1162022 1 Sterile Body Fluids types types Specimen
1/16/2022 1

Sterile Body Fluids (types, types Specimen Collection and Transport ) 1/16/2022 2
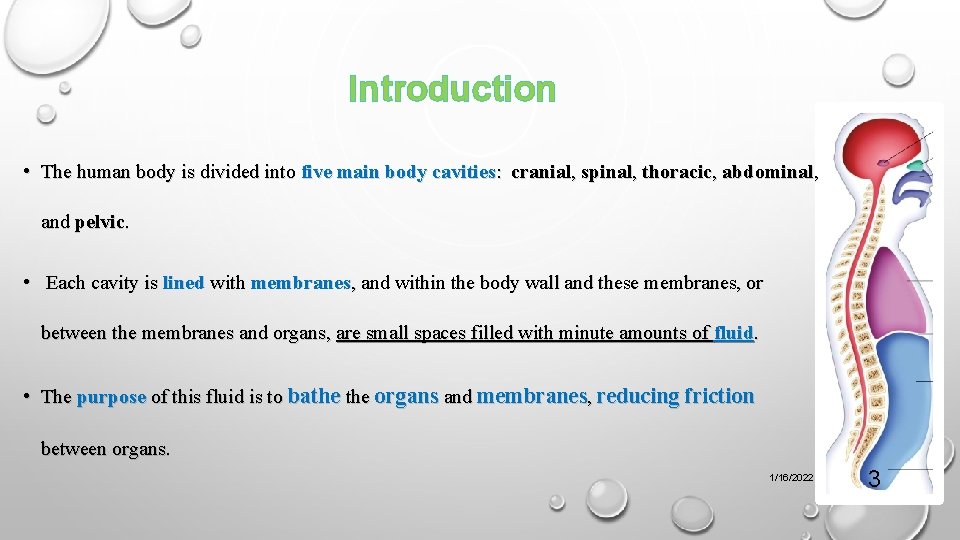
Introduction • The human body is divided into five main body cavities: cranial, spinal, thoracic, abdominal, and pelvic. • Each cavity is lined with membranes, and within the body wall and these membranes, or between the membranes and organs, are small spaces filled with minute amounts of fluid. • The purpose of this fluid is to bathe organs and membranes, reducing friction between organs. 1/16/2022 3
Introduction… • Bacteria, fungi, viruses, or parasites can invade any body tissue or sterile body fluid site. • Therefore even one colony of a potentially pathogenic microorganism may be significant. • Infection of normally sterile body fluids often results in severe morbidity and mortality; therefore, rapid and accurate microbiological assessment of these samples is important to successful patient management. 1/16/2022 4
Introduction… • Most organisms infecting these sites are not difficult to culture, but finding a low number of commensal organisms does present an interpretative challenge. • Any microorganisms found where no resident microbiota is present must be considered significant. 1/16/2022 5
Introduction… • With the increased use of prostheses, immunosuppressive therapeutic regimens, and long-term care of individuals with chronic debilitating disease, the likelihood of true infection with this type of commensal organism has increased. • In response to infection, fluid may accumulate in any body cavity. 1/16/2022 6
A normally sterile sites : • Cerebrospinal fluid (CSF) • Pleural fluid • Peritoneal fluid • Pericardial fluid • Joint fluid 1/16/2022 7
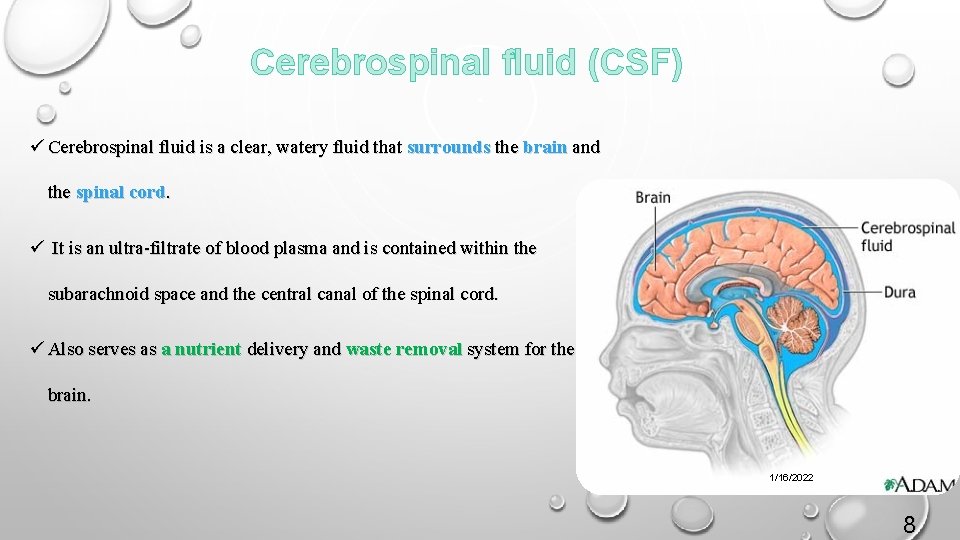
Cerebrospinal fluid (CSF) ü Cerebrospinal fluid is a clear, watery fluid that surrounds the brain and the spinal cord. ü It is an ultra-filtrate of blood plasma and is contained within the subarachnoid space and the central canal of the spinal cord. ü Also serves as a nutrient delivery and waste removal system for the brain. 1/16/2022 8
CSF… • The purpose of a CSF analysis is to diagnose medical disorders that affect the central nervous system. Some of these conditions are as follows: q Meningitis and encephalitis , which may be viral, bacterial, fungal, or parasitic infections q Metastatic tumors (e. g. , leukemia) and central nervous system tumors that shed cells into the CSF q Syphilis, a sexually transmitted bacterial disease q Bleeding (hemorrhaging) in the brain and spinal cord q Guillain-Barré, a demyelinating disease involving peripheral sensory and motor nerves 1/16/2022 9
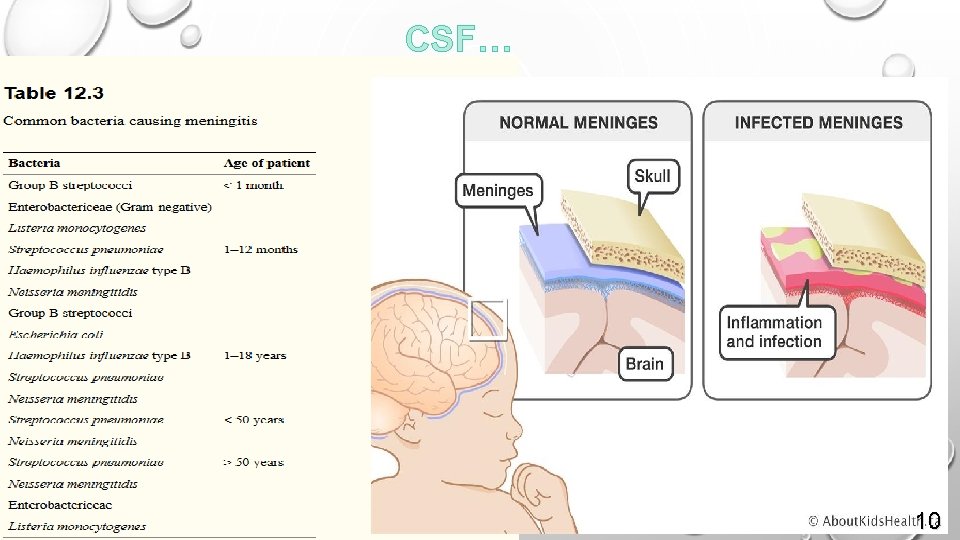
CSF… 1/16/2022 10
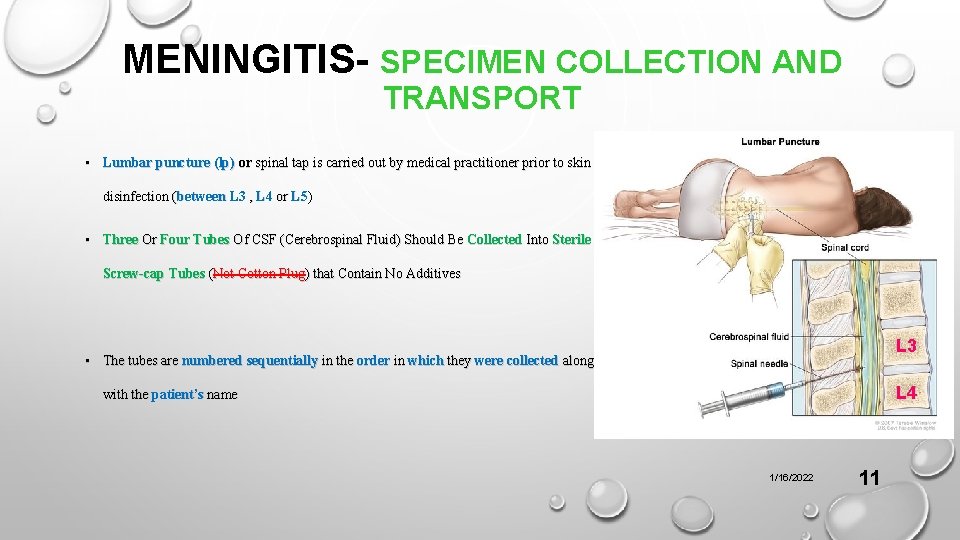
MENINGITIS- SPECIMEN COLLECTION AND TRANSPORT • Lumbar puncture (lp) or spinal tap is carried out by medical practitioner prior to skin disinfection (between L 3 , L 4 or L 5) • Three Or Four Tubes Of CSF (Cerebrospinal Fluid) Should Be Collected Into Sterile Screw-cap Tubes (Not Cotton Plug) that Contain No Additives L 3 • The tubes are numbered sequentially in the order in which they were collected along L 4 with the patient’s name 1/16/2022 11
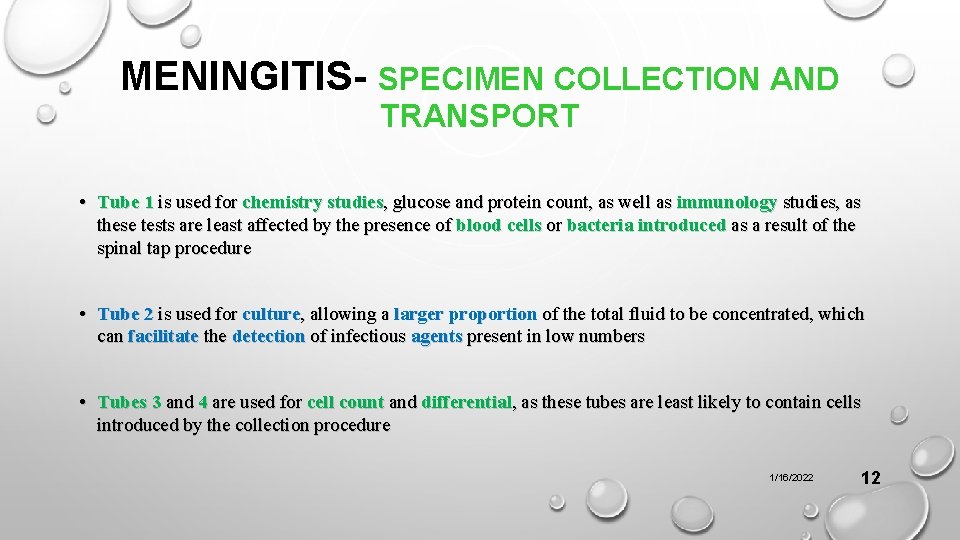
MENINGITIS- SPECIMEN COLLECTION AND TRANSPORT • Tube 1 is used for chemistry studies, glucose and protein count, as well as immunology studies, as these tests are least affected by the presence of blood cells or bacteria introduced as a result of the spinal tap procedure • Tube 2 is used for culture, allowing a larger proportion of the total fluid to be concentrated, which can facilitate the detection of infectious agents present in low numbers • Tubes 3 and 4 are used for cell count and differential, as these tubes are least likely to contain cells introduced by the collection procedure 1/16/2022 12
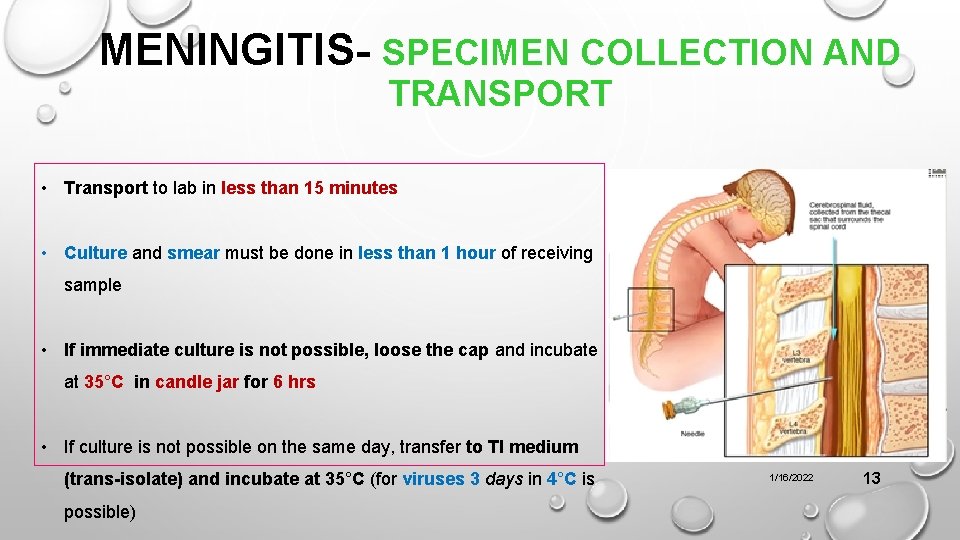
MENINGITIS- SPECIMEN COLLECTION AND TRANSPORT • Transport to lab in less than 15 minutes • Culture and smear must be done in less than 1 hour of receiving sample • If immediate culture is not possible, loose the cap and incubate at 35°C in candle jar for 6 hrs • If culture is not possible on the same day, transfer to TI medium (trans-isolate) and incubate at 35°C (for viruses 3 days in 4°C is possible) 1/16/2022 13
CSF… Cases of non-acceptance of CSF samples by the laboratory 1. Tubes without the relevant specifications 2. Tubes without numbering 3. Samples containing blood clots 4. Tubes containing less than 0. 5 ml of CSF fluid 5. Samples that are left in the section more than usual 1/16/2022 14
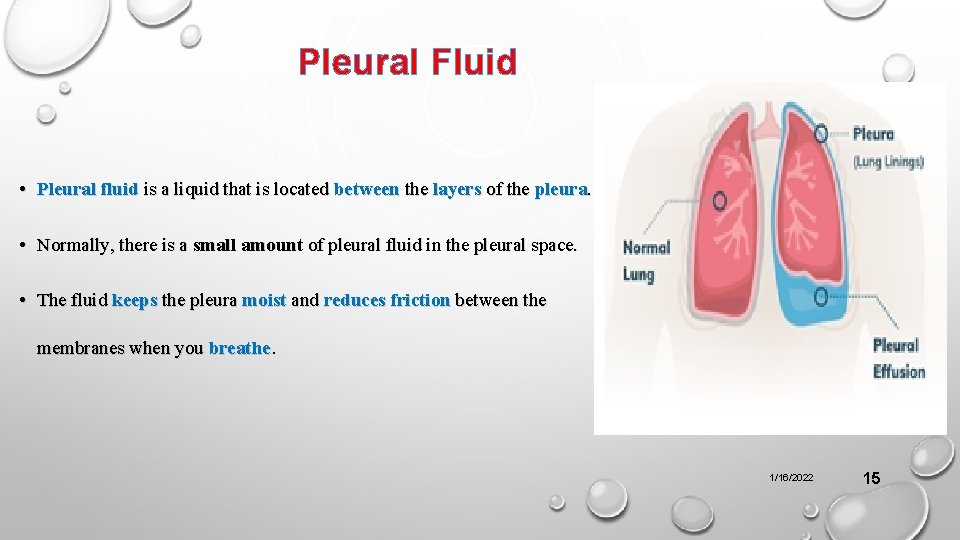
Pleural Fluid • Pleural fluid is a liquid that is located between the layers of the pleura. • Normally, there is a small amount of pleural fluid in the pleural space. • The fluid keeps the pleura moist and reduces friction between the membranes when you breathe. 1/16/2022 15
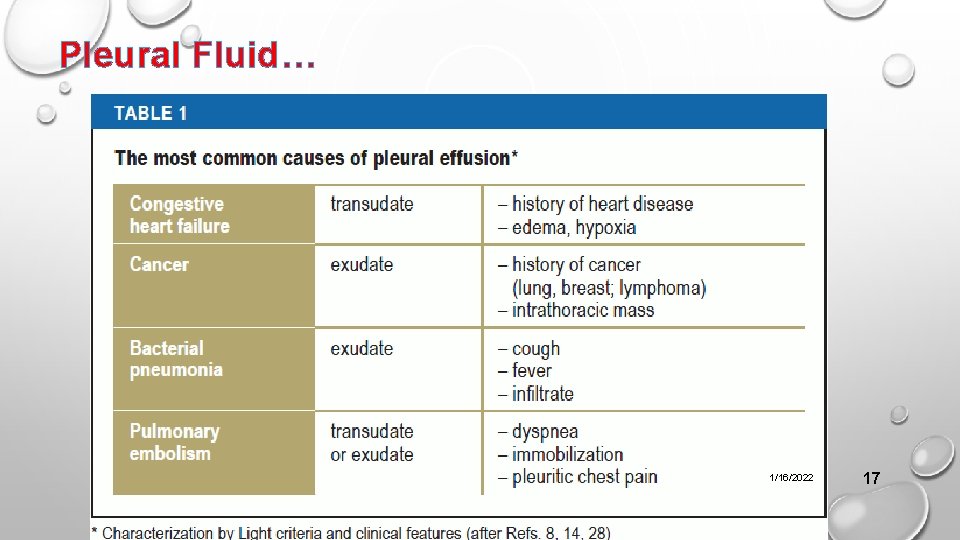
Pleural Fluid… • A pleural fluid analysis is used to find the cause of pleural effusion. There are two main types of pleural effusion: • Transudate, which happens when there is an imbalance of pressure in certain blood vessels. This causes extra fluid to leak into the pleural space. Transudate pleural effusion is most often caused by heart failure or cirrhosis. • Exudate, which happens when there is an injury or inflammation of the pleura. This can make excess fluid leak out of certain blood vessels. Exudate pleural effusion has many causes. These include infections such as pneumonia, cancer, kidney disease, and autoimmune diseases. It commonly affects only one side of the chest. 1/16/2022 16
Pleural Fluid… 1/16/2022 17
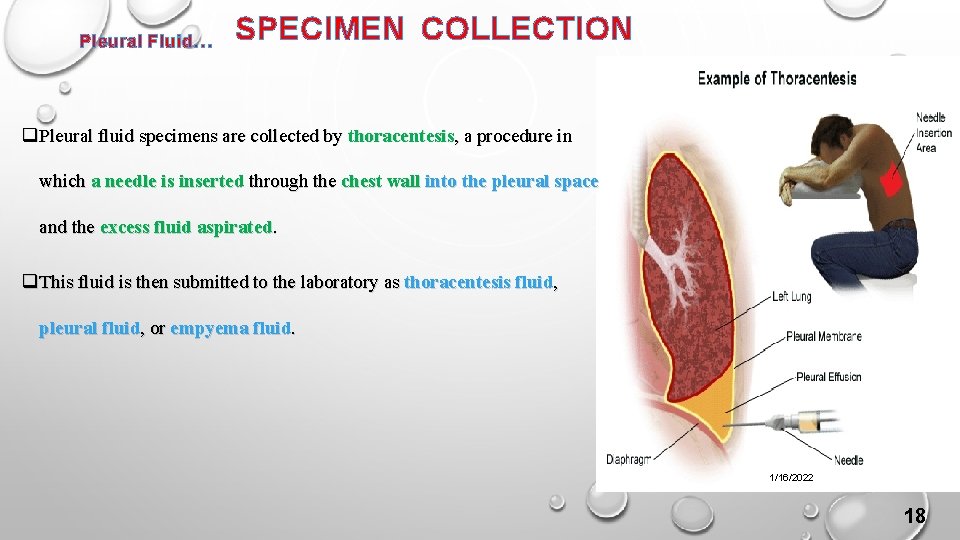
Pleural Fluid… SPECIMEN COLLECTION q Pleural fluid specimens are collected by thoracentesis, a procedure in which a needle is inserted through the chest wall into the pleural space and the excess fluid aspirated. q This fluid is then submitted to the laboratory as thoracentesis fluid, pleural fluid, or empyema fluid. 1/16/2022 18
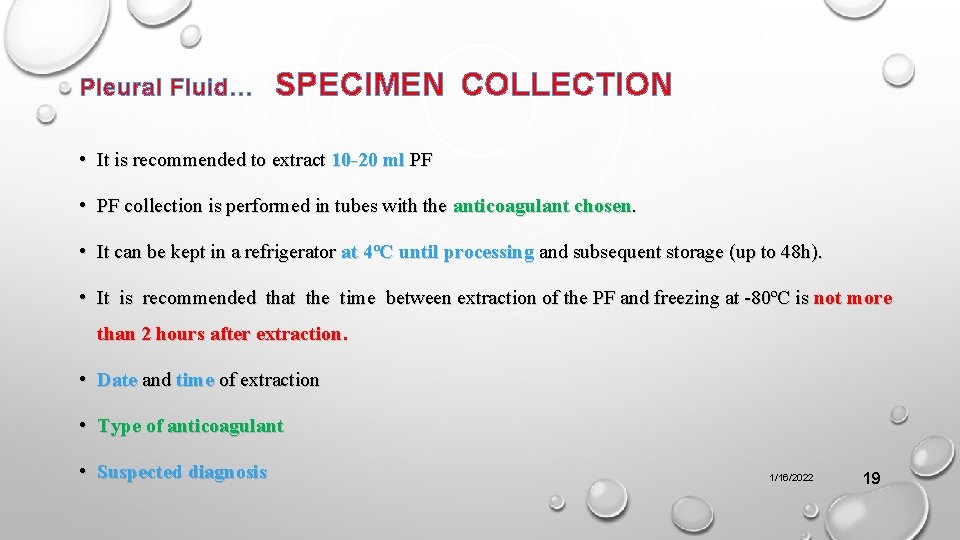
Pleural Fluid… SPECIMEN COLLECTION • It is recommended to extract 10 -20 ml PF • PF collection is performed in tubes with the anticoagulant chosen. • It can be kept in a refrigerator at 4ºC until processing and subsequent storage (up to 48 h). • It is recommended that the time between extraction of the PF and freezing at -80ºC is not more than 2 hours after extraction. • Date and time of extraction • Type of anticoagulant • Suspected diagnosis 1/16/2022 19
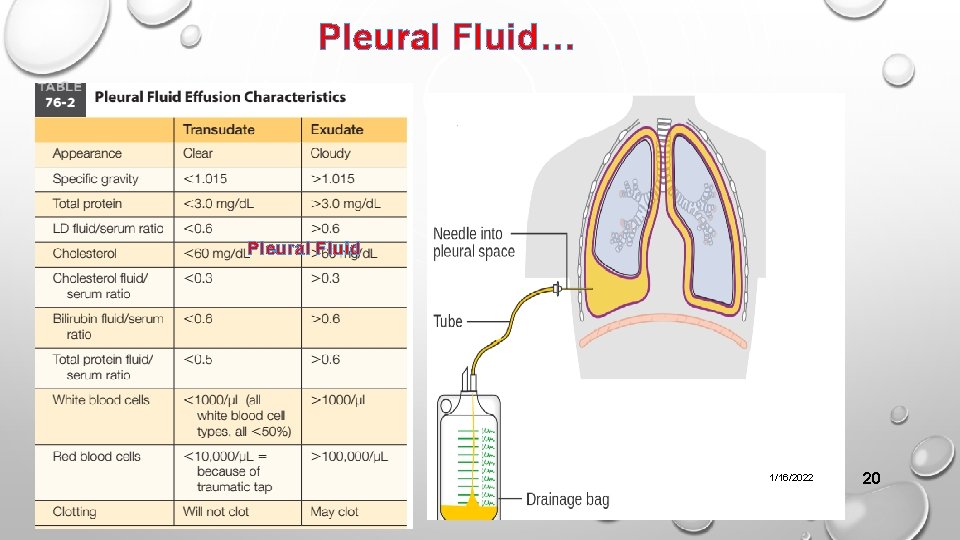
Pleural Fluid… Pleural Fluid 1/16/2022 20
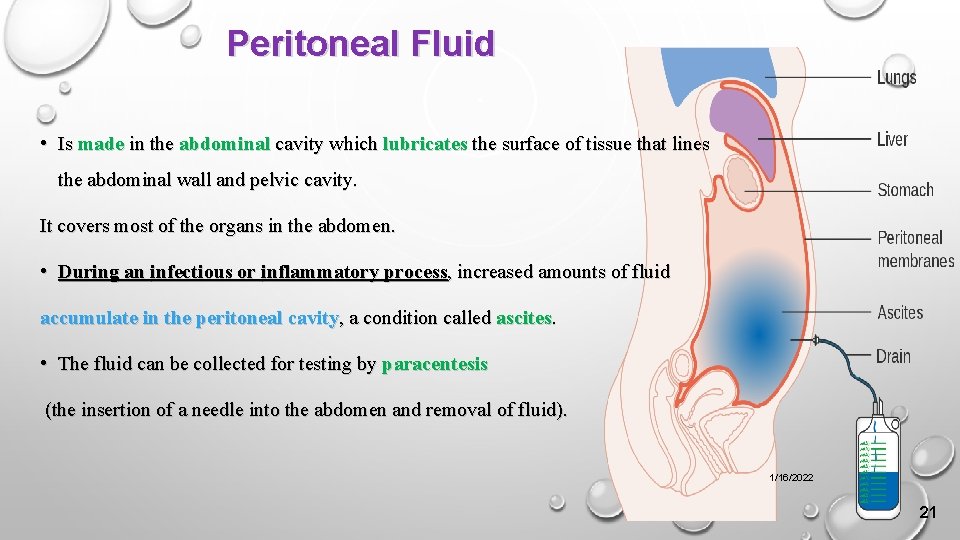
Peritoneal Fluid • Is made in the abdominal cavity which lubricates the surface of tissue that lines the abdominal wall and pelvic cavity. It covers most of the organs in the abdomen. • During an infectious or inflammatory process, increased amounts of fluid accumulate in the peritoneal cavity, a condition called ascites. • The fluid can be collected for testing by paracentesis (the insertion of a needle into the abdomen and removal of fluid). 1/16/2022 21
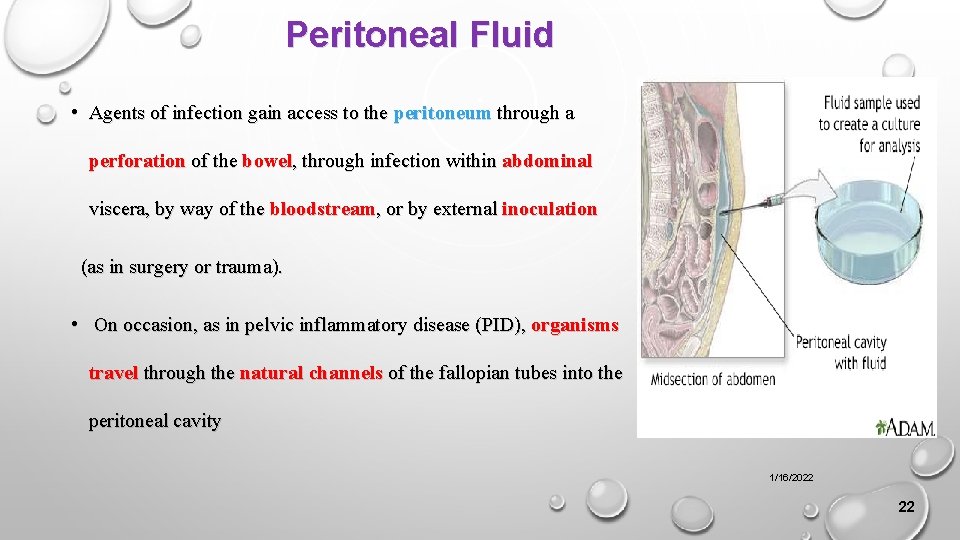
Peritoneal Fluid • Agents of infection gain access to the peritoneum through a perforation of the bowel, through infection within abdominal viscera, by way of the bloodstream, or by external inoculation (as in surgery or trauma). • On occasion, as in pelvic inflammatory disease (PID), organisms travel through the natural channels of the fallopian tubes into the peritoneal cavity 1/16/2022 22
Peritoneal Fluid… PERITONITIS • Peritonitis results when the peritoneal membrane becomes inflamed and can be either primary or secondary. • Primary peritonitis is rare and results when infection spreads from the blood and lymph nodes with no apparent evidence of infection. • The most common etiologic agents in children are Streptococcus pneumoniae and group A streptococci, Enterobacteriaceae, other gram-negative bacilli, and staphylococci. • In adults, Escherichia coli is the most common bacterium. • Secondary peritonitis is a complication of a perforated viscus (organ), surgery, traumatic injury, loss of bowel wall integrity (e. g. , ulcerative colitis, ruptured appendix, carcinoma), obstruction, or a preceding infection (liver abscess, salpingitis, septicemia). 1/16/2022 23
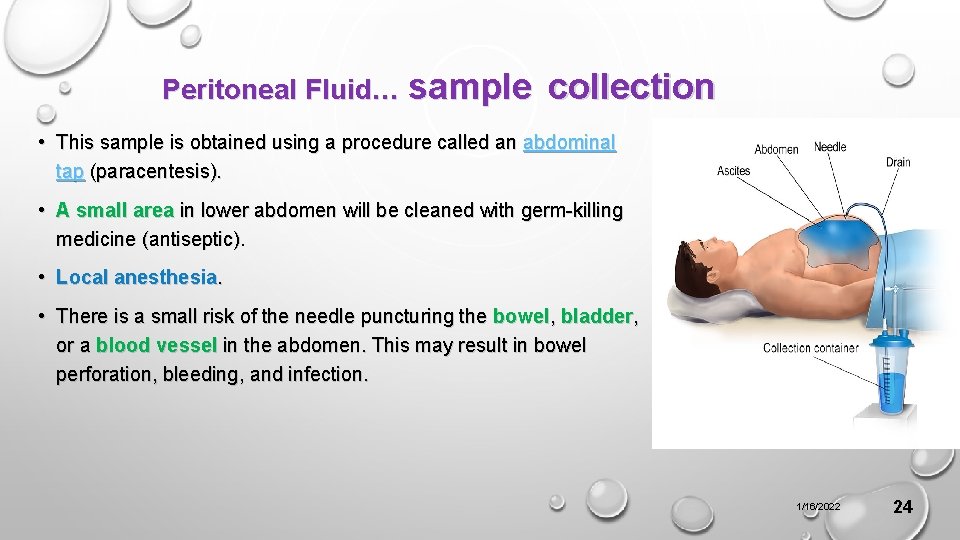
Peritoneal Fluid… sample collection • This sample is obtained using a procedure called an abdominal tap (paracentesis). • A small area in lower abdomen will be cleaned with germ-killing medicine (antiseptic). • Local anesthesia. • There is a small risk of the needle puncturing the bowel, bladder, or a blood vessel in the abdomen. This may result in bowel perforation, bleeding, and infection. 1/16/2022 24
Peritoneal Dialysis Fluid • Because the dialysate fluid is injected into the peritoneal cavity via a catheter, the break in the skin barrier places the dialysis patient at significant risk for infection. • Peritonitis is diagnosed by the presence of two of the following: cloudy dialysate, abdominal pain, or a positive culture from dialysate. • Most infections originate from the patient’s ow`n skin flora; S. epidermidis and S. aureus • The oxygen content of peritoneal dialysate is usually too high for the development of anaerobic infection. 1/16/2022 25
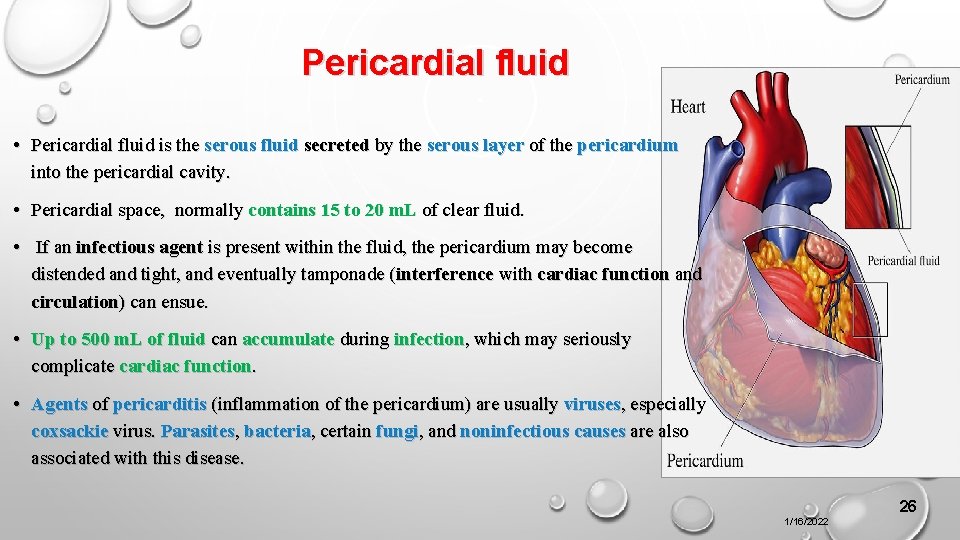
Pericardial fluid • Pericardial fluid is the serous fluid secreted by the serous layer of the pericardium into the pericardial cavity. • Pericardial space, normally contains 15 to 20 m. L of clear fluid. • If an infectious agent is present within the fluid, the pericardium may become distended and tight, and eventually tamponade (interference with cardiac function and circulation) can ensue. • Up to 500 m. L of fluid can accumulate during infection, which may seriously complicate cardiac function. • Agents of pericarditis (inflammation of the pericardium) are usually viruses, especially coxsackie virus. Parasites, bacteria, certain fungi, and noninfectious causes are also associated with this disease. 26 1/16/2022
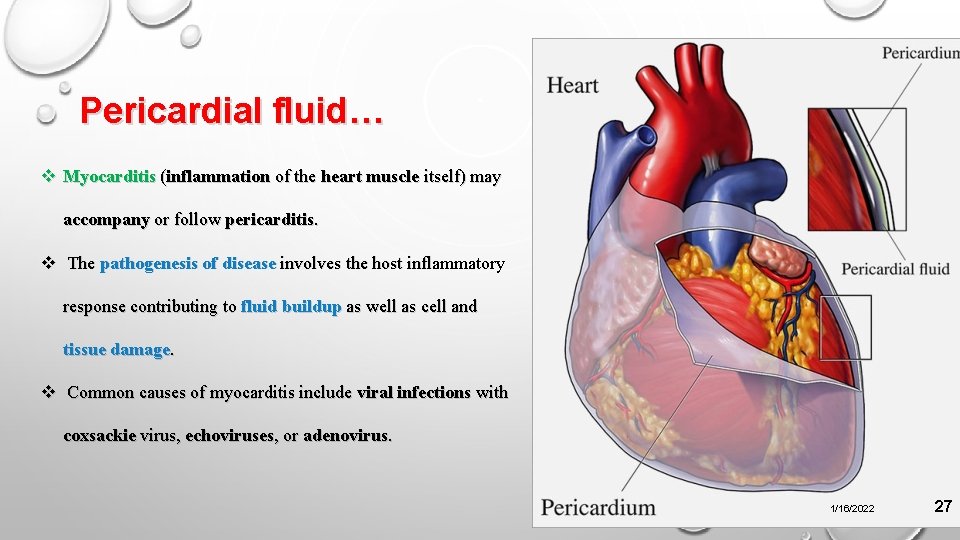
Pericardial fluid… v Myocarditis (inflammation of the heart muscle itself) may accompany or follow pericarditis. v The pathogenesis of disease involves the host inflammatory response contributing to fluid buildup as well as cell and tissue damage. v Common causes of myocarditis include viral infections with coxsackie virus, echoviruses, or adenovirus. 1/16/2022 27
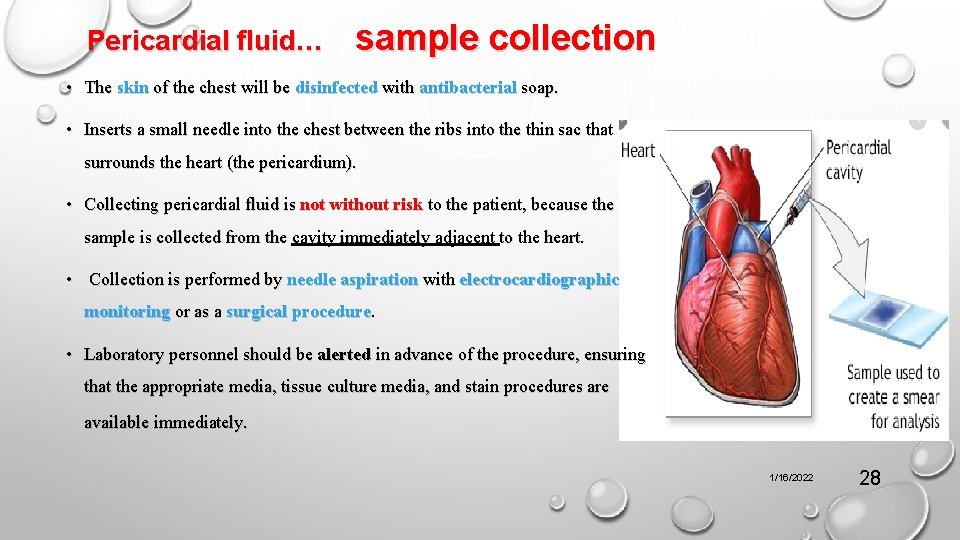
Pericardial fluid… sample collection • The skin of the chest will be disinfected with antibacterial soap. • Inserts a small needle into the chest between the ribs into the thin sac that surrounds the heart (the pericardium). • Collecting pericardial fluid is not without risk to the patient, because the sample is collected from the cavity immediately adjacent to the heart. • Collection is performed by needle aspiration with electrocardiographic monitoring or as a surgical procedure. • Laboratory personnel should be alerted in advance of the procedure, ensuring that the appropriate media, tissue culture media, and stain procedures are available immediately. 1/16/2022 28
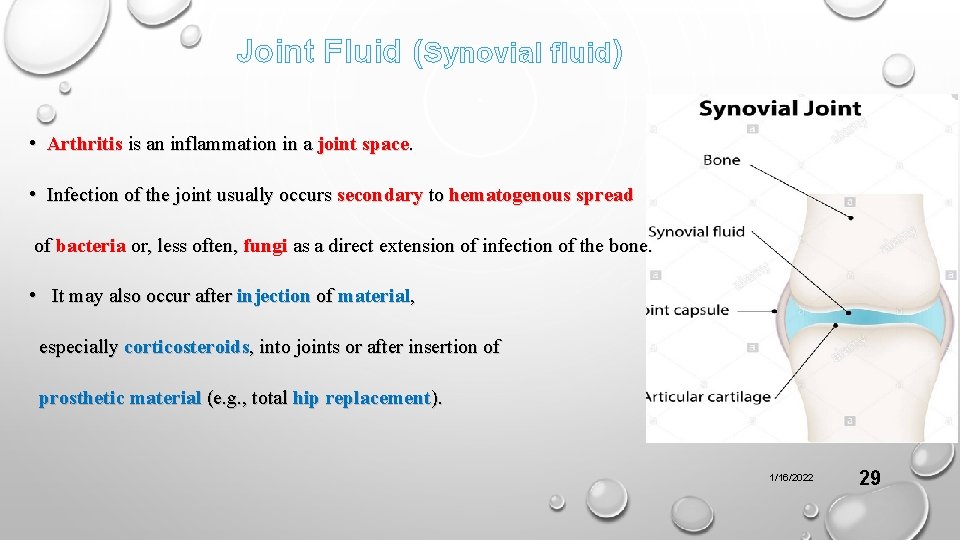
Joint Fluid (Synovial fluid) • Arthritis is an inflammation in a joint space. • Infection of the joint usually occurs secondary to hematogenous spread of bacteria or, less often, fungi as a direct extension of infection of the bone. • It may also occur after injection of material, especially corticosteroids, into joints or after insertion of prosthetic material (e. g. , total hip replacement). 1/16/2022 29
Joint Fluid… sample collection • The synovial fluid is obtained by aspiration of a joint. • About 1 ml is present in each large joint such as the knee, ankle, hip, elbow, wrist or shoulder. • The specimen is obtained only by a trained nurse or by the attending physician. • Dispatch of the specimen to the laboratory is done as early as possible. • Anticoagulant is added to the specimen which will be used for cell counting while fluoride is added to the specimen to be used for glucose analysis. 1/16/2022 30
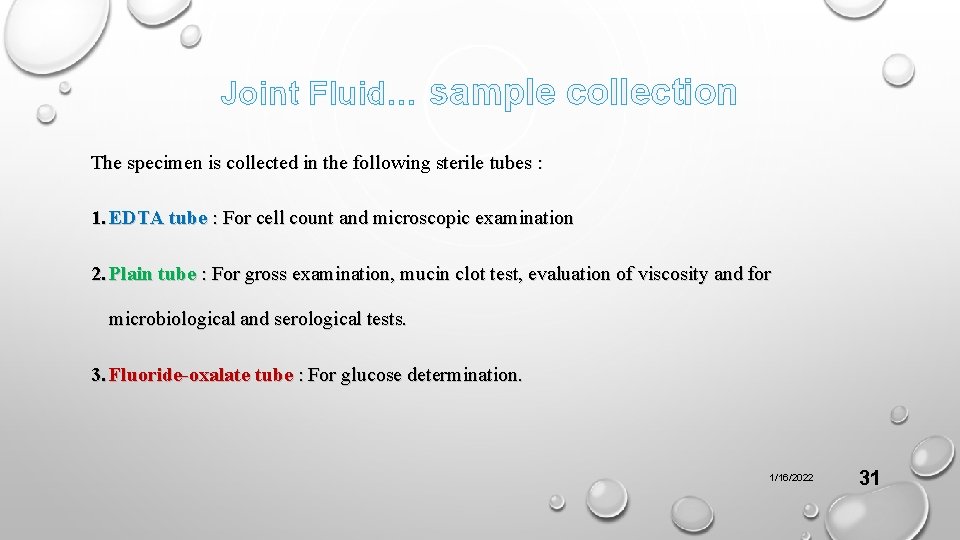
Joint Fluid… sample collection The specimen is collected in the following sterile tubes : 1. EDTA tube : For cell count and microscopic examination 2. Plain tube : For gross examination, mucin clot test, evaluation of viscosity and for microbiological and serological tests. 3. Fluoride-oxalate tube : For glucose determination. 1/16/2022 31
Joint Fluid… • Overall, S. aureus is the most common etiologic agent of septic arthritis, accounting for approximately 70% of infections. • In adults younger than 30 years of age, however, N. gonorrhoeae is commonly isolated. • Haemophilus influenzae has been the most common agent of bacteremia in children younger than 2 years of age, and consequently it has been the most common cause of infectious arthritis in these patients, followed by S. aureus. 1/16/2022 32
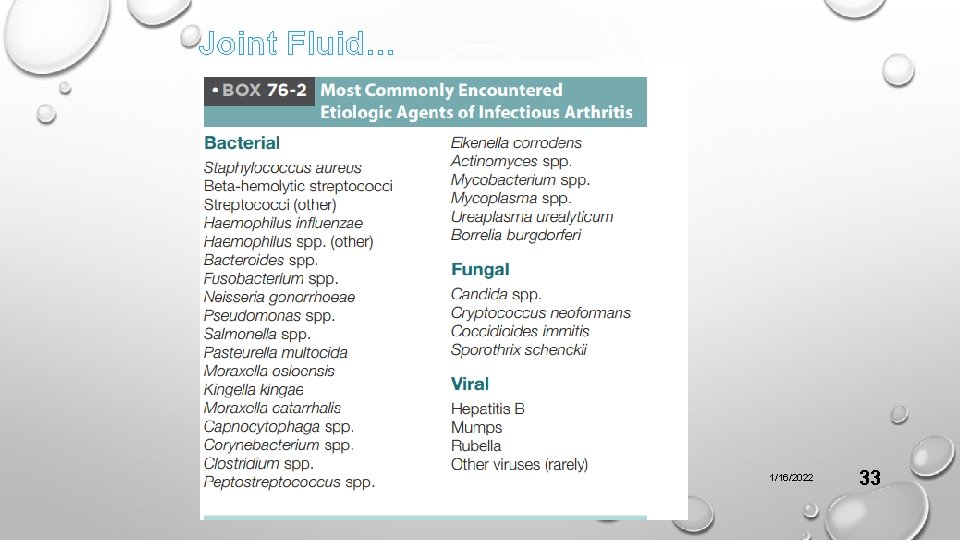
Joint Fluid… 1/16/2022 33
Specimen Collection and Transport • Most specimens (pleural, peritoneal, pericardial, and synovial fluids) are collected by aspiration with a needle and syringe. • Body fluids from sterile sites should be transported to the laboratory in a sterile tube or airtight vial. • Between 1 and 5 m. L of specimen is adequate for isolation of most bacteria, but the larger the specimen, the better, particularly for isolation of Mycobacterium tuberculosis and fungi; at least 5 m. L should be submitted for recovery of these organisms. 1/16/2022 34
Specimen Collection and Transport • Ten milliliters of fluid is recommended for the diagnosis of peritonitis. • Anaerobic transport vials is needed. • These vials are prepared in an oxygen-free atmosphere and are sealed with a rubber septum or short stopper through which the fluid is injected. • Transportation of fluid in a syringe capped with a sterile rubber stopper is not recommended. • Most clinically significant anaerobic bacteria survive adequately in aerobic transport containers (e. g. , sterile, screw-capped tubes) for short periods if the specimen is purulent and of adequate volume. 1/16/2022 35
Specimen Collection and Transport • However, collection in anaerobic transport media is recommended. • Specimens received in anaerobic transport vials should be inoculated to routine aerobic (an enriched broth, blood, chocolate, and sometimes Mac. Conkey agar plates) and anaerobic media as quickly as possible. • Specimens for recovery of fungi or mycobacteria may be transported in sterile, screw-capped tubes. • At least 5 to 10 m. L of fluid are required for adequate recovery of small numbers of organisms. • If gonococci or chlamydia are suspected, additional aliquots should be sent to the laboratory for smears and appropriate cultures. 1/16/2022 36
Specimen Collection and Transport v Percutaneous catheters are placed during many surgical procedures to prevent the accumulation of exudate and blood at the operative site. v Often, the laboratory receives drainage fluids from these catheters for culture when signs and symptoms suggest infection. v However, culture of such fluid is potentially misleading when the fluid becomes contaminated within the catheter or collection device, or when the fluid does not originate from a site of the infection. ü Direct aspiration of potentially infected fluid collections rather than catheter drainage fluid. 1/16/2022 37

Thank you 1/16/2022 38
- Slides: 38