1909 Starling The Kidney presents in the highest



- Slides: 28
1909 Starling: „The Kidney presents in the highest degree the phenomenon of sensibility… must be endowed with intelligence. ” 1957 Homer-Smith: … only a passive agent operating blinly and automatically according to the dictates of receptor- effector systems located elsewhere in the body
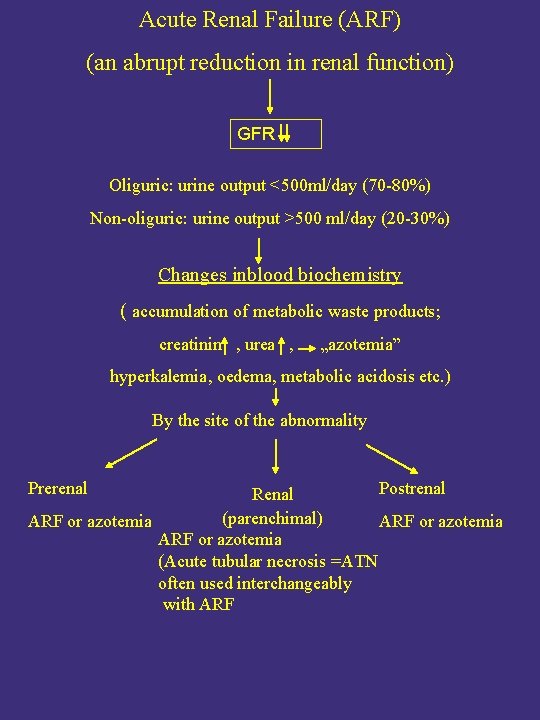
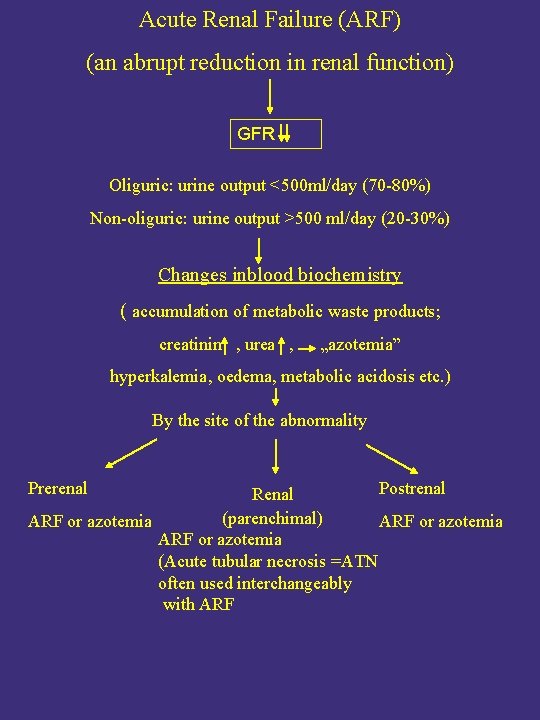
Acute Renal Failure (ARF) (an abrupt reduction in renal function) GFR Oliguric: urine output <500 ml/day (70 -80%) Non-oliguric: urine output >500 ml/day (20 -30%) Changes inblood biochemistry ( accumulation of metabolic waste products; creatinin , urea , „azotemia” hyperkalemia, oedema, metabolic acidosis etc. ) By the site of the abnormality Prerenal Postrenal Renal (parenchimal) ARF or azotemia (Acute tubular necrosis =ATN often used interchangeably with ARF
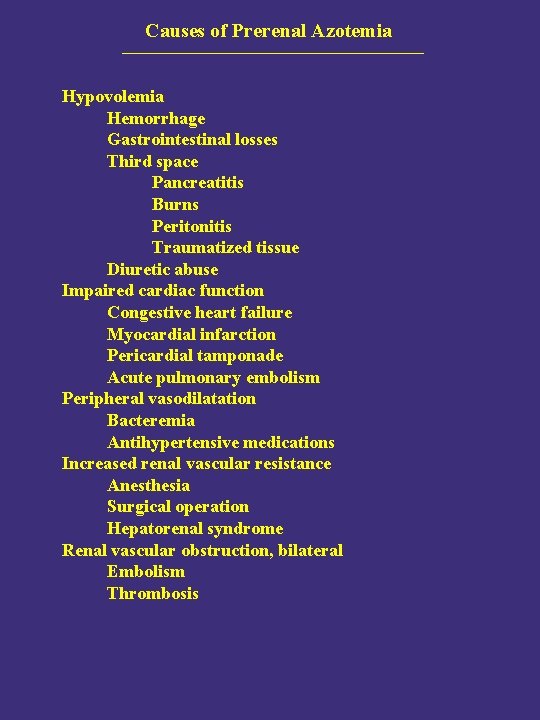
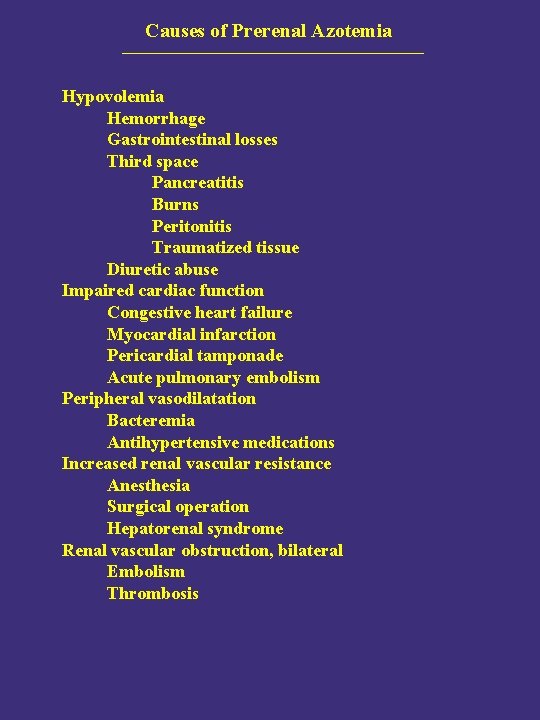
Causes of Prerenal Azotemia Hypovolemia Hemorrhage Gastrointestinal losses Third space Pancreatitis Burns Peritonitis Traumatized tissue Diuretic abuse Impaired cardiac function Congestive heart failure Myocardial infarction Pericardial tamponade Acute pulmonary embolism Peripheral vasodilatation Bacteremia Antihypertensive medications Increased renal vascular resistance Anesthesia Surgical operation Hepatorenal syndrome Renal vascular obstruction, bilateral Embolism Thrombosis
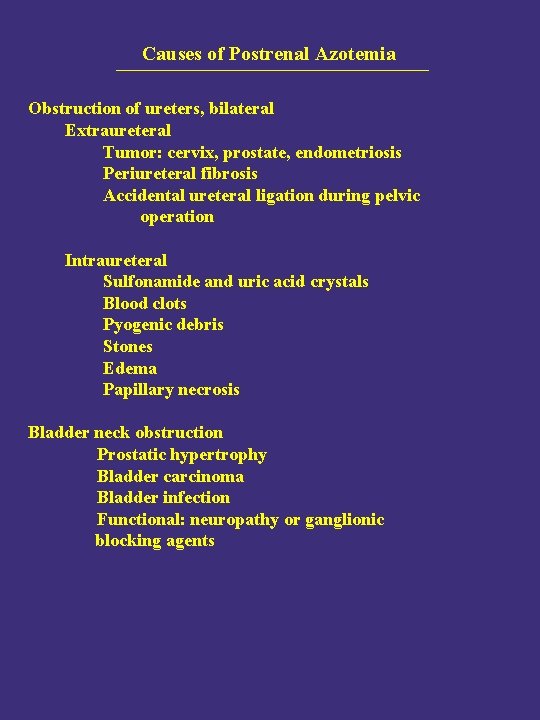
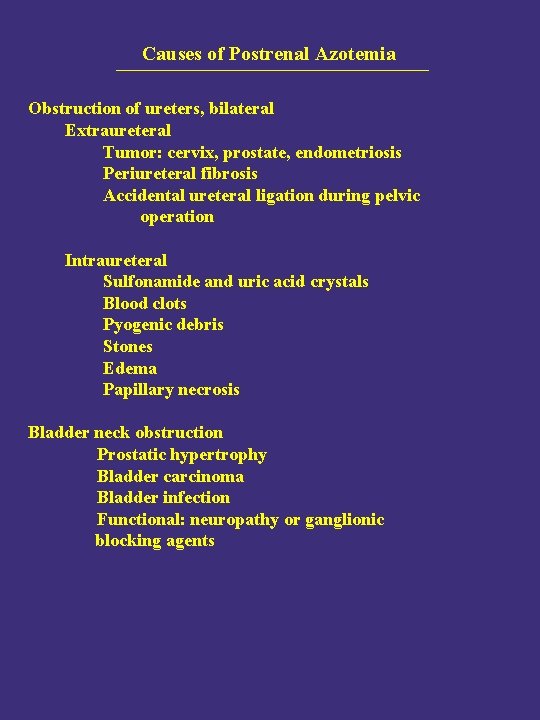
Causes of Postrenal Azotemia Obstruction of ureters, bilateral Extraureteral Tumor: cervix, prostate, endometriosis Periureteral fibrosis Accidental ureteral ligation during pelvic operation Intraureteral Sulfonamide and uric acid crystals Blood clots Pyogenic debris Stones Edema Papillary necrosis Bladder neck obstruction Prostatic hypertrophy Bladder carcinoma Bladder infection Functional: neuropathy or ganglionic blocking agents
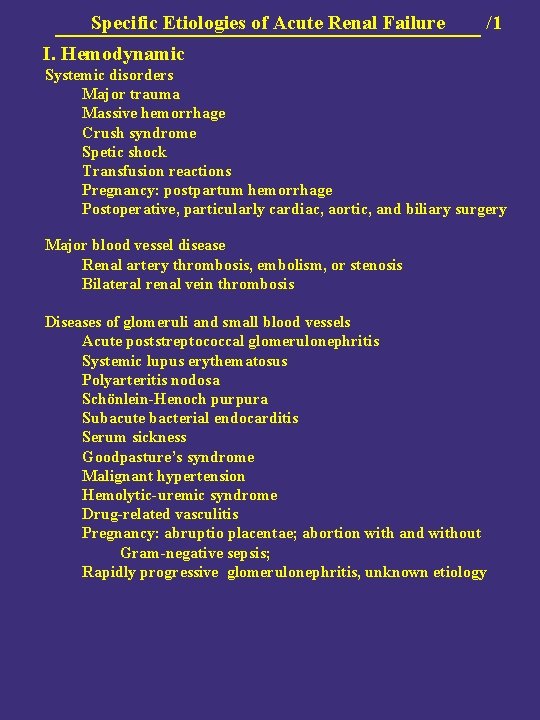
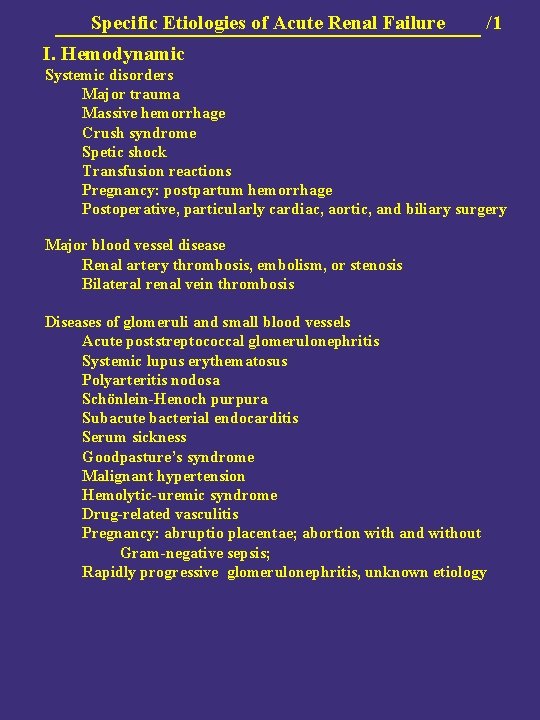
Specific Etiologies of Acute Renal Failure /1 I. Hemodynamic Systemic disorders Major trauma Massive hemorrhage Crush syndrome Spetic shock Transfusion reactions Pregnancy: postpartum hemorrhage Postoperative, particularly cardiac, aortic, and biliary surgery Major blood vessel disease Renal artery thrombosis, embolism, or stenosis Bilateral renal vein thrombosis Diseases of glomeruli and small blood vessels Acute poststreptococcal glomerulonephritis Systemic lupus erythematosus Polyarteritis nodosa Schönlein-Henoch purpura Subacute bacterial endocarditis Serum sickness Goodpasture’s syndrome Malignant hypertension Hemolytic-uremic syndrome Drug-related vasculitis Pregnancy: abruptio placentae; abortion with and without Gram-negative sepsis; Rapidly progressive glomerulonephritis, unknown etiology
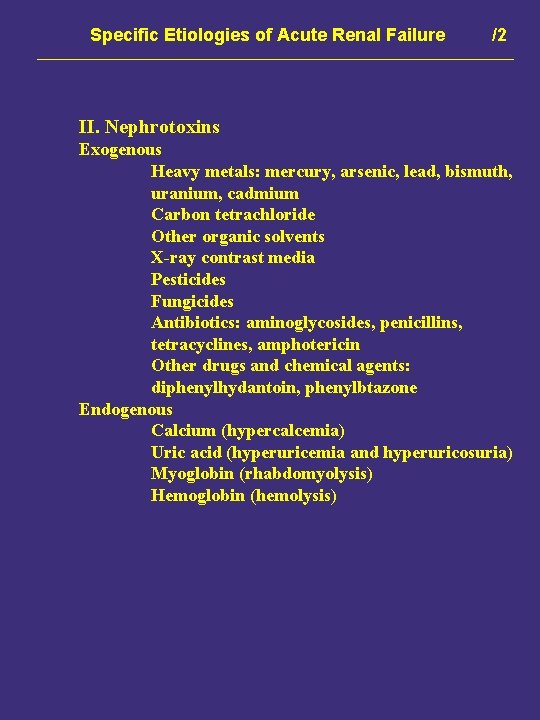
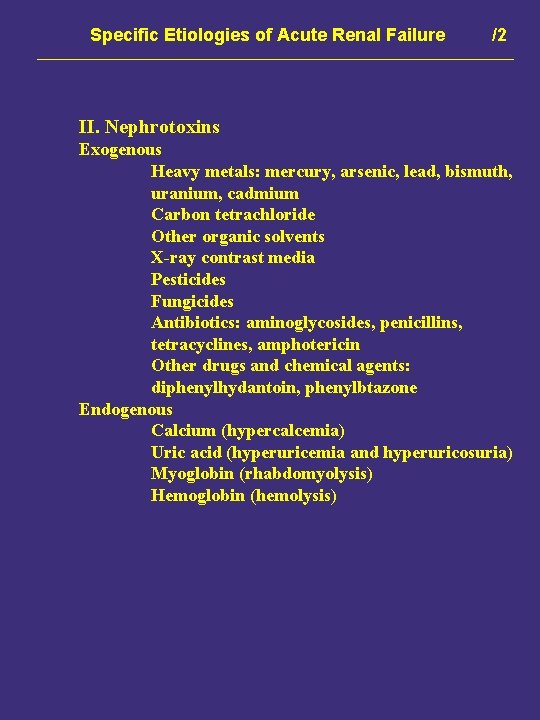
Specific Etiologies of Acute Renal Failure /2 II. Nephrotoxins Exogenous Heavy metals: mercury, arsenic, lead, bismuth, uranium, cadmium Carbon tetrachloride Other organic solvents X-ray contrast media Pesticides Fungicides Antibiotics: aminoglycosides, penicillins, tetracyclines, amphotericin Other drugs and chemical agents: diphenylhydantoin, phenylbtazone Endogenous Calcium (hypercalcemia) Uric acid (hyperuricemia and hyperuricosuria) Myoglobin (rhabdomyolysis) Hemoglobin (hemolysis)
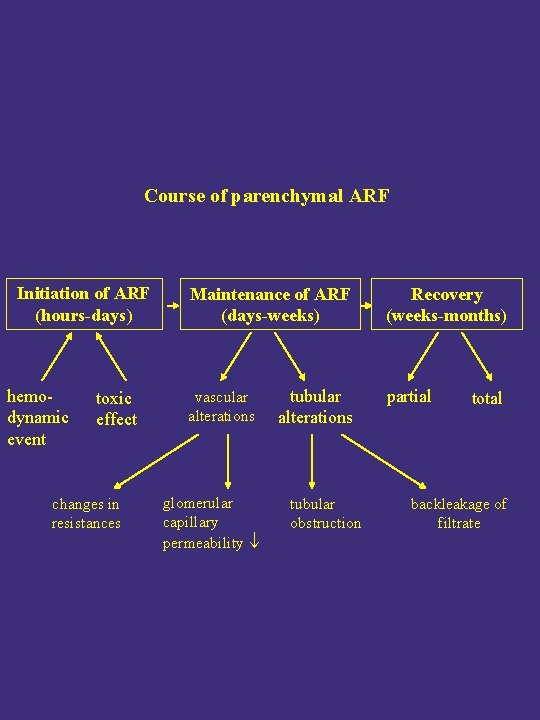
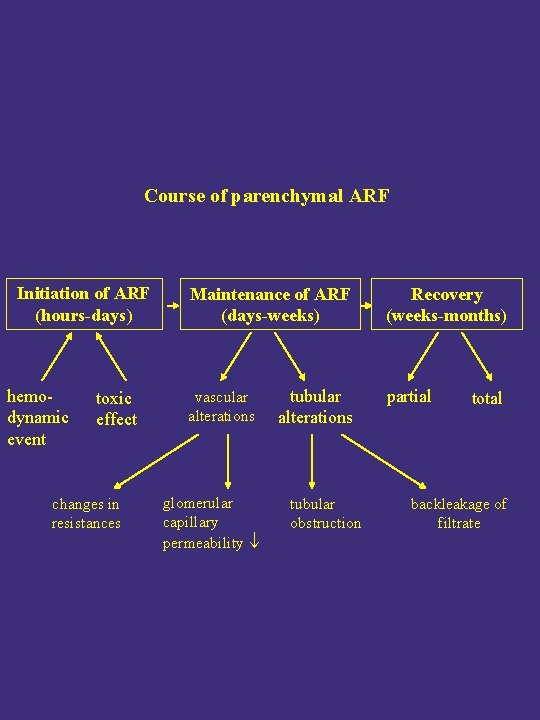
Course of parenchymal ARF Initiation of ARF (hours-days) hemodynamic event toxic effect changes in resistances Maintenance of ARF (days-weeks) vascular alterations glomerular capillary permeability tubular alterations tubular obstruction Recovery (weeks-months) partial total backleakage of filtrate
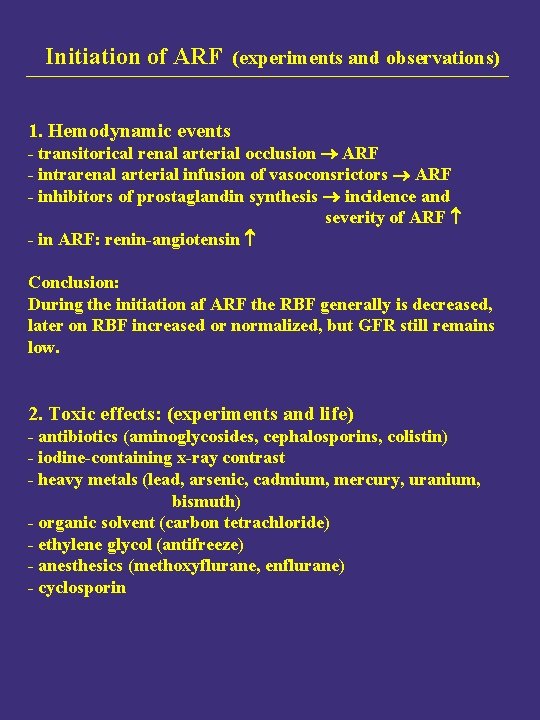
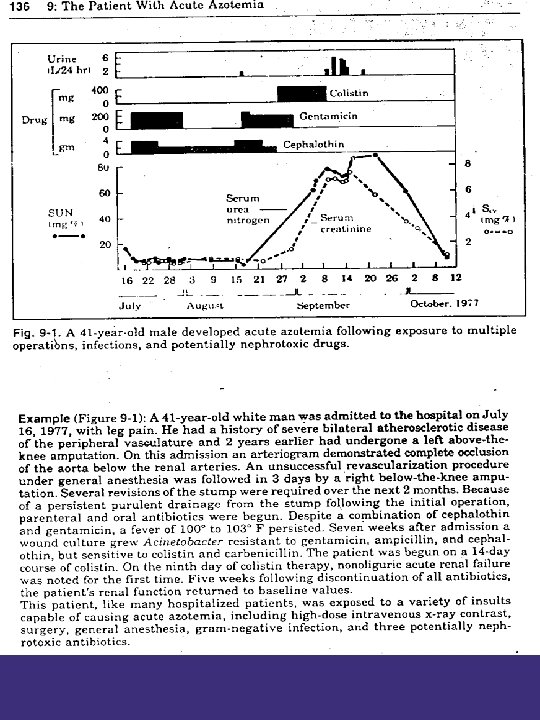
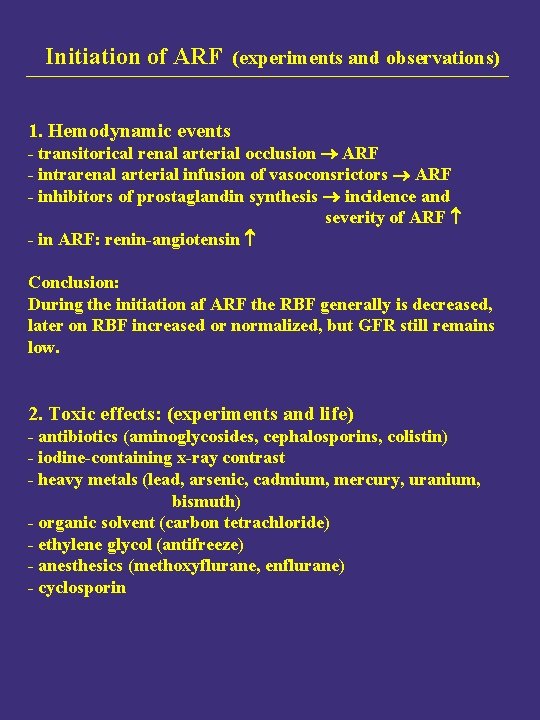
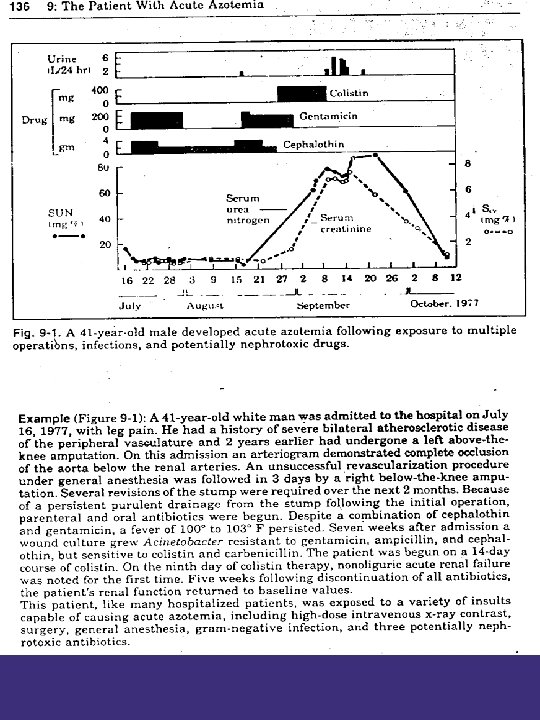
Initiation of ARF (experiments and observations) 1. Hemodynamic events - transitorical renal arterial occlusion ARF - intrarenal arterial infusion of vasoconsrictors ARF - inhibitors of prostaglandin synthesis incidence and severity of ARF - in ARF: renin-angiotensin Conclusion: During the initiation af ARF the RBF generally is decreased, later on RBF increased or normalized, but GFR still remains low. 2. Toxic effects: (experiments and life) - antibiotics (aminoglycosides, cephalosporins, colistin) - iodine-containing x-ray contrast - heavy metals (lead, arsenic, cadmium, mercury, uranium, bismuth) - organic solvent (carbon tetrachloride) - ethylene glycol (antifreeze) - anesthesics (methoxyflurane, enflurane) - cyclosporin
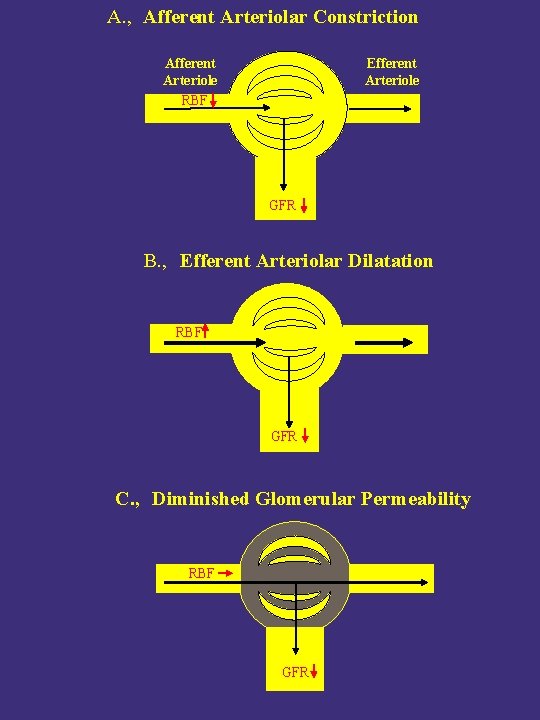
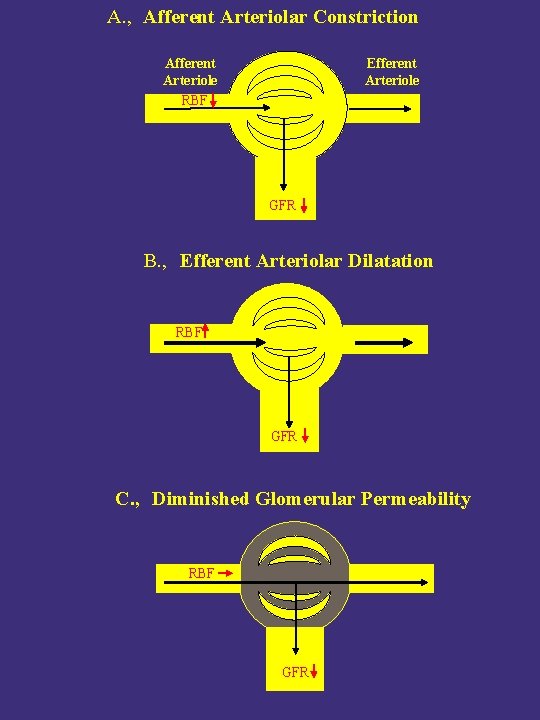
A. , Afferent Arteriolar Constriction Afferent Arteriole RBF Efferent Arteriole GFR B. , Efferent Arteriolar Dilatation RBF GFR C. , Diminished Glomerular Permeability RBF GFR

Changes in Endothelial Fenestration of Glomerular Capillary during ARF Induced by Ischemia

Changes in Podocytes’ Foot Processes of Glomerular Capillary during ARF Induced by Ischemia
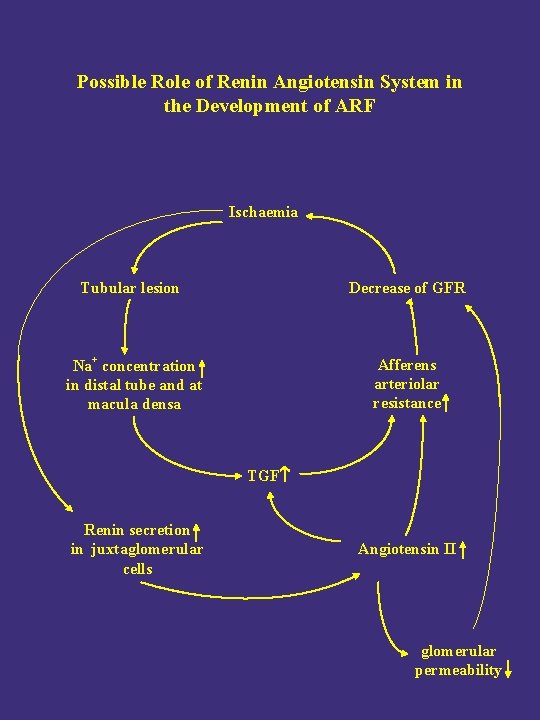
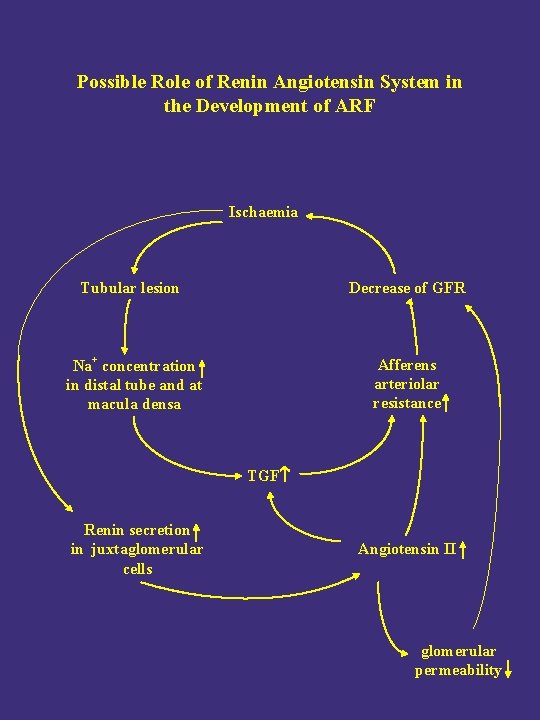
Possible Role of Renin Angiotensin System in the Development of ARF Ischaemia Tubular lesion Decrease of GFR Na+ concentration in distal tube and at macula densa Afferens arteriolar resistance TGF Renin secretion in juxtaglomerular cells Angiotensin II glomerular permeability
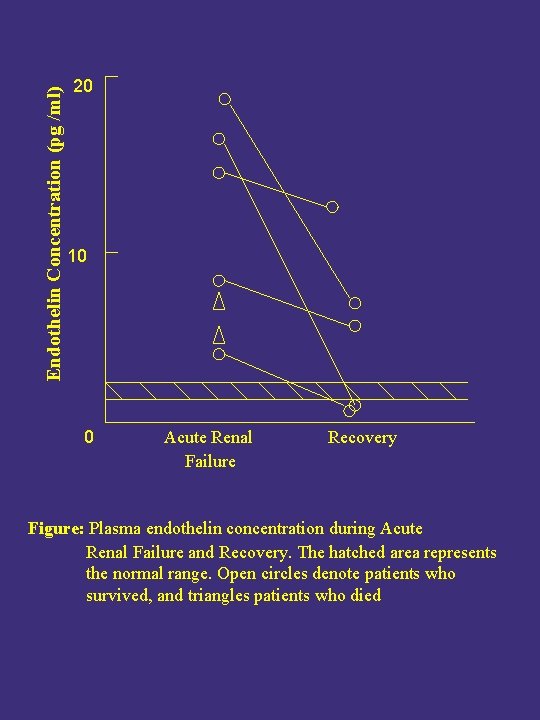
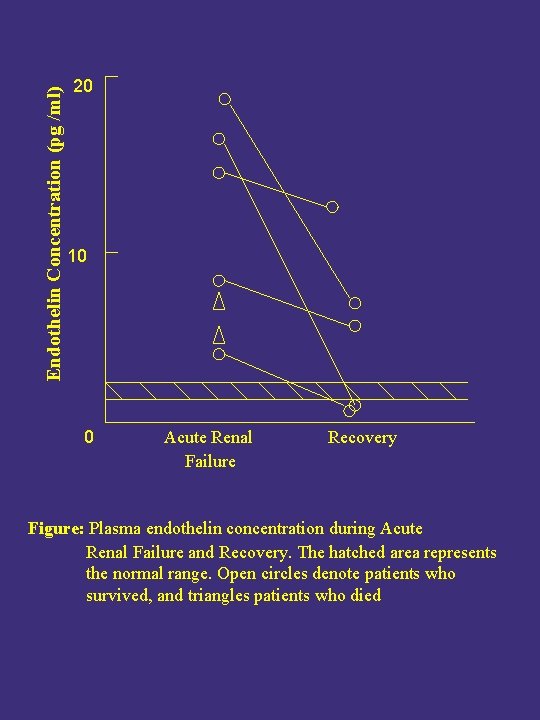
Endothelin Concentration (pg /ml) 20 10 0 Acute Renal Failure Recovery Figure: Plasma endothelin concentration during Acute Renal Failure and Recovery. The hatched area represents the normal range. Open circles denote patients who survived, and triangles patients who died
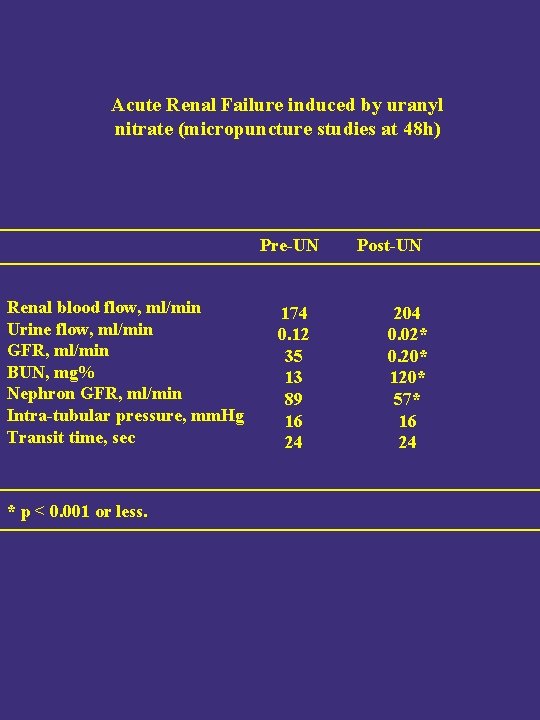
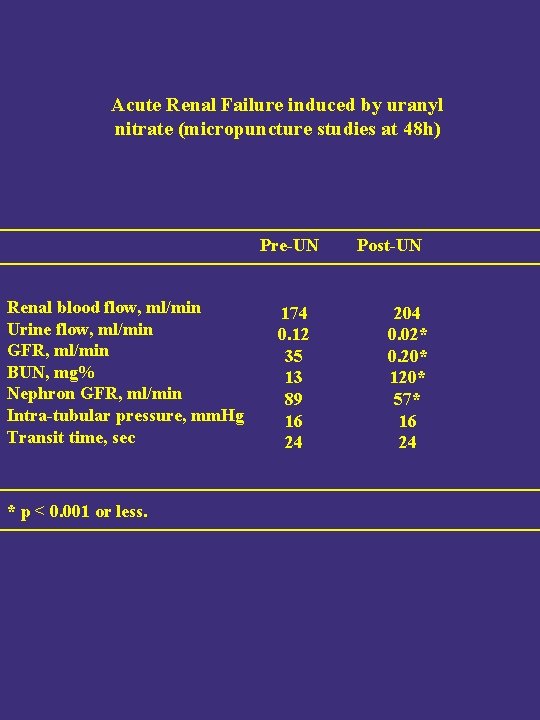
Acute Renal Failure induced by uranyl nitrate (micropuncture studies at 48 h) Pre-UN Renal blood flow, ml/min Urine flow, ml/min GFR, ml/min BUN, mg% Nephron GFR, ml/min Intra-tubular pressure, mm. Hg Transit time, sec * p < 0. 001 or less. 174 0. 12 35 13 89 16 24 Post-UN 204 0. 02* 0. 20* 120* 57* 16 24
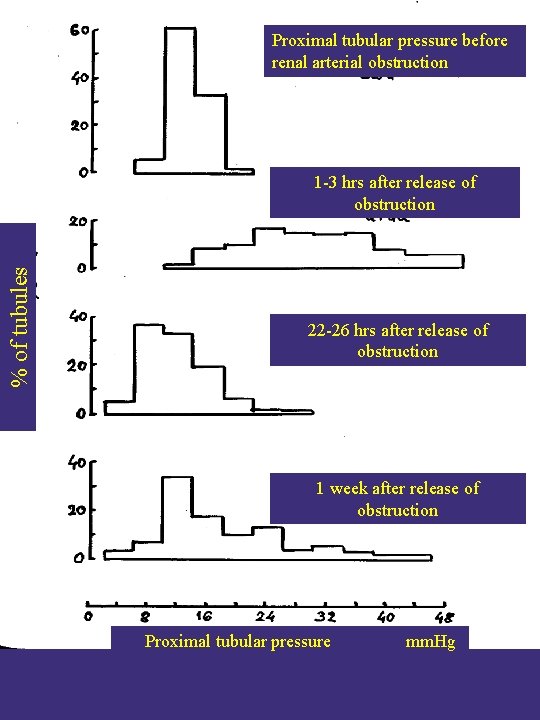
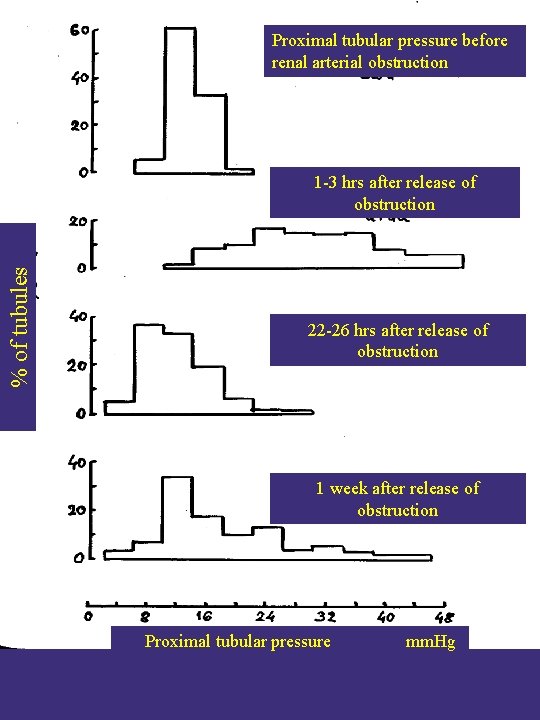
Proximal tubular pressure before renal arterial obstruction % of tubules 1 -3 hrs after release of obstruction 22 -26 hrs after release of obstruction 1 week after release of obstruction Proximal tubular pressure mm. Hg
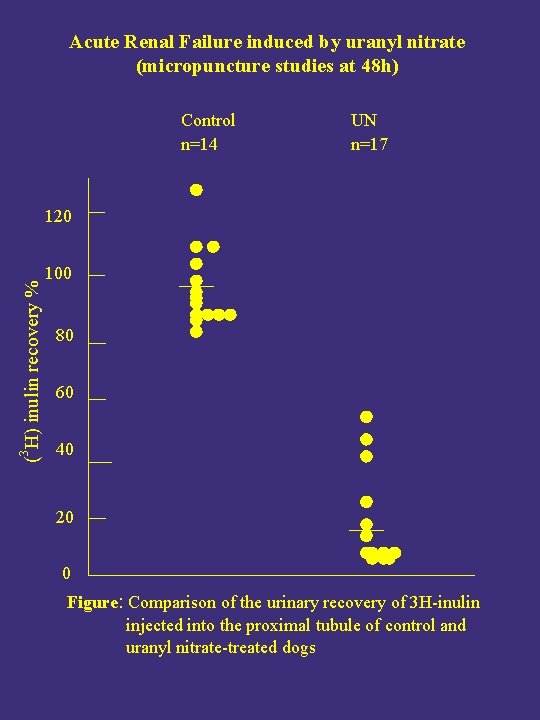
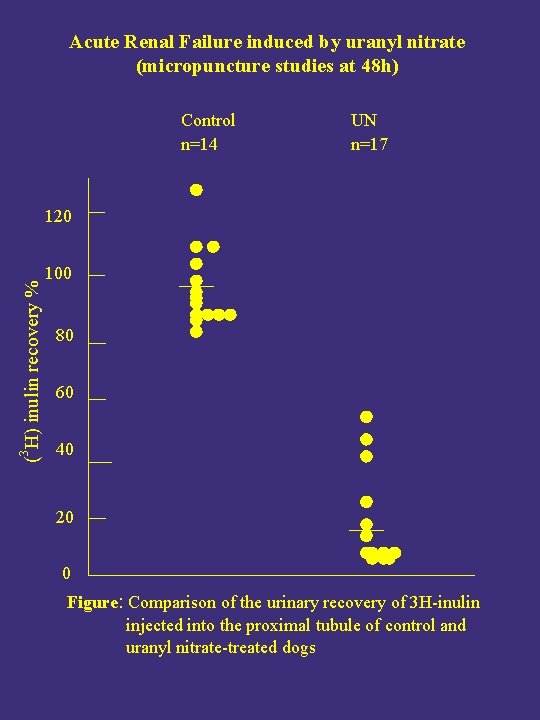
Acute Renal Failure induced by uranyl nitrate (micropuncture studies at 48 h) Control n=14 UN n=17 3 ( H) inulin recovery % 120 100 80 60 40 20 0 Figure: Comparison of the urinary recovery of 3 H-inulin injected into the proximal tubule of control and uranyl nitrate-treated dogs

Nephrons disected from a human kidney during ARF
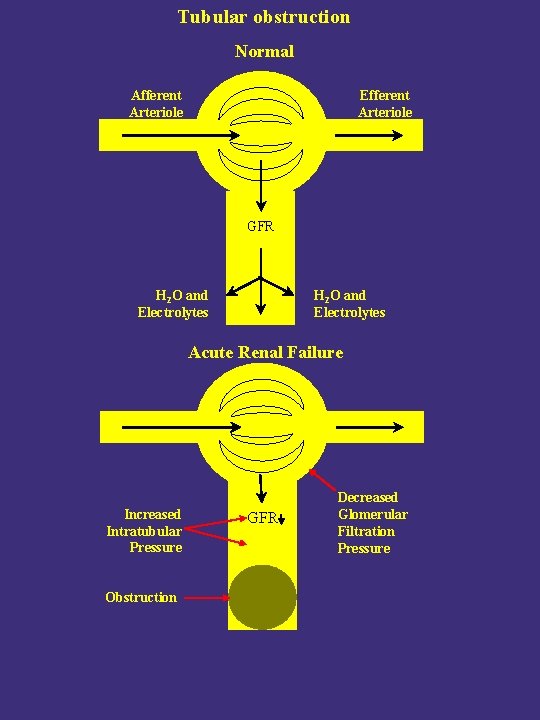
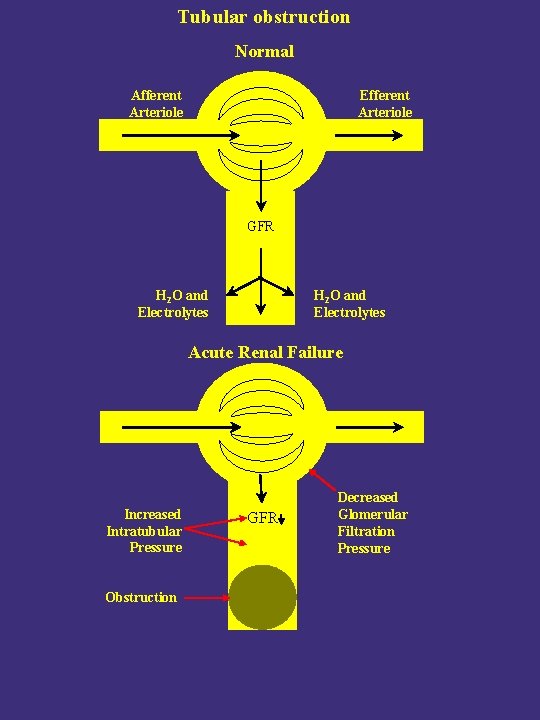
Tubular obstruction Normal Afferent Arteriole Efferent Arteriole GFR H 2 O and Electrolytes Acute Renal Failure Increased Intratubular Pressure Obstruction GFR Decreased Glomerular Filtration Pressure
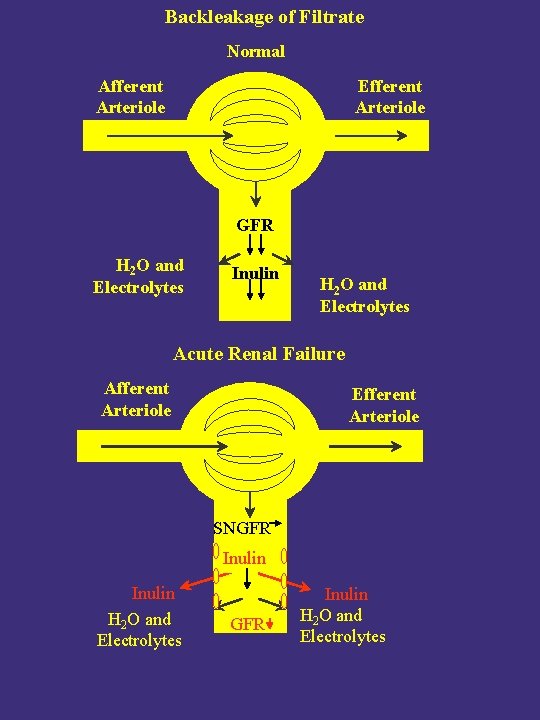
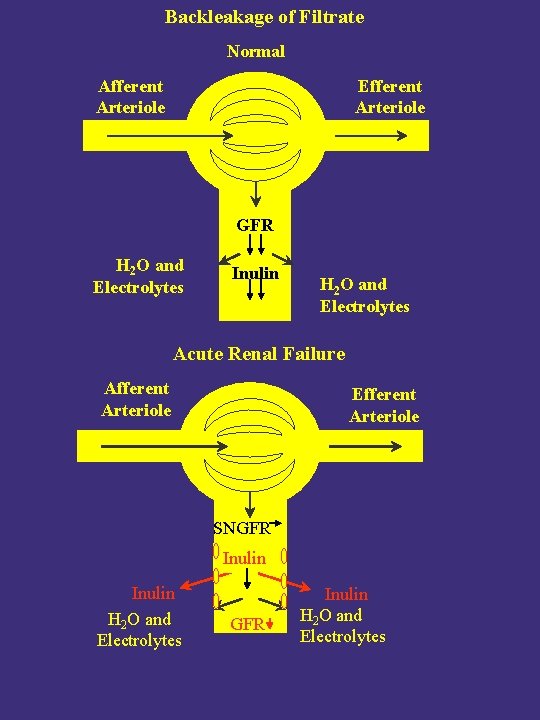
Backleakage of Filtrate Normal Afferent Arteriole Efferent Arteriole GFR H 2 O and Electrolytes Inulin H 2 O and Electrolytes Acute Renal Failure Afferent Arteriole Efferent Arteriole SNGFR Inulin H 2 O and Electrolytes
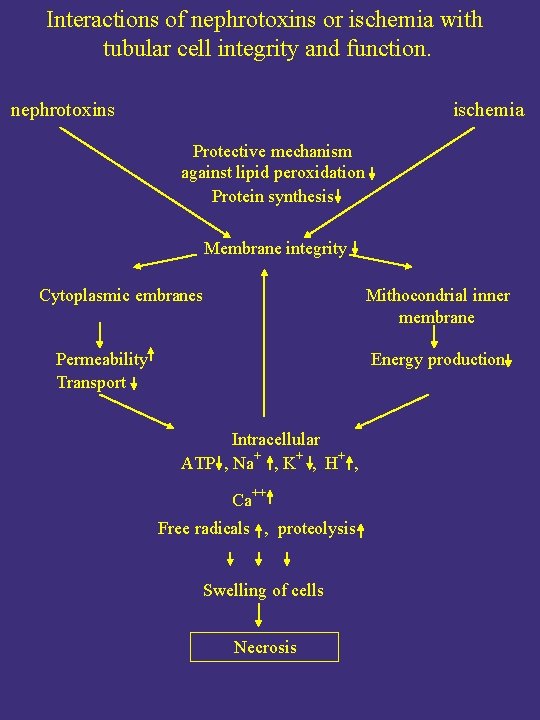
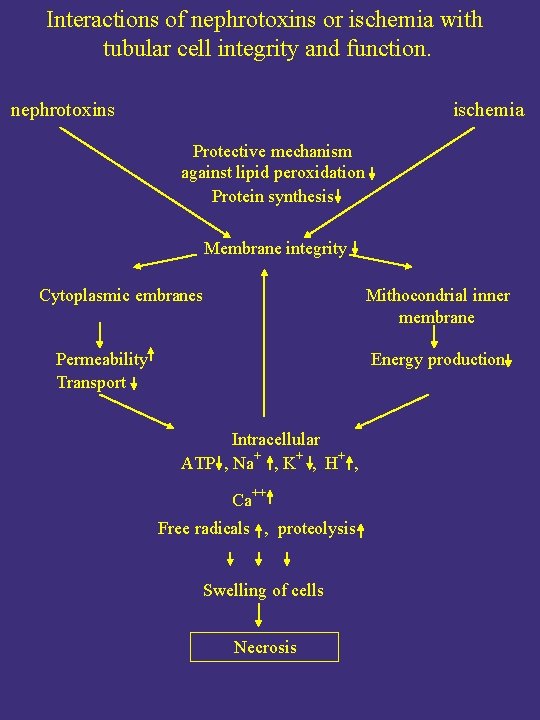
Interactions of nephrotoxins or ischemia with tubular cell integrity and function. nephrotoxins ischemia Protective mechanism against lipid peroxidation Protein synthesis Membrane integrity Cytoplasmic embranes Mithocondrial inner membrane Permeability Transport Energy production Intracellular ATP , Na+ , K+ , H+ , Ca++ Free radicals , proteolysis Swelling of cells Necrosis
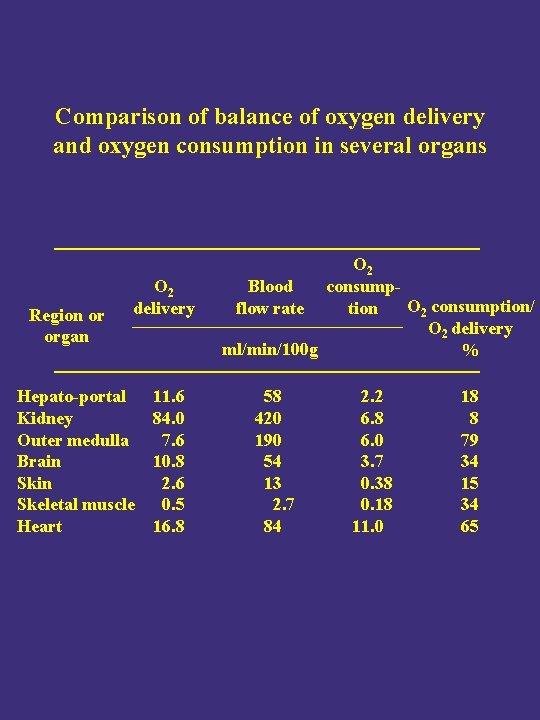
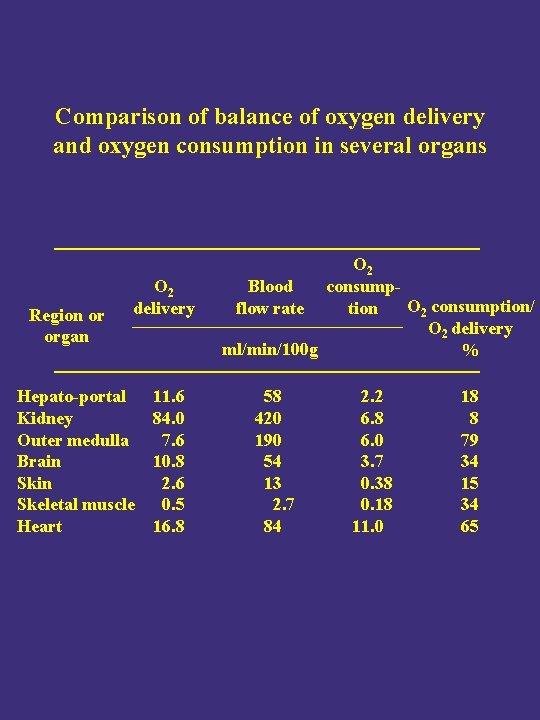
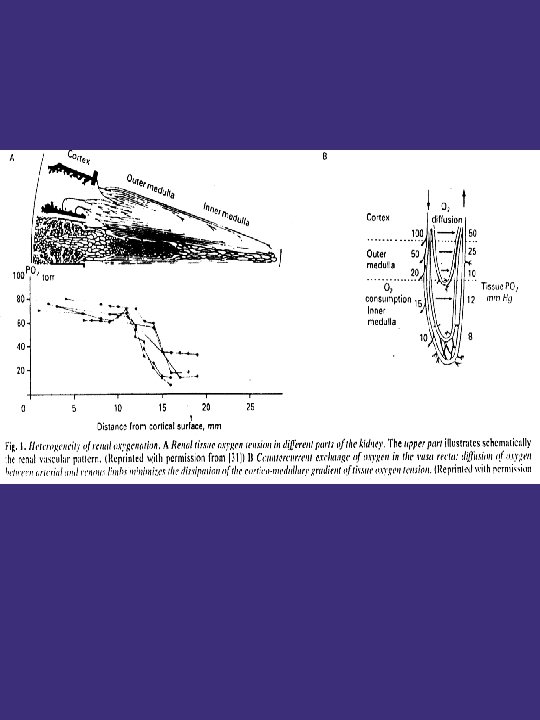
Comparison of balance of oxygen delivery and oxygen consumption in several organs Region or organ O 2 delivery Hepato-portal Kidney Outer medulla Brain Skeletal muscle Heart 11. 6 84. 0 7. 6 10. 8 2. 6 0. 5 16. 8 O 2 consump. Blood O 2 consumption/ tion flow rate O 2 delivery ml/min/100 g % 58 420 190 54 13 2. 7 84 2. 2 6. 8 6. 0 3. 7 0. 38 0. 18 11. 0 18 8 79 34 15 34 65
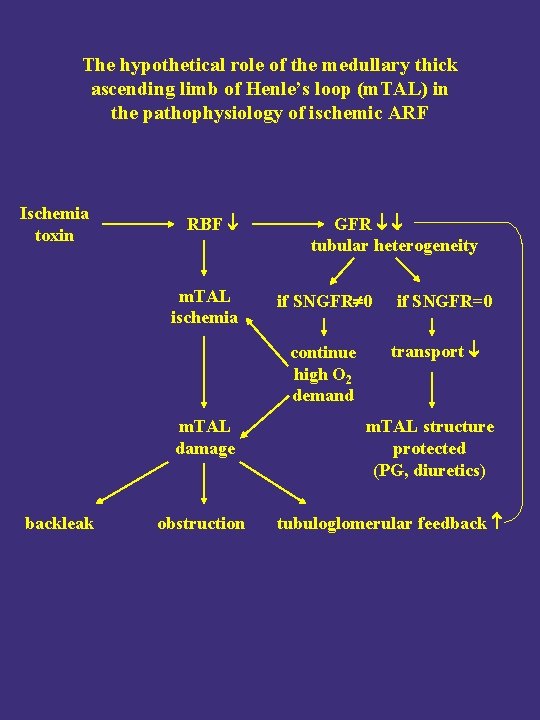
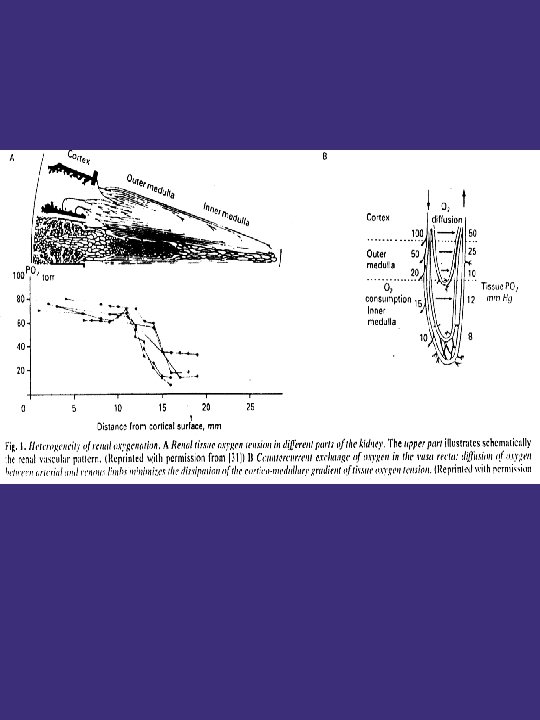
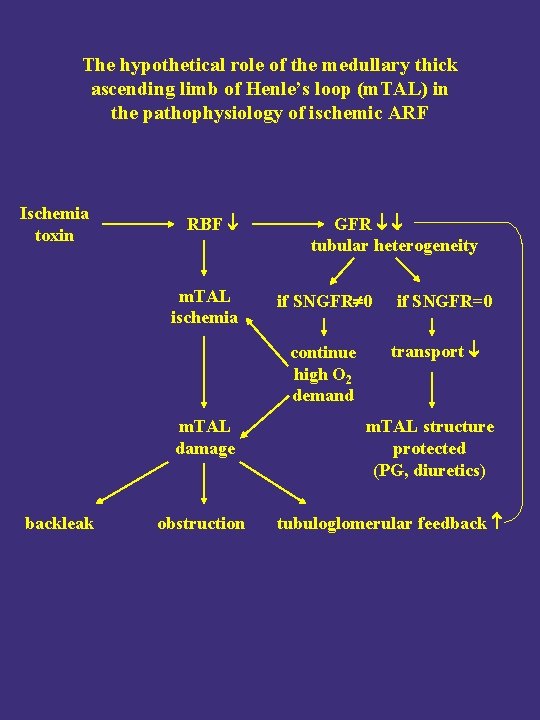
The hypothetical role of the medullary thick ascending limb of Henle’s loop (m. TAL) in the pathophysiology of ischemic ARF Ischemia toxin RBF m. TAL ischemia GFR tubular heterogeneity if SNGFR 0 continue high O 2 demand m. TAL damage backleak obstruction if SNGFR=0 transport m. TAL structure protected (PG, diuretics) tubuloglomerular feedback
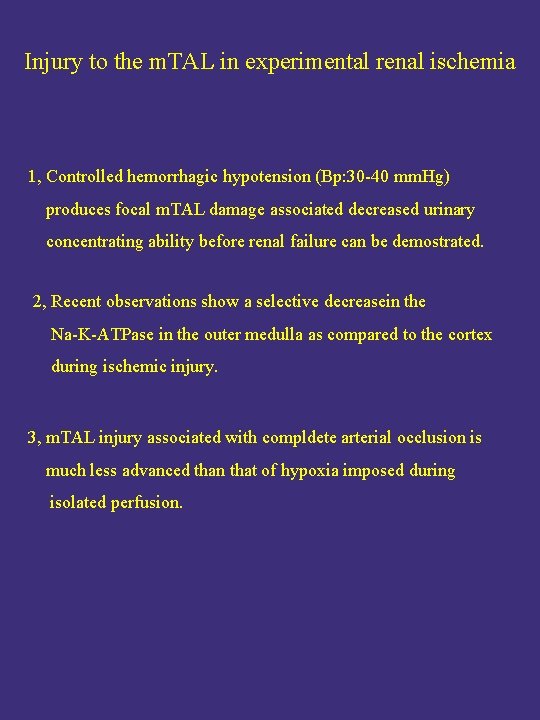
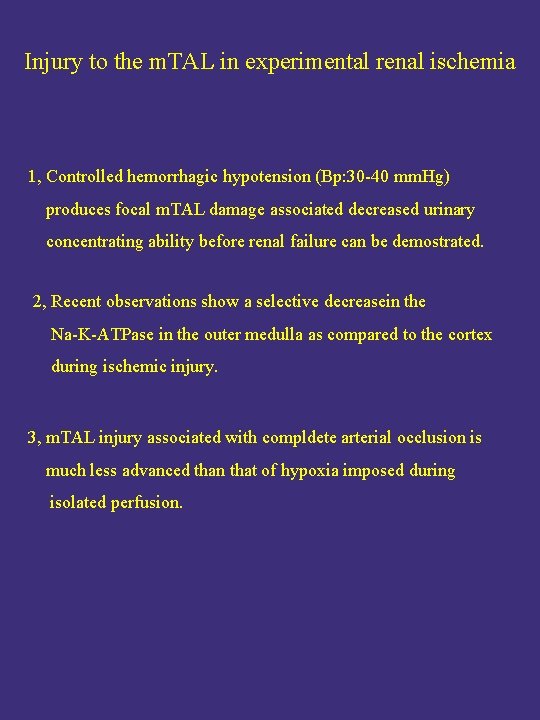
Injury to the m. TAL in experimental renal ischemia 1, Controlled hemorrhagic hypotension (Bp: 30 -40 mm. Hg) produces focal m. TAL damage associated decreased urinary concentrating ability before renal failure can be demostrated. 2, Recent observations show a selective decreasein the Na-K-ATPase in the outer medulla as compared to the cortex during ischemic injury. 3, m. TAL injury associated with compldete arterial occlusion is much less advanced than that of hypoxia imposed during isolated perfusion.
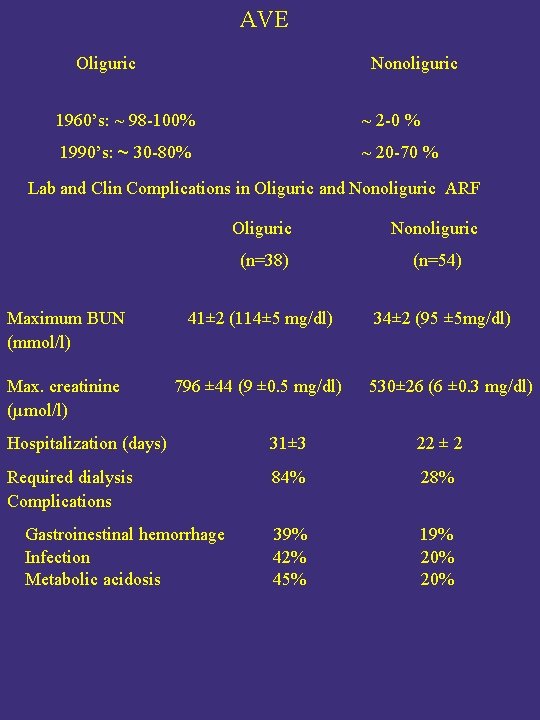
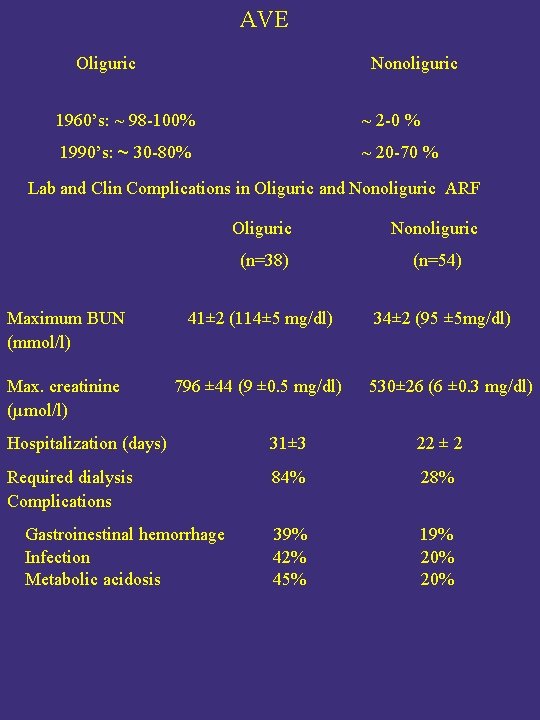
AVE Oliguric Nonoliguric 1960’s: ~ 98 -100% ~ 2 -0 % 1990’s: ~ 30 -80% ~ 20 -70 % Lab and Clin Complications in Oliguric and Nonoliguric ARF Oliguric Nonoliguric (n=38) (n=54) Maximum BUN (mmol/l) 41± 2 (114± 5 mg/dl) 34± 2 (95 ± 5 mg/dl) Max. creatinine (µmol/l) 796 ± 44 (9 ± 0. 5 mg/dl) 530± 26 (6 ± 0. 3 mg/dl) Hospitalization (days) 31± 3 22 ± 2 Required dialysis Complications 84% 28% 39% 42% 45% 19% 20% Gastroinestinal hemorrhage Infection Metabolic acidosis
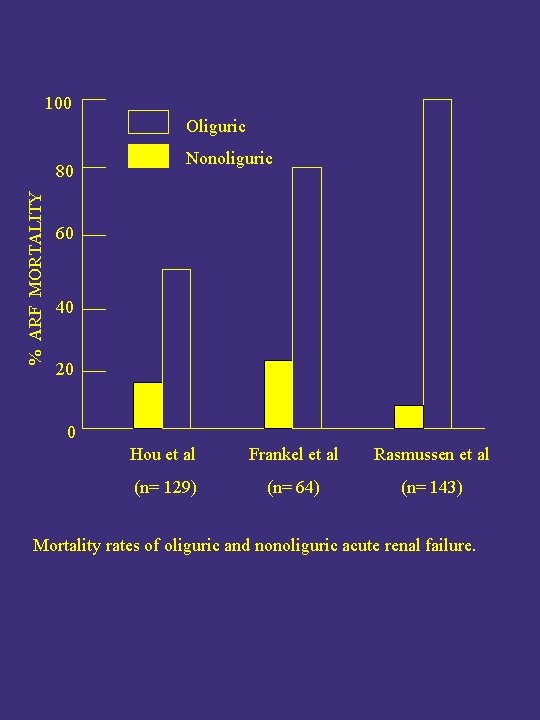
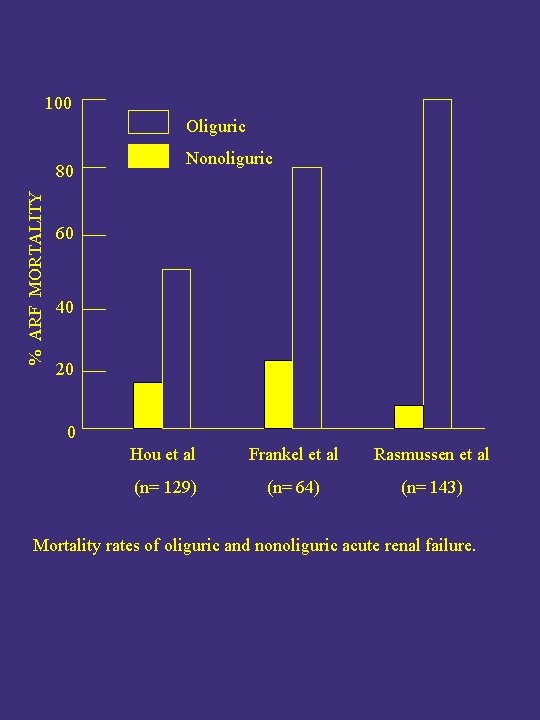
100 Oliguric % ARF MORTALITY 80 Nonoliguric 60 40 20 0 Hou et al Frankel et al Rasmussen et al (n= 129) (n= 64) (n= 143) Mortality rates of oliguric and nonoliguric acute renal failure.
Possible explanations for nonoliguric ARF 1, In some healthy nephronns there are still filtration but there is almost no reabsorption. 2, Decreased medullary osmotic concentration decreased reabsorption of H 2 O