2021 Office EM Coding Changes Beginning January 2021
2021 Office E/M Coding Changes
Beginning January 2021 • Physicians billing for Medicare patients will no longer have to use a patient's history or physical exam to determine the appropriate level of E/M coding • The amount of information documented for the history and physical exam is at the discretion of the physician, however, they will no longer have to use two out of the three elements (history, exam, medical decision making) to determining the level of E/M to bill • Now, physicians can choose from either (1) time OR (2) medical decision making to determine code selection 2
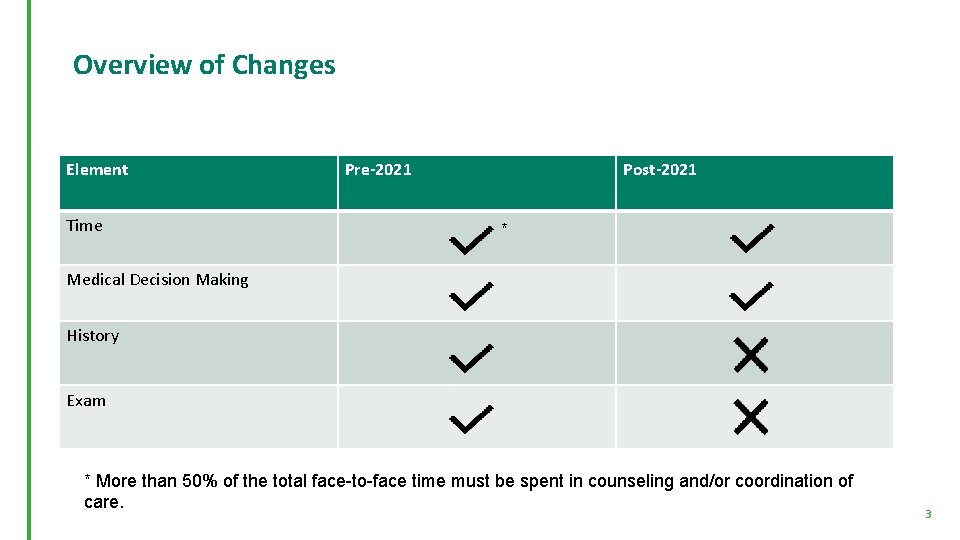
Overview of Changes Element Time Pre-2021 Post-2021 * Medical Decision Making History Exam * More than 50% of the total face-to-face time must be spent in counseling and/or coordination of care. 3
Using Time • Total time includes both the total face-to-face and non-face-to-face time spent on the date of the patient encounter by the physicians and other qualified health professionals • The requirement that 50% of the total time be spent providing counseling and/or coordination of care no longer applies beginning in 2021 • These activities count toward time, if they are performed on the day of the visit: • preparing to see the patient (reviewing tests, etc. ) • obtaining and/or reviewing separately obtained history • performing a medically appropriate examination and/or evaluation • counseling and educating the patient/family/caregiver • ordering medications, tests, or procedures • referring and communicating with other health care professionals (when not separately reported) • documenting clinical information in the electronic or other health record • independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver • coordinating care (not separately reported) 4
Medical Decision Making • Physician's billing Medicare may continue to use medical decision making to determine E/M code selection using three elements: • the number and complexity of problem(s) that are addressed during the encounter, • the amount and/or complexity of data to be reviewed analyzed, and • the risk of complications, morbidity, and/or mortality of patient management decisions made at the visit associated with the patient’s problem(s), the diagnostic procedure(s), and treatment(s). • Once physicians have reviewed these elements, they are able to determine the level of medical decision making; straightforward, low complexity, moderate complexity, or high complexity. In turn, this determination allows for the appropriate code selection • Comorbidities/underlying diseases, in and of themselves, are not considered in selecting a level of E/M services unless their presence significantly increases the complexity of the MDM 5
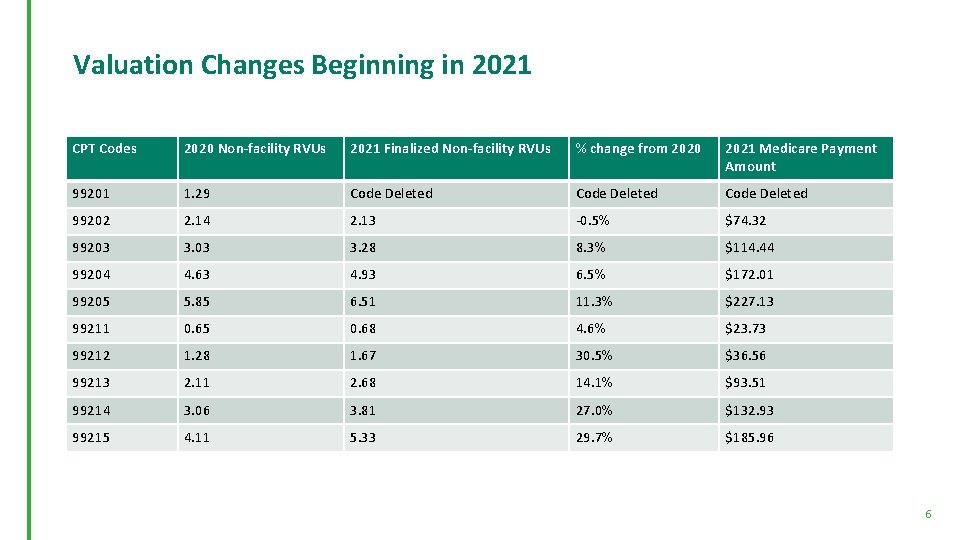
Valuation Changes Beginning in 2021 CPT Codes 2020 Non-facility RVUs 2021 Finalized Non-facility RVUs % change from 2020 2021 Medicare Payment Amount 99201 1. 29 Code Deleted 99202 2. 14 2. 13 -0. 5% $74. 32 99203 3. 28 8. 3% $114. 44 99204 4. 63 4. 93 6. 5% $172. 01 99205 5. 85 6. 51 11. 3% $227. 13 99211 0. 65 0. 68 4. 6% $23. 73 99212 1. 28 1. 67 30. 5% $36. 56 99213 2. 11 2. 68 14. 1% $93. 51 99214 3. 06 3. 81 27. 0% $132. 93 99215 4. 11 5. 33 29. 7% $185. 96 6
99417 G 2212 • Physicians can now bill a new prolonged services code 99417 • Prolonged office or other outpatient evaluation and management service(s) beyond the maximum required time of the primary procedure which has been selected using total time on the date of the primary service; each additional 15 minutes by the physician or qualified healthcare professional, with or without direct patient contact • Prolonged office or other outpatient E/M service(s), each 15 minutes • This can be billed with CPT codes 99205 and 99215 when time is used as the primary basis for code selection 7
- Slides: 7