2 Neoplastic Proliferations of White Cells Myeloid Neoplasms


- Slides: 39
2. Neoplastic Proliferations of White Cells ~ Myeloid Neoplasms II Ghadeer Hayel, MD
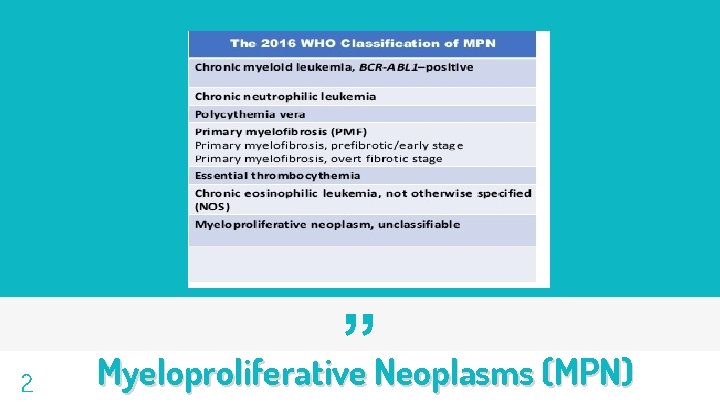
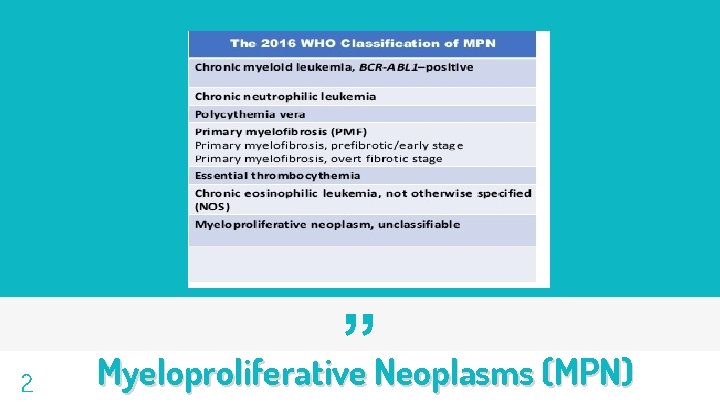
2 ” Myeloproliferative Neoplasms (MPN)
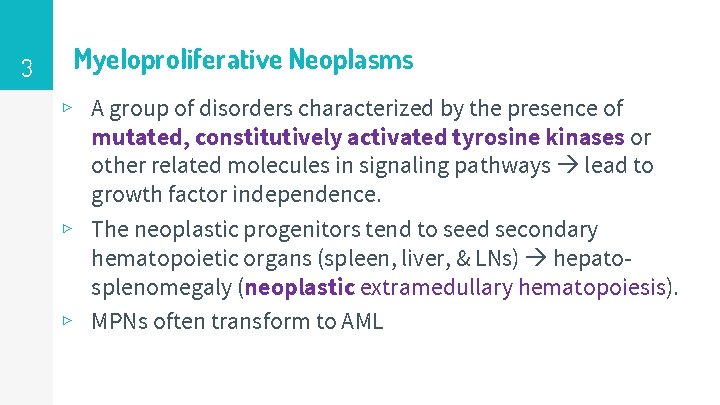
3 Myeloproliferative Neoplasms ▹ A group of disorders characterized by the presence of mutated, constitutively activated tyrosine kinases or other related molecules in signaling pathways lead to growth factor independence. ▹ The neoplastic progenitors tend to seed secondary hematopoietic organs (spleen, liver, & LNs) hepatosplenomegaly (neoplastic extramedullary hematopoiesis). ▹ MPNs often transform to AML
4 Myeloproliferative Neoplasms ▹ 1) 2) 3) 4) Four major diagnostic entities are recognized: Chronic myeloid leukemia (CML). Polycythemia vera (PCV). Primary myelofibrosis (PM). Essential thrombocythemia (ET).
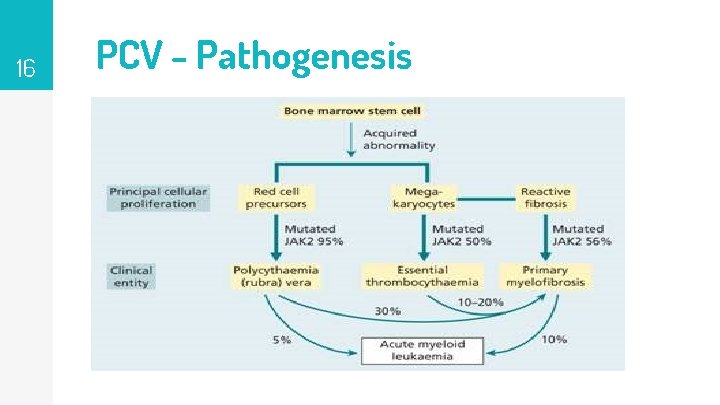
5 Myeloproliferative Neoplasms ▹ CML is separated from the others by its characteristic BCR-ABL ▹ ▹ 1) 2) ▹ fusion gene produces a constitutively active BCR-ABL tyrosine kinase. The most common genetic abnormalities in “BCRABL–negative” MPNs are activating mutations in the tyrosine kinase JAK 2. all MPNs have variable propensities to transform to: a “spent phase”: resembling primary myelofibrosis a “blast crisis” identical to AML Both triggered by the acquisition of other somatic mutations
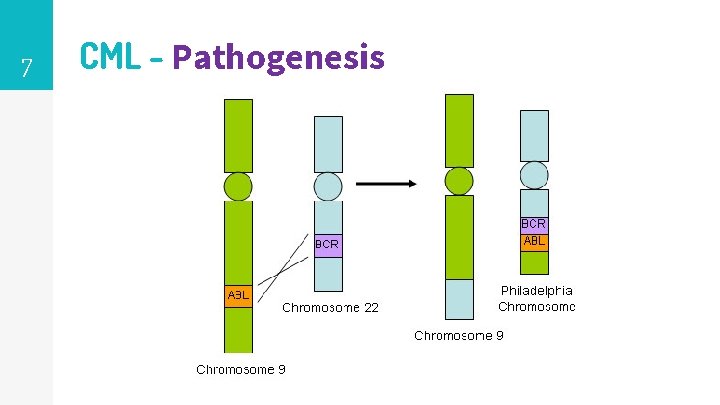
6 Chronic Myeloid Leukemia (CML) Pathogenesis ▹ CML is distinguished from other MPN by the presence of a chimeric BCR-ABL gene, derived from portions of the BCR gene on chr. 22 & the ABL gene on chr. 9. ▹ 95% of cases, the BCR-ABL gene is the product of a balanced t(9; 22) translocation that moves ABL from chr. 9 to a position on chr. 22 adjacent to BCR. ▹ Translocation identified in some B-ALL.
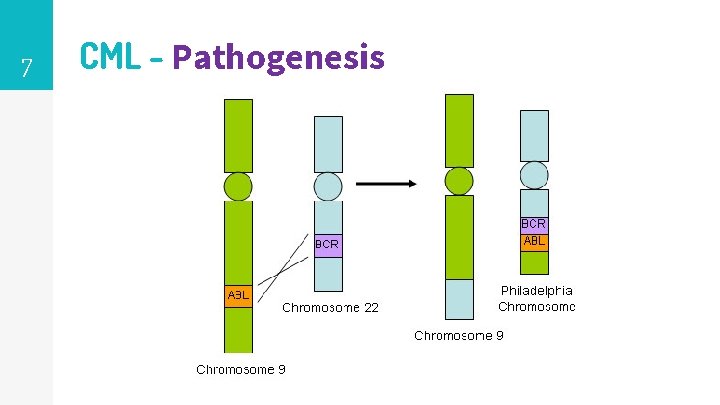
7 CML - Pathogenesis
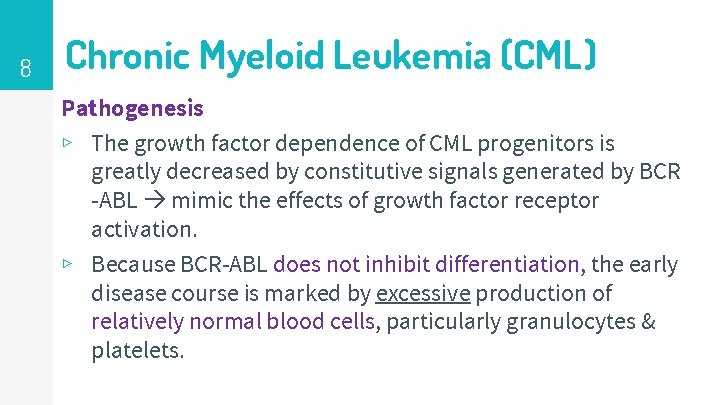
8 Chronic Myeloid Leukemia (CML) Pathogenesis ▹ The growth factor dependence of CML progenitors is greatly decreased by constitutive signals generated by BCR -ABL mimic the effects of growth factor receptor activation. ▹ Because BCR-ABL does not inhibit differentiation, the early disease course is marked by excessive production of relatively normal blood cells, particularly granulocytes & platelets.
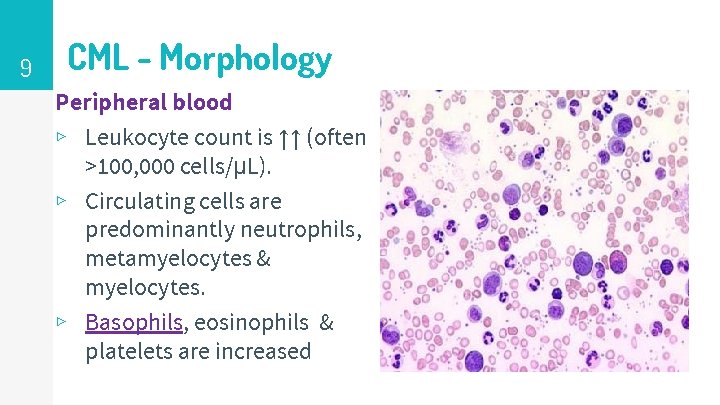
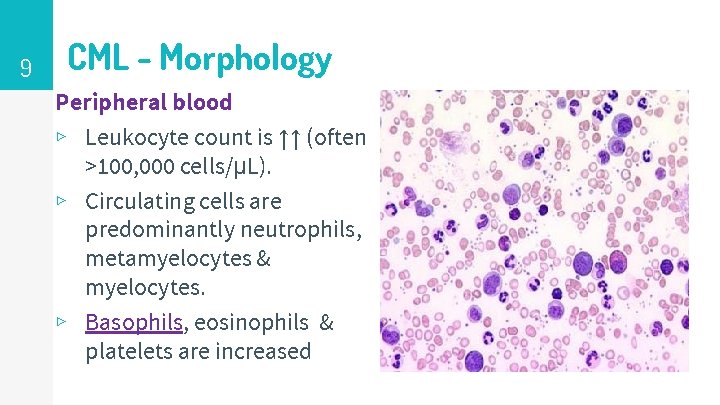
9 CML - Morphology Peripheral blood ▹ Leukocyte count is ↑↑ (often >100, 000 cells/μL). ▹ Circulating cells are predominantly neutrophils, metamyelocytes & myelocytes. ▹ Basophils, eosinophils & platelets are increased
10
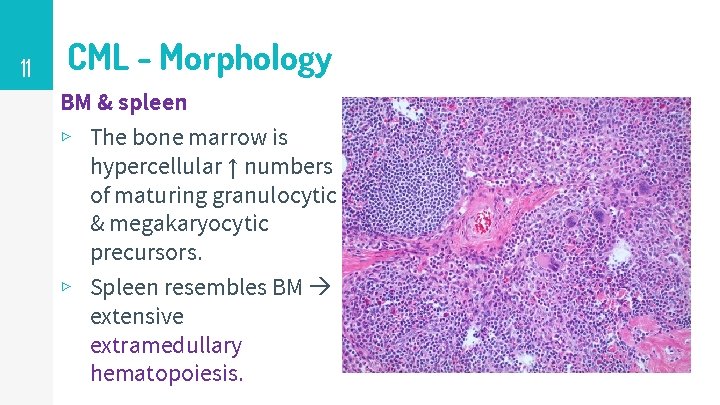
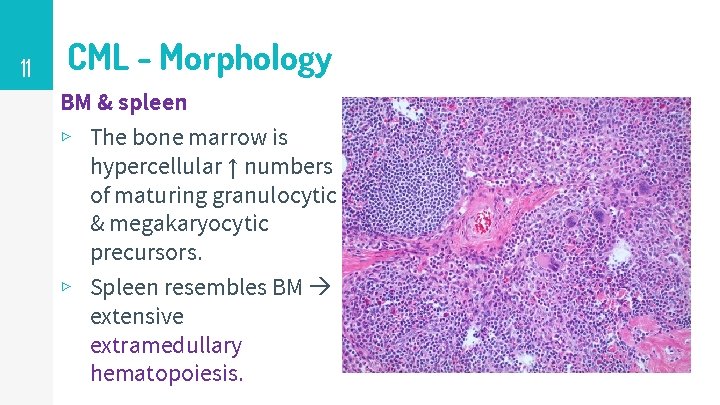
11 CML - Morphology BM & spleen ▹ The bone marrow is hypercellular ↑ numbers of maturing granulocytic & megakaryocytic precursors. ▹ Spleen resembles BM extensive extramedullary hematopoiesis.
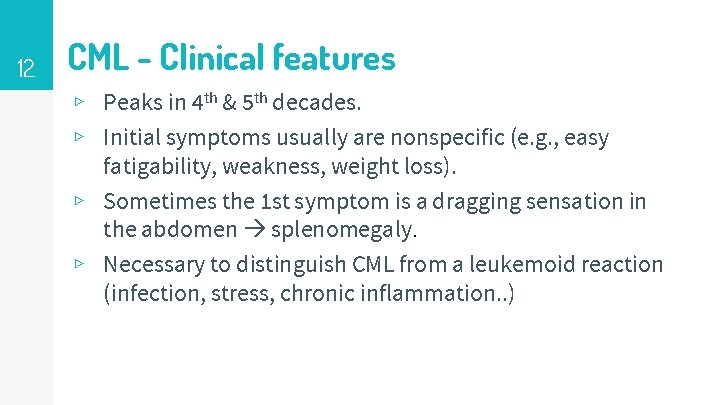
12 CML - Clinical features ▹ Peaks in 4 th & 5 th decades. ▹ Initial symptoms usually are nonspecific (e. g. , easy fatigability, weakness, weight loss). ▹ Sometimes the 1 st symptom is a dragging sensation in the abdomen splenomegaly. ▹ Necessary to distinguish CML from a leukemoid reaction (infection, stress, chronic inflammation. . )
13 CML - Clinical features ▹ Slowly progressive disease Median survival is 3 years without treatment ▹ Can progress to accelerated phase Anemia, thombocytopenia & additional genetic mutations. ▹ Progress to blast phase: 1) 70% AML 2) 30% ALL ▹ Rarely progresses to spent phase with fibrosis.
14 Polycythemia Vera (PCV) ▹ Excessive proliferation of erythroid, granulocytic, and megakaryocytic elements panmyelosis ▹ Most clinical signs & symptoms are related to an absolute increase in red cell mass. ▹ Must be distinguished from relative polycythemia results from hemoconcentration. ▹ Unlike reactive absolute polycythemia, PCV is associated with low serum erythropoietin a reflection of growth factor–independent growth of the neoplastic clone.
15 PCV - Pathogenesis ▹ Strongly associated (> 97%) with activating point mutations in the tyrosine kinase JAK 2. ▹ JAK 2 normally acts in the signaling pathways downstream of the erythropoietin receptor. ▹ The JAK 2 mutation lowers the dependence of hematopoietic cells on growth factors for growth and survival.
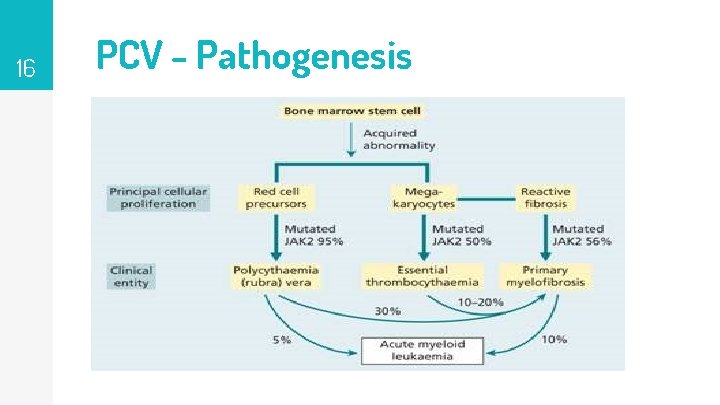
16 PCV - Pathogenesis
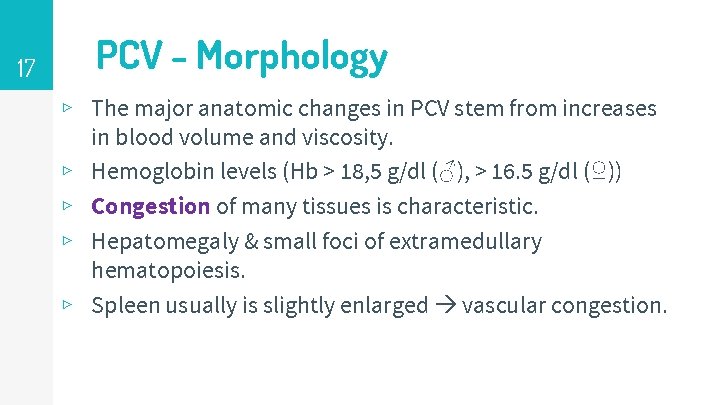
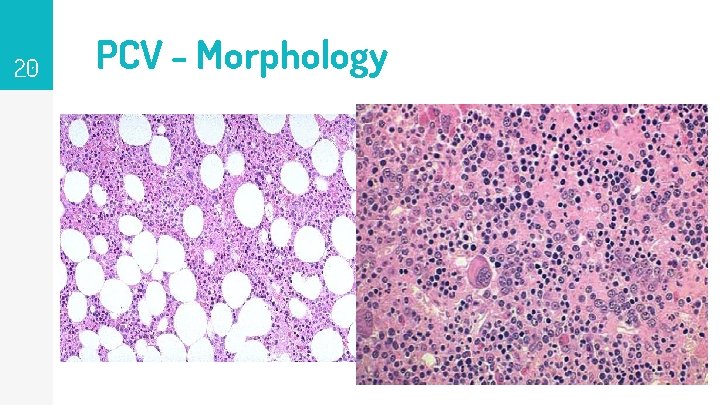
17 PCV - Morphology ▹ The major anatomic changes in PCV stem from increases in blood volume and viscosity. ▹ Hemoglobin levels (Hb > 18, 5 g/dl (♂), > 16. 5 g/dl (♀)) ▹ Congestion of many tissues is characteristic. ▹ Hepatomegaly & small foci of extramedullary hematopoiesis. ▹ Spleen usually is slightly enlarged vascular congestion.
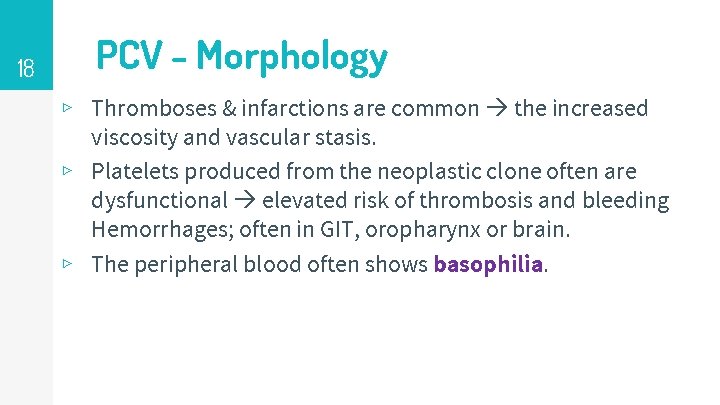
18 PCV - Morphology ▹ Thromboses & infarctions are common the increased viscosity and vascular stasis. ▹ Platelets produced from the neoplastic clone often are dysfunctional elevated risk of thrombosis and bleeding Hemorrhages; often in GIT, oropharynx or brain. ▹ The peripheral blood often shows basophilia.
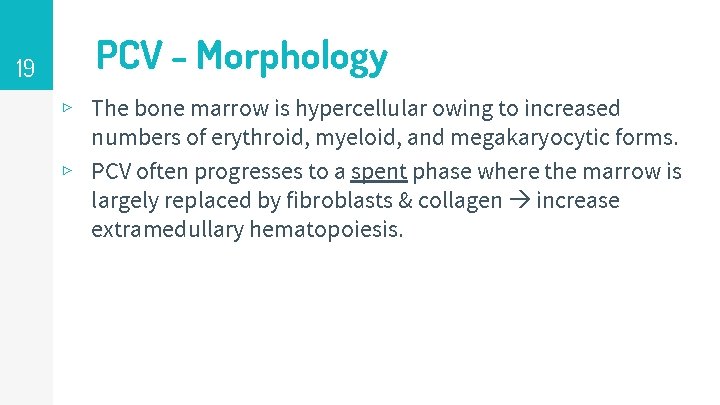
19 PCV - Morphology ▹ The bone marrow is hypercellular owing to increased numbers of erythroid, myeloid, and megakaryocytic forms. ▹ PCV often progresses to a spent phase where the marrow is largely replaced by fibroblasts & collagen increase extramedullary hematopoiesis.
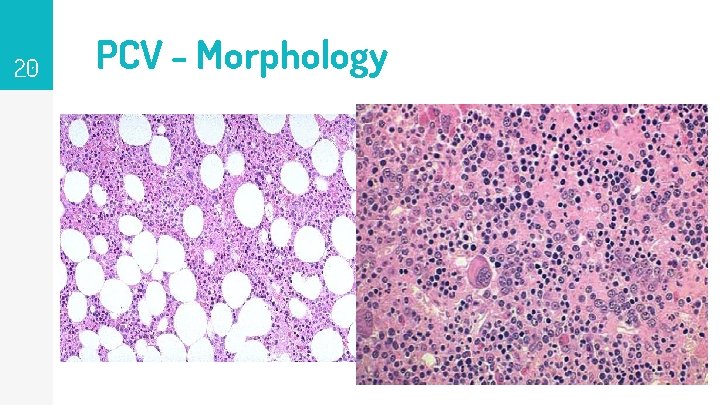
20 PCV - Morphology
21 PCV – Clinical features ▹ Insidious, usually in late middle age. ▹ Patients are plethoric & often cyanotic. ▹ Pruritus Histamine released from the neoplastic basophils. ▹ Thrombotic and hemorrhagic tendencies & hypertension. Headache, dizziness, GIT (hematemesis &melena) common.
22 PCV – Prognosis ▹ Without treatment, death occurs from vascular complications within months. ▹ Median survival is increased to ~10 years by lowering the red cell count to near normal repeated phlebotomy. ▹ Prolonged survival a propensity to evolve to a “spent phase” (resembling PM) ~10 years. ▹ Extensive marrow fibrosis, hematopoiesis shifts to the spleen, which enlarges markedly.
23 Essential Thrombocythemia (ET) ▹ Megakaryocyte proliferation with overproduction of platelets. ▹ Elevated platelet counts (>600 x 10 x 9/L). ▹ Separated from PCV and primary myelofibrosis based on the absence of polycythemia and marrow fibrosis, respectively.
24 Essential Thrombocythemia – Pathogenesis ▹ ET is associated with activating point mutations in JAK 2 (50%), a receptor tyrosine kinase that is normally activated by thrombopoietin. ▹ Constitutive JAK 2 renders the progenitor thrombopoietinindependent and leads to hyperproliferation. ▹ The JAK 2 mutation is the same as that found in almost all cases of PCV. ▹ Why some patients with JAK 2 mutations present with PCV & others with ET not understood.
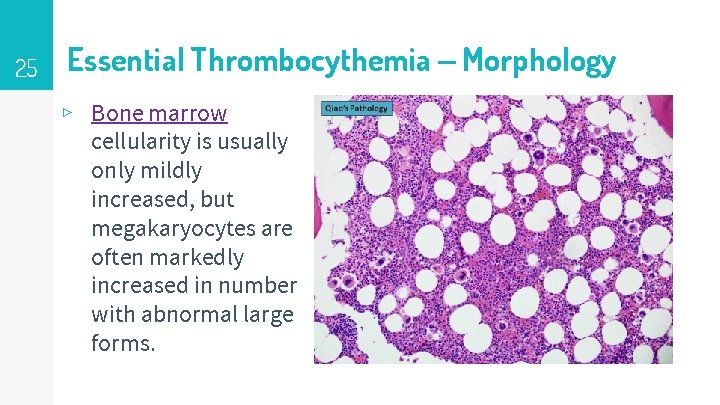
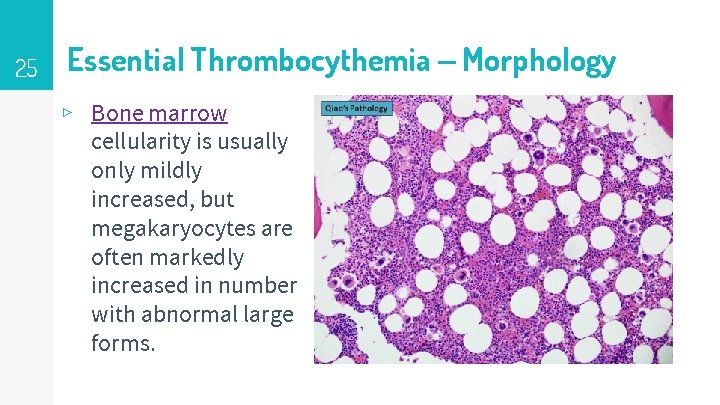
25 Essential Thrombocythemia – Morphology ▹ Bone marrow cellularity is usually only mildly increased, but megakaryocytes are often markedly increased in number with abnormal large forms.
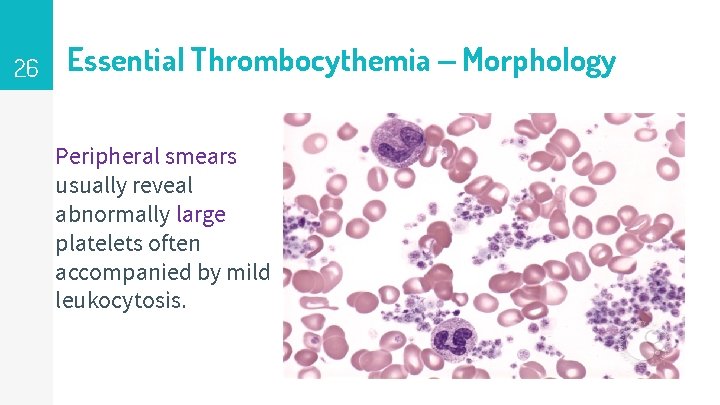
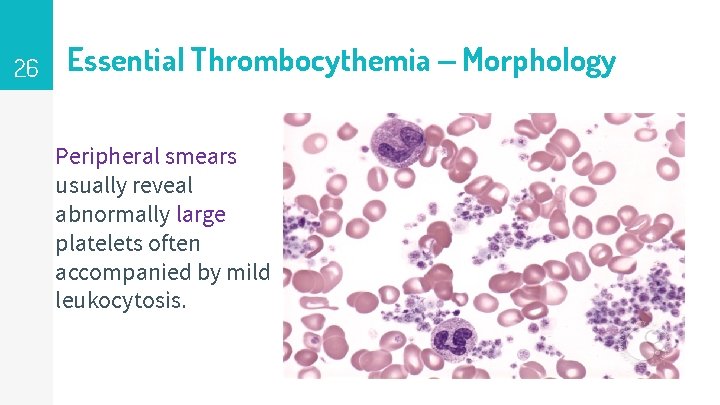
26 Essential Thrombocythemia – Morphology Peripheral smears usually reveal abnormally large platelets often accompanied by mild leukocytosis.
27 ET– Clinical features ▹ ET is an indolent disorder with long asymptomatic periods only occasional thrombotic or hemorrhagic crises. ▹ ET manifests clinically with elevated platelet counts. ▹ Causes of reactive thrombocytosis, (such as inflammatory disorders & iron deficiency) must be excluded before the diagnosis can be established
28 ET– Clinical features ▹ Platelets are not only increased in numbers but also frequently demonstrate qualitative abnormalities in functional tests. ▹ The types of thrombotic events resemble those observed in PCV. ▹ A characteristic symptom erythromelalgia, a throbbing and burning of hands and feet caused by occlusion of small arterioles by platelet aggregates may also be seen in PCV.

29
30 ET– Prognosis ▹ Median survival times 12~15 years ▹ Transformation to myelofibrosis (spent phase). ▹ Transformation to acute leukemia is rare.
31 Primary Myelofibrosis (PM) ▹ The hallmark of primary myelofibrosis is the development of obliterative marrow fibrosis reduces bone marrow hematopoiesis 1) Cytopenias. 2) Extensive extramedullary hematopoiesis. ▹ Histologically, the appearance is identical to the spent phase that occurs occasionally late in the course of other MPN.
32 PM - Pathogenesis ▹ JAK 2 mutations are present in 50% to 60% of cases ▹ Most of the remaining cases have other mutations which also stimulate increased JAK signaling. ▹ Why JAK 2 mutations are associated PCV in some patients & PM in others is not understood.
33 PM - Pathogenesis ▹ Pathogenesis is similar between PM and spent phase MPN ▹ The characteristic marrow fibrosis is caused by the inappropriate release of fibrogenic factors from neoplastic megakaryocytes. ▹ Two factors synthesized by megakaryocytes have been implicated (fibrogenic factors ): 1) Platelet-derived growth factor (PDGF). 2) TGF-β.
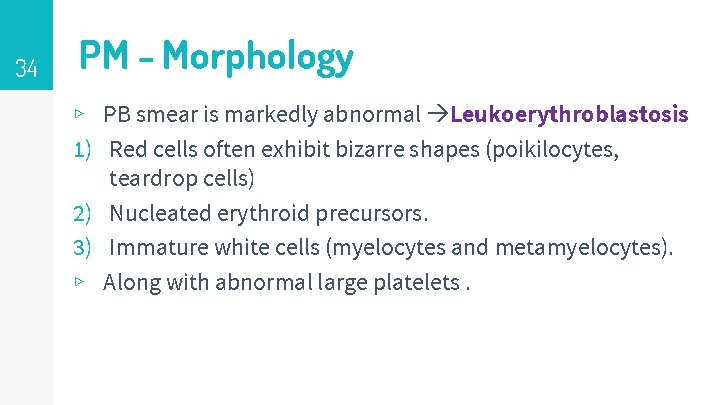
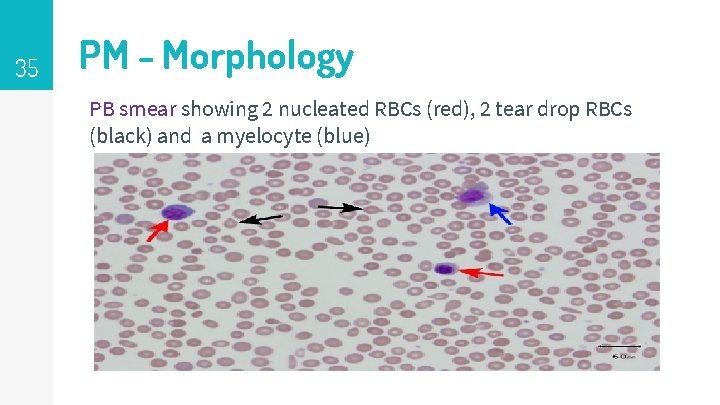
34 PM - Morphology ▹ PB smear is markedly abnormal Leukoerythroblastosis 1) Red cells often exhibit bizarre shapes (poikilocytes, teardrop cells) 2) Nucleated erythroid precursors. 3) Immature white cells (myelocytes and metamyelocytes). ▹ Along with abnormal large platelets.
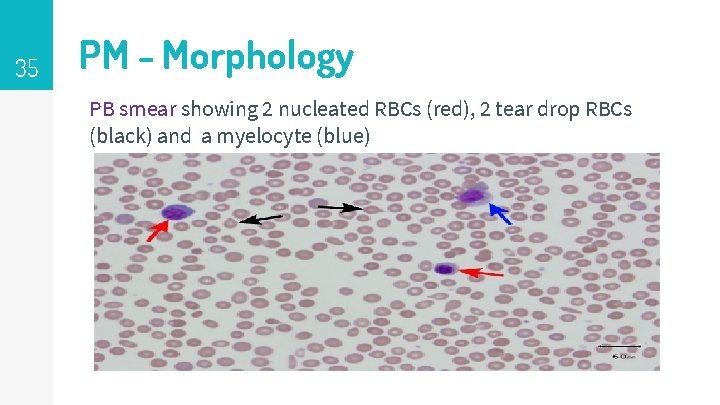
35 PM - Morphology PB smear showing 2 nucleated RBCs (red), 2 tear drop RBCs (black) and a myelocyte (blue)
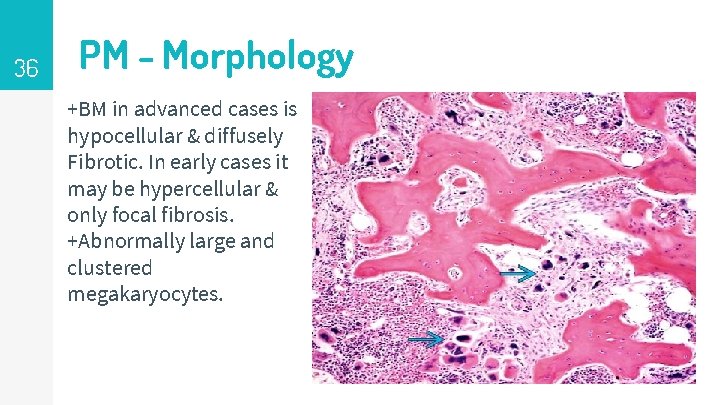
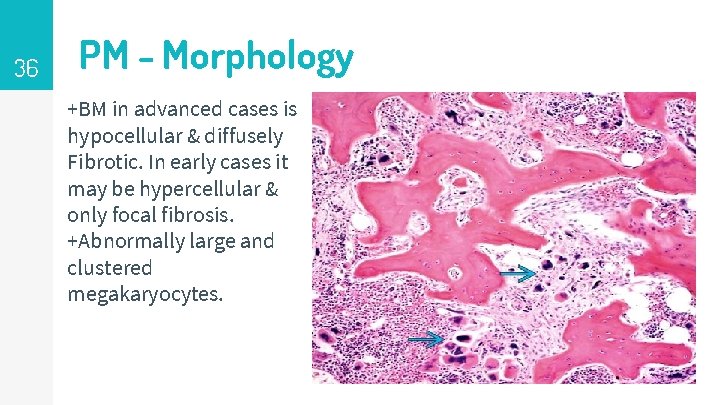
36 PM - Morphology +BM in advanced cases is hypocellular & diffusely Fibrotic. In early cases it may be hypercellular & only focal fibrosis. +Abnormally large and clustered megakaryocytes.

37 PM - Clinical Features Age more than 60 Anemia and splenomegaly. Fatigue, weakness and night sweats Lab results; normochromic and normocytic anemia and Leukoerythroblatosis ▹ Bone marrow is essential for the diagnosis. ▹ ▹
38 PM - Prognosis ▹ ▹ Median survival is 4 -5 years. 5 -20% transform to AML. More difficult to treat than PCV and CML. Treat with JAK 2 inhibitors and HSCT.
39