16 Neurological and Psychiatric Disorders Cognitive Neuroscience David


















- Slides: 76
16: Neurological and Psychiatric Disorders Cognitive Neuroscience David Eagleman Jonathan Downar © 2018 1

Chapter Outline • Alzheimer’s Disease: Burning Out with Age? • Frontotemporal Dementia: Like a Cancer of the Soul • Huntington’s Disease: A Genetic Rarity, in Two Senses • Tourette Syndrome: A Case of Involuntary Volition? © 2018 2 2
Chapter Outline • Obsessive-Compulsive Disorder: Neurological or Psychiatric? • Schizophrenia: A Dementia of the Young • Bipolar Disorder • Depression: A Global Burden © 2018 3 3

Alzheimer’s Disease: Burning Out with Age? • Dementias are neurologic disorders characterized by slow deterioration of higher cognitive functions. • Such functions include language, memory, judgement, and emotion. • Alzheimer’s disease or Alzheimer’s dementia is thought to affect about 24 million people world-wide. © 2018 4 4

Alzheimer’s Disease: Burning Out with Age? Figure 16. 2 Subtypes of dementia. Alzheimer’s disease is the most common form of dementia worldwide. 5 © 2018 5
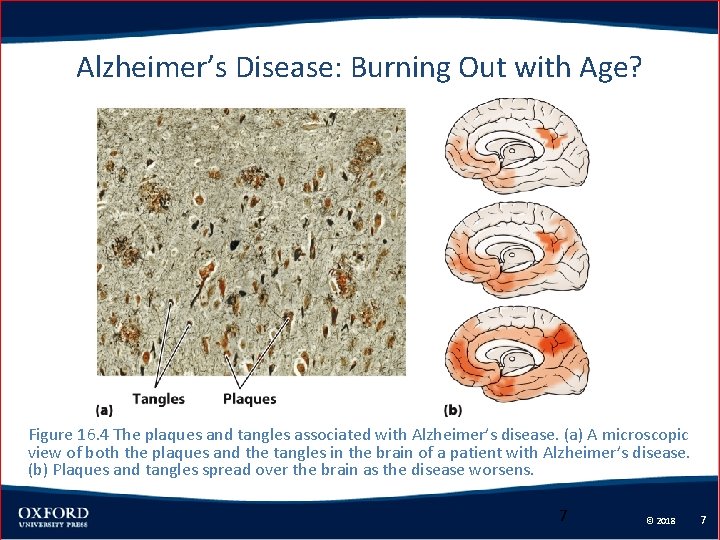
Alzheimer’s Disease: Burning Out with Age? • The major deficit of Alzheimer’s is the loss of episodic memory. • Executive functions decline throughout Alzheimer’s disease. • Biological markers of Alzheimer’s disease include amyloid-beta plaques and neurofibrillary tau tangles. © 2018 6 6
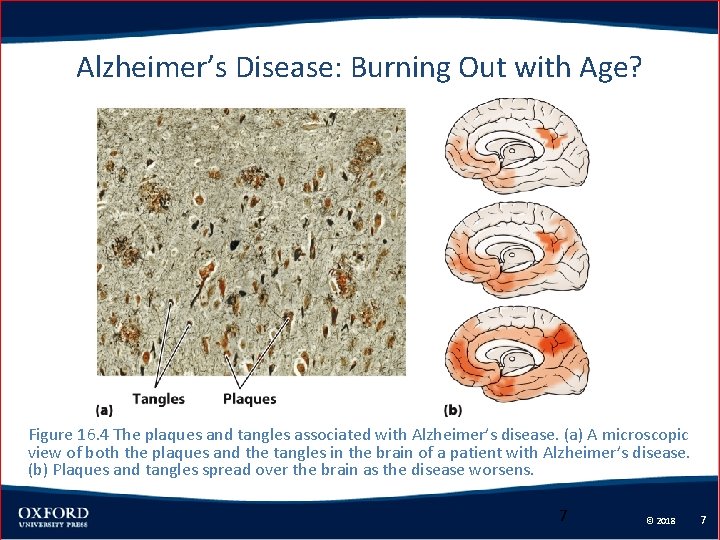
Alzheimer’s Disease: Burning Out with Age? Figure 16. 4 The plaques and tangles associated with Alzheimer’s disease. (a) A microscopic view of both the plaques and the tangles in the brain of a patient with Alzheimer’s disease. (b) Plaques and tangles spread over the brain as the disease worsens. 7 © 2018 7
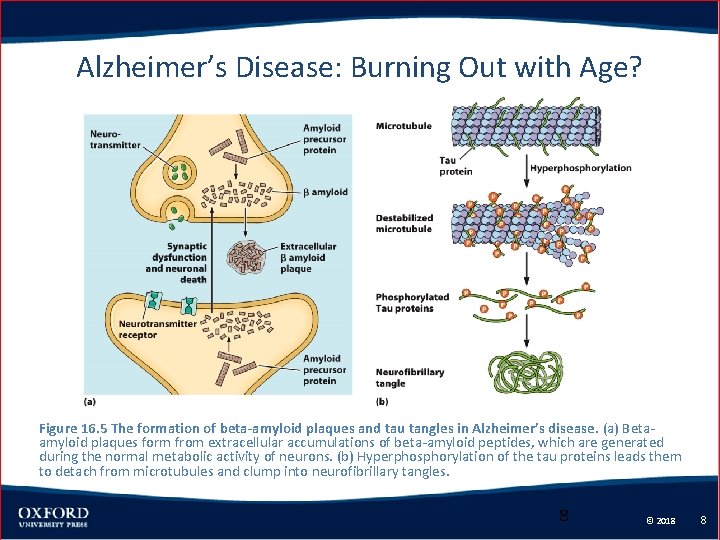
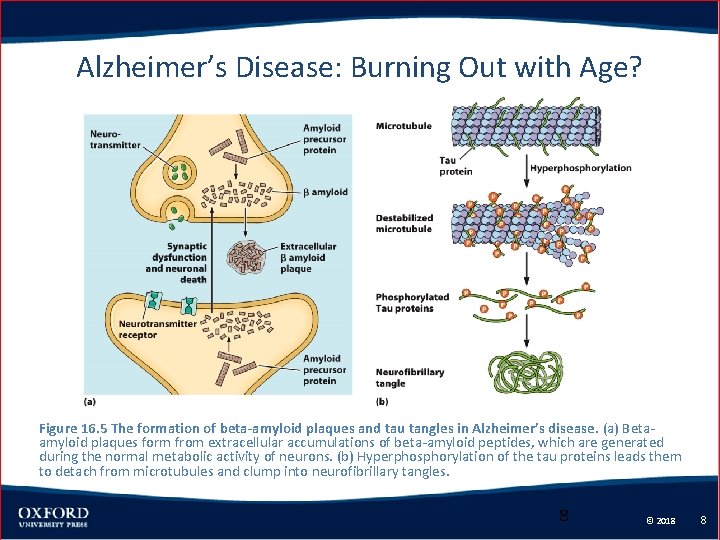
Alzheimer’s Disease: Burning Out with Age? Figure 16. 5 The formation of beta-amyloid plaques and tau tangles in Alzheimer’s disease. (a) Betaamyloid plaques form from extracellular accumulations of beta-amyloid peptides, which are generated during the normal metabolic activity of neurons. (b) Hyperphosphorylation of the tau proteins leads them to detach from microtubules and clump into neurofibrillary tangles. 8 © 2018 8
Alzheimer’s Disease: Burning Out with Age? • Most cases of Alzheimer’s disease occur in individuals over age 60. • The epsilon 4 variant of the apolipoprotein E (Apo. E 4) gene seems to increase the risk of developing the disease. • Genetic forms of Alzheimer’s disease account for only a small percentage of cases. © 2018 9 9
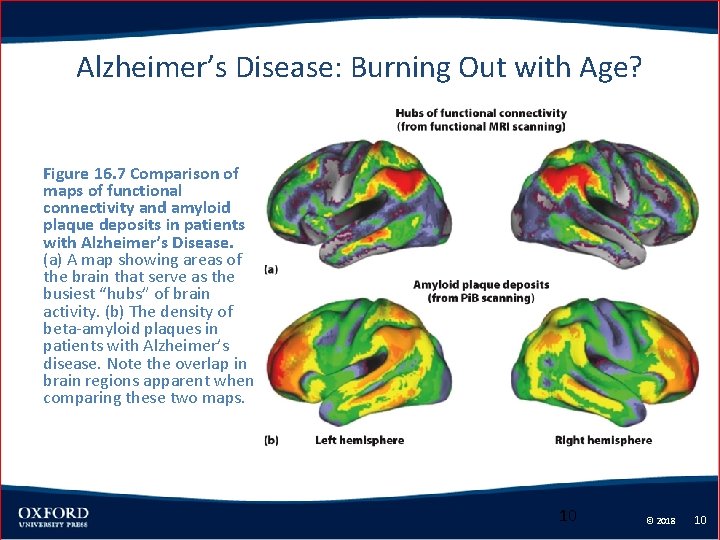
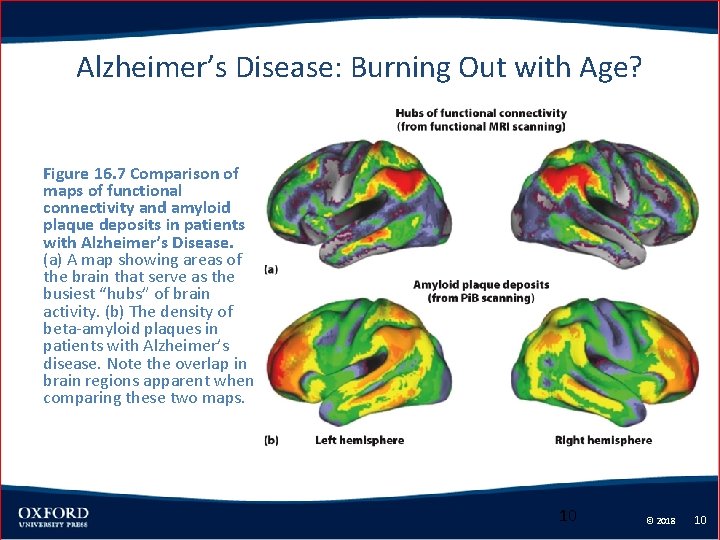
Alzheimer’s Disease: Burning Out with Age? Figure 16. 7 Comparison of maps of functional connectivity and amyloid plaque deposits in patients with Alzheimer’s Disease. (a) A map showing areas of the brain that serve as the busiest “hubs” of brain activity. (b) The density of beta-amyloid plaques in patients with Alzheimer’s disease. Note the overlap in brain regions apparent when comparing these two maps. 10 © 2018 10
Alzheimer’s Disease: Burning Out with Age? • Treatment of Alzheimer’s disease – There are currently no cures for Alzheimer’s disease. – No medications significantly slow down or reverse the progression of the disease. – Acetylcholinesterase inhibitors and NMDA glutamate receptor antagonists sometimes slow the progression of the disease. © 2018 11 11
Alzheimer’s Disease: Burning Out with Age? • A potential treatment uses the immune system to remove plaques, but this has not resulted in any clinical improvement. • Social, mental, and physical activity can decrease the risk and severity of Alzheimer’s disease. © 2018 12 12
Frontotemporal Dementia: Like a Cancer of the Soul • This dementia results from progressive atrophy of the brain. • This is most common in the inferior frontal lobes and anterior temporal lobe. • The age of onset is typically about 40 – 50 years of age. • Personality and social behaviors change significantly. © 2018 13 13

Frontotemporal Dementia: Like a Cancer of the Soul Figure 16. 8 In patients with frontotemporal dementia, the frontal lobes and temporal pole degenerate, leaving smaller gyri and larger sulci. 14 © 2018 14
Frontotemporal Dementia: Like a Cancer of the Soul • Behavioral variant frontotemporal dementia (bv. FTD) is most common. • This is characterized by progressive semantic dementia, personality changes and loss of empathy. • Frontotemporal dementia is sometimes associated with an increase in creativity. © 2018 15 15
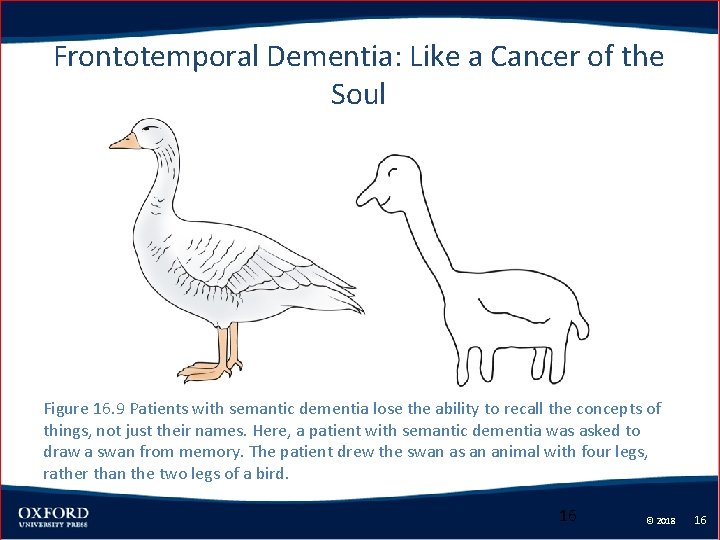
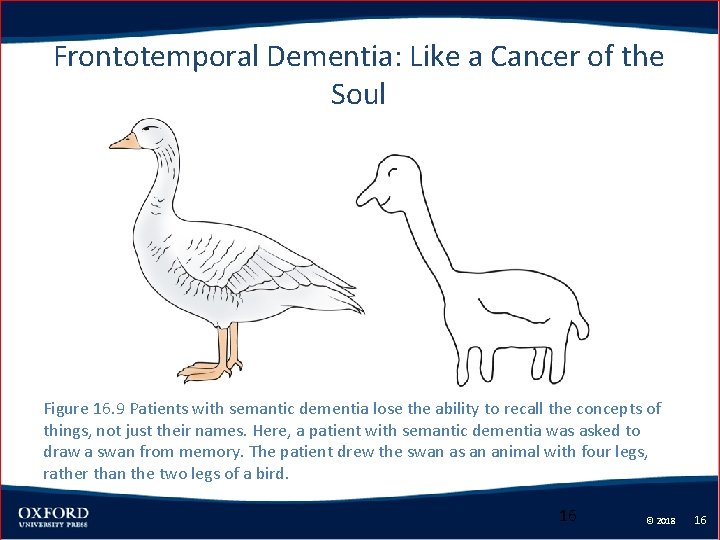
Frontotemporal Dementia: Like a Cancer of the Soul Figure 16. 9 Patients with semantic dementia lose the ability to recall the concepts of things, not just their names. Here, a patient with semantic dementia was asked to draw a swan from memory. The patient drew the swan as an animal with four legs, rather than the two legs of a bird. 16 © 2018 16

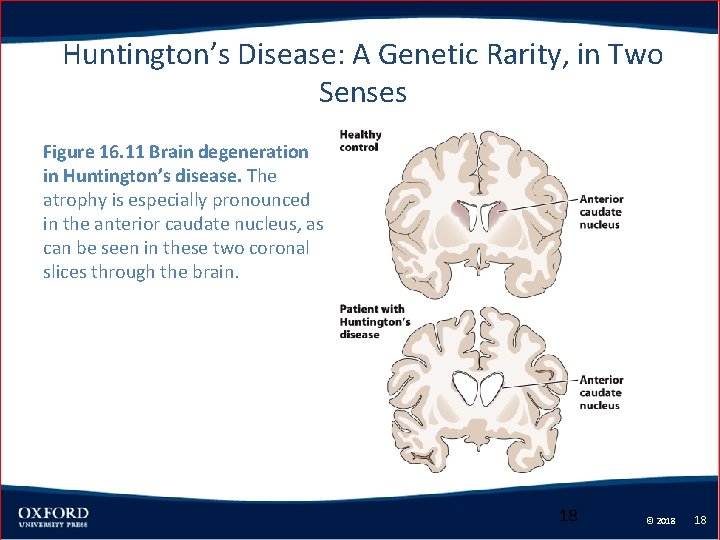
Huntington’s Disease: A Genetic Rarity, in Two Senses • Patients perform restless involuntary movements of the face, trunk, and limbs. • It commonly also includes psychiatric symptoms such as depression, apathy, anxiety, delusions, and hallucinations. • The biological cause is degeneration of the anterior caudate nucleus of the striatum. © 2018 17 17
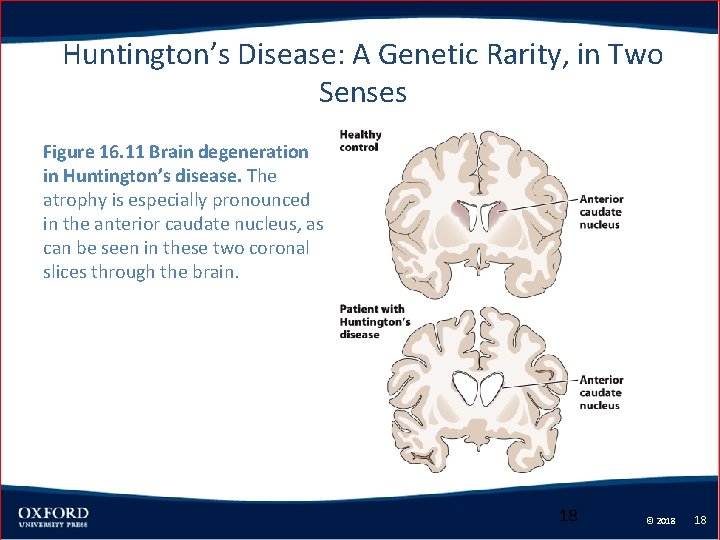
Huntington’s Disease: A Genetic Rarity, in Two Senses Figure 16. 11 Brain degeneration in Huntington’s disease. The atrophy is especially pronounced in the anterior caudate nucleus, as can be seen in these two coronal slices through the brain. 18 © 2018 18
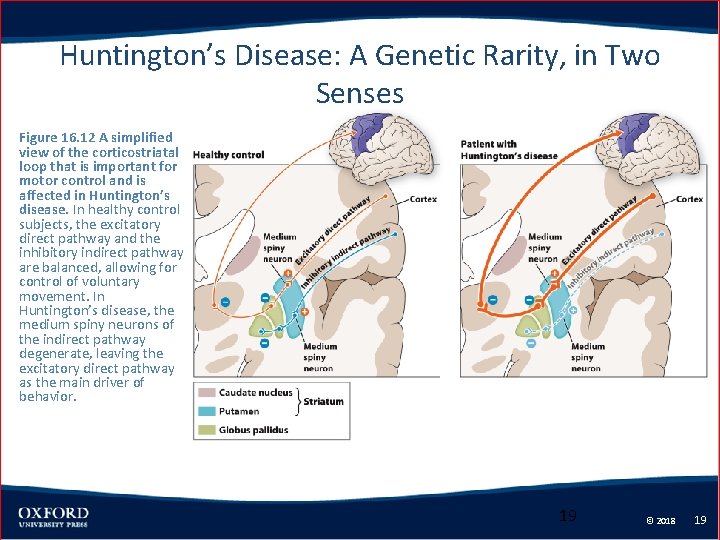
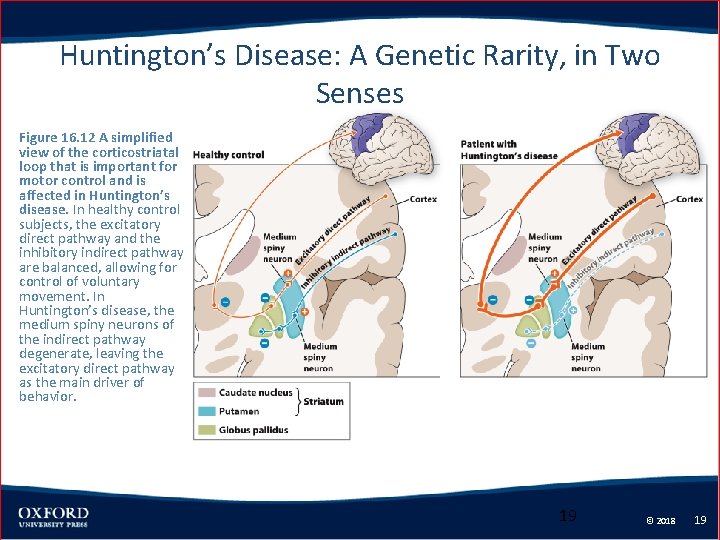
Huntington’s Disease: A Genetic Rarity, in Two Senses Figure 16. 12 A simplified view of the corticostriatal loop that is important for motor control and is affected in Huntington’s disease. In healthy control subjects, the excitatory direct pathway and the inhibitory indirect pathway are balanced, allowing for control of voluntary movement. In Huntington’s disease, the medium spiny neurons of the indirect pathway degenerate, leaving the excitatory direct pathway as the main driver of behavior. 19 © 2018 19
Huntington’s Disease: A Genetic Rarity, in Two Senses • Huntington’s disease is caused by the mutation of an autosomal dominant gene. • This mutation encodes the inclusion of a trinucleotide repeat of the sequence CAG in the final protein. – Most people have fewer than 28 CAG repeats, and this results in no issues. – Individuals with more than 35 repeats are at an increased risk of developing the disease. © 2018 20 20

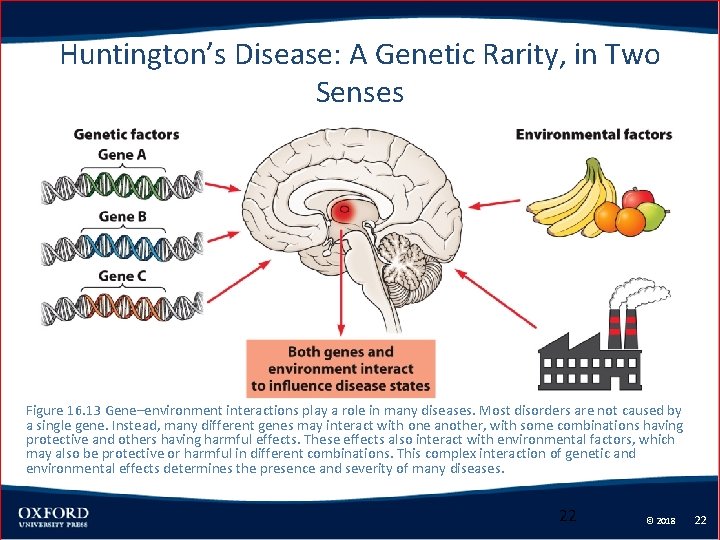
Huntington’s Disease: A Genetic Rarity, in Two Senses • Risk factors for Huntington’s disease include both genetic and environmental factors. • Treatment for Huntington’s disease involves dopamine receptor antagonists. • These relieve some of the motor and psychiatric symptoms. © 2018 21 21
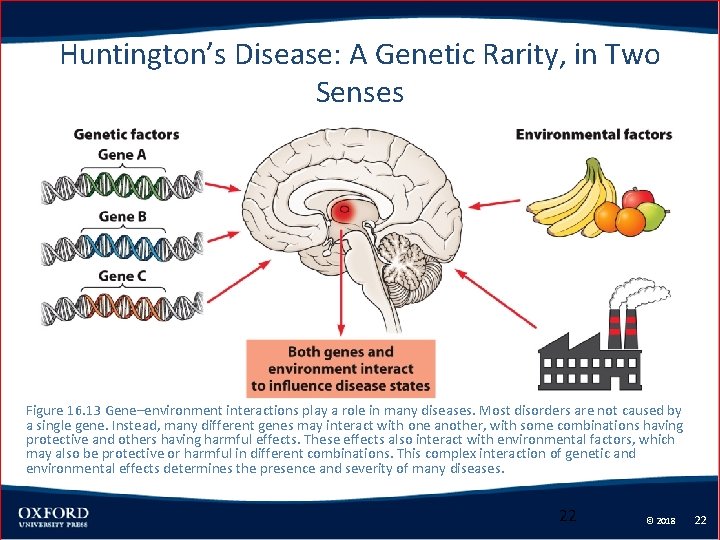
Huntington’s Disease: A Genetic Rarity, in Two Senses Figure 16. 13 Gene–environment interactions play a role in many diseases. Most disorders are not caused by a single gene. Instead, many different genes may interact with one another, with some combinations having protective and others having harmful effects. These effects also interact with environmental factors, which may also be protective or harmful in different combinations. This complex interaction of genetic and environmental effects determines the presence and severity of many diseases. 22 © 2018 22
Tourette Syndrome: A Case of Involuntary Volition? • In Tourette syndrome, the individual repeats purposeless movements of the face, head, shoulders, or hands. • There also verbal tics, which are purposeless noises like throat-clearing and snorting or meaningless phrases. © 2018 23 23
Tourette Syndrome: A Case of Involuntary Volition? • Tourette syndrome is typically a disorder of childhood. • Studies suggest there is a genetic basis to Tourette syndrome, but no gene has been isolated. © 2018 24 24
Tourette Syndrome: A Case of Involuntary Volition? • Pediatric Autoimmune Neuropsychiatric Disorder Associated with group A Streptococcal infection (PANDAS) – This is characterized by the tics of Tourette syndrome or the intrusive thoughts and behaviors of obsessive compulsive disorder. – Sometimes occurs in patients shortly after they have had a throat infection caused by the bacteria Group A streptococcus. © 2018 25 25
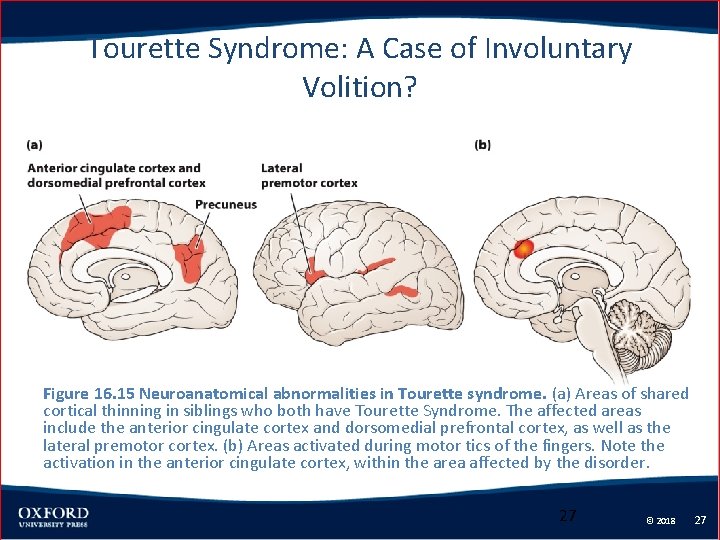
Tourette Syndrome: A Case of Involuntary Volition? • Patients have a decrease in gray matter in the caudate nucleus and lateral motor and premotor cortex. • Gray matter is thinner in medial motor areas. © 2018 26 26
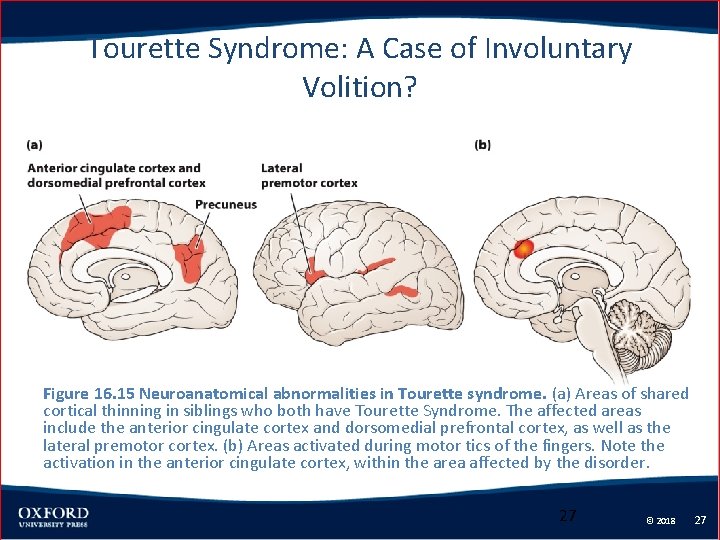
Tourette Syndrome: A Case of Involuntary Volition? Figure 16. 15 Neuroanatomical abnormalities in Tourette syndrome. (a) Areas of shared cortical thinning in siblings who both have Tourette Syndrome. The affected areas include the anterior cingulate cortex and dorsomedial prefrontal cortex, as well as the lateral premotor cortex. (b) Areas activated during motor tics of the fingers. Note the activation in the anterior cingulate cortex, within the area affected by the disorder. 27 © 2018 27
Tourette Syndrome: A Case of Involuntary Volition? • Therapy for Tourette syndrome includes education and acceptance. • Neurolepic medications are prescribed for the most severe cases, where the tics interfere significantly with daily life. © 2018 28 28
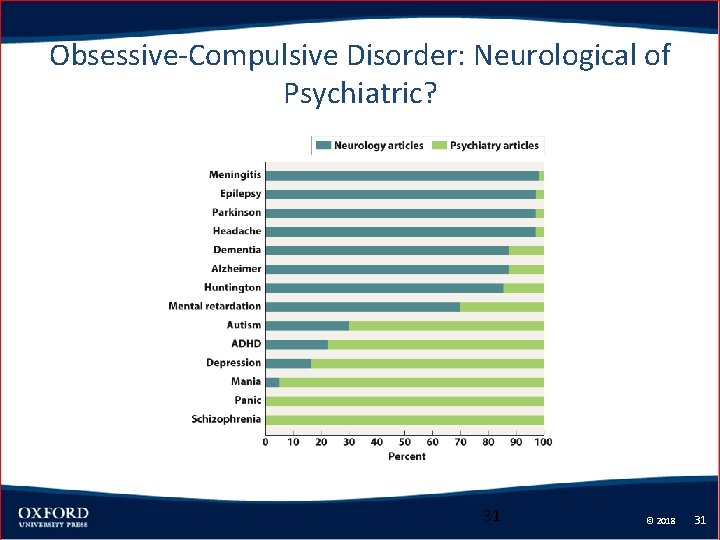
Obsessive-Compulsive Disorder: Neurological of Psychiatric? • “Neurological” disorders and “psychiatric” disorders are grouped based on the nature of the condition. • Conditions with an observable brain abnormality were considered neurological. © 2018 29 29

Obsessive-Compulsive Disorder: Neurological of Psychiatric? • A more modern criteria based on the symptoms. – Psychiatric conditions impact emotion, motivation, social behaviors, personality, or reality testing. – Neurological conditions impact strength, movement, sensory perception, memory, attention, or level of consciousness. © 2018 30 30
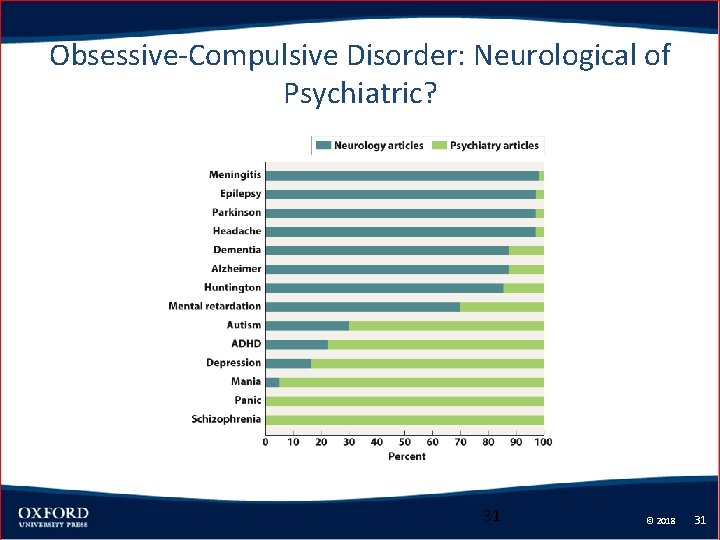
Obsessive-Compulsive Disorder: Neurological of Psychiatric? 31 © 2018 31
Obsessive-Compulsive Disorder: Neurological of Psychiatric? • Obsessive-compulsive disorder is a psychiatric disorder that affects about 2 – 3% of the population. • Symptoms include obsessions (intrusive, disturbing thoughts) and compulsions (stereotyped, ritualized behaviors). © 2018 32 32
Obsessive-Compulsive Disorder: Neurological of Psychiatric? • Obsessions include contamination, fear of committing inappropriate acts, symmetry and number, and hoarding. • The most common age of onset for symptoms of obsessive-compulsive disorder is either about age 11 or 23. © 2018 33 33

Obsessive-Compulsive Disorder: Neurological of Psychiatric? Figure 16. 18 Two corticostriatal loops are consistently identified as important in studies of patients with OCD. One of the loops goes from the anterior caudate nucleus to the dorsomedial prefrontal cortex and nearby anterior cingulate cortex. The other loop goes from the ventral striatum to the lateral orbitofrontal cortex. These loop circuits tend to show excessive activity in OCD compared to healthy controls. 34 © 2018 34
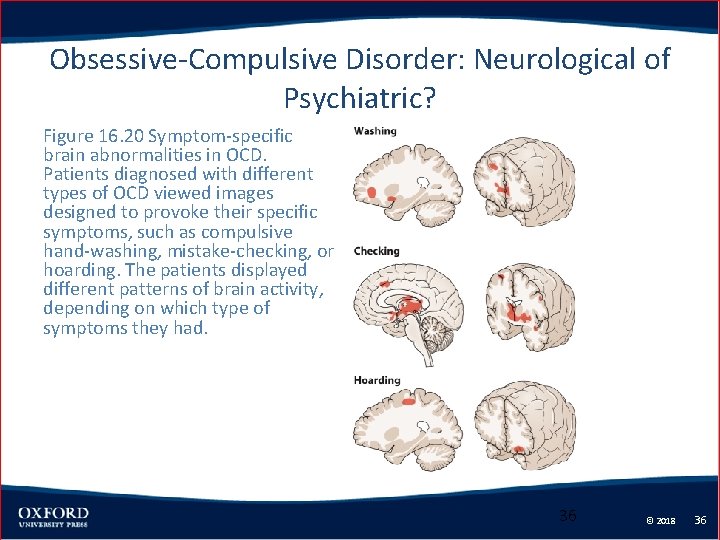
Obsessive-Compulsive Disorder: Neurological of Psychiatric? • There is increased activity in the circuits connecting the basal ganglia to the orbitofrontal, anterior cingulate, and dorsomedial prefrontal cortex. • The pattern of activity differs depending on the types of obsession. © 2018 35 35
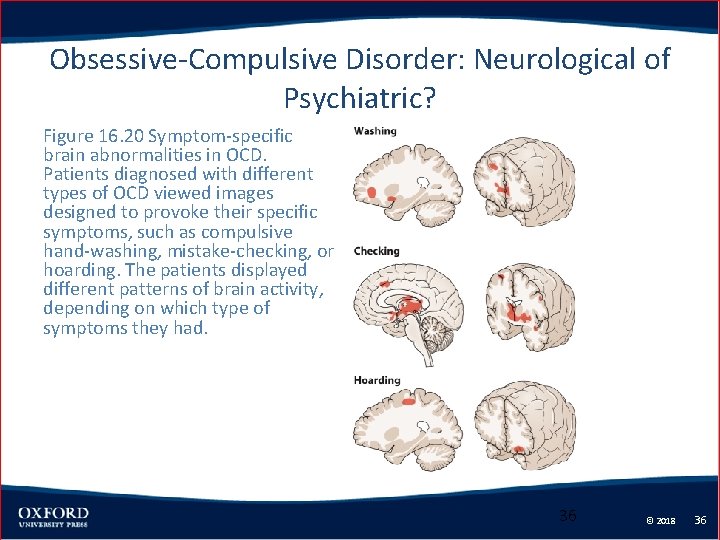
Obsessive-Compulsive Disorder: Neurological of Psychiatric? Figure 16. 20 Symptom-specific brain abnormalities in OCD. Patients diagnosed with different types of OCD viewed images designed to provoke their specific symptoms, such as compulsive hand-washing, mistake-checking, or hoarding. The patients displayed different patterns of brain activity, depending on which type of symptoms they had. 36 © 2018 36
Obsessive-Compulsive Disorder: Neurological of Psychiatric? • Cognitive behavioral therapy addresses cognitive distortions and decreases anxiety. • Medications than increase serotonin reduce the obsessions, compulsions, and anxiety. • Neuroleptics are sometime prescribed for severe cases. © 2018 37 37

Schizophrenia: A Dementia of the Young • Schizophrenia is characterized by loss of contact with reality. • The age of onset is typically around early adulthood. • Schizophrenia affects about 1% of the world’s population. © 2018 38 38
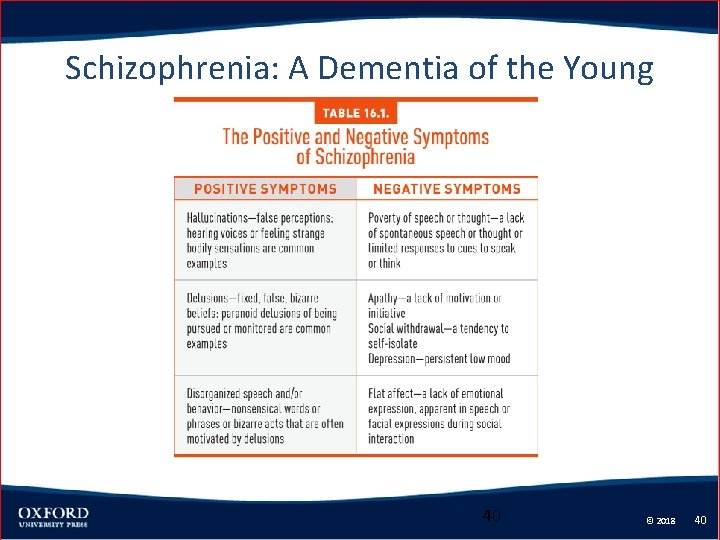
Schizophrenia: A Dementia of the Young • Positive symptoms include hallucinations and delusions. – Delusions include paranoid delusions, delusions of reference, delusions of passivity, and somatic delusions. • Negative symptoms include poverty of speech, apathy, social withdrawal, and loss of emotion. © 2018 39 39
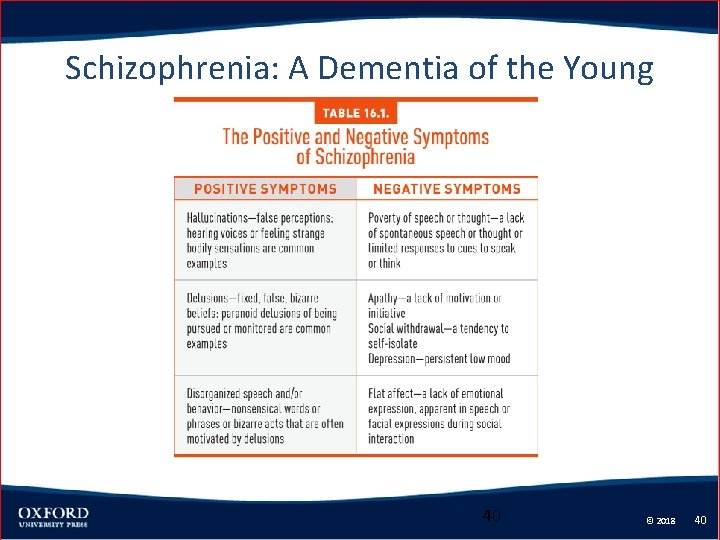
Schizophrenia: A Dementia of the Young 40 © 2018 40
Schizophrenia: A Dementia of the Young • Antipsychotic medications treat the positive symptoms, but do not treat the negative symptoms. • Such medications often cause unwanted side effects. • Second-generation antipsychotic medications are no better at treating the negative symptoms. © 2018 41 41
Schizophrenia: A Dementia of the Young • There is a genetic basis to schizophrenia, but no specific genes have been identified. • Environmental factors during fetal development or early life seem important in the incidence of schizophrenia. © 2018 42 42

Schizophrenia: A Dementia of the Young Figure 16. 22 A family pedigree of the DISC 1 gene. This pedigree shows five generations of a family known to carry the DISC 1 mutation. Individuals with the mutation are marked with a dot, and individuals with a known diagnosis are indicated by a color code. Note that the same genetic mutation leads to different types of mental illness in different individuals, and that not everyone who carries the mutation has an illness; this illustrates the importance of gene–gene and gene–environment interactions. 43 © 2018 43
Schizophrenia: A Dementia of the Young • Neurodevelopmental factors – Abnormal pruning of neurons – Smaller cell bodies of neurons – Decreased functioning of inhibitory GABA interneurons in the cortex © 2018 44 44

Schizophrenia: A Dementia of the Young Figure 16. 23 Compared with healthy control subjects, individuals with schizophrenia show a decrease in gray matter over time. The abnormal loss of gray matter usually begins in adolescence, well before the symptoms of psychosis become prominent in early adulthood. 45 © 2018 45

Schizophrenia: A Dementia of the Young Figure 16. 24 The hypothesis of abnormal neuron migration in schizophrenia. If neurons fail to migrate to the correct layers of the cortex during development, they may not connect or communicate properly. In some studies of the layers of cortex in individuals with schizophrenia, the GABAergic interneurons fail to migrate to the correct location. This disrupts the circuitry of the cortex at a microscopic level. 46 © 2018 46
Schizophrenia: A Dementia of the Young • Dopamine hypothesis – There is too much dopamine signaling or the dopamine receptors are oversensitive. – The first-generation antipsychotic drugs were dopamine D 2 receptor antagonists. – Drugs that increase dopamine, such as amphetamines and cocaine, can mimic the positive symptoms of schizophrenia. © 2018 47 47
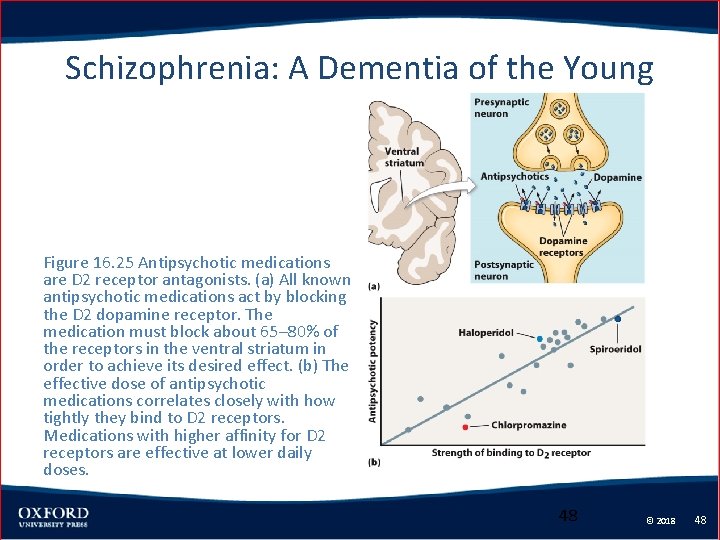
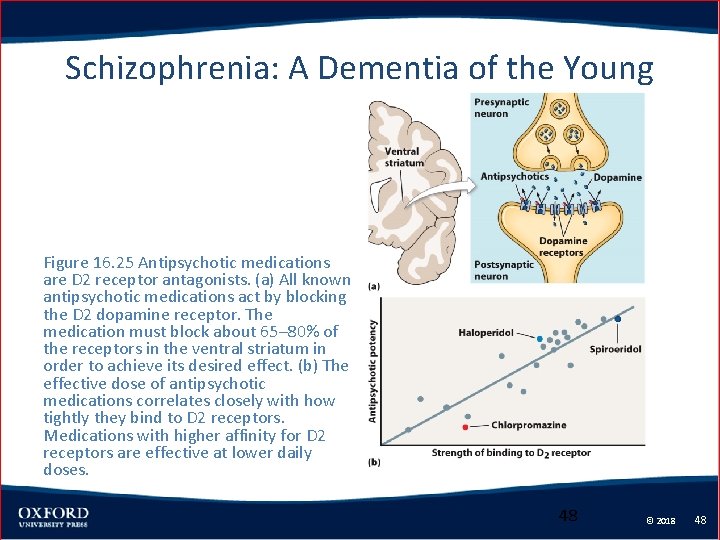
Schizophrenia: A Dementia of the Young Figure 16. 25 Antipsychotic medications are D 2 receptor antagonists. (a) All known antipsychotic medications act by blocking the D 2 dopamine receptor. The medication must block about 65– 80% of the receptors in the ventral striatum in order to achieve its desired effect. (b) The effective dose of antipsychotic medications correlates closely with how tightly they bind to D 2 receptors. Medications with higher affinity for D 2 receptors are effective at lower daily doses. 48 © 2018 48
Schizophrenia: A Dementia of the Young • Glutamate hypothesis – Schizophrenia is caused by too little glutamate neurotransmission. – NMDA receptor antagonists, like ketamine, can mimic both the positive and negative symptoms of schizophrenia. – Many of the genes associated with schizophrenia affect NMDA glutamate receptors. © 2018 49 49
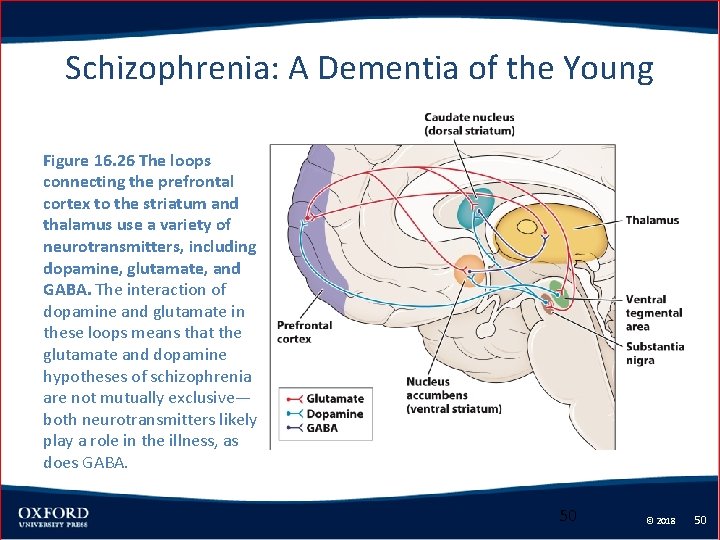
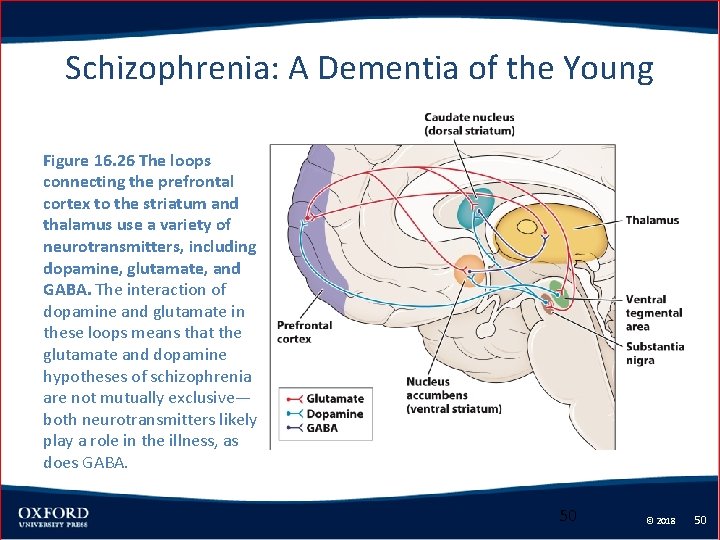
Schizophrenia: A Dementia of the Young Figure 16. 26 The loops connecting the prefrontal cortex to the striatum and thalamus use a variety of neurotransmitters, including dopamine, glutamate, and GABA. The interaction of dopamine and glutamate in these loops means that the glutamate and dopamine hypotheses of schizophrenia are not mutually exclusive— both neurotransmitters likely play a role in the illness, as does GABA. 50 © 2018 50
Bipolar Disorder • Normal mood alternates with periods of depression and mania. • This affects 1% of the population and a milder form may affect as much as 4 -5% of the population. • The age of onset is about 20 years of age. • There is a genetic basis to the condition, but no specific genes have been identified. © 2018 51 51
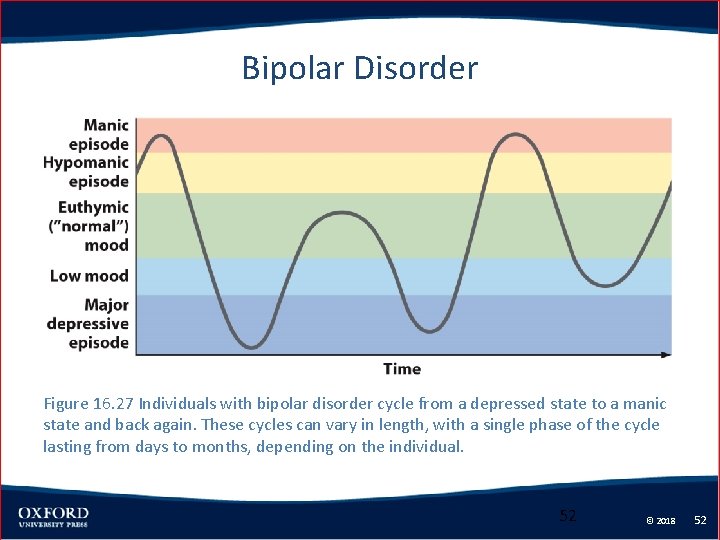
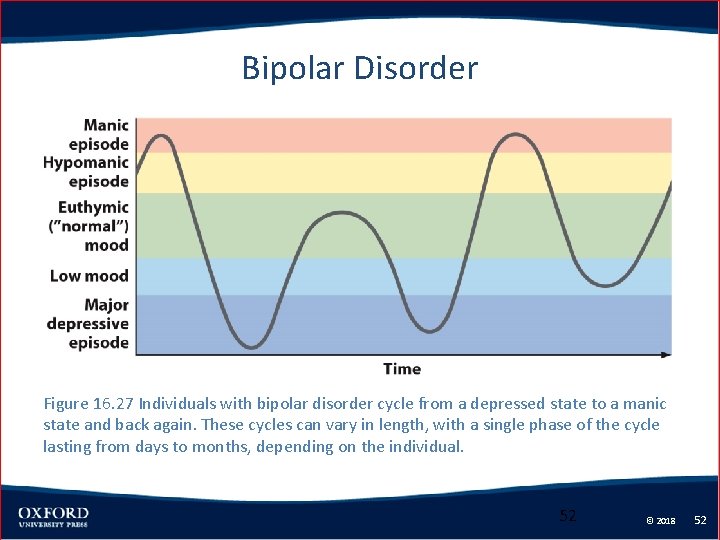
Bipolar Disorder Figure 16. 27 Individuals with bipolar disorder cycle from a depressed state to a manic state and back again. These cycles can vary in length, with a single phase of the cycle lasting from days to months, depending on the individual. 52 © 2018 52
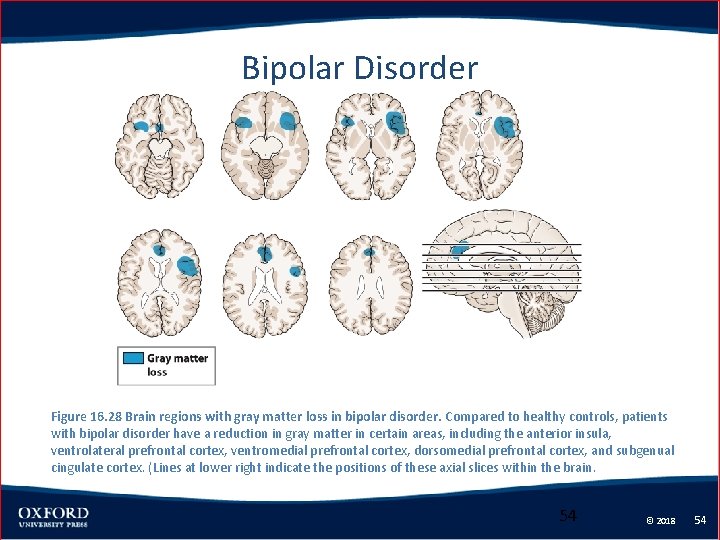
Bipolar Disorder • Individuals with bipolar disorder show thinner gray matter in the – Bilateral ventrolateral frontal cortex – Bilateral anterior insula Dorsomedial prefrontal cortex – Subgenual cingulate cortex • Some of these regions are also affected in unipolar depression. © 2018 53 53
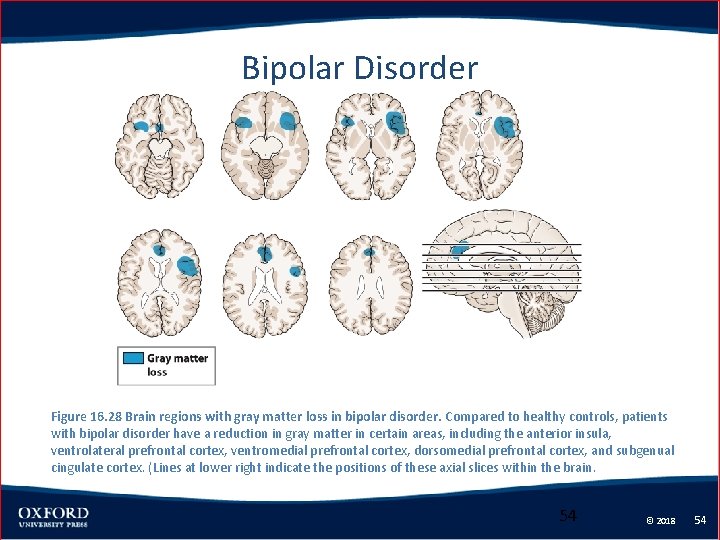
Bipolar Disorder Figure 16. 28 Brain regions with gray matter loss in bipolar disorder. Compared to healthy controls, patients with bipolar disorder have a reduction in gray matter in certain areas, including the anterior insula, ventrolateral prefrontal cortex, ventromedial prefrontal cortex, dorsomedial prefrontal cortex, and subgenual cingulate cortex. (Lines at lower right indicate the positions of these axial slices within the brain. 54 © 2018 54
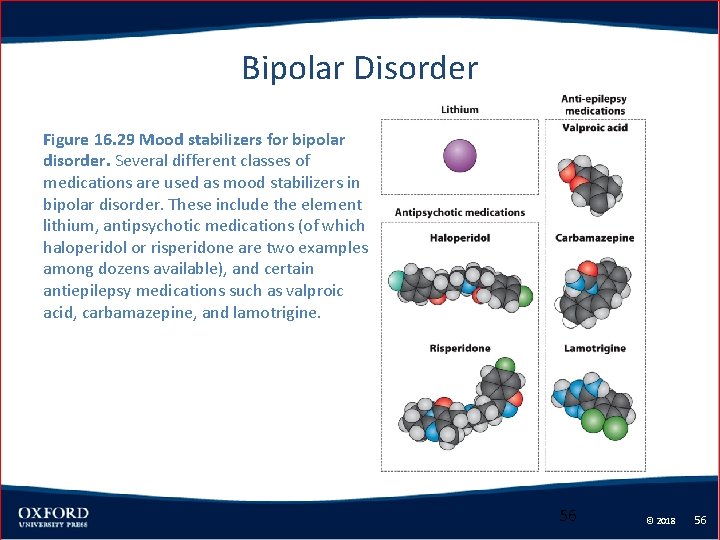
Bipolar Disorder • Common treatments include – Mood-stabilizing drugs, such as lithium – Anti-dpileptic drugs © 2018 55 55
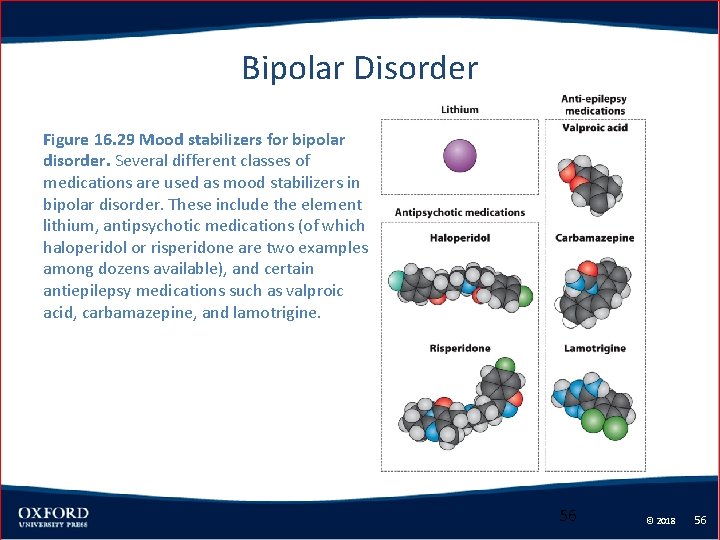
Bipolar Disorder Figure 16. 29 Mood stabilizers for bipolar disorder. Several different classes of medications are used as mood stabilizers in bipolar disorder. These include the element lithium, antipsychotic medications (of which haloperidol or risperidone are two examples among dozens available), and certain antiepilepsy medications such as valproic acid, carbamazepine, and lamotrigine. 56 © 2018 56
Depression: A Global Burden • • • Impact of Depression Causes of Depression Neurochemical Effects of Depression on Brain Functional Effect of Depression on the Brain Treatment of Depression © 2018 57 57
Impact of Depression • Depression is characterized by a low mood that makes it difficult to carry out the functions necessary for daily life. • Individuals with depression do not take pleasure in typical activities, lack motivation and energy, and have altered sleep patterns and appetite. © 2018 58 58
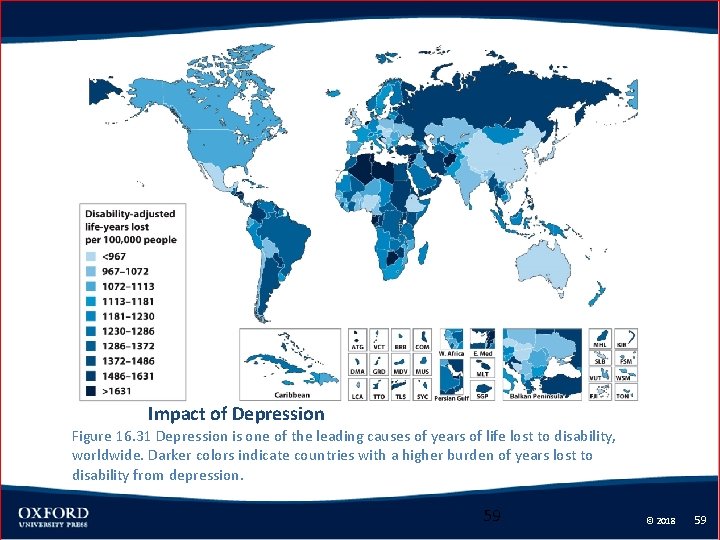
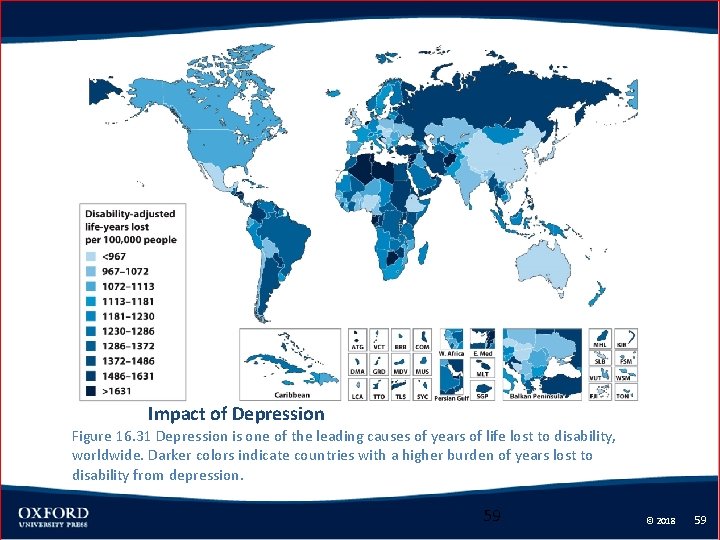
Impact of Depression Figure 16. 31 Depression is one of the leading causes of years of life lost to disability, worldwide. Darker colors indicate countries with a higher burden of years lost to disability from depression. 59 © 2018 59
Impact of Depression • The worldwide incidence of depression is 5% at any one time. • In the United States, the incidence is 5% for men and 10% for women. • Lifetime incidence is roughly double the onetime incidence rates. • The cost of depression is estimated to be about $80 billion per year in the U. S. © 2018 60 60
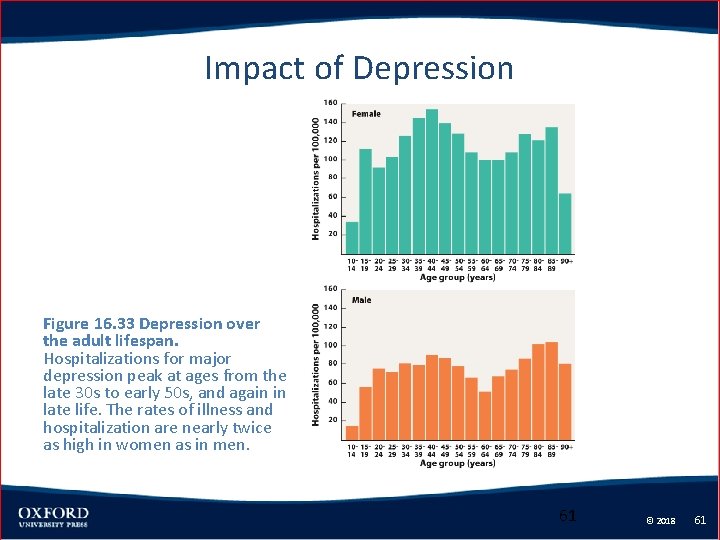
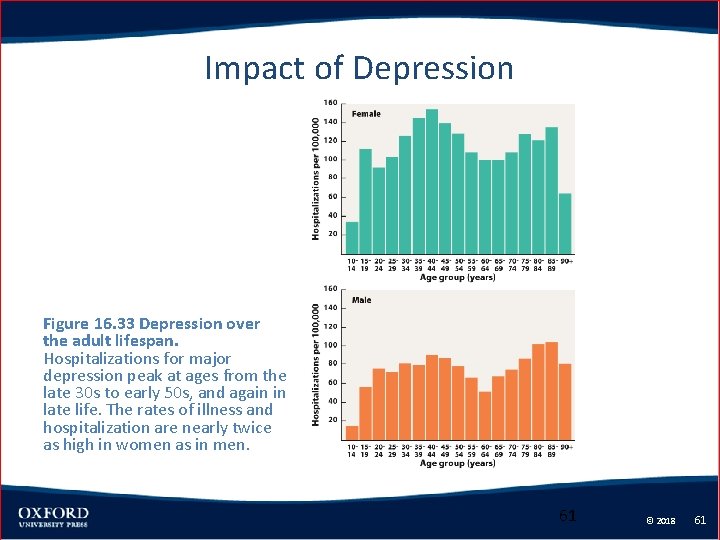
Impact of Depression Figure 16. 33 Depression over the adult lifespan. Hospitalizations for major depression peak at ages from the late 30 s to early 50 s, and again in late life. The rates of illness and hospitalization are nearly twice as high in women as in men. 61 © 2018 61
Causes of Depression • Mood disorders run in families, suggesting a genetic basis. • Depression may be an evolutionary adaptation to suffering a trauma or defeat • Depression causes the individual to stay away from opponents and predators while waiting for better times. © 2018 62 62

Causes of Depression Figure 16. 34 Interacting effects of genetic background and environmental events in depression. In one influential study (Caspi et al. , 2003), having two copies of the short form of the 5 HTTLPR serotonin transporter gene, as well as a more stressful life, significantly increased the individual’s chance of developing depression. 63 © 2018 63
Neurochemical Effects of Depression on Brain • Monoamine hypothesis of depression – There is a shortage of the monoamine neurotransmitters. – By inhibiting the enzyme monoamine oxidase, which breaks down these transmitters, mood will be improved. © 2018 64 64
Neurochemical Effects of Depression on Brain • Serotonin hypothesis – More specific than the monoamine hypothesis. – There is, specifically, a shortage of serotonin. – Selective serotonin reuptake inhibitors specifically affect serotonin levels. © 2018 65 65
Neurochemical Effects of Depression on Brain • Other biological theories – There abnormalities with glutamate neurotransmission. – There are low levels of the neuronal growth factor brain-derived neurotrophic factor (BDNF). © 2018 66 66

Neurochemical Effects of Depression on Brain Figure 16. 35 Selective serotonin reuptake inhibitors (SSRIs) work by blocking the reuptake of serotonin into the presynaptic terminal, thus increasing the concentration of serotonin in the synaptic cleft. 67 © 2018 67

Functional Effect of Depression on the Brain • Networks of brain areas are under- and overactivated in individuals with depression. – The subgenual cingulate cortex is consistently hyperactive. – This hyperactivity returns to normal following successful treatment of depression. – The dorsolateral and dorsomedial prefrontal cortex tend to be less active. © 2018 68 68

Functional Effect of Depression on the Brain Figure 16. 36 The subgenual cingulate cortex plays a key role in regulating the amygdala and other core limbic structures, and it is overactive in major depression. It is part of a larger network of cortical and subcortical regions involved in emotion regulation. In patients who recover from depression, the activity of the subgenual cingulate cortex returns to normal—a consistent finding across many different types of treatment for depression, including medications, therapy, and brain stimulation. 69 © 2018 69
Functional Effect of Depression on the Brain • The pattern of hyper- and hypo-active brain regions differs across individuals. • Current research is examining the interactions between different brain regions. © 2018 70 70

Treatment of Depression • Three major treatments are used for individuals with depression – Psychotherapy – Pharmacotherapy – Somatic therapy © 2018 71 71
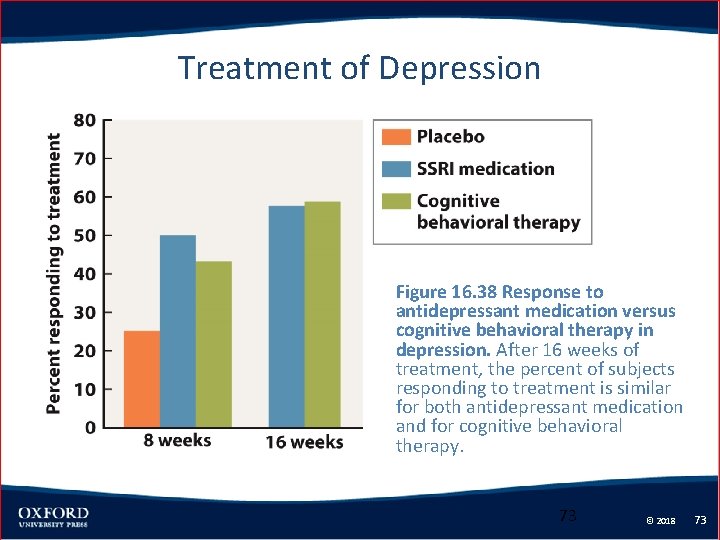
Treatment of Depression • In psychotherapy, the patient interacts with a clinician to work through the causes of their depression. • Cognitive therapy is about as effective as pharmacotherapy • The effects seem to persist for a longer time than the medication does. © 2018 72 72
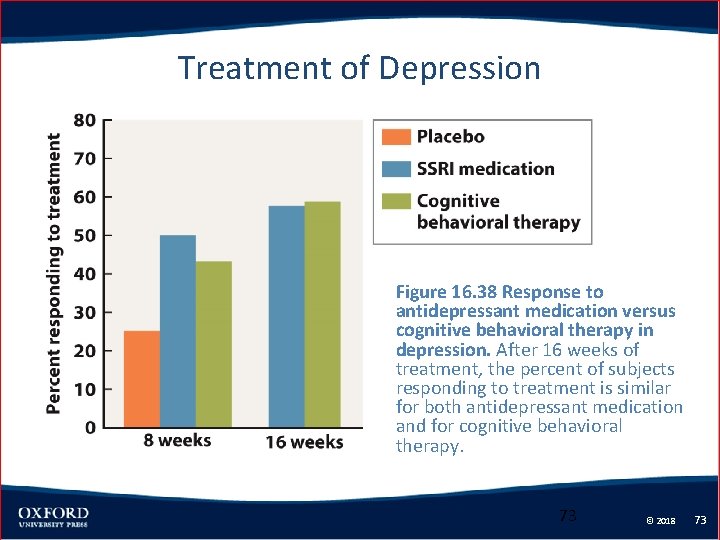
Treatment of Depression Figure 16. 38 Response to antidepressant medication versus cognitive behavioral therapy in depression. After 16 weeks of treatment, the percent of subjects responding to treatment is similar for both antidepressant medication and for cognitive behavioral therapy. 73 © 2018 73
Treatment of Depression • Anti-depressant medications include – Monoamine oxidase inhibitors (MAOIs) – Tricyclic antidepressants (TCAs) – Selective serotonin reuptake inhibitors (SSRIs) • All of these are about equally effective. • Different medications are more or less effective for different individuals. © 2018 74 74

Treatment of Depression Figure 16. 37 Successfully alleviating the symptoms of depression is associated with a decrease in activity in the subgenual cingulate cortex. This proved to be true not just for patients treated with an SSRI medication, but even for patients who improved while taking a placebo. 75 © 2018 75
Treatment of Depression • Somatic therapies are more invasive. • These include – Repetitive transcranial magnetic stimulation – Electroconvulsive therapy – Deep brain stimulation © 2018 76 76
 Psychiatric disorders
Psychiatric disorders Cognitive modelling
Cognitive modelling Cognitive and non cognitive religious language
Cognitive and non cognitive religious language Legal issues in psychiatric nursing
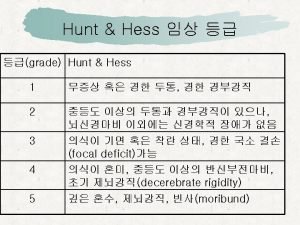
Legal issues in psychiatric nursing Wfns grading scale
Wfns grading scale Neuro wdl
Neuro wdl Motor function neurological assessment
Motor function neurological assessment What is focal neurological signs
What is focal neurological signs Neurological assessment chart
Neurological assessment chart Is adhd a neurological disorder
Is adhd a neurological disorder Mrc scale
Mrc scale Villa fridheim haapsalu
Villa fridheim haapsalu Neurological based behavior
Neurological based behavior Neurological examination
Neurological examination Muscle power neurological examination
Muscle power neurological examination Neurological exam
Neurological exam Compare and contrast first and second language acquisition
Compare and contrast first and second language acquisition Trait theory criminology
Trait theory criminology Solent msk physiotherapy
Solent msk physiotherapy Neurological examination
Neurological examination Neurological disease
Neurological disease Uw neurological surgery
Uw neurological surgery Normal pressure hydrocephalus triad
Normal pressure hydrocephalus triad Neurological observations glasgow coma scale
Neurological observations glasgow coma scale Psychiatric nursing meaning
Psychiatric nursing meaning Assessment skills
Assessment skills Nursing diagnosis format
Nursing diagnosis format History of psychiatric nurse
History of psychiatric nurse Cmc psychiatric hospital
Cmc psychiatric hospital Role of psychiatric nurse
Role of psychiatric nurse A behavioral crisis is most accurately defined as
A behavioral crisis is most accurately defined as Psychiatric security review board
Psychiatric security review board Psychiatric rehabilitation
Psychiatric rehabilitation Psychiatric nurse conference
Psychiatric nurse conference American psychiatric association annual meeting 2020
American psychiatric association annual meeting 2020 Northeast florida state hospital
Northeast florida state hospital Liberty hill academy
Liberty hill academy Southern psychiatric association
Southern psychiatric association Chronic insomnia
Chronic insomnia Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Psychiatric emergency
Psychiatric emergency Psychiatric emergency
Psychiatric emergency Calgary family assessment model
Calgary family assessment model Defense mechanisms nursing
Defense mechanisms nursing Nature neuroscience
Nature neuroscience Usc neuroscience undergraduate
Usc neuroscience undergraduate Dynamical systems neuroscience
Dynamical systems neuroscience James lange theory
James lange theory Cornell university neuroscience
Cornell university neuroscience Federation of european neuroscience societies
Federation of european neuroscience societies Developmental neuroscience textbook
Developmental neuroscience textbook Via indiretta gangli della base
Via indiretta gangli della base Collaborative neuroscience network
Collaborative neuroscience network Unsolved problems in neuroscience
Unsolved problems in neuroscience Fundamentals of computational neuroscience
Fundamentals of computational neuroscience Psb ucf
Psb ucf Systems neuroscience textbook
Systems neuroscience textbook Chess addiction treatment
Chess addiction treatment Neuroscience example
Neuroscience example Australasian neuroscience nurses association
Australasian neuroscience nurses association Neuroscience example
Neuroscience example Neuroscience psychology
Neuroscience psychology Porter neuroscience research center
Porter neuroscience research center Nolte
Nolte Neuroscience
Neuroscience Nature neuroscience
Nature neuroscience Jelle bruineberg
Jelle bruineberg Neuroscience afms
Neuroscience afms Matlab neuroscience tutorial
Matlab neuroscience tutorial Uw madison neuroscience
Uw madison neuroscience Unit 14 physiological disorders examples
Unit 14 physiological disorders examples Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Assistive technology for emotional disturbance
Assistive technology for emotional disturbance Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Neurotic stress related and somatoform disorders
Neurotic stress related and somatoform disorders