2019 4 23 M 115 Genitourinary Cancer Surgery



- Slides: 49
2019 -4 -23 M 115 Genitourinary Cancer Surgery 吳 勝 堂 醫師 三軍總醫院 泌尿外科
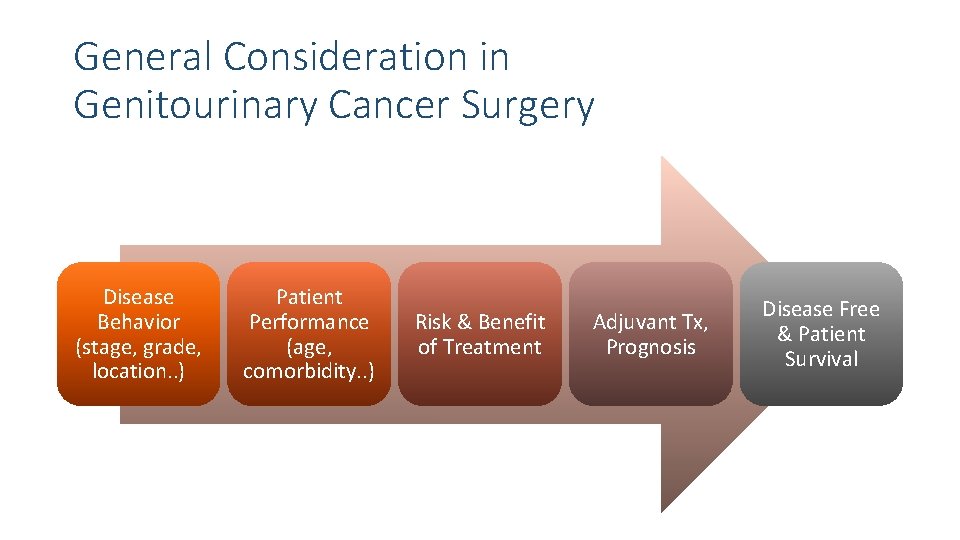
General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . )
General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . ) Patient Performance (age, comorbidity. . )

General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . ) Patient Performance (age, comorbidity. . ) Risk & Benefit of Treatment
General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . ) Patient Performance (age, comorbidity. . ) Risk & Benefit of Treatment Adjuvant Tx, Prognosis
General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . ) Patient Performance (age, comorbidity. . ) Risk & Benefit of Treatment Adjuvant Tx, Prognosis Disease Free & Patient Survival
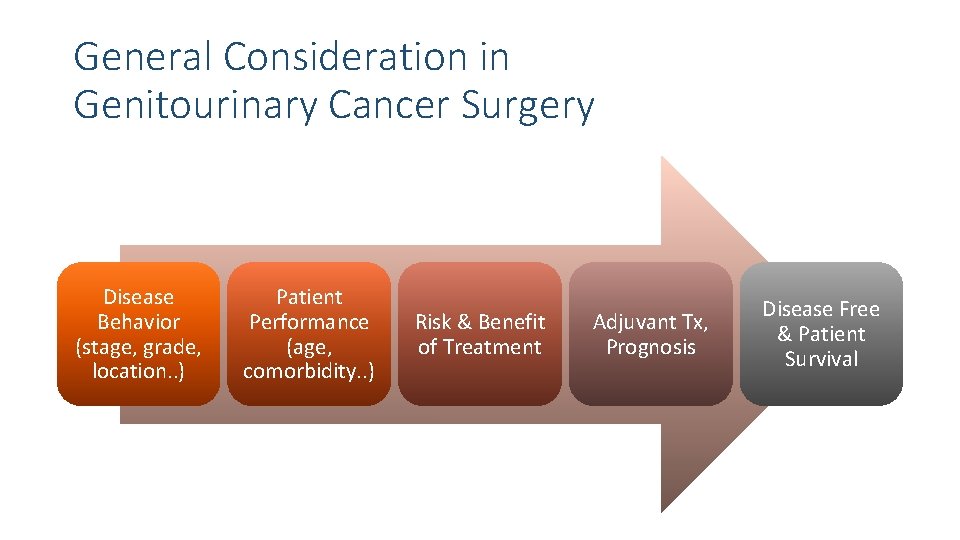
General Consideration in Genitourinary Cancer Surgery Disease Behavior (stage, grade, location. . ) Patient Performance (age, comorbidity. . ) Risk & Benefit of Treatment Adjuvant Tx, Prognosis Disease Free & Patient Survival
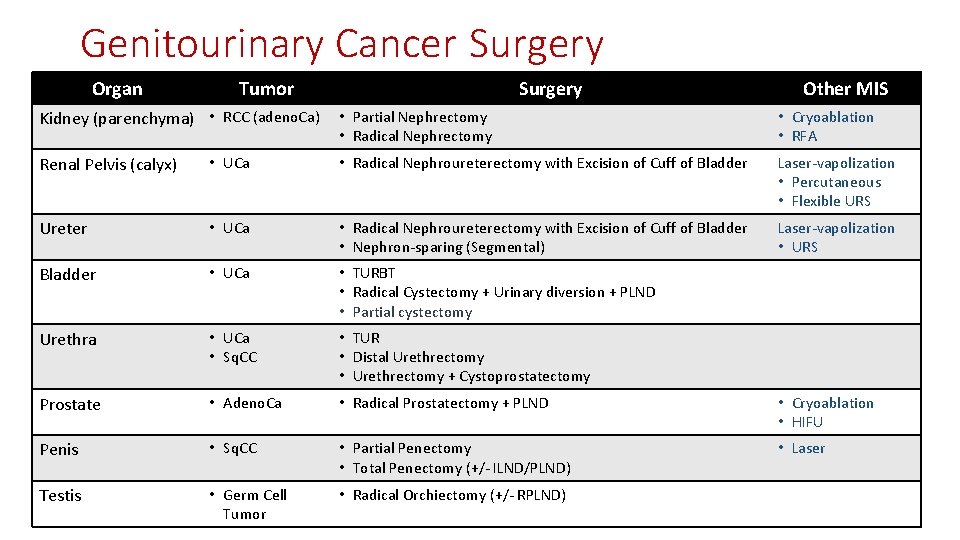
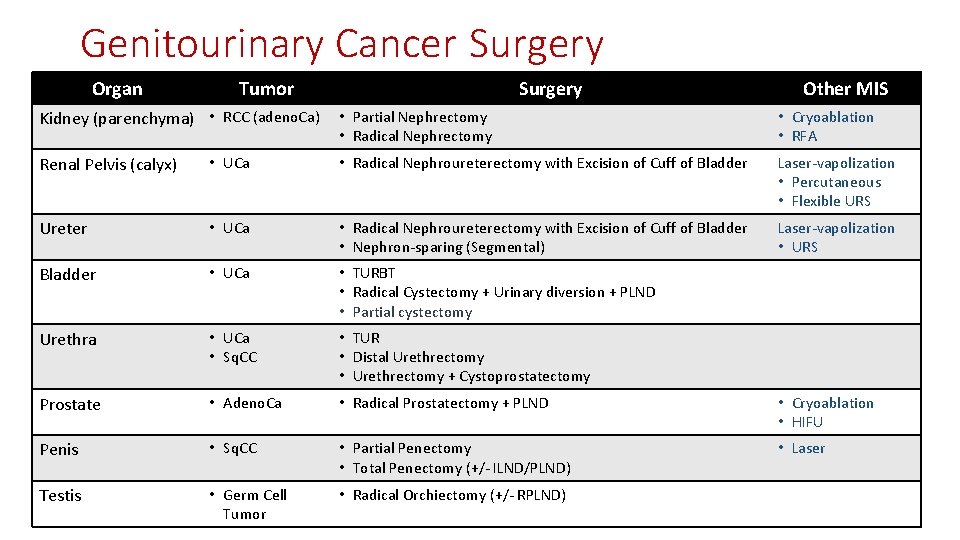
Genitourinary Cancer Surgery Organ Tumor Surgery Other MIS Kidney (parenchyma) • RCC (adeno. Ca) • Partial Nephrectomy • Radical Nephrectomy • Cryoablation • RFA Renal Pelvis (calyx) • UCa • Radical Nephroureterectomy with Excision of Cuff of Bladder Laser-vapolization • Percutaneous • Flexible URS Ureter • UCa • Radical Nephroureterectomy with Excision of Cuff of Bladder • Nephron-sparing (Segmental) Laser-vapolization • URS Bladder • UCa • TURBT • Radical Cystectomy + Urinary diversion + PLND • Partial cystectomy Urethra • UCa • Sq. CC • TUR • Distal Urethrectomy • Urethrectomy + Cystoprostatectomy Prostate • Adeno. Ca • Radical Prostatectomy + PLND • Cryoablation • HIFU Penis • Sq. CC • Partial Penectomy • Total Penectomy (+/- ILND/PLND) • Laser Testis • Germ Cell Tumor • Radical Orchiectomy (+/- RPLND)
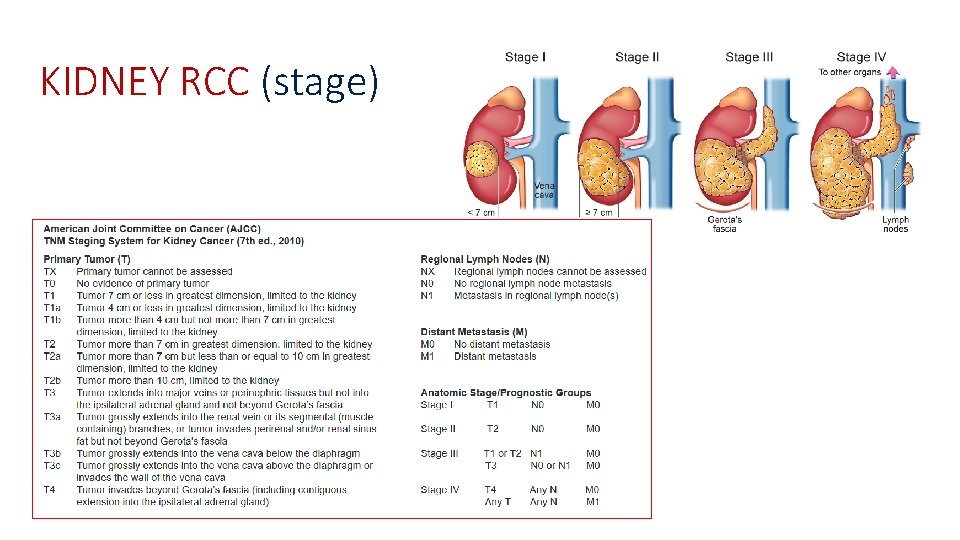
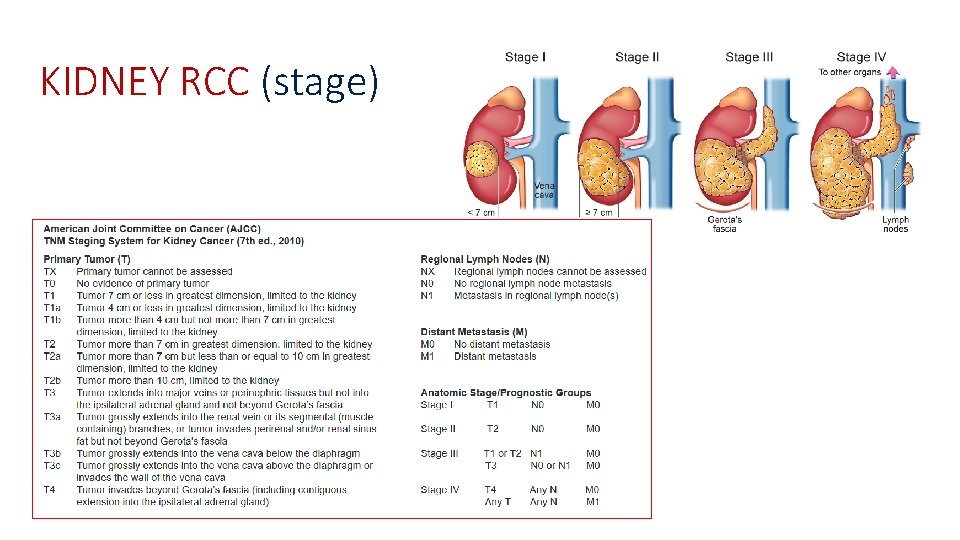
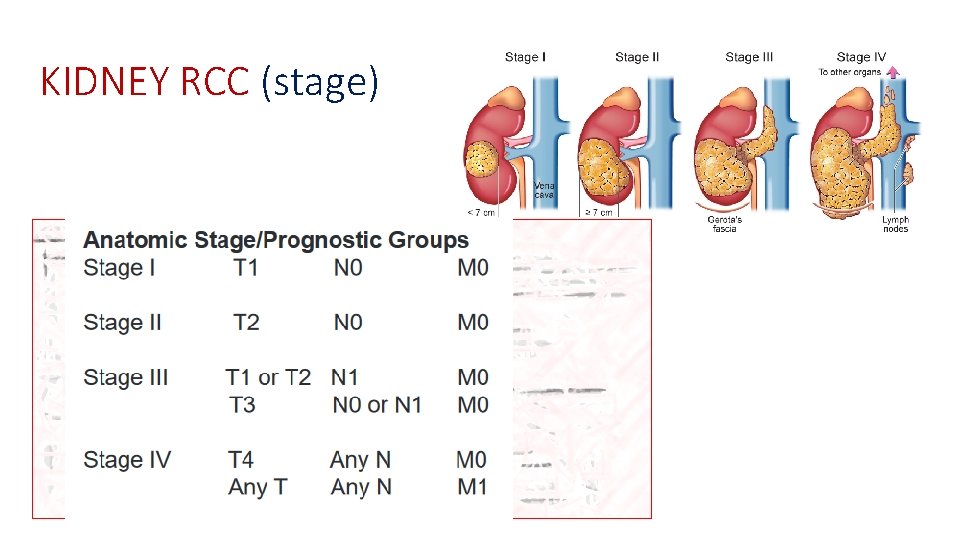
KIDNEY RCC (stage)
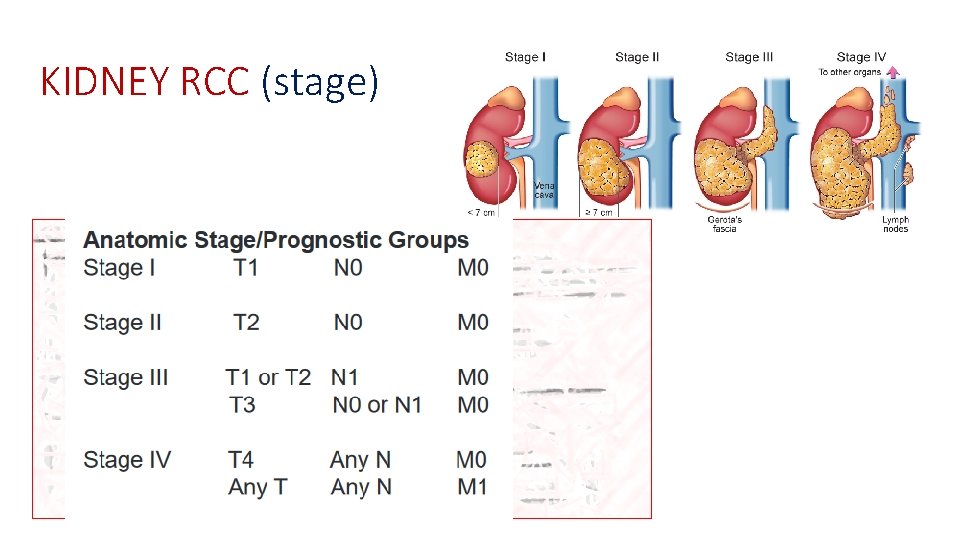
KIDNEY RCC (stage)
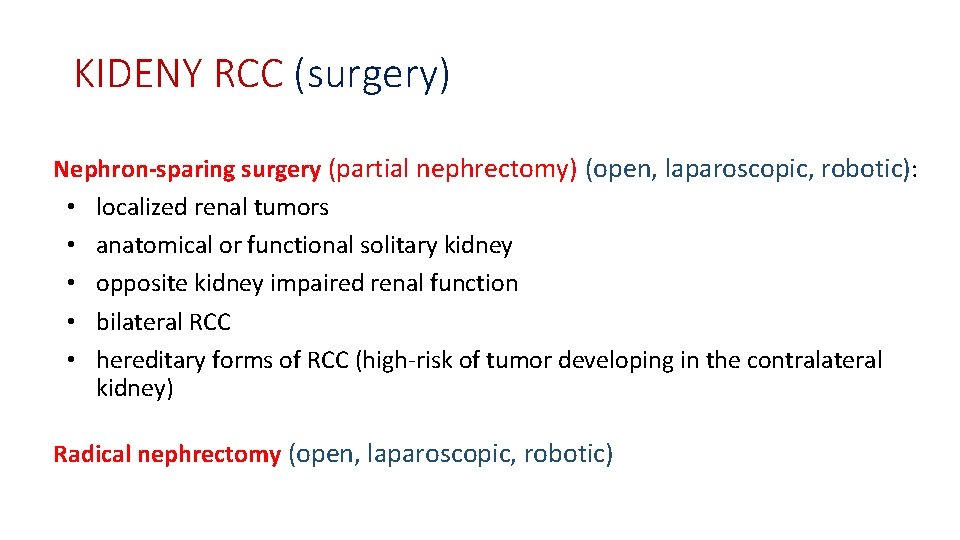
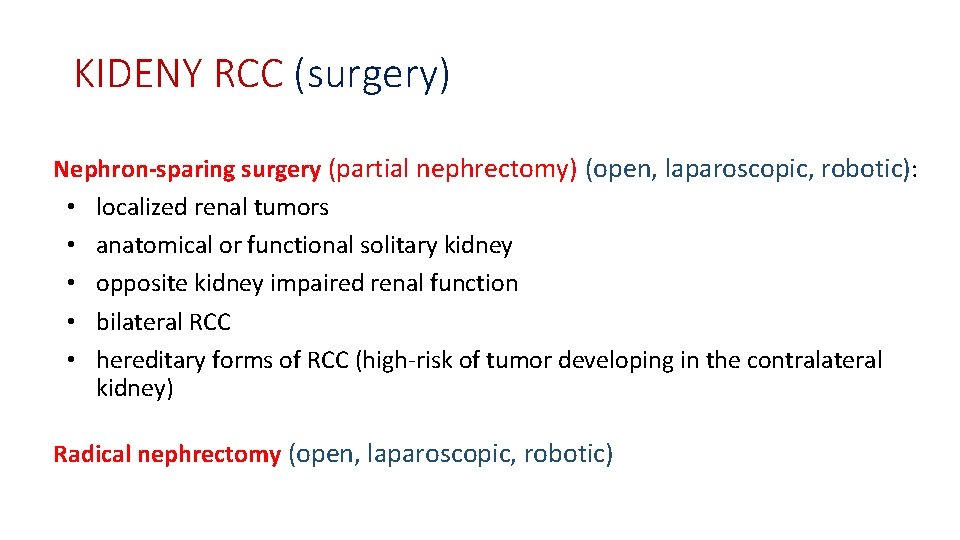
KIDENY RCC (surgery) Nephron-sparing surgery (partial nephrectomy) (open, laparoscopic, robotic): • localized renal tumors • anatomical or functional solitary kidney • opposite kidney impaired renal function • bilateral RCC • hereditary forms of RCC (high-risk of tumor developing in the contralateral kidney) Radical nephrectomy (open, laparoscopic, robotic)
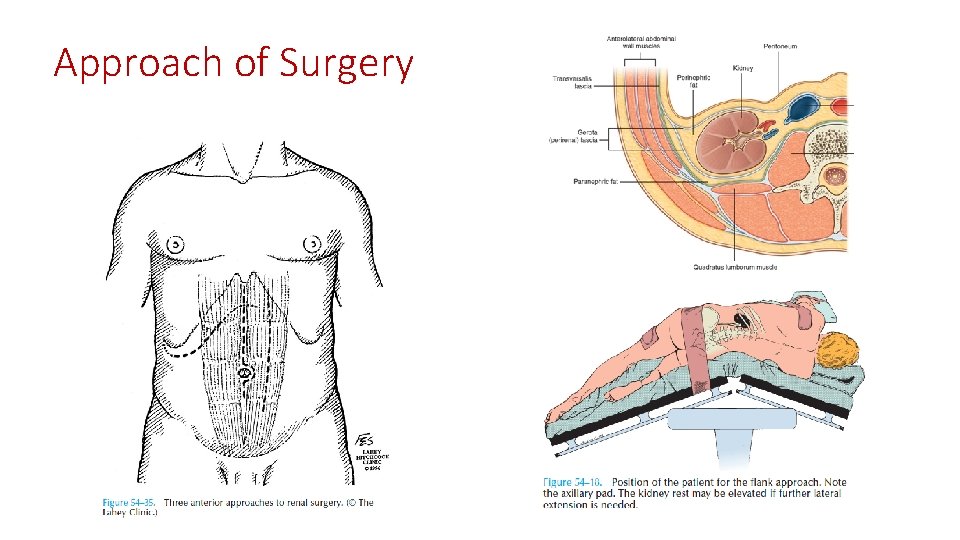
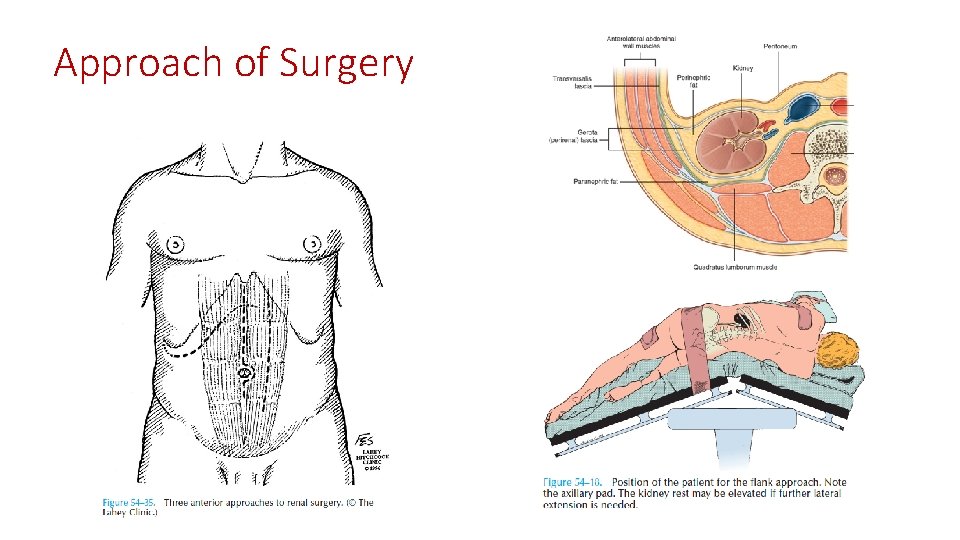
Approach of Surgery

Partial vs Radical Nephrectomy
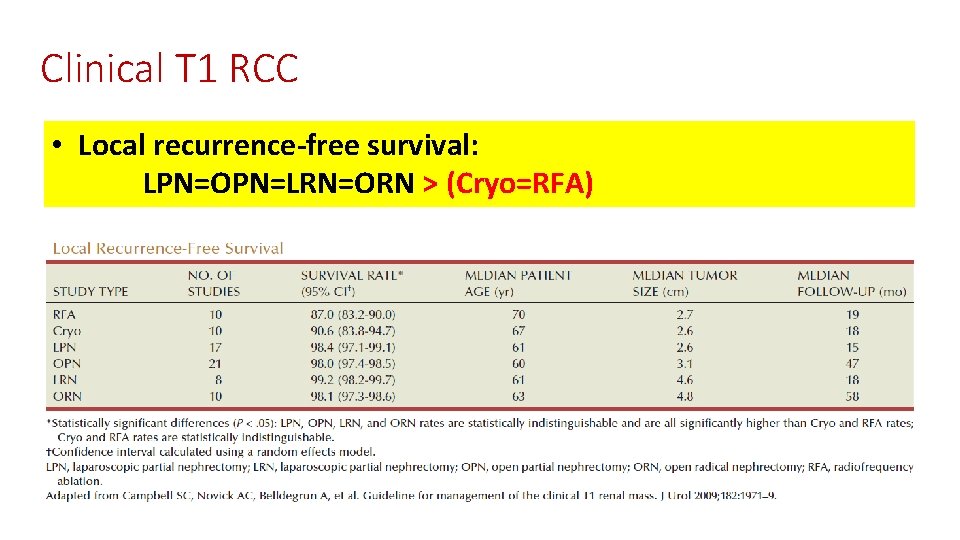
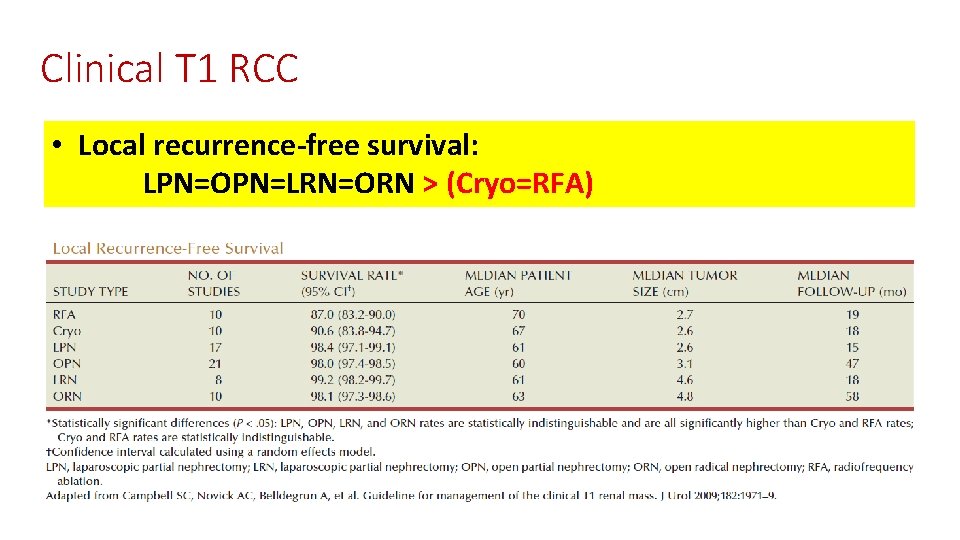
Clinical T 1 RCC • Local recurrence-free survival: LPN=OPN=LRN=ORN > (Cryo=RFA)
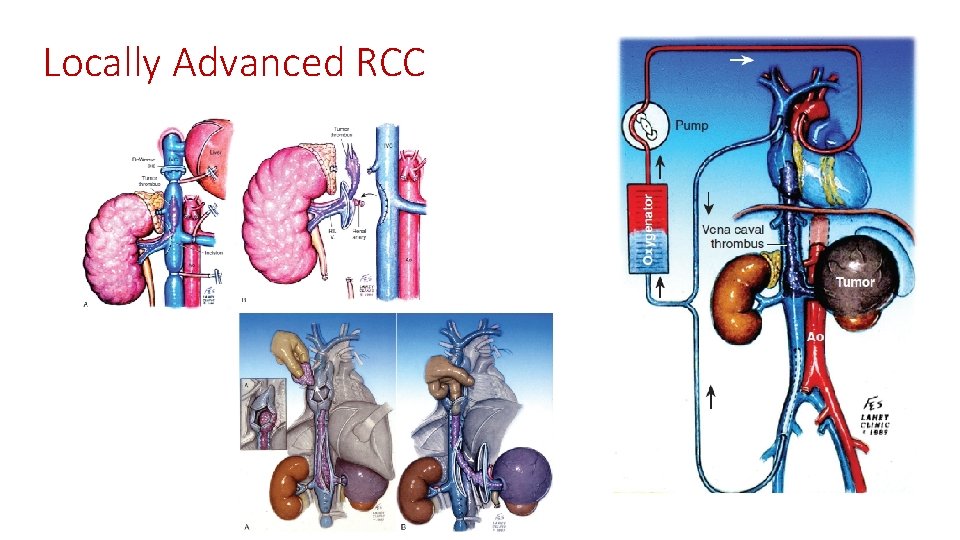
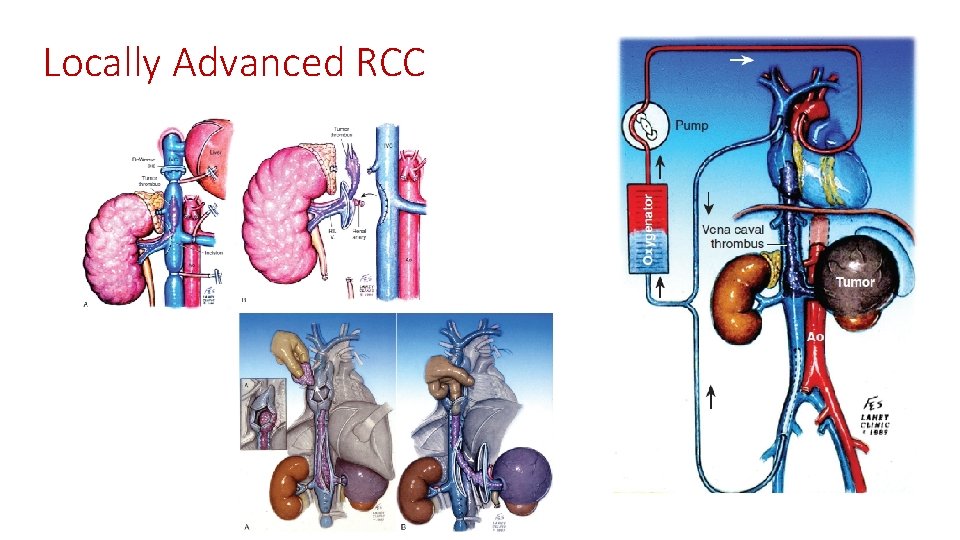
Locally Advanced RCC
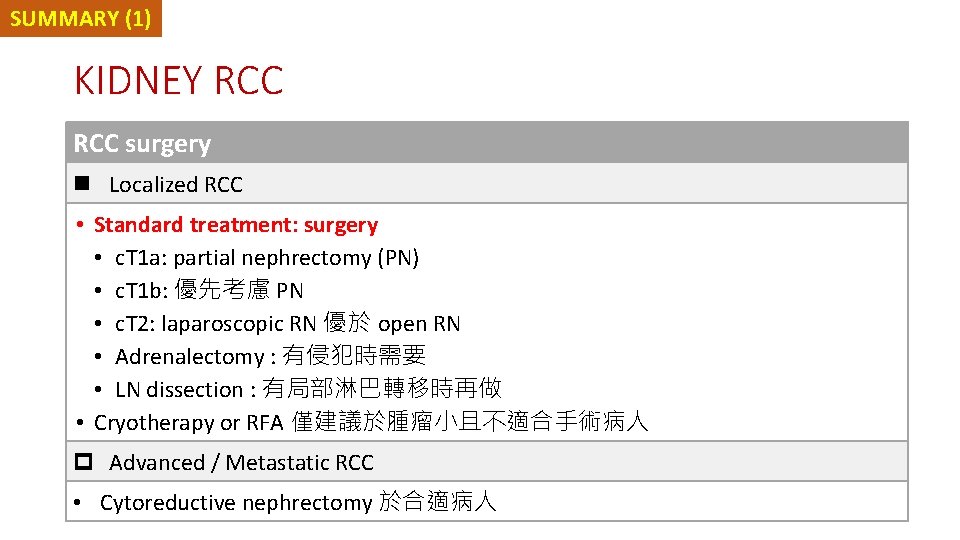
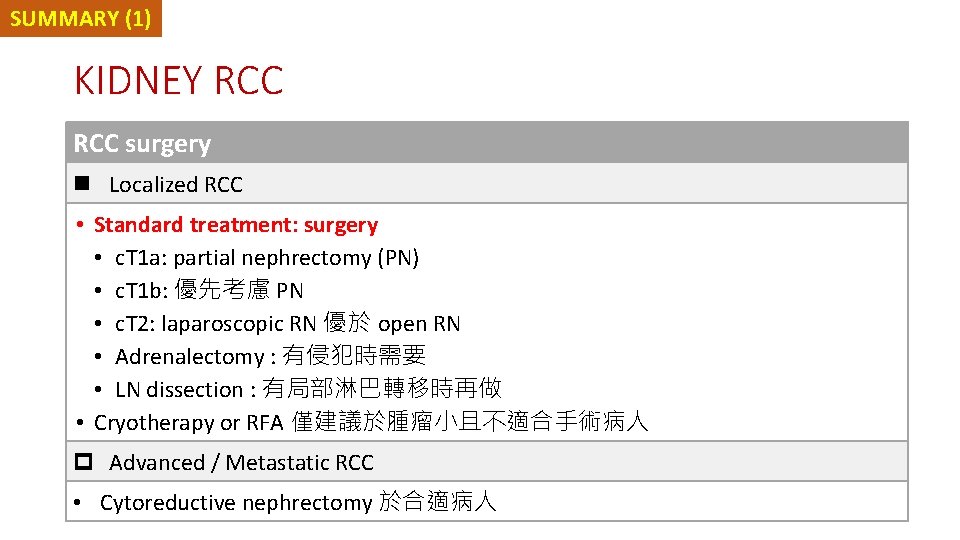
SUMMARY (1) KIDNEY RCC surgery n Localized RCC • Standard treatment: surgery • c. T 1 a: partial nephrectomy (PN) • c. T 1 b: 優先考慮 PN • c. T 2: laparoscopic RN 優於 open RN • Adrenalectomy : 有侵犯時需要 • LN dissection : 有局部淋巴轉移時再做 • Cryotherapy or RFA 僅建議於腫瘤小且不適合手術病人 p Advanced / Metastatic RCC • Cytoreductive nephrectomy 於合適病人
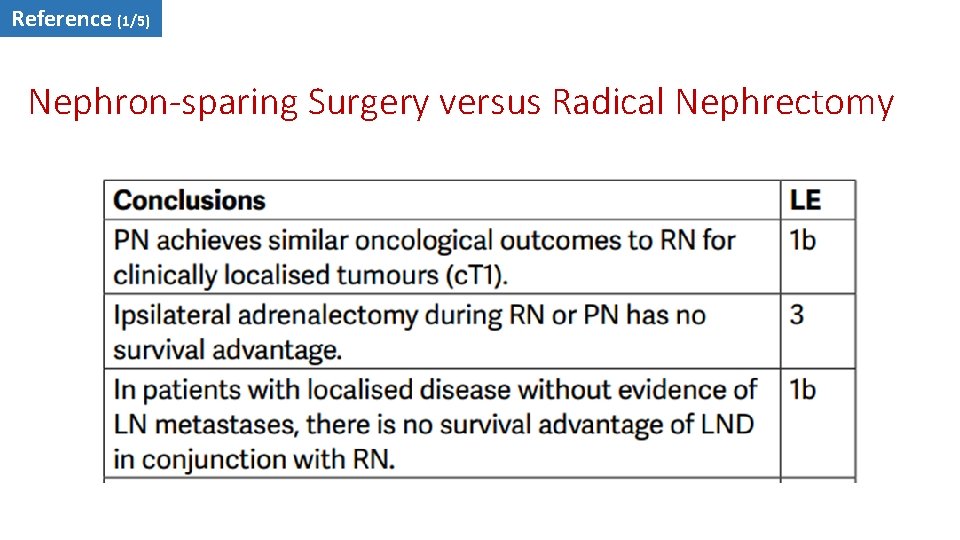
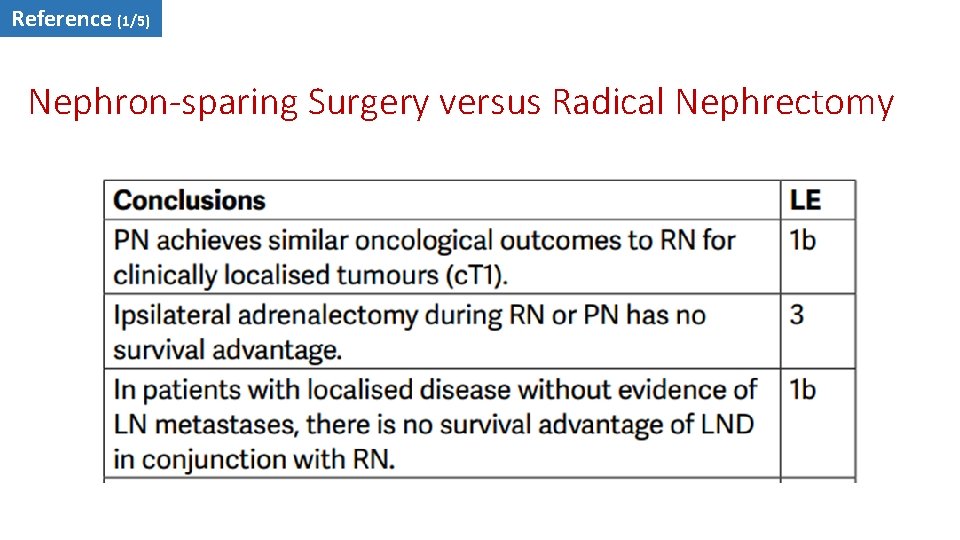
Reference (1/5) Nephron-sparing Surgery versus Radical Nephrectomy
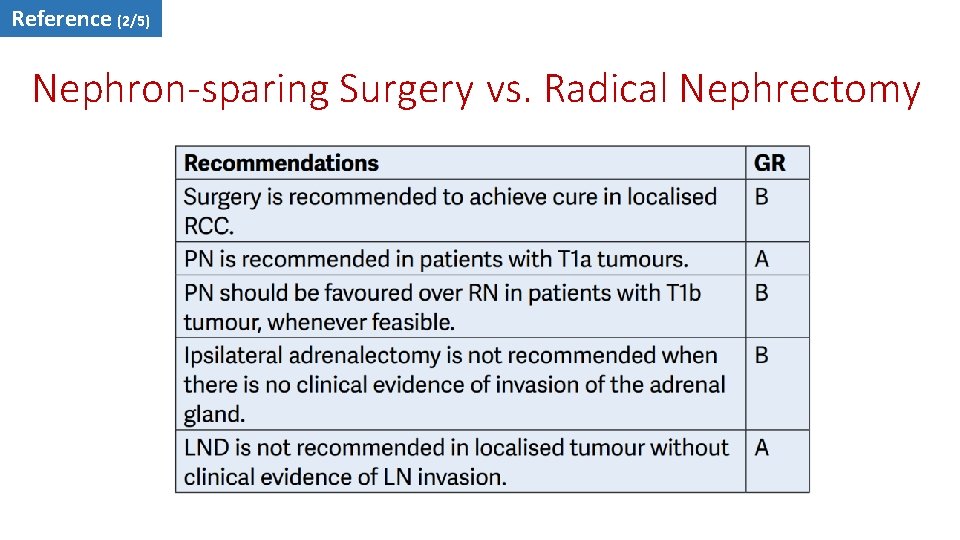
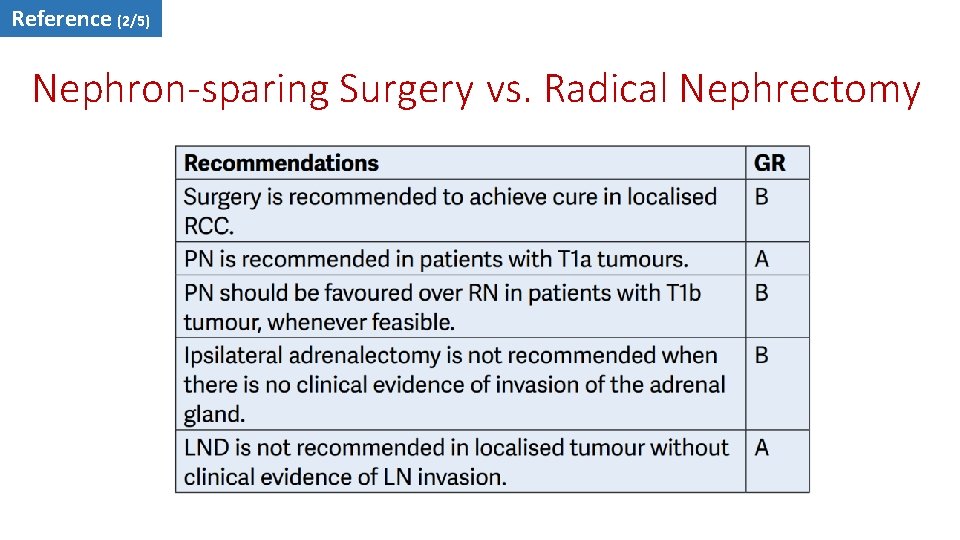
Reference (2/5) Nephron-sparing Surgery vs. Radical Nephrectomy
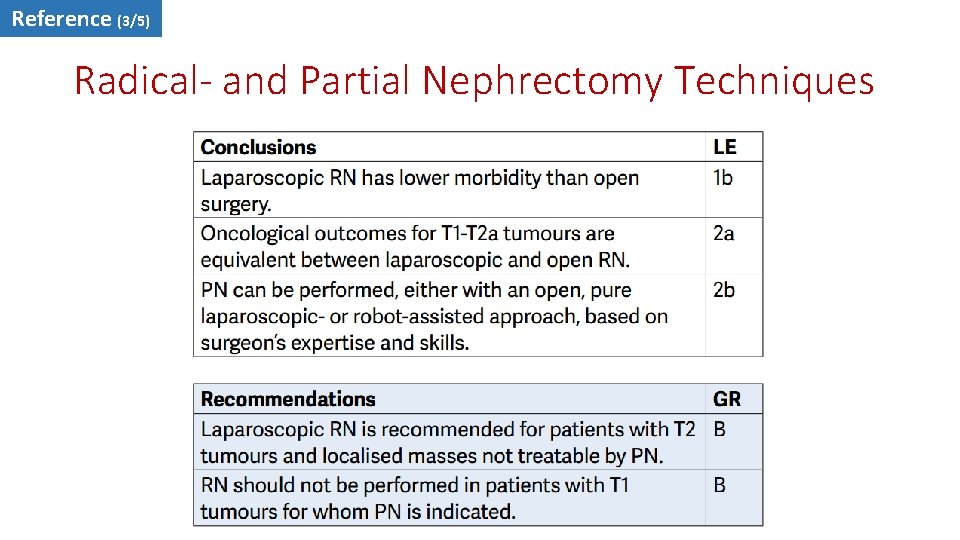
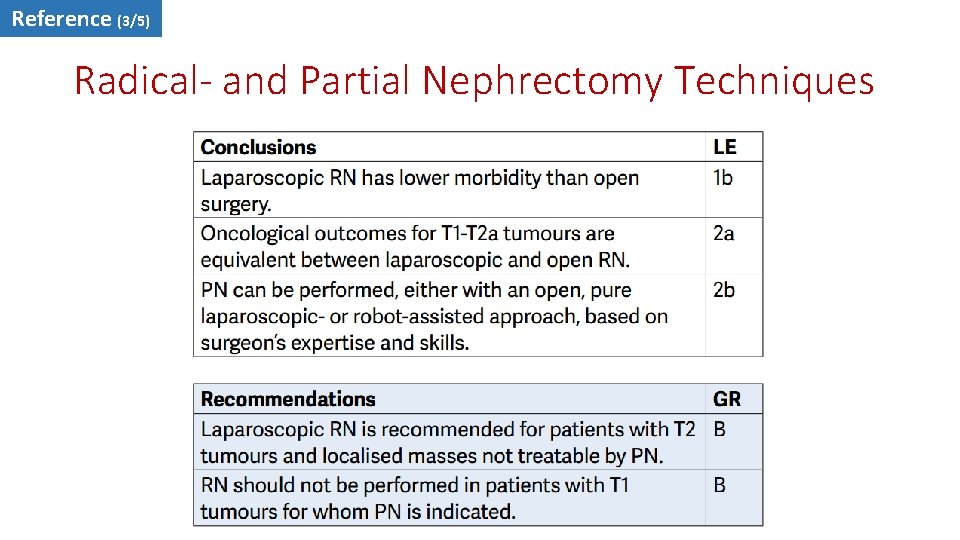
Reference (3/5) Radical- and Partial Nephrectomy Techniques
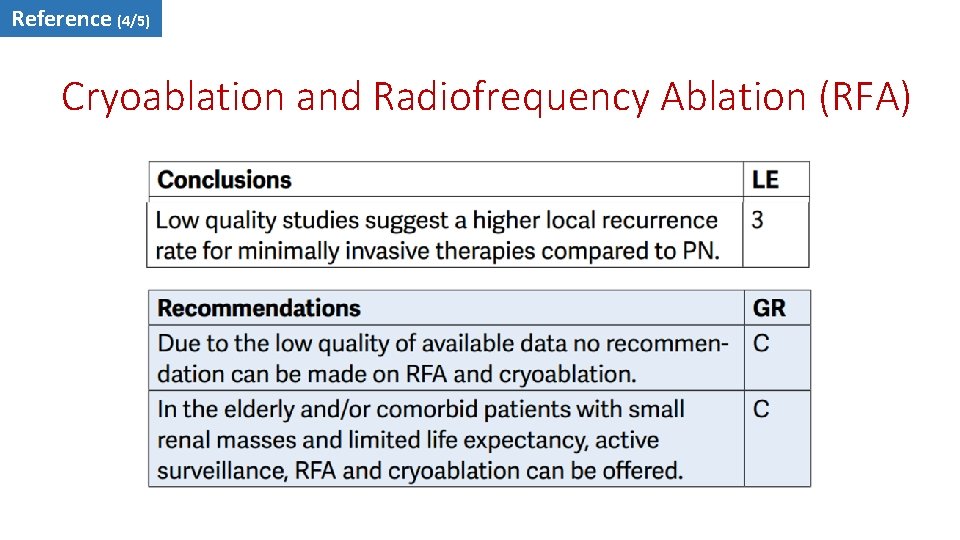
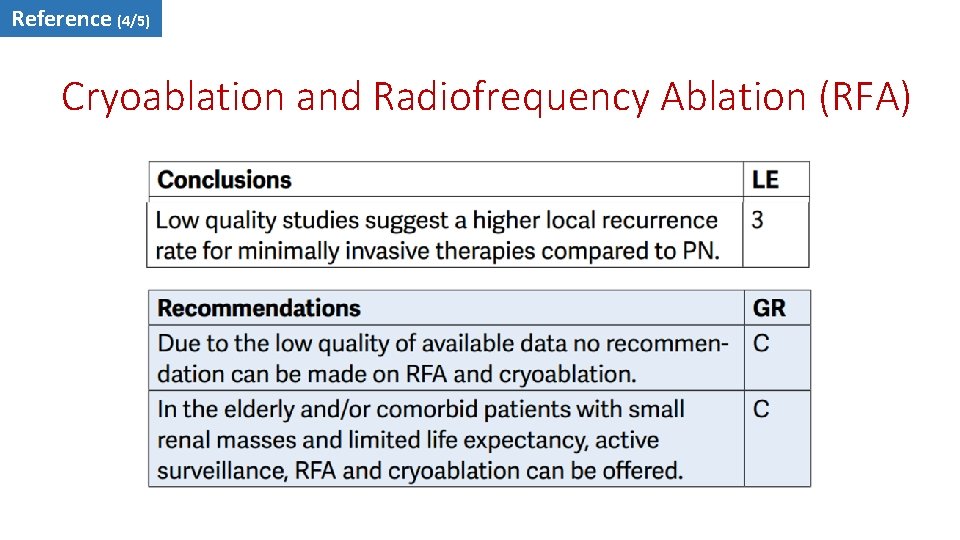
Reference (4/5) Cryoablation and Radiofrequency Ablation (RFA)
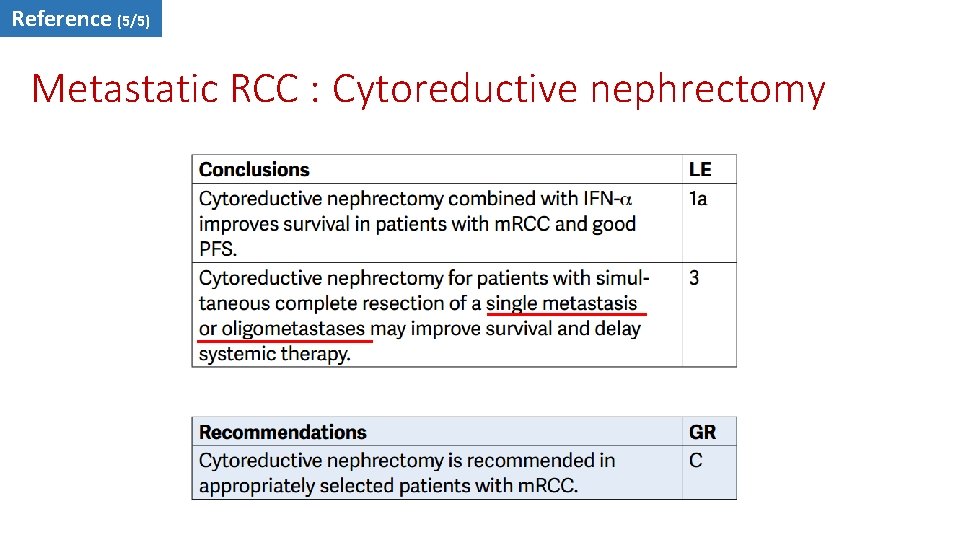
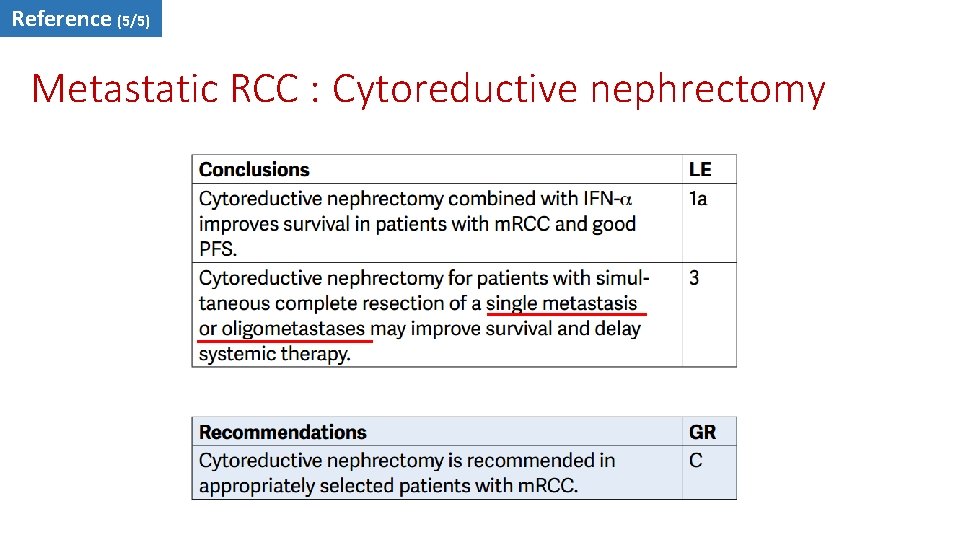
Reference (5/5) Metastatic RCC : Cytoreductive nephrectomy
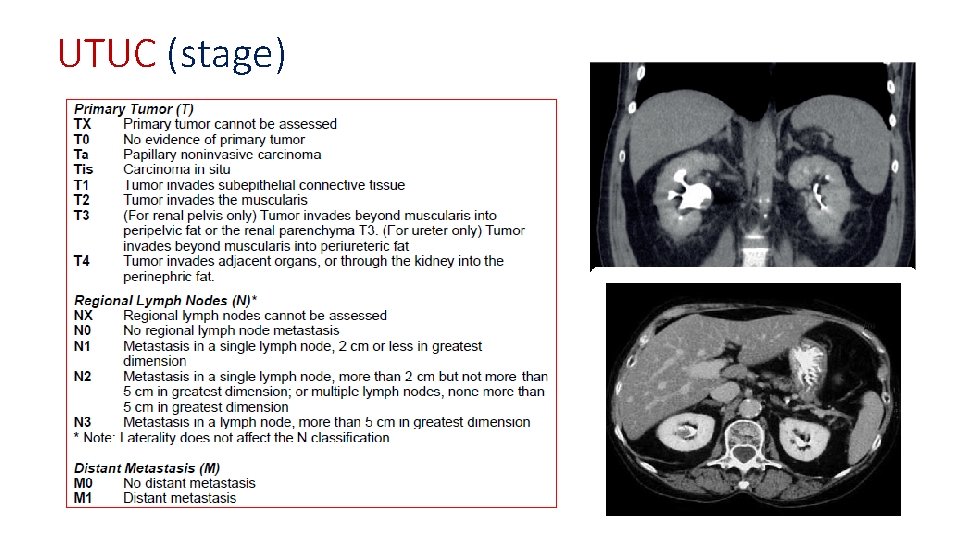
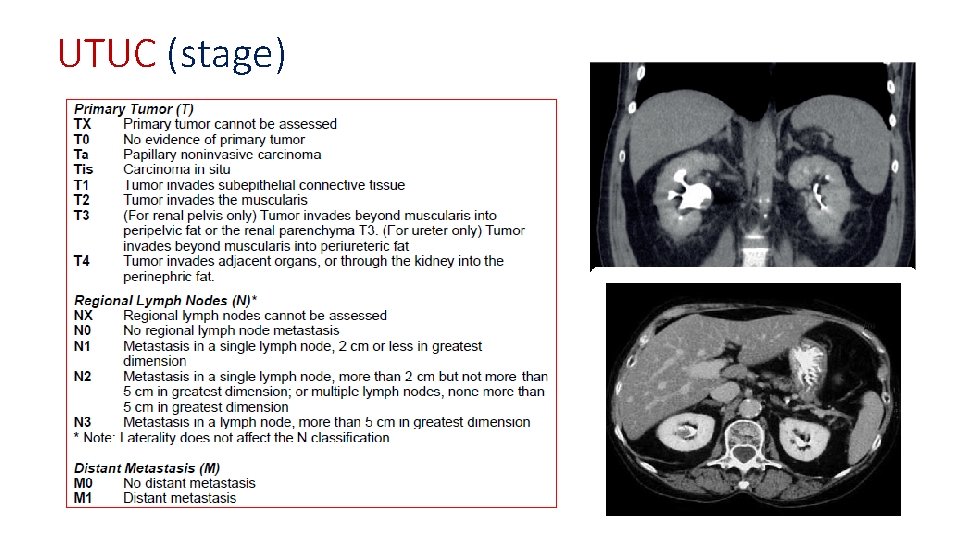
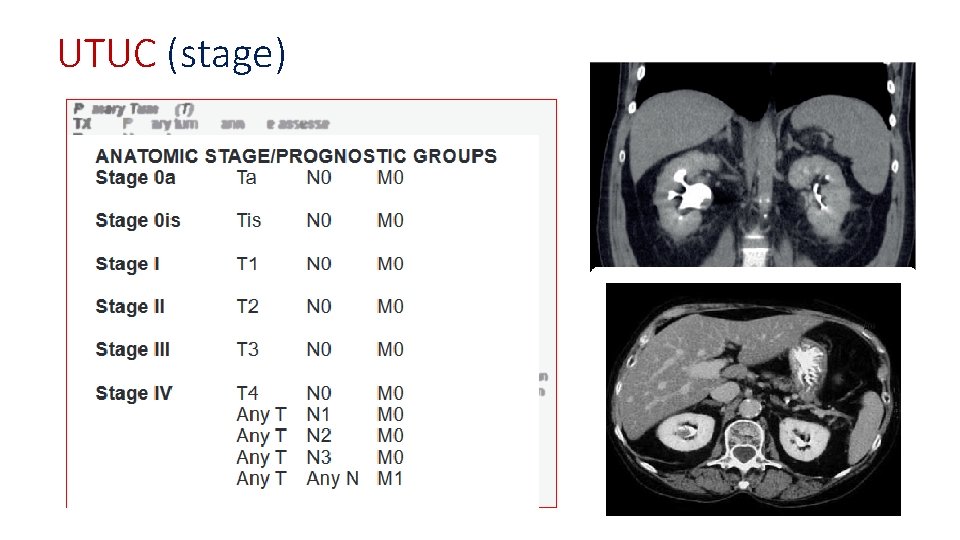
UTUC (stage)
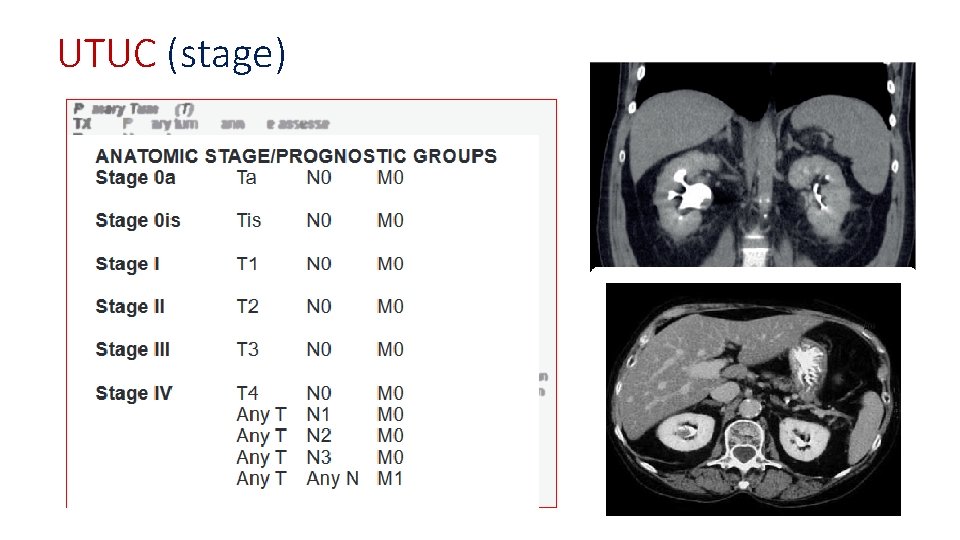
UTUC (stage)
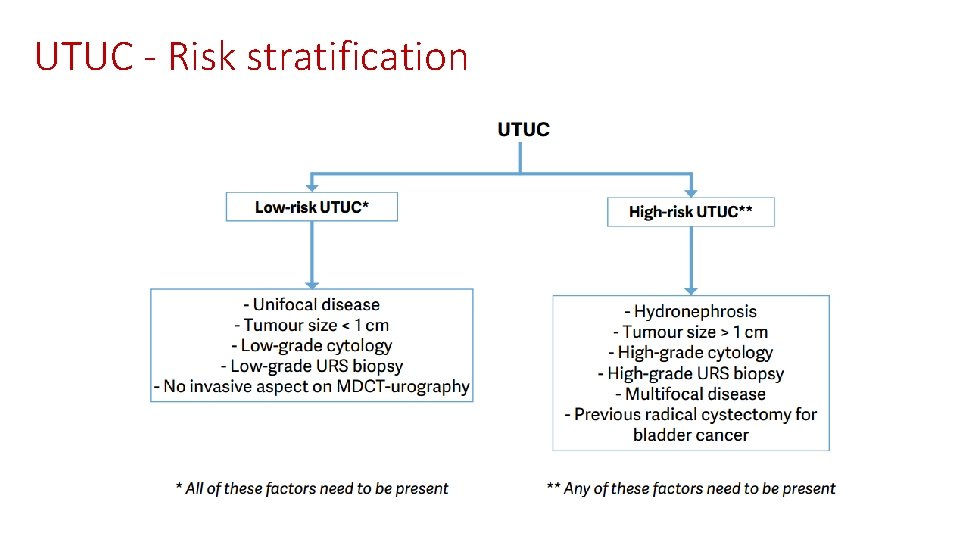
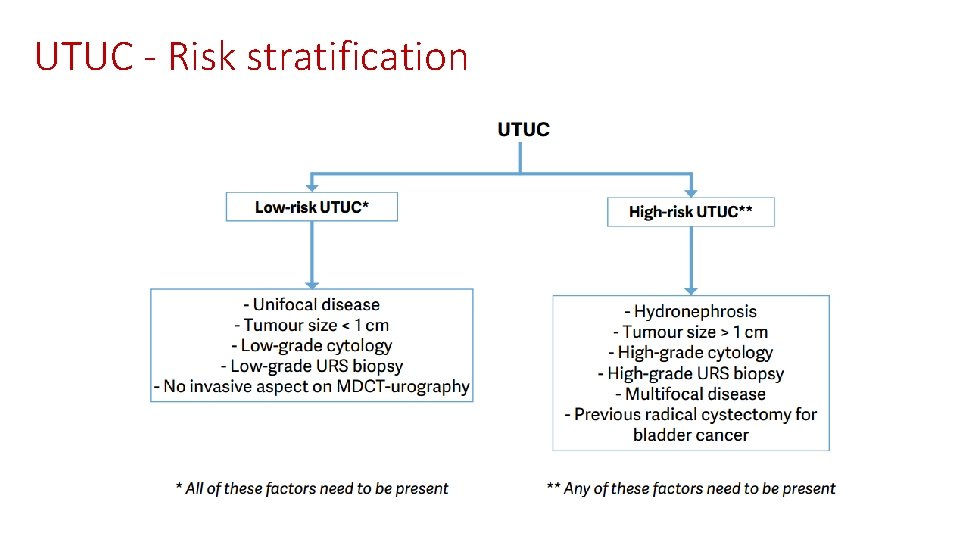
UTUC - Risk stratification
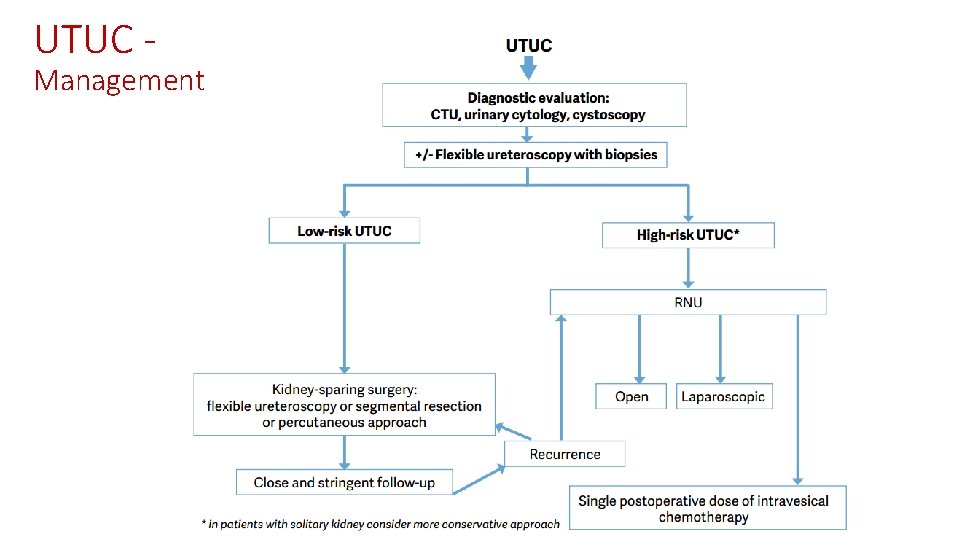
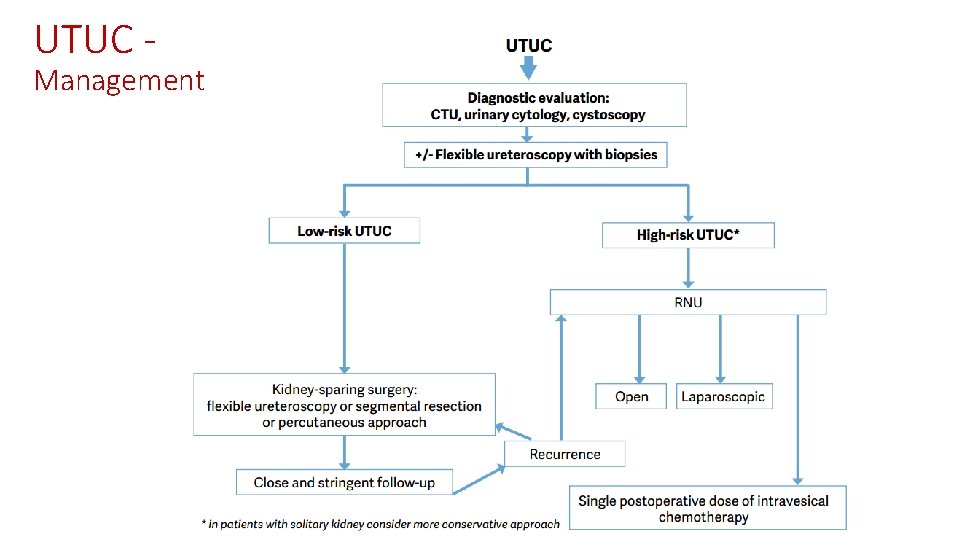
UTUC - Management
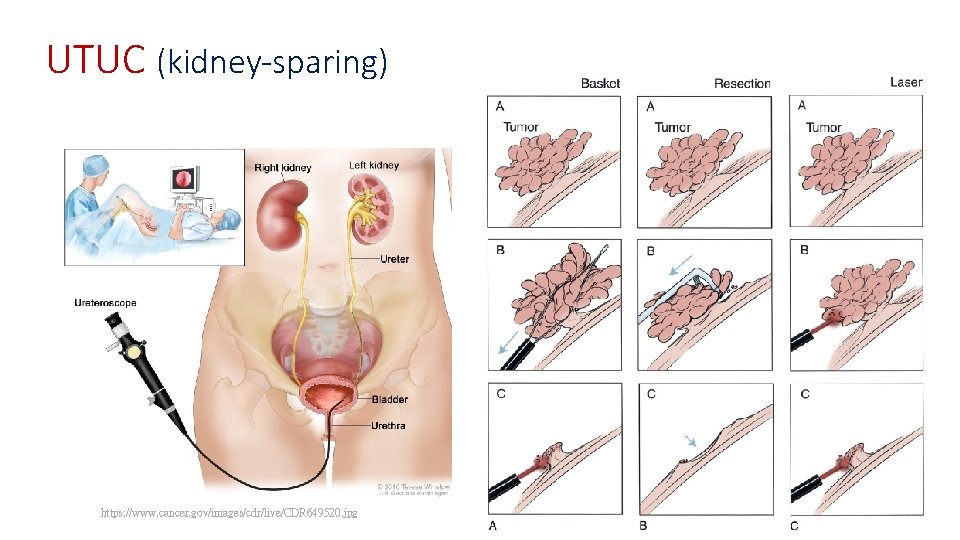
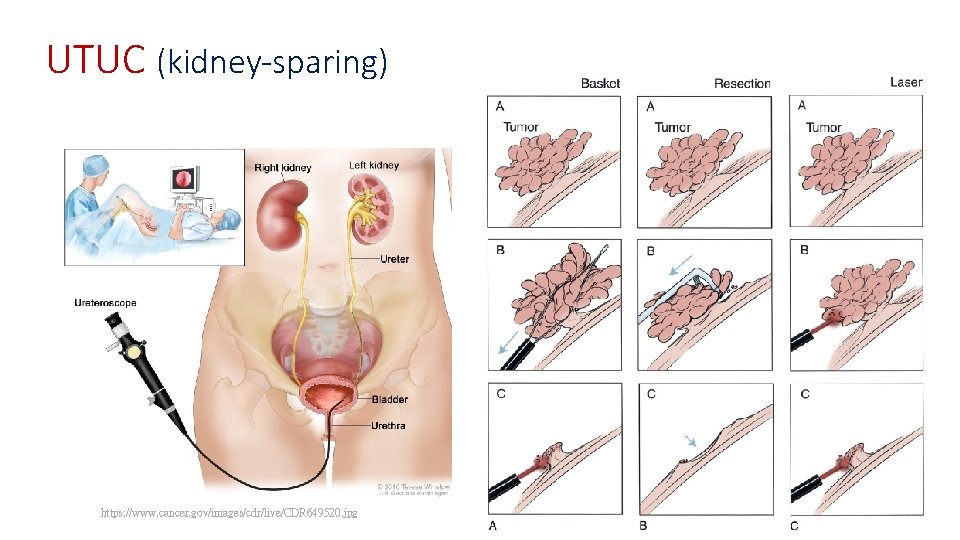
UTUC (kidney-sparing) https: //www. cancer. gov/images/cdr/live/CDR 649520. jpg
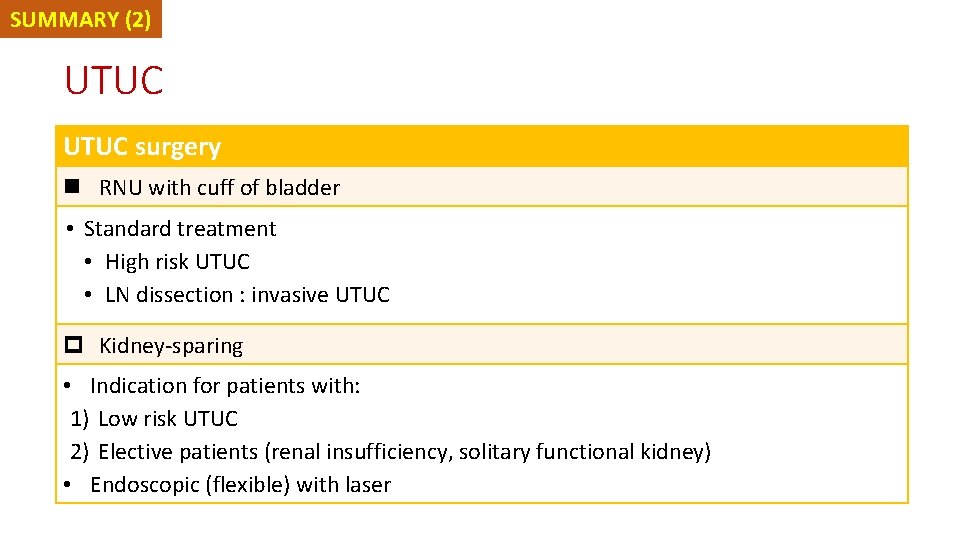
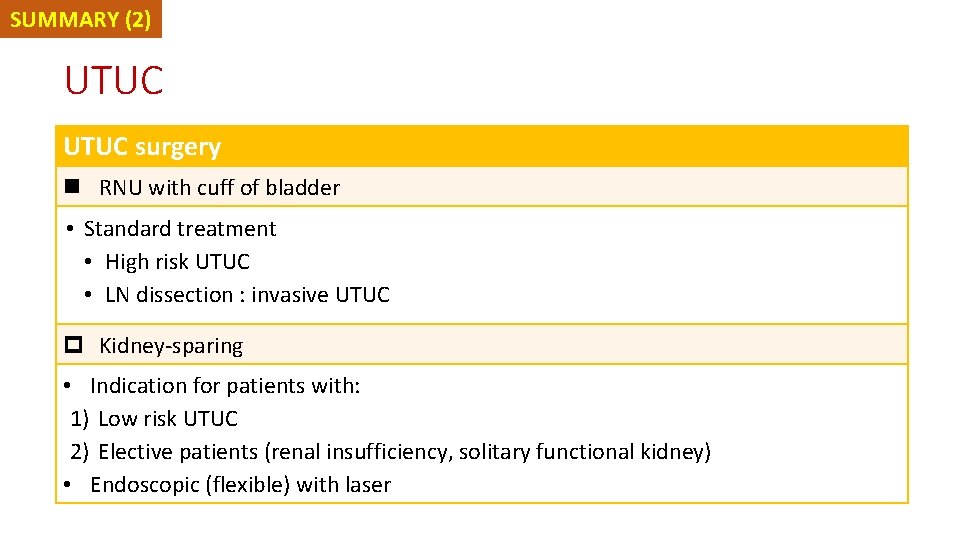
SUMMARY (2) UTUC surgery n RNU with cuff of bladder • Standard treatment • High risk UTUC • LN dissection : invasive UTUC p Kidney-sparing • Indication for patients with: 1) Low risk UTUC 2) Elective patients (renal insufficiency, solitary functional kidney) • Endoscopic (flexible) with laser
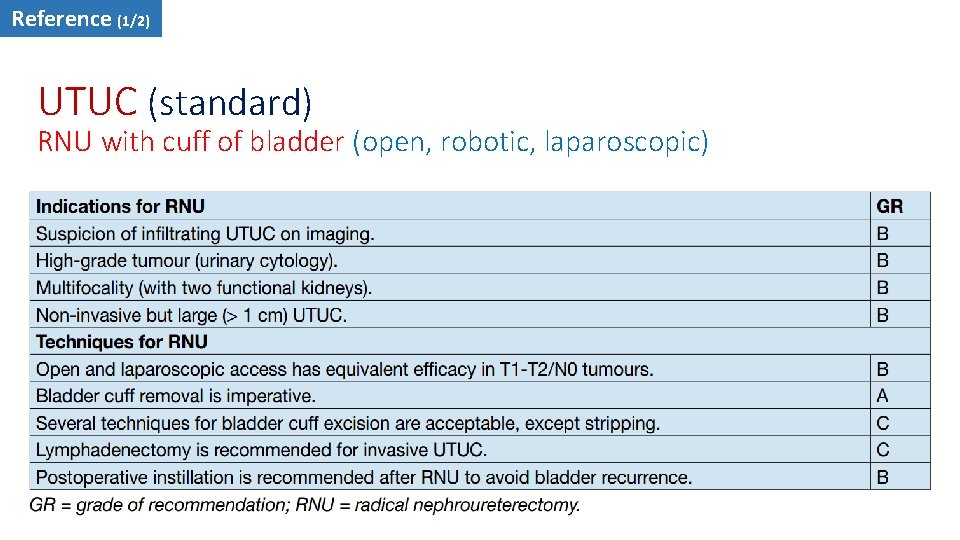
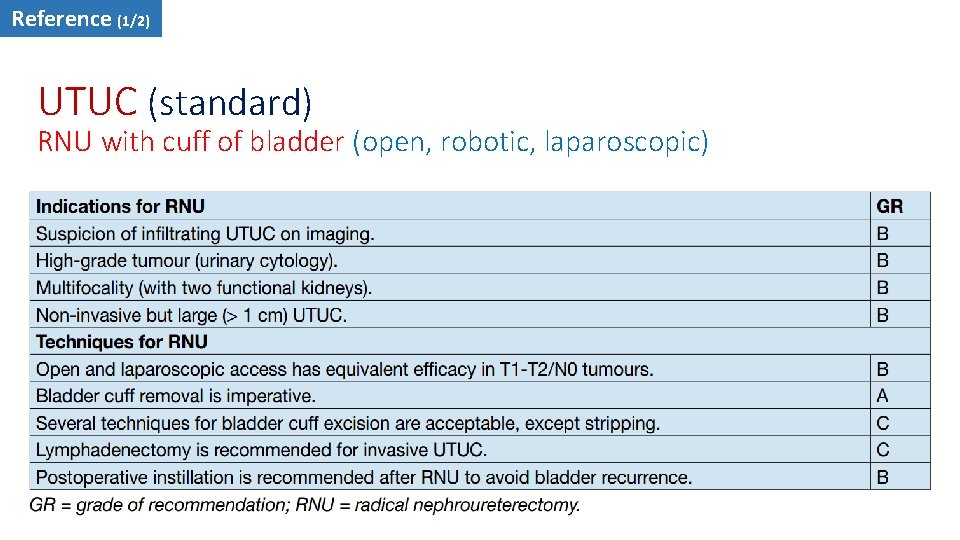
Reference (1/2) UTUC (standard) RNU with cuff of bladder (open, robotic, laparoscopic)
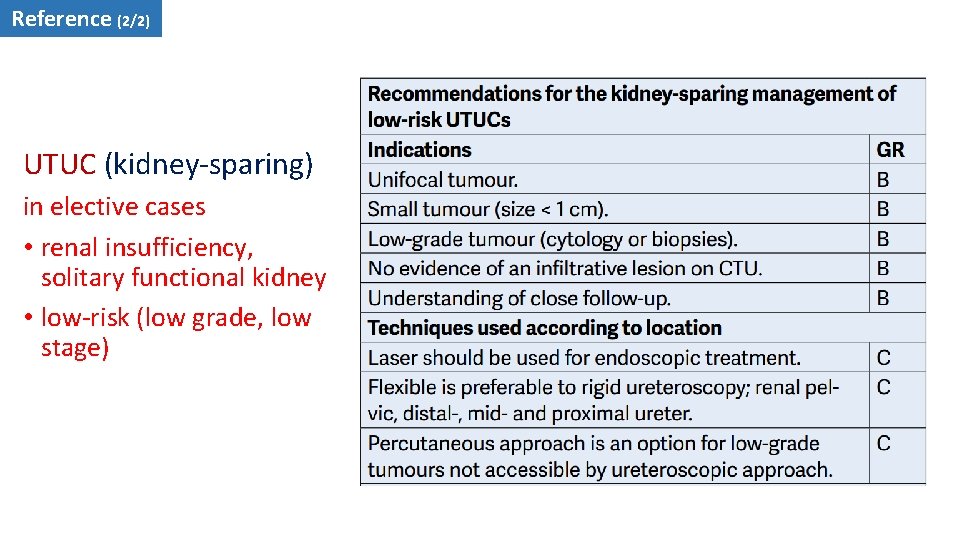
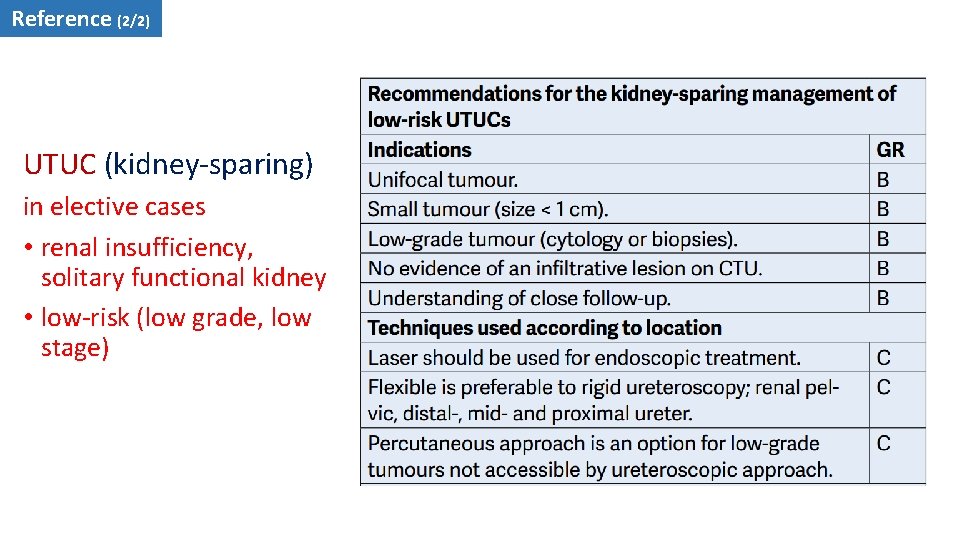
Reference (2/2) UTUC (kidney-sparing) in elective cases • renal insufficiency, solitary functional kidney • low-risk (low grade, low stage)
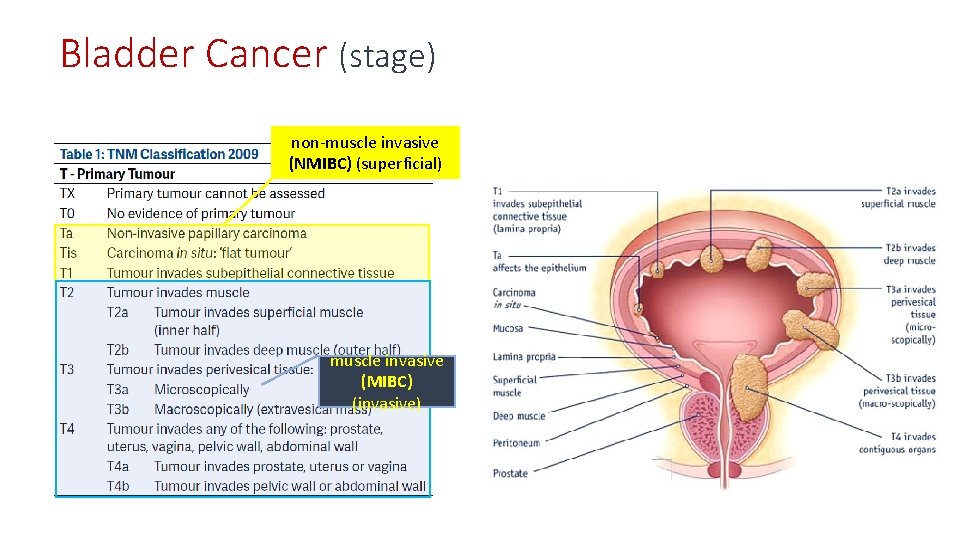
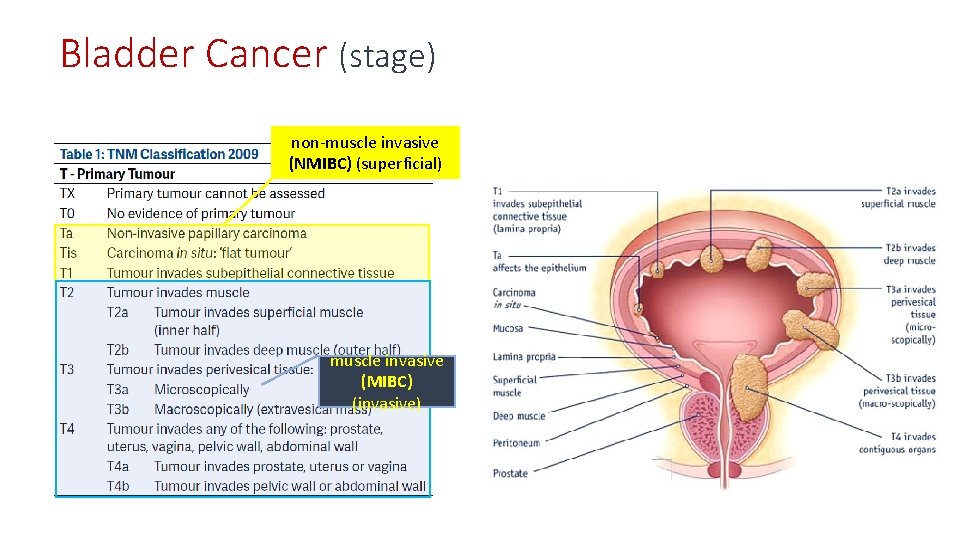
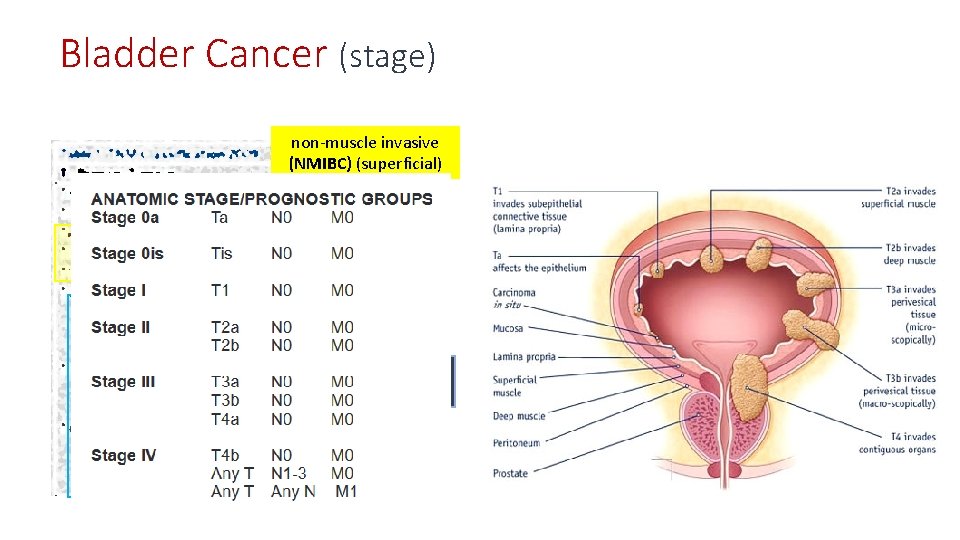
Bladder Cancer (stage) non-muscle invasive (NMIBC) (superficial) muscle invasive (MIBC) (invasive)
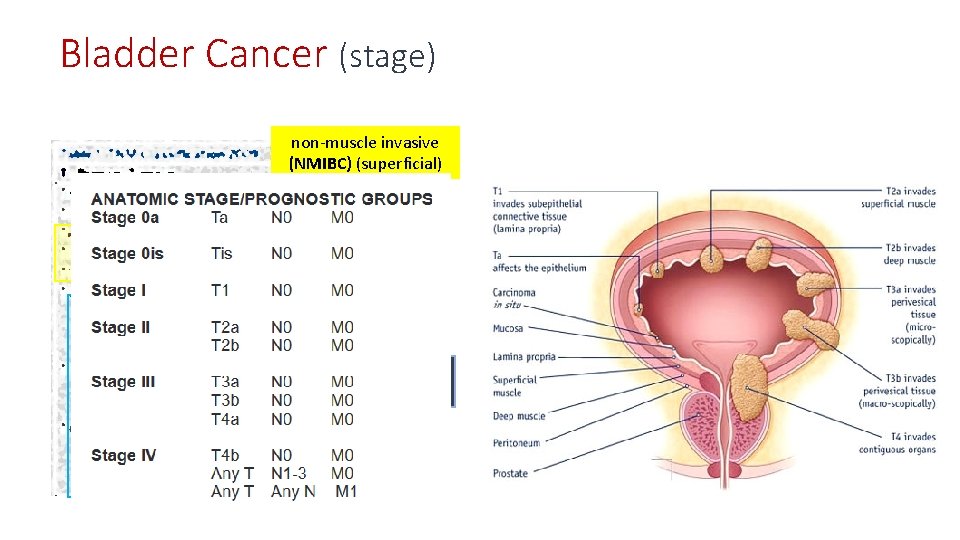
Bladder Cancer (stage) non-muscle invasive (NMIBC) (superficial) muscle invasive (MIBC) (invasive)
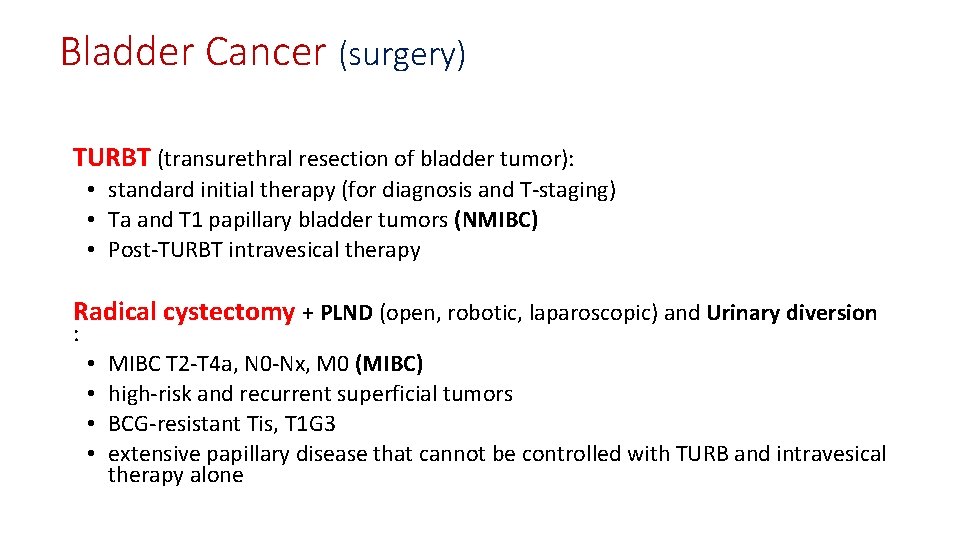
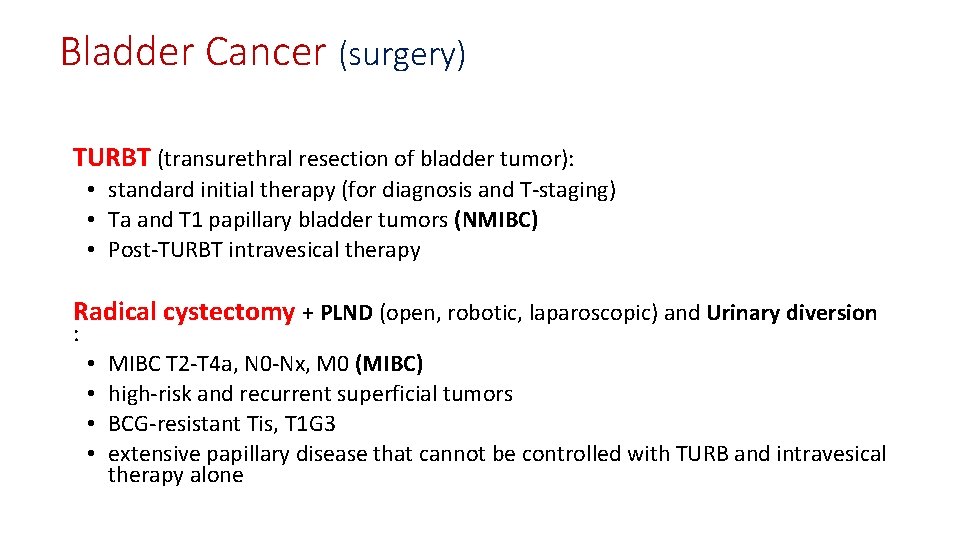
Bladder Cancer (surgery) TURBT (transurethral resection of bladder tumor): • standard initial therapy (for diagnosis and T-staging) • Ta and T 1 papillary bladder tumors (NMIBC) • Post-TURBT intravesical therapy Radical cystectomy + PLND (open, robotic, laparoscopic) and Urinary diversion : • • MIBC T 2 -T 4 a, N 0 -Nx, M 0 (MIBC) high-risk and recurrent superficial tumors BCG-resistant Tis, T 1 G 3 extensive papillary disease that cannot be controlled with TURB and intravesical therapy alone
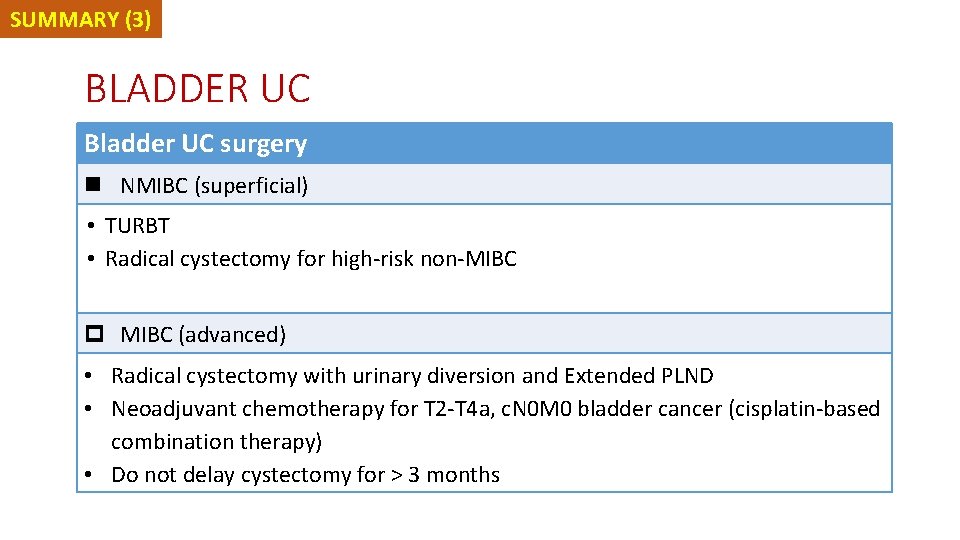
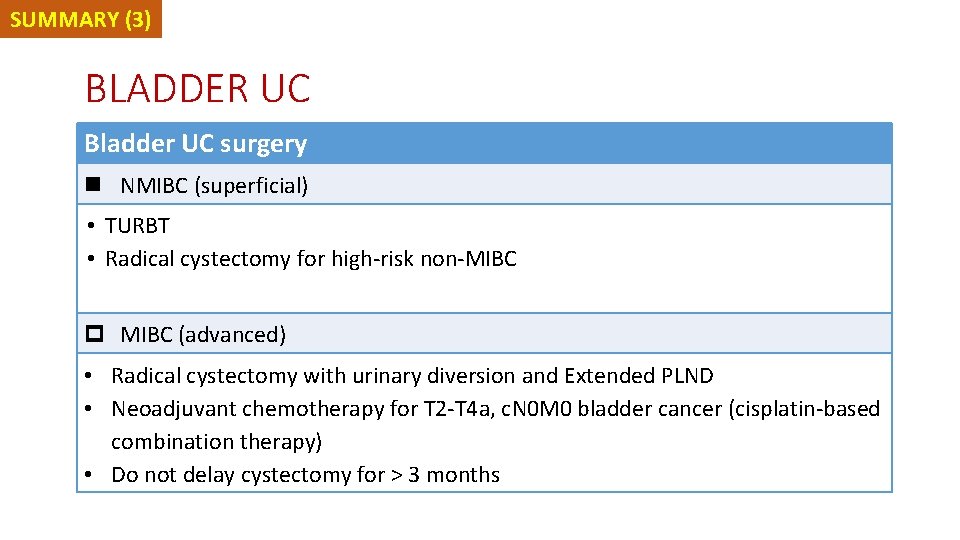
SUMMARY (3) BLADDER UC Bladder UC surgery n NMIBC (superficial) • TURBT • Radical cystectomy for high-risk non-MIBC p MIBC (advanced) • Radical cystectomy with urinary diversion and Extended PLND • Neoadjuvant chemotherapy for T 2 -T 4 a, c. N 0 M 0 bladder cancer (cisplatin-based combination therapy) • Do not delay cystectomy for > 3 months
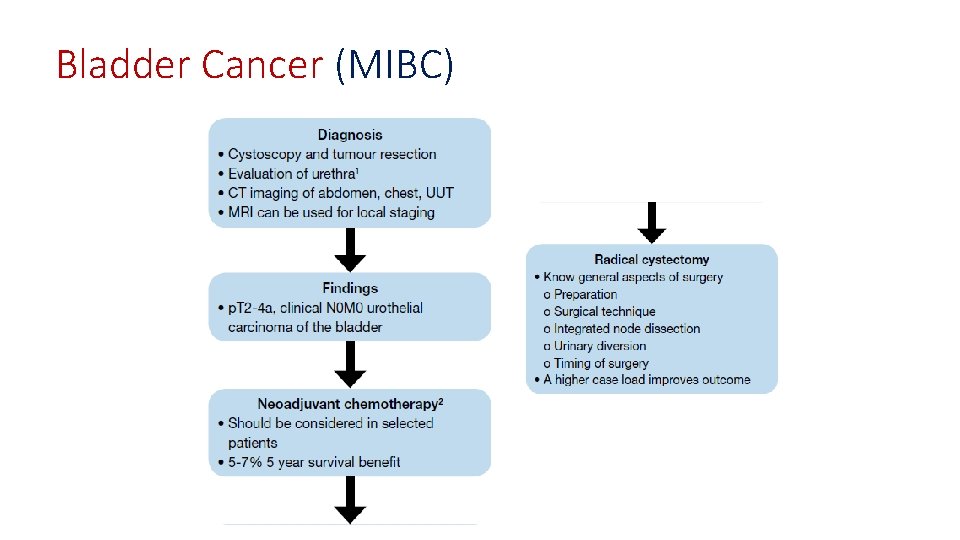
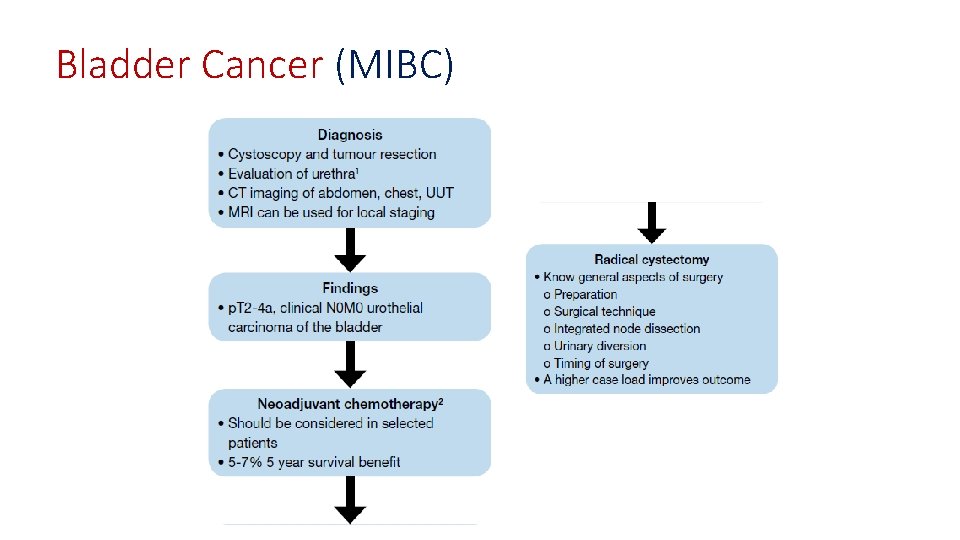
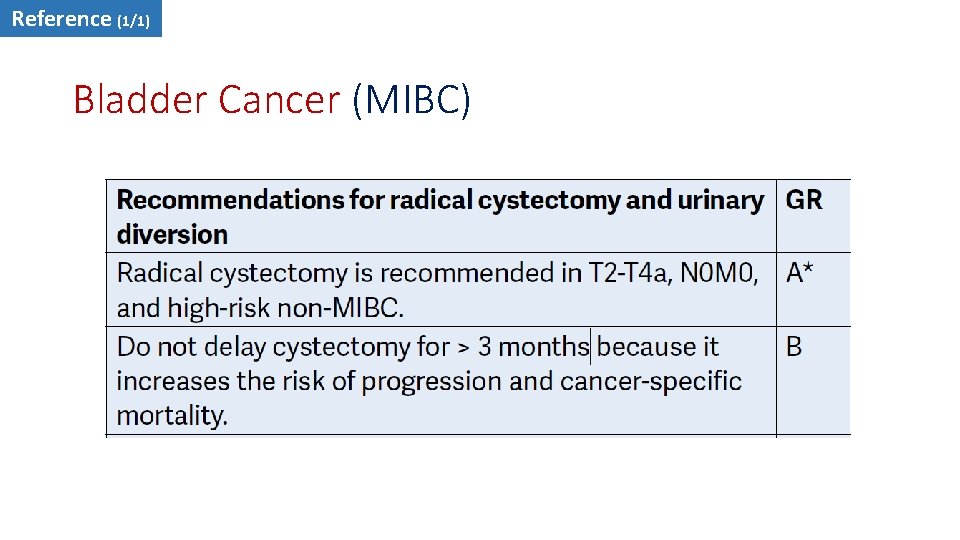
Bladder Cancer (MIBC)
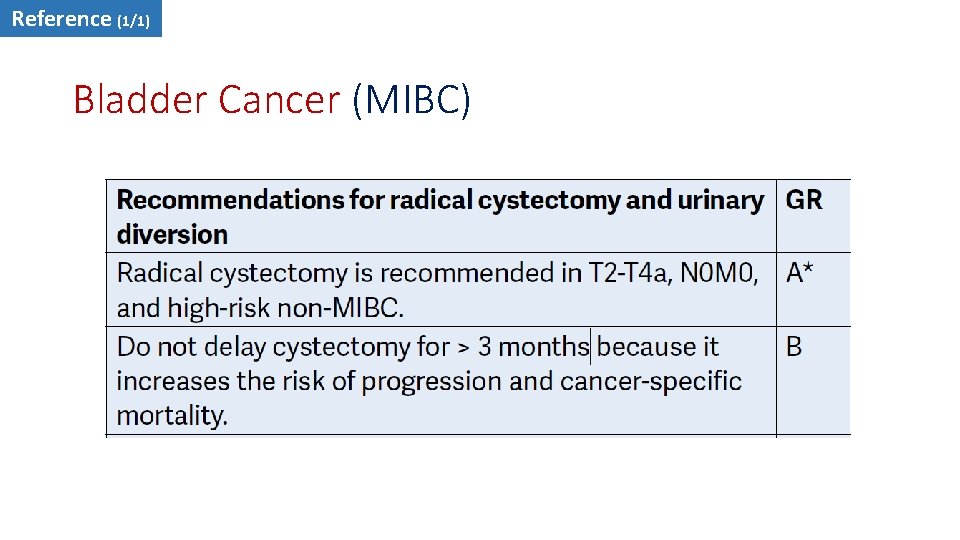
Reference (1/1) Bladder Cancer (MIBC)
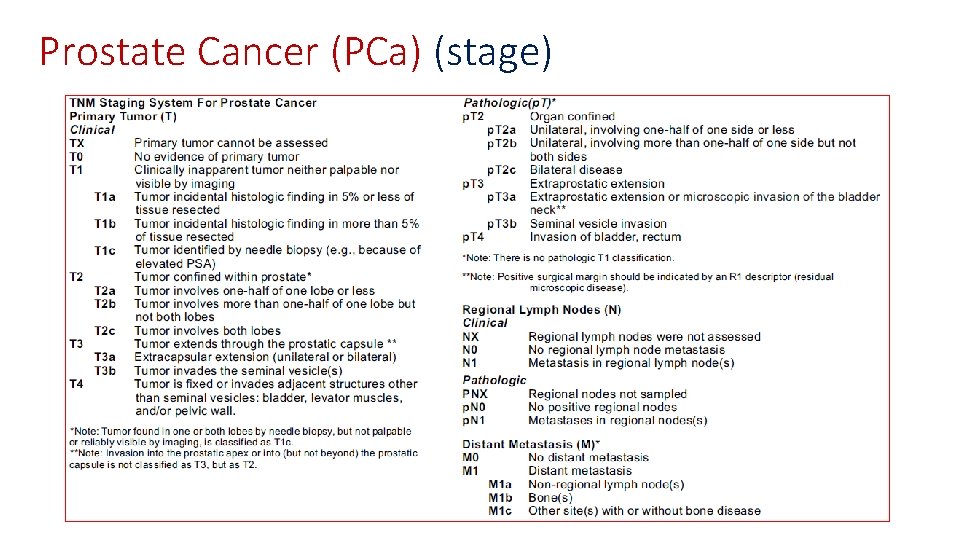
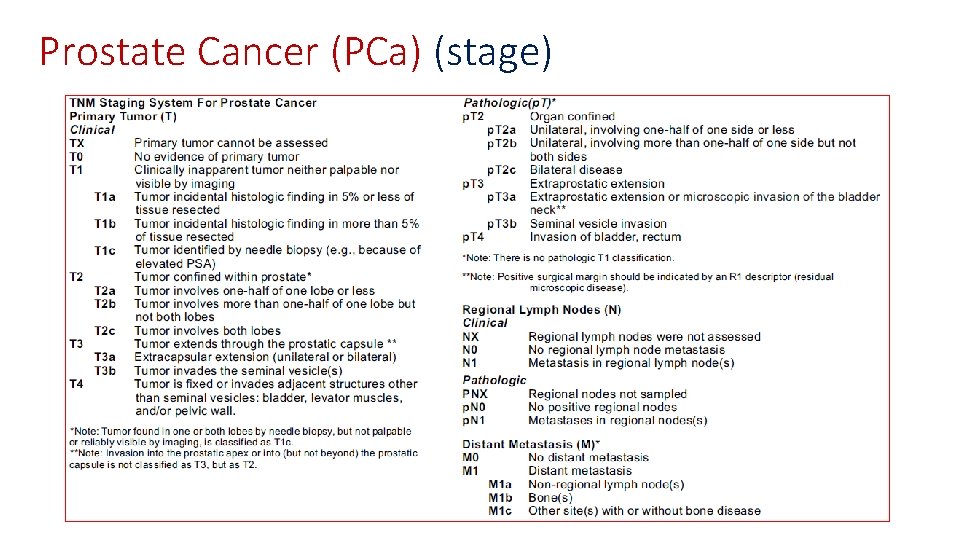
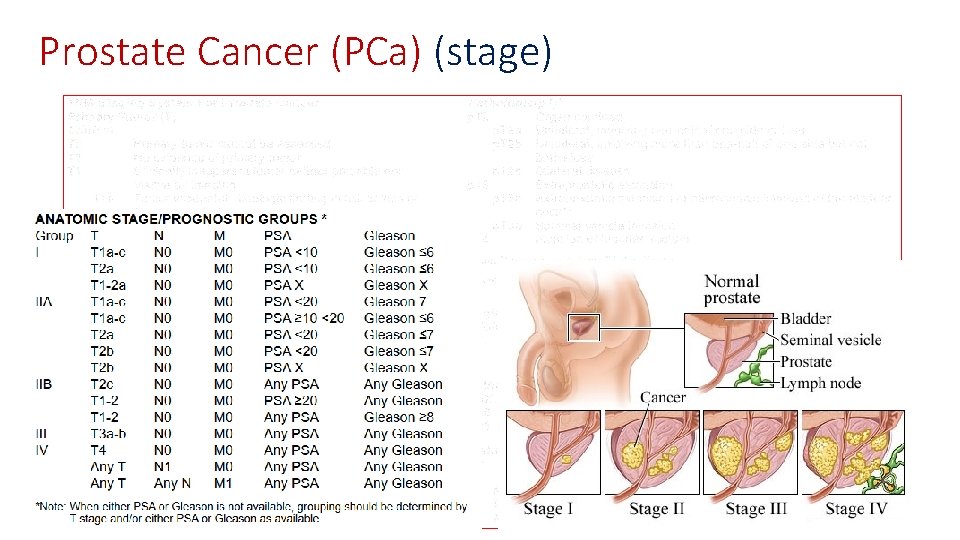
Prostate Cancer (PCa) (stage)
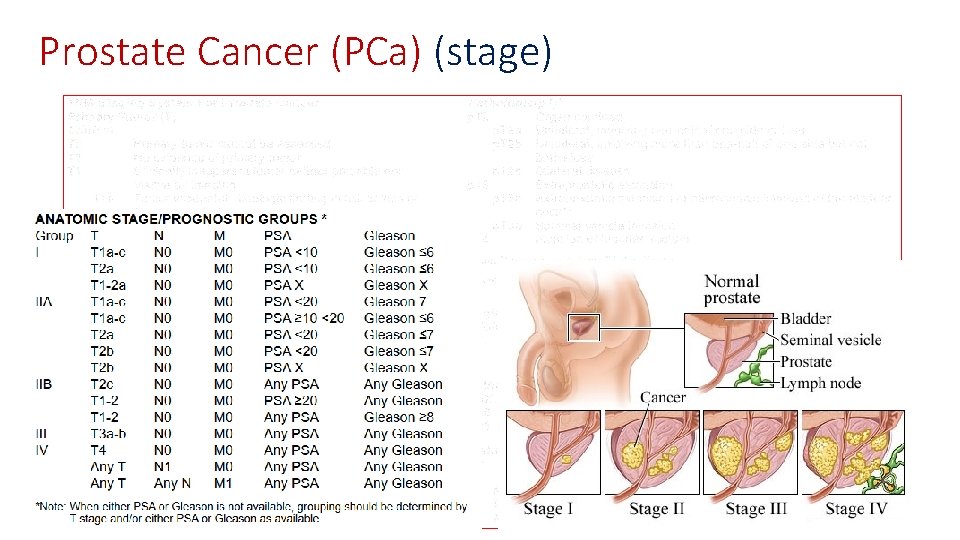
Prostate Cancer (PCa) (stage)
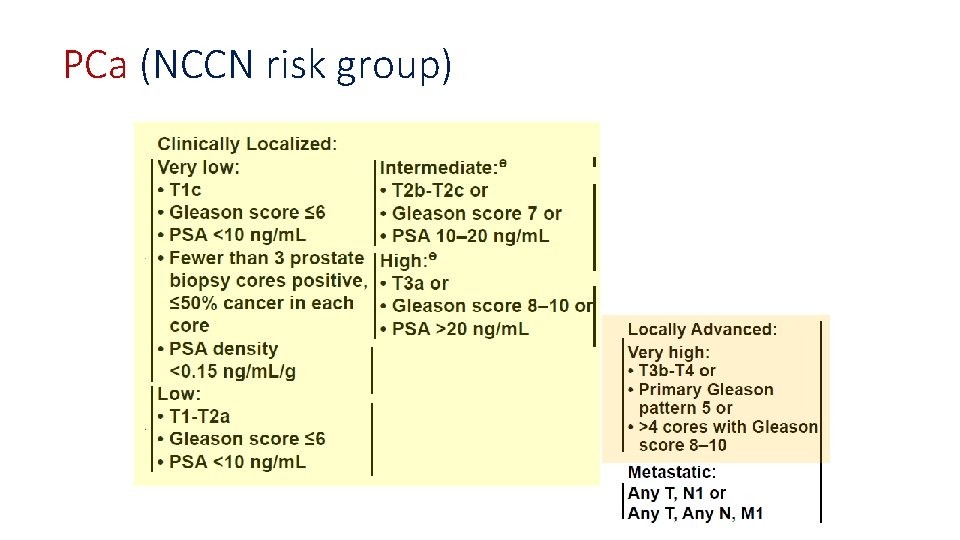
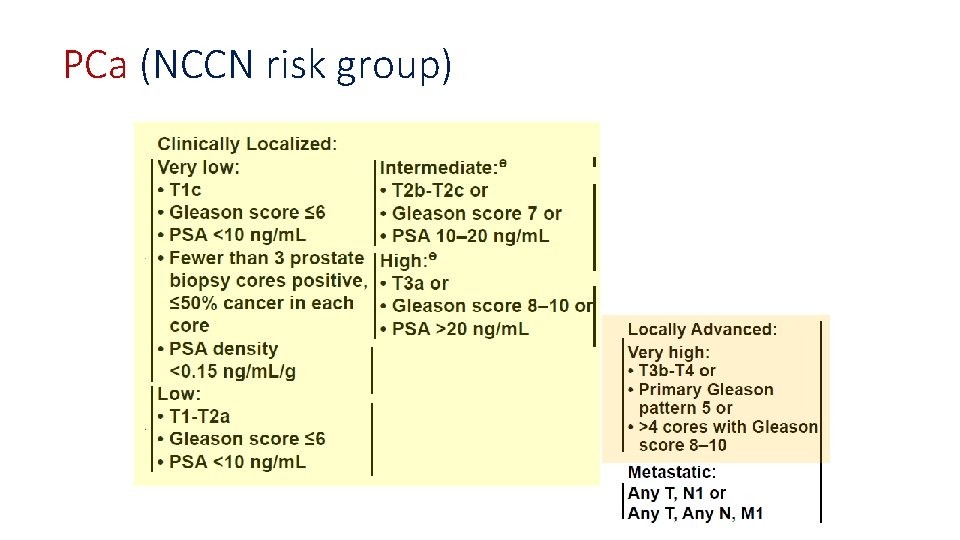
PCa (NCCN risk group)
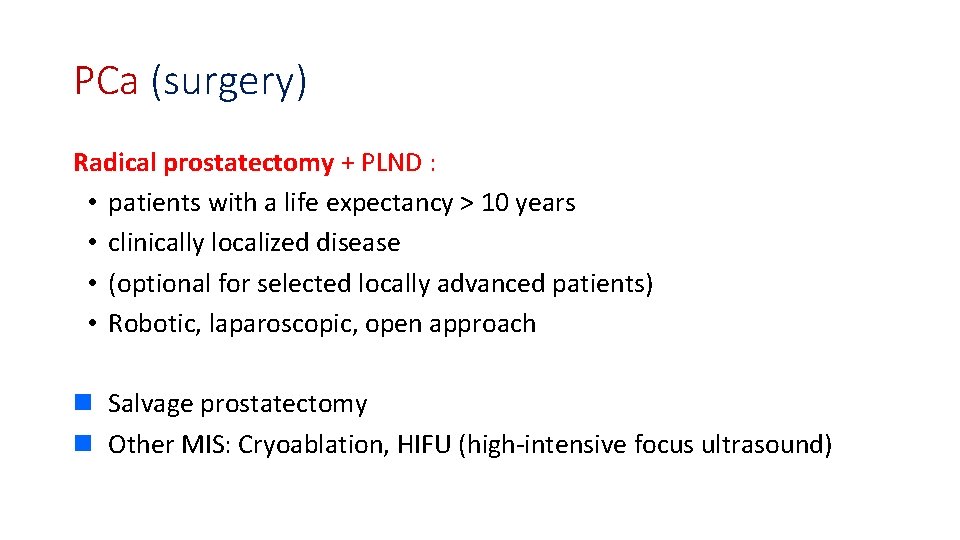
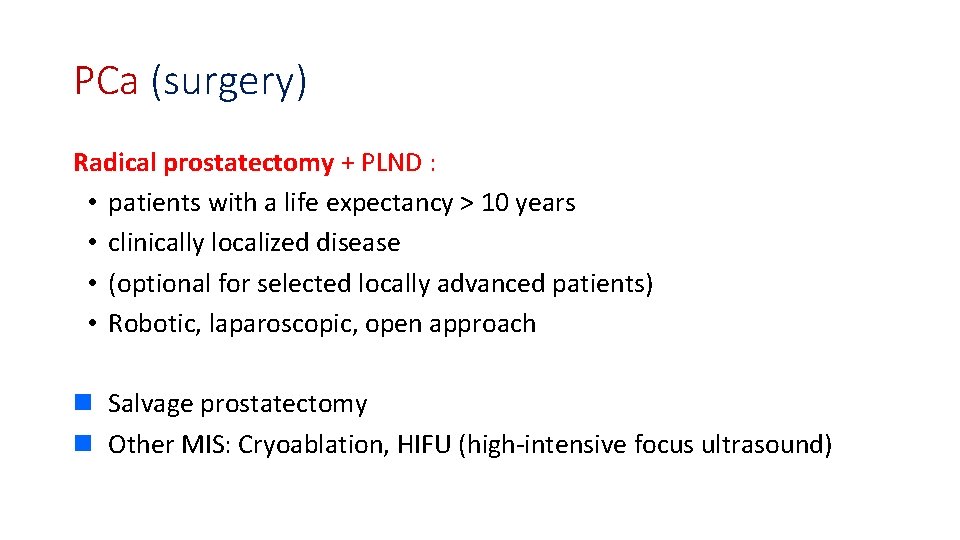
PCa (surgery) Radical prostatectomy + PLND : • patients with a life expectancy > 10 years • clinically localized disease • (optional for selected locally advanced patients) • Robotic, laparoscopic, open approach n Salvage prostatectomy n Other MIS: Cryoablation, HIFU (high-intensive focus ultrasound)
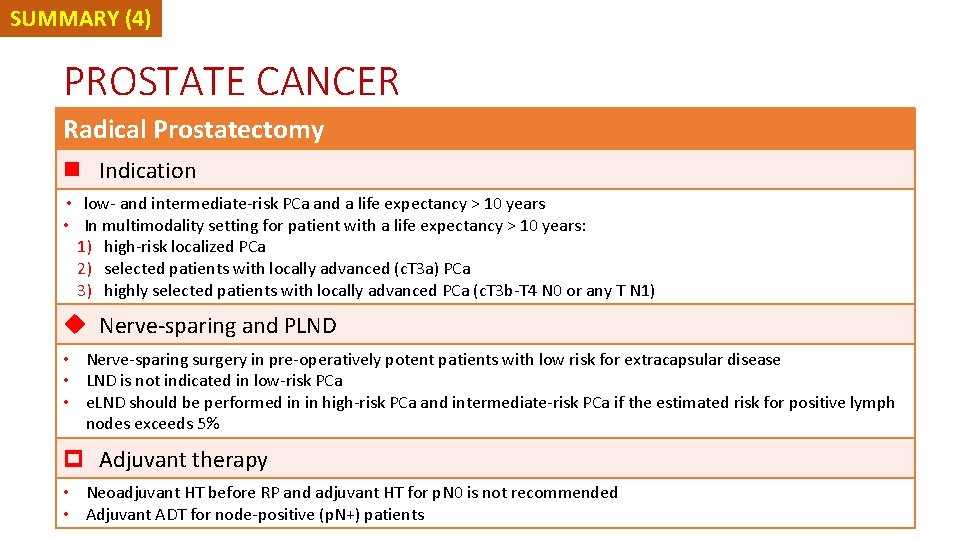
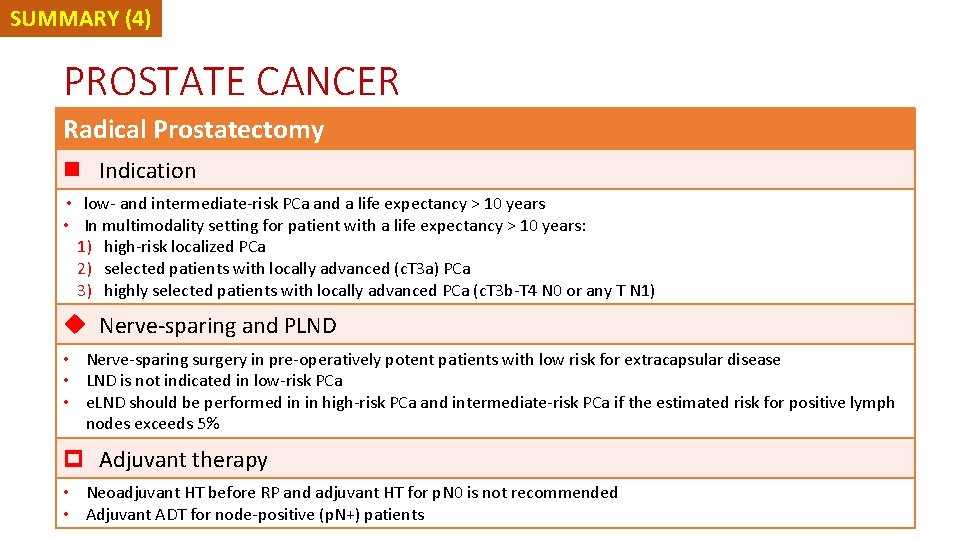
SUMMARY (4) PROSTATE CANCER Radical Prostatectomy n Indication • low- and intermediate-risk PCa and a life expectancy > 10 years • In multimodality setting for patient with a life expectancy > 10 years: 1) high-risk localized PCa 2) selected patients with locally advanced (c. T 3 a) PCa 3) highly selected patients with locally advanced PCa (c. T 3 b-T 4 N 0 or any T N 1) u Nerve-sparing and PLND • Nerve-sparing surgery in pre-operatively potent patients with low risk for extracapsular disease • LND is not indicated in low-risk PCa • e. LND should be performed in in high-risk PCa and intermediate-risk PCa if the estimated risk for positive lymph nodes exceeds 5% p Adjuvant therapy • Neoadjuvant HT before RP and adjuvant HT for p. N 0 is not recommended • Adjuvant ADT for node-positive (p. N+) patients
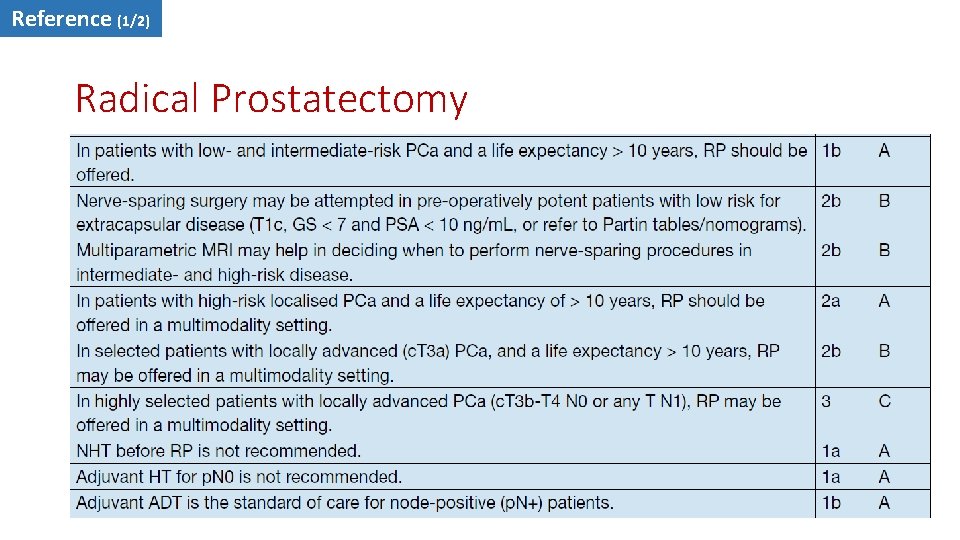
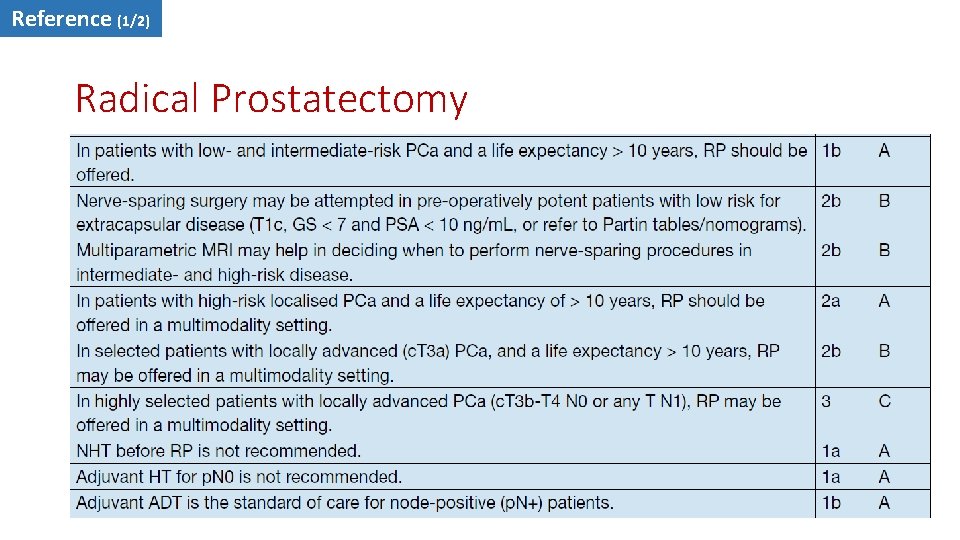
Reference (1/2) Radical Prostatectomy
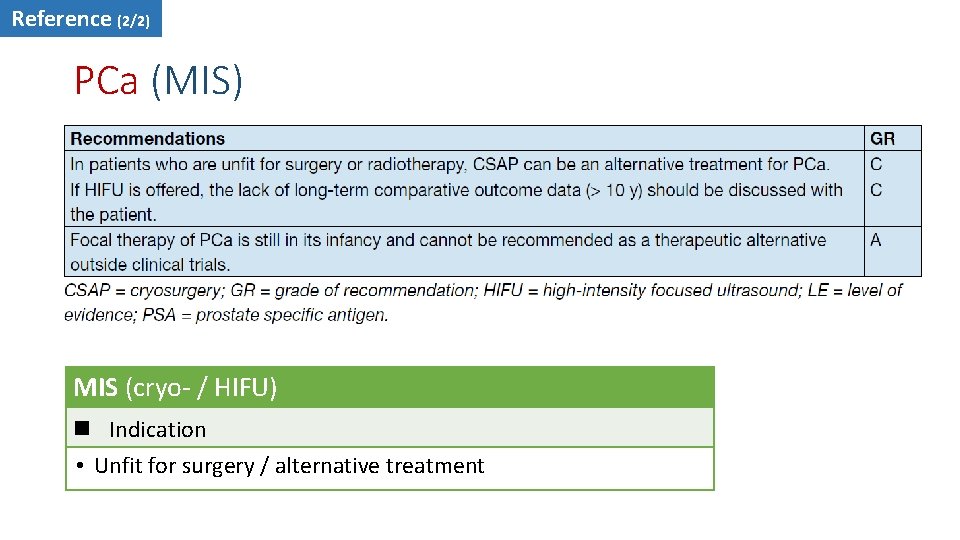
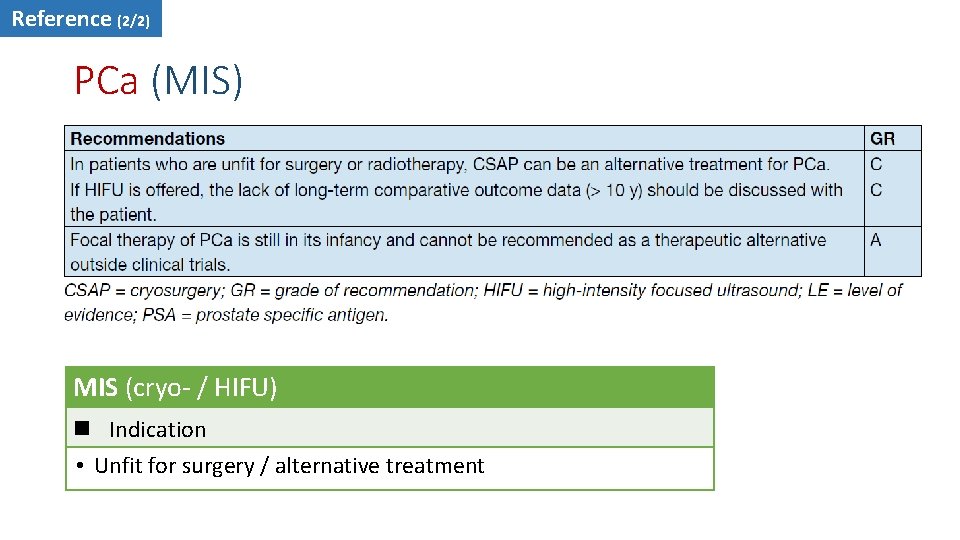
Reference (2/2) PCa (MIS) MIS (cryo- / HIFU) n Indication • Unfit for surgery / alternative treatment
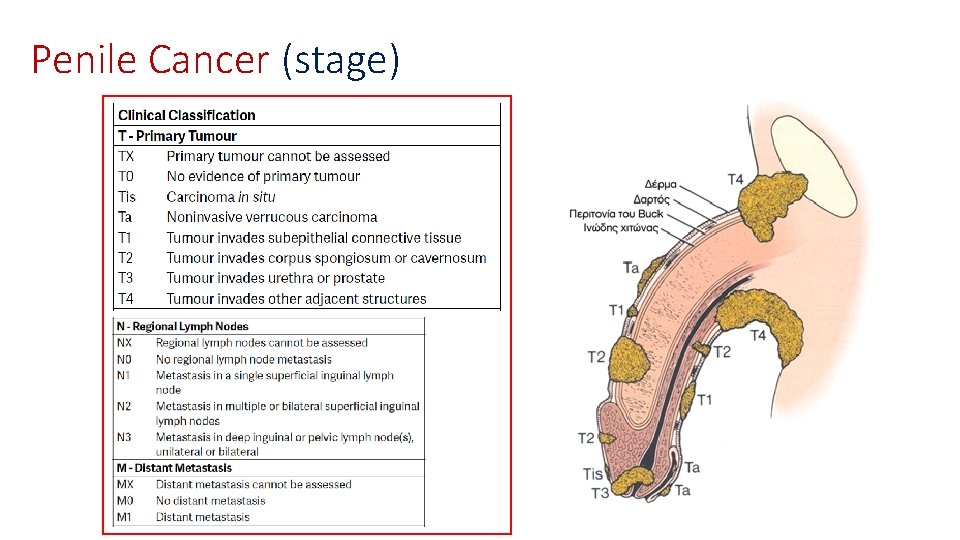
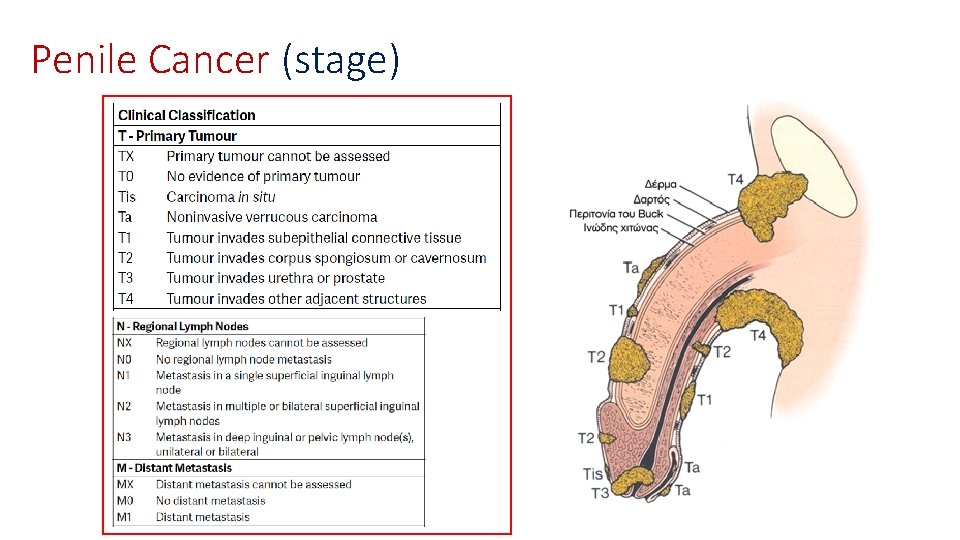
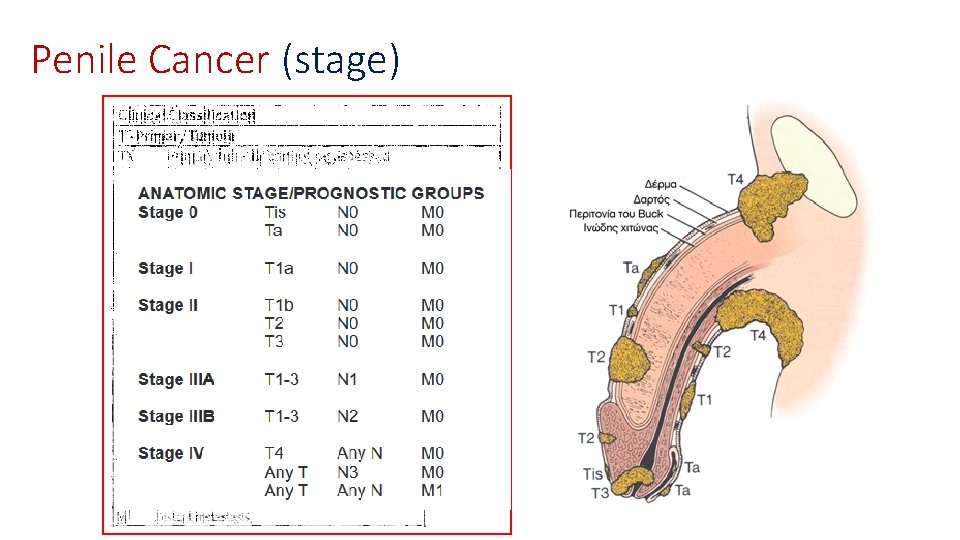
Penile Cancer (stage)
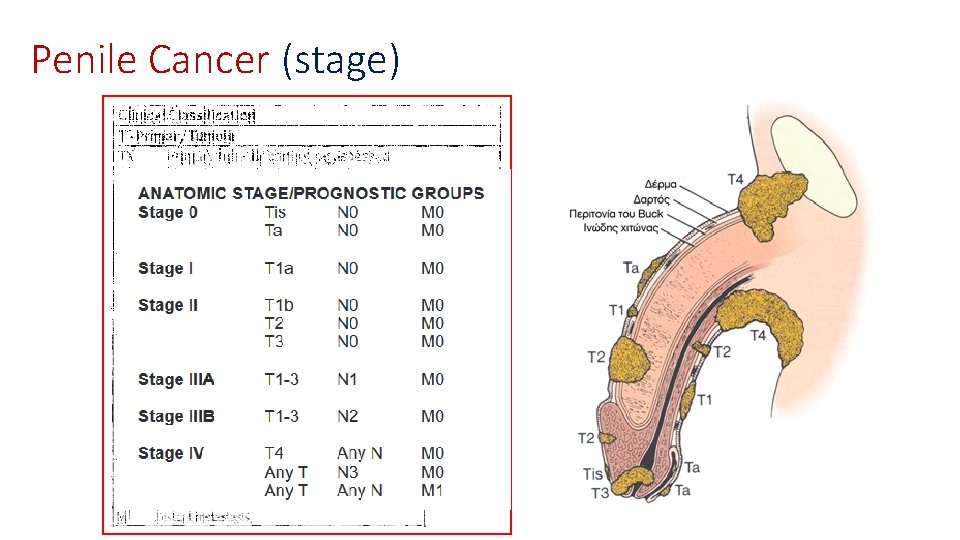
Penile Cancer (stage)
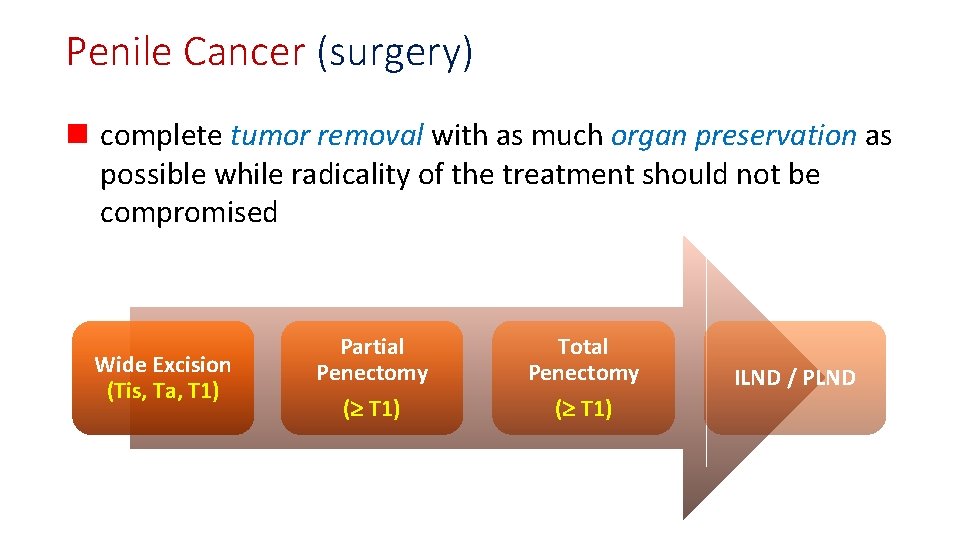
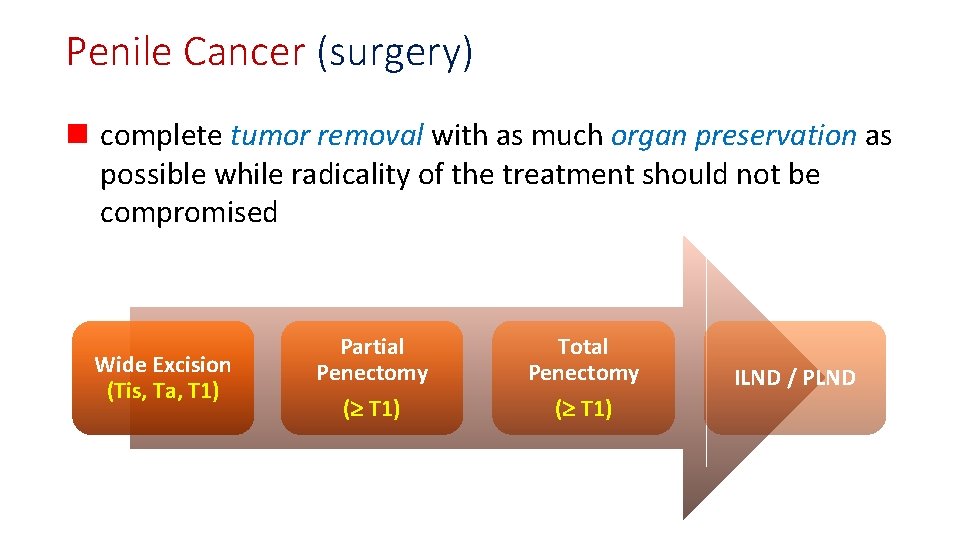
Penile Cancer (surgery) n complete tumor removal with as much organ preservation as possible while radicality of the treatment should not be compromised Wide Excision (Tis, Ta, T 1) Partial Penectomy Total Penectomy ( T 1) ILND / PLND
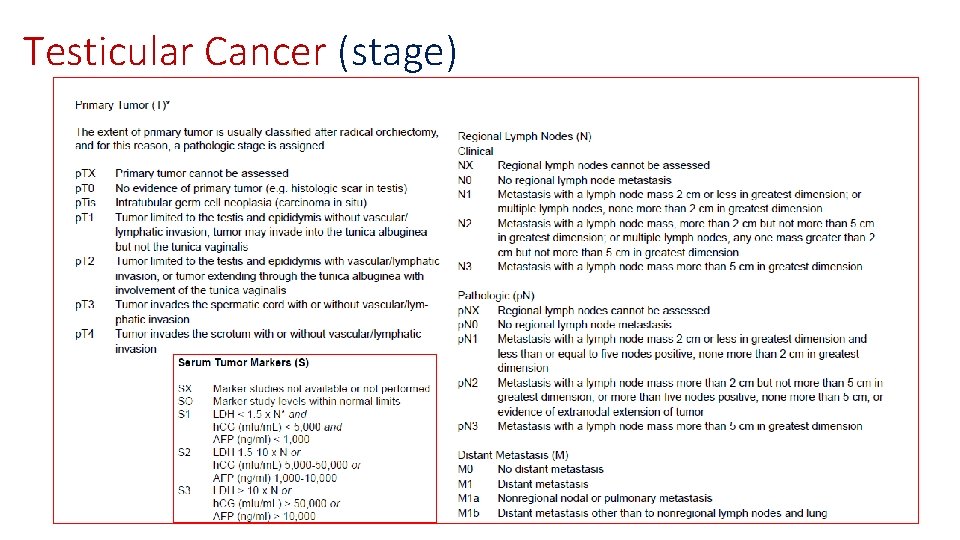
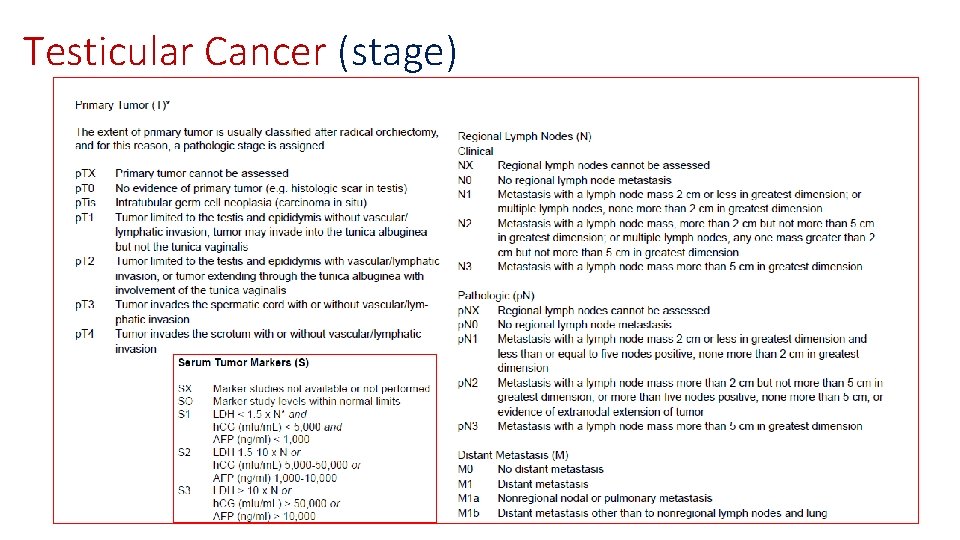
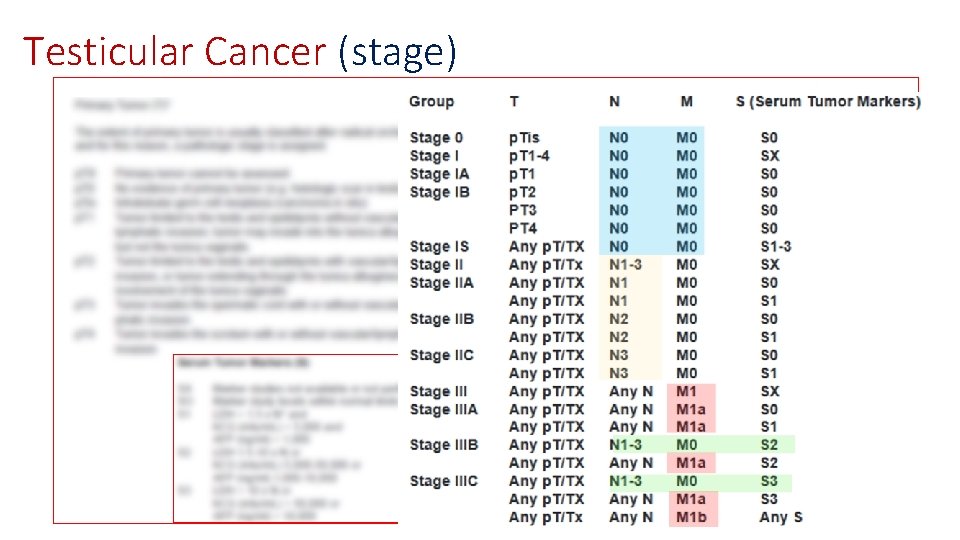
Testicular Cancer (stage)
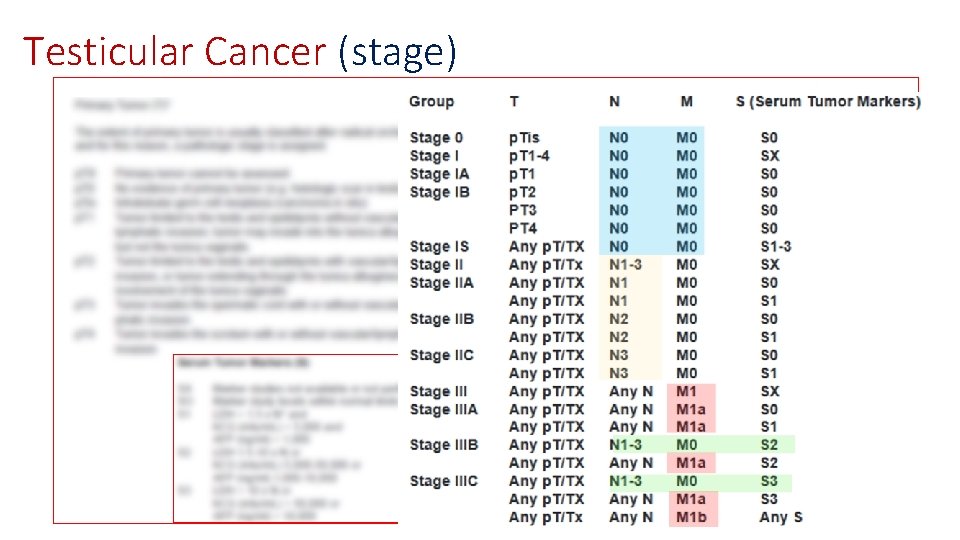
Testicular Cancer (stage)
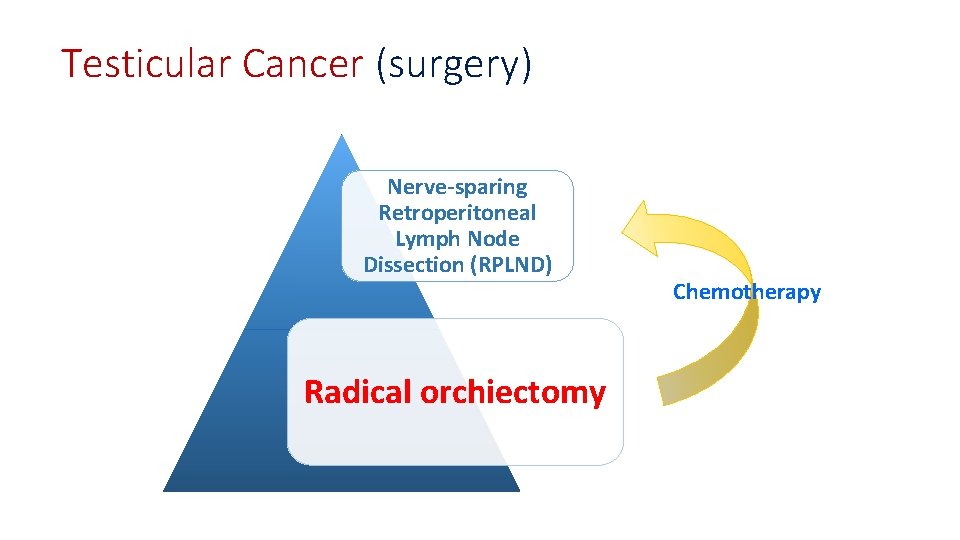
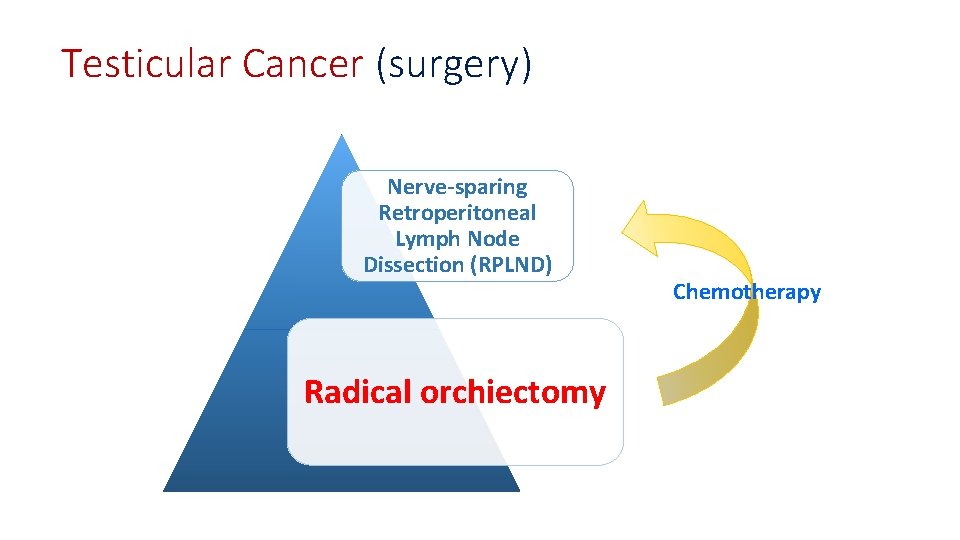
Testicular Cancer (surgery) Nerve-sparing Retroperitoneal Lymph Node Dissection (RPLND) Radical orchiectomy Chemotherapy

THANK YOU