24 3 2016 30 mins Dr Irfan Elahi



- Slides: 52
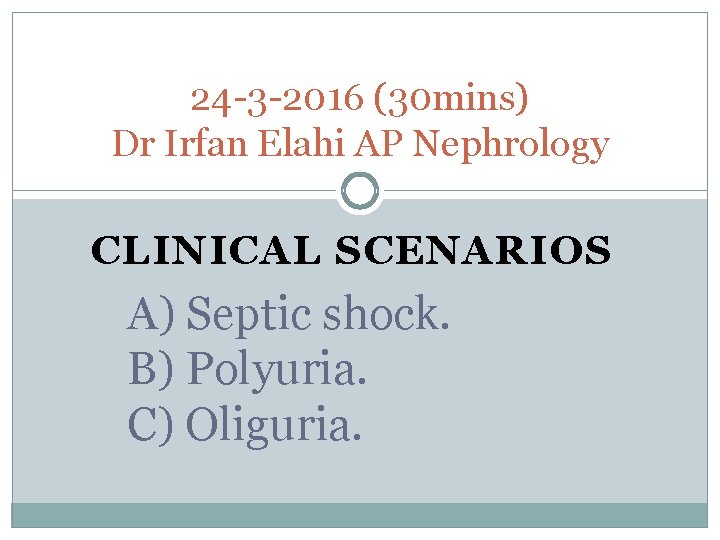
24 -3 -2016 (30 mins) Dr Irfan Elahi AP Nephrology CLINICAL SCENARIOS A) Septic shock. B) Polyuria. C) Oliguria.

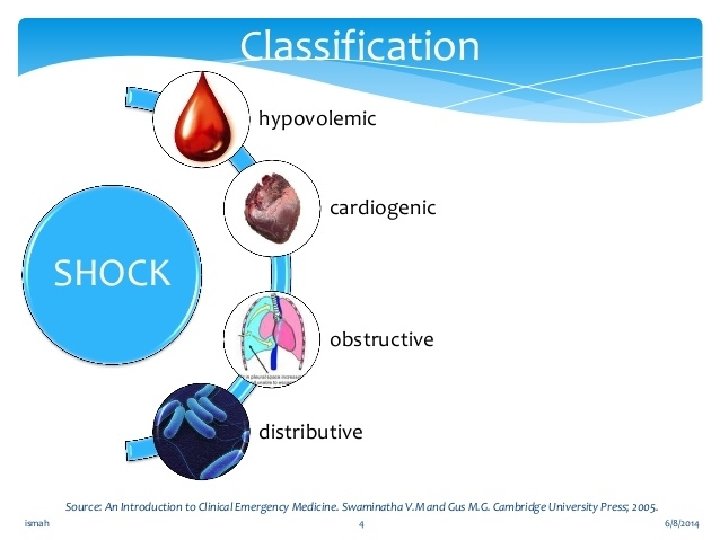
Shock

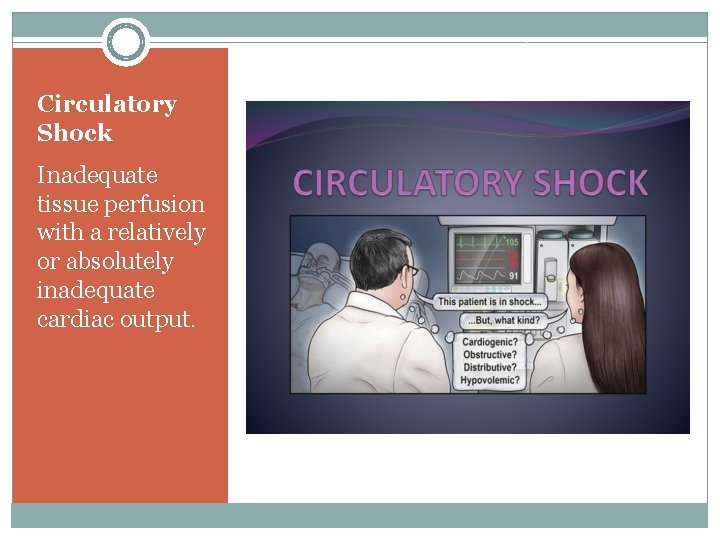
Circulatory Shock Inadequate tissue perfusion with a relatively or absolutely inadequate cardiac output.
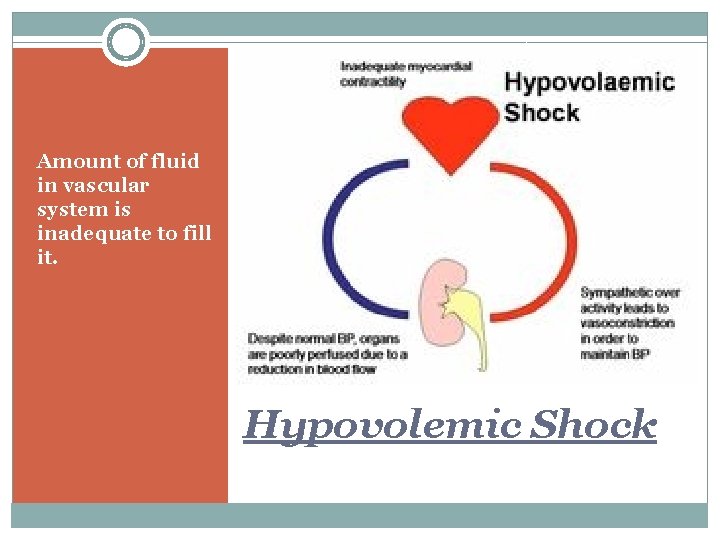
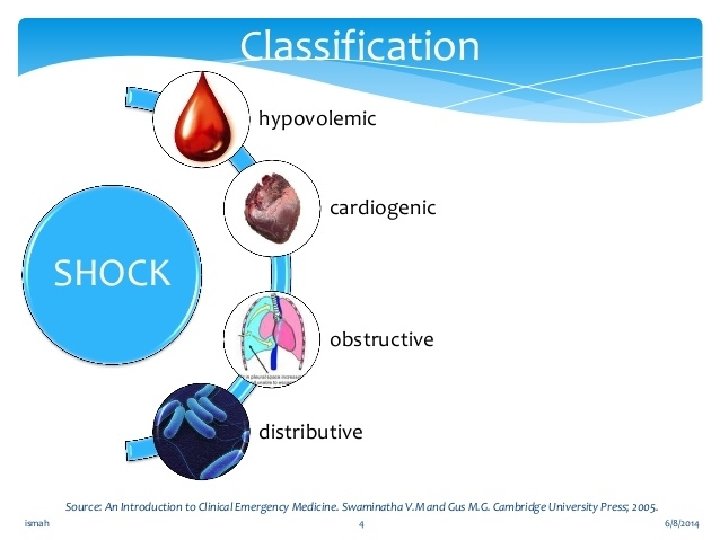
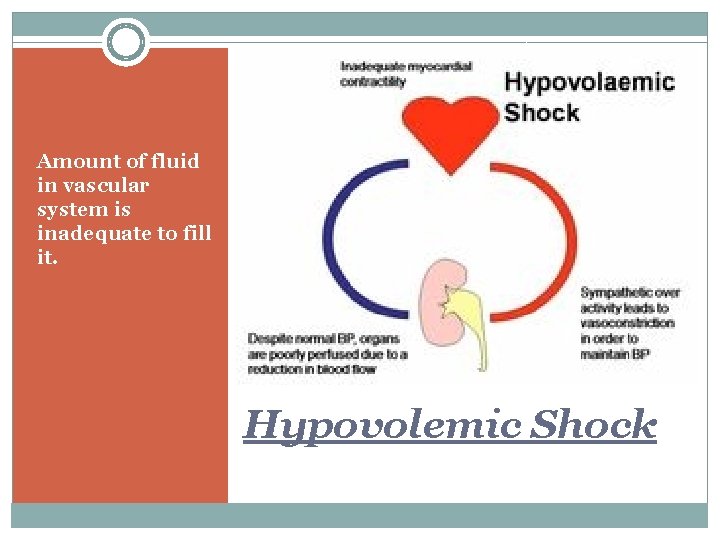
Amount of fluid in vascular system is inadequate to fill it. Hypovolemic Shock
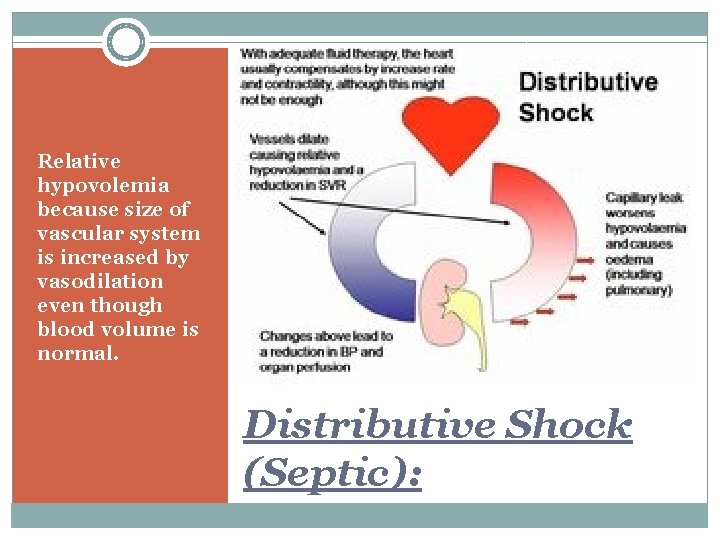
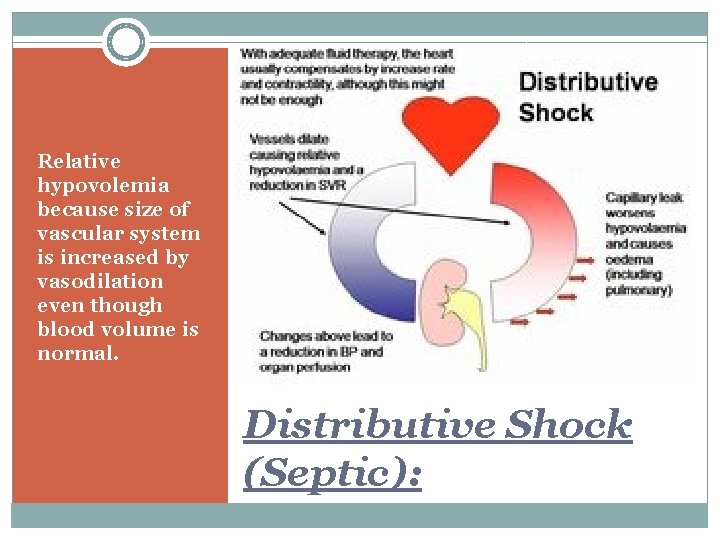
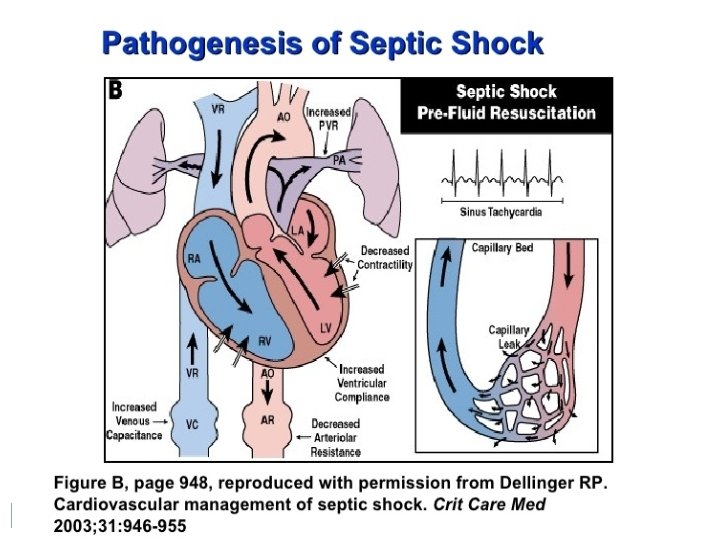
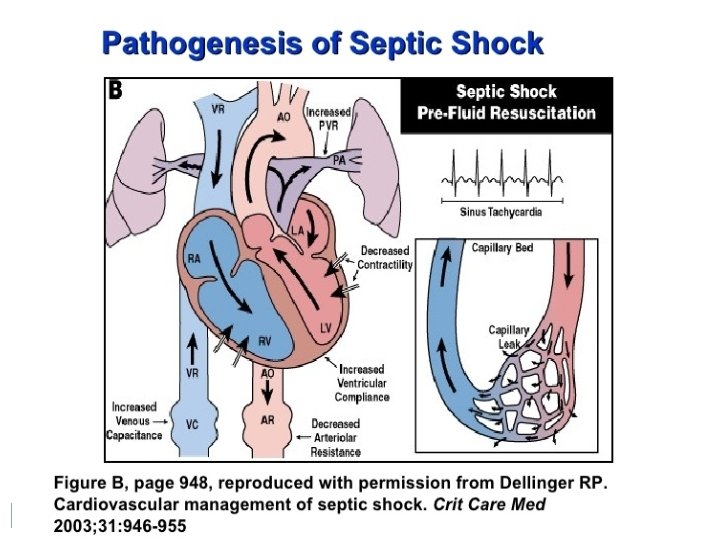
Relative hypovolemia because size of vascular system is increased by vasodilation even though blood volume is normal. Distributive Shock (Septic):
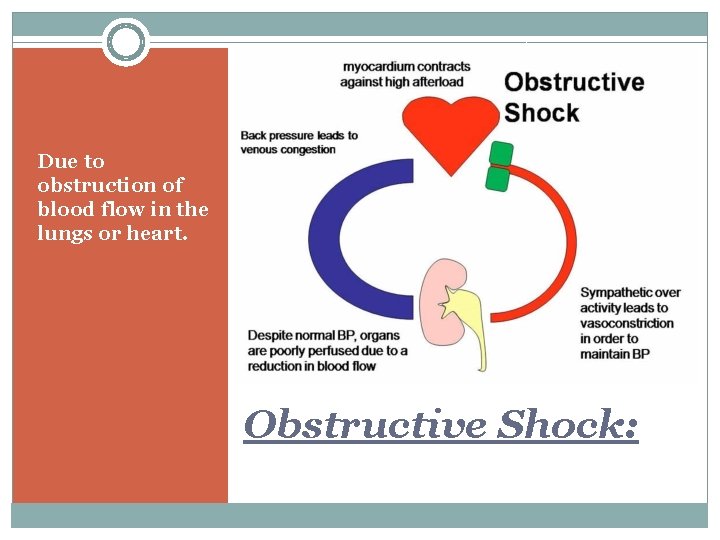
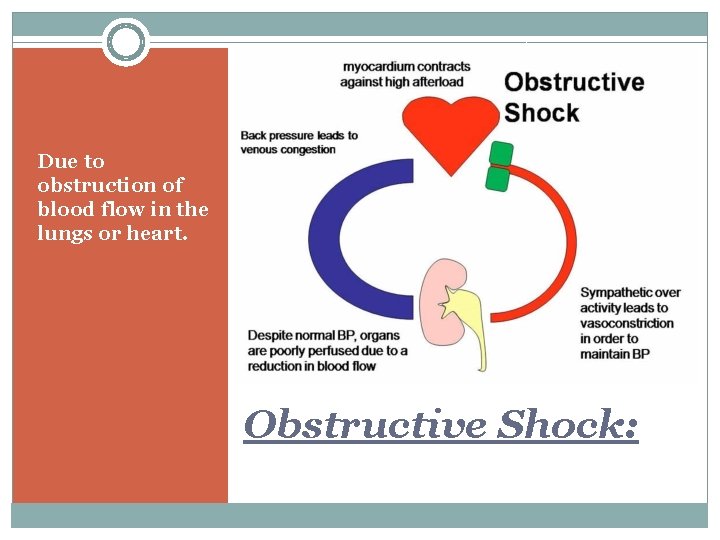
Due to obstruction of blood flow in the lungs or heart. Obstructive Shock:
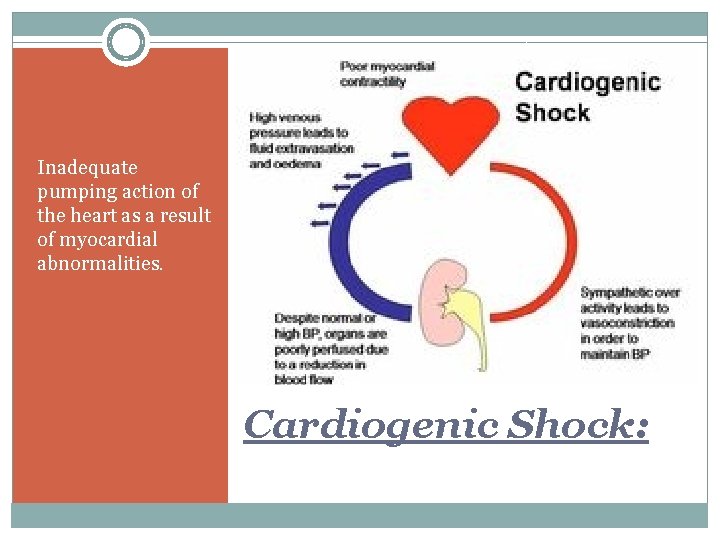
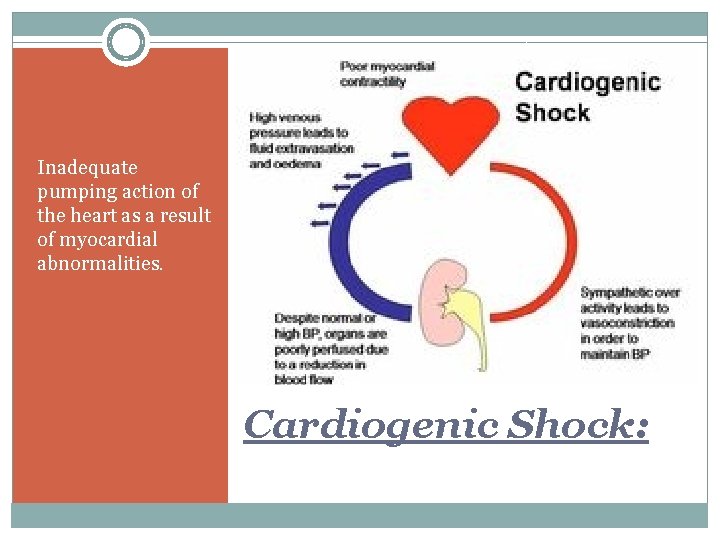
Inadequate pumping action of the heart as a result of myocardial abnormalities. Cardiogenic Shock:
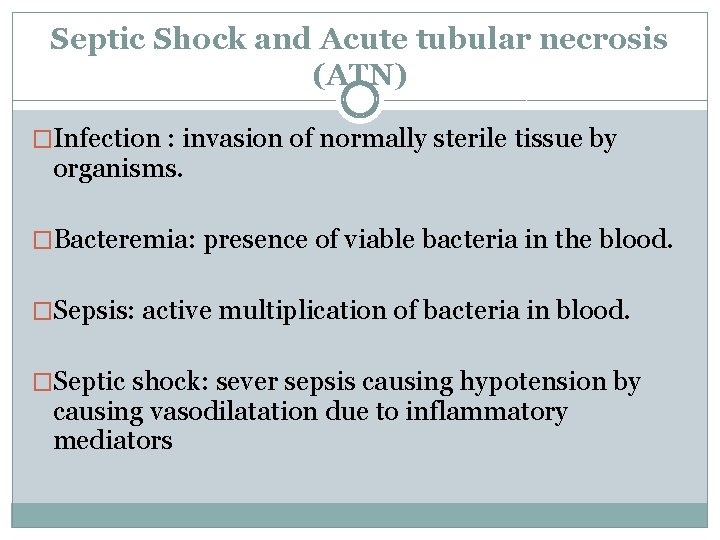
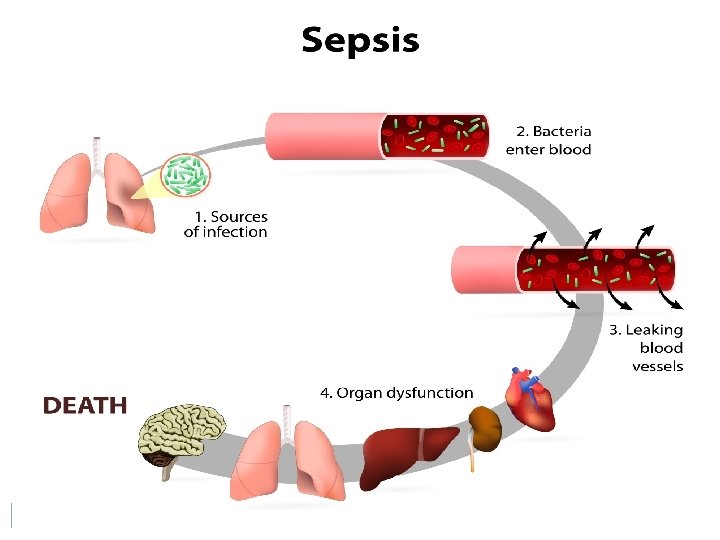
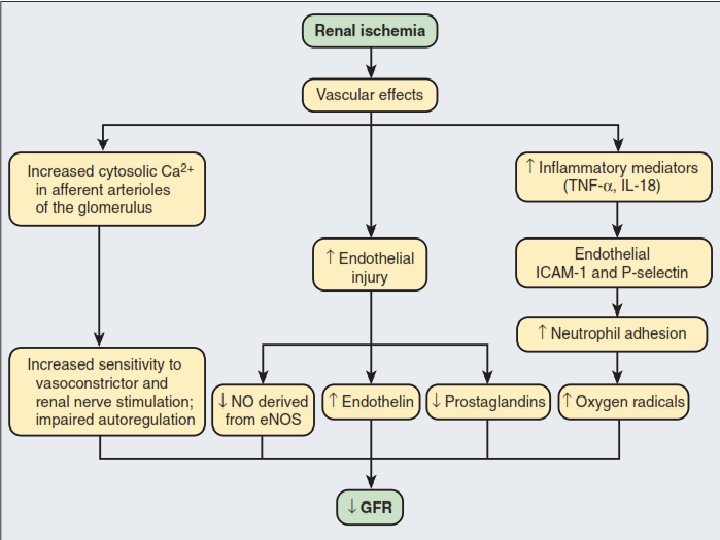
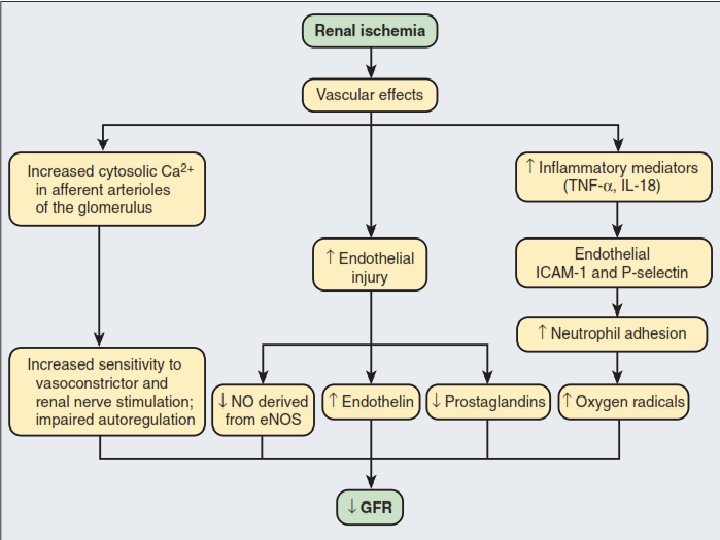
Septic Shock and Acute tubular necrosis (ATN) �Infection : invasion of normally sterile tissue by organisms. �Bacteremia: presence of viable bacteria in the blood. �Sepsis: active multiplication of bacteria in blood. �Septic shock: sever sepsis causing hypotension by causing vasodilatation due to inflammatory mediators
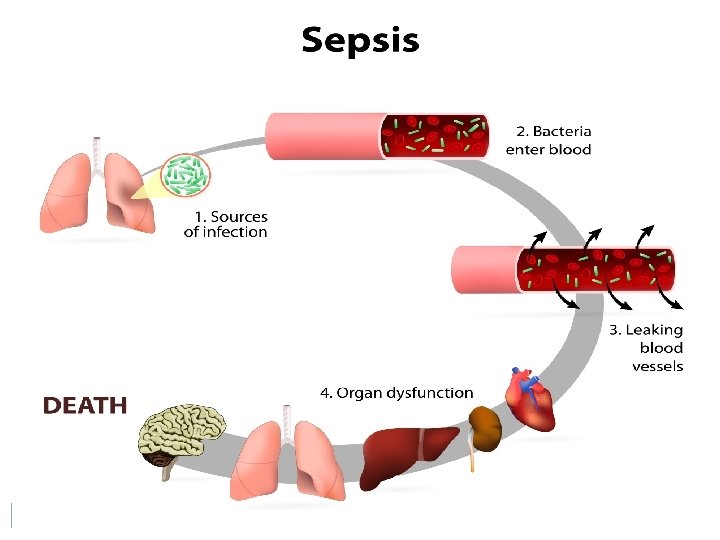
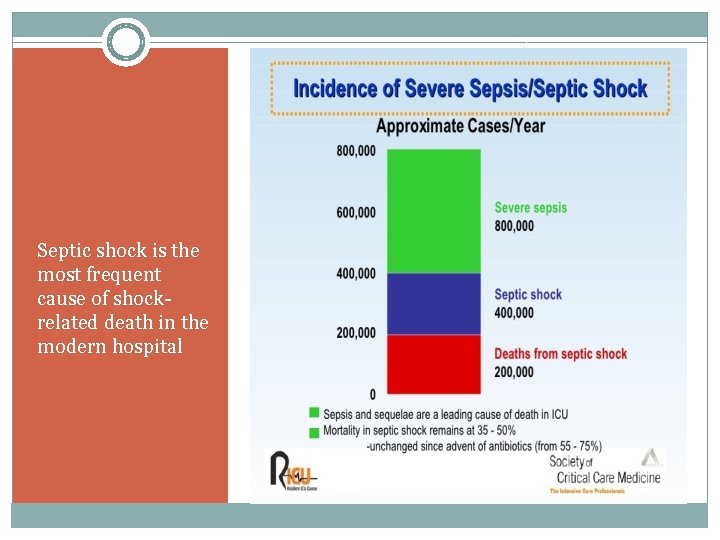
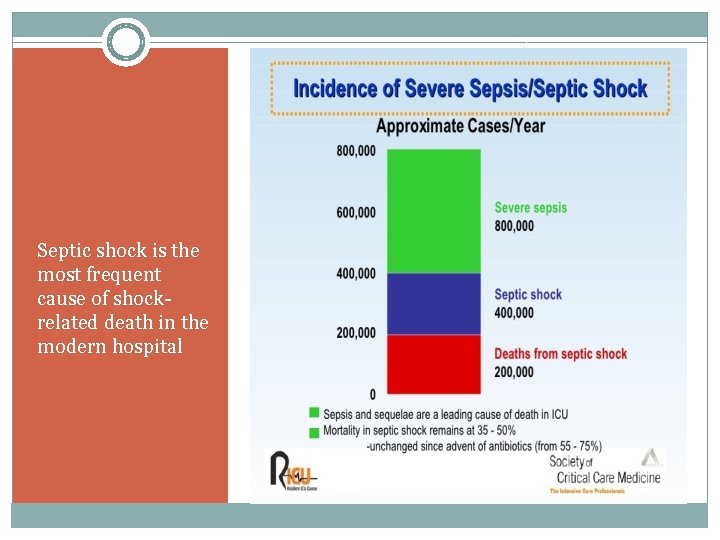
Septic shock is the most frequent cause of shockrelated death in the modern hospital
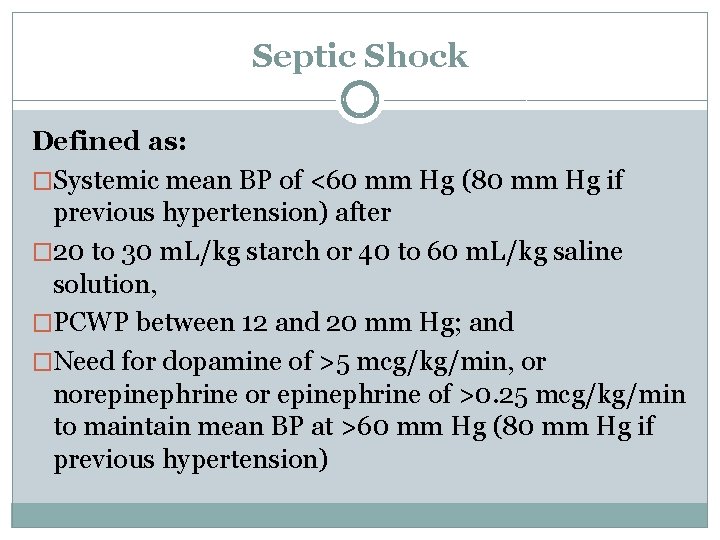
Septic Shock Defined as: �Systemic mean BP of <60 mm Hg (80 mm Hg if previous hypertension) after � 20 to 30 m. L/kg starch or 40 to 60 m. L/kg saline solution, �PCWP between 12 and 20 mm Hg; and �Need for dopamine of >5 mcg/kg/min, or norepinephrine or epinephrine of >0. 25 mcg/kg/min to maintain mean BP at >60 mm Hg (80 mm Hg if previous hypertension)
Acute Kidney Injury �Abrupt decline in GFR sufficient to decrease the elimination of nitrogenous waste products (urea and creatinine) and other uremic toxins. Definition of AKI �Decline in kidney function over 48 hours as demonstrated by An increase in serum creatinine of greater than 0. 3 mg/dl, An increase in serum creatinine of more than 50%, or The development of Oliguria.
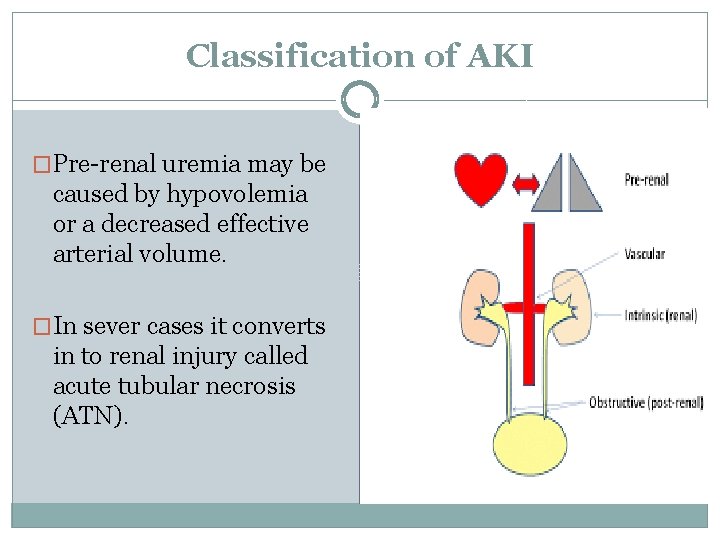
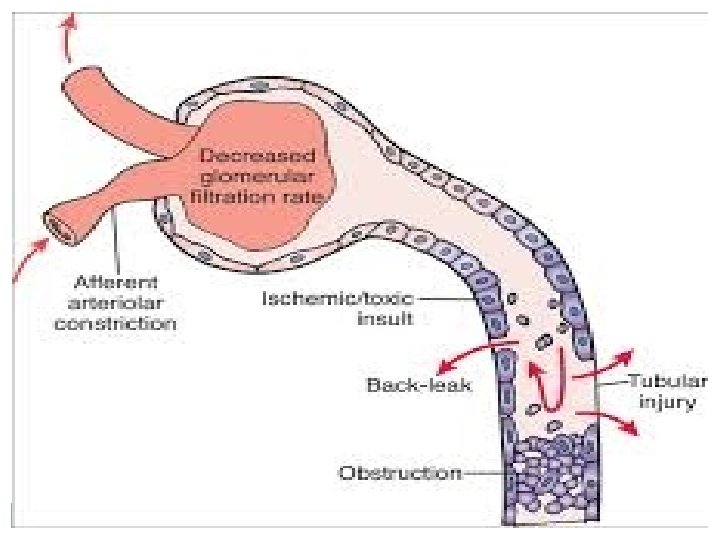
Classification of AKI �Pre-renal uremia may be caused by hypovolemia or a decreased effective arterial volume. �In sever cases it converts in to renal injury called acute tubular necrosis (ATN).
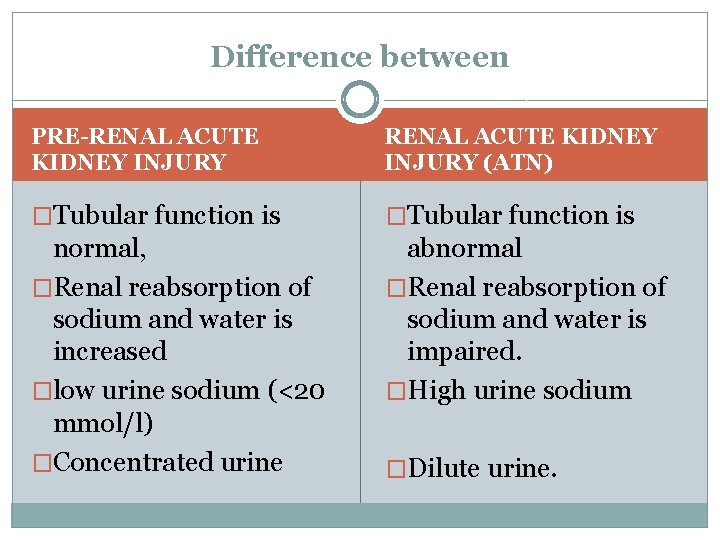
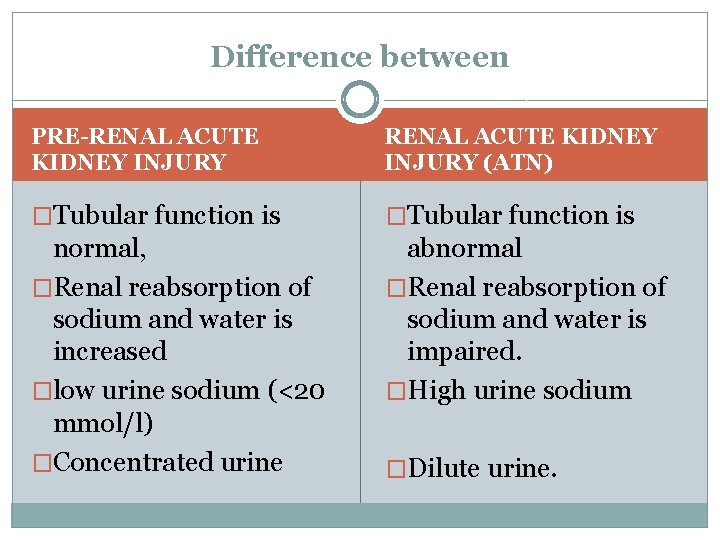
Difference between PRE-RENAL ACUTE KIDNEY INJURY (ATN) �Tubular function is normal, �Renal reabsorption of sodium and water is increased �low urine sodium (<20 mmol/l) �Concentrated urine abnormal �Renal reabsorption of sodium and water is impaired. �High urine sodium �Dilute urine.
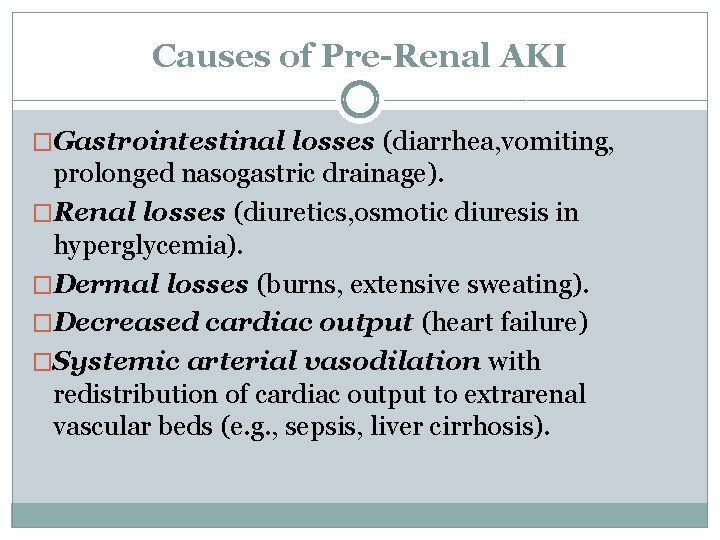
Causes of Pre-Renal AKI �Gastrointestinal losses (diarrhea, vomiting, prolonged nasogastric drainage). �Renal losses (diuretics, osmotic diuresis in hyperglycemia). �Dermal losses (burns, extensive sweating). �Decreased cardiac output (heart failure) �Systemic arterial vasodilation with redistribution of cardiac output to extrarenal vascular beds (e. g. , sepsis, liver cirrhosis).
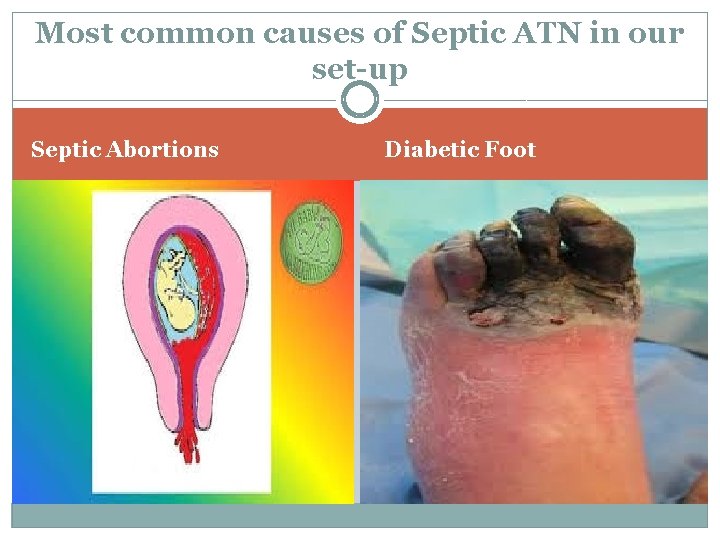
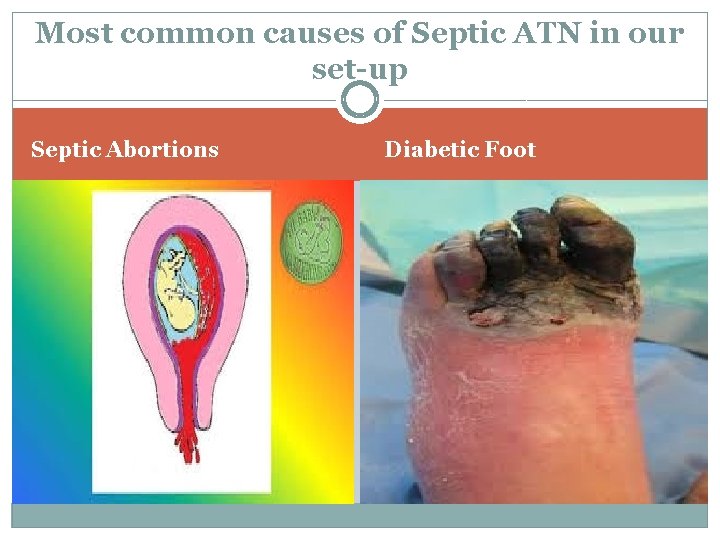
Most common causes of Septic ATN in our set-up Septic Abortions Diabetic Foot
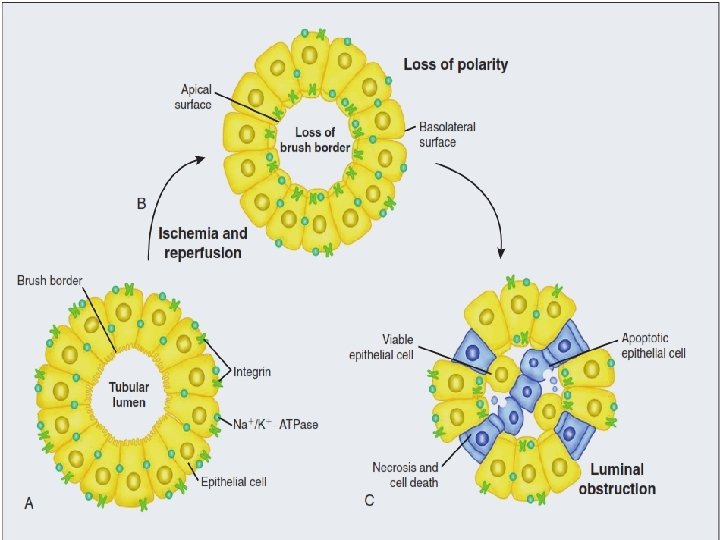
�Pre-renal AKI can be corrected if the extra-renal factors causing the renal hypoperfusion are rapidly reversed. �Failure to restore renal blood flow (RBF) during the functional pre-renal stage will ultimately lead to ATN and tubular cell injury
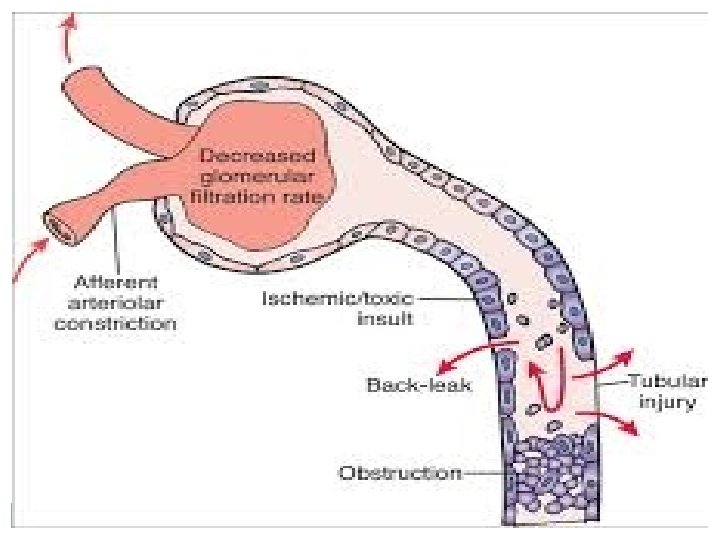
ATN �ATN is responsible for most cases of hospital- acquired AKI. �In the intensive care unit, two thirds of cases of AKI are a result of the combination of Impaired renal perfusion, Sepsis and Nephrotoxic agents
Single insult alone is rarely sufficient to induce ATN �Prolonged hypotension alone does not cause ATN. �Very high doses of single nephrotoxic agents are required to induce AKI. �Fever exacerbate ATN by increasing the renal tubular metabolic rate, thereby increasing ATP consumption. �In an experimental model (renal artery occlusion in the rat), renal ischemia for 40 minutes resulted in minimal renal injury at 32° C but marked renal injury at 39. 4° C.
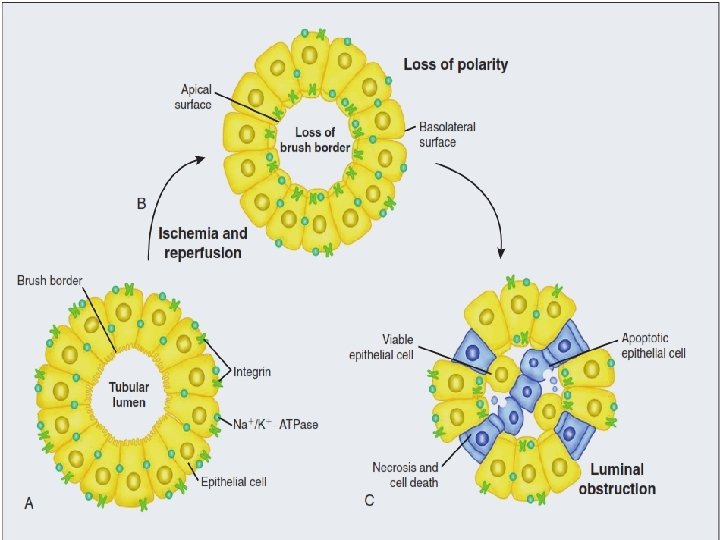
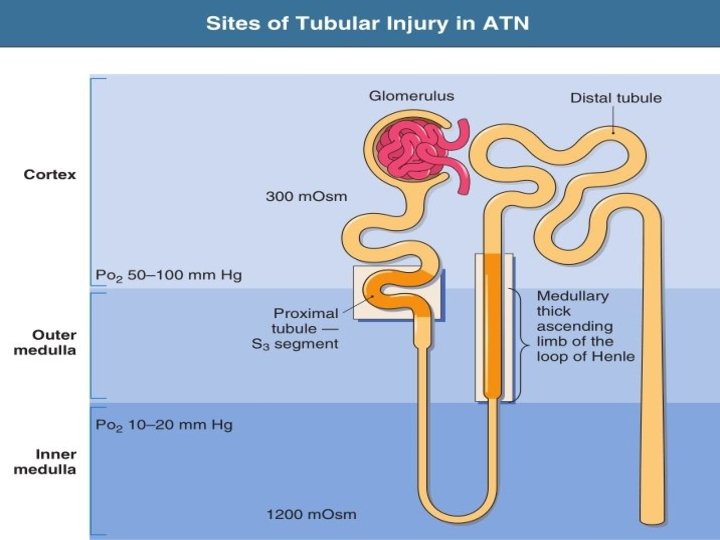
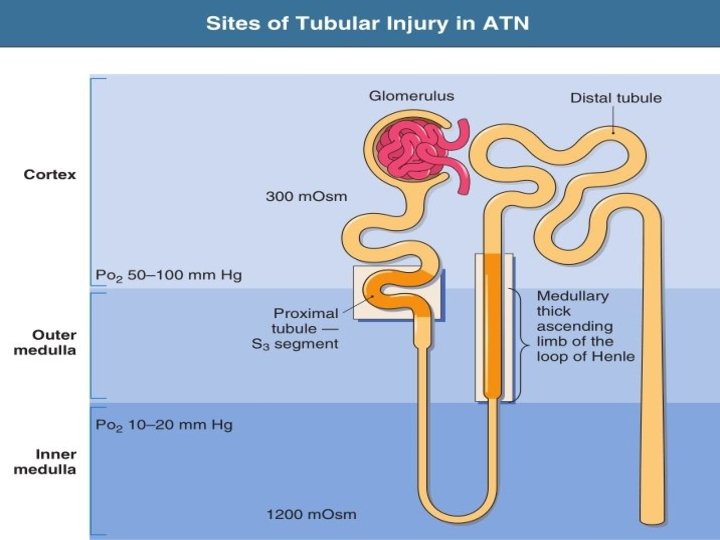
Course of uncomplicated ATN �Recovery over 2 to 3 weeks. �Superimposed renal insults often alter this pattern. �For example, episodes of hypotension induced by hemodialysis may lead to additional ischemic lesions, potentially prolonging renal functional recovery. �the S 3 segment of the proximal tubule and the medullary thick ascending limb (m. TAL) are particularly vulnerable to hypoxic injury
Polyuria
Polyuria �Urine output exceeding 3 L/day in adults and 2 L/m 2 in children �It must be differentiated from the more common complaints of frequency or nocturia, which are not associated with an increase in the total urine output
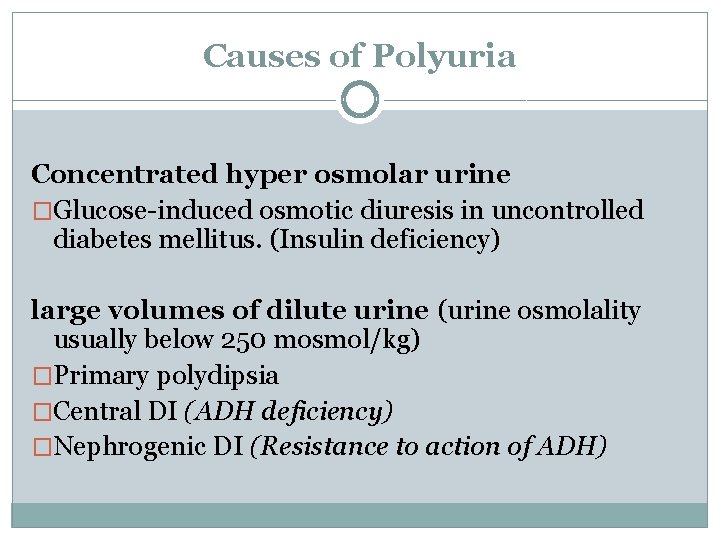
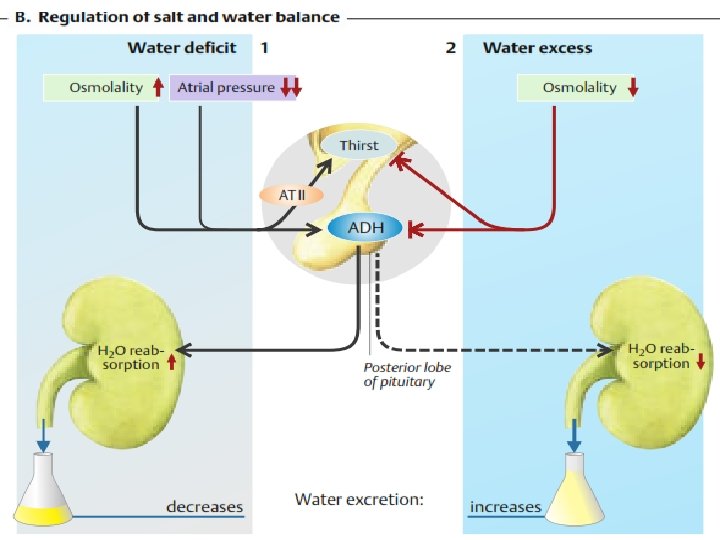
Causes of Polyuria Concentrated hyper osmolar urine �Glucose-induced osmotic diuresis in uncontrolled diabetes mellitus. (Insulin deficiency) large volumes of dilute urine (urine osmolality usually below 250 mosmol/kg) �Primary polydipsia �Central DI (ADH deficiency) �Nephrogenic DI (Resistance to action of ADH)
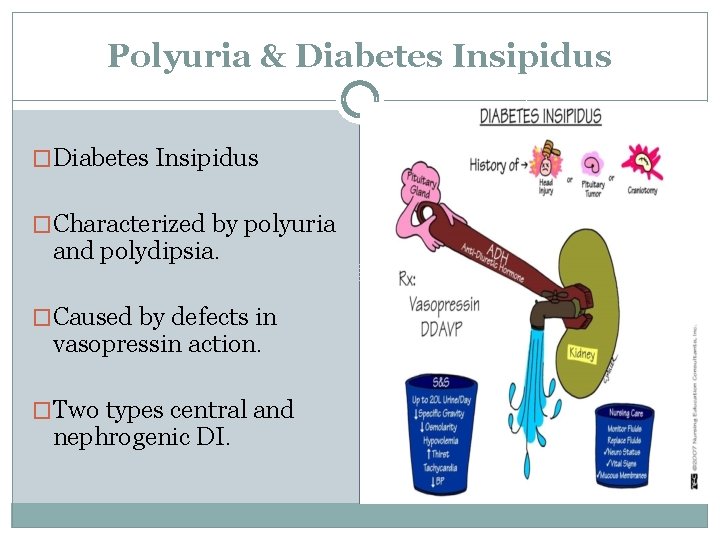
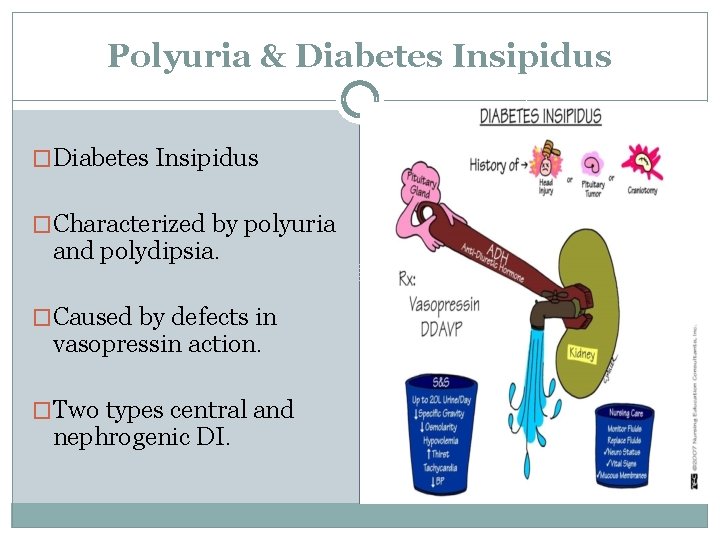
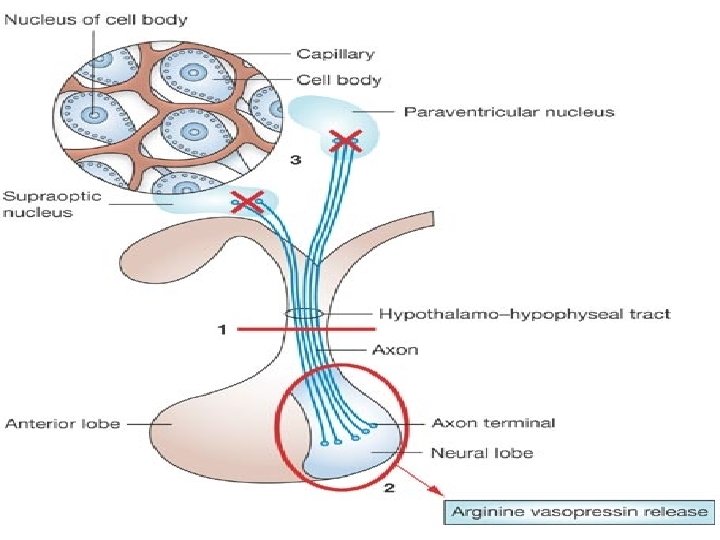
Polyuria & Diabetes Insipidus �Characterized by polyuria and polydipsia. �Caused by defects in vasopressin action. �Two types central and nephrogenic DI.
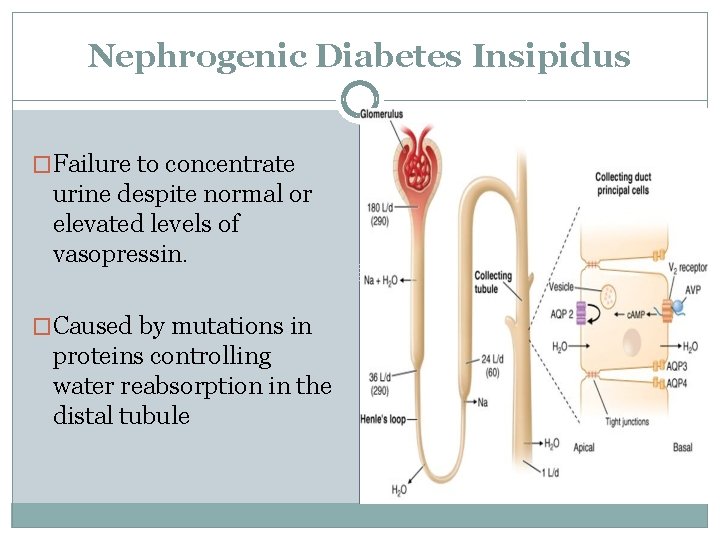
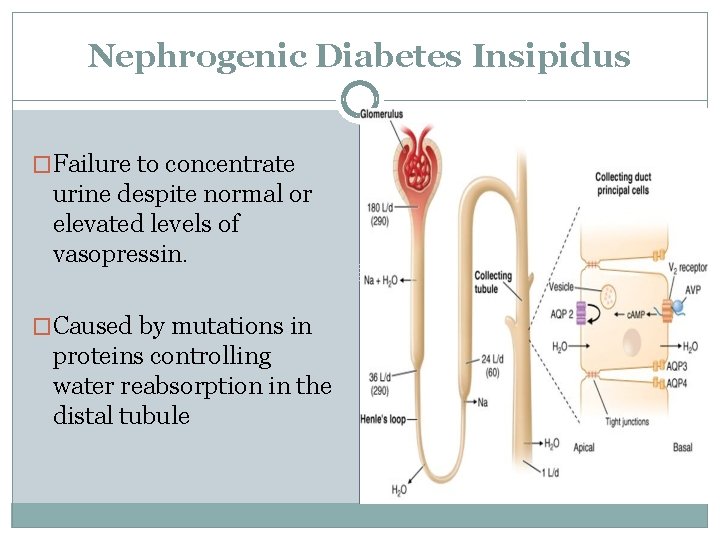
Nephrogenic Diabetes Insipidus �Failure to concentrate urine despite normal or elevated levels of vasopressin. �Caused by mutations in proteins controlling water reabsorption in the distal tubule
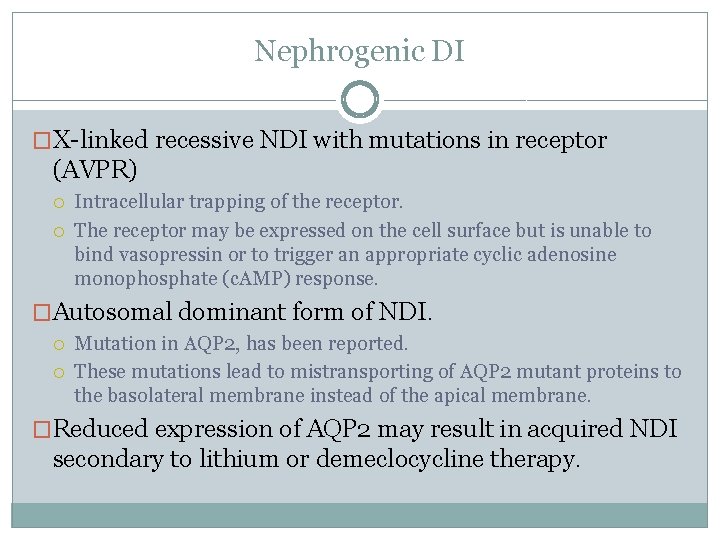
Nephrogenic DI �X-linked recessive NDI with mutations in receptor (AVPR) Intracellular trapping of the receptor. The receptor may be expressed on the cell surface but is unable to bind vasopressin or to trigger an appropriate cyclic adenosine monophosphate (c. AMP) response. �Autosomal dominant form of NDI. Mutation in AQP 2, has been reported. These mutations lead to mistransporting of AQP 2 mutant proteins to the basolateral membrane instead of the apical membrane. �Reduced expression of AQP 2 may result in acquired NDI secondary to lithium or demeclocycline therapy.
Clinical Features �Marked polyuria and excessive thirst. �Recurrent episodes of severe hypernatremic dehydration. �Delayed development and mental retardation. �Reduced intake of calories because of the large quantities of water that are ingested leads to growth failure beginning in early Childhood.
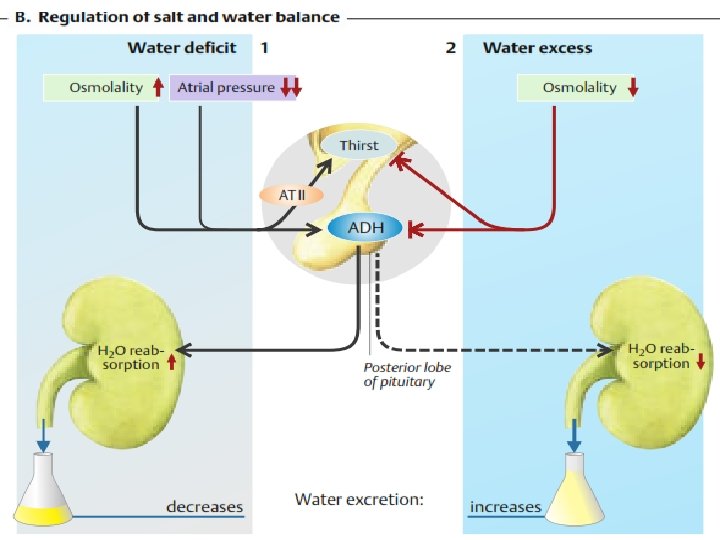
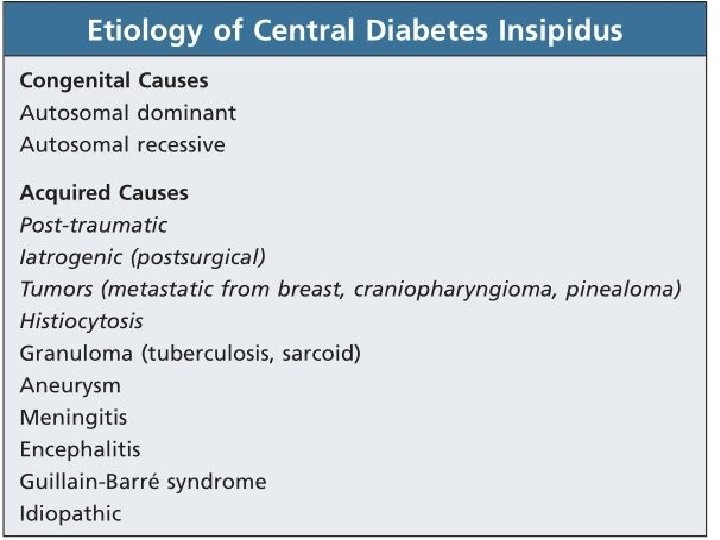
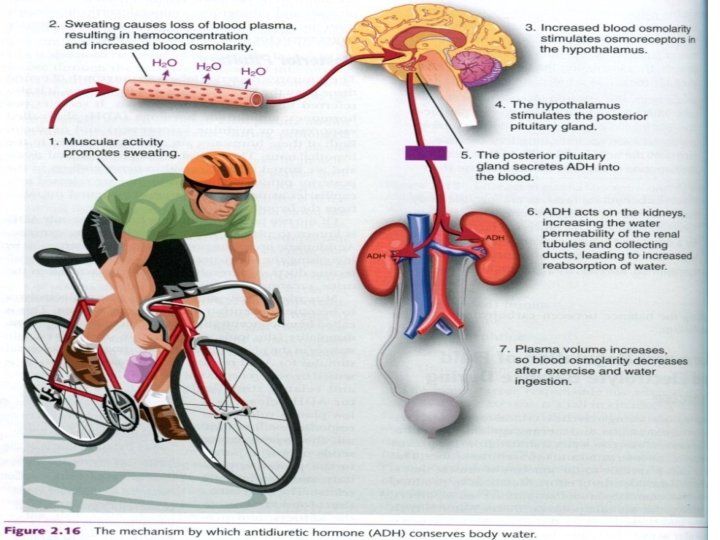
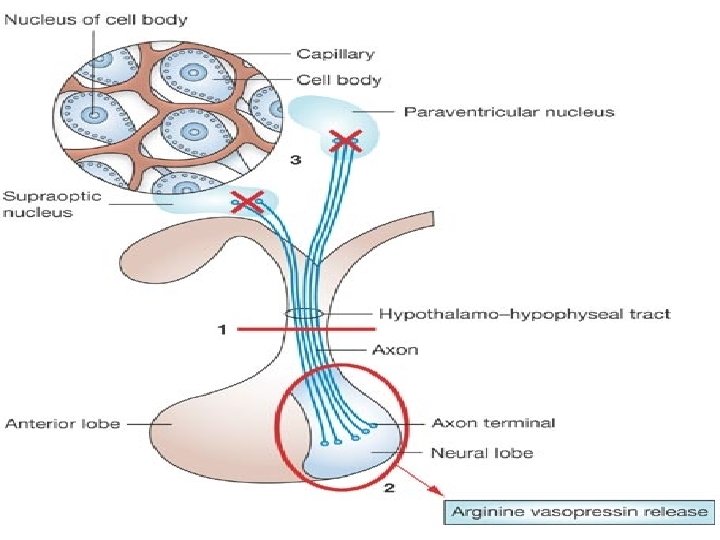
Central Diabetes Insipidus �Deficient secretion of antidiuretic hormone (ADH) �Central DI usually has an abrupt onset. �Patients have a constant need to drink, have a predilection for cold water, and typically have nocturia. �A plasma osmolality of more than 295 m. Osm/kg suggests central DI, and less than 270 m. Osm/kg suggests compulsive water drinking.
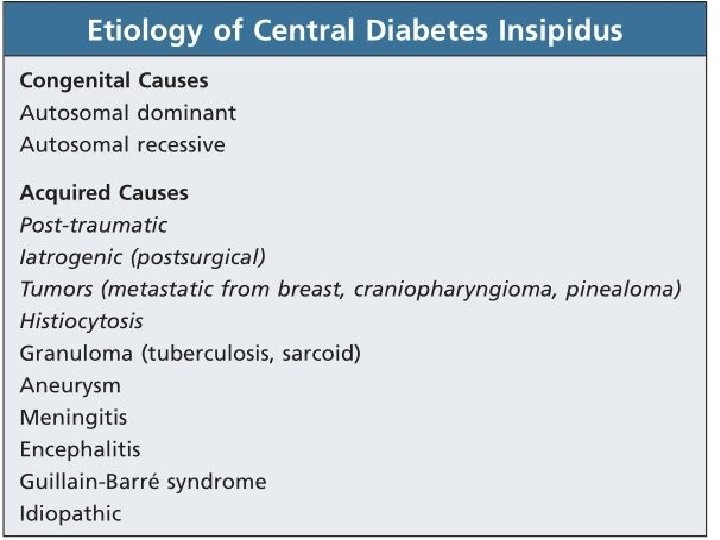
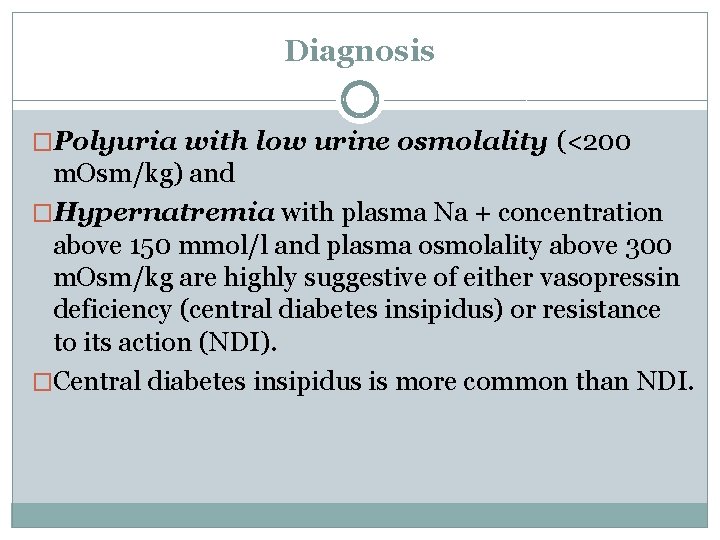
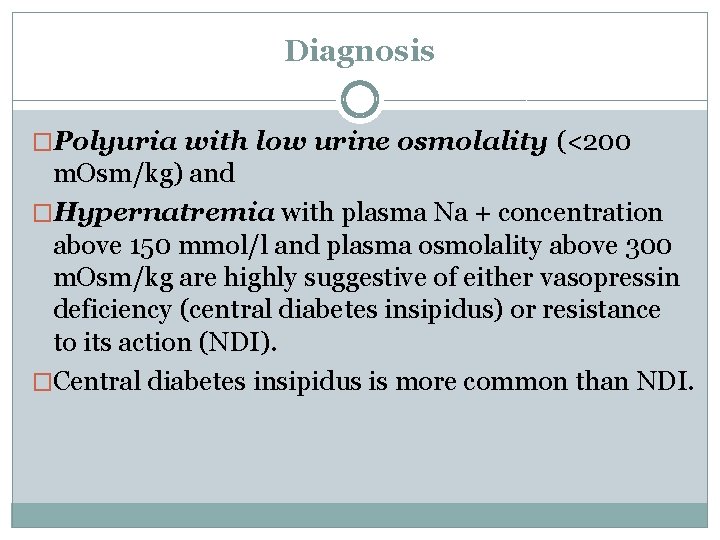
Diagnosis �Polyuria with low urine osmolality (<200 m. Osm/kg) and �Hypernatremia with plasma Na + concentration above 150 mmol/l and plasma osmolality above 300 m. Osm/kg are highly suggestive of either vasopressin deficiency (central diabetes insipidus) or resistance to its action (NDI). �Central diabetes insipidus is more common than NDI.
Differential Diagnosis �Patients with central diabetes insipidus show hypernatremia with inappropriately dilute urine, no primary renal disease, and a rise in urine osmolality after administration of vasopressin or its analogues.
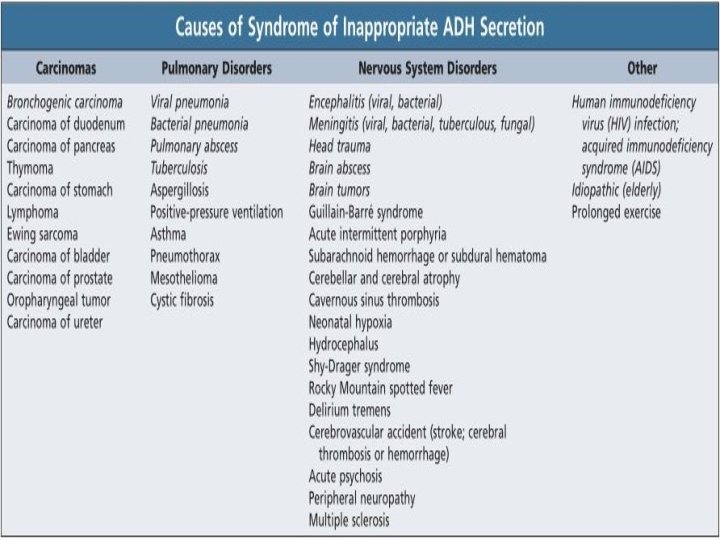
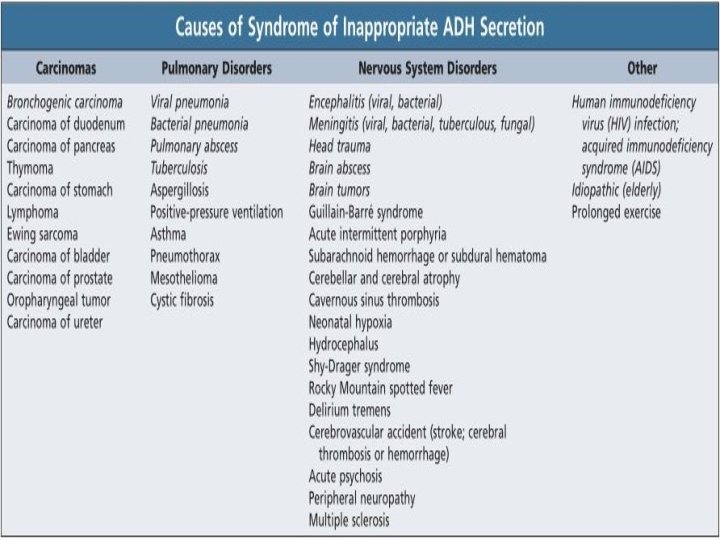
Syndrome of Inappropriate Antidiurectic Hormone (SIADH) �Most common cause of hyponatremia in hospitalized patients. �SIADH is a diagnosis of exclusion. �A defect in osmoregulation causes vasopressin to be inappropriately stimulated, leading to urine concentration �Vasopressin is responsible not only for dilutional hyponatremia (serum sodium < 135 mmol/L) but �Also for loss of salt in the urine when water retention is sufficient to expand the ECF volume, reducing aldosterone secretion
Anuria & Oliguria
Anuria & oliguria �Anuria urine volume 0 f less than 50 m. L in 24 hours. �Oliguria 50 to 400 m. L in 24 hours Causes �Shock �Complete bilateral urinary tract obstruction �Hemolytic-uremic syndrome �Renal cortical necrosis �Bilateral renal arterial obstruction �Crescentic or rapidly progressive glomerulonephritis.
Osmotic diuresis �The presence of large quantities of unreabsorbed solutes in the renal tubules causes an increase in urine volume called osmotic diuresis. �Solutes that are not reabsorbed in the proximal tubules exert an appreciable osmotic effect as the volume of tubular fluid decreases and their concentration rises.
�Proximal reabsorption of Na+ is prevented; more Na remains in the tubule, and water stays with it. �The result is that the loop of Henle is presented with a greatly increased volume of isotonic fluid. �This fluid has a decreased Na+ concentration, but the total amount of Na+ reaching the loop per unit time is increased
Causes �Administration of compounds such as Mannitol that is filtered but not reabsorbed. �Naturally occurring substances For example, in diabetes mellitus, if blood glucose is high, glucose in the glomerular filtrate is high, thus the filtered load will exceed the Tm and glucose will remain in the tubules causing polyuria
�Diuresis can also be produced by the infusion of large amounts of sodium chloride or urea. �It is important to recognize the difference between osmotic diuresis and water diuresis
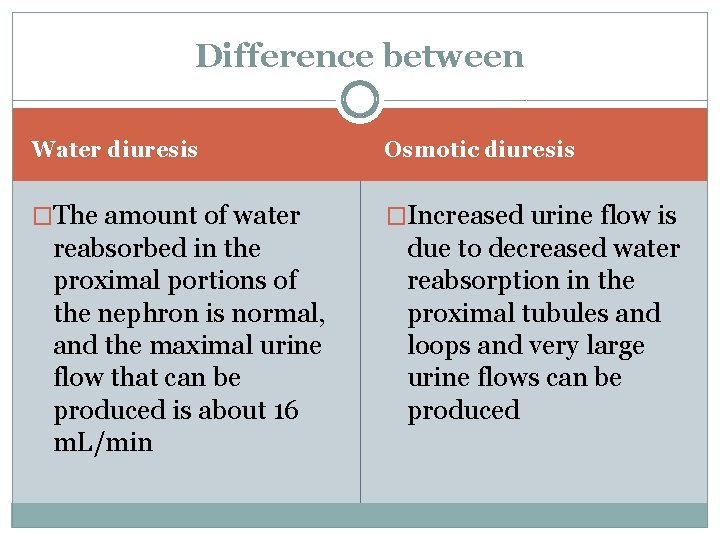
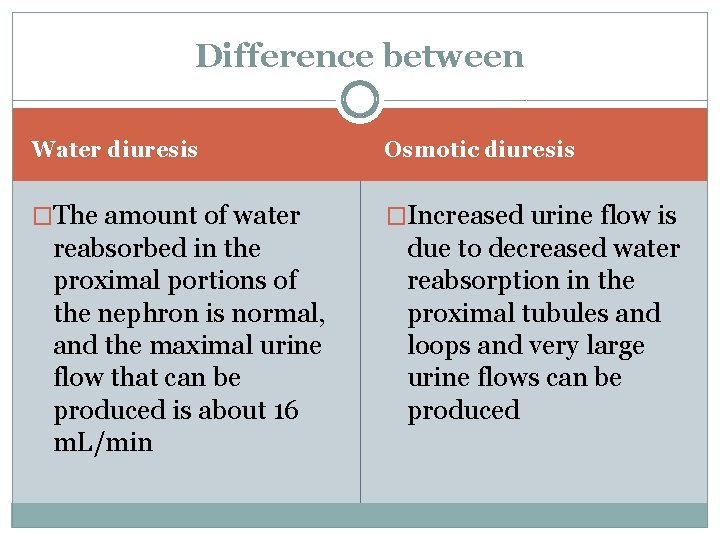
Difference between Water diuresis Osmotic diuresis �The amount of water �Increased urine flow is reabsorbed in the proximal portions of the nephron is normal, and the maximal urine flow that can be produced is about 16 m. L/min due to decreased water reabsorption in the proximal tubules and loops and very large urine flows can be produced
