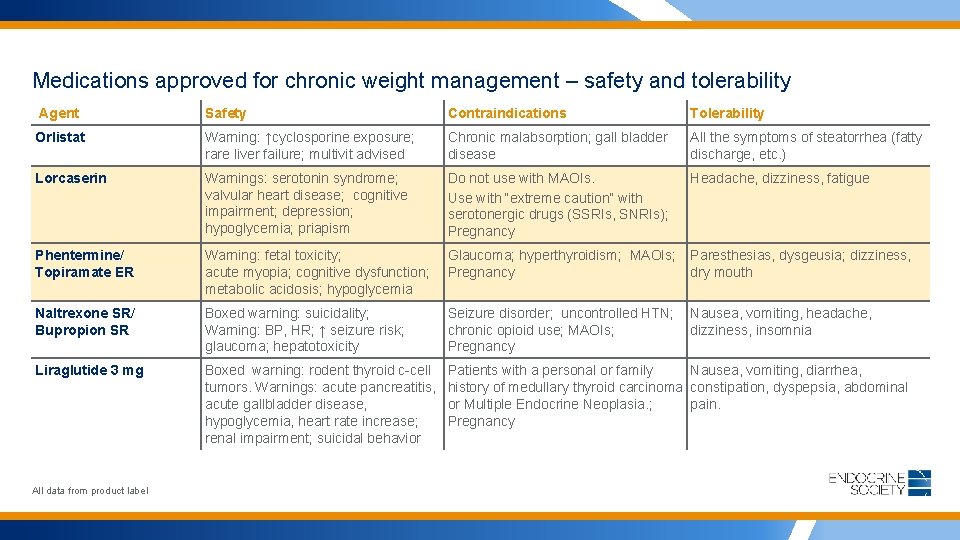
Medications approved for chronic weight management – safety and tolerability Agent Safety Contraindications Tolerability Orlistat Warning: ↑cyclosporine exposure; rare liver failure; multivit advised Chronic malabsorption; gall bladder disease All the symptoms of steatorrhea (fatty discharge, etc. ) Lorcaserin Warnings: serotonin syndrome; valvular heart disease; cognitive impairment; depression; hypoglycemia; priapism Do not use with MAOIs. Use with “extreme caution” with serotonergic drugs (SSRIs, SNRIs); Pregnancy Headache, dizziness, fatigue Phentermine/ Topiramate ER Warning: fetal toxicity; acute myopia; cognitive dysfunction; metabolic acidosis; hypoglycemia Glaucoma; hyperthyroidism; MAOIs; Pregnancy Paresthesias, dysgeusia; dizziness, dry mouth Naltrexone SR/ Bupropion SR Boxed warning: suicidality; Warning: BP, HR; ↑ seizure risk; glaucoma; hepatotoxicity Seizure disorder; uncontrolled HTN; chronic opioid use; MAOIs; Pregnancy Nausea, vomiting, headache, dizziness, insomnia Liraglutide 3 mg Boxed warning: rodent thyroid c-cell tumors. Warnings: acute pancreatitis, acute gallbladder disease, hypoglycemia, heart rate increase; renal impairment; suicidal behavior Patients with a personal or family Nausea, vomiting, diarrhea, history of medullary thyroid carcinoma constipation, dyspepsia, abdominal or Multiple Endocrine Neoplasia. ; pain. Pregnancy All data from product label
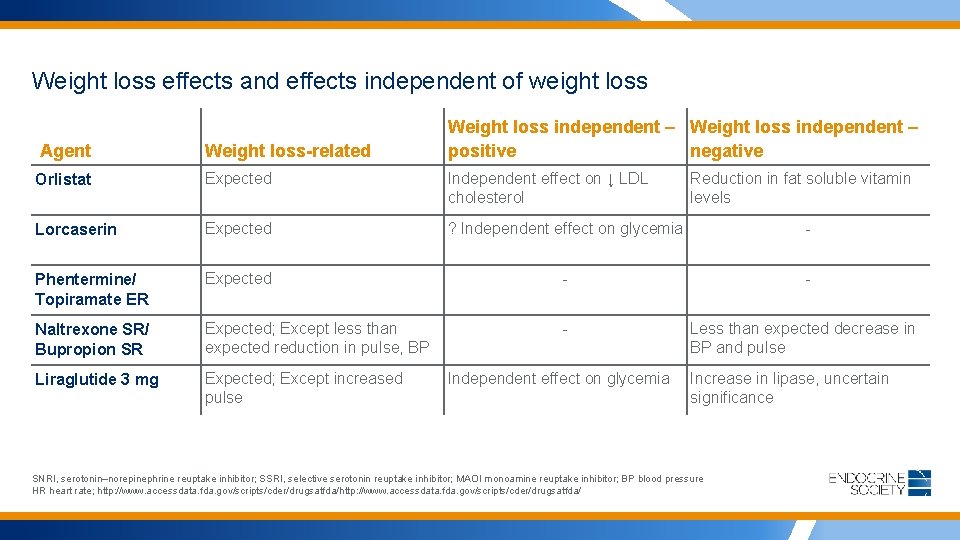
Weight loss effects and effects independent of weight loss Agent Weight loss-related Weight loss independent – positive negative Orlistat Expected Independent effect on ↓ LDL cholesterol Lorcaserin Expected ? Independent effect on glycemia - Phentermine/ Topiramate ER Expected - - Naltrexone SR/ Bupropion SR Expected; Except less than expected reduction in pulse, BP - Liraglutide 3 mg Expected; Except increased pulse Independent effect on glycemia Reduction in fat soluble vitamin levels Less than expected decrease in BP and pulse Increase in lipase, uncertain significance SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; MAOI monoamine reuptake inhibitor; BP blood pressure HR heart rate; http: //www. accessdata. fda. gov/scripts/cder/drugsatfda/
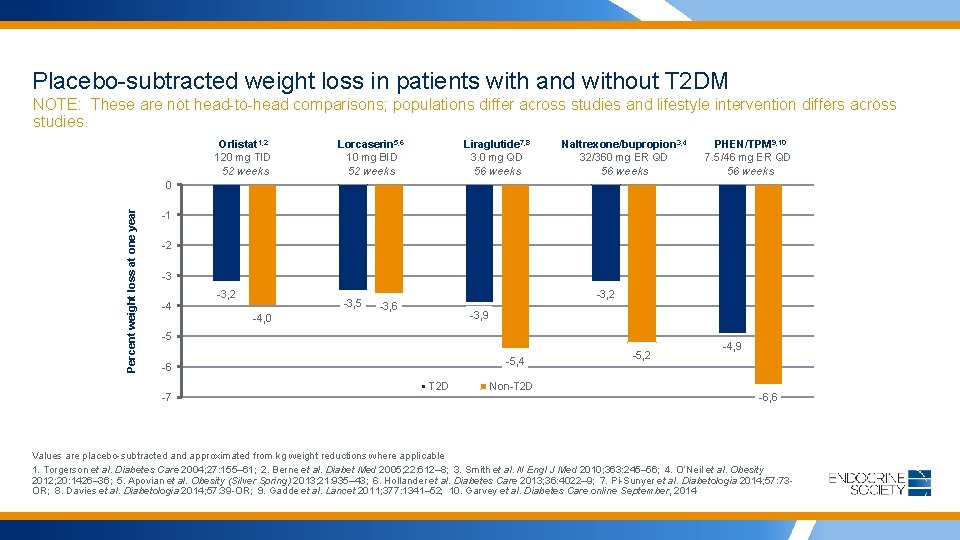
Placebo-subtracted weight loss in patients with and without T 2 DM NOTE: These are not head-to-head comparisons; populations differ across studies and lifestyle intervention differs across studies. Orlistat 1, 2 120 mg TID 52 weeks Lorcaserin 5, 6 10 mg BID 52 weeks Liraglutide 7, 8 3. 0 mg QD 56 weeks Naltrexone/bupropion 3, 4 32/360 mg ER QD 56 weeks PHEN/TPM 9, 10 7. 5/46 mg ER QD 56 weeks Percent weight loss at one year 0 -1 -2 -3 -4 -3, 2 -3, 5 -4, 0 -3, 2 -3, 6 -3, 9 -5 -5, 4 -6 -7 T 2 D Non-T 2 D -5, 2 -4, 9 -6, 6 Values are placebo-subtracted and approximated from kg weight reductions where applicable 1. Torgerson et al. Diabetes Care 2004; 27: 155– 61; 2. Berne et al. Diabet Med 2005; 22: 612– 8; 3. Smith et al. N Engl J Med 2010; 363: 245– 56; 4. O’Neil et al. Obesity 2012; 20: 1426– 36; 5. Apovian et al. Obesity (Silver Spring) 2013; 21: 935– 43; 6. Hollander et al. Diabetes Care 2013; 36: 4022– 9; 7. Pi-Sunyer et al. Diabetologia 2014; 57: 73 OR; 8. Davies et al. Diabetologia 2014; 57: 39 -OR; 9. Gadde et al. Lancet 2011; 377: 1341– 52; 10. Garvey et al. Diabetes Care online September, 2014
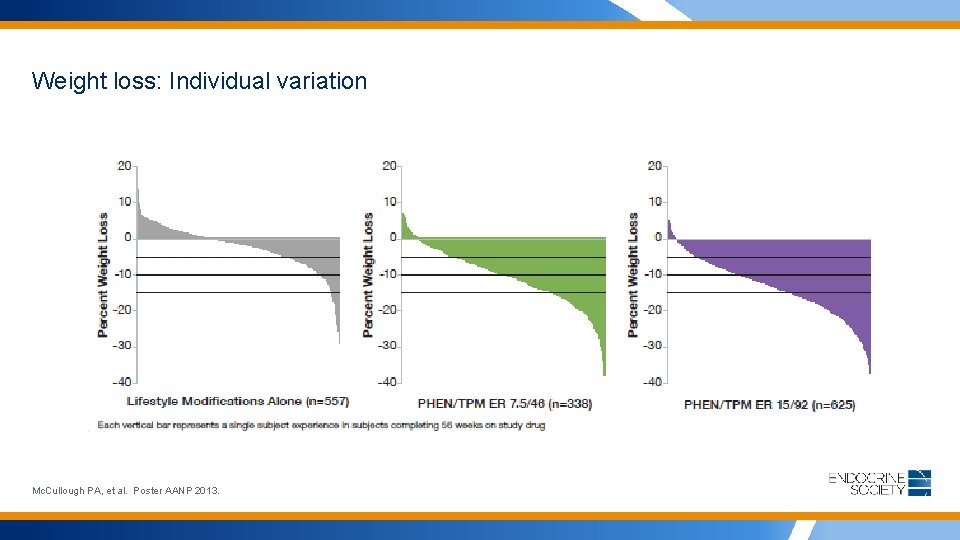
Weight loss: Individual variation Mc. Cullough PA, et al. Poster AANP 2013.
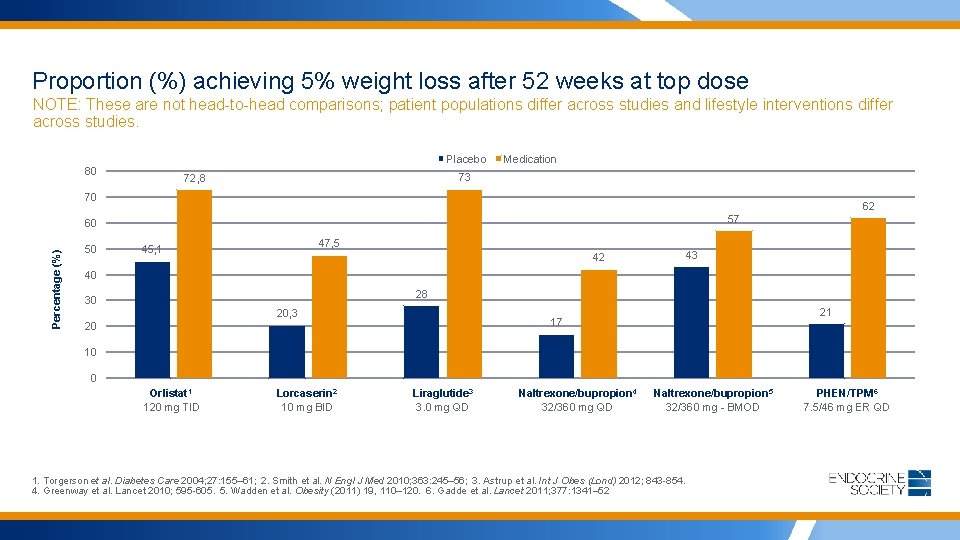
Proportion (%) achieving 5% weight loss after 52 weeks at top dose NOTE: These are not head-to-head comparisons; patient populations differ across studies and lifestyle interventions differ across studies. Placebo 80 Medication 73 72, 8 70 62 57 Percentage (%) 60 50 47, 5 45, 1 42 43 40 28 30 20, 3 21 17 20 10 0 Orlistat 1 120 mg TID Lorcaserin 2 10 mg BID Liraglutide 3 3. 0 mg QD Naltrexone/bupropion 4 32/360 mg QD Naltrexone/bupropion 5 32/360 mg - BMOD 1. Torgerson et al. Diabetes Care 2004; 27: 155– 61; 2. Smith et al. N Engl J Med 2010; 363: 245– 56; 3. Astrup et al. Int J Obes (Lond) 2012; 843 -854. 4. Greenway et al. Lancet 2010; 595 -605. 5. Wadden et al. Obesity (2011) 19, 110– 120. 6. Gadde et al. Lancet 2011; 377: 1341– 52 PHEN/TPM 6 7. 5/46 mg ER QD
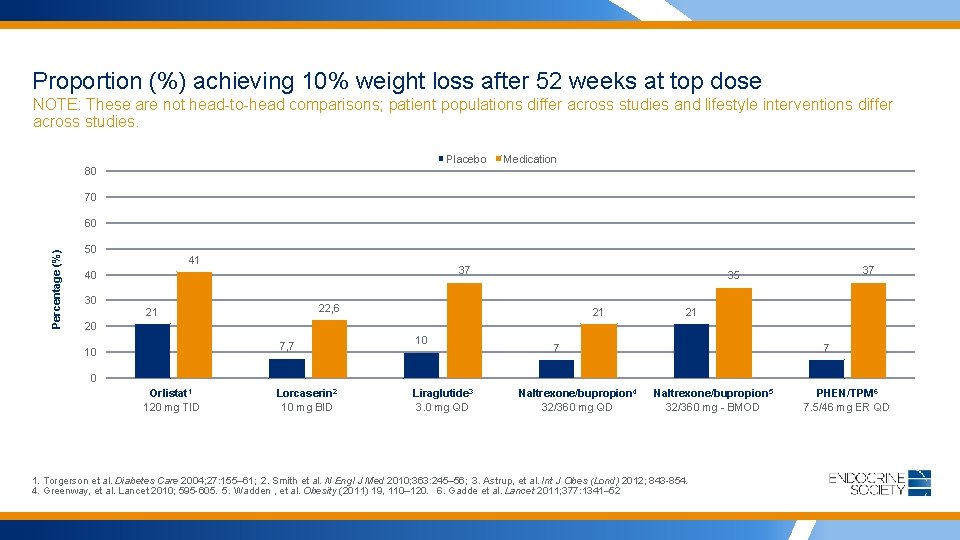
Proportion (%) achieving 10% weight loss after 52 weeks at top dose NOTE: These are not head-to-head comparisons; patient populations differ across studies and lifestyle interventions differ across studies. Placebo Medication 80 70 Percentage (%) 60 50 41 37 40 30 22, 6 21 37 35 21 21 20 7, 7 10 10 7 7 0 Orlistat 1 120 mg TID Lorcaserin 2 10 mg BID Liraglutide 3 3. 0 mg QD Naltrexone/bupropion 4 32/360 mg QD Naltrexone/bupropion 5 32/360 mg - BMOD 1. Torgerson et al. Diabetes Care 2004; 27: 155– 61; 2. Smith et al. N Engl J Med 2010; 363: 245– 56; 3. Astrup, et al. Int J Obes (Lond) 2012; 843 -854. 4. Greenway, et al. Lancet 2010; 595 -605. 5. Wadden , et al. Obesity (2011) 19, 110– 120. 6. Gadde et al. Lancet 2011; 377: 1341– 52 PHEN/TPM 6 7. 5/46 mg ER QD
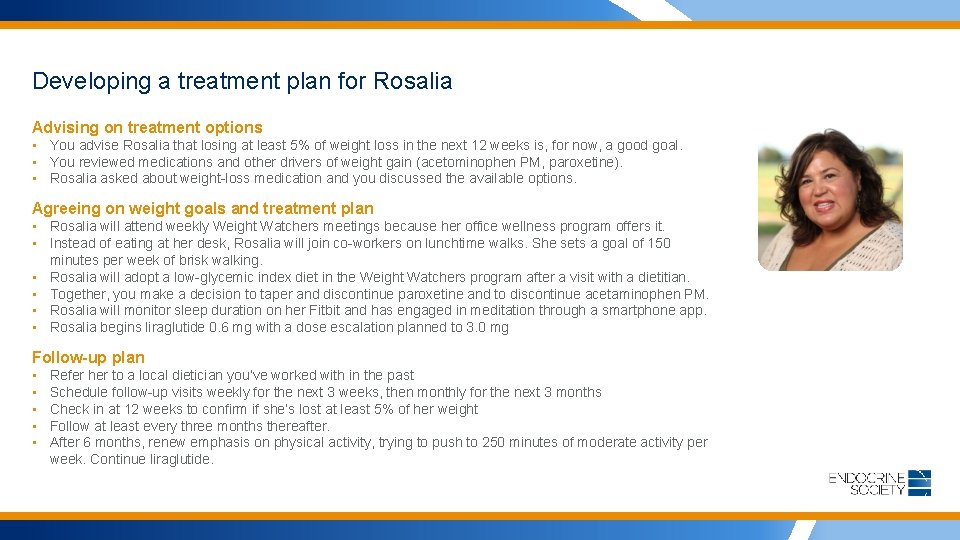
Developing a treatment plan for Rosalia Advising on treatment options • You advise Rosalia that losing at least 5% of weight loss in the next 12 weeks is, for now, a good goal. • You reviewed medications and other drivers of weight gain (acetominophen PM, paroxetine). • Rosalia asked about weight-loss medication and you discussed the available options. Agreeing on weight goals and treatment plan • Rosalia will attend weekly Weight Watchers meetings because her office wellness program offers it. • Instead of eating at her desk, Rosalia will join co-workers on lunchtime walks. She sets a goal of 150 minutes per week of brisk walking. • Rosalia will adopt a low-glycemic index diet in the Weight Watchers program after a visit with a dietitian. • Together, you make a decision to taper and discontinue paroxetine and to discontinue acetaminophen PM. • Rosalia will monitor sleep duration on her Fitbit and has engaged in meditation through a smartphone app. • Rosalia begins liraglutide 0. 6 mg with a dose escalation planned to 3. 0 mg Follow-up plan • • • Refer her to a local dietician you’ve worked with in the past Schedule follow-up visits weekly for the next 3 weeks, then monthly for the next 3 months Check in at 12 weeks to confirm if she’s lost at least 5% of her weight Follow at least every three months thereafter. After 6 months, renew emphasis on physical activity, trying to push to 250 minutes of moderate activity per week. Continue liraglutide.

Rosalia’s treatment strategy Ask ü Ask for permission to discuss weight ü Explore readiness for change Assess ü Assess obesity class and stage ü Assess for drivers (root cause), complications, and barriers Advise ü Advise on obesity risks (related more to obesity stage than BMI) ü Explain benefits of modest weight loss focusing on improving health & wellbeing ü Explain need for long-term strategy ü Discuss treatment options Agree ü Agree on realistic weight-loss expectations ü Agree on treatment plan Assist ü ü Address drivers and barriers Provide education and resources Refer to appropriate provider Arrange follow-up Vallis M, et al. Can Fam Physician. 2013; 59: 27 -31; Meriwether RA, et al. Am Fam Physician. 2008; 77(8): 1129 -3.
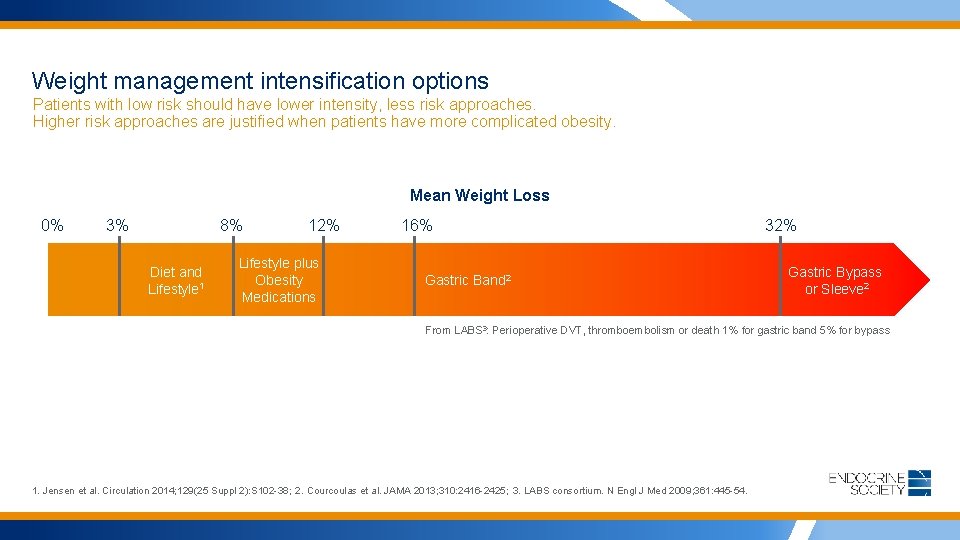
Weight management intensification options Patients with low risk should have lower intensity, less risk approaches. Higher risk approaches are justified when patients have more complicated obesity. Mean Weight Loss 0% 3% 8% Diet and Lifestyle 1 12% Lifestyle plus Obesity Medications 16% Gastric Band 2 32% Gastric Bypass or Sleeve 2 From LABS 3: Perioperative DVT, thromboembolism or death 1% for gastric band 5% for bypass 1. Jensen et al. Circulation 2014; 129(25 Suppl 2): S 102 -38; 2. Courcoulas et al. JAMA 2013; 310: 2416 -2425; 3. LABS consortium. N Engl J Med 2009; 361: 445 -54.
Meet Dennis: A CEO with hypertension, OSA, DM, and a history of depression A candidate for bariatric surgery Annual Physical Exam • 55 -year-old CEO, divorced, 2 grown children • Lives alone, eats out frequently, snacks in evening • Feels tired all the time and no regular physical activity (was “very athletic” in college) • Gained 50 pounds over the last 10 years • Meds: • Sulfonylurea for DM • propanolol and hydrodiuril for HTN • doxepin for depression • acetominophen PM for sleep • Was prescribed a CPAP machine for his severe OSA but has been non-compliant • Drinks socially; denies tobacco use • Lost and regained ~20 lbs on Atkins a few times over the last 10 years Workup • Height: 5’ 9”; Hg (treated); weight: 273 lbs; BMI: 40. 1 kg/m 2 • BP: 132/82 mm; pulse: 64 bpm • Lab findings normal except TGs: 280 mg/d. L; FBS: 142 mg/d. L, AST/ALT 2 x normal, A 1 C: 8%
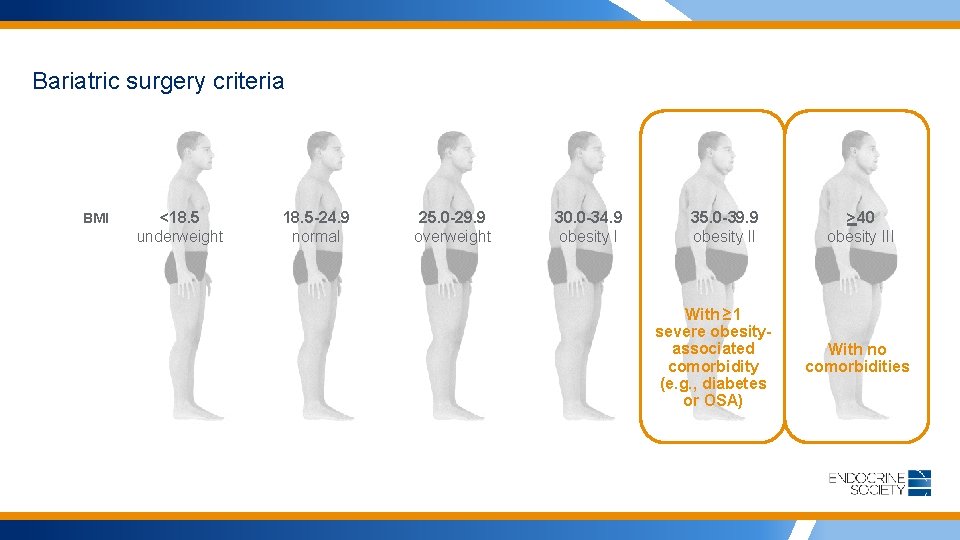
Bariatric surgery criteria BMI <18. 5 underweight 18. 5 -24. 9 normal 25. 0 -29. 9 overweight 30. 0 -34. 9 obesity I 35. 0 -39. 9 obesity II With ≥ 1 severe obesityassociated comorbidity (e. g. , diabetes or OSA) >40 obesity III With no comorbidities

Effectiveness and risks of bariatric surgery and devices: RESULTS An Updated Systematic Review and Meta-analysis, 2003 -2012 Bariatric surgery 1: • Provides substantial and sustained effects on weight loss • Ameliorates obesity-attributable comorbidities in most patients • Risks of complication, reoperation, and death exist Gastric Bypass • More effective weight loss • More complications Adjustable Gastric Banding • Lower mortality • Lower complication rates • Higher reoperation rate • Less weight loss than gastric bypass Re. Shape™ Integrated Dual Balloon System 2 • Two attached balloons placed into stomach through mouth and inflated • 25. 44% EWL and 11. 27% TBWL at 12 months Sleeve Gastrectomy • More effective weight loss than adjustable gastric banding; comparable with gastric bypass ORBERA™ Intragastric Balloon System 3 • Balloon placed into stomach through mouth and filled with saline • 10. 2% WL at 6 months 1 Change S-H, et al. JAMA Surg. 2014; 149(3): 275 -287; 2 ASGE Bariatric Endoscopy Task Force, et al. Gastrointest Endosc. 2015 Sep; 82(3): 425 -38. e 5 3 www. fda. gov/Medical. Devices
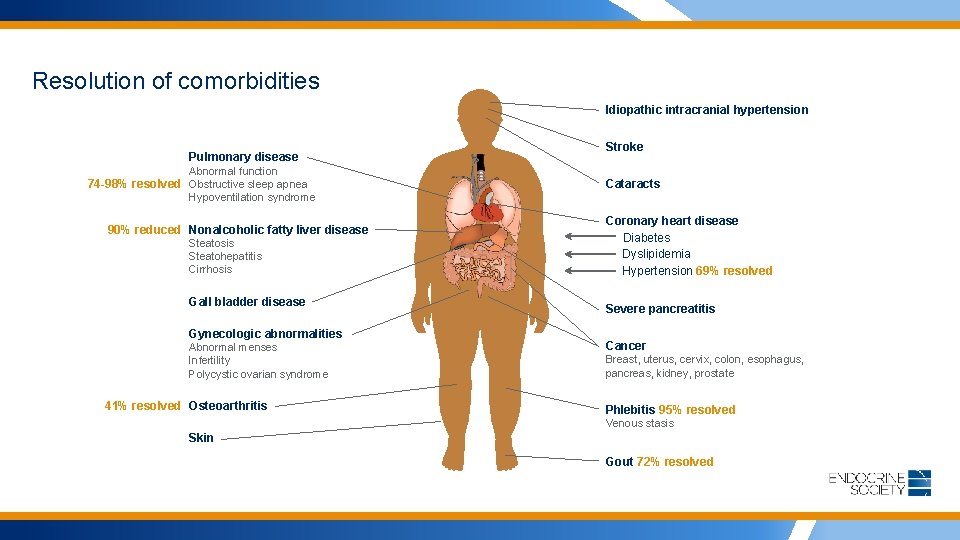
Resolution of comorbidities Idiopathic intracranial hypertension Pulmonary disease Abnormal function 74 -98% resolved Obstructive sleep apnea Hypoventilation syndrome 90% reduced Nonalcoholic fatty liver disease Steatosis Steatohepatitis Cirrhosis Gall bladder disease Gynecologic abnormalities Abnormal menses Infertility Polycystic ovarian syndrome 41% resolved Osteoarthritis Stroke Cataracts Coronary heart disease Diabetes Dyslipidemia Hypertension 69% resolved Severe pancreatitis Cancer Breast, uterus, cervix, colon, esophagus, pancreas, kidney, prostate Phlebitis 95% resolved Venous stasis Skin Gout 72% resolved
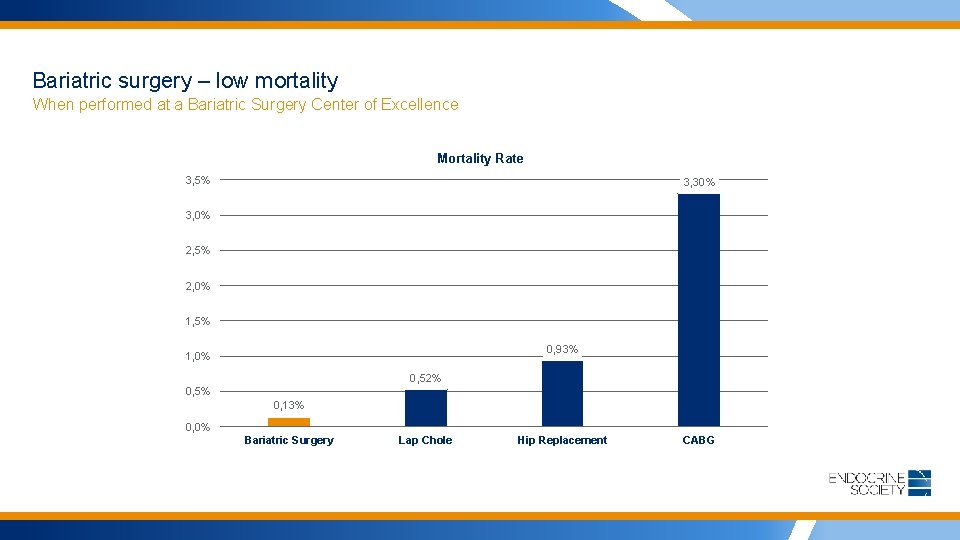
Bariatric surgery – low mortality When performed at a Bariatric Surgery Center of Excellence Mortality Rate 3, 5% 3, 30% 3, 0% 2, 5% 2, 0% 1, 5% 0, 93% 1, 0% 0, 52% 0, 5% 0, 13% 0, 0% Bariatric Surgery Lap Chole Hip Replacement CABG
Putting it all together: • Obesity is a complex, chronic disease • Risk for obesity is driven by environmental and biologic factors in genetically susceptible individuals • Moderate weight loss can improve health, but response to treatment is highly variable and weight regain is common • When patients struggle, intensification of approach is appropriate • Combinations of approaches (diet, exercise, drugs, devices and surgery) produce more weight loss and health benefit
STEP 3: Get reimbursed Reimbursement for Obesity Management
Reimbursement of IBT for obesity Key Considerations • Obesity is a disease and should be treated like one. • If you can’t treat it like a disease, treat comorbid conditions, billed using E&M codes. • Medicare Part B allows reimbursement for IBT for obesity w/some restrictions for: • screening for obesity in adults using BMI; • dietary (nutritional) assessment; and, • intensive behavioral counseling and therapy to promote sustained weight loss through high-intensity interventions on diet and exercise. • Medicare coinsurance and Part B deductible are waived. • Private insurance coverage of IBT for obesity remains highly variable However, because Medicare policy exerts a major influence on the commercial health care system, which often adopts its reimbursement and coverage policies. Centers for Medicare and Medicaid Services
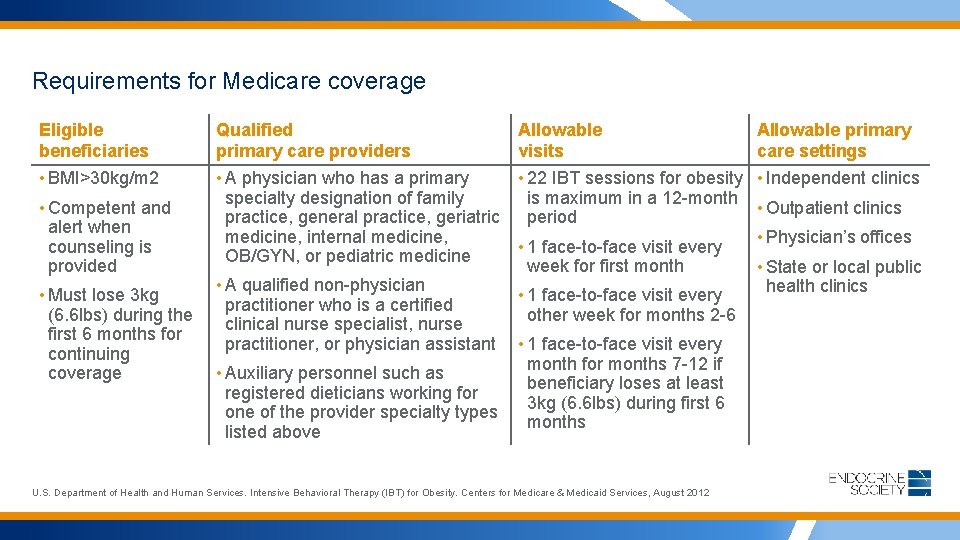
Requirements for Medicare coverage Eligible beneficiaries Qualified primary care providers • BMI>30 kg/m 2 • A physician who has a primary • 22 IBT sessions for obesity specialty designation of family is maximum in a 12 -month practice, general practice, geriatric period medicine, internal medicine, • 1 face-to-face visit every OB/GYN, or pediatric medicine week for first month • A qualified non-physician • 1 face-to-face visit every practitioner who is a certified other week for months 2 -6 clinical nurse specialist, nurse practitioner, or physician assistant • 1 face-to-face visit every month for months 7 -12 if • Auxiliary personnel such as beneficiary loses at least registered dieticians working for 3 kg (6. 6 lbs) during first 6 one of the provider specialty types months listed above • Competent and alert when counseling is provided • Must lose 3 kg (6. 6 lbs) during the first 6 months for continuing coverage Allowable visits U. S. Department of Health and Human Services. Intensive Behavioral Therapy (IBT) for Obesity. Centers for Medicare & Medicaid Services, August 2012 Allowable primary care settings • Independent clinics • Outpatient clinics • Physician’s offices • State or local public health clinics

Documentation for IBT for obesity • Medical records must document all coverage requirements, including the determination of weight loss at the 6 month visit • Must document treatment consistent with the 5 A’s approach • Stand Alone Benefit: The IBT for obesity covered by Medicare is a stand alone billable service separate from the initial preventive physical exam (IPPE) or the Annual Wellness Visit (AMV). • Medicare beneficiaries may obtain IBT for obesity services at any time following Medicare Part B enrollment, including during IPPE or AMV encounter. • Note: Obesity counseling is not separately payable with another visit on the same day with the exception initial physical exams, diabetes self-management and medical nutrition therapy services (code 77 X), and distinct procedural services claims (modifier 59) CMS. MLN Matters MM 7641. 2012.

Billing and coding requirements for IBT • Submitting Professional Claims • Report the appropriate HCPCS code and the corresponding ICD-10 -CM diagnosis code in the X 12 837 -P (Professional) electronic claim format • Include Place of Service (POS) codes to indicate where service was provided • ASCA requires providers to submit claims to Medicare electronically, with limited exceptions • Submitting Institutional Claims • Report the appropriate HCPCS code, revenue code, and the corresponding ICD-10 -CM diagnosis code in the Xl 2 837 -1 (Institutional) electronic • claim format Types of Bill (TOBs) Allowed for Institutional Claims: hospital outpatient, rural health clinic (RHC), federally qualitied health center (FQHC), critical access hospital (CAH) • Coding and Diagnosis Information • Use the Healthcare Common Procedure Coding System (HCPCS code) G 0447 (face-to-face behavioral counseling for obesity) and relevant ICD 10 -DM Diagnosis Code for BMI 30. 0 and over (Z 68. 30 -Z 68. 39, Z 68. 41 -Z 68. 45) • Do not use E 66. 01 or E 66. 09 • No need to add comorbid diagnoses • Use preventative codes 99401 -99404 mandated by ACA for follow-up and management • Covered IBT can be provided “incident to” i. e. , by auxiliary staff member such as NP or PA under direct supervision of physician • Can be an efficient and cost-effective way to provide IBT for obesity in a busy practice setting • Physicians of other specialties may be compensated for IBT if they have multiple credentials and bill under approved taxonomy codes – e. g. , NP or PA Centers for Medicare and Medicaid Services
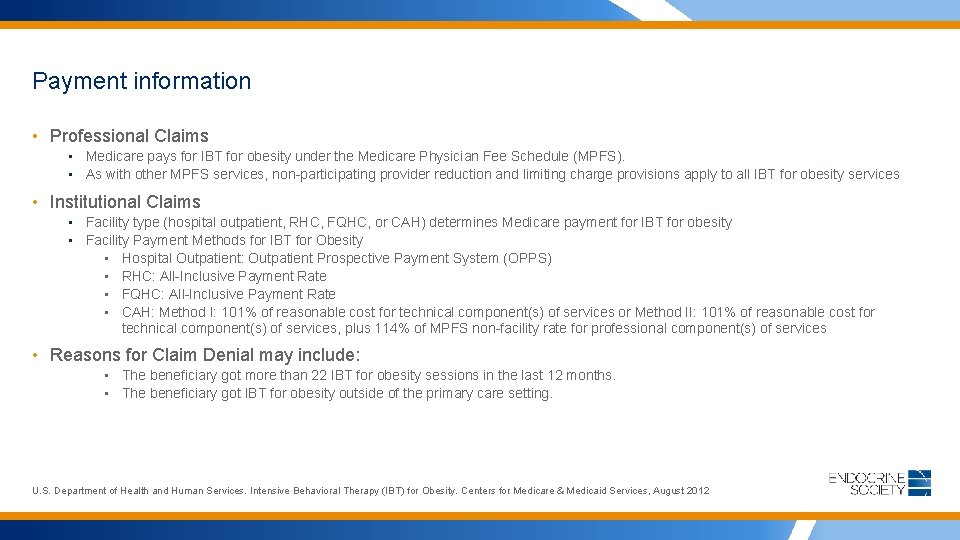
Payment information • Professional Claims • Medicare pays for IBT for obesity under the Medicare Physician Fee Schedule (MPFS). • As with other MPFS services, non-participating provider reduction and limiting charge provisions apply to all IBT for obesity services • Institutional Claims • Facility type (hospital outpatient, RHC, FQHC, or CAH) determines Medicare payment for IBT for obesity • Facility Payment Methods for IBT for Obesity • Hospital Outpatient: Outpatient Prospective Payment System (OPPS) • RHC: All-Inclusive Payment Rate • FQHC: All-Inclusive Payment Rate • CAH: Method I: 101% of reasonable cost for technical component(s) of services or Method II: 101% of reasonable cost for technical component(s) of services, plus 114% of MPFS non-facility rate for professional component(s) of services • Reasons for Claim Denial may include: • The beneficiary got more than 22 IBT for obesity sessions in the last 12 months. • The beneficiary got IBT for obesity outside of the primary care setting. U. S. Department of Health and Human Services. Intensive Behavioral Therapy (IBT) for Obesity. Centers for Medicare & Medicaid Services, August 2012
Summary: Learning Objectives • Review recent findings about the biologic regulation of eating and weight control • Discuss the clinical recommendations and benefits of sustained weight loss in overweight and obese patients • Apply principles of motivational interviewing and shared decision-making to improve the clinical management of obesity and promote behavioral changes • Understand current guidelines for managing obesity, including the role of pharmacological therapy as an adjunct to lifestyle changes in reducing weight gain and promoting weight loss • Review reimbursement options for intensive behavioral therapy (IBT) in obesity management
Resources WWW. TREATWEIGHTFIRST. ORG • On the official Weight First website, you can find: • Links to guidelines, papers, and studies referenced in the presentation • Access to presentation slides • Opportunity for AMA PRA Category 1 CME credit • More information about obesity medical management
- Slides: 64